Abstract
Summary
In a cross-sectional study assessing the experiences of individuals with osteogenesis imperfecta accessing care during the COVID-19 pandemic, participants reported high rates of delays in accessing medical care and high utilization of telehealth. Considering the needs of individuals with complex medical conditions is important when improving access to care.
Purpose
Individuals with osteogenesis imperfecta (OI) often have complex care needs requiring that they see a variety of specialists. The onset of the COVID-19 pandemic in March 2020 led to delays in medical care for many health conditions. The goal of this study was to describe the experiences of individuals with OI accessing medical care during this time.
Methods
Responses to an electronic survey distributed via the OI Foundation mailing list were collected from August 2020 until February 2021. Participants were instructed to compare their experiences in the months since the start of the pandemic with their experiences prior to this date. Data were analyzed using descriptive statistics and were compared across demographic groups using logistic regression and chi-squared tests.
Results
Surveys were completed by 110 participants. Most participants (72%) reported experiencing delays in accessing at least one care provider. The majority of participants reported less or similar amounts of bone pain (74.3%) and less or the same rate of fracture (88.6%) as before the start of the pandemic.
Conclusion
While most study participants experienced delays in care, they did not report an increase in symptoms associated with OI. They also frequently utilized telehealth as a tool to see their providers. Future research should focus on the impact of changes in telehealth legislation on patients’ ability to access care. As methods for care delivery evolve, the needs of people with OI and other rare diseases should be considered and prioritized.
Keywords: Osteogenesis imperfecta, Access to healthcare, Telemedicine, Bisphosphonates
Introduction
Osteogenesis imperfecta (OI) is a rare genetic condition characterized by increased bone fragility, low bone mass, and risk for fracture and skeletal deformities [1]. The majority of OI cases are caused by autosomal dominant mutations in genes involved in the biosynthesis and regulation of type I collagen, which can result in a variety of clinical manifestations beyond those related to the skeleton, including blue sclerae, dentinogenesis imperfecta, hearing loss (otosclerosis), and joint hypermobility [1, 2]. OI is commonly classified into four subtypes by the Sillence system, which initially classified cases based on severity ranging from mild (Types I and IV) to severe (Types II and III) as well as suspected mode of inheritance [3]. Types V-XIX have since been reported, highlighting distinct phenotypes and genetic mutations [4].
Multidisciplinary care is essential for treating individuals with OI and often involves diverse specialties including orthopedics, endocrinology, dental, physiatry, physical and occupational therapy, nutrition, genetics, audiology, and others [1, 2] with key goals of maximizing mobility, minimizing the risk of fracture, and improving quality of life. Bisphosphonates are still the most commonly prescribed medications for skeletal fragility due to OI [2]. Surgical intervention, including osteotomies and rod placement, may also be utilized, especially in more severe subtypes [5].
The onset of the COVID-19 pandemic in March 2020 had a major impact on healthcare systems, both in the USA and abroad, with many patients facing delays in routine and specialized healthcare services [6–8]. For example, delays have been described in the surgical treatment of early-stage breast and prostate cancers [9], diagnosis of head and neck cancers [10], and administration of childhood vaccinations [11]. People with rare diseases, who likely had barriers to receiving medical care and support even prior to the COVID-19 pandemic [12], might be expected to be more likely to experience delays in care during the pandemic and uncertainty regarding the impact of COVID-19 on their conditions [13]. Research on the experiences of these populations is limited. While there has been research about the experiences of individuals with OI living in the UK during the COVID-19 pandemic [14], no published research exists describing the experiences of their counterparts living in the USA. The goal of this study is to assess the experiences of people with OI living in the USA during the COVID-19 pandemic with regard to delays in access to healthcare services as well as their impact on OI-related symptoms.
