Abstract
Background:
Natriuretic peptides (NPs) are hormones with a range of key functions vital for cardiometabolic health. However, the reference ranges of NPs and the prevalence of NP deficiency in the healthy US population remains poorly defined.
Objective:
To establish the reference range for NT-proBNP (N-terminal proB-type natriuretic peptide) values, and assess the prevalence of NP deficiency in a nationally representative healthy US population.
Methods:
Healthy participants with NT-proBNP measurements from the 1999–2004 National Health and Nutrition Examination Survey were included. Weighted multivariable-adjusted linear regression models were used to assess the adjusted percentage difference of NT-proBNP concentrations by sex and race and ethnicity. NP deficiency was defined as concentrations below the 2.5th percentile in the study cohort.
Result:
Among 18,145 individuals (median age: 33.9 years [IQR: 17.1, 49.0 years], 49.8% males, and 68.5% non-Hispanic White individuals), females had similar NT-proBNP concentrations in the 1–10 years group (4.2% [95% CI: 3.3% to12.2%]), and highest differences in the 20–30 years group (150.5% [95% CI: 123.5%–180.8%]) compared with males in their respective age groups. Compared with non-Hispanic White individuals, non-Hispanic Black individuals had lower NT-proBNP concentrations in the 1- to 10-year group (19.6% [95% CI: 10.7%–27.6%]) and these differences were most pronounced in the 30–40 years group (40.2% [95% CI: 33.7%–46.0%]). An estimated 9.1 million United States individuals have NP deficiency. NP deficiency was associated with a higher risk of cardiometabolic diseases such as hypertension, dyslipidemia, obesity, and insulin resistance.
Conclusion:
This study establishes the normative NP concentrations across the lifespan of a healthy US population.
Keywords: N-Terminal Pro-B-Type Natriuretic Peptide, NHANES, Sex, Race and Ethnicity
Introduction
Ever since the discovery of natriuretic peptides (NPs), their clinical significance has been primarily focused on diagnosing and prognosticating heart failure (1). However, NPs have a range of physiological functions including natriuresis, vasodilation, lipolysis, and improved glucose utilization (2,3). The concentrations of these cardiometabolic hormones have been shown to vary by age, sex, and race and ethnicity (4–6). Considering the cardiometabolic functions regulated by NPs and the variation of NP concentrations with age, sex, and race and ethnicity, it is important to characterize the reference range of NPs accounting for these factors. Previous efforts characterizing the normative concentrations of NPs were limited in accounting for these determinants simply due to the lack of NP measurements in a racially diverse healthy population across the spectrum of age (7–9). Although NPs are widely recognized as hormones with beneficial cardiometabolic effects, unlike other hormones, normative data from a nationally representative cohort are lacking.
Given the cardiometabolic functions regulated by NPs, it could be postulated that NP deficiency would impair these functions leading to an increased risk of cardiometabolic diseases such as hypertension, insulin resistance, and obesity (10). As NP concentrations are known to vary by sex and race and ethnicity (4–6), variation in the circulating NP concentrations in these subgroups may provide insights into the sex and race and ethnicity-based disparities in cardiovascular disease (11). Therefore, there is an unmet need to characterize the normative concentrations of NPs across the spectrum of age accounting for sex and race and ethnicity and establish a threshold for NP deficiency.
This National Health and Nutrition Examination Survey (NHANES) based study characterized the normative NP concentrations across the lifespan in the overall population and stratified by sex and race and ethnicity, defined the threshold for NP deficiency, and assessed the association of NP deficiency with the prevalence of cardiometabolic disease in a nationally representative US cohort of healthy individuals.
Methods
Data Source
The NHANES cycles from 1999 to 2004 were combined for this study. NHANES is a nationally representative cross-sectional study conducted biennially by the National Center for Health Statistics (NCHS) and the Center for Disease Control and Prevention (CDC) (12). The National Health and Nutrition Examination Survey (NHANES) aims to examine the health status of a reference cohort representative of the non-institutionalized population of the United States. This reference cohort is selected using a multistage probability sampling design (12–17). All selected participants undergo a home interview during which data is collected on demographics, medical conditions such as diabetes mellitus and hypertension, and medication use (12). A clinical examination at a mobile examination center was conducted during which anthropometric measurements, clinical examination, and blood sampling for laboratory testing were done (12). Participants provided written informed consent before the home interview and physical examination (12). The University of Alabama at Birmingham institutional review board provided ethical oversight for this study.
Study Cohort
Participants with NT-proBNP measurements from 3 consecutive cycles (1999–2000 to 2003–2004) were included in this study. Participants with a history of cardiovascular disease (stroke, heart failure, coronary heart disease, angina, and “heart attack”), heart failure as defined by age-stratified NT-proBNP concentrations (≥450 pg/mL in adults <50 years old, ≥900 pg/mL in adults 50–75 years old, and ≥1,800 pg/mL in adults >75 years old) (1), history of renal disease, morbid obesity (BMI ≥40 kg/m2), and pregnant females were excluded. Self-identified race and ethnicity (non-Hispanic White, non-Hispanic Black, Mexican American, and others) and sex were used in this analysis.
Study Measures
Stored serum samples were used to measure NT-proBNP concentrations on the Roche Cobas e601 analyzer between 2018–2020. The lower limit of detection of the assay was 5 pg/mL [Coefficients of variation (CV) were 3.1% (low, 46 pg/mL) and 2.7% (high, 32,805 pg/mL)].
NP deficiency was defined individually in each sex and race group as the NT-proBNP concentrations below the weighted 2.5th percentile. Furthermore, NP deficiency using the sex and race-specific 5th and 10th percentiles of NT-proBNP concentrations was also described.
Cardiometabolic Diseases
Hypertension was defined as a systolic blood pressure ≥130 mmHg or a diastolic blood pressure ≥80 mmHg or the current use of anti-hypertensive medications (18).
Insulin resistance was assessed using the homeostatic model assessment for insulin resistance (HOMA-IR) using the following formula:
Insulin resistance was defined as a HOMA-IR value of ≥2.5 (19).
Hyperlipidemia was defined as a serum total cholesterol value ≥240 mg/dL (19,20). Serum low-density lipoprotein values ≥160 mg/dL were considered as raised (20). A serum triglyceride level ≥200 mg/dL was considered elevated (20).
Obesity was defined as body mass index (BMI) ≥30 kg/m2 (19).
Statistical Analysis
SAS 9.4 (Cary, NC) was used to perform statistical analysis. Based on analytical recommendations of the NCHS, SURVEY procedures in SAS were used to account for the complex multistage selection design of the NHANES. The cardiac biomarker subsample weights were used for this study. Adjusted weights, accounting for combining 3 NHANES cycles, were used for all analyses (21). SURVEYMEANS procedures were used to estimate the 2.5th, 5th, 25th, 50th, 75th, 95th, and 97.5th centile NT-proBNP values for each 10-year age group in the overall population and stratified by sex and race. To account for the relatively higher NT-proBNP concentrations and rapid changes in concentrations with age in childhood, the centiles of NT-proBNP were estimated per year of age without applying any NT-proBNP based exclusion criteria in the 1–18 year age group. Generalized Additive Models for Location, Scale, and Shape (GAMLSS), accounting for the skewness of distribution, were used to fit the quantiles of NT-proBNP according to age in the overall population and stratified by sex and race and ethnicity (22). Multivariable-adjusted linear regression models were used to assess the clinical correlates of NT-proBNP in the overall population and stratified by sex by regressing log-transformed NT-proBNP concentrations on age, sex, race and ethnicity, BMI, systolic blood pressure, and diastolic blood pressure. To allow comparison of variables, continuous variables were standardized. Similar models were run in the 1–10 years (maximum value before dropping to minimum value), 20–30 years (minimum lifetime value), and ≥70 years (maximum lifetime value) age groups to assess the percentage difference of NT-proBNP by sex and race and ethnicity. The SURVEYLOGISTIC procedure, adjusted for age, sex, race, and BMI, was used to determine the association of NT-proBNP deficiency with cardiometabolic diseases. The two-sided p-value of <0.05 was considered statistically significant.
Results
NT-proBNP data was available for 21,206 participants. After excluding 280 individuals with heart failure based on NT-proBNP concentrations, 1,256 participants with a self-reported history of cardiovascular disease, 192 participants with a self-reported history of kidney disease, 763 pregnant females, and 570 morbidly obese individuals, the study sample consisted of 18,145 individuals representing 230.4 million US individuals (Figure 1). The median age was 33.9 (17.1, 49.0) years, 49.8% were males, and 68.5% were non-Hispanic White individuals (Table 1). In the overall population, median NT-proBNP concentrations were 41.0 (20.7, 78.6) pg/mL with females [55.4 vs. 28.9 pg/mL] and non-Hispanic White individuals [45.5 vs. 30.3 pg/mL in non-Hispanic Black and 32.4 pg/mL in Mexican American individuals] having higher concentrations in their respective subgroups.
Figure 1: Study Population Flowchart.
