Abstract
Key Clinical Message
Rituximab which is established as a main treatment for pemphigus vulgaris can be a potential causative factor for development of psoriasis in some patients. It is preferred to avoid using rituximab in patients who had a history of psoriasis. Acquainting medical doctors about rituximab‐related cutaneous complications will help them in detection and management.
Abstract
Rituximab is a human/murine monoclonal antibody targeting the CD20 antigen on B‐lymphocytes surface. Although it is used as promising treatment for pemphigus, nowadays it is also a new therapy for other autoimmune diseases including systemic lupus erythematosus and rheumatoid arthritis, and others like non‐Hodgkin's lymphoma. Although there is increasing evidence regarding the safety and effectiveness of rituximab in these diseases, many cutaneous adverse effects have been reported. Here, we describe a 48‐years‐old patient affected with pemphigus vulgaris who developed psoriatic lesions on her on scalp, trunk, and extremities, 4 months after the second course of rituximab.
Keywords: pemphigus, psoriasis, rituximab‐induced psoriasis
1. INTRODUCTION
Psoriasis and pemphigus are two chronic inflammatory immune mediated cutaneous disorders. Rituximab (RTX) is a chimeric murine/human anti‐CD20 monoclonal antibody known as a potential drug for the treatment of pemphigus vulgaris. It is administrated via intravenous infusion. 1 Here we present a case of a 48‐year‐old patient affected with pemphigus vulgaris and developed psoriatic plaques on her scalp, trunk, and extremities 4 months after the second course of RTX.
2. CASE HISTORY/EXAMINATION
A 48‐year‐old female known case of pemphigus vulgaris, presented to our dermatology clinic with a 2 month history of pruritic lesions on the scalp, trunk, and extremities (Figure 1).
FIGURE 1.
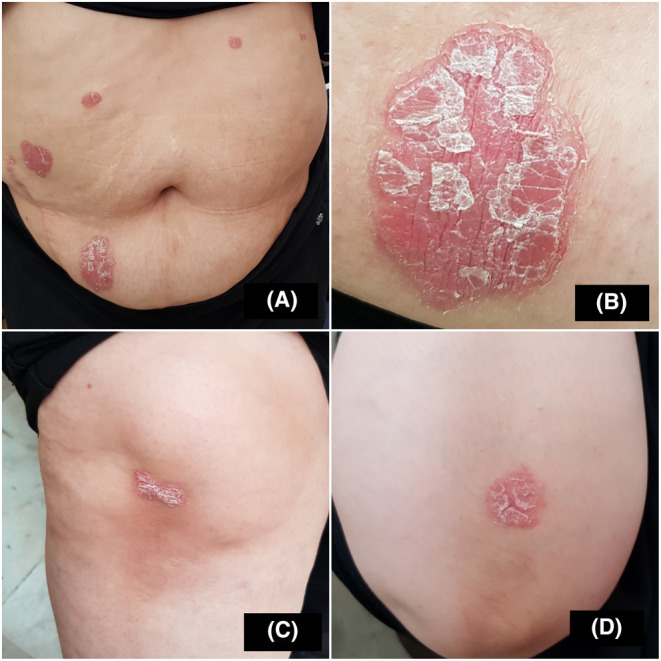
Multiple scaly erythematous plaques on the abdomen (A, B), extensor surfaces of the lower (C) and upper (D) extremities.
The patient had been diagnosed with mucocutaneous pemphigus vulgaris from 16 years earlier. She had received multiple courses of corticosteroid pulse therapy, followed by maintenance treatment with oral prednisolone. Four months before the current presentation, the patient was admitted due to pemphigus recurrence (Figure 2) and treated with a course of RTX (two infusions of 1 g 2 weeks apart) in addition to 30 mg of oral prednisolone. One month later, she had complete resolution for her skin lesions, and prednisolone was tapered gradually to 10 mg/day.
FIGURE 2.

