Abstract
Worldwide stroke is the second leading cause of death and the third leading cause of death and disability combined. The estimated global economic burden by stroke is over US$891 billion per year. Within three decades (1990–2019), the incidence increased by 70%, deaths by 43%, prevalence by 102%, and DALYs by 143%. Of over 100 million people affected by stroke, about 76% are ischemic stroke (IS) patients recorded worldwide. Contextually, ischemic stroke moves into particular focus of multi-professional groups including researchers, healthcare industry, economists, and policy-makers. Risk factors of ischemic stroke demonstrate sufficient space for cost-effective prevention interventions in primary (suboptimal health) and secondary (clinically manifested collateral disorders contributing to stroke risks) care. These risks are interrelated. For example, sedentary lifestyle and toxic environment both cause mitochondrial stress, systemic low-grade inflammation and accelerated ageing; inflammageing is a low-grade inflammation associated with accelerated ageing and poor stroke outcomes. Stress overload, decreased mitochondrial bioenergetics and hypomagnesaemia are associated with systemic vasospasm and ischemic lesions in heart and brain of all age groups including teenagers. Imbalanced dietary patterns poor in folate but rich in red and processed meat, refined grains, and sugary beverages are associated with hyperhomocysteinaemia, systemic inflammation, small vessel disease, and increased IS risks. Ongoing 3PM research towards vulnerable groups in the population promoted by the European Association for Predictive, Preventive and Personalised Medicine (EPMA) demonstrates promising results for the holistic patient-friendly non-invasive approach utilising tear fluid-based health risk assessment, mitochondria as a vital biosensor and AI-based multi-professional data interpretation as reported here by the EPMA expert group. Collected data demonstrate that IS-relevant risks and corresponding molecular pathways are interrelated. For examples, there is an evident overlap between molecular patterns involved in IS and diabetic retinopathy as an early indicator of IS risk in diabetic patients. Just to exemplify some of them such as the 5-aminolevulinic acid/pathway, which are also characteristic for an altered mitophagy patterns, insomnia, stress regulation and modulation of microbiota-gut-brain crosstalk. Further, ceramides are considered mediators of oxidative stress and inflammation in cardiometabolic disease, negatively affecting mitochondrial respiratory chain function and fission/fusion activity, altered sleep–wake behaviour, vascular stiffness and remodelling. Xanthine/pathway regulation is involved in mitochondrial homeostasis and stress-driven anxiety-like behaviour as well as molecular mechanisms of arterial stiffness. In order to assess individual health risks, an application of machine learning (AI tool) is essential for an accurate data interpretation performed by the multiparametric analysis. Aspects presented in the paper include the needs of young populations and elderly, personalised risk assessment in primary and secondary care, cost-efficacy, application of innovative technologies and screening programmes, advanced education measures for professionals and general population—all are essential pillars for the paradigm change from reactive medical services to 3PM in the overall IS management promoted by the EPMA.
Keywords: Predictive preventive personalised medicine (PPPM / 3PM), Ischemic stroke, Sudden cardiac arrest/death, Suboptimal health, Health-to-disease transition, Primary and secondary care, Patient-friendly non-invasive approach, Tear fluid analysis, Viromics and metabolomics, Mitochondrial health, Mitophagy, Inflammation, Cytokine storm (COVID-19), Diabetes mellitus, Diabetic retinopathy, Flammer syndrome, Health risk assessment, Sleep medicine, Behavioural patterns, Individualised patient profile, Artificial intelligence, Population screening, Healthcare economy, Health policy, Expert recommendations
Ischemic stroke: alarming statistics and well-acknowledged risks
According to the most recent Global Burden of Disease (GBD) estimates, worldwide stroke is the second leading cause of death and the third leading cause of death and disability (see disability-adjusted life-years lost, DALYs statistics presented below) combined [1]. The estimated global economic burden by stroke is over US$891 billion per year comprising 1.12% of the global GDP [2]. Within three decades (years 1990–2019) considering the absolute number of all stroke cases, the burden increased as follows: incidence by 70%, deaths by 43%, prevalence by 102%, and DALYs by 143%. The age-standardised difference between countries is remarkable taking into consideration the six-fold incidence, 15-fold mortality, four-fold prevalence, and 20-fold DALYs rates, which are particularly high in lower- and middle-income countries situated in Eastern Europe, Asia, and Sub-Saharan Africa [1].
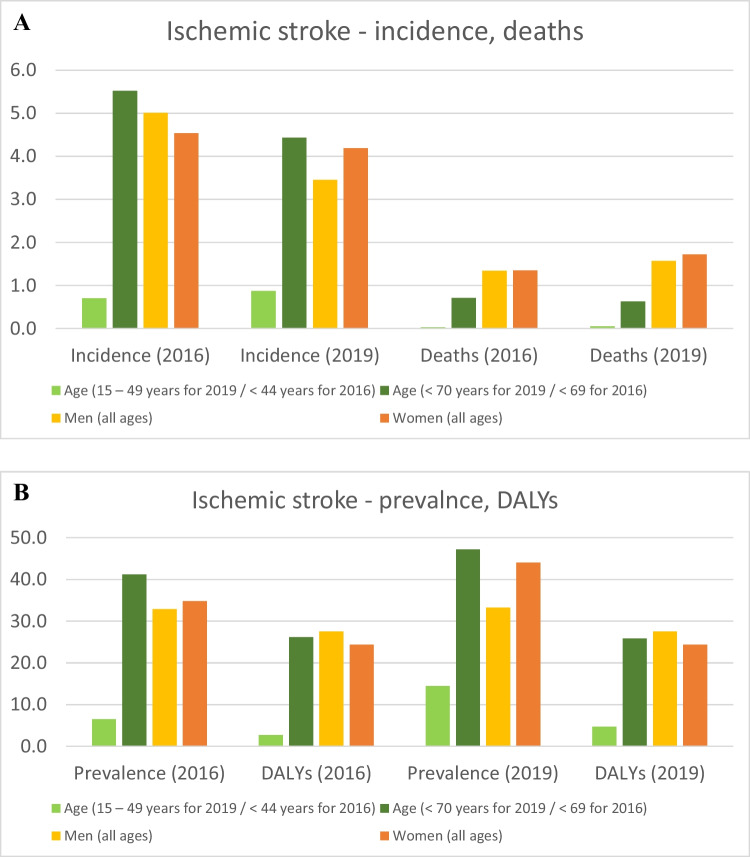
Of 101.5 million (2019) people affected by stroke, about 76% are ischemic stroke (IS) patients recorded worldwide. Table 1 and Fig. 1A and B both compare statistics originated from 2016 and 2019 (GBD) [1, 3–5]. From altogether, 13.68 million new strokes occurred in 2016, and 9.56 million (69.9%) accounted for IS with 51.9 million disability-adjusted life-years (DALYs) [3, 4]. Three years later (2019), IS-related deaths increased by 22.3% against 18.5% from all strokes, and DALYs increased by 23% for all strokes [1, 5]. Noteworthy, the IS prevalence increased for both sexes but more remarkably for females. Although all age groups demonstrate an increase in the IS prevalence, specifically the young (< 49 y.o.) stroke prevalence has doubled within 3 years followed by concomitant DALYs increase due to IS in this age group. Contextually, ischemic stroke moves into particular focus of multi-professional groups including researchers, healthcare industry, economists, and policy-makers. All aspects are of great importance, namely, the needs of young populations and elderly, personalised risk assessment in primary and secondary care, cost-efficacy, innovative screening programmes, and advanced education measures for professionals and general population, amongst others—altogether resulting in the paradigm change from reactive medical services to a predictive approach, targeted prevention, and treatments tailored to the person (predictive, preventive, and personalised medicine, shortly PPPM/3PM).
Table 1.
Incidence, prevalence, deaths, and DALYs for stroke (all types) and ischemic stroke compared for the year 2019 versus 2016
| 2016 | 2019 | |||
|---|---|---|---|---|
| All stroke | Ischemic stroke (all ages, both sexes) | All stroke | Ischemic stroke (all ages, both sexes) | |
| Incidence | 13 676 761 | 9 556 444 | 12 224 551 | 7 630 803 |
| Prevalence | 80 065 453 | 67 595 368 | 101 474 558 | 77 192 498 |
| Deaths | 5 528 232 | 2 690 171 | 6 552 724 | 3 293 397 |
| DALYs | 116 445 136 | 51 897 437 | 143 232 184 | 63 478 271 |
Fig. 1.
A Numbers (million) of ischemic stroke incidence and deaths amongst different age and sex categories in 2016 and 2019. B Numbers (million) of ischemic stroke prevalence and DALYs amongst different age and sex categories in 2016 and 2019
Multi-factorial risks of IS with sufficient space for preventive interventions
As presented by GBD 2016 Stroke Collaborators, 87.9% of ischemic stroke DALYs were associated with potentially preventable risks such as smoking, inappropriate dietary habits and behavioural patterns, physical inactivity, and toxic environmental, amongst others [1, 6]. Therefore, appropriate educational measures and improved lifestyle patterns in the population are considered a potentially effective strategy to reduce ischemic stroke mortality and morbidity [7]. However, health risk assessment should evaluate comprehensive individualised profiles including both modifiable and non-modifiable risk factors for cost-effective targeted prevention in primary (suboptimal health conditions with reversible damage to health) and secondary (clinically manifested disorders) care in the framework of 3PM.
According to the biopsychosocial model of health and disease, a multifactorial concept for the risk evaluation towards prevention and prediction have to be taken into consideration. For example, considering lifestyle factors, an imbalanced diet and inappropriate nutritional patterns are frequently observed in patients with clinically manifested IS compared to healthy controls and generally accepted Mediterranean diet [8–12]. Malnutrition, underweight, overweight, and obesity represent highly relevant risks of IS [10, 11, 13, 14]. The rise in adolescent obesity as well as underweight may significantly increase future young stroke prevalence [15–17]. Further, not the BMI deviation itself but rather individual metabolic consequences contribute to the stroke predisposition [13]. To this end, the “obesity paradox” has been described suggesting a lower risk of mortality and favourable outcomes in obese or overweight patients compared to the normal BMI range [16–21].
Physical inactivity/sedentary lifestyle is a strong contributor to IS [22, 23] as a multi-faceted risk factor including mitochondrial stress and chronic inflammation with characteristic cardiovascular and metabolic alterations, that in sum contribute to a pathophysiological status to be defined as biomolecular allostatic load [24–28].
Several studies demonstrated environmental pollution as a health risk highly relevant for an increased IS incidence [29]. Further, an exposure to a toxic environment such as heavy metals, per evidence, is associated with an increased frequency of non-communicable diseases, such as arterial hypertension and diabetes mellitus with an increased risk of IS [30].
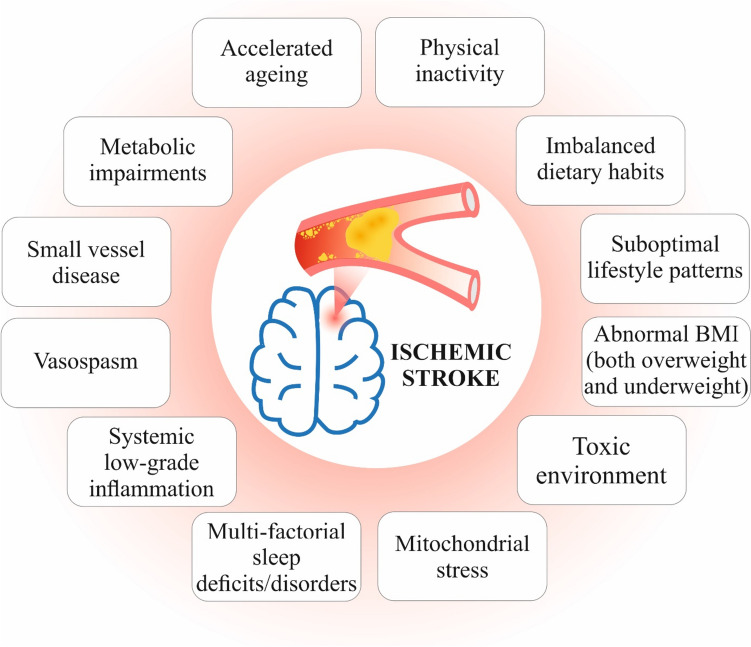
Finally, acute and chronic infectious diseases may significantly contribute to IS risks. For example, pulmonary tuberculosis survivors are at significantly higher risk of IS [31]. Moreover, pulmonary tuberculosis patients were demonstrated to develop IS even in absence of conventional vascular risk factors [32] that makes tuberculosis to a very important proof-of-principle model in understanding IS pathomechanisms linked to pulmonary infections and inflammatory pathways. Figure 2 summarises most prominent IS risks with a sufficient space for prevention intervention by the 3PM approach.
Fig. 2.
Risk factors of ischemic stroke with sufficient space for cost-effective prevention interventions in primary (suboptimal health) and secondary (clinically manifested collateral disorders contributing to stroke risks) care; these risks are interrelated. For example, sedentary lifestyle and toxic environment both cause mitochondrial stress, systemic low-grade inflammation, and accelerated ageing; inflammageing is a low-grade inflammation associated with accelerated ageing and poor stroke outcomes. Stress overload, decreased mitochondrial bioenergetics, and hypomagnesaemia are associated with systemic vasoconstriction (vasospasm) and ischemic lesions in the brain, e.g. in case of the Flammer syndrome phenotype discussed later on in the article. Imbalanced dietary patterns poor in folate but rich in red and processed meat, refined grains, and sugary beverages are associated with hyperhomocysteinaemia, systemic inflammation, small vessel disease, and increased IS risks. In contrast, Mediterranean diet characterised by strong and systemic anti-inflammatory effects being rich in olive oil, nuts, whole grain, fruits and vegetables, and seafood consumption, but light on dairy and red/processed meat, is known to enhance anti- to pro-inflammatory ratio and to decrease IS risks [33]
Clinically manifested strokes are only the “tip of the iceberg”: IS with unclear risk factors is a severe challenge to healthcare systems
Worldwide accumulating data indicate that clinically manifested and officially recorded stroke cases do contribute a noticeable portion, which, however, creates a minor share of the entire issue of brain infarction. Rough estimations state that uncovered portion is about 14 times bigger in the population compared to the IS diagnosed portion, which reactive medical approach is applied to [16, 34]. This evident discrepancy is huge dramatically reducing healthcare efficacy and life-quality of populations with significant economic burden to healthcare systems around the world. As early as for the year 1998, the very first evidence-based estimates were published for the USA considering the annual incidence of silent strokes to be at the level of eleven million [35]. Since two decades these levels are continuously increasing.