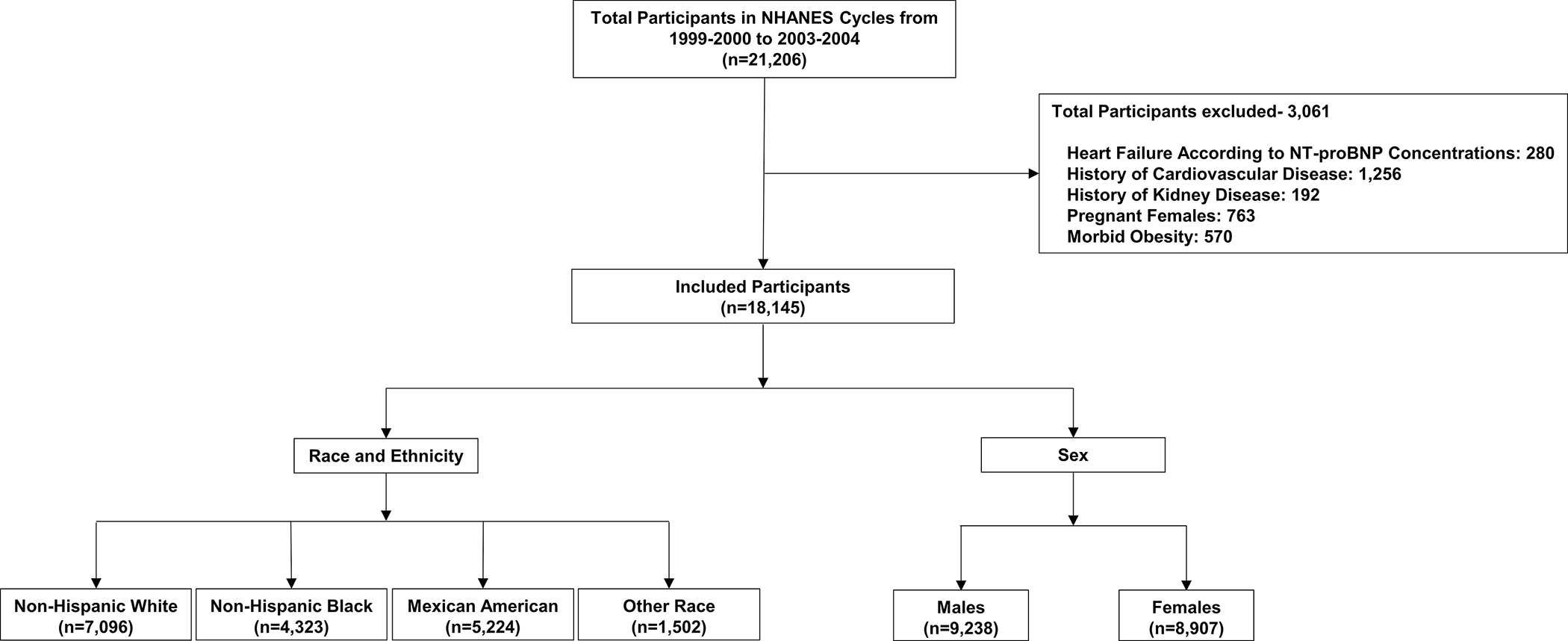
Table 1:
Baseline Characteristics and Prevalence of Cardiometabolic Diseases in the Overall Population and Stratified by Sex
| Parameter | Overall [n=18,145 (230,354,341)*] | Male [n= 9,238 (114,762,636)*] | Female [n=8,907 (115,591,704)*] |
|---|---|---|---|
| Median Age (Years) | 33.9 (17.1, 49.0) | 32.5 (16.7, 47.3) | 35.2 (17.5, 50.7) |
| Race and Ethnicity | |||
| Mexican American | 8.9 (6.7–11.0) | 11.2 (7.5–12.0) | 8.1 (8.5–13.6) |
| Non-Hispanic White | 68.5 (64.9–71.9) | 67.7 (64.3–71.1) | 69.1 (65.4–72.9) |
| Non-Hispanic Black | 11.5 (9.4–13.7) | 11.4 (9.3–13.4) | 11.7 (9.4–14.0) |
| Education Level | |||
| High School or Less | 44.7 (42.5–46.9) | 45.1 (42.5–47.7) | 44.4 (42.0–46.7) |
| Some College | 30.0 (28.4–31.5) | 28.2 (26.6–29.7) | 31.7 (29.7–33.8) |
| College Graduate | 25.3 (23.2–28.4) | 26.8 (24.0–29.5) | 23.9 (21.5–26.3) |
| Family Poverty Income Ratio | |||
| >=3.50 | 39.3 (36.4–42.1) | 41.1 (38.1–44.0) | 37.5 (34.6–40.4) |
| 1.30–3.49 | 36.4 (34.6–38.2) | 36.2 (34.2–38.2) | 36.6 (34.5–38.7) |
| <1.30 | 24.3 (22.2–26.5) | 22.7 (20.7–24.8) | 25.9 (23.5–28.3) |
| Prevalence of Cardiometabolic Diseases | |||
| Obesity | 22.1 ( 21.0–23.3) | 21.3 (20.0–22.6) | 23.0 ( 21.3–24.6) |
| Hypertriglyceridemia | 29.5 ( 28.2–30.7) | 34.7 ( 33.1–36.3) | 24.3 ( 22.8–25.7) |
| Hypertension | 36.3 ( 34.8–37.8) | 39.3 ( 37.6–41.0) | 33.3 ( 31.6–35.0) |
| Insulin Resistance | 38.6 (36.5– 40.7) | 42.1 (39.6–44.6) | 35.1 (32.6–37.5) |
| Elevated Low-Density Lipoprotein Cholesterol Levels | 16.5 (14.9–18.1) | 17.5 (15.7–19.4) | 15.4 (13.3–17.5) |
| Hypercholesterolemia | 19.0 (17.9–20.1) | 18.9 (17.6–20.3) | 19.1 (17.6–20.6) |
Values in the paratheses indicate the weighted sample size
Continuous and categorical variables are presented as median (interquartile range) and percentage (95% confidence interval), respectively.
Age-Specific NT-proBNP Concentrations in the Overall Population
NT-proBNP concentrations had a U-shaped distribution with age with higher concentrations in the 1–10 years age group [57.3 (95%CI: 53.5–61.0) pg/mL] followed by a decline to a minimum concentration in the 20–30 years age group [26.6 (95%CI: 24.6–28.5) pg/mL] and a consistent increase in concentrations with age thereafter reaching a maximum concentration in the ≥70 years age group [163.9 (95%CI: 150.1–177.7) pg/mL] (Table 2, Figure 2). NT-proBNP concentrations per year of age in the 1–10 years age group have been depicted in Table 3.
Table 2:
Age-Specific Centiles of N-Terminal Pro B-Type Natriuretic Peptide in the Overall Population and Stratified by Sex
| 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Overall (n=18,145) | Males (n=9,238) | Females (n=8,907) | ||||||||||||||||||
| 1–10 Years (n=2,384) | 10.2 | 13.9 | 33.2 | 57.3 | 95.3 | 197.2 | 247.4 | 9.0 | 13.0 | 32.1 | 55.4 | 94.6 | 197.9 | 269.5 | 12.1 | 15.9 | 34.3 | 59.7 | 96.5 | 191.5 | 220.0 |
| 10–20 Years (n=6,291) | <5 | 5.9 | 16.2 | 30.9 | 52.7 | 114.9 | 144.5 | <5 | <5 | 12.9 | 25.9 | 45.8 | 107 | 139.4 | 6.8 | 9.7 | 20.9 | 36.2 | 58.7 | 120.4 | 145.5 |
| 20–30 Years (n=1,728) | <5 | <5 | 13.4 | 26.6 | 49.4 | 109.4 | 146.7 | <5 | <5 | 9.2 | 17.2 | 30.0 | 64.0 | 82.0 | 8.0 | 10.7 | 24.1 | 44.0 | 72.1 | 146.6 | 171.9 |
| 30–40 Years (n=1,693) | <5 | 6.2 | 16.3 | 31.3 | 59.2 | 120.6 | 157.3 | <5 | <5 | 11.9 | 21.1 | 35.5 | 77.2 | 101.3 | 8.0 | 12.4 | 28.2 | 48.5 | 80.3 | 153.4 | 184.6 |
| 40–50 Years (n=1,796) | <5 | 5.9 | 19.1 | 35.7 | 65.8 | 147.5 | 177.8 | <5 | <5 | 12.5 | 23.4 | 39.6 | 89.5 | 110.8 | 8.9 | 13.8 | 30.6 | 53.8 | 91.5 | 173.3 | 211.0 |
| 50–60 Years (n=1,277) | 6.8 | 11.3 | 27.9 | 49.1 | 83.5 | 220.7 | 295.8 | 5.1 | 8.7 | 20.7 | 37 | 59.5 | 156.1 | 229.8 | 11.0 | 17.0 | 41.9 | 66.1 | 109.0 | 265.1 | 340.0 |
| 60–70 Years (n=1,418) | 10.9 | 16.2 | 42.9 | 77.2 | 141.5 | 346.4 | 492.8 | 9.6 | 11.7 | 28.9 | 55.6 | 98.9 | 304.6 | 410.2 | 18.4 | 24.1 | 57.5 | 103.1 | 176.0 | 409.8 | 578.0 |
| ≥70 Years (n=1,558) | 29.8 | 41.4 | 91.8 | 163.9 | 309.8 | 892.4 | 1,112.7 | 24.3 | 29.9 | 77.4 | 147.7 | 275.1 | 872.2 | 1106.9 | 39.5 | 48.6 | 98.0 | 176.6 | 329.4 | 896.3 | 1,111.5 |
The values depicted are weighted estimates of the 2.5th, 5th, 25th, 50th, 75th, 95th, and 97.5th centiles of N-terminal proB-type natriuretic peptide in the overall population and stratified by sex. The cohort was further stratified by age into 10-year bins. The values in the parenthesis indicate the unweighted sample size for each group.
Figure 2: Age-Specific Centiles of N-Terminal Pro-B-Type Natriuretic Peptide in the Overall Population.