Methods
Study design
This cross-sectional study was conducted to investigate the access to healthcare and medical services by people with OI. This study was reviewed by the Emory University Institutional Review Board. All participants consented to participate in the study and verified that they were over 18 years of age before completing the survey. Participants were also eligible if they were at least 18 years old and completing the survey on behalf of a person with OI. As no identifying information was collected, responses from participants who reported the same age were reviewed to determine if they had the same self-reported OI subtype, gender, and relationship to the person with OI (i.e., self or on behalf of another person). Based on these criteria, we feel that there were no duplicate surveys.
Participants
The survey was distributed to potential participants through the OI Foundation mailing list. The OI Foundation is a patient advocacy organization dedicated to improving the quality of life of individuals affected by OI. The survey was first distributed to individuals on the OI Foundation mailing lists on August 31, 2020. The survey was also sent to healthcare providers who were members of the Pediatric Endocrine Society Bone and Mineral Special Interest Group to be shared with their patients with OI. Survey responses were collected from August 31, 2020, through February 14, 2021. Survey responses were included in the analysis if they answered questions regarding how the COVID-19 pandemic affected the individual with OI. Survey responses that only included consent or demographics about the individual with OI were excluded from the analysis.
Data collected
Participants completed a Research Electronic Data Capture (REDCap, Vanderbilt University, Nashville, TN) survey answering questions regarding demographics, use of and access to healthcare services and medications, bone pain and fractures. The day that the World Health Organization classified COVID-19 as a global pandemic, March 11, 2020, was selected as the reference date. Participants were asked to compare their experiences during the beginning of the COVID-19 pandemic (March 11, 2020–July 10, 2020) to the months preceding the COVID-19 pandemic (December 11, 2019–March 10, 2020).
Participants self-reported their OI subtype. For analysis, participants were classified as having severe OI if they self-identified as having types 2, 3, 6–8 or “severe” OI. Participants were classified as having mild OI if they self-identified as having types 1, 4 5, or “mild.” Participants were classified as unknown if they reported that their OI subtype was “unknown.”
Analysis
Descriptive statistics were complied. Outcomes were compared by demographic groups using logistic regression and chi-squared tests. Due to the descriptive and observational nature of this study, complete data was analyzed. Analysis was done using Stata release 17 (StataCorp, College Station, TX). A sensitivity analysis was performed including only participants living in the USA. Results were similar when including and excluding participants living outside the USA, so results are reported including all participants.
Results
Baseline demographics: geography, age, sex, OI subtype
A total of 110 participant responses were analyzed; 9 surveys were partially complete. An additional 21 surveys were initialized but not completed. Due to the methods of survey distribution, the response rate is unknown. The demographics of survey participants are summarized in Table 1. Notably, 62% of survey respondents were female, and the median age was 32.5 years (interquartile range 8.2–58.4 years); 45 individuals (40.9%) were less than 18 years of age. Most individuals (68, 61.8%) reported having mild OI, 37 (33.6%) reported having severe OI, and 5 individuals reported their OI subtype was unknown. Participants represented a diverse sampling from regions of the USA. The region with the greatest representation was the southeast USA (27.5%).
Table 1.