Photo of patient when she had pemphigus vulgaris; multiple erosions on trunk.
Physical examination revealed multiple sharply demarcated, scaly, and erythematous plaques distributed over the scalp, retroauricular area, abdomen, presacral, and extensor surfaces of the extremities (PASI score 14.1). Examination of nails, mucosa, and joints was normal.
3. DIFFERENTIAL DIAGNOSIS, INVESTIGATIONS AND TREATMENT
Skin biopsy revealed psoriasiform acanthosis, munds of parakeratosis, and suprapapillary plate thinning. Papillary dermis showed vascular tortuosity and perivascular lymphocytic infiltration compatible with the diagnosis of psoriasis. Laboratory tests, including complete blood count, lipid profile, liver function tests, urea, creatinine, ESR, and CRP, were normal. We administered treatment for psoriasis included tablet methotrexate 7.5 mg/week and topical clobetasol.
4. OUTCOMES AND FOLLOW UP
During 6 months' of follow‐up, psoriatic plaques had partially improved (PASI score = 3.2), and no other sites were involved. The patient was maintained on oral methotrexate (10 mg/week), and prednisolone was also tapered to 2.5 mg/day.
5. DISCUSSION
The exact underlying mechanism for the association between psoriasis and RTX is still unclear, but there are various hypotheses that could clarify this relationship to some extent.
First of all, RTX leads to B‐cell depletion, resulting in the elimination of B‐cell regulation on T‐cell and therefore T‐cell activation. 2 , 3 Since psoriasis has been regarded as a T‐cell‐driven disease, the T‐cell dysregulation after RTX therapy might be responsible for the development of psoriasis. 3
RTX, which is widely used for treatment of pemphigus vulgaris, can be a potential contributing factor for the development of psoriatic plaques in some patients. Several psoriasis cases have been reported following RTX administration in previous studies (Table 1).
TABLE 1.
Review of literature for rituximab‐induced psoriasis for a variety of underlying disorders.
| Author | Underlying disease | Age | Sex | Type of lesions | Time onset | Treatment |
|---|---|---|---|---|---|---|
| Dae‐Woo Kim 4 | NHL | 6 | M | Psoriatic plaques on shoulder, chest, abdomen, back and scalp | 3 month after starting RTX | Topical corticosteroid |
| Mielke 5 | NHL | 66 | F | Psoriatic arthritis onycholysis tenosynovitis of the Achilles tendon | 6–8 weeks | Methotrexate 15 mg/week including initial prednisolone 20 mg/d |
| Venables 6 | NHL | 53 | F | Palmoplantar pustulosis psoriasis | About 2–3 weeks after each cycle | Self‐limited Topical corticosteroid |
| Shouvik Dass 7 | RA | 17 | F | Scalp psoriasis onycholysis, pan‐uveitis, and ruptures of the Achilles tendon | 6 months | Not reported |
| Markatseli 2 | RA | 55 | F | Plaques on arms and thighs | 6 month after first course and 10 days after second | Not reported |
| Shouvik Dass 7 | RA | 52 | F | Psoriatic plaques over both knees and on the extensor surfaces of thighs. | 12 month | Topical corticosteroid |
| Alexandra Maria Giovanna Brunasso, 8 | RA | 45 | F | Plantar pustlosis | 3 month | Topical clobetasol Intramuscular methotrexate at 15 mg/week |
| Guidelli 9 | RA | 69 | F | Psoriatic papuloplaques on her trunk and arms | 3 months (14 weeks after first infusion) after the second course of rituximab | Topical fluticasone |
| Gulsen Ozen 10 | RA | 50 | F | Psoriatic patch‐plaque on extremities | Five months after 3rd cycle, 25 months after 1st infusion | Not reported |
| Hardcastle 11 | RA | 49 | F | Plantar pustular psoriasis nail changes. Two months later itchy, scaly patches around the ankles and heels were seen, including some well‐defined plaques | 4 weeks | Topical corticosteroid, topical salicylic acid, and coal |
| Jayasekera 12 | RA | 80 | F | Plantar pustular psoriasis | 2 years | Tocilizumab |
| Fiorillo 13 | ITP | 16‐month‐old | M | Psoriatic plaques on the legs, arms, back, and over the scalp over | 7 weeks |
