Abstract
Solid tumours often endure nutrient insufficiency during progression. How tumour cells adapt to temporal and spatial nutrient insufficiency remains unclear. We previously identified STC2 as one of the most upregulated genes in cells exposed to nutrient insufficiency by transcriptome screening, indicating the potential of STC2 in cellular adaptation to nutrient insufficiency. However, the molecular mechanisms underlying STC2 induction by nutrient insufficiency and subsequent adaptation remain elusive. Here, we report that STC2 protein is dramatically increased and secreted into the culture media by Gln-/Glc-deprivation. STC2 promoter contains cis-elements that are activated by ATF4 and p65/RelA, two transcription factors activated by a variety of cellular stress. Biologically, STC2 induction and secretion promote cell survival but attenuate cell proliferation during nutrient insufficiency, thus switching the priority of cancer cells from proliferation to survival. Loss of STC2 impairs tumour growth by inducing both apoptosis and necrosis in mouse xenografts. Mechanistically, under nutrient insufficient conditions, cells have increased levels of reactive oxygen species (ROS), and lack of STC2 further elevates ROS levels that lead to increased apoptosis. RNA-Seq analyses reveal STC2 induction suppresses the expression of monoamine oxidase B (MAOB), a mitochondrial membrane enzyme that produces ROS. Moreover, a negative correlation between STC2 and MAOB levels is also identified in human tumour samples. Importantly, the administration of recombinant STC2 to the culture media effectively suppresses MAOB expression as well as apoptosis, suggesting STC2 functions in an autocrine/paracrine manner. Taken together, our findings indicate that nutrient insufficiency induces STC2 expression, which in turn governs the adaptation of cancer cells to nutrient insufficiency through the maintenance of redox homeostasis, highlighting the potential of STC2 as a therapeutic target for cancer treatment.
Keywords: nutrient insufficiency, stanniocalcin 2, reactive oxygen species, monoamine oxidase B, tumour progression
Introduction
The major characteristics of tumour metabolism include the Warburg effect, active glutaminolysis and hypoxia1, 2, 3; as such, tumour cells have increased demand of glucose (Glc), glutamine (Gln) and oxygen to keep cell survival and proliferation4, 5, 6. However, solid tumours often have poor circulation that leads to insufficient supply of Glc, Gln and oxygