Abstract
There is a complex link between tuberculous meningitis (TBM) and aphasia, in which a language impairment is caused by an injury to the cortical language centre. The parts of the brain that function for speech and language production are the Wernicke's, Broca's, and arcuate fasciculus regions. This case report mainly highlights the neurological consequences of TBM, and how it affects language and speech functioning. It outlines a comprehensive physiotherapy rehabilitation program that targets a range of issues for the patient, such as verbal output, weakness, motor deficits, articulation issues in speech, and coordination issues. Various treatment modalities can help correct weakness, improve balance and coordination, increase flexibility and range of motion (ROM), and make speech more fluent. The case report emphasizes the necessity of using an integrated approach that combines speech-language therapy (SLT), melodic intonation therapy (MIT), constraint-induced aphasia therapy (CIAT), medication treatments, and physical therapy to address the multifaceted impacts of TBM-induced aphasia on a patient's quality of life (QOL).
Keywords: speech-language therapy, tubercular meningitis, recurrent low-frequency transcranial magnetic stimulation, transcranial direct current stimulation, medical therapy, broca's aphasia
Introduction
Schutz recorded the early documentation of an instance of aphasia caused by tuberculous meningitis (TBM) in 1881. Mycobacterium tuberculosis (MTB) is still a common central nervous system infection source, causing a broad spectrum of clinical symptoms [1]. Aphasia occurs when an injury to a cortical language centre induces a loss of language understanding or formulation. Typically, language centres are situated in the dominant hemisphere of the brain. These structures illustrate the arcuate fasciculus, Broca's area, and Wernicke's area. It serves as a centre for word comprehension and planning by fusing audio and visual data. The Broca's area is situated in the inferior frontal brain and is responsible for muscular speech execution and sentence construction. The arcuate fasciculus is the neural pathway that connects the Wernicke's and Broca's areas [2]. Strokes frequently induce aphasias, but brain traumas, brain tumours, and other pathological conditions such as neurodegenerative diseases and dementia can also cause them.
Broca's, Wernicke's, global, and transcortical aphasias are the most prevalent forms of aphasia; conduction aphasia has been observed in cortical injury instances without subcortical extension. Also, Wernicke's and motor/premotor frontal areas are connected by the arcuate fasciculus rather than Wernicke's and Broca's areas. Patients with conduction aphasia may take weeks to months to recover. Conduction aphasia differs from Wernicke's aphasia and Broca's aphasia in that there is an isolated inability to repeat. Therefore, it is necessary to plan rehabilitation protocols to get better outcomes [3]. Aphasia is an impairment that affects 21-38% of stroke survivors. The annual community incidence is 43/100,000, and the prevalence is 3000 per million [4]. The right-sided lateralization of the Broca's area is caused by a nidus near the Broca's region in patients with cerebral arteriovenous malformations (AVMs). Conversely, a nidus near the Wernicke's area is responsible for the right-sided lateralization of the Wernicke's region [5]. Benson and Geshwind categorize aphasic patients into two groups, which are aphasia without repetitive disorders and aphasia with repetitive disorders [6]. The most common aetiology for non-fluent aphasia is a lesion impacting Broca's area in the left posterior inferior frontal region of the left frontal lobe [7].
In recent years, language and speech processing have also been linked to several additional brain regions, including the subcortical structures known as the basal ganglia and the right and left hemispheres of the cerebral cortex [8]. A neuroscience-inspired approach to aphasia therapy allows the physician to start thinking about intervention at the neuronal assembly level and viewing therapy insights into other methods that can be used to improve learning. One area for improvement is the errorless learning process. In an errorless learning activity, the learner's chances of making mistakes are lowered or eliminated [9]. Since intensive, comprehensive aphasia programs (ICAPs) address many areas through distinct treatment methodologies and formats, they are different from programs that offer a single treatment very intensely, like constraint-induced language therapy [10]. The benefits of transcranial magnetic stimulation alone are insufficient. Although speech and language therapy alone is effective in naming ability, transcranial magnetic stimulation in addition to speech and language therapy significantly increases the gain obtained with therapies [11]. In our case, there was an acute infarct in the left caudate. The relationship between TBM and Broca's aphasia is a typical complication in these patients with TBM. Therefore, an integrated physiotherapy treatment plan, including speech therapy, should be planned to improve the patient's Quality of Life (QoL) [12].