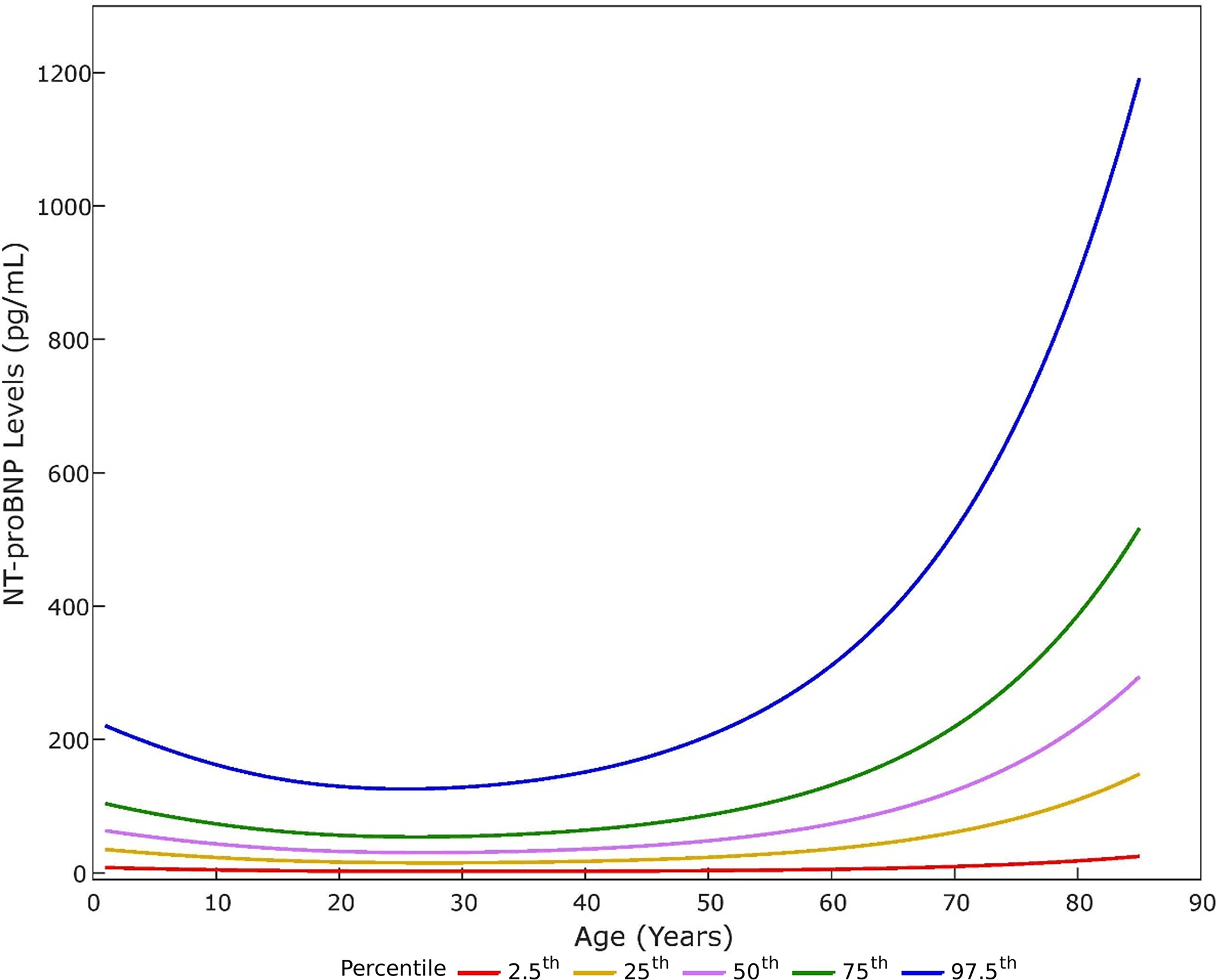
The 2.5th, 25th, 50th, 75th, and 97.5th centiles of N-terminal pro-B-type natriuretic peptide (NT-proBNP) according to age in the overall population have been depicted. The 2.5th, 25th, 50th, 75th, and 97.5th centiles of NT-proBNP have been depicted in red, yellow, purple, green, and blue, respectively.
Table 3:
Age-Specific Centiles of N-Terminal Pro B-Type Natriuretic Peptide in the Pediatric Population Stratified by Sex
| 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Overall (n=2,736) | Males (n=1,400) | Females (n=1,336) | ||||||||||||||||||
| 1 Year (n=247) | 16.8 | 26.3 | 54.7 | 88.5 | 143 | 266.8 | 287.9 | 20.0 | 26.8 | 48.4 | 75.2 | 141.2 | 248 | 271.5 | 14.5 | 24.8 | 58.6 | 94.3 | 145.3 | 279.9 | 336.8 |
| 2 Years (n=260) | 13.5 | 16.6 | 34.5 | 60.7 | 91.2 | 242.9 | 270.6 | 12.6 | 14.3 | 34.5 | 60.7 | 108.3 | 253.6 | 324.1 | 12.3 | 18.6 | 35.2 | 59.4 | 81.2 | 147.1 | 245.0 |
| 3 Years (n=149) | 13.7 | 15.5 | 37.3 | 65.8 | 100.5 | 163.9 | 248.4 | 12.7 | 15.0 | 31.9 | 54 | 93 | 182.4 | 240.3 | 12.8 | 17.5 | 51.5 | 81.1 | 104.4 | 143.7 | 227.4 |
| 4 Years (n=155) | 11.2 | 16.0 | 35.8 | 63.4 | 108.1 | 218.4 | 247.3 | 10.2 | 12.4 | 36.2 | 63.8 | 107.8 | 239.3 | 274.2 | 12.4 | 19.3 | 34.3 | 61.2 | 107.5 | 215.9 | 220.7 |
| 5 Years (n=141) | 9.4 | 13.2 | 31.5 | 49.5 | 87.4 | 205.7 | 238.7 | 6.8 | 9.9 | 26.3 | 49.2 | 86.9 | 145.3 | 196.9 | 10.6 | 18.7 | 33.9 | 49.3 | 89.9 | 211.6 | 235.7 |
| 6 Years (n=340) | 10.8 | 15.3 | 36.9 | 56.7 | 91.8 | 179.2 | 227.3 | 8.7 | 14.4 | 36.5 | 55.2 | 86.7 | 197.3 | 309.5 | 12.9 | 16 | 36.6 | 59.8 | 106.4 | 173.3 | 177.4 |
| 7 Years (n=369) | 6.7 | 12.1 | 34.8 | 57.3 | 103.4 | 151.8 | 199.9 | 6.0 | 11.9 | 33.7 | 55.5 | 94.8 | 154.4 | 201 | 7.2 | 12 | 34.8 | 58.2 | 108.9 | 150.5 | 198.3 |
| 8 Years (n=363) | 8.1 | 12.9 | 25.4 | 48.0 | 86.2 | 154.4 | 175.9 | 5.0 | 12.7 | 28.7 | 49.8 | 85.7 | 161.5 | 175.3 | 9.9 | 12.5 | 24.6 | 43.8 | 86.3 | 154.3 | 173.4 |
| 9 Years (n=360) | 8.9 | 10.9 | 26.7 | 45.2 | 70.8 | 153.7 | 164 | 8.9 | 9.3 | 21.7 | 41.3 | 69.9 | 157 | 164.3 | 8.7 | 13.4 | 28.7 | 46.9 | 70.8 | 123.4 | 137.9 |
| 10 Years (n=352) | 7.4 | 11.1 | 25.0 | 43.1 | 77.9 | 153.8 | 173.4 | <5 | 8.8 | 24.4 | 38.9 | 77.0 | 150.2 | 158.7 | 12.4 | 16.1 | 26.7 | 48.6 | 78.1 | 160.8 | 178.5 |
The values depicted are weighted estimates of the 2.5th, 5th, 25th, 50th, 75th, 95th, and 97.5th centiles of N-terminal proB-type natriuretic peptide in the overall population and stratified by sex among children aged 10 years and below. The cohort was further stratified by age into 1-year bins. The values in the parenthesis indicate the unweighted sample size for each group.
Age-Specific NT-proBNP Concentrations Stratified Sex
NT-proBNP concentrations were similar by sex in the 1–10 years group [Males: 55.4 (95%CI: 51.0–59.9), Females: 59.7 (95%CI: 54.3–65.1) pg/mL]. Concentrations were higher in females compared with males beginning from the 10–20 years age group [36.2 (95%CI: 34.0–38.5) vs. 25.9 (95%CI: 24.1–27.8)] and persisted across the age range (Table 2, Figure 3). The lowest lifetime median NT-proBNP concentration was recorded in the 20–30 years age group for males [17.2 (95%CI: 15.2–19.3) pg/mL] and 10–20 years age group for females [36.2 (95%CI: 34.0–38.5) pg/mL] (Table 2). NT-proBNP concentrations reached their peak in the ≥70-year age group in males [147.7 (95%CI: 130.9–164.5) pg/mL] and females [176.6 (95%CI: 158.2–195.0) pg/mL].
Figure 3: Age-Specific Centiles of NT-proBNP Concentrations Stratified by Sex.