Course of 6 weeks Methotrexate |
| Dass 7 | SLE | 26 | F | Psoriatic plaques on elbows and the extensor surfaces of arms and thighs, trunk, onycholysis | 4 month | Topical corticosteroid |
| Mok 14 | IMN | 51 | M | Psoriatic papulopustules over trunk and limbs | 4 month | Topical corticosteroid |
| Alahmar 3 | GPA | 38 | F | Plaques over the abdomen, and extensor surface of the upper and lower extremities bilaterally | Three months after the third course of RTX (18 months from the first course) | Subcutaneous adalimumab 40 mg every 2 weeks along with a topical corticosteroid |
Abbreviations: F, female; GPA, granulomatosis with polyangiitis; IMN, idiopathic membranous nephropathy; ITP, immune thrombocytopenic purpura; M, male; NHL, non‐Hodgkin lymphoma; RA, rheumatoid arthritis; RTX, rituximab; SLE, systemic lupus erythematosus.
According to the literature, in patients with RTX‐induced psoriasis, nail changes, pustular and plantar psoriasis, and psoriatic arthritis, as well as all the plaque type psoriasis were detected in patients. Psoriasis onset varied between 10 days and 2 years after the first course of RTX. In our case, psoriatic lesions developed 4 months after the second course of RTX.
Among the blistering disorders, Bullous pemphigoid is the most common auto‐immune bullous disease associated with psoriasis, 15 followed by pemphigus vulgaris, pemphigus foliaceous, 2 , 3 , 15 , 16 , 17 and herpetiform pemphigus. 16 On the other hand, less commonly, there are some reports of pemphigus preceding psoriasis similar to our case. 18 , 19
In a recent study recorded by Balighi et al., three patients with pemphigus vulgaris developed psoriasis; two of them did not receive RTX. 17 This may also highlight another contributing factor other than RTX. For instant, corticosteroids used for treatment of vesiculobullous diseases could be a trigger for psoriasis. 15 Furthermore, the role of spreading epitope may be a suggested etiology for this coincidence. According to this model, many proteins, which were not recognizable by immune system cells, become identifiable after the activation of a chronic autoimmune response that leads to a new autoimmune reaction (epitope phenomenon, 1998). 20
In 1987, Yokoo et al. reported a case of pemphigus foliaceous coexistence with psoriasis in one patient, focusing on the fact that the activation of plasminogen is involved in acantholysis in pemphigus. 18 Also, increased concentrations of plasminogen activator have been detected in psoriasis lesions. 18
Based on genome‐wide association studies, psoriasis and pemphigus are both related to HLA DRB1 alleles. 19 , 21 As a result, genetic factors may also play a remarkable role in the association between these two auto‐inflammatory skin diseases.
Some data mentioned that Th17 and neutrophils play an important role in the pathogenesis of psoriasis, which are stimulated by IL‐6. 22 A study was recorded by Zhong et al. mentioned that there is an increased level for IL‐6 and IL‐17A after administration of RTX, 23 which mean that it may have played a main role in our patient.
Rituximab has rarely been used to treat psoriasis 24 ; however, there are a few cases that have shown some improvement in psoriasis following RTX therapy. 25 , 26 According to our study and to previous recorded studies, it is better to avoid using RTX who had a history of psoriasis.
6. CONCLUSION
Rituximab is a human/murine monoclonal antibody targeting the CD20 antigen on B‐lymphocytes surface. Although it is used as a promising treatment for pemphigus, nowadays it is also a new therapy for other autoimmune diseases, including systemic lupus erythematous and rheumatoid arthritis, and others like non‐Hodgkin's lymphoma. Although there is increasing evidence regarding the safety and effectiveness of RTX in these diseases, psoriasis rarely occurs after RTX.