Being characteristic for the silent brain infarction (SBI), lacunar strokes represent up to 30% of all ischemic strokes. Silent lacunar brain infarctions are either diagnosed by a routine health check-up or by autopsy; frequently these are individuals without stroke history, and brain infarctions discovered are unexpected for them. As the matter of fact, currently reported prevalence of the SBI ranges between 6 and 55% for examined sub/populations depending on the patient stratification criteria and targeted groups under investigation [36–44]. Noteworthy, there is a significant sex-dependent difference in the SBI manifestation, since the silent lesions are more prevalent in females, in contrast to the clinically manifested ischemic strokes which are more typical for males [36, 45–49]. Contextually, the symptomatic interpretation of cerebrovascular diseases and cerebrovascular infarcts is traditionally adapted to the male patient cohorts with the better described clinical picture and more precise recommendations. Therefore, more subtle female-specific symptoms might be wrongly interpreted or even overlooked resulting in poor individual outcomes more frequent for female patient cohorts [50]. Finally, the needs of young populations remain unmet, since SBI-characteristic data for these patient cohorts are underdeveloped [36]. Consequently, an effective protection of young populations against ischemic stroke is lacking in primary care. Considering the tremendous prevalence of IS with unclear risk factors, a robust predictive approach based on individualised health risk assessment and followed by targeted prevention in primary and secondary care is of great clinical utility benefiting millions of high-risk individuals and society at large.
Key issues to be solved for a cost-effective protection against IS
As notified above, screening towards uncovered SBI cases is expected to result in about 14-times bigger vulnerable subpopulations compared to clinically manifested SBI identified by currently applied reactive medical approach. Specifically, for young sub-populations, SBI-related prevalence is strongly underestimated that significantly hinders targeted protection of youth and young adults in primary care and decreases overall cost-efficacy of IS management. The trend has to be reversed by applying individualised health risk assessment. To this end, an applicability of innovative screening programmes depends to major extent from their effectivity to catch up with vulnerable groups within the stage of reversible damage (focus on suboptimal health, in order to protect individuals against the health-to-disease transition) associated with high cost-efficacy (positive health economy), as well as from the level of acceptance by professionals and in the population. Accompanying educational measures adapted to target groups seem to be the clue.
Per evidence, IS is a multifactorial disease with a highly individual set-up of risk factors which promote the disease development in a synergistic way. Therefore, a holistic diagnostic approach based on individualised patient profiles is essential. Contextually, health risk assessment has to be focused on systemic effects monitored, for example, by natural/physiologic or artificially created (implanted) biosensors. To this end, mitochondria are considered a highly effective multi-functional physiologic biosensor applicable to vulnerable groups in suboptimal health to monitor and to correct their health status protecting against health-to-disease transition [51]. For a non-invasive approach which in many cases reasonably to be performed in a life-long way and certainly highly appreciated by customers, body fluids allowing for monitoring systemic effects are considered highly appropriate. To this end, specifically tear fluid as possessing many advantages (non-invasive holistic approach for monitoring of systemic effects with highly stable biomarkers, amongst others) is extensively under consideration for establishing evidence-based health risk assessment [52–56]. Finally, medical services of high geographic density are decisive to meet urgent needs of populations implementing concepts of predictive diagnostics and targeted protection against preventable disorders [34, 57–59].
Ongoing 3PM research towards vulnerable groups in the population
Tear fluid analysis of ischemic stroke patients with multi-factorial risks: preliminary results from international research project
Study design
The European proof-of-principle study (Czech Republic–Germany–Austria) aimed to collect and analyse tear fluid samples of stroke patients (16) versus health status well-checked controls (12). Commercially available Schirmer tear strips (sterile diagnostic strips, individually packed, Aivimed GmbH, Wiesbaden, Germany) were used to collect tear fluid samples according to the protocols provided by the manufacturer. After 3 min, the wetting of the Schirmer paper in mm was recorded for both eyes. Immediately after each individual strip was placed into a sterile Eppendorf tube and stored at – 80 °C until mass spectrometry (MS) analysis. MS analysis was performed by Biocrates Life Sciences AG, Innsbruck, Austria, utilising the MxPR Quant 500 kit for metabolomics. The entire analytical procedure is detailed in our previously published article [55]. The experimental metabolomics measurement technique is described by patents EP1897014B1 and EP1875401B1 [60, 61]. The commercially available kit settled by Biocrates Life Sciences was used for qualification and quantification of metabolites classified into 26 different clusters: acylcarnitines, alkaloids, amine oxides, amino acid related, amino acids, bile acids, biogenic amines, carbohydrates and related, carboxylic acids, ceramides, cholesteryl esters, cresols, diglycerides, dihexosylceramides, dihydroceramides, fatty acids, hexosylceramides, hormones and related, indoles and derivatives, lysophosphatidyl-cholines, nucleobases and related, phosphatidyl-cholines, sphingomyelins, triglycerides, trihexosylceramides, vitamins, and cofactors.
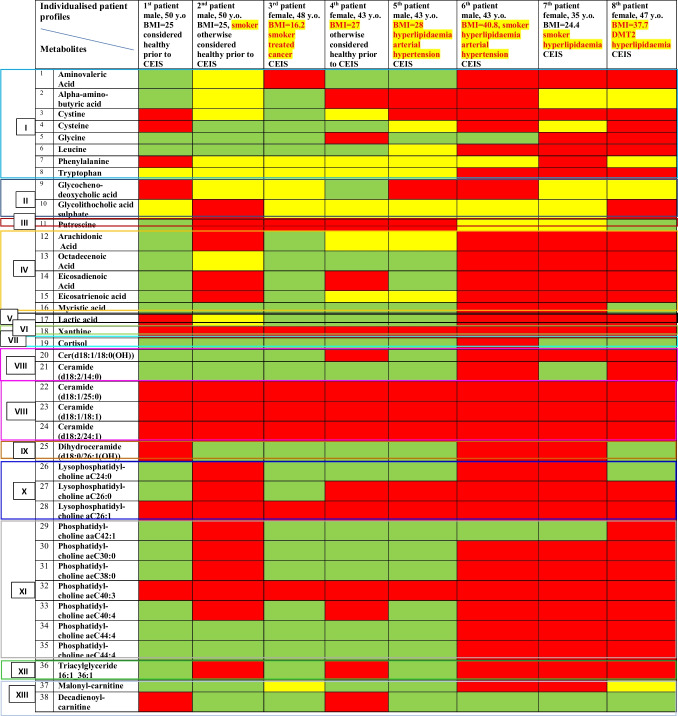
Metabolic patterns specific for cardio-embolic ischemic stroke (CEIS)
Statistical analysis revealed thirteen metabolic clusters as highly specific for CEIS metabolic shifts (see Table 2). Based on the level of metabolic profile deviation, a “traffic light” system for the health risk assessment has been created, namely, in green colour, metabolic patterns are marked which demonstrate levels similar to controls; in yellow colour, metabolic patterns are marked which up to 2 times are deviated from the control levels; in red colour, metabolic patterns are marked which are either several-times deviated from the control levels or even measurable only in the stroke patients but not in controls (such as xanthine; ceramides (d18:1/25:0), (d18:1/18:1), and (d18:2/24:1); lysophosphatidyl-choline aC26:1; phosphatidyl-choline aeC40:3). Individualised metabolic profiles are exemplified by eight CEIS patients who differ from each other by clinical (BMI, hyperlipidaemia, arterial hypertension, diabetic history) and non-clinical risk factors (age, sex, smoking). Noteworthy, a very important discovery has been made: the more risk factors (clinical, non-clinical, metabolic) are coming together, the younger is the patient e.g. in case of the following:
1st patient with CEIS, 50 y.o., no any clinically manifested risk factors, 12 “red” metabolites” and 2 yellow metabolites) versus
7th patient (35 y.o.), who is a smoker suffering from hyperlipidaemia and demonstrating 28 metabolic parameters in the red area and 5 in the yellow one
Table 2.
Thirteen metabolic clusters relevant specifically for cardio-embolic ischemic stroke (CEIS) versus healthy controls; Individualised metabolic profiles are exemplified by eight patients who differ from each other by clinical (BMI, hyperlipidemia, arterial hypertension, diabetic history) and non-clinical risk factors (age, sex, smoking); green areas = metabolic patterns which demonstrate levels similar to controls; yellow areas = metabolic patterns which up to 2-times are deviated from the control levels; red areas = metabolic patterns which are either several-times deviated from the control level or measurable only in the stroke patients but not in controls (such as xanthine; ceramides (d18:1/25:0), (d18:1/18:1), (d18:2/24:1); lysophosphatidyl-choline aC26:1; phosphatidyl-choline aeC40:3)
Herewith, we shortly analyse the relevance of the detected metabolites for predictive approach, targeted prevention, and personalised treatments in overall stroke management.
Cluster I: amino acids and related derivatives
In analytical sets presented here, both proteogenic amino acids/their derivatives (cystine, cysteine, glycine, leucine, phenylalanine, tryptophan) and non-proteogenic amino acids (which the human body obtains from microbiota production, such as 5-amino-valeric acid, and food, such as alpha-amino-butyric acid) were detected in the tear fluid. In consensus, similar patterns including glycine, phenylalanine, and tryptophan which forms a risk score for cardiovascular disease and stroke were reported for blood analysis performed [62–64]. Identification of 5-amino-valeric acid (5-AVA) in relation to the CEIS is an important indication that microbiome profiles are crucial for considering CEIS risks which is instrumental for health risk assessment, predictive diagnostics, and targeted treatments. To this end, pre-clinical research utilising rat model revealed an involvement of 5-AVA in pathogenesis of cardiovascular disease [65].
Cluster II: bile acids
Alterations in bile acid metabolism were demonstrated as associated with atherosclerosis and inflammation, which are known risk factors of cardiovascular and cerebrovascular diseases [66]. Specifically metabolism of glycochenodeoxycholic acid and glycolithocholic acid sulphate detected in our analytical sets involves complex interactions between the liver, intestine, and gut microbiota, which are known to be involved into multi-factorial risks of CEIS. Further, an increased blood level of glycochenodeoxycholic acid was observed in young patients diagnosed with IS compared to healthy controls [67] which is instrumental for innovative screening programmes focused on healthcare needs of young populations.
Cluster III: biogenic amines
A panel of biogenic amines was described as a urine biomarker candidate for early diagnosis and prognosis of stroke [68]. Specific for our analytical sets, putrescine significantly increased in CEIS was also identified by Lee et al. (2022) in blood as a novel biomarker specific for the large artery atherosclerosis stroke [69]. Putrescine is involved into neuronal cell damage associated with various type of excitatory neurotoxicity, and the hippocampal putrescine level is increased by global ischemia but is inhibited by L-deprenyl treatment [70] which is instrumental for cost-effective targeted prevention.
Cluster IV: fatty acids
The central role of fatty acids in the stroke pathomechanisms is evident by in-depth research performed over decades [71]. Specifically saturated fatty acids are involved into atherosclerosis formation. Similarly to our analytical sets, arachidonic acid, octadecenoic acid, and myristic acid patterns were elevated also in blood of IS patients as described by other research groups [72, 73] which is instrumental for health risk assessment and treatment algorithms tailored to individualised patient profiles.
Cluster V: carboxylic acids
Of the large cluster of carboxylic acids, lactic acid was detected in our analytical sets as highly relevant for CEIS. To this end, lactic acid is a highly sensitive metabolic indicator of the injury progression in cerebral ischemia [74], and corresponding metabolic acidosis is well described as significantly increasing major cardiovascular risks with severe consequences including sudden heart attack and stroke [75] which is instrumental for health risk assessment and cost-effective targeted prevention in general population.
Cluster VI: nucleobases
In our analytical sets, specifically high xanthine levels were strongly associated with CEIS. Xanthine is a product of the purine degradation pathway subsequently converted to uric acid by the xanthine oxidase. Noteworthy, increased xanthine levels in the cerebrospinal fluid are considered a predictor of IS lethal outcomes [76]. Corresponding pathomechanisms involve xanthine into severe oxidative stress by converting xanthine to uric acid and generating reactive oxygen species (ROS) as a by-product that is directly associated with high IS risks [77] which is instrumental for predictive and prognostic approach in primary and secondary care.
Cluster VII: hormones
The stress-associated hormone cortisol was detected in one of the severe cases of CEIS with particularly poor outcome. In consensus, an increased serum cortisol level is considered a marker of severity, short- and long-term prognosis, and mortality after acute IS [78].
Clusters VIII and IX: ceramides and derivatives
Circulating ceramide levels are considered powerful predictors upstream to severe cardiovascular events later on, such as myocardial infarction and stroke. Ceramides containing the C16, C18, and C24:1 acyl chains demonstrate a superior independent predictive value for plaque instability and/or future fatality than conventional lipid profile measures, including LDL cholesterol [16, 79–83]. Still, there are very few studies which have investigated individual fractions of ceramides in the blood associated with IS risks and mortality [84].
Clusters X and XI: lysophosphatidyl-cholines and derivatives
Lysophosphatidyl-cholines (LPC) are bioactive lipids derived from phosphatidylcholines. LPC also serve as signal molecules released by apoptotic cells to attract phagocytes being, therewith directly linked to inflammatory disorders [85]. Corresponding mechanisms are complex and vary significantly from case to case, depending on the multi-factorial context ranging from damaging effects (e.g. via endothelial dysfunction) leading to IS development, to regeneration processes after IS (anti-inflammatory mechanisms) which they are involved in [85–88]. Contextually, individual LPC fractions and derivatives should be carefully considered for individualised patient profiles for predictive molecular sets, health risk assessment, and treatments tailored to the person.
Cluster XII: triglycerides
Hypertriglyceridemia arises from disruptions in triglyceride metabolism, leading to elevated levels of plasma triglycerides. Elevated plasma triglycerides, especially in non-fasting states, have been described as a risk factor of IS. Well investigated pathomechanisms which hypertriglyceridemia is involved in are atherosclerosis, thrombosis, and elevated blood viscosity [89]. Specifically, the triacylglyceride 16:1_36:1 fraction identified in our analytical sets was reported as being specific (tear fluid) for diabetic patients diagnosed with diabetic retinopathy as a risk factor highly relevant for IS [55] which is instrumental for predictive diagnostic approached followed by cost-effective preventive measures.