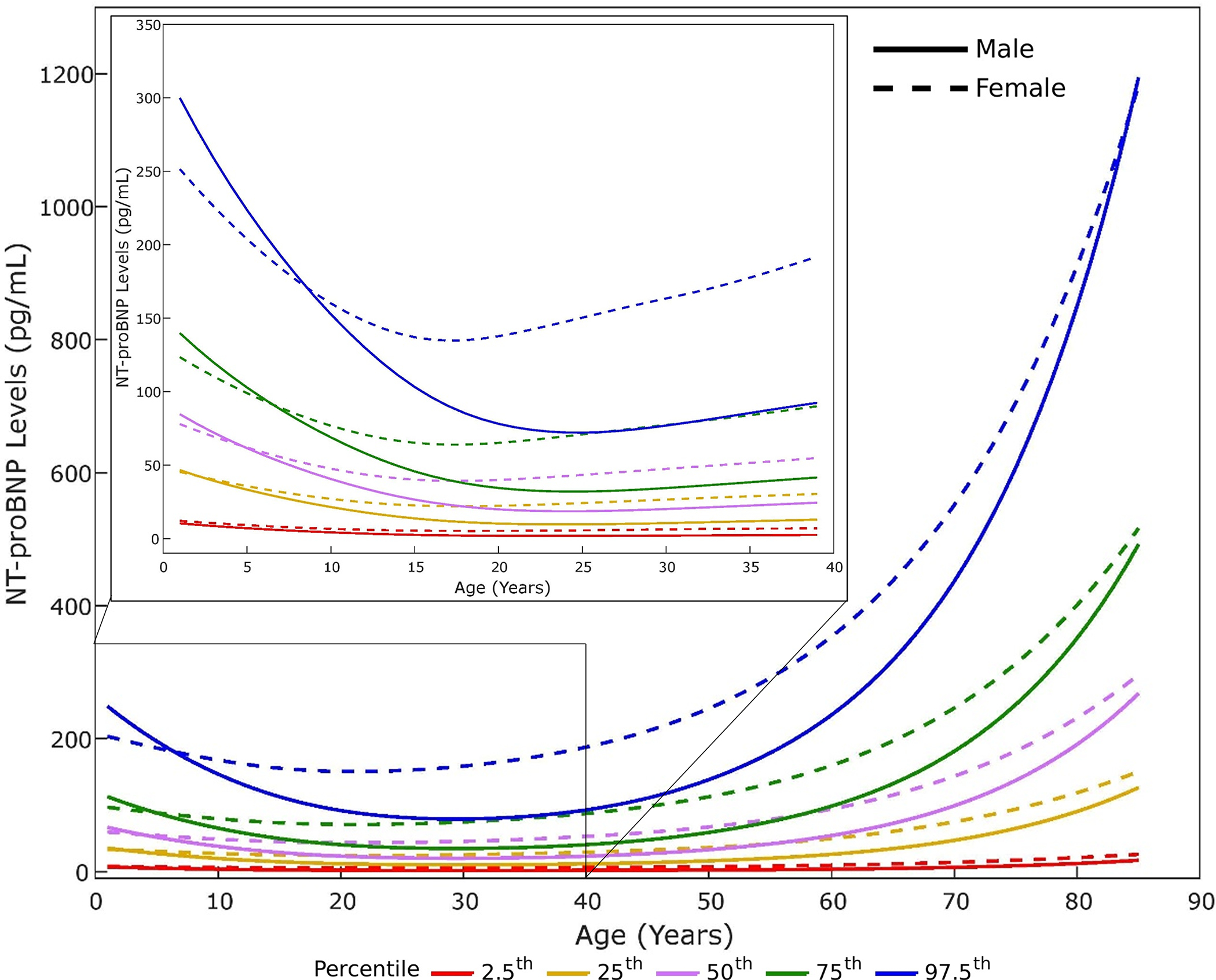
The age-specific 2.5th, 25th, 50th, 75th, and 97.5th centiles of N-terminal pro-B-type natriuretic peptide (NT-proBNP) according to by sex have been depicted. Males have been depicted as solid lines and females have been depicted as dashed lines. The 2.5th, 25th, 50th, 75th, and 97.5th centiles of NT-proBNP have been depicted in red, yellow, purple, green, and blue, respectively. The inset in the figure shows the 2.5th, 25th, 50th, 75th, and 97.5th centiles of NT-proBNP on a magnified y-axis in individuals below 40 years of age.
Age-Specific NT-proBNP Concentrations Stratified Race and Ethnicity
NT-proBNP concentrations were the highest in non-Hispanic White individuals [45.5 (95%CI: 43.9–47.1) pg/mL] followed Mexican American individuals [32.4 (95%CI: 30.0–34.8) pg/mL] and non-Hispanic Black individuals [30.3 (95%CI: 28.5–32.1) pg/mL]. Racial differences in NT-proBNP concentrations were present in childhood and persisted across the age range. Mexican American and Non-Hispanic Black individuals had lower concentrations of NT-proBNP compared with non-Hispanic White individuals across the age range (Table 4, Figure 4). Sex differences in NT-proBNP concentrations persisted across racial groups (Table 4).
Table 4:
Age-Specific Centiles of N-Terminal Pro-B-Type Natriuretic Peptide Stratified by Sex and Race and Ethnicity
| 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | 2.5th Centile | 5th Centile | 25th Centile | 50th Centile | 75th Centile | 95th Centile | 97.5th Centile | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White | |||||||||||||||||||||
| Overall (n=7,096) | Male (n=3,561) | Female (n=3,535) | |||||||||||||||||||
| 1–10 Years (n=622) | 13.1 | 15.6 | 34.9 | 59.0 | 98.9 | 202.7 | 253.5 | 13.0 | 15.0 | 34.5 | 56.6 | 99.0 | 208.1 | 270.9 | 13.1 | 16.5 | 35.5 | 62.5 | 98.8 | 197.5 | 216.8 |
| 10–20 Years (n=1,677) | <5 | 6.6 | 17.1 | 32.6 | 54.4 | 116.0 | 141.7 | <5 | 5.0 | 13.2 | 26.4 | 45.6 | 105.0 | 136.1 | 8.0 | 10.5 | 23.7 | 39.7 | 61.6 | 122.0 | 145.4 |
| 20–30 Years (n=750) | <5 | <5 | 15.9 | 29.7 | 56.8 | 122.3 | 154 | <5 | <5 | 10.2 | 20.2 | 32.9 | 71.1 | 91.6 | 10.1 | 13.5 | 28.6 | 51.2 | 78.9 | 153.6 | 217.8 |
| 30–40 Years (n=806) | 5.6 | 7.4 | 19.7 | 37.0 | 66.0 | 129.5 | 160.6 | <5 | 6.0 | 13.1 | 23.6 | 39.4 | 81.6 | 105.8 | 13.3 | 16.7 | 31.8 | 54.6 | 86.6 | 157.3 | 188.0 |
| 40–50 Years (n=817) | <5 | 6.6 | 20.5 | 36.8 | 68.1 | 151.4 | 180.4 | <5 | <5 | 13.5 | 25.0 | 41.7 | 94.4 | 111.8 | 12.4 | 15.6 | 33.3 | 58.3 | 93.9 | 179.1 | 214.3 |
| 50–60 Years (n=736) | 9.1 | 12.1 | 30.1 | 51.8 | 83.5 | 222.7 | 297.8 | 6.9 | 9.7 | 22.3 | 38.6 | 59.7 | 156.1 | 224.0 | 12.4 | 22.3 | 44.6 | 66.6 | 111.1 | 268.0 | 366.1 |
| 60–70 Years (n=667) | 11.7 | 17.5 | 46.5 | 83.2 | 150.1 | 346.5 | 468.9 | 9.7 | 13.9 | 30.6 | 57.8 | 102.2 | 305.9 | 381.1 | 21.7 | 30.5 | 63.3 | 110.6 | 183.7 | 408.8 | 533.8 |
| ≥70 Years (n=1,021) | 36.7 | 44.1 | 97.3 | 170.9 | 321.4 | 914.4 | 1133.7 | 25.5 | 34.1 | 81.6 | 150.8 | 285.2 | 872.7 | 1126.9 | 43.0 | 53.3 | 102.7 | 189.5 | 342.2 | 924.7 | 1,132.6 |
| Non-Hispanic Black | |||||||||||||||||||||
| Overall (n=4,323) | Male (n=2,262) | Female (n=2,061) | |||||||||||||||||||
| 1–10 Years (n=722) | 5.8 | 9.0 | 27.1 | 48.3 | 85.7 | 174.4 | 217.8 | 6 | 10.2 | 26.8 | 45.9 | 78.1 | 172.1 | 212.7 | 4.3 | 7.9 | 28.2 | 50.1 | 90.1 | 180.3 | 229.3 |
| 10–20 Years (n=1,923) | <5 | <5 | 14.1 | 26.2 | 47.5 | 108.6 | 141.4 | <5 | <5 | 11.8 | 24.8 | 47.6 | 108.8 | 142.6 | <5 | 5.5 | 15.7 | 27.8 | 47.0 | 108.2 | 139.1 |
| 20–30 Years (n=323) | <5 | <5 | 10.7 | 19.5 | 33.3 | 82.3 | 117.9 | <5 | <5 | 9.1 | 13.4 | 22.9 | 45.6 | 52.5 | <5 | 6.6 | 15.5 | 27.5 | 41.9 | 118.7 | 144.5 |
| 30–40 Years (n=324) | <5 | <5 | 11.4 | 21.3 | 38.5 | 89.9 | 139.6 | <5 | <5 | 7.6 | 15.2 | 24.5 | 51.7 | 61.9 | <5 | <5 | 16.4 | 31.1 | 49.7 | 112.4 | 153.9 |
| 40–50 Years (n=386) | <5 | <5 | 13.2 | 27.0 | 52.7 | 159.1 | 196.8 | <5 | <5 | 8.5 | 17.2 | 35.5 | 75.5 | 87.2 | <5 | 3.9 | 22.3 | 39.9 | 74.1 | 187.9 | 230.3 |
| 50–60 Years (n=212) | <5 | 6.5 | 21.1 | 40.2 | 87.3 | 253.5 | 341.0 | <5 | 4.1 | 15.6 | 29.3 | 63.6 | 240.9 | 298.4 | 8.7 | 10.7 | 27.0 | 55.3 | 107.6 | 252.9 | 373.3 |
| 60–70 Years (n=246) | 5.6 | 10.8 | 28.3 | 53.3 | 110.4 | 326.3 | 569.3 | 5.6 | 9.9 | 24.6 | 51.0 | 96.8 | 373.4 | 661.7 | 4.8 | 11.3 | 29.8 | 55.1 | 113.6 | 313.5 | 363.3 |
| ≥70 Years (n=187) | 16.6 | 23.7 | 65.7 | 124.5 | 254.6 | 687.8 | 849.7 | 12.5 | 16.5 | 51.5 | 93.8 | 235.7 | 861.2 | 960.1 | 21.2 | 31.3 | 77.3 | 134.0 | 255.2 | 642.5 | 704.0 |
| Mexican American | |||||||||||||||||||||
| Overall (n=5,224) | Male (n=2,666) | Female (n=2,558) | |||||||||||||||||||
| 1–10 Years (n=820) | 8.7 | 14.9 | 36.2 | 60.1 | 97.2 | 207.5 | 262.7 | 6.2 | 10.1 | 33.7 | 57.3 | 96.9 | 220.5 | 268.1 | 14.7 | 19.3 | 39.9 | 66.7 | 97.3 | 190.6 | 224.7 |
| 10–20 Years (n=2,196) | <5 | <5 | 15.5 | 28.9 | 52.3 | 119.8 | 150.0 | <5 | <5 | 11.6 | 23.9 | 45.4 | 118.1 | 157.2 | 6.3 | 8.3 | 21.0 | 33.9 | 59.0 | 119.8 | 142.9 |
| 20–30 Years (n=477) | <5 | <5 | 10.7 | 22.7 | 41.0 | 82.4 | 102.9 | <5 | <5 | 7.9 | 13.9 | 27.4 | 51.2 | 63.6 | 7.6 | 9.8 | 22.2 | 35.8 | 59.8 | 103.8 | 123.2 |
| 30–40 Years (n=394) | <5 | <5 | 11.9 | 25.1 | 43.2 | 98.7 | 128.4 | <5 | <5 | 8.0 | 18.1 | 28.8 | 55.7 | 68.9 | 7.1 | 9.8 | 26.4 | 40.4 | 71.0 | 129.2 | 149.5 |
| 40–50 Years (n=467) | <5 | 5.2 | 16.3 | 30.5 | 55.8 | 111.6 | 140.3 | <5 | <5 | 12.3 | 21.2 | 39.2 | 87.0 | 113.5 | 7.9 | 9.7 | 25.1 | 45.4 | 70.4 | 138.9 | 169.5 |
| 50–60 Years (n=209) | <5 | 5.8 | 18.1 | 38.3 | 74.0 | 161.6 | 190.9 | <5 | 6.0 | 14.7 | 24.9 | 48.8 | 92.6 | 128.1 | <5 | <5 | 26.4 | 53.2 | 104.3 | 187.2 | 206.8 |
| 60–70 Years (n=403) | 14.1 | 17.5 | 35.2 | 70.9 | 125.0 | 263.7 | 405.3 | 13.3 | 14.2 | 26.8 | 47.3 | 90.9 | 174.5 | 193.9 | 15.6 | 23.1 | 48.1 | 86.7 | 152.5 | 361.1 | 568.5 |
| ≥70 Years (n=258) | 22.9 | 27.0 | 69.5 | 144.0 | 239.2 | 766.3 | 1,220.2 | 22.1 | 24.2 | 59.6 | 131.0 | 227.6 | 705.0 | 1,163.0 | 22.6 | 36.8 | 86.2 | 145.7 | 259.9 | 778.3 | 1,384.2 |
The values depicted are weighted estimates of the 2.5th, 5th, 25th, 50th, 75th, 95th, and 97.5th centiles of N-terminal proB-type natriuretic peptide stratified by sex and race and ethnicity. The cohort was further stratified by age into 10-year bins. The values in the parenthesis indicate the unweighted sample size for each group.