Demographics by OI severity
| Mild (n = 68) | Severe (n = 37) | Unknown (n = 5) | Total (n = 110) | |
|---|---|---|---|---|
| Age (years) | 30.9 (7.0–58.8) | 37.4 (15.5–53.1) | 65.9 (18.1–67.1) | 32.5 (8.2–58.4) |
| < 18 years old | 28 (41.1%) | 16 (43.2%) | 1 (20%) | 45 (40.9%) |
| Sex | ||||
| Male | 23 (33.8%) | 17 (45.9%) | 2 (40.0%) | 42 (38.2%) |
| Female | 45 (66.2%) | 20 (54.1%) | 3 (60.0%) | 68 (61.8%) |
| Uses bisphosphonates | ||||
| No | 39 (57.4%) | 22 (59.5%) | 4 (80.0%) | 65 (59.1%) |
| Yes | 29 (42.6%) | 15 (40.5%) | 1 (20.0%) | 45 (40.9%) |
| Regiona | ||||
| West | 12 (17.6%) | 6 (16.7%) | 0 (0%) | 18 (16.5%) |
| Southwest | 3 (4.4%) | 5 (13.9%) | 1 (20%) | 9 (8.3%) |
| Midwest | 10 (14.7%) | 4 (11.1%) | 1 (20%) | 15 (13.8%) |
| Southeast | 19 (27.9%) | 8 (22.2%) | 3 (60%) | 30 (27.5%) |
| Northeast | 14 (20.6%) | 8 (22.2%) | 0 (0%) | 22 (20.2%) |
| Outside the USA | 10 (14.7%) | 5 (13.9%) | 0 (0%) | 15 (13.8%) |
Participants self-reported what state they lived in; states were grouped into regions utilizing National Geographic Society criteria [20]. Variables are reported as median (interquartile range) or counts (percent)
Access to care
Most survey respondents (79 individuals, 71.8%) reported delays in accessing healthcare services including aquatic therapy, physical therapy, occupational therapy, audiology, and physiatry (Fig. 1). Nearly half (44%) of participants reported receiving some care via telehealth, most commonly for appointments with their primary care providers. While many individuals did report delays in accessing their physician teams, many were able to access their primary care and specialist providers in their usual manner as before the pandemic (42.9% for primary care, 52.5% for orthopedics, and 44.2% for endocrinology). Access to aquatic therapy (24 individuals delayed, 82.8% of individuals receiving aquatic therapy) and dentistry (53 individuals delayed, 71.6% of individuals needing dental services) were most impacted. Among individuals who reported delays in accessing care, 63.6% indicated that they had used telehealth services. Several participants commented on increased or new needs for mental health services for anxiety.
Fig. 1.
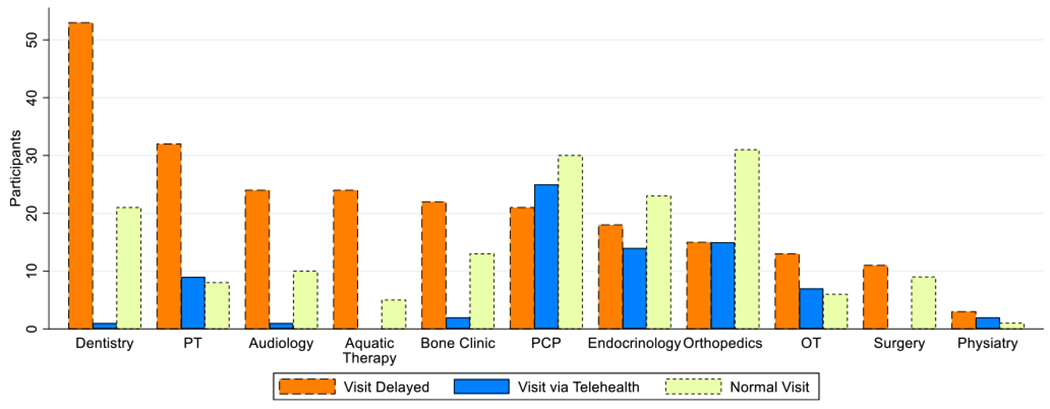
Access to services. Participants responded if their access to various specialists was delayed, via telehealth or like normal. Abbreviations: PT (physical therapy), PCP (primary care provider), OT (occupational therapy)
Additionally, 11 individuals (55% of those scheduled for surgery) had delays in scheduled elective surgeries including 6 orthopedic procedures and 1 dental procedure. Children under 16 years of age (35.5% of participants) were 3 times more likely to experience delays in some aspect of care than participants older than 16 (p = 0.031).
Bisphosphonates
Of the 45 individuals who reported using bisphosphonate therapy, 40 (88.9%) were using intravenous, 8 (17.8%) were using oral, and 3 individuals reported using both oral and intravenous formulations. The median dosing interval for bisphosphonate infusions was 6 months. As expected, children under 16 were > 6 times as likely to be on bisphosphonates (p < 0.001). Of the 16 individuals who reported bisphosphonate infusion delays, 15 individuals reported that their delay was, indeed, due to the COVID-19 pandemic, either because the infusion site was unavailable or because of concerns about the pandemic (Table 2). The majority of patients (11) who reported delays in bisphosphonate treatment were under 16.
Table 2.
Intravenous bisphosphonate use and delays
| No delay (n = 24) | Delay (n = 16) | Total (n = 40) | |
|---|---|---|---|
| Age (years) | 9.8 (3.9–21.3) | 10.4 (5.6–34.8) | 10.4 (4.3–21.3) |
| Sex | |||
| Male | 12 (50%) | 8 (50%) | 20 (50%) |
| Female | 12 (50%) | 8 (50%) | 20 (50%) |
| OI Severity | |||
| Mild | 14 (58%) | 12 (75%) | 26 (65%) |
| Severe | 10 (42%) | 3 (19%) | 13 (33%) |
| Unknown | 0 (0%) | 1 (6%) | 1 (3%) |
| Bisphosphonate treatment location | |||
| Hospital-based inpatient | 2 (8%) | 2 (13%) | 4 (10%) |
| Hospital-based outpatient | 21 (88%) | 13 (82%) | 34 (85%) |
| Home infusion | 0 (0%) | 1 (6%) | 1 (3%) |
| Multiple | 1 (4%) | 0 (0%) | 1 (3%) |
| Bisphosphonate infusion interval (months) | 4.5 (3–6) | 6 (4–9) | 6 (3–6) |
| Delay in receiving bisphosphonates (months) | 0 (0–0) | 2 (1–3) | 2 (1–3) |
| Reason for bisphosphonate delay | |||
| Infusion site not available (1) | 0 (0%) | 8 (50%) | 8 (47%) |
| Worry about COVID-19 (2) | 0 (0%) | 4 (25%) | 4 (24%) |
| Reason unrelated to COVID-19 (3) | 1 (100%) | 1 (6%) | 2 (12%) |
| (1) and (2) | 0 (0%) | 2 (13%) | 2 (12%) |
| (2) and (3) | 0 (0%) | 1 (6%) | 1 (6%) |
Variables are reported as median (interquartile range) or counts (percent)
Symptoms
When comparing the early COVID-19 pandemic to the months before the COVID-19 pandemic, most participants reported that they had similar bone pain and similar rate of fractures. Participants over age 16 were three times more likely than younger participants to report increased bone pain (p = 0.040); this was not associated with receiving bisphosphonate infusions. Most participants indicated that they were as likely to seek care for their fractures in an emergency healthcare setting or physician’s office or to treat at home during the COVID-19 pandemic as before. Notably, 43.1% and 38.1% of participants reported they were less likely to seek care in an emergency healthcare setting or physician’s office, respectively, and 30.8% of participants answered that they were more likely to treat a fracture at home during the COVID-19 pandemic (Table 3).
Table 3.