Cluster XIII: acylcarnitines
Acylcarnitines are the key molecules for energy production via β-oxidation by transporting fatty acids to mitochondria, for example, when IS causes an imbalanced energy pathways and deprived glucose supply. Distributions of acylcarnitines in brain affected by IS was studied in animal models demonstrating significant deviation in corresponding metabolic patterns and indicating an importance for quantitative monitoring of acylcarnitines profiles for targeted handling of damage caused by stroke [90]. Finally, decanoylcarnitine and octanoylcarnitine were demonstrated as independent discriminants specifically for the cardioembolic stroke. The levels of decanoylcarnitine and octanoylcarnitine is significantly higher in blood of stroke patients at high risk of cardioembolism compared to low and intermediate risk [91] which is instrumental for health risk assessment followed by cost-effective preventive measures.
Tear fluid analysis of diabetic patients with retinopathy: making ophthalmologic units to the check-point for personalised IS prediction in diabetes care
“Ut imago est animi voltus sic indices oculi”, “the face is a picture of the mind as the eyes are its interpreter”, has been already declared by Cicero (106–43 BC). Scientists translated and transformed the citation to “the eye is the window to the brain”, and this phrase is more than a philosophical consideration but an anatomical truth. The eye belongs to the central nervous system, and axons of the retinal ganglion cells are bundled to the optic nerve projecting to the optic chiasma, thus into the brain. Therefore, multiple studies evaluated potential ocular signs of CNS diseases from neurodegenerative disease like multiple sclerosis and Alzheimer’s disease to cardiovascular diseases like stroke.
Diabetes mellitus type 2 (DMT2) patients are several times more susceptible to a stroke event due to various cerebrovascular complications [92]. Micro- and macro-vascular changes characteristic for DM lead to particularly poor IS outcomes, increased mortality, and poor post-procedural quality of life [93, 94]. Moreover, glucose-lowering therapies are insufficient protection against IS risks in DM [95, 96]. DM and stroke are synergistically involved in the induction of cerebral-cardiac syndrome (CCS) characterized by arrhythmias, myocardial damage, and heart failure: DM drives chronic inflammation which aggravates CCS. Corresponding pathomechanisms involve inflammasomes [97]. IS has emerged as a serious complication of inflammation and cytokine storm by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [98]. To this end, COVID-19-related IS with particularly high rates and poor outcomes was recorded for patients with diabetes, hypertension, and hyperlipidaemia [99, 100]. Contextually, primary prevention of DMT2 is the most cost-effective approach against DM-associated IS with particularly poor outcomes.
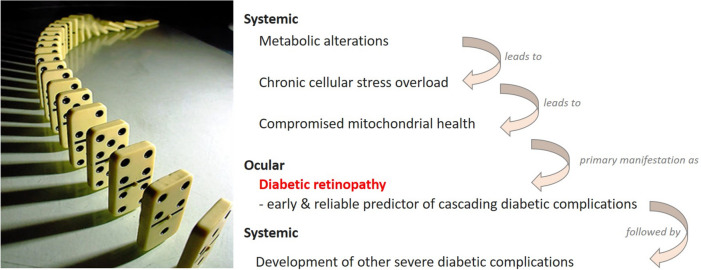
Diabetic retinopathy (DR) is a microvascular disease of the retina caused by systemic damaging effects triggered by metabolic disorders (diabetes mellitus, DM types 1 and 2). DR is clinically manifested as a progressing damage of retinal capillaries with secondary visual impairment widely recognised as the leading cause of blindness in the working-age population [101]. By far, not every DM patient develops DR and other secondary complications. However, once manifested, DR acts as an early indicator of complications related to DM. To this end, specifically proliferative DR is considered an independent predictor of cascading DM-related complications appearing as a “domino effect” as demonstrated in Fig. 3 [102].
Fig. 3.
DM-associated complications cascade appears as a “domino effect” downstream to proliferative DR characteristic for patients predisposed to severe comorbidities such as ischemic stroke; the image is adapted from [102]
An accumulated scientific evidence demonstrates the clinical manifestation of DM as a significant risk factor for stroke predisposition: patients with DM-history are at 2 to 4 times higher stroke risk compared to individuals without DM history. Moreover, the stroke risk severity correlates well with an increasing DR stage and disease progression [103]. Consequently, the prediction of DR progression in DM patients is highly instrumental for the cost-effective secondary care of the affected patient cohort with the potential to protect them against DM-promoted stroke manifestation. This concept has been implemented in the EPMA-promoted European project dedicated to biomarker-panels specific for the progressive DR which can be potentially identified in the tear fluid of affected individuals [55].
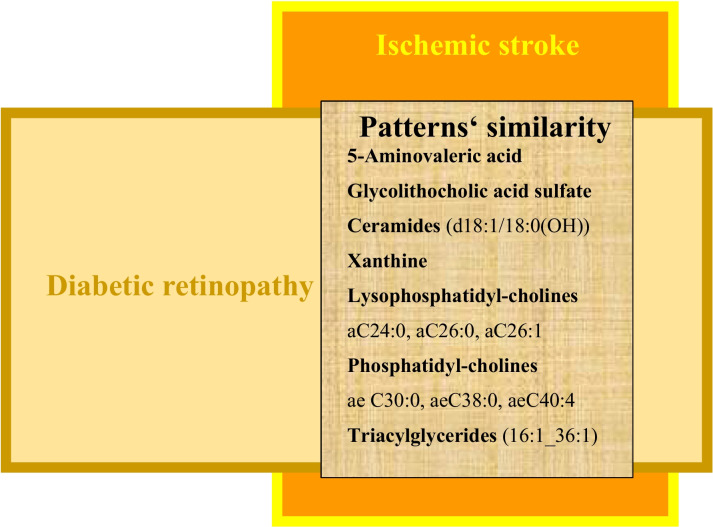
Indeed, preliminary data resulted from the study demonstrate a unique metabolic signature which is characteristic for proliferative retinopathy and can be routinely detected by applying mass spectrometric analysis to the tear fluid taken from vulnerable individuals. Furthermore, a great discovery has been made towards pattern’s similarity between both patient cohorts, namely, patients with diabetic retinopathy as a group at risk for stroke development and patients with clinically manifested ischemic stroke as imaged in Fig. 4. To this end, the implementation of a 3PM approach analysing the tear fluid of diabetic patients can identify the combined risk for diabetic retinopathy and IS with below presented metabolites as potential biomarker-sets.
5-Aminovaleric acid
Fig. 4.
Pattern’s similarity in the tear fluid detected in the vulnerable group of DR patients and patients with clinically manifested cardio-embolic ischemic stroke
Glucose and amino acid metabolism are closely related [104]. We found 5-aminovaleric acid and betaine distinguishable specifically in the tear fluid of the DR patients [55]. A similar association with cardiovascular morbidity and mortality has been found in the gut microbiome [105].
Glycolithocholic acid sulphate
Bile acids are critical factors in regulation of glucose, energy, and lipid associated metabolic pathways. In this context, a disturbed bile acid homeostasis has been linked to metabolic diseases like obesity, dyslipidaemia, and DM type 2 [106], which are well-known main risk factors for cardiovascular disease and stroke. In our study, in which the metabolic profile of diabetic patients was determined in tears, particularly the glycolithocholic acid sulphate, a molecule that is part of the bile acid metabolic cluster could only be detected in DR patients [55]. Moreover, regulation of bile acid and the gut microbiome have been proposed as predictive biomarkers, protective factors, and treatment targets for diabetes, atherosclerosis, and IS [107–109].
Ceramides
We found ceramide fractions specific for patients affected by diabetic retinopathy [55]. This result is consistent with the implication of lipotoxic ceramides in inflammation, β-cell apoptosis, and insulin resistance; moreover, they are involved in inducing and promoting microvascular and macrovascular complications relevant for DM and cardiovascular disease [110–112]. In vitro experiments could show that amongst others, ceramides disrupt vasodilation [113]. Thus, ceramides are considered reliable biomarkers for DM and cardiovascular disease, and its inhibitors are potential treatment targets in preventing DM and IS.
Xanthine
Xanthine was found in tears of DR patients [55]. The intermediate product of the purine nucleotide catabolism can bind in vitro to all nucleotide bases and normally does not incorporates into DNA and RNA [114]. Oxidative and nitrosative stress, however, can lead to oxidative deamination of DNA and the build of harmful deoxyxanthosine [114]. Both, oxidative and nitrosative stress, play a well-known key role in pathogenesis of DM type 2 and cardiovascular disease responsible for cellular stress, mitochondrial dysfunction, metabolic syndrome, inflammation, and apoptosis [115].
Lysophosphatidyl-cholines (LPC)
Highly increased LPC are correlated to neurodegeneration and diabetic retinopathy [87]. We found LPC profiles from diabetic retinopathy patients different to healthy controls [55]. Studies found increased level of LPC involved in blood-retinal-barrier damage, oxidative stress, and induction of vasopermeability [116, 117]. Similarly, Yuan et al. provoked demyelination in cerebellar organ culture treated with LPC that could be recovered by co-culture with regulatory T cells as potential treatment target after stroke [118].
Phosphatidyl-cholines
Phosphatidyl-cholines are components of plasma lipoproteins regulating circulating lipoprotein levels such as low-density (VLDLs) and high density (HDL) lipoproteins 113. Consequently, several studies demonstrated phosphatidyl-cholines related to a decreased risk for diabetes, cardiovascular disease and stroke [119–121].
Triacylglycerides
Though the exact role of distinct lipid classes in DM and stroke is still unknown, it is widely accepted that lipids and lipoproteins significantly contribute to their pathogenesis. We found triglycerides profiles measured in the tear fluid specific for the diabetic proliferative retinopathy [55]. Consistent with this data, an association between hypertriglyceridemia in diabetic patients and lower-extremity amputation risk has been shown [122]; blood triglycerides have been demonstrated as reliable pre/diabetes biomarkers [123]. In parallel, specific lipid profiles were demonstrated to be linked to high-risk for ischemic stroke [121].
Silent brain infarction (SBI) as an independent indicator of an active health‑to‑disease transition: making GP practice to the check-point for cost-effective IS protection in primary care.
“Silent strokes are not so silent” as stated by experts [16] who deal daily with abnormal brain scans looking for subtle changes indicated by SBI. Indeed, manifested SBI strongly predicts extended patterns of silent infarction zones [124] acting therefore as a powerful predictor of ischemic stroke in affected individuals. To this end, several research groups demonstrated over 50% prevalence of SBI in the ischemic stroke patients [125]. Moreover, an intensity of cognitive impairment and dementia correlates with SBI extend [126–129]. Similarly, in a Japanese study dedicated to the cognitive impairments of Alzheimer’s disease patients, every 3rd patient was co-diagnosed with SBI [130]. Specifically when localised in the thalamus, SBI causes impaired short-term memory performance [131–133], and non-thalamic SBI impairs psychomotor speed task performance [125]. SBI are frequently reported for people diagnosed with major depression [125, 134–136] and bipolar disorder type II with a suicide attempt [137]. Further, there is an association between migraine attacks and SBI manifestation [138, 139]. Due to high oestrogen levels, the female sex is a well-acknowledged risk factor of migraine with aura, thromboembolism, ischemia-induced aura, and ischemic stroke [140]. Female sex and migraine with aura are the characteristics for the Flammer syndrome phenotype (FSP, below is a case report presented), the affected carriers of which are strongly predisposed to SBI and normal-tension glaucoma (NTG) [141, 142].
Flammer syndrome phenotype (FSP) carriers are predisposed to silent lacunar brain lesions: a prominent clinically relevant example for the cost-effective primary protection against IS.
FSP is a well-described clinically relevant suboptimal health condition [143] strongly predisposed to disorders related to non-compensated stress overload such as pregnancy-associated complications, normal-tension glaucoma, lacunar ischemic lesions, and aggressive metastatic cancers [16, 144–149]. Corresponding pathomechanisms include primary vasospasm and low blood pressure, shifted circadian rhythms and sleep patterns, shifted sense regulation patterns (e.g. reduced thirst perception and thermal dysregulation), psychosomatic particularities (e.g. perfectionism), and compromised mitochondrial health, amongst others [144]. Corresponding systemic effects are well reflected in altered molecular patterns recorded in the blood of FSP carriers [150–152].
Herewith, we introduce the case of a 59-year-old woman who is a FSP carrier in suboptimal health condition. A specialised survey revealed strongly pronounced signs and symptoms of FSP including low body mass index, low blood pressure, migraine with aura, and strong vasospastic reactions under stress conditions; high stress-sensitivity further aggravated by meticulous personality and permanent work/stress overload caused by a highly ambitious international academic career of the patient.
Objectively diagnosed and measured are as follows:
-
A.
Family history of ischemic stroke (both parents with a successful academic career and high education level in medicine).
-
B.
Significantly increased endothelin-1 level (3.2 pg/ml) in blood serum, retinal ischemic lesions diagnosed early in life, and connective tissue impairments.
-
C.
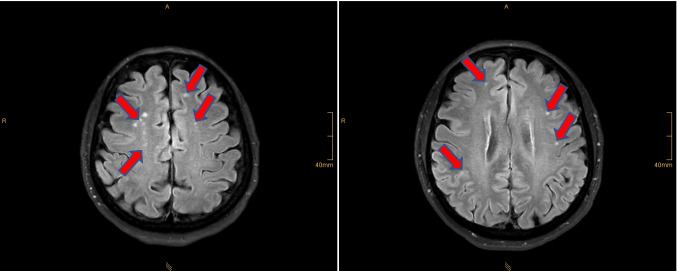
Brain MRI revealed silent lacunar ischemic lesions (see Fig. 5).
Fig. 5.
Brain-MRI; the multi-site pattern of lacunar microinfarction zones is clearly visible in the image (red arrows); 3Tesla-MRI was performed at the radiological clinic, University of Bonn, Germany; weight-adjusted intravenous contrast medium administration (CMA, gadolinium) was used
Protection against sudden cardiac arrest/death as a positive side effect benefiting populations by 3PM approach in IS primary care
An unexpected loss of cardi-vascular function resulting in circulatory collapse and death is defined as sudden cardiac death (SCD) as the end result of the sudden cardiac arrest (SCA) associated with about 90% mortality and high functional/cognitive disability of survivors [153]. Approximately 2 million cases of SCD are registered annually worldwide [153, 154]. Although the SCA incidence is relatively low in the general population, this medical condition is considered most unpredictable and demands robust health risk assessment for timely prediction and targeted prevention. To this end, a high level of similarity between risk factors of IS and SCA is instrumental for advanced health risk assessment to be implemented for innovative population screening saving lives and money. Table 3 summarises available data considering the most prominent demographic, socio-economic, non-clinical, and clinical risks.
Table 3.