Case presentation
A 73-year-old male patient visited a tertiary care hospital in the emergency department at Sawangi, Wardha, India, with the chief complaints of headache, fever, and blurred vision, leading to a fall in the bathroom. He was taken to a local practitioner, where medications were given, and he got relief. After four days, he had slurred speech, generalized weakness, multiple episodes of diarrhoea, reduced food intake, headache, generalized seizures, visual disturbances, sensory deficits, and behavioural changes. For these complaints, he was again brought to the hospital, where a neurological examination, which included normal reflexes and tone assessment, indicated hypotonia. Signs of TBM (Brudzinski's sign) were positive, indicating neck rigidity; passive neck flexion caused a slight flexion of both legs and thigh, as depicted in Figure 1. The diagnostic investigation included an MRI of the brain. The assessment of reflexes has been mentioned in Table 1.
Table 1. Reflexes assessment .
+: Diminished, ++: Normal reflex, +++: Brisk reflex, ++++: Exaggerated reflex
| Reflexes | Right | Left |
| Biceps reflex | ++ | ++ |
| Triceps reflex | ++ | ++ |
| Supinator reflex | Absent | Not assessable |
| Knee reflex | ++ | Absent |
| Achilles reflex | Not assessable | Not assessable |
| Plantar reflex | Extensor response | Flexor response |
Figure 1. Brudzinski's sign was positive indicating neck rigidity; passive flexion of the neck caused slight flexion of both legs and thigh.
Assessment
Tone assessment in the upper and lower limbs indicated hypotonia, according to the tone grading scale as mentioned in Table 2.
Table 2. Tone assessment in bilateral upper and lower limbs according to the tone grading scale.
1+: Decreased response (hypotonia)
| Side | Upper limb | Lower limb |
| Right | 1+ | 1+ |
| Left | 1+ | 1+ |
Investigations
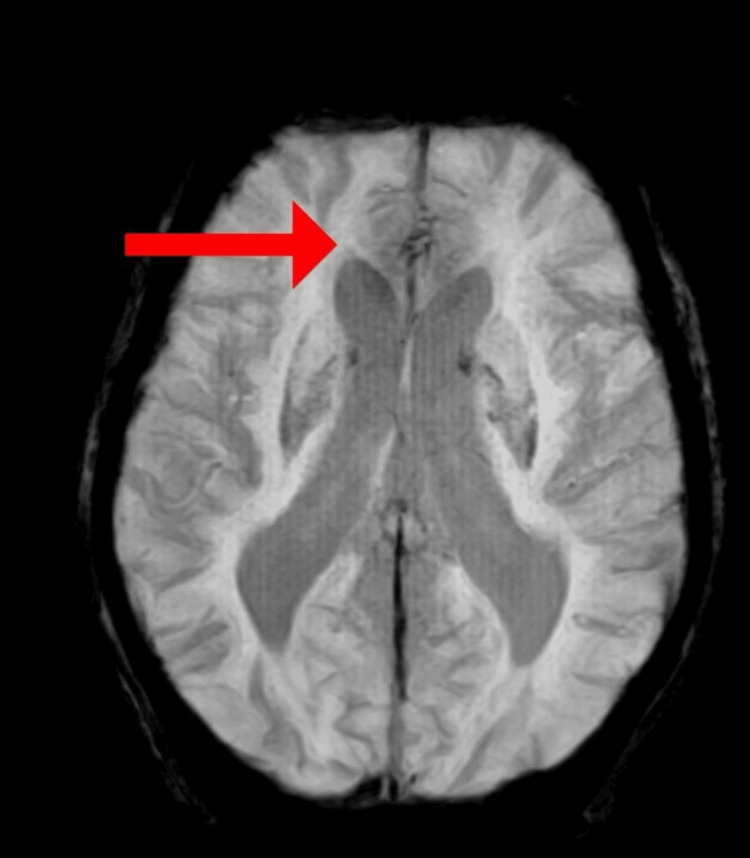
MRI of the brain was done, which revealed bilateral periventricular deep white matter showing small vessel ischemic changes, as shown in Figure 2.
Figure 2. MRI showing bilateral periventricular deep white matter showing small vessel ischemic changes (red arrow).
Physiotherapy management
A detailed physiotherapy protocol was planned that targeted the patient's symptoms. This protocol was planned for six weeks, six days per week. Depending on the severity of the symptoms, the treatment protocol was planned for better recovery. The patient's recovery was monitored, and accordingly, the progression of exercises was done, as mentioned in Table 3.