Comparing symptoms and the likelihood of receiving care at various locations to before the start of the COVID-19 pandemic
| Mild OI (n = 68) | Severe OI (n = 37) | Unknown OI severity (n = 5) | Total (n = 105) | |
|---|---|---|---|---|
| Bone pain | ||||
| Less | 0 (0%) | 3 (8.6%) | 0 (0%) | 3 (2.9%) |
| Same | 48 (73.8%) | 23 (65.7%) | 4 (80.0%) | 75 (71.4%) |
| More | 17 (26.2%) | 9 (25.7%) | 1 (20.0%) | 27 (25.7%) |
| Number of OI-related complications | ||||
| Less | 5 (7.7%) | 0 (0%) | 0 (0%) | 5 (4.8%) |
| Same | 45 (69.2%) | 29 (82.9%) | 5 (100.0%) | 79 (75.2%) |
| More | 15 (23.1%) | 6 (17.1%) | 0 (0%) | 21 (20.0%) |
| Number of fractures | ||||
| Less | 10 (15.4%) | 4 (11.4%) | 1 (20.0%) | 15 (14.3%) |
| Same | 45 (69.2%) | 29 (82.9%) | 4 (80.0%) | 78 (74.3%) |
| More | 10 (15.4%) | 2 (5.7%) | 0 (0%) | 12 (11.4%) |
| Likelihood to treat at home | ||||
| Less | 7 (10.9%) | 3 (8.6%) | 1 (20.0%) | 11 (10.6%) |
| Same | 33 (51.6%) | 24 (68.6%) | 4 (80.0%) | 61 (58.7%) |
| More | 24 (37.5%) | 8 (22.9%) | 0 (0.0%) | 32 (30.8%) |
| Likelihood to treat at doctor’s office | ||||
| Less | 26 (40.0%) | 14 (40.0%) | 0 (0%) | 40 (38.1%) |
| Same | 36 (55.4%) | 19 (54.3%) | 4 (80.0%) | 59 (56.2%) |
| More | 3 (4.6%) | 2 (5.7%) | 1 (20.0%) | 6 (5.7%) |
| Likelihood to seek emergency care (emergency department or urgent care) | ||||
| Less | 28 (44.4%) | 15 (44.1%) | 1 (20.0%) | 44 (43.1%) |
| Same | 34 (54.0%) | 18 (52.9%) | 3 (60.0%) | 55 (53.9%) |
| More | 1 (1.6%) | 1 (2.9%) | 1 (20.0%) | 3 (2.9%) |
Discussion
This study found that many individuals with OI experienced delays in receiving care including bisphosphonate treatment as a direct result of the COVID-19 pandemic after initial lockdowns in March 2020. However, the majority did not experience increased symptoms associated with OI, including fracture and bone pain.
These results are consistent with other studies about access to care during the COVID-19 pandemic among individuals with rare bone diseases as well as a myriad of other conditions. In a study conducted by Smyth et al. in the UK around the same time period, 63% of participants reported having delays in access to various aspects of medical care [14]. This difference between the results in our study and the UK study might have been due to differences in regulations regarding medical care in the two nations or because of differences in specific specialties queried (e.g., dentistry). A longitudinal retrospective study in France by Soussand and colleagues similarly reported a 45% decrease in care activities to treat rare diseases during the early months of the pandemic [8]. They reported that telehealth usage dramatically increased but only compensated for 1/3 of the decrease in care activities for those with rare diseases [8].
While telehealth certainly facilitated access to care for some study participants, the 36.4% of participants who experienced delays but did not access telehealth services indicates that telehealth alone was insufficient to fill gaps in access to care at the beginning of the pandemic. This may have been due to delays in the establishment of telehealth services by providers or issues regarding insurance coverage of telehealth visits. Furthermore, the nearly 72% of individuals in our study who reported experiencing delays in care is significantly higher than the national estimates of all patients experiencing delays, which range from 20 to 48% [16, 17]. This may, in part, be due to the many medical services commonly utilized by individuals with OI. According to the OI Foundation, the medical team for individuals with OI might include “a primary care doctor, orthopedists, endocrinologists, geneticists, rehabilitation specialists, neurologists, and pulmonologists,” in addition to physical and occupational therapists [17].
This survey did not explicitly ask about participant experiences seeking mental healthcare during the pandemic, but several participants reported feeling an increase in their anxiety and depression in free text responses, with one participant even reporting receiving a new diagnosis of depression. Studies suggest that people with OI may have increased baseline depression and anxiety, in part due to fear of falling and fracture beginning at a young age [19]. These findings support that the provision of mental healthcare for individuals with OI should be an ongoing priority, in addition to ongoing research efforts [20].
While this study benefited from a large number of participants, especially for a study of a rare disease, it also had several key limitations. As a cross-sectional study with no identifiable participant information, it was impossible to assess change in access to care over time or temporal change in any other variables. In particular, given that the survey was initially distributed in August of 2020, only 4 months following the onset of the pandemic, it is possible that some individuals had not yet experienced delays in direct care or utilized telehealth services at this time point, even if they went on to do so further into the pandemic. Furthermore, since the median interval between bisphosphonate infusions was 6 months, some participants may not have experienced delays or symptoms because they had not yet been due for their next infusion. In other longitudinal studies, for example, the percentage of participants who reported experiencing delays in care increased from 63 to 72% over the course of the first year of the pandemic, and telehealth utilization increased from 52 to 74% [14]. Finally, the survey did not ask about socioeconomic status, which may create an additional barrier to accessing care, particularly via telehealth.
These results indicate that, overall, individuals with OI were able to receive the majority of their medical care during the early pandemic period. Patients and providers adapted to the ever-changing circumstances, often offering telehealth services when in-person appointments were limited or deemed unsafe. Further research should continue to focus on the impact of delays in care, as health outcomes, especially adverse outcomes, are unlikely to manifest immediately following delays in care. There is also an ongoing need for increased access to care, especially within treatment modalities that may not effectively translate to telehealth (e.g., aquatic therapy, dental, and surgery). Furthermore, laws enacted at the beginning of the pandemic to enable increased access to telehealth are now undergoing modification/elimination, and both providers and policymakers should remain mindful of the effects of decreasing access to telehealth, particularly for individuals with rare diseases for whom components of healthcare may be more susceptible to limitations in accessibility. As methods for care diversify and evolve, it is essential that the needs of those with OI and other complex chronic conditions are recognized and prioritized.
Supplementary Material
Acknowledgements
The authors wish to acknowledge the OI Foundation and OI healthcare providers who assisted with distributing the survey link to participants.
Funding
This study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (TL1TR002382, UL1TR002378) (Wu) to Emory University and Cystic Fibrosis Foundation (WU21Q0) (Wu), (WU20D0) (Wu). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Cystic Fibrosis Foundation.
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s11657-023-01355-2.
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee (Emory University Institutional Review Board) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Emory University Institutional Review Board determined formal consent was not required for this study.
Conflicts of interest Author JCF has served as a paid consultant for Orthofix Inc. and Nuvasive Specialized Orthopaedics. Authors SNM, KJL, and MW declare that they have no conflict of interest.
Data availability
Data are available upon request to the corresponding author.
References
- 1.Rauch F, Glorieux FH (2004) Osteogenesis imperfecta. The Lancet 363(9418):1377–1385. 10.1016/S0140-6736(04)16051-0 [DOI] [PubMed] [Google Scholar]
- 2.Tournis S, Dede AD (2018) Osteogenesis imperfecta–a clinical update. Metabolism 80:27–37. 10.1016/j.metabol.2017.06.001 [DOI] [PubMed] [Google Scholar]
- 3.Sillence DO, Senn A, Danks DM (1979) Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 16(2):101. 10.1136/jmg.16.2.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Osteogenesis Imperfecta (OI) (2023). https://my.clevelandclinic.org/health/diseases/15807-osteogenesis-imperfecta-oi. Accessed 4 Aug 2023