Significant similarity between risk factors of IS and SCA: demographic, anthropometric, socio-economic, clinical, and non-clinical factors are considered. Abbreviations: IS ischemic stroke, SCA sudden cardiac arrest, Hhcy hyperhomocysteinaemia
| Health risk factors | IS | SCA | Comments | Scientific literature |
|---|---|---|---|---|
| Demographic | ||||
| Progressing age | Yes | Yes | Although elderly is an acknowledged risk for both IS and SCA, IS incidence is particularly increasing in young populations during last decade | Abundantly available |
| Male sex | Yes | Yes | Female sex is frequently associated with poorer outcomes, since symptoms are adapted to males | Abundantly available |
| Anthropometric | ||||
| Abnormal BMI | Yes | Yes | Both underweight and overweight are risks for IS and SCA, but the so-called obesity paradox is described as being potentially protective against poor IS outcomes, concluding that not BMI itself but rather shifted metabolism may be risky | [16, 17, 20, 154–156] |
| Central adiposity (waist-to-hip ratio) | Yes | Yes | Systemic effects | [154, 157] |
| Socio-economic | ||||
|
- Low education - Low income - Career-dedicated individuals (meticulous personality) |
Yes | Yes | “Blue collar-workers” are considered a vulnerable socio-economic category. On the other hand, “white collar-workers” demonstrate category-specific vulnerability as well | [16, 154] |
| Clinical | ||||
|
Cardiovascular susceptibility (in general) |
Yes | Yes | Including primary vasospasm (e.g. in Flammer syndrome phenotype susceptible to silent brain lesions, lacunar iIS) |
Abundantly available [16] |
| Arterial hypertension | ||||
|
Psychosomatic and psychiatric conditions |
Yes | Yes |
- Pre-existing psychiatric conditions - Psychotropic medication - Meticulous personality (e.g. Flammer syndrome) |
[16, 154] |
|
Short sleep, sleep apnoea, poor sleep quality |
Yes | Yes | A longer sleep duration (< 9 h a day) protects from SCA |
Abundantly available [158] |
| Chronic pain (CP) | Yes | Yes | Strong association between chronic low back pain, incident transient ischemic attack and stroke. Further, CP-medication increases risks of potentially fatal ventricular arrhythmia | [159, 160] |
| Systemic inflammation | Yes | Yes | Both microflora-induced and sterile inflammation with predictive and prognostic power | Abundantly available |
| Asthma | Yes | Yes | Asthma is associated significantly with increased risk of both IS and SCA | [161–163] |
| Metabolic shifts and impairments | Yes | Yes |
- Hyperglycaemia - Hypoglycaemia - Hypokalaemia - Hypomagnesemia - Hyperhomocysteinaemia |
Abundantly available |
| Mitochondrial homeostasis and signalling | Yes | Yes | Mitophagy is an excellent target for prediction, therapy and prognosis of both IS and SCA | Abundantly available |
| Trauma | Yes | Yes | Highly individual outcomes | Abundantly available |
| Treated and active malignancy | Yes | Yes | Systemic effects | Abundantly available |
| Drug overdose | Yes | Yes | Systemic effects | Abundantly available |
| Epilepsy | Yes | Yes | Reciprocity of mechanisms | Abundantly available |
| Sepsis | Yes | Yes | Systemic effects | Abundantly available |
| Non-clinical | ||||
| Hyperthermia | Yes | Yes | Systemic effects | Abundantly available |
| Dehydration | Yes | Yes | Systemic effects | Abundantly available |
| Asphyxia/hypoxia | Yes | Yes | Systemic effects | Abundantly available |
| Physical inactivity/overload | yes | Yes | Systemic effects | Abundantly available |
| Imbalanced diet | Yes | Yes | Systemic effects | Abundantly available |
| Stress overload | Yes | Yes | Systemic effects | Abundantly available |
| Smoking | Yes | Yes | Systemic effects | Abundantly available |
| Abnormal alcohol intake | Yes | Yes | Systemic effects | Abundantly available |
| Malnutrition | Yes | Yes | Systemic effects | Abundantly available |
| Toxic environment | Yes | Yes | Systemic effects | Abundantly available |
Case report
A male patient, 72 years of age, underwent investigations utilising a questionnaire and multi-omic analysis (metabolites’ profiling and mitophagy quantification) of his tear fluid three months before a sudden heart arrest/death which happened to him rather unexpectedly according to comments of his medical doctor in charge.
Below, we report on multi-factorial risks which are well in consensus with the data presented in Table 3. Moreover, according to metabolic analysis performed in the tear fluid, 10 biomarkers correspond to the molecular patterns relevant specifically for cardio-embolic ischemic stroke (clusters I, IV, V, VIII).
Demographic risks: male, 72 y.o.
Socio-economic risks: blue collar-worker, low level of education, low income—all socio-economic risks
Clinical risks: treated arterial hypertension; BMI = 28; higher waist-to-hip ratio; short sleep (6 h daily), snoring; since 5 years daily intake of pain-killers due to orthopaedic medical conditions (chronic pain/ inflammation).
Non-clinical risks: severe smoker, red meat-rich diet
- Risky metabolic patterns in the tear fluid (see Section "Tear fluid analysis of ischemic stroke patients with multi-factorial risks – preliminary results from international research project", Table 3)
- Cluster I: alpha-amino-butyric acid (4 times higher, red area), cysteine (3 times higher, red area), cysteine (1.5 times higher, yellow area), leucine (2 times higher, yellow area), and phenylalanine (2 times higher, yellow area) against the average value in the control group
- Cluster IV: arachidonic acid (4 times higher, red area), octadecenoic acid (2 times higher, yellow area), and eicosatrienoic acid (4 times higher, red area) against the average value in the control group
- Cluster V: lactic acid (3 times higher, red area) against the average value in the control group
- Cluster XIII: malonyl-carnitine (3 times higher, red area) against the average value in the control group.
Finally, quantitative PCR analysis of cf-mtDNA demonstrated mitochondrial burnout by extremely low levels of mitophagy measured in the tear fluid and compared with the age-matched reference data. The mitophagy quantification methodology in a liquid biopsy (blood) is described elsewhere such as [164] and further adapted to the tear fluid analysis followed by individualised data interpretation (the know-how of “3PMedicon GmbH” performing internationally validated tests [165]).
Expert recommendations for multi-professional consideration
3PM innovation to advance health risk assessment and protection against IS
Keeping in mind the above presented research data, for the follow-up studies, we state herewith that a number of risk factors are currently insufficiently considered which synergistically may predispose individuals at any age to IS development. To this end, a contribution specifically to young IS can be expected by below listed medical conditions which are to great extent unexplored but earned a strong indication in this paper.
Vascular stiffness of heterogeneous causality and primary vasospasm particularly in young individuals without traditional IS risks [16, 166].
Brain tissue remodelling (e.g. early in life mild and severe pre- and perinatal asphyxia [58].
Reciprocity between IS and cancers [16].
Mitochondrial stress reflected in condition-specific homeostasis patterns (see below Section “Mitochondria as a vital biosensor and attractive therapeutic target”).
Microbiota-gut-brain related inflammageing (see below Section" Microbiota-gut-brain axis: A promising intervention by pro- and prebiotics").
Specific psycho-somatic conditions: according to the biopsychosocial model of health and disease, psychological functioning is a crucial but rather neglected factor to be further used for the patient stratification. Specifically with a focus on stress coping capabilities, innovative biomarker sets are of pivotal importance to assess biopsychosocial profiles towards healthy aging in a society constantly getting older.
Accelerated ageing of heterogeneous causality (e.g. unhealthy lifestyle, suboptimal dietary habits, stress overload, toxic environment, metabolic syndrome, sleep disorders).
Corresponding risks can be estimated individually applying specialised surveys (to be further developed) at the level of primary care (general practitioners; see Section "General practitioners at the forefront of individualised IS prevention: preventable risks and reversible health-to-disease transition are in focus") and secondary care (e.g. ophthalmologic units; see Section "Tear fluid analysis of diabetic patients with retinopathy: making ophthalmologic units to the check-point for personalised IS prediction in diabetes care") followed by the tear fluid analysis of validated targets.
Considering the reciprocity between IS and cancers (above point 3), IS and cancers share several risk factors and pathomechanisms including oxidative stress, vascular impairments (including primary and secondary vasospasm), compromised mitochondrial health, and inflammation, which synergistically cause a vicious circle of the key systemic effects, namely, ischemia-reperfusions, ischemic lesions, blood–brain barrier breakdown, extensive tissue remodelling by the core of metalloproteinases, and pre-metastatic niches [16]. Further, cancer therapies can lead to an increased risk of IS: Meta-analysis shows that tamoxifen, a synthetic chemo-preventive drug in breast cancer management, increases ischemic stroke risk (82%) in women diagnosed with breast cancer [167]. Similarly, the use of aromatase inhibitors leads to a higher risk of IS and myocardial infarction in individuals diagnosed with breast cancer. Contextually, individualised patient profile is instrumental for IS-associated health risk assessment to advance overall management in cancer affected and cancer predisposed individuals.
Preliminary data considering molecular patterns in the tear fluid with a significant predictive power towards IS predisposition are presented in this paper (see Sections "Tear fluid analysis of ischemic stroke patients with multi-factorial risks – preliminary results from international research project" and "Tear fluid analysis of diabetic patients with retinopathy: making ophthalmologic units to the check-point for personalised IS prediction in diabetes care"). In terms of causality, several molecular pathways demonstrate an important role in and high specificity for some or several above listed medical conditions. For examples, there is an evident overlap between molecular patterns involved in IS and diabetic retinopathy as an early indicator of IS risk in DM as demonstrated in Fig. 4. Just to exemplify some of them such as the 5-aminolevulinic acid/pathway, which are also characteristic for an altered mitophagy [168], insomnia [169], stress regulation [170], and modulation of microbiota-gut-brain crosstalk [171, 172], amongst others. Further, ceramides are considered mediators of oxidative stress and inflammation in cardiometabolic disease [173], negatively affecting mitochondrial respiratory chain function and fission/fusion activity [174], altered sleep–wake behaviour [175], vascular stiffness, and remodelling [176], amongst others. Xanthine/pathway regulation is involved in mitochondrial homeostasis and stress-driven anxiety-like behaviour [177] as well as molecular mechanisms of arterial stiffness [178]. In order to assess individual health risks, an application of machine learning/artificial intelligence is unavoidable for an accurate data interpretation performed by the multiparametric analysis (see Section "Application of artificial intelligence to the 3PM approach").
Mitochondria as a vital biosensor and attractive therapeutic target
Mitochondria, acting as the “powerhouse”, routes the key events in human cells including proliferation, differentiation, growth and death, and modulate systemic effects such as stress response, redox balance, and severity of the acute and chronic disorders, amongst others. The reciprocity between mitochondrial and organismal health status has been demonstrated: on one hand, compromised mitochondrial health causes systemic damage, and on the other hand, organismal health-to-disease transition is reflected in mitochondrial dysfunction. To this end, mitochondrial population size, fission, fusion, biogenesis, and mitophagy are measurable parameters of mitochondrial homeostasis and, therefore, instrumental for predictive diagnostics and targeted treatments. Contextually, holistic 3PM strategies consider mitochondria as natural health status biosensor and an attractive therapeutic target in primary and secondary care. Table 5 presents conditions with elevated IS risk and mitochondrial component as an attractive target for 3PM strategies in primary and secondary care [179].
Table 4.
Conditions relevant for IS risks with mechanisms involving mitochondria as a natural vital biosensor [179]
| Conditions | Prominent examples and clarifying notes |
|---|---|
| Environmental and professional occupation risks with adverse effects on mitochondrial health status relevant for IS management in primary and secondary care | |
| Exposure to air pressure drop and elevation | Professional occupation; frequent flights |
| Toxic environment | Ambient air pollution, amongst others |
| Shift work | Changing physiologic circadian rhythms |
| Time-frame of daily activities deviating from individual circadian rhythm | Circadian rhythm associated sub/cellular mechanisms |
| Socio-economic and life-style associated risks relevant for mitochondrial impairments and IS | |
| Malnutrition and suboptimal dietary habits | Body weight gain and lost, shifted metabolism |
| Suboptimal lifestyle | Multifactorial risks including imbalanced stress overload and sedentary life-style, amongst others |
| Genetic risks relevant for mitochondrial impairments and IS | |
| Family predisposition to severe pathologies | Inborn disorders and genetic predisposition, e.g. to CVDs, autoimmune disorders, and stroke |
| Medical conditions highly relevant for mitochondrial impairments and IS predisposition | |
| Suboptimal health conditions | Health-to-disease transition linked to decreasing mitochondrial health quality |
| Vascular status associated conditions | Abnormally low and high blood pressure, vascular stiffness, increased endothelin-1 level, primary and secondary vasospasm, subtle but chronic ischemia–reperfusion, for example, typical for individuals with Flammer syndrome phenotype |
| Psychologic distress, psycho-trauma, and post-traumatic stress disorder | Mitochondrial stress potentially leading to mitochondrial burnout |
| Chronic fatigue and burnout syndrome | |
| Sleep disorders | |
| Chronic inflammation and associated conditions | Mitochondrial impairments to be diagnosed and treated |
| Prolonged and impaired wound healing | |
| Microbiome shifts/dysbiosis | Mitochondrial stress caused by bio-toxins; relevant sources of information: body fluids, skin, oral and vaginal cavities, digestive and urogenital tracts, airways, wounds, etc |
| Allergies | Breathing-related ischemia, mitochondrial stress |
| Asthma | |
| Premature ageing | Of multi-factorial origin progressed biologic age against chronologic one associated with decreased mitochondrial functionality |
| Medications highly relevant for mitochondrial impairments and IS predisposition | |
| Complex treatment of multi-factorial diseases | Mitochondrial component has to be considered in secondary prevention, monitoring of the therapy efficacy and predisposition to IS such as aggressive treatment of malignancies |
Microbiota-gut-brain axis: a promising intervention by pro- and prebiotics
Microbiota-gut-brain axis plays the central role in brain pathologies, ageing related systemic inflammation (inflammageing), premature ageing, and ageing-associated disorders with poor outcomes. To this end, the reciprocity between acute ischaemic stroke and gut dysbiosis has been clearly demonstrated: Ischaemic stroke is associated with acute gut microbiome dysbiosis indicated by prevalent Enterobacteriaceae which in turn exacerbates brain infarction [180]. Further, experimental stroke (middle cerebral artery occlusion) in young and aged male mice demonstrated microbiota-dependent outcomes. Dysbiosis characteristic for poor microbiota in aged mice, if transplanted to young mice, increased their mortality after induced stroke, thereby decreasing quality of behavioural patterns and increasing overall cytokines’ level [181]. In the same experimental sets, microbiota rejuvenation in aged mice significantly improved their outcomes after induced stroke. Contextually, pathogenesis of stroke involves imbalanced intestinal microbiota with strong pro-inflammatory response. Therefore, preventive probiotics and prebiotics application is considered a promising therapeutic intervention with significant health benefits to vulnerable subpopulations. Probiotics are defined as “live strains of strictly selected microorganisms which, when administered in adequate amounts, confer a health benefit on the host”, whereas prebiotics are defined as “a substrate that is selectively utilized by host microorganisms conferring a health benefit” [182]. These natural food supplements demonstrate evidenced properties to mitigate IS risks through several mechanisms modulating immune response and microflora composition with strong systemic effects [183] instrumental for predictive and preventive approach in overall IS management.