Table 3. Physiotherapy rehabilitation protocol.
SLT: Speech-language therapy; MIT: Melodic intonation therapy; PNF: Proprioceptive Neuromuscular Facilitation; D1: Diagonal pattern; ACBT: Active cyclic breathing technique; TRT: Task-Related Training; MRP: Motor Relearning Programme; CIAT: Constraint-Induced Aphasia Therapy; PACE: Promoting Aphasics Communication Effectiveness
| No. | Problem list | Goals | Interventions |
| 1 | Generalized weakness | To reduce symptoms of generalized weakness | Enhance the strength of each muscle group (strengthening exercises). Initially start with PNF D1 flexion and extension pattern for the upper limb and lower limb with hold relax technique. The ability to maintain one's weight when sitting and standing can be improved by MRP, task-specific training, TRT, and focus on progression to resisted exercises for weak muscles |
| 2 | Reduced range of motion and flexibility | To improve range of motion and flexibility | Weeks one and three mainly focus on active assisted and then, in weeks four and six, active ROM exercises and stretching |
| 3 | Reduced core strength | To improve core strength | Initially static abdominals, and then progress to abdominal curls, pelvic bridging |
| 4 | Impaired balance and coordination | To maintain good balance and coordination | Initially to improve balance: For static balance - weight shifts over both sides in sitting balance, for standing balance - tandem standing, Once static balance is achieved, the patient can progress to dynamic balance- multidirectional reach-outs for sitting balance, standing with shifting body weight side to side, tandem stance |
| 5 | Hemispatial visual neglect, other disorders such as depression and anxiety | To reduce the symptoms of hemispatial visual neglect and other conditions like depression and anxiety | Mirror treatment has been shown to improve motor skills along with impairment, daily living activities, pain, and visuospatial neglect in a variety of subjects. Action observation therapy - the Benson relaxation method (BRM) (10 minutes in the morning and evening to gain the health benefits associated with relaxation), touch-based skills reduce levels of anxiety and depression and can be initiated as early as possible to get better recovery |
| 6 | Excessive secretions in the chest | To clear the chest of excessive secretions | ACBT, postural drainage in lower zones, suctioning, and breathing exercises: diaphragmatic breathing, pursed lip breathing |
| 7 | Difficulty in articulating speech | To enhance articulation along with the tone and melody of speech | SLT (for roughly 30 to 60 minutes a day, two times a week, for a duration of six weeks), transcranial magnetic stimulation |
| 8 | Decreased verbal output in non-fluent aphasia | To improve verbal output in non-fluent aphasia | MIT for six weeks, with each session for about 30 to 40 minutes |
| 9 | Word retrieval difficulty | To improve word retrieval capacity | Word retrieval approach - in this, semantic and phonological hierarchical clues are used to stimulate the recovery of verbs and objects and then the intervention progresses to the formation of sentences |
| 10 | Paraphasias: difficulty in finding words, different comprehension affected at different levels, writing along with reading problems | To improve comprehension and alleviate writing and reading problems | The intense therapy model CIAT is predicated on making patients use verbal oral language as the only means of communication |
| 11 | Lack of good communication skills | To improve communication skills | PACE therapy |
In Figure 3, the patient is performing active assisted lower limb exercises.
Figure 3. Patient performing active assisted lower limb exercises.
In Figure 4, the patient is performing active assisted pelvic bridging.
Figure 4. Patient performing active assisted pelvic bridging.
Figure 5 depicts the therapist assisting in performing upper limb mobility exercises.
Figure 5. Therapist assisting in performing upper limb mobility exercises .
The patient was asked to perform balloon activities to improve his inspiratory capacity (Figure 6).
Figure 6. The patient was asked to perform balloon activities to improve the inspiratory capacity.
Outcome measures
Outcome measures like the ICU Mobility Scale, Functional Independence Measure, and Progressive Aphasia Severity Scale (PASS) were taken before, after treatment, and in a follow-up after three weeks of treatment to monitor the patient's recovery (Table 4).
Table 4. Outcome measures.
| Outcome measure | Pre-intervention | Post-intervention | Follow-up (after three weeks of treatment) |
| ICU Mobility Scale | Score 0 - Nothing (lying in bed) | Score 3 - Sitting over the edge of the bed | Score 4 - The patient was able to stand with minimal assistance |
| Functional Independence Measure | Level 2 - Maximal assistance | Level 4- Minimal assistance | Level 5 - Supervision |
| Progressive Aphasia Severity Scale (PASS) | 3 (severe impairment) | 1 (mild impairment) | 1 (mild impairment) |
Manual muscle testing according to the Oxford scale is shown in Table 5.