Figure 4: Age-Specific Centiles of NT-proBNP Concentrations Stratified by Race and Ethnicity.
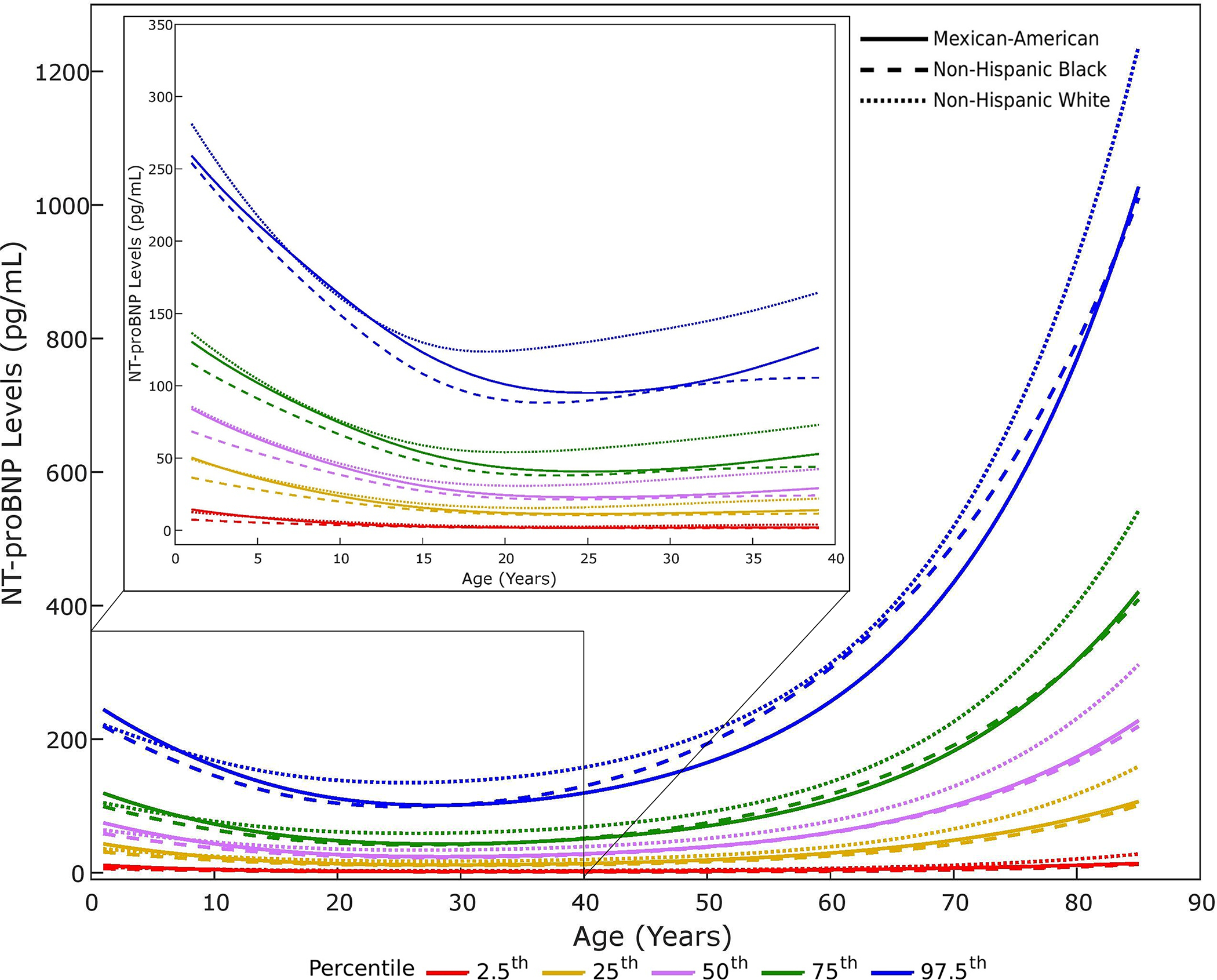
The age-specific 2.5th, 25th, 50th, 75th, and 97.5th centiles of N-terminal pro-B-type natriuretic peptide (NT-proBNP) stratified by race and ethnicity have been depicted. Non-Hispanic White, non-Hispanic Black, and Mexican American individuals have been depicted as dotted, dashed, and solid lines, respectively. The 2.5th, 25th, 50th, 75th, and 97.5th centiles of NT-proBNP have been depicted in red, yellow, purple, green, and blue, respectively. The inset in the figure shows the 2.5th, 25th, 50th, 75th, and 97.5th centiles of NT-proBNP on a magnified y-axis in individuals below 40 years of age.
Association of NT-proBNP with Clinical Correlates
In the adjusted weighted linear regression models, log NT-proBNP concentrations were 90.2% (95%CI: 84.4%–96.2%) higher in females. Log NT-proBNP concentrations were 28.0% (95%CI: 23.8%–32.0%) lower in non-Hispanic Black individuals and 20.3% (95%CI: 15.6%–24.8%) lower in Mexican American individuals compared with non-Hispanic White individuals. Among the standardized continuous variables, the largest increase in log NT-proBNP concentrations was noted with age [63.7% (95%CI: 59.6%–68.0%)] followed by systolic BP [16.2% (95%CI: 13.2%–19.3%)]. Log NT-proBNP concentrations decreased by 17.6% (95%CI: 15.6%–19.7%) per SD increase in BMI.
In the 1–10 years age group, the log NT-proBNP concentrations did not vary in females [4.2% (95%CI: −3.3%–12.2%)] compared with males. Non-Hispanic Black individuals had 19.6% (95%CI: 10.7%–27.6%) lower log NT-proBNP values compared with non-Hispanic White individuals.
In the 20–30 years age group, females had 150.5% (95%CI: 123.5%–180.8%) higher log NT-proBNP concentrations compared with males. Non-Hispanic Black and Mexican American individuals had 33.2% (95%CI: 25.7%–40.0%) and 23.5% (95%CI: 11.8%–33.6%) lower log NT-proBNP concentrations compared with non-Hispanic White individuals, respectively.
In the ≥70 years age group, log NT-proBNP concentrations were 18.7% (95%CI: 8.3%–30.1%) higher in females compared with males. Compared with non-Hispanic White individuals, non-Hispanic Black individuals, and Mexican American individuals had 28.9% (95%CI: 17.8%–38.6%) and 18.6% (95%CI: 5.6%–29.8%) lower log NT-proBNP concentrations, respectively.
The sex-stratified association of the NT-proBNP with clinical correlates has been depicted in Table 5.
Table 5:
Clinical Correlates of Log NT-pro-BNP in the Reference Sample
| Covariates | Percent Difference (95% Confidence Interval)† | P-Value |
|---|---|---|
| Whole Sample | ||
| Female Sex | 90.2 (84.4–96.2) | <0.001 |
| Age (Years) | 63.7 (59.6–68.0) | <0.001 |
| Body Mass Index (kg/m 2 ) | −17.6 (−19.7- −15.6) | <0.001 |
| Diastolic Blood Pressure (mmHg) | −18.3 (−20.4- −16.2) | <0.001 |
| Systolic Blood Pressure (mmHg) | 16.2 (13.2–19.3) | <0.001 |
| Race and Ethnicity | ||
| Non-Hispanic White | Reference | |
| Non-Hispanic Black | −28.0 (−32.0- −23.8) | <0.001 |
| Mexican American | −20.3 (−24.8- −15.6) | <0.001 |
| Males | ||
| Age (Years) | 71.2 (64.3–78.4) | <0.001 |
| Body Mass Index (kg/m 2 ) | −21.6 (−24.8- −18.3) | <0.001 |
| Diastolic Blood Pressure (mmHg) | −20.5 (−23.4- −17.6) | <0.001 |
| Systolic Blood Pressure (mmHg) | 16.4 (11.9–21.1) | <0.001 |
| Race and Ethnicity | ||
| Non-Hispanic White | Reference | |
| Non-Hispanic Black | −23.7 (−29.5- −17.4) | <0.001 |
| Mexican American | −21.1 (−27.3- −14.3) | <0.001 |
| Females | ||
| Age (Years) | 57.4 (52.2–62.8) | <0.001 |
| Body Mass Index (kg/m 2 ) | −14.0 (−16.4- −11.6) | <0.001 |
| Diastolic Blood Pressure (mmHg) | −15.4 (−18.1- −12.6) | <0.001 |
| Systolic Blood Pressure (mmHg) | 16.7 (13.0–20.4) | <0.001 |
| Race and Ethnicity | ||
| Non-Hispanic White | Reference | |
| Non-Hispanic Black | −33.5 (−38.5- −28.2) | <0.001 |
| Mexican American | −19.4 (−24.6- −13.9) | <0.001 |
The continuous variables (age, body mass index, diastolic blood pressure, and systolic blood pressure) were standardized (mean=0 and standard deviation=1). A weighted linear regression model was used to estimate the β values for each variable in the model.