Application of artificial intelligence to the 3PM approach
As argued above, IS is a multi-factorial disease. Contextually, a robust health risk assessment is pivotal for 3PM innovation, and data-driven AI/machine learning (ML) techniques are required [184]. Generally speaking, ML is a multi-parametric statistical model adapted to the data available; this “learning” process results in a “pattern” or “rule” characteristic for the medical condition under consideration. ML can be supervised or unsupervised. In a supervised learning, the model is trained based on datasets coupled with known clinical outcomes such as IS manifestation and severity grade. In the next step, based on the established model health risk assessment/prediction/prognosis have to be validated by application of algorithms to a new patient cohort which was not part of the training round. ML models are particularly applicable to cases, when there is no any “decisive” biomarker capable to rigorously discriminate between “yes” and “no” disease. Noteworthy, opportunities for ML go significantly beyond the disease classification covering a possibility to predict disease development, progression and severity. Opposed to supervised learning, unsupervised learning aims at inferring patterns from data without having access to a label, such as phenotype. Consequently, ML models can discard features which are irrelevant for the prediction (sparse models). The set of features selected by the algorithm can then establish a precise biomarker signature which is characteristic for the medical condition under consideration [185–187]. However, any ML model is capable to capture a pattern involving the data which the algorithm was originally trained on. Therefore, the next step is thus to integrate data (coming from the same patient) across all relevant biological scales and then to develop more advanced AI/ML models on these combined data sources. Single organizations typically do not possess or are unable to collect such multi-modal data in sufficient quantity and representativeness of the entire disease population. Hence, it will be necessary to set up an according data ecosystem across multiple international institutions. Given the current legal constraints on sharing of patient-level data in many areas of the world (such as the GDPR in the European Union), such an effort can only be successful, if data can be accessed and used in a decentralized manner, for example, with the help of federated data access and federated machine learning concepts, including swarm learning [188]. Noteworthy, implementation of such concepts is technically, legally, and organisationally challenging, and requires a close collaboration between multi-professional groups including physicians, data scientists, software engineers, lawyers, patient organisations, and policy-makers.
General practitioners at the forefront of individualised IS prevention: preventable risks and reversible health-to-disease transition are in focus
The majority of IS cases are preventable, and modifiable risk factors are known. Contextually, the paradigm in overall IS management has to be shifted from reactive care of clinically manifested pathology to prediction, targeted prevention, and personalised treatment of suboptimal health conditions characterised by a reversible damage to health. Therefore, specifically general practitioners are at the forefront implementing the paradigm of 3P medicine in targeted prevention of IS. For doing that, predictive diagnostic tools are developed to a great extent as highlighted above. What might be the practicable workflow in the overall procedure and what are the remaining bottle-necks?
-
A.
Phenotyping based on specialised surveys
Highly relevant information can be received by routed interviews performed at regular check-up including family predisposition, health status, lifestyle habits, sleep and dietary patterns, and anthropometrics, amongst others—all highly relevant for preliminary health risk assessment followed by in-depth genotyping.
-
B.
In-depth molecular analysis based on liquid biopsy
This tool is instrumental for predictive diagnostics based on molecular patterns specific for disease pre-stages. Section "Tear fluid analysis of ischemic stroke patients with multi-factorial risks – preliminary results from international research project" provides an example on how non-invasive tear fluid analysis can be of great clinical utility to predict IS development in individuals with and without clinically evident IS predisposition. Follow-up studies are essential to finalise validation of proposed biomarker-patterns.
-
C.
Health risk assessment based on individualised patient profiles
A combination of (A) and (B) comprises a set of parameters for an individualised risk assessment. Due to precise multi-parametric analysis, an involvement of artificial intelligence (AI) is essential to create algorithms which allow for highly precise predictive diagnosis, evaluation of modifiable risks, and elaboration of programmes for targeted mitigation measures. The AI aspects are further detailed in the below presented Section "Application of artificial intelligence to the 3PM approach".
-
D.
Multi-professional collaboration in 3P medicine
A tight collaboration between all relevant stakeholders is essential including healthcare industry, researchers, educators, patient organisations, and policymakers, amongst others. Effective realisation of 3PM principles, strategies, and approaches saves human and financial resources. However, 3PM innovation should be supported administratively and economically at any stage “from bench to bedside”.
-
E.
Educational programmes in 3P medicine is a “must” for the society
In order to implement 3PM innovation, the essential pillars are as follows: broad acceptance in the population, patient-doctor cooperation (participatory medicine), and high level of professionalism at the side of caregivers. This is challenging and can be achieved by introducing specialised educational programmes for professionals and general population utilising high level of 3PM didactic materials [189].
Acknowledgements
The authors thank to Assoc. Prof. Dr. C. Pieper and Dr. O. Kaverina for the Brain-MRI (Figure 5) performance.
Abbreviations
- AI
Artificial intelligence
- 5-AVA
5-Amino-valeric acid
- BMI
Body mass index
- CEIS
Cardio-embolic ischemic stroke
- cf-mtDNA
Cell-free mitochondrial DNA
- CP
Chronic pain
- DALYs
Disability-adjusted life-years
- DM
Diabetes mellitus
- DMT2
Diabetes mellitus type 2
- EPMA
European Association for Predictive, Preventive and Personalised Medicine
- FSP
Flammer syndrome phenotype
- GBD
Global burden of disease
- GDPR
General data protection regulation
- Hhcy
Hyperhomocysteinaemia
- IS
Ischemic stroke
- ML
Machine learning
- PCR
Polymerase chain rection
- PPPM/3PM
Predictive preventive personalised medicine
- ROS
Reactive oxygen species
- SBI
Silent brain infarction
- SCA
Sudden cardiac arrest
- SCD
Sudden cardiac death
Author contribution
O.G. was responsible for the study conception, project coordination, data analysis, and interpretation. J.P. coordinated the neurological expert group. J.P. Jr., P.P., and M.P. were responsible for the project dedicated to the stroke-specific tear fluid multi-omic analysis. I.St. provided expertise in stroke management. M.Kr., G.T., and C.E. provided expertise in ophthalmology. M.Kr. and G.T. were responsible for the project dedicated to the tear fluid multi-omic analysis in diabetic retinopathy. A.M., L.L., and P.K. performed literature search on stroke statistics and risks. O.G. provided expertise in mitochondrial health check-up. H.F. provided expertise in AI. W.W. contributed with his expertise in sub-optimal health. B.B. provided expertise in inflammageing. M.Ka. contributed with expertise in molecular medicine. N.S. provided expertise in nutrition. K.R. contributed with expertise in sleep medicine. A.K. provided expertise in project-relevant psycho-somatic conditions. I.Sm. contributed with expertise in diabetes management. F.P. provided expertise in neurology. P.P. contributed with expertise in cardio-vascular aspects. C.S. and E.G. contributed with expertise in reciprocity between cancers and stroke. The manuscript was drafted by O.G., J.P. Jr., M.P, A.M., L.L., P.K. M.Kr., H.F., B.B., N.S., and I.Sm. and critically revised by P.P., I.St., G.T., C.E., W.W., M.Ka., K.R., A.K., C.S., E.G., F.P., P.P., and J.P. All authors have read and agreed to the published version of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
The cumulative research paper was supported by the following:
• The European Association for Predictive, Preventive and Personalised Medicine, EPMA, Brussels
• The Cooperation Programme, research area MED/DIAG, Charles University and by a grant from the Ministry of Health of the Czech Republic - Conceptual Development of Research Organization (University Hospital Pilsen—FNPL, 00669806)
• The LHW Foundation, Liechtenstein.
Data Availability
Not applicable.
Code availability
Not applicable.
Declarations
Ethics approval
All investigations made on human participants were conducted according to the guidelines of the Declaration of Helsinki. Ethical approval has been provided by responsible bodies in Germany (Ethical Commission of Medical Faculty, University of Bonn, protocol number 505/20 dated on November 11th, 2020), Switzerland (Commission cantonale d’éthique de la recherche de Genève, CCER, University of Geneva, protocol code 2020–02196, 19 November 2020) and Czech Republic Czech Republic (University Hospital Pilsen and Faculty of Medicine in Plzen, Charles University, Prague, protocol number FN/1252/01 dated on July 2nd 2020).
Conflicts of Interest
The authors declare no conflict of interest. Prof. Dr. Olga Golubnitschaja is an editor of the EPMA J., and recused herself from all decisions about the paper. She is a shareholder of 3PMedicon. Dr. Jiri Polivka Jr. is a shareholder of 3PMedicon.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.GBD 2019 Stroke Collaborators Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820. doi: 10.1016/S1474-4422(21)00252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Owolabi MO, Thrift AG, Mahal A, et al. Primary stroke prevention worldwide: translating evidence into action. Lancet Public Health. 2022;7(1):e74–85. doi: 10.1016/S2468-2667(21)00230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson CO, Nguyen M, Roth GA, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):439–58. doi: 10.1016/S1474-4422(19)30034-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindsay MP, Norrving B, Sacco RL, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2019. Int J Stroke. 2019;14(8):806–817. doi: 10.1177/1747493019881353. [DOI] [PubMed] [Google Scholar]
- 5.Feigin VL, Brainin M, Norrving B, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int J Stroke. 2022;17(1):18–29. doi: 10.1177/17474930211065917. [DOI] [PubMed] [Google Scholar]
- 6.GBD 2016 Stroke Collaborators Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):439–58. doi: 10.1016/S1474-4422(19)30034-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ak C, Gupta R, Warkade V. Study of clinical profile and risk factors for ischemic stroke in young adults. J Assoc Phys India. 2022;70(4):11–12. [Google Scholar]
- 8.Rodríguez-Campello A, Jiménez-Conde J, Ois Á, et al. Dietary habits in patients with ischemic stroke: a case-control study. PLoS ONE. 2014;9(12):e114716. doi: 10.1371/journal.pone.0114716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lavados PM, Mazzon E, Rojo A, Brunser AM, Olavarría VV. Pre-stroke adherence to a Mediterranean diet pattern is associated with lower acute ischemic stroke severity: a cross-sectional analysis of a prospective hospital-register study. BMC Neurol. 2020;20(1):252. doi: 10.1186/s12883-020-01824-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang H, Gong F, Guo H, et al. Malnutrition and risk of mortality in ischemic stroke patients treated with intravenous thrombolysis. Front Aging Neurosci. 2022;14:834973. doi: 10.3389/fnagi.2022.834973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bouziana SD, Tziomalos K. Malnutrition in patients with acute stroke. J Nutr Metab. 2011;2011:167898. doi: 10.1155/2011/167898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoo S-H, Kim JS, Kwon SU, Yun S-C, Koh J-Y, Kang D-W. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol. 2008;65(1):39–43. doi: 10.1001/archneurol.2007.12. [DOI] [PubMed] [Google Scholar]
- 13.Horn JW, Feng T, Mørkedal B, et al. Obesity and risk for first ischemic stroke depends on metabolic syndrome: the HUNT study. Stroke. 2021;52(11):3555–3561. doi: 10.1161/STROKEAHA.120.033016. [DOI] [PubMed] [Google Scholar]
- 14.Shiozawa M, Kaneko H, Itoh H, et al. Association of body mass index with ischemic and hemorrhagic stroke. Nutrients. 2021;13(7):2343. doi: 10.3390/nu13072343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bardugo A, Fishman B, Libruder C, et al. Body mass index in 1.9 million adolescents and stroke in young adulthood. Stroke. 2021;52(6):2043–52. doi: 10.1161/STROKEAHA.120.033595. [DOI] [PubMed] [Google Scholar]
- 16.Golubnitschaja O, Potuznik P, Polivka J, et al. Ischemic stroke of unclear aetiology: a case-by-case analysis and call for a multi-professional predictive, preventive and personalised approach. EPMA J. 2022;13(4):535–545. doi: 10.1007/s13167-022-00307-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Golubnitschaja O, Liskova A, Koklesova L, et al. Caution, “normal” BMI: health risks associated with potentially masked individual underweight-EPMA Position Paper 2021. EPMA J. 2021;12(3):243–264. doi: 10.1007/s13167-021-00251-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Song DK, Hong YS, Sung Y-A, Lee H. Body mass index and stroke risk among patients with diabetes mellitus in Korea. PLoS ONE. 2022;17(9):e0275393. doi: 10.1371/journal.pone.0275393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaudhary D, Khan A, Gupta M, et al. Obesity and mortality after the first ischemic stroke: Is obesity paradox real? PLoS ONE. 2021;16(2):e0246877. doi: 10.1371/journal.pone.0246877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oesch L, Tatlisumak T, Arnold M, Sarikaya H. Obesity paradox in stroke – myth or reality? A systematic review. PLoS ONE. 2017;12(3):e0171334. doi: 10.1371/journal.pone.0171334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho L-C, Wang H-K, Chiu L-T, et al. Protein energy wasting–based nutritional assessment predicts outcomes of acute ischemic stroke and solves the epidemiologic paradox. Nutrition. 2022;93:111431. doi: 10.1016/j.nut.2021.111431. [DOI] [PubMed] [Google Scholar]