Table 5. Manual muscle testing .
2+: Full range of motion in a gravity-eliminated plane, breaks upon minimum resistance; 3: Full range of motion against gravity with no resistance
| Joint | Pre-intervention | Post-intervention |
| Shoulder flexors | 2+ | 3 |
| Wrist flexors | 2+ | 3 |
| Hip flexors | 2+ | 3 |
| Hip extensors | 2+ | 3 |
| Knee flexors | 2+ | 3 |
| Knee extensors | 2+ | 3 |
| Ankle flexors | 2+ | 3 |
| Ankle extensors | 2+ | 3 |
Discussion
Broca’s aphasia occurs because of injury to the cortical language centre of the brain that is situated in the frontal lobe, on the left side, which is responsible for speech along with some motor movements [18]. Some drugs like catecholaminergic agents, acetylcholine esterase inhibitors, neurotrophic factors, transcranial magnetic stimulation, and transcranial direct stimulation can be used in managing patients with Broca's aphasia. Belin et al. have studied the recovery from non-fluent aphasia after melodic intonation therapy (MIT). It was found that subjects who had aphasia had good results with MIT [19]. Patients with tuberculosis may have lymphadenomegaly [20].
In the above case report, the patient complained of slurred speech, visual impairments, stiffness in the neck, seizures, and headache, for which reflex, tone, and some neurological signs of TBM (Brudzinski's sign) were positive. Outcome measures included the ICU Mobility Scale, Functional Independence Measure, and Manual Muscle Testing were used. In the investigation, an MRI of the brain was done. The case report details a comprehensive rehabilitation approach for non-fluent aphasia, encompassing physical therapy for muscle strength and stability, cognitive interventions like constraint-induced aphasia therapy (CIAT) for comprehension and communication, and speech-language therapy (SLT) for speech articulation. Balance exercises and mirror therapy were employed to address spatial awareness issues, while anxiety symptoms were managed with relaxation techniques. The integrated program aims to alleviate symptoms and enhance verbal output and language comprehension. All these above interventions used in this study are found to be more effective in improving the patient's QoL and overall well-being.
Conclusions
The above case highlights the intricate relationship between TBM and Broca's aphasia, resulting in a myriad of neurological symptoms and some other complaints of headache, fever, and blurred vision leading to neurological deficits, seizures, and language impairment. An integrated physiotherapy approach encompassing various interventions including MIT, CIAT, Promoting Aphasics' Communicative Efficiency (PACE) therapy, SLT, and targeted exercises focusing on the patient's symptoms like weakness, articulation, balance, and coordination, had shown significant improvements in the patient's functional abilities and communication skills. Addressing not only the linguistic deficits but also associated physical weaknesses and functional limitations, this holistic rehabilitation approach led to improved mobility, speech articulation, comprehension, and overall communication effectiveness. In conclusion, the integrated physiotherapy rehabilitation program outlined in this case report exemplifies its efficacy in ameliorating the multifaceted impact of Broca's aphasia induced by TBM, thereby enhancing the patient's overall well-being and functional independence.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Ghanishtha C. Burile , Neha P. Arya, Nikita H. Seth, Pallavi Harjpal
Acquisition, analysis, or interpretation of data: Ghanishtha C. Burile , Neha P. Arya, Nikita H. Seth, Pallavi Harjpal
Drafting of the manuscript: Ghanishtha C. Burile , Neha P. Arya, Nikita H. Seth, Pallavi Harjpal
Critical review of the manuscript for important intellectual content: Ghanishtha C. Burile , Neha P. Arya, Nikita H. Seth, Pallavi Harjpal
Supervision: Ghanishtha C. Burile , Neha P. Arya, Nikita H. Seth, Pallavi Harjpal
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Conduction aphasia as initial manifestation of tuberculous meningitis. Garcia-Grimshaw MA, Gutierrez-Manjarrez FA, Gonzalez-Duarte A. Cureus. 2018;10:0. doi: 10.7759/cureus.2889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Le H, Lui MY. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2023. Aphasia. [Google Scholar]