Values represent the estimated percent change in N-terminal proB-type natriuretic peptide (NT-proBNP) per standard deviation increment for the continuous variables or associated with the presence of the categorical variable. Percent change was obtained using the β values for each variable generated from the regression models by applying the following equation: [eβ−1] × 100%.
NP Deficiency and Association with Prevalent Cardiometabolic Diseases
The weighted sex and race-specific 2.5th percentile value of NT-proBNP have been depicted in Table 6. Additionally, the sex and race-specific 5th and 10th percentiles have been described in Table 6. Using the 2.5th percentile as the threshold, NP deficiency was present in 815 individuals representing 9.1 million individuals of the US population. NP deficiency was associated with adjusted higher odds of hypertension [1.39 (95%CI: 1.05–1.85)], obesity [1.66 (95%CI: 1.30–2.12)], hyperlipidemia [1.79 (95%CI: 1.38–2.31)], hypertriglyceridemia [1.66 (95%CI: 1.30–2.11)], and insulin resistance [2.40 (95%CI: 1.66–3.45)] (Figure 5). The association of NP deficiency defined using the 5th and 10th percentiles of NT-proBNP concentrations with cardiometabolic diseases has been depicted in Table 7.
Table 6:
Race and Sex-Specific N-Terminal ProB-Type Natriuretic Peptide Cut-offs for Defining NP Deficiency
| 10th Percentile | 5th Percentile | 2.5th Percentile | ||||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| Non-Hispanic White | 8.7 | 21.4 | 5.7 | 15.6 | <5 | 11.8 |
| Non-Hispanic Black | 5.5 | 11.2 | <5 | 6.8 | <5 | <5 |
| Mexican American | 5.1 | 15.4 | <5 | 10.4 | <5 | 7.6 |
| Other | 6.2 | 13.9 | <5 | 10.6 | <5 | 6.7 |
The values depicted the weighted estimates of the 2.5th, 5th, and 10th percentiles of N-terminal proB-type natriuretic peptide (NT-proBNP) stratified by sex and race and ethnicity. These values were used to define natriuretic peptide deficiency for further analysis.
Figure 5: Association of Cardiometabolic Diseases with Natriuretic Peptide Deficiency.
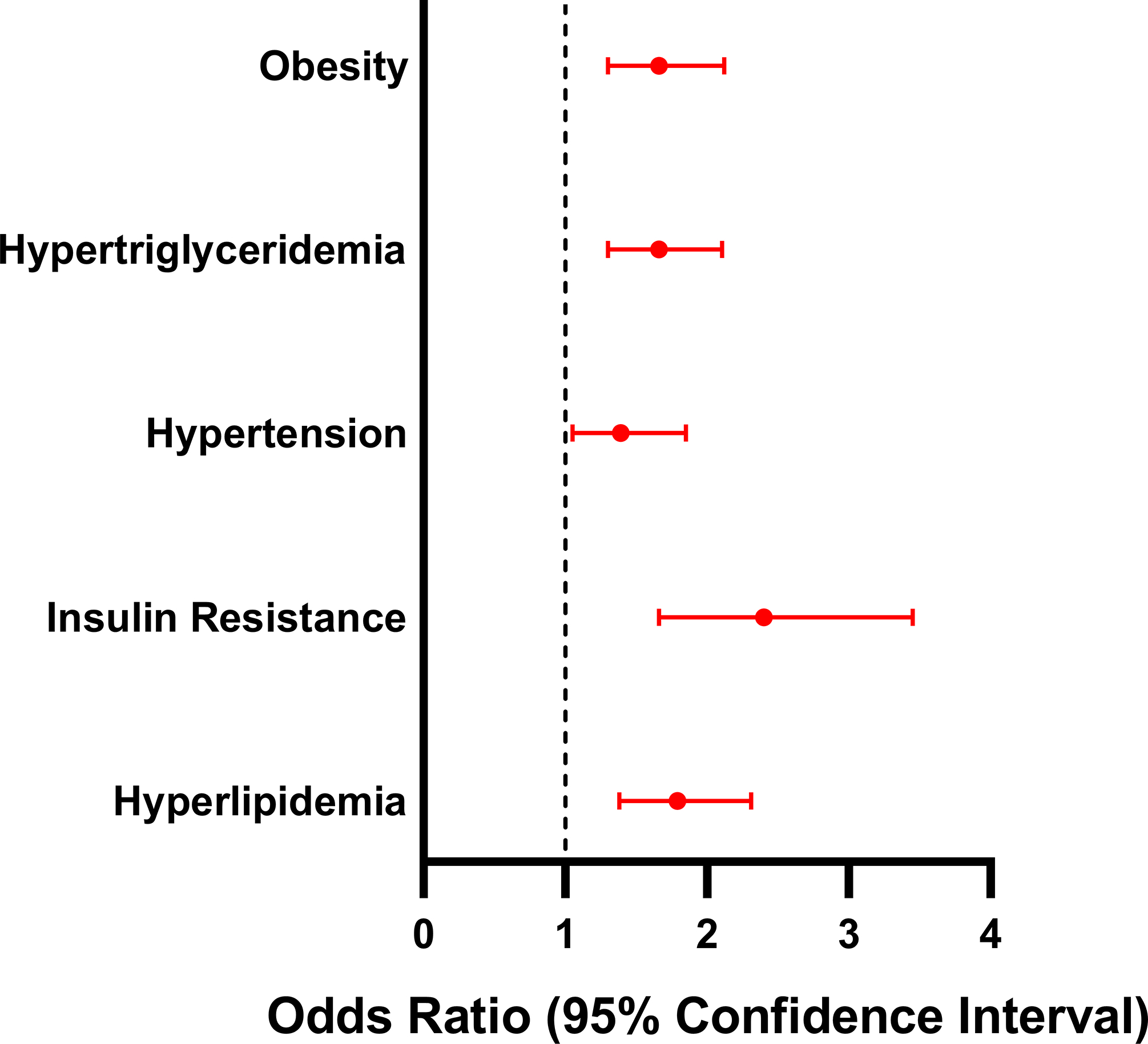
The association of cardiometabolic diseases (obesity, hypertriglyceridemia, hypertension, insulin resistance, and hyperlipidemia) with natriuretic peptide (NP) deficiency has been depicted in this figure. The point and error bars depict the effect estimates and 95% confidence interval, respectively.
Table 7:
Association of Cardiometabolic Disease with Natriuretic Peptide Deficiency Using Various Thresholds to Define Deficiency
| 10th Percentile | 5th Percentile | 2.5th Percentile | |
|---|---|---|---|
| Obesity | 1.61 (95%CI: 1.35–1.93) | 1.68 (95%CI: 1.39–2.04) | 1.66 (95%CI: 1.30–2.12) |
| Hypertriglyceridemia | 1.87 (95%CI: 1.58–2.22) | 1.95 (95%CI: 1.58–2.41) | 1.66 (95%CI: 1.30–2.11) |
| Hypertension | 1.79 (95%CI: 1.49–2.14) | 1.69 (95%CI: 1.38–2.08) | 1.39 (95%CI: 1.05–1.85) |
| Insulin Resistance | 2.27 (95%CI: 1.81–2.86) | 2.79 (95%CI: 2.13–3.66) | 2.40 (95%CI: 1.66–3.45) |
| Increased LDL Levels | 1.87 (95%CI: 1.36–2.55) | 1.69 (95%CI: 1.10–2.59) | 1.61 (95%CI: 0.95–2.73) |
| Dyslipidemia | 1.86 (95%CI: 1.50–2.31) | 1.83 (95%CI: 1.46–2.30) | 1.79 (95%CI: 1.38–2.31) |
The effect estimates and 95% confidence interval for the odds ratio of cardiometabolic diseases in natriuretic peptide (NP) deficient individuals have been depicted. NP deficiency was defined using multiple thresholds, including the sex and race-specific 2.5th, 5th, and 10th percentile values.
The prevalence and odds of cardiometabolic diseases across the quintiles of NT-proBNP stratified by race and sex have been depicted in Supplemental Table 1–4.
Discussion
This is the first study to establish reference intervals for NT-proBNP concentrations in a healthy nationally representative US population including individuals across the lifespan. NT-proBNP concentrations were noted to decrease from childhood to the lowest lifetime value in the 20–30 age group. From the third decade of life, NT-proBNP concentrations consistently increased with age in the overall cohort and in the sex and racial and ethnic subgroups. In the overall cohort, when stratified by sex, females had ~90% higher NT-proBNP concentrations compared with males. However, the sex-specific NT-proBNP concentration differences were not seen during childhood (1–10 years age group). Higher NT-proBNP concentrations in females compared with males were first noted in adolescence and persisted thereafter with increasing age (Central Illustration). Upon stratification by race and ethnic subgroups, non-Hispanic Black and Mexican-American individuals had ~28% and ~20% lower NT-proBNP concentrations compared with non-Hispanic White individuals, respectively. NT-proBNP concentrations in non-Hispanic Black individuals were consistently lower than non-Hispanic White individuals across the age spectrum (Central Illustration). NP deficiency was associated with a higher risk of cardiometabolic diseases, as noted in this study.