- 22.Middleton LE, Corbett D, Brooks D, et al. Physical activity in the prevention of ischemic stroke and improvement of outcomes: a narrative review. Neurosci Biobehav Rev. 2013;37(2):133–137. doi: 10.1016/j.neubiorev.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 23.Cowan LT, Tome J, Mallhi AK, et al. Changes in physical activity and risk of ischemic stroke: the ARIC study. Int J Stroke. 2023;18(2):173–179. doi: 10.1177/17474930221094221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo S, Huang Y, Zhang Y, Huang H, Hong S, Liu T. Impacts of exercise interventions on different diseases and organ functions in mice. J Sport Health Sci. 2020;9(1):53–73. doi: 10.1016/j.jshs.2019.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krako Jakovljevic N, Pavlovic K, Jotic A, et al. Targeting mitochondria in diabetes. IJMS. 2021;22(12):6642. doi: 10.3390/ijms22126642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee Y, Min K, Talbert EE, et al. Exercise protects cardiac mitochondria against ischemia-reperfusion injury. Med Sci Sports Exerc. 2012;44(3):397–405. doi: 10.1249/MSS.0b013e318231c037. [DOI] [PubMed] [Google Scholar]
- 27.Di Meo S, Venditti P. Mitochondria in exercise-induced oxidative stress. Biol Signals Recept. 2001;10(1–2):125–140. doi: 10.1159/000046880. [DOI] [PubMed] [Google Scholar]
- 28.Layec G, Blain GM, Rossman MJ, et al. Acute high-intensity exercise impairs skeletal muscle respiratory capacity. Med Sci Sports Exerc. 2018;50(12):2409–2417. doi: 10.1249/MSS.0000000000001735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Avellaneda-Gómez C, Vivanco-Hidalgo RM, Olmos S, et al. Air pollution and surrounding greenness in relation to ischemic stroke: a population-based cohort study. Environ Int. 2022;161:107147. doi: 10.1016/j.envint.2022.107147. [DOI] [PubMed] [Google Scholar]
- 30.Dev P, Gupta P, Mahapatra A, et al. Systematic review and meta-analysis of environmental toxic metal contaminants and the risk of ischemic stroke. Ann Indian Acad Neurol. 2022;25(6):1159–1166. doi: 10.4103/aian.aian_530_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee HR, Yoo JE, Choi H, et al. Tuberculosis and risk of ischemic stroke: a nationwide cohort study. Stroke. 2022;53(11):3401–3409. doi: 10.1161/STROKEAHA.122.039484. [DOI] [PubMed] [Google Scholar]
- 32.Wei Y, Tang S, Xie Z, et al. Pulmonary tuberculosis-related ischemic stroke: a retrospective case control study. J Inflamm Res. 2022;15:4239–4249. doi: 10.2147/JIR.S368183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li J, Lee DH, Hu J, et al. Dietary inflammatory potential and risk of cardiovascular disease among men and women in the U.S. J Am Coll Cardiol. 2020;76(19):2181–93. doi: 10.1016/j.jacc.2020.09.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Golubnitschaja O, Baban B, Boniolo G, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7(1):23. doi: 10.1186/s13167-016-0072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leary MC, Saver JL. Annual incidence of first silent stroke in the United States: a preliminary estimate. Cerebrovasc Dis. 2003;16(3):280–285. doi: 10.1159/000071128. [DOI] [PubMed] [Google Scholar]
- 36.Vermeer SE, Longstreth WT, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6(7):611–619. doi: 10.1016/S1474-4422(07)70170-9. [DOI] [PubMed] [Google Scholar]
- 37.Kobayashi S, Okada K, Koide H, Bokura H, Yamaguchi S. Subcortical silent brain infarction as a risk factor for clinical stroke. Stroke. 1997;28(10):1932–9. doi: 10.1161/01.STR.28.10.1932. [DOI] [PubMed] [Google Scholar]
- 38.Uehara T, Tabuchi M, Mori E. Risk factors for silent cerebral infarcts in subcortical white matter and basal ganglia. Stroke. 1999;30(2):378–382. doi: 10.1161/01.STR.30.2.378. [DOI] [PubMed] [Google Scholar]
- 39.Lee S-C, Park S-J, Ki H-K, et al. Prevalence and risk factors of silent cerebral infarction in apparently normal adults. Hypertension. 2000;36(1):73–77. doi: 10.1161/01.HYP.36.1.73-a. [DOI] [PubMed] [Google Scholar]
- 40.Matsui T, Arai H, Yuzuriha T, et al. Elevated plasma homocysteine levels and risk of silent brain infarction in elderly people. Stroke. 2001;32(5):1116–1119. doi: 10.1161/01.STR.32.5.1116. [DOI] [PubMed] [Google Scholar]
- 41.Maeshima S, Moriwaki H, Ozaki F, Okita R, Yamaga H, Ueyoshi A. Silent cerebral infarction and cognitive function in middle-aged neurologically healthy subjects. Acta Neurol Scand. 2002;105(3):179–184. doi: 10.1034/j.1600-0404.2002.1o068.x. [DOI] [PubMed] [Google Scholar]
- 42.Waldstein SR, Siegel EL, Lefkowitz D, et al. Stress-induced blood pressure reactivity and silent cerebrovascular disease. Stroke. 2004;35(6):1294–1298. doi: 10.1161/01.STR.0000127774.43890.5b. [DOI] [PubMed] [Google Scholar]
- 43.Kotani K, Osaki Y, Sakane N, Adachi S, Ishimaru Y. Risk factors for silent cerebral infarction in the elderly. Arch Med Res. 2004;35(6):522–524. doi: 10.1016/j.arcmed.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 44.Kwon H-M, Kim BJ, Lee S-H, Choi SH, Oh B-H, Yoon B-W. Metabolic syndrome as an independent risk factor of silent brain infarction in healthy people. Stroke. 2006;37(2):466–470. doi: 10.1161/01.STR.0000199081.17935.81. [DOI] [PubMed] [Google Scholar]
- 45.Goldstein LB, Adams R, Becker K, et al. Primary prevention of ischemic stroke. Stroke. 2001;32(1):280–299. doi: 10.1161/01.STR.32.1.280. [DOI] [PubMed] [Google Scholar]
- 46.Vogels EA, Lagro-Janssen AL, van Weel C. Sex differences in cardiovascular disease: are women with low socioeconomic status at high risk? Br J Gen Pract. 1999;49(449):963–966. [PMC free article] [PubMed] [Google Scholar]
- 47.Herlitz J, Bang A, Karlson BW, Hartford M. Is there a gender difference in aetiology of chest pain and symptoms associated with acute myocardial infarction? Eur J Emerg Med. 1999;6(4):311. doi: 10.1097/00063110-199912000-00007. [DOI] [PubMed] [Google Scholar]
- 48.Holroyd-Leduc JM, Kapral MK, Austin PC, Tu JV. Sex differences and similarities in the management and outcome of stroke patients. Stroke. 2000;31(8):1833–1837. doi: 10.1161/01.STR.31.8.1833. [DOI] [PubMed] [Google Scholar]
- 49.Ramani S, Byrne-Logan S, Freund KM, Ash A, Yu W, Moskowitz MA. Gender differences in the treatment of cerebrovascular disease. J Am Geriatr Soc. 2000;48(7):741–745. doi: 10.1111/j.1532-5415.2000.tb04747.x. [DOI] [PubMed] [Google Scholar]
- 50.Golubnitschaja O. Changing long-held beliefs is never easy: a proposal for multi-modal approach in female healthcare – an integrative view. In: Healthcare overview - new perpectives. In the book “Healthcare Overview - New Perspectives” (Ed: Vincenzo Costigliola), Springer Dordrecht Heidelberg New York London. 2012. 10.1007/978-94-007-4602-2.
- 51.Golubnitschaja O. Mitochondrion – The subordinated partner who agreed to come short but insists in healthy life. In: Wang Wei., editor. All Around Suboptimal Health - Advanced approaches by Predictive, Preventive and Personalised Medicine for Healthy Populations. Switzerland: Springer; 2023. [Google Scholar]
- 52.Hagan S, Martin E, Enríquez-de-Salamanca A. Tear fluid biomarkers in ocular and systemic disease: potential use for predictive, preventive and personalised medicine. EPMA J. 2016;7(1):15. doi: 10.1186/s13167-016-0065-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gerner C, Costigliola V, Golubnitschaja O. Multiomic patterns in body fluids: technological challenge with a great potential to implement the advanced paradigm of 3p medicine. Mass Spectrom Rev. 2020;39(5–6):442–451. doi: 10.1002/mas.21612. [DOI] [PubMed] [Google Scholar]
- 54.Zhan X, Li J, Guo Y, Golubnitschaja O. Mass spectrometry analysis of human tear fluid biomarkers specific for ocular and systemic diseases in the context of 3P medicine. EPMA J. 2021;12:449–475. doi: 10.1007/s13167-021-00265-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kropp M, De Clerck E, Vo T-TKS, Thumann G, Costigliola V, Golubnitschaja O. Short communication: unique metabolic signature of proliferative retinopathy in the tear fluid of diabetic patients with comorbidities - preliminary data for PPPM validation. EPMA J. 2023;14(1):43–51. doi: 10.1007/s13167-023-00318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim J, Campbell AS, de Ávila BE, Wang J. Wearable biosensors for healthcare monitoring. Nat Biotechnol. 2019;37(4):389–406. doi: 10.1038/s41587-019-0045-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Golubnitschaja O, Costigliola V, Olga EPMA. General report & recommendations in predictive, preventive and personalised medicine 2012: white paper of the European Association for Predictive, Preventive and Personalised Medicine. EPMA J. 2012;3(1):14. doi: 10.1186/1878-5085-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Golubnitschaja O, Yeghiazaryan K, Cebioglu M, Morelli M, Herrera-Marschitz M. Birth asphyxia as the major complication in newborns: moving towards improved individual outcomes by prediction, targeted prevention and tailored medical care. EPMA J. 2011;2(2):197–210. doi: 10.1007/s13167-011-0087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Golubnitschaja O, Watson ID, Topic E, Sandberg S, Ferrari M, Costigliola V. Position paper of the EPMA and EFLM: a global vision of the consolidated promotion of an integrative medical approach to advance health care. EPMA J. 2013;4(1):12. doi: 10.1186/1878-5085-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ramsay SL, STÖGGL WM, Weinberger KM, Graber A, Guggenbichler W. Apparatus for analyzing a metabolite profile. Patent 2014;EP1897014B1. Available from: https://patents.google.com/patent/EP1897014B1/en. Accessed 22 Jan 2024.
- 61.Ramsay SL, Guggenbichler W, Weinberger KM, Graber A, STÖGGL WM. Device for quantitative analysis of a metabolite profile. Patent 2014;EP1875401B1. Available from: https://patents.google.com/patent/EP1875401B1/en. Accessed 22 Jan 2024.
- 62.Takeshita M, Tabara Y, Setoh K, et al. Development of a plasma-free amino acid-based risk score for the incidence of cardiovascular diseases in a general population: The Nagahama study. Clin Nutr. 2023;42(12):2512–2519. doi: 10.1016/j.clnu.2023.10.024. [DOI] [PubMed] [Google Scholar]
- 63.Jauhiainen R, Vangipurapu J, Laakso A, Kuulasmaa T, Kuusisto J, Laakso M. The association of 9 amino acids with cardiovascular events in Finnish men in a 12-year follow-up study. J Clin Endocrinol Metab. 2021;106(12):3448–3454. doi: 10.1210/clinem/dgab562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hajsl M, Hlavackova A, Broulikova K, et al. Tryptophan metabolism, inflammation, and oxidative stress in patients with neurovascular disease. Metabolites. 2020;10(5):208. doi: 10.3390/metabo10050208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Haikonen R, Kärkkäinen O, Koistinen V, Hanhineva K. Diet- and microbiota-related metabolite, 5-aminovaleric acid betaine (5-AVAB), in health and disease. Trends Endocrinol Metab. 2022;33(7):463–480. doi: 10.1016/j.tem.2022.04.004. [DOI] [PubMed] [Google Scholar]
- 66.Tveter KM, Mezhibovsky E, Wu Y, Roopchand DE. Bile acid metabolism and signaling: emerging pharmacological targets of dietary polyphenols. Pharmacol Ther. 2023;248:108457. doi: 10.1016/j.pharmthera.2023.108457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu J, Yuan J, Zhao J, Zhang L, Wang Q, Wang G. Serum metabolomic patterns in young patients with ischemic stroke: a case study. Metabolomics. 2021;17(2):24. doi: 10.1007/s11306-021-01774-7. [DOI] [PubMed] [Google Scholar]
- 68.Miękus N, Olędzka I, Kowalski P, Miękus P, Baczek T. Practical application of biogenic amine profiles for the diagnosis of patients with ischemic stroke. J Stroke Cerebrovasc Dis. 2018;27(4):945–950. doi: 10.1016/j.jstrokecerebrovasdis.2017.10.041. [DOI] [PubMed] [Google Scholar]
- 69.Lee E, Kim DJ, Cho J-Y, Jung K. Abstract WMP114: putrescine and kynurenine are associated with large artery atherosclerosis stroke: targeted metabolomics study. Stroke. 2022;53(Suppl_1):AWMP114–AWMP114. doi: 10.1161/str.53.suppl_1.WMP114. [DOI] [Google Scholar]
- 70.Lee H, Chu Y-K, Shon J-H, Chun K-H, Kim J-I, Lee S-R. Effect of L-deprenyl on the putrescine level and neuronal damage after transient global cerebral ischemia in gerbils. Int J Org Chem. 2017;7(2):171–184. doi: 10.4236/ijoc.2017.72014. [DOI] [Google Scholar]
- 71.Li Z, Lei H, Jiang H, et al. Saturated fatty acid biomarkers and risk of cardiometabolic diseases: a meta-analysis of prospective studies. Front Nutr. 2022;9:963471. doi: 10.3389/fnut.2022.963471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jung JY, Lee H-S, Kang D-G, et al. 1H-NMR-based metabolomics study of cerebral infarction. Stroke. 2011;42(5):1282–1288. doi: 10.1161/STROKEAHA.110.598789. [DOI] [PubMed] [Google Scholar]
- 73.Li M, Xiao H, Qiu Y, et al. Identification of potential diagnostic biomarkers of cerebral infarction using gas chromatography-mass spectrometry and chemometrics. RSC Adv. 2018;8(41):22866–22875. doi: 10.1039/C8RA03132K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tóth OM, Menyhárt Á, Frank R, Hantosi D, Farkas E, Bari F. Tissue acidosis associated with ischemic stroke to guide neuroprotective drug delivery. Biology (Basel) 2020;9(12):460. [DOI] [PMC free article] [PubMed]