Physicians should be aware of this complication, and may be it is better to avoid using RTX who had a history of psoriasis. More studies should be recorded.
AUTHOR CONTRIBUTIONS
Leila Ghadirzade Arani: Resources; writing – original draft. Shima Moslemi Haghighi: Formal analysis; writing – original draft. Soheila Nasiri: Validation; visualization; writing – review and editing. Sahar Dadkhahfar: Writing – review and editing.
FUNDING INFORMATION
Not applicable.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
We are truly thankful to the patient for permitting us to use and publish her picture.
Ghadirzade Arani L, Moslemi Haghighi S, Nasiri S, Dadkhahfar S. Rituximab‐induced psoriasis in a patient with pemphigus vulgaris: A case report and literature review. Clin Case Rep. 2024;12:e8541. doi: 10.1002/ccr3.8541
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are available from the corresponding author upon request.
REFERENCES
- 1. Vinay K, Dogra S. Rituximab in pemphigus: road covered and challenges ahead: Indian. Dermatol Online J. 2018;9(6):367‐372. doi: 10.4103/idoj.IDOJ_290_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Markatseli TE, Kaltsonoudis ES, Voulgari PV, Zioga A, Drosos AA. Induction of psoriatic skin lesions in a patient with rheumatoid arthritis treated with rituximab. Clin Exp Rheumatol. 2009;27(6):996‐998. [PubMed] [Google Scholar]
- 3. Alahmari HS, Alhowaish NY, Omair MA. Rituximab‐induced psoriasis in a patient with granulomatosis with polyangitis treated with adalimumab. Case Rep Rheumatol. 2019;2019:5450863. doi: 10.1155/2019/5450863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim DW, Park SK, Woo SH, Yun SK, Kim HU, Park J. New‐onset psoriasis induced by rituximab therapy for non‐Hodgkin lymphoma in a child. Eur J Dermatol. 2016;26(2):190‐191. [DOI] [PubMed] [Google Scholar]
- 5. Mielke F, Schneider‐Obermeyer J, Dörner T. Onset of psoriasis with psoriatic arthropathy during rituximab treatment of non‐hodgkin lymphoma. Ann Rheum Dis. 2008;67(7):1056‐1057. doi: 10.1136/ard.2007.080929 [DOI] [PubMed] [Google Scholar]
- 6. Venables ZC, Swart SS, Soon CS. Palmoplantar pustulosis secondary to rituximab: a case report and literature review. Clin Exp Dermatol. 2015;40(4):451‐452. doi: 10.1111/ced.12527 [DOI] [PubMed] [Google Scholar]
- 7. Dass S, Vital EM, Emery P. Development of psoriasis after B cell depletion with rituximab. Arthritis Rheum. 2007;56(8):2715‐2718. [DOI] [PubMed] [Google Scholar]
- 8. Brunasso AM, Massone C. Plantar pustulosis during rituximab therapy for rheumatoid arthritis. J Am Acad Dermatol. 2012;67(4):e148‐e150. doi: 10.1016/j.jaad.2011.12.010 [DOI] [PubMed] [Google Scholar]
- 9. Guidelli GM, Fioravanti A, Rubegni P, Feci L. Induced psoriasis after rituximab therapy for rheumatoid arthritis: a case report and review of the literature. Rheumatol Int. 2013;33(11):2927‐2930. [DOI] [PubMed] [Google Scholar]
- 10. Ozen G, Ergun T, Oner SY, Demirkesen C, Inanc N. Widespread psoriasis induced by rituximab in a patient with rheumatoid arthritis: an unexpected adverse reaction. Joint Bone Spine. 2013;80(5):545‐547. doi: 10.1016/j.jbspin.2013.02.001 [DOI] [PubMed] [Google Scholar]