- 5.Hidalgo Perea S, Green DW (2021) Osteogenesis imperfecta:treatment and surgical management. Curr Opin Pediatr 33(1):74–48. 10.1097/MOP.0000000000000968 [DOI] [PubMed] [Google Scholar]
- 6.Aktas P (2021) Chronic and rare disease patients’ access to healthcare services during a health crisis: the example of the COVID-19 pandemic in Turkey. Health Expect 24(5):1812–1820. 10.1111/hex.13321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Papautsky EL, Rice DR, Ghoneima H, McKowen ALW, Anderson N, Wootton AR et al. (2021) Characterizing health care delays and interruptions in the United States during the COVID-19 pandemic: internet-based, cross-sectional survey study. J Med Internet Res 23(5):e25446. 10.2196/25446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soussand L, Kuchenbuch M, Messiaen C, Sandrin A, Jannot AS, Nabbout R (2022) Impact of the COVID-19 pandemic on the care of rare and undiagnosed diseases patients in France: a longitudinal population-based study. Orphanet J Rare Dis 17(1):430. 10.1186/s13023-022-02580-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sokas C, Kelly M, Sheu C, Song J, Welch HG, Bergmark R et al. (2021) Cancer in the shadow of COVID: early-stage breast and prostate cancer patient perspectives on surgical delays due to COVID-19. Ann Surg Oncol 28(13):8688–8696. 10.1245/s10434-021-10319-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Luca P, Bisogno A, Colacurcio V, Marra P, Cassandro C, Camaioni A et al. (2022) Diagnosis and treatment delay of head and neck cancers during COVID-19 era in a tertiary care academic hospital: what should we expect? Eur Arch Otorhinolaryngol 279(2):961–965. 10.1007/s00405-021-06834-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee DID, Vanderhout S, Aglipay M, Birken CS, Morris SK, Piché-Renaud PP et al. (2022) Delay in childhood vaccinations during the COVID-19 pandemic. Can J Public Health 113(1):126–134. 10.17269/s41997-021-00601-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nutt S, Limb L (2011) Survey of patients’ and families’ experiences of rare diseases reinforces calls for a rare disease strategy. Soc Care Neurodisability 2(4):195–199. 10.1108/20420911111188443 [DOI] [Google Scholar]
- 13.Halley MC, Stanley T, Maturi J, Goldenberg AJ, Bernstein JA, Wheeler MT et al. (2021) “It seems like COVID-19 now is the only disease present on Earth”: living with a rare or undiagnosed disease during the COVID-19 pandemic. Genet Med 23(5):837–844. 10.1038/s41436-020-01069-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smyth D, Hytiris M, Kelday C, McDonnell C, Burren C, Gardner A et al. (2022) Patient-reported experience of clinical care of osteogenesis imperfecta (OI) during the COVID-19 pandemic.Front Public Health 10:951569. 10.3389/fpubh.2022.951569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Findling MG, Blendon RJ, Benson JM (2020) Delayed care with harmful health consequences—reported experiences from national surveys during coronavirus disease 2019. JAMA Health Forum 1(12):e201463–e. 10.1001/jamahealthforum.2020.1463 [DOI] [PubMed] [Google Scholar]
- 16.Atherly A, Van Den Broek-Altenburg E, Hart V, Gleason K, Carney J (2020) Consumer reported care deferrals due to the COVID-19 pandemic, and the role and potential of telemedicine: crosssectional analysis. JMIR Public Health Surveill 6(3):e21607. 10.2196/21607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.About OI (2023). https://oif.org/informationcenter/about-oi/. Accessed 1 Aug 2023
- 18.Swezey T, Reeve BB, Hart TS, Floor MK, Dollar CM, Gillies AP et al. (2019) Incorporating the patient perspective in the study of rare bone disease: insights from the osteogenesis imperfecta community. Osteoporos Int 30(2):507–511. 10.1007/s00198-018-4690-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mc Donald D, Mc Donnell T, Martin-Grace J, Mc Manus G, Crowley RK (2023) Systematic review of health related-quality of life in adults with osteogenesis imperfecta. Orphanet J Rare Dis 18(1):36. 10.1186/s13023-023-02643-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United States Regions (2023). https://education.nationalgeographic.org/resource/united-states-regions/. Accessed 1 Aug 2023
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon request to the corresponding author.