- 75.Collister D, Ferguson TW, Funk SE, Reaven NL, Mathur V, Tangri N. Metabolic acidosis and cardiovascular disease in CKD. Kidney Med. 2021;3(5):753–761.e1. doi: 10.1016/j.xkme.2021.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Oreshnikov E, Oreshnikova S, Oreshnikov A. 741: Purine metabolites, hormones, and lethal outcome in acute cerebral ischemia: some aspects. Crit Care Med. 2021;49(1):367. [Google Scholar]
- 77.Tariq MA, Shamim SA, Rana KF, Saeed A, Malik BH. Serum uric acid - risk factor for acute ischemic stroke and poor outcomes. Cureus. 2019;11(10):e6007. doi: 10.7759/cureus.6007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Saini G, Kaur K, Bhatia L, Kaur R, Singh J, Singh G. Single Serum Cortisol Value as a Prognostic Marker in Acute Ischemic Stroke. Cureus. 2023;15(6):e40887. doi: 10.7759/cureus.40887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Busik JV. Lipid metabolism dysregulation in diabetic retinopathy. J Lipid Research 2021;62:100017. [DOI] [PMC free article] [PubMed]
- 80.Aljanabi NM, Mamtani SS, Acharya A, Gupta Rauniyar RP, Malik BH. Association between cerebrovascular accident and vasculitis: myth or reality? Cureus. 2023;11(12):e6345. doi: 10.7759/cureus.6345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Elkind MSV, Boehme AK, Smith CJ, Meisel A, Buckwalter MS. Infection as a stroke risk factor and determinant of outcome after stroke. Stroke. 2020;51(10):3156–3168. doi: 10.1161/STROKEAHA.120.030429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nagel MA, Mahalingam R, Cohrs RJ, Gilden D. Virus vasculopathy and stroke: an under-recognized cause and treatment target. Infect Disord Drug Targets. 2010;10(2):105–111. doi: 10.2174/187152610790963537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ziu E, Khan Suheb MZ, Mesfin FB. Subarachnoid hemorrhage. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. http://www.ncbi.nlm.nih.gov/books/NBK441958/. Accessed 22 Jan 2024. [PubMed]
- 84.Katajamäki TT, Koivula M-K, Hilvo M, et al. Ceramides and phosphatidylcholines associate with cardiovascular diseases in the elderly. Clin Chem. 2022;68(12):1502–1508. doi: 10.1093/clinchem/hvac158. [DOI] [PubMed] [Google Scholar]
- 85.Huang M, Xu S, Zhou M, et al. Lysophosphatidylcholines and phosphatidylcholines as biomarkers for stroke recovery. Frontiers in Neurology 2022;13:1047101 [DOI] [PMC free article] [PubMed]
- 86.Law S-H, Chan M-L, Marathe GK, Parveen F, Chen C-H, Ke L-Y. An updated review of lysophosphatidylcholine metabolism in human diseases. Int J Mol Sci. 2019;20(5):1149. doi: 10.3390/ijms20051149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cheng L, Han X, Shi Y. A regulatory role of LPCAT1 in the synthesis of inflammatory lipids, PAF and LPC, in the retina of diabetic mice. Am J Physiol-Endocrinol Metab. 2009;297(6):E1276–E1282. doi: 10.1152/ajpendo.00475.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jové M, Mauri-Capdevila G, Suárez I, et al. Metabolomics predicts stroke recurrence after transient ischemic attack. Neurology. 2015;84(1):36–45. doi: 10.1212/WNL.0000000000001093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liang H-J, Zhang Q-Y, Hu Y-T, Liu G-Q, Qi R. Hypertriglyceridemia: a neglected risk factor for ischemic stroke? J Stroke. 2022;24(1):21–40. doi: 10.5853/jos.2021.02831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mavroudakis L, Lanekoff I. Ischemic Stroke causes disruptions in the carnitine shuttle system. Metabolites. 2023;13(2):278. doi: 10.3390/metabo13020278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Seo W-K, Jo G, Shin M-J, Oh K. Medium-chain acylcarnitines are associated with cardioembolic stroke and stroke recurrence. Arterioscler Thromb Vasc Biol. 2018;38(9):2245–2253. doi: 10.1161/ATVBAHA.118.311373. [DOI] [PubMed] [Google Scholar]
- 92.Maida CD, Daidone M, Pacinella G, Norrito RL, Pinto A, Tuttolomondo A. Diabetes and ischemic stroke: an old and new relationship an overview of the close interaction between these diseases. Int J Mol Sci. 2022;23(4):2397. doi: 10.3390/ijms23042397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen R, Ovbiagele B, Feng W. Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. Am J Med Sci. 2016;351(4):380–386. doi: 10.1016/j.amjms.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bradley SA, Smokovski I, Bhaskar SMM. Impact of diabetes on clinical and safety outcomes in acute ischemic stroke patients receiving reperfusion therapy: a meta-analysis. Adv Clin Exp Med. 2022;31(6):583–596. doi: 10.17219/acem/146273. [DOI] [PubMed] [Google Scholar]
- 95.Hill MD. Stroke and diabetes mellitus. Handb Clin Neurol. 2014;126:167–174. doi: 10.1016/B978-0-444-53480-4.00012-6. [DOI] [PubMed] [Google Scholar]
- 96.Johnston KC, Bruno A, Pauls Q, et al. Intensive vs standard treatment of hyperglycemia and functional outcome in patients with acute ischemic stroke: the SHINE randomized clinical trial. JAMA. 2019;322(4):326–335. doi: 10.1001/jama.2019.9346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lin H-B, Li F-X, Zhang J-Y, et al. Cerebral-cardiac syndrome and diabetes: cardiac damage after ischemic stroke in diabetic state. Front Immunol. 2021;12:737170. doi: 10.3389/fimmu.2021.737170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vogrig A, Gigli GL, Bnà C, Morassi M. Stroke in patients with COVID-19: clinical and neuroimaging characteristics. Neurosci Lett. 2021;743:135564. doi: 10.1016/j.neulet.2020.135564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Luo W, Liu X, Bao K, Huang C. Ischemic stroke associated with COVID-19: a systematic review and meta-analysis. J Neurol. 2022;269(4):1731–1740. doi: 10.1007/s00415-021-10837-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nannoni S, de Groot R, Bell S, Markus HS. Stroke in COVID-19: a systematic review and meta-analysis. Int J Stroke. 2021;16(2):137–149. doi: 10.1177/1747493020972922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bourne RRA, Jonas JB, Bron AM, et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe in 2015: magnitude, temporal trends and projections. Br J Ophthalmol. 2018;102(5):575–585. doi: 10.1136/bjophthalmol-2017-311258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kropp M, Golubnitschaja O, Mazurakova A, et al. Diabetic retinopathy as the leading cause of blindness and early predictor of cascading complications-risks and mitigation. EPMA J. 2023;14(1):21–42. doi: 10.1007/s13167-023-00314-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hu K, Jiang M, Zhou Q, et al. Association of diabetic retinopathy with stroke: a systematic review and meta-analysis. Front Neurol. 2021;12:626996. doi: 10.3389/fneur.2021.626996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gar C, Rottenkolber M, Prehn C, Adamski J, Seissler J, Lechner A. Serum and plasma amino acids as markers of prediabetes, insulin resistance, and incident diabetes. Crit Rev Clin Lab Sci. 2018;55(1):21–32. doi: 10.1080/10408363.2017.1414143. [DOI] [PubMed] [Google Scholar]
- 105.Nemet I, Li XS, Haghikia A, et al. Atlas of gut microbe-derived products from aromatic amino acids and risk of cardiovascular morbidity and mortality. Eur Heart J. 2023;44(32):3085–3096. doi: 10.1093/eurheartj/ehad333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.McGlone ER, Bloom SR. Bile acids and the metabolic syndrome. Ann Clin Biochem. 2019;56(3):326–337. doi: 10.1177/0004563218817798. [DOI] [PubMed] [Google Scholar]
- 107.Chávez-Talavera O, Tailleux A, Lefebvre P, Staels B. Bile acid control of metabolism and inflammation in obesity, type 2 diabetes, dyslipidemia, and nonalcoholic fatty liver disease. Gastroenterology. 2017;152(7):1679–1694.e3. doi: 10.1053/j.gastro.2017.01.055. [DOI] [PubMed] [Google Scholar]
- 108.Ferrell JM, Chiang JYL. Understanding bile acid signaling in diabetes: from pathophysiology to therapeutic targets. Diabetes Metab J. 2019;43(3):257–272. doi: 10.4093/dmj.2019.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhang W, Dong XY, Huang R. Gut microbiota in ischemic stroke: role of gut bacteria-derived metabolites. Transl Stroke Res. 2023;14(6):811–828. doi: 10.1007/s12975-022-01096-3. [DOI] [PubMed] [Google Scholar]
- 110.Chaurasia B, Tippetts TS, Mayoral Monibas R, et al. Targeting a ceramide double bond improves insulin resistance and hepatic steatosis. Science. 2019;365(6451):386–392. doi: 10.1126/science.aav3722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yaribeygi H, Bo S, Ruscica M, Sahebkar A. Ceramides and diabetes mellitus: an update on the potential molecular relationships. Diabet Med. 2020;37(1):11–19. doi: 10.1111/dme.13943. [DOI] [PubMed] [Google Scholar]
- 112.Mandal N, Grambergs R, Mondal K, Basu SK, Tahia F, Dagogo-Jack S. Role of ceramides in the pathogenesis of diabetes mellitus and its complications. J Diabetes Complicat. 2021;35(2):107734. doi: 10.1016/j.jdiacomp.2020.107734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Choi RH, Tatum SM, Symons JD, Summers SA, Holland WL. Ceramides and other sphingolipids as drivers of cardiovascular disease. Nat Rev Cardiol. 2021;18(10):701–711. doi: 10.1038/s41569-021-00536-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kulikowska E, Kierdaszuk B, Shugar D. Xanthine, xanthosine and its nucleotides: solution structures of neutral and ionic forms, and relevance to substrate properties in various enzyme systems and metabolic pathways. Acta Biochim Pol. 2004;51(2):493–531. doi: 10.18388/abp.2004_3587. [DOI] [PubMed] [Google Scholar]
- 115.Ramasubbu K, Devi RV. Impairment of insulin signaling pathway PI3K/Akt/mTOR and insulin resistance induced AGEs on diabetes mellitus and neurodegenerative diseases: a perspective review. Mol Cell Biochem. 2023;478(6):1307–1324. doi: 10.1007/s11010-022-04587-x. [DOI] [PubMed] [Google Scholar]
- 116.Zhao H, He Y. Lysophosphatidylcholine offsets the protective effects of bone marrow mesenchymal stem cells on inflammatory response and oxidative stress injury of retinal endothelial cells via TLR4/NF-κB signaling. J Immunol Res. 2021;2021:2389029. doi: 10.1155/2021/2389029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Canning P, Kenny B-A, Prise V, et al. Lipoprotein-associated phospholipase A2 (Lp-PLA2) as a therapeutic target to prevent retinal vasopermeability during diabetes. Proc Natl Acad Sci U S A. 2016;113(26):7213–7218. doi: 10.1073/pnas.1514213113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Yuan C, Shi L, Sun Z, et al. Regulatory T cell expansion promotes white matter repair after stroke. Neurobiol Dis. 2023;179:106063. doi: 10.1016/j.nbd.2023.106063. [DOI] [PubMed] [Google Scholar]
- 119.Alesi S, Ghelani D, Rassie K, Mousa A. Metabolomic biomarkers in gestational diabetes mellitus: a review of the evidence. Int J Mol Sci. 2021;22(11):5512. doi: 10.3390/ijms22115512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lee G, Choi S, Chang J, et al. Association of L-α glycerylphosphorylcholine with subsequent stroke risk after 10 years. JAMA Netw Open. 2021;4(11):e2136008. doi: 10.1001/jamanetworkopen.2021.36008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Purroy F, Ois A, Jove M, et al. Lipidomic signature of stroke recurrence after transient ischemic attack. Sci Rep. 2023;13(1):13706. doi: 10.1038/s41598-023-40838-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Callaghan BC, Feldman E, Liu J, et al. Triglycerides and amputation risk in patients with diabetes: ten-year follow-up in the DISTANCE study. Diabetes Care. 2011;34(3):635–640. doi: 10.2337/dc10-0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jasim OH, Mahmood MM, Ad’hiah AH. Significance of lipid profile parameters in predicting pre-diabetes. Arch Razi Inst. 2022;77(1):277–84. doi: 10.22092/ARI.2021.356465.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Vermeer SE, Den Heijer T, Koudstaal PJ, Oudkerk M, Hofman A, Breteler MMB. Incidence and risk factors of silent brain infarcts in the population-based rotterdam scan study. Stroke. 2003;34(2):392–396. doi: 10.1161/01.STR.0000052631.98405.15. [DOI] [PubMed] [Google Scholar]
- 125.Vermeer SE, Prins ND, Den Heijer T, Hofman A, Koudstaal PJ, Breteler MMB. Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med. 2003;348(13):1215–1222. doi: 10.1056/NEJMoa022066. [DOI] [PubMed] [Google Scholar]
- 126.Neuropathology Group Medical research council cognitive function and aging study. Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Neuropathology Group of the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS) Lancet. 2001;357(9251):169–75. doi: 10.1016/S0140-6736(00)03589-3. [DOI] [PubMed] [Google Scholar]
- 127.Jellinger KA, Mitter-Ferstl E. The impact of cerebrovascular lesions in Alzheimer disease–a comparative autopsy study. J Neurol. 2003;250(9):1050–1055. doi: 10.1007/s00415-003-0142-0. [DOI] [PubMed] [Google Scholar]
- 128.Bennett DA, Schneider JA, Bienias JL, Evans DA, Wilson RS. Mild cognitive impairment is related to Alzheimer disease pathology and cerebral infarctions. Neurology. 2005;64(5):834–841. doi: 10.1212/01.WNL.0000152982.47274.9E. [DOI] [PubMed] [Google Scholar]
- 129.Makin SDJ, Turpin S, Dennis MS, Wardlaw JM. Cognitive impairment after lacunar stroke: systematic review and meta-analysis of incidence, prevalence and comparison with other stroke subtypes. J Neurol Neurosurg Psychiatry. 2013;84(8):893–900. doi: 10.1136/jnnp-2012-303645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Matsui T, Nemoto M, Maruyama M, et al. Plasma homocysteine and risk of coexisting silent brain infarction in Alzheimer’s disease. Neurodegener Dis. 2005;2(6):299–304. doi: 10.1159/000092316. [DOI] [PubMed] [Google Scholar]
- 131.Bogousslavsky J, Regli F, Uske A. Thalamic infarcts: clinical syndromes, etiology, and prognosis. Neurology. 1988;38(6):837–837. doi: 10.1212/WNL.38.6.837. [DOI] [PubMed] [Google Scholar]
- 132.Tatemichi TK, Steinke W, Duncan C, et al. Paramedian thalamopeduncular infarction: Clinical syndromes and magnetic resonance imaging. Ann Neurol. 1992;32(2):162–171. doi: 10.1002/ana.410320207. [DOI] [PubMed] [Google Scholar]