Central Illustration: Age-Specific N-Terminal B-Type Natriuretic Peptide Concentrations Stratified by Age and Race and Ethnicity.
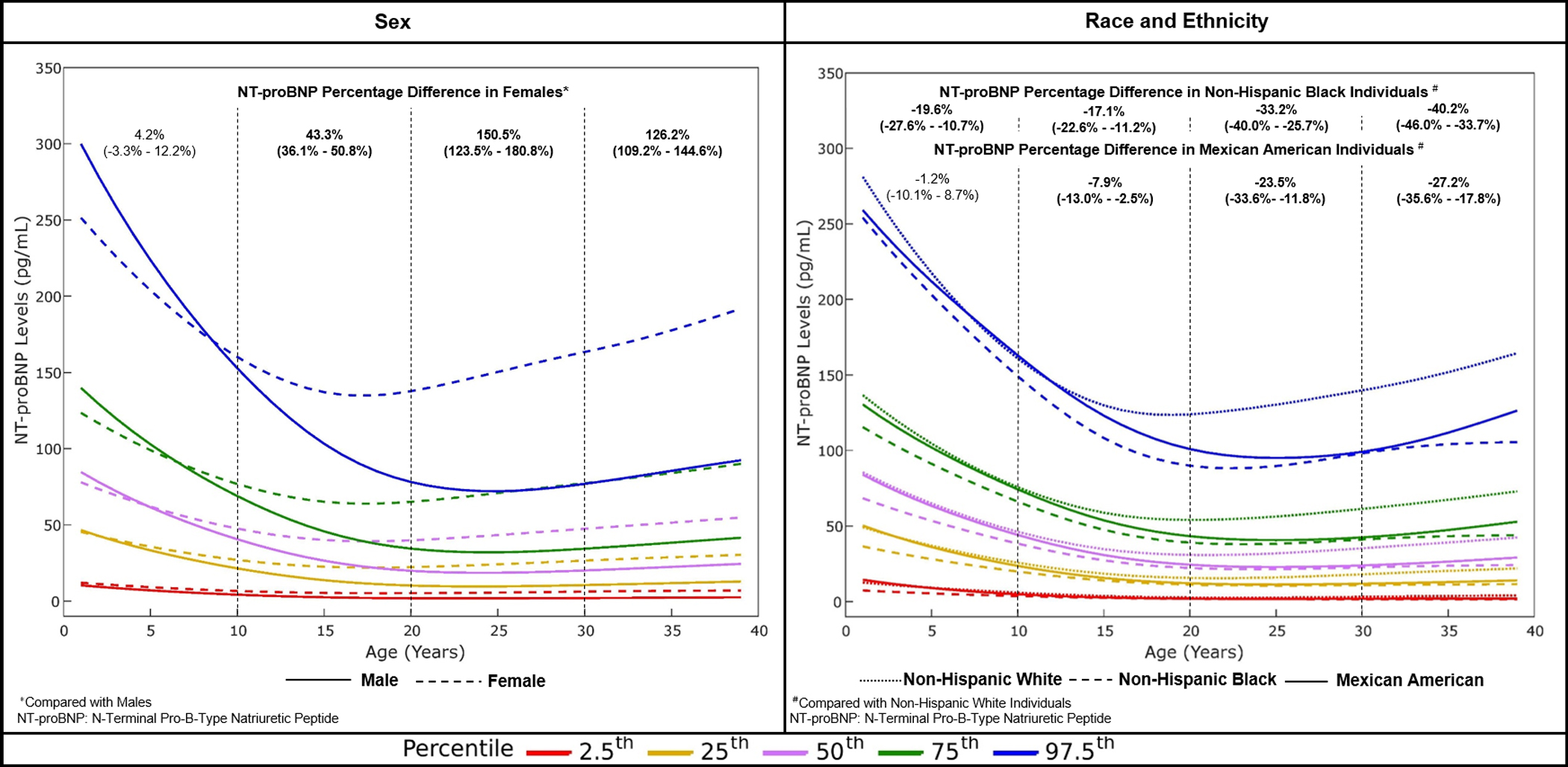
The age-specific 2.5th, 25th, 50th, 75th, and 97.5th centiles of N-terminal pro-B-type natriuretic peptide (NT-proBNP) stratified by sex and race and ethnicity in individuals below 40 years of age have been depicted. The panel on the left depicts sex-stratified NT-proBNP concentrations. Males have been depicted as solid lines and females have been depicted as dashed lines. The percentage difference of NT-proBNP in females compared with males per 10-year age group has been depicted. The panel on the right depicts race and ethnicity stratified NT-proBNP concentrations. Non-Hispanic White, non-Hispanic Black, and Mexican American individuals have been depicted as dotted, dashed, and solid lines, respectively. The percentage difference of NT-proBNP in non-Hispanic Black and Mexican American individuals compared with non-Hispanic White individuals per 10-year age group has been depicted. In both panels, the 2.5th, 25th, 50th, 75th, and 97.5th centiles of NT-proBNP have been depicted in red, yellow, purple, green, and blue, respectively.
The higher NT-proBNP concentrations in childhood may be attributed to the ongoing development of the heart and adaptations of the heart to meet the metabolic requirement of growth (23). After reaching its nadir in the 20–30 years age group, NT-proBNP concentrations continue to rise with age. Decreased clearance of NPs through renal and non-renal mechanisms with age may partly explain the rising NT-proBNP concentrations with age (24). Due to the large variations in NT-proBNP concentrations in childhood, the diagnostic value of NT-proBNP may be improved by generating age-adjusted reference intervals. A recent study showed that the use of age-adjusted NT-proBNP concentrations had superior predictive value for major adverse cardiovascular events in children with congenital heart disease compared with absolute values of NT-proBNP (25).
The presence of sex-associated differences in NT-proBNP concentrations varied with age. Though the mechanism of sex-associated differences in NT-proBNP concentrations is unclear, the absence of this difference in childhood, appearance in adolescence, and persistence into adulthood thereafter may indicate that sex hormones play a role regulation of NT-proBNP concentrations (24,26). Building on the previous report by Nir et al describing the sex difference in NP levels in the pediatric population, this is the first US-based population-level study highlighting that sex differences in NP concentrations are not present in children (28). It has been posited that androgens suppress NP concentrations while estrogen increases NP concentrations (26). However, the presence of modest sex-associated differences in NT-proBNP concentrations in the age group >70 years may suggest that only a part of the noted sex-associated NP differences can be explained by sex hormones. Renin is an endogenous antagonist to the NP system (27). Females have lower renin concentrations compared with males which may play a role in the higher NT-proBNP concentrations observed in females (24).
NP concentrations have been shown to be lower in non-Hispanic Black adults compared with non-Hispanic White adults previously (4,6). The presence of lower concentrations of NT-proBNP since childhood in non-Hispanic Black individuals supports the role of genetic variants as a determinant of NT-proBNP concentrations. Genetic variants that impair processing and increase clearance are more prevalent in non-Hispanic Black individuals compared with non-Hispanic White individuals which may explain the observed differences in NT-proBNP concentrations (6). Additionally, the current study is the first to describe the age-specific normative NT-proBNP concentrations in Mexican American individuals to our knowledge. The NT-proBNP concentrations in Mexican American individuals were lower in adulthood compared with non-Hispanic White individuals (29). Mexican Americans are an admixed population having variable proportions of African and European ancestry (29). Considering that the NT-proBNP concentrations decrease with increasing proportions of African ancestry, it is likely that the NT-proBNP concentrations of Mexican American individuals are determined by the proportion of African ancestry present at an individual level (29). Further work is needed to assess the determinants of NT-proBNP concentrations in Mexican American individuals.
Previous efforts of estimating NT-proBNP reference values were conducted in smaller cohorts and limited to older individuals which limited their generalizability (7–9). Furthermore, the prior studies focused on defining the upper normal limit of NT-proBNP (7–9). The current study reports the NP concentrations across the lifespan and presents normative NP concentrations across sex and race and ethnic subgroups. The reference ranges generated in this study are more robust as the ranges were developed using the GAMLSS method that accounts for the changing skewness in NT-proBNP concentrations with age in a nationally representative US population (22).
Apart from describing the normative concentrations of NT-proBNP, this study established the threshold to define NP deficiency and demonstrated the association of cardiometabolic diseases with NP deficiency. Previously, animal and genetic models have shown that NP deficiency is associated with the development of cardiometabolic diseases. NP gene knockout experiments in animal models to study the effects of NP deficiency have elucidated that the impairment of the physiological roles of the NPs leads to the development of salt-sensitive hypertension, insulin resistance, and obesity (30–32). The current study validates these findings using humans as model systems. Furthermore, this study highlights the importance of detecting NP deficiency early in life as NP deficiency may be obscured by the age-related increase in NP concentrations.
Defining the threshold for NP deficiency may permit the identification of individuals at a higher risk of cardiometabolic diseases. Thus, interventions targeting the NP axis by inhibiting NP degradation or NP augmentation may reduce the risk of cardiometabolic diseases and the burden of cardiovascular disease in NP-deficient individuals. The current study underlines the need to recognize NP deficiency as a precursor to cardiometabolic disease to promote the discovery of new interventions to increase NP concentrations. Future research should focus on identifying the underlying causes of NP deficiency and the generation of tailored therapeutic agents which will target the cause of NP deficiency.
Limitations
This study has some limitations. First, sex and race and ethnicity were self-reported. Race and ethnicity are social constructs that may not correspond with the genetic ancestry of an individual. Second, causality cannot be inferred due to the cross-sectional nature of the survey. Third, NPs are known to have a diurnal rhythm with higher concentrations during the day and lower concentrations at night. The timing of blood draws for NT-proBNP measurement was not recorded in the NHANES preventing adjustment for the diurnal rhythmicity of NPs (27). Fourth, the exclusion of individuals may lead to increased variance in estimates due to variability in the assignment of weights. Fifth, NT-proBNP concentrations were measured in 2018–2020 using serum samples stored from 1999–2004. However, NT-proBNP is known to be stable under adequate storage conditions (33). Sixth, this study was unable to characterize the reference intervals of NT-proBNP in children below 1 year as the NHANES did not contain NT-proBNP measurements for this age group. Seventh, the NHANES lacked data on echocardiography and clinical symptomatology which reduced the granularity of identifying a healthy study sample. Lastly, cautious interpretation of the low values of NT-proBNP concentrations is recommended due to the intermediate precision CV at the lower end of the detectable range of the analyzer.
Conclusion
This study establishes the reference range of NT-proBNP and the threshold for NT-proBNP deficiency in a nationally representative healthy US population. Sex-associated differences in NT-proBNP concentrations appear during adolescence but race and ethnicity-based differences are present since birth. NP deficiency affects an estimated 9.1 million individuals. Defining the threshold of NP deficiency may allow the identification of individuals at an increased risk of cardiometabolic diseases. Further studies are needed to identify therapies to increase NP concentrations in NP-deficient individuals.
Clinical Perspectives
Competency in Medical Knowledge 1:
This is the first study to characterize the age-specific NT-proBNP concentrations across the spectrum of age in a nationally representative cohort of healthy individuals.
Competency in Medical Knowledge 2:
The absence of sex-associated differences in NT-proBNP concentrations in childhood, the appearance in adolescence, and persistence in adulthood noted in this study may imply that sex hormones play a role in the regulation of NT-proBNP concentrations.
Competency in Medical Knowledge 3:
Non-Hispanic Black individuals have lower NT-proBNP concentrations compared with non-Hispanic White individuals which may be attributable to the higher prevalence of genetic variants that impair NP processing and increase NP degradation in non-Hispanic Black individuals.
Translational Outlook 1:
The NT-proBNP reference intervals established in this study may help guide future research based on NP biology.
Translational Outlook 2:
This study highlights the need to detect NP deficiency at an early age before the onset of subclinical cardiovascular disease, unravel the etiology of NP deficiency, and the development of targeted therapeutic agents to increase NP concentrations.
Supplementary Material
Acknowledgments:
We would like to acknowledge the individuals who participated in the National Health and Nutrition Examination Survey 1999–2004. The authors would also like to extend their gratitude to the Biomarkers Consortium of the Foundation for the National Institutes of Health for funding the measurement of NT-proBNP (N-Terminal proB-Type Natriuretic Peptides) concentrations. We thank Dr. Elizabeth Selvin and Dr. Robert Christenson for conducting the stored specimen study to measure the NT-proBNP concentrations.
Sources of Funding:
Dr. Pankaj Arora is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH) awards R01HL160982, R01HL163852, R01HL163081, and K23HL146887.
Abbreviations:
- BMI
Body Mass Index
- CDC
Center for Disease Control and Prevention
- CV
Coefficient of Variation
- GAMLSS
Generalized Additive Models for Location, Scale, and Shape
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- NP
Natriuretic Peptide
- NT-proBNP
N-Terminal B-Type Natriuretic Peptide
Footnotes
Disclosures: None of the other authors had any conflicts of interest or financial disclosures to declare.
References
- 1.Chow SL, Maisel AS, Anand I et al. Role of Biomarkers for the Prevention, Assessment, and Management of Heart Failure: A Scientific Statement From the American Heart Association. Circulation 2017;135:e1054–e1091. [DOI] [PubMed] [Google Scholar]
- 2.Arora P, Wu C, Hamid T et al. Acute Metabolic Influences on the Natriuretic Peptide System in Humans. J Am Coll Cardiol 2016;67:804–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arora P, Wu C, Khan AM et al. Atrial natriuretic peptide is negatively regulated by microRNA-425. J Clin Invest 2013;123:3378–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bajaj NS, Gutierrez OM, Arora G et al. Racial Differences in Plasma Levels of N-Terminal Pro-B-Type Natriuretic Peptide and Outcomes: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. JAMA Cardiol 2018;3:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel N, Gutierrez OM, Arora G et al. Race-based demographic, anthropometric and clinical correlates of N-terminal-pro B-type natriuretic peptide. Int J Cardiol 2019;286:145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel N, Russell GK, Musunuru K et al. Race, Natriuretic Peptides, and High-Carbohydrate Challenge: A Clinical Trial. Circ Res 2019;125:957–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fradley MG, Larson MG, Cheng S et al. Reference limits for N-terminal-pro-B-type natriuretic peptide in healthy individuals (from the Framingham Heart Study). Am J Cardiol 2011;108:1341–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Welsh P, Campbell RT, Mooney L et al. Reference Ranges for NT-proBNP (N-Terminal Pro-B-Type Natriuretic Peptide) and Risk Factors for Higher NT-proBNP Concentrations in a Large General Population Cohort. Circ Heart Fail 2022;15:e009427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galasko GI, Lahiri A, Barnes SC, Collinson P, Senior R. What is the normal range for N-terminal pro-brain natriuretic peptide? How well does this normal range screen for cardiovascular disease? Eur Heart J 2005;26:2269–76. [DOI] [PubMed] [Google Scholar]
- 10.Zois NE, Bartels ED, Hunter I, Kousholt BS, Olsen LH, Goetze JP. Natriuretic peptides in cardiometabolic regulation and disease. Nat Rev Cardiol 2014;11:403–12. [DOI] [PubMed] [Google Scholar]
- 11.Tsao CW, Aday AW, Almarzooq ZI et al. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999–2010. Vital Health Stat 1 2013:1–37. [PubMed] [Google Scholar]
- 13.Parcha V, Patel N, Kalra R, Arora G, Arora P. Prevalence, Awareness, Treatment, and Poor Control of Hypertension Among Young American Adults: Race-Stratified Analysis of the National Health and Nutrition Examination Survey. Mayo Clin Proc 2020;95:1390–1403. [DOI] [PubMed] [Google Scholar]
- 14.Kalra R, Parcha V, Patel N et al. Increased awareness, inadequate treatment, and poor control of cardiovascular risk factors in American young adults: 2005–2016. Eur J Prev Cardiol 2021;28:304–312. [DOI] [PubMed] [Google Scholar]
- 15.Patel N, Bhargava A, Kalra R et al. Trends in Lipid, Lipoproteins, and Statin Use Among U.S. Adults: Impact of 2013 Cholesterol Guidelines. J Am Coll Cardiol 2019;74:2525–2528. [DOI] [PubMed] [Google Scholar]
- 16.Patel N, Kalra R, Bhargava A, Arora G, Arora P. Ideal Cardiovascular Health Among American Adults After the Economic Recession of 2008–2009: Insights from NHANES. Am J Med 2019;132:1182–1190 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shetty NS, Parcha V, Patel N et al. AHA Life’s essential 8 and ideal cardiovascular health among young adults. Am J Prev Cardiol 2023;13:100452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 19.Parcha V, Heindl B, Kalra R et al. Insulin Resistance and Cardiometabolic Risk Profile Among Nondiabetic American Young Adults: Insights From NHANES. J Clin Endocrinol Metab 2022;107:e25–e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–421. [PubMed] [Google Scholar]
- 21.Ingram DD, Malec DJ, Makuc DM et al. National Center for Health Statistics Guidelines for Analysis of Trends. Vital Health Stat 2 2018:1–71. [PubMed] [Google Scholar]
- 22.Rigby RA, Stasinopoulos DM. Automatic smoothing parameter selection in GAMLSS with an application to centile estimation. Stat Methods Med Res 2014;23:318–32. [DOI] [PubMed] [Google Scholar]
- 23.de Jonge LL, van Osch-Gevers L, Willemsen SP et al. Growth, obesity, and cardiac structures in early childhood: the Generation R Study. Hypertension 2011;57:934–40. [DOI] [PubMed] [Google Scholar]
- 24.Wang TJ, Larson MG, Levy D et al. Impact of age and sex on plasma natriuretic peptide levels in healthy adults. Am J Cardiol 2002;90:254–8. [DOI] [PubMed] [Google Scholar]
- 25.Palm J, Holdenrieder S, Hoffmann G et al. Predicting Major Adverse Cardiovascular Events in Children With Age-Adjusted NT-proBNP. J Am Coll Cardiol 2021;78:1890–1900. [DOI] [PubMed] [Google Scholar]
- 26.Lam CS, Cheng S, Choong K et al. Influence of sex and hormone status on circulating natriuretic peptides. J Am Coll Cardiol 2011;58:618–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parcha V, Patel N, Gutierrez OM et al. Chronobiology of Natriuretic Peptides and Blood Pressure in Lean and Obese Individuals. J Am Coll Cardiol 2021;77:2291–2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nir A, Lindinger A, Rauh M et al. NT-pro-B-type natriuretic peptide in infants and children: reference values based on combined data from four studies. Pediatr Cardiol 2009;30:3–8. [DOI] [PubMed] [Google Scholar]
- 29.Gupta DK, Daniels LB, Cheng S et al. Differences in Natriuretic Peptide Levels by Race/Ethnicity (From the Multi-Ethnic Study of Atherosclerosis). Am J Cardiol 2017;120:1008–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miyashita K, Itoh H, Tsujimoto H et al. Natriuretic peptides/cGMP/cGMP-dependent protein kinase cascades promote muscle mitochondrial biogenesis and prevent obesity. Diabetes 2009;58:2880–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bordicchia M, Liu D, Amri EZ et al. Cardiac natriuretic peptides act via p38 MAPK to induce the brown fat thermogenic program in mouse and human adipocytes. J Clin Invest 2012;122:1022–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holditch SJ, Schreiber CA, Nini R et al. B-Type Natriuretic Peptide Deletion Leads to Progressive Hypertension, Associated Organ Damage, and Reduced Survival: Novel Model for Human Hypertension. Hypertension 2015;66:199–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ishigami J, Karger AB, Lutsey PL, Coresh J, Matsushita K. Stability of Serum Bone-Mineral, Kidney, and Cardiac Biomarkers after a Freeze-Thaw Cycle: The Aric Study. Am J Epidemiol 2022;191:534–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