- 11. Hardcastle SA, Gibbs S, Williamson L. Atypical psoriasis following rituximab for rheumatoid arthritis. J Rheumatol. 2012;39(6):1303‐1304. doi: 10.3899/jrheum.111256 [DOI] [PubMed] [Google Scholar]
- 12. Jayasekera P, Parslew R, Al‐Sharqi A. A case of tumour necrosis factor‐α inhibitor‐ and rituximab‐induced plantar pustular psoriasis that completely resolved with tocilizumab. Br J Dermatol. 2014;171(6):1546‐1549. [DOI] [PubMed] [Google Scholar]
- 13. Fiorillo L, Wang C, Hemmati I. Rituximab induced psoriasis in an infant. Pediatr Dermatol. 2014;31(6):12437. [DOI] [PubMed] [Google Scholar]
- 14. Mok MM, Yeung CK, Chan DT, Lo WK. New onset psoriasis after rituximab for treatment of idiopathic membranous nephropathy. Nephrology (Carlton). 2014;19(1):60. doi: 10.1111/nep.12147 [DOI] [PubMed] [Google Scholar]
- 15. Ohata C, Ishii N, Koga H, et al. Coexistence of autoimmune bullous diseases (AIBDs) and psoriasis: a series of 145 cases. J Am Acad Dermatol. 2015;73(1):50‐55. [DOI] [PubMed] [Google Scholar]
- 16. Sanchez‐Palacios C, Chan LS. Development of pemphigus herpetiformis in a patient with psoriasis receiving UV‐light treatment. J Cutan Pathol. 2004;31(4):346‐349. [DOI] [PubMed] [Google Scholar]
- 17. Balighi K, Daneshpazhooh M, Mahmoudi H, Tavakolpour S. Switching from pemphigus vulgaris to psoriasis: a rare report of three cases. Int J Dermatol. 2020;59(5):e144‐e146. doi: 10.1111/ijd.14823 [DOI] [PubMed] [Google Scholar]
- 18. Yokoo M, Oka D, Ueki H. Coexistence of psoriasis vulgaris and pemphigus foliaceus. Dermatologica. 1989;179(4):222‐223. doi: 10.1159/000248369 [DOI] [PubMed] [Google Scholar]
- 19. Yan L, Wang JM, Zeng K. Association between HLA‐DRB1 polymorphisms and pemphigus vulgaris: a meta‐analysis. Br J Dermatol. 2012;167(4):768‐777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Didona D, Di Zenzo G. Humoral epitope spreading in autoimmune bullous diseases. Front Immunol. 2018;9:779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zalzala HH, Abdullah GA, Abbas MY, Mohammedsalih HR, Mahdi BM. Relationship between human leukocyte antigen DRB1 and psoriasis in Iraqi patients. Saudi Med J. 2018;39(9):886‐890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Blauvelt A, Chiricozzi A. The immunologic role of IL‐17 in psoriasis and psoriatic arthritis pathogenesis. Clin Rev Allergy Immunol. 2018;55(3):379‐390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhong W, Xu X, Zhu Z, et al. Increased interleukin‐17A levels promote rituximab resistance by suppressing p53 expression and predict an unfavorable prognosis in patients with diffuse large B cell lymphoma. Int J Oncol. 2018;52(5):1528‐1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chang YS, Lee HT, Chen WS, et al. Treatment of psoriasis with rituximab. J Am Acad Dermatol. 2012;66(5):e184‐e185. doi: 10.1016/j.jaad.2010.08.007 [DOI] [PubMed] [Google Scholar]
- 25. Cohen JD. Successful treatment of psoriatic arthritis with rituximab. Ann Rheum Dis. 2008;67(11):1647‐1648. doi: 10.1136/ard.2007.085290 [DOI] [PubMed] [Google Scholar]
- 26. Singh F, Weinberg JM. Partial remission of psoriasis following rituximab therapy for non‐Hodgkin lymphoma. Cutis. 2005;76(3):186‐188. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.