- 133.Gold G, Kövari E, Herrmann FR, et al. Cognitive consequences of thalamic, basal ganglia, and deep white matter lacunes in brain aging and dementia. Stroke. 2005;36(6):1184–1188. doi: 10.1161/01.STR.0000166052.89772.b5. [DOI] [PubMed] [Google Scholar]
- 134.Fujikawa T, Yamawaki S, Touhouda Y. Silent cerebral infarctions in patients with late-onset mania. Stroke. 1995;26(6):946–949. doi: 10.1161/01.STR.26.6.946. [DOI] [PubMed] [Google Scholar]
- 135.Yamashita H, Fujikawa T, Yanai I, Morinobu S, Yamawaki S. Cognitive dysfunction in recovered depressive patients with silent cerebral infarction. Neuropsychobiology. 2002;45(1):12–18. doi: 10.1159/000048667. [DOI] [PubMed] [Google Scholar]
- 136.Hamada T, Murata T, Omori M, et al. Abnormal nocturnal blood pressure fall in senile-onset depression with subcortical silent cerebral infarction. Neuropsychobiology. 2003;47(4):187–191. doi: 10.1159/000071213. [DOI] [PubMed] [Google Scholar]
- 137.Antelmi E, Fabbri M, Cretella L, Guarino M, Stracciari A. Late onset bipolar disorder due to a lacunar state. Behav Neurol. 2014;2014:1–5. doi: 10.1155/2014/780742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Price TR, Manolio TA, Kronmal RA, et al. Silent brain infarction on magnetic resonance imaging and neurological abnormalities in community-dwelling older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Stroke. 1997;28(6):1158–64. doi: 10.1161/01.STR.28.6.1158. [DOI] [PubMed] [Google Scholar]
- 139.Kruit MC. Migraine as a Risk factor for subclinical brain lesions. JAMA. 2004;291(4):427. doi: 10.1001/jama.291.4.427. [DOI] [PubMed] [Google Scholar]
- 140.Tietjen GE, Maly EF. Migraine and ischemic stroke in women. A narrative review. Headache. 2020;60(5):843–863. doi: 10.1111/head.13796. [DOI] [PubMed] [Google Scholar]
- 141.Leung DYL, Tham CCY, Li FCH, Kwong YYY, Chi SCC, Lam DSC. Silent cerebral infarct and visual field progression in newly diagnosed normal-tension glaucoma: a cohort study. Ophthalmology. 2009;116(7):1250–1256. doi: 10.1016/j.ophtha.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 142.Leung DYL, Tham CC. Normal-tension glaucoma: current concepts and approaches-a review. Clin Experiment Ophthalmol. 2022;50(2):247–259. doi: 10.1111/ceo.14043. [DOI] [PubMed] [Google Scholar]
- 143.Konieczka K, Ritch R, Traverso CE, et al. Flammer syndrome. EPMA J. 2014;5(1):11. doi: 10.1186/1878-5085-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Golubnitschaja O. Flammer syndrome – from phenotype to associated pathologies, prediction, prevention and personalisation. Springer; 2019. [Google Scholar]
- 145.Golubnitschaja O, Yeghiazaryan K, Flammer J. Key molecular pathways affected by glaucoma pathology: is predictive diagnosis possible? EPMA J. 2010;1(2):237–244. doi: 10.1007/s13167-010-0031-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Golubnitschaja O. Feeling cold and other underestimated symptoms in breast cancer: anecdotes or individual profiles for advanced patient stratification? EPMA J. 2017;8(1):17–22. doi: 10.1007/s13167-017-0086-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Golubnitschaja O, Flammer J. Individualised patient profile: clinical utility of Flammer syndrome phenotype and general lessons for predictive, preventive and personalised medicine. EPMA J. 2018;9(1):15-20. [DOI] [PMC free article] [PubMed]
- 148.Bubnov R, Polivka J, Zubor P, Konieczka K, Golubnitschaja O. “Pre-metastatic niches” in breast cancer: are they created by or prior to the tumour onset? “Flammer Syndrome” relevance to address the question. EPMA J. 2017;8(2):141–157. doi: 10.1007/s13167-017-0092-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Evsevieva M, Sergeeva O, Mazurakova A, et al. Pre-pregnancy check-up of maternal vascular status and associated phenotype is crucial for the health of mother and offspring. EPMA J. 2022;13(3):351–366. doi: 10.1007/s13167-022-00294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Golubnitschaja-Labudova O, Liu R, Decker C, Zhu P, Haefliger IO, Flammer J. Altered gene expression in lymphocytes of patients with normal-tension glaucoma. Curr Eye Res. 2000;21(5):867–876. doi: 10.1076/ceyr.21.5.867.5534. [DOI] [PubMed] [Google Scholar]
- 151.Yeghiazaryan K, Flammer J, Golubnitschaja O. Predictive molecular profiling in blood of healthy vasospastic individuals: clue to targeted prevention as personalised medicine to effective costs. EPMA J. 2010;1(2):263–272. doi: 10.1007/s13167-010-0032-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Koklesova L, Mazurakova A, Samec M, et al. Mitochondrial health quality control: measurements and interpretation in the framework of predictive, preventive, and personalized medicine. EPMA J. 2022;13(2):177–193. doi: 10.1007/s13167-022-00281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Narayan SM, Wang PJ, Daubert JP. New concepts in sudden cardiac arrest to address an intractable epidemic: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73(1):70–88. doi: 10.1016/j.jacc.2018.09.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ha ACT, Doumouras BS, Wang CN, Tranmer J, Lee DS. Prediction of sudden cardiac arrest in the general population: review of traditional and emerging risk factors. Can J Cardiol. 2022;38(4):465–478. doi: 10.1016/j.cjca.2022.01.007. [DOI] [PubMed] [Google Scholar]
- 155.Kim YG, Han K-D, Roh S-Y, et al. Being Underweight Is Associated with increased risk of sudden cardiac death in people with diabetes mellitus. J Clin Med. 2023;12(3):1045. doi: 10.3390/jcm12031045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Chen H, Deng Y, Li S. Relation of body mass index categories with risk of sudden cardiac death. Int Heart J. 2019;60(3):624–630. doi: 10.1536/ihj.18-155. [DOI] [PubMed] [Google Scholar]
- 157.Dale CE, Fatemifar G, Palmer TM, et al. Causal Associations of adiposity and body fat distribution with coronary heart disease, stroke subtypes, and type 2 diabetes mellitus: a mendelian randomization analysis. Circulation. 2017;135(24):2373–2388. doi: 10.1161/CIRCULATIONAHA.116.026560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chiu Y-W, Su M-H, Lin Y-F, Chen C-Y, Chen T-T, Wang S-H. Causal influence of sleeping phenotypes on the risk of coronary artery disease and sudden cardiac arrest: a mendelian randomization analysis. Sleep Health. 2023;S2352–7218(23):00097–99. doi: 10.1016/j.sleh.2023.05.009. [DOI] [PubMed] [Google Scholar]
- 159.Modesto-Lowe V, Brooks D, Petry N. Methadone deaths: risk factors in pain and addicted populations. J Gen Intern Med. 2010;25(4):305–309. doi: 10.1007/s11606-009-1225-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Jacob L, Smith L, Koyanagi A, et al. Chronic low back pain and incident transient ischemic attack and stroke in general practices in Germany. Healthcare (Basel) 2023;11(10):1499. doi: 10.3390/healthcare11101499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Wen L-Y, Ni H, Li K-S, et al. Asthma and Risk of stroke: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2016;25(3):497–503. doi: 10.1016/j.jstrokecerebrovasdis.2015.11.030. [DOI] [PubMed] [Google Scholar]
- 162.Finocchiaro G, Radaelli D, D’Errico S, et al. Sudden cardiac death among adolescents in the United Kingdom. J Am Coll Cardiol. 2023;81(11):1007–1017. doi: 10.1016/j.jacc.2023.01.041. [DOI] [PubMed] [Google Scholar]
- 163.Gullach AJ, Risgaard B, Lynge TH, et al. Sudden death in young persons with uncontrolled asthma- a nationwide cohort study in Denmark. BMC Pulm Med. 2015;15:35. doi: 10.1186/s12890-015-0033-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hummel EM, Hessas E, Müller S, Beiter T, Fisch M, Eibl A, Wolf OT, Giebel B, Platen P, Kumsta R, Moser DA. Cell-free DNA release under psychosocial and physical stress conditions. Transl Psychiatry. 2018;8(1):236. doi: 10.1038/s41398-018-0264-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.3P Medicon your risk reducer. Available from: https://www.3pmedicon.com/en/scientific-evidence/compromised-mitochondrial-health. Accessed 22 Jan 2024.
- 166.Crigna AT, Link B, Samec M, Giordano FA, Kubatka P, Golubnitschaja O. Endothelin-1 axes in the framework of predictive, preventive and personalised (3P) medicine. EPMA J. 2021;12(3):265–305. doi: 10.1007/s13167-021-00248-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bushnell CD, Goldstein LB. Risk of ischemic stroke with tamoxifen treatment for breast cancer: a meta-analysis. Neurology. 2004;63(7):1230–1233. doi: 10.1212/01.WNL.0000140491.54664.50. [DOI] [PubMed] [Google Scholar]
- 168.D’Onofrio N, Martino E, Mele L, et al. Colorectal cancer apoptosis induced by dietary δ-valerobetaine involves PINK1/Parkin dependent-mitophagy and SIRT3. Int J Mol Sci. 2021;22(15):8117. doi: 10.3390/ijms22158117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Liu J-X, Li J-H, Du C-H, Yan Y. Metabonomic study of biochemical changes in serum of PCPA-induced insomnia rats after treatment with Suanzaoren Decoction. Zhongguo Zhong Yao Za Zhi. 2022;47(6):1632–1641. doi: 10.19540/j.cnki.cjcmm.20211204.701. [DOI] [PubMed] [Google Scholar]
- 170.He J, Zheng W, Lu M, Yang X, Xue Y, Yao W. A controlled heat stress during late gestation affects thermoregulation, productive performance, and metabolite profiles of primiparous sow. J Therm Biol. 2019;81:33–40. doi: 10.1016/j.jtherbio.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 171.Ahmed H, Leyrolle Q, Koistinen V, et al. Microbiota-derived metabolites as drivers of gut-brain communication. Gut Microbes. 2022;14(1):2102878. doi: 10.1080/19490976.2022.2102878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Pochakom A, Mu C, Rho JM, Tompkins TA, Mayengbam S, Shearer J. Selective probiotic treatment positively modulates the microbiota-gut-brain axis in the BTBR mouse model of autism. Brain Sci. 2022;12(6):781. doi: 10.3390/brainsci12060781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Gaggini M, Ndreu R, Michelucci E, Rocchiccioli S, Vassalle C. Ceramides as mediators of oxidative stress and inflammation in cardiometabolic disease. Int J Mol Sci. 2022;23(5):2719. doi: 10.3390/ijms23052719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Roszczyc-Owsiejczuk K, Zabielski P. Sphingolipids as a culprit of mitochondrial dysfunction in insulin resistance and type 2 diabetes. Front Endocrinol (Lausanne) 2021;12:635175. doi: 10.3389/fendo.2021.635175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Liu H, Wang X, Chen L, et al. Microglia modulate stable wakefulness via the thalamic reticular nucleus in mice. Nat Commun. 2021;12(1):4646. doi: 10.1038/s41467-021-24915-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Habibi J, DeMarco VG, Hulse JL, et al. Inhibition of sphingomyelinase attenuates diet - Induced increases in aortic stiffness. J Mol Cell Cardiol. 2022;167:32–39. doi: 10.1016/j.yjmcc.2022.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Fan K-Q, Li Y-Y, Wang H-L, et al. Stress-induced metabolic disorder in peripheral CD4+ T cells leads to anxiety-like behavior. Cell. 2019;179(4):864–879.e19. doi: 10.1016/j.cell.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 178.Dumor K, Shoemaker-Moyle M, Nistala R, Whaley-Connell A. Arterial stiffness in hypertension: an update. Curr Hypertens Rep. 2018;20(8):72. doi: 10.1007/s11906-018-0867-x. [DOI] [PubMed] [Google Scholar]
- 179.Golubnitschaja O. What is the routine mitochondrial health check-up good for? A holistic approach in the framework of 3P medicine. In: Podbielska H, Kapalla M, editors. Predictive, preventive, and personalised medicine: from bench to bedside. Switzerland: Springer International Publishing; 2023. 10.1007/978-3-031-34884-6_3.
- 180.Xu K, Gao X, Xia G, et al. Rapid gut dysbiosis induced by stroke exacerbates brain infarction in turn. Gut 2021:gutjnl-2020-323263. [DOI] [PubMed]
- 181.Spychala MS, Venna VR, Jandzinski M, et al. Age-related changes in the gut microbiota influence systemic inflammation and stroke outcome. Ann Neurol. 2018;84(1):23–36. doi: 10.1002/ana.25250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Hill C, Guarner F, Reid G, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506–14. doi: 10.1038/nrgastro.2014.66. [DOI] [PubMed] [Google Scholar]
- 183.Wu H, Chiou J. Potential benefits of probiotics and prebiotics for coronary heart disease and stroke. Nutrients. 2021;13(8):2878. doi: 10.3390/nu13082878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Fröhlich H, Balling R, Beerenwinkel N, et al. From hype to reality: data science enabling personalized medicine. BMC Med. 2018;16(1):150. doi: 10.1186/s12916-018-1122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Linden T, De Jong J, Lu C, Kiri V, Haeffs K, Fröhlich H. An explainable multimodal neural network architecture for predicting epilepsy comorbidities based on administrative claims data. Front Artif Intell. 2021;4:610197. doi: 10.3389/frai.2021.610197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Jung S, Song M-K, Lee E, et al. Predicting ischemic stroke in patients with atrial fibrillation using machine learning. Front Biosci (Landmark Ed) 2022;27(3):80. doi: 10.31083/j.fbl2703080. [DOI] [PubMed] [Google Scholar]
- 187.Fröhlich H, Bontridder N, Petrovska-Delacréta D, et al. Leveraging the potential of digital technology for better individualized treatment of Parkinson’s disease. Front Neurol. 2022;13:788427. doi: 10.3389/fneur.2022.788427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Warnat-Herresthal S, Schultze H, Shastry KL, et al. Swarm Learning for decentralized and confidential clinical machine learning. Nature. 2021;594(7862):265–270. doi: 10.1038/s41586-021-03583-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Advances in predictive, preventive and personalised medicine. Book series, Switzerland, Springer. Available from: https://link.springer.com/bookseries/10051. Accessed 22 Jan 2024.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.