- 3.Kirshner HS. Encyclopedia of Human Behavior. Vol. 2. 2012: Elsevier; 2012. Aphasia; p. 0. [Google Scholar]
- 4.Expert group meeting on aphasia: a report. Pauranik A, George A, Sahu A, et al. Ann Indian Acad Neurol. 2019;22:137–146. doi: 10.4103/aian.AIAN_330_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Comparison of language cortex reorganization patterns between cerebral arteriovenous malformations and gliomas: a functional MRI study. Deng X, Zhang Y, Xu L, et al. J Neurosurg. 2015;122:996–1003. doi: 10.3171/2014.12.JNS14629. [DOI] [PubMed] [Google Scholar]
- 6.Relative frequency and prognosis of vascular aphasia (follow-up at 3 months) in the neurology department of assiut university hospital. El-Tallawy HN, Gad HA, Ali AM, Abd-El-Hakim MN. Egypt J Neurol Psychiatry Neurosurg. 2019;55:41. [Google Scholar]
- 7.Evidence for plasticity in white matter tracts of chronic aphasic patients undergoing intense intonation-based speech therapy. Schlaug G, Marchina S, Norton A. Ann N Y Acad Sci. 2009;1169:385–394. doi: 10.1111/j.1749-6632.2009.04587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Predominance of caudate nucleus lesions in acute ischaemic stroke patients with impairment in language and speech. Grönholm EO, Roll MC, Horne MA, Sundgren PC, Lindgren AG. Eur J Neurol. 2016;23:148–153. doi: 10.1111/ene.12822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rethinking aphasia therapy: a neuroscience perspective. Varley R. Int J Speech Lang Pathol. 2011;13:11–20. doi: 10.3109/17549507.2010.497561. [DOI] [PubMed] [Google Scholar]
- 10.Intensive comprehensive aphasia programs: an international survey of practice. Rose ML, Cherney LR, Worrall LE. Top Stroke Rehabil. 2013;20:379–387. doi: 10.1310/tsr2005-379. [DOI] [PubMed] [Google Scholar]
- 11.Speech and language therapy for aphasia following subacute stroke. Koyuncu E, Çam P, Altınok N, Çallı DE, Duman TY, Özgirgin N. Neural Regen Res. 2016;11:1591–1594. doi: 10.4103/1673-5374.193237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Temporal lobe encephalitis need not always be herpes simplex encephalitis: think of tuberculosis. Madireddi J, Reddy G, Stanley W, Prabu M. J Clin Diagn Res. 2016;10:0–2. doi: 10.7860/JCDR/2016/15952.7717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Use of the progressive aphasia severity scale (PASS) in monitoring speech and language status in primary progressive aphasia. Sapolsky D, Domoto-Reilly K, Dickerson BC. Aphasiology. 2014;28:993–1003. doi: 10.1080/02687038.2014.931563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adaptation of melodic intonation therapy to greek: a clinical study in broca’s aphasia with brain perfusion SPECT validation. Martzoukou M, Nousia A, Nasios G, Tsiouris S. Front Aging Neurosci. 2021;13:664581. doi: 10.3389/fnagi.2021.664581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mirror therapy for improving motor function after stroke. Thieme H, Morkisch N, Mehrholz J, Pohl M, Behrens J, Borgetto B, Dohle C. Cochrane Database Syst Rev. 2018;7:0. doi: 10.1002/14651858.CD008449.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Motor relearning program versus proprioceptive neuromuscular facilitation technique for improving basic mobility in chronic stroke patients-a comparative study. Singha R. Int J Physiother Res. 2017;5:2490–2500. [Google Scholar]
- 17.A review of constraint-induced therapy applied to aphasia rehabilitation in stroke patients. Balardin JB, Miotto EC. Dement Neuropsychol. 2009;3:275–282. doi: 10.1590/S1980-57642009DN30400003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The efficacy of pace in the remediation of naming deficits. Li EC, Kitselman K, Dusatko D, Spinelli C. J Commun Disord. 1988;21:491–503. doi: 10.1016/0021-9924(88)90019-6. [DOI] [PubMed] [Google Scholar]
- 19.Confusion vs broca aphasia: a case report. Wang R, Wiley C. Perm J. 2020;24 doi: 10.7812/TPP/19-061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lymph nodes of the head and neck: in normal and pathological conditions. Nikolaev N, Yankov Y. Varna Medical Forum. 2023;12:69–74. [Google Scholar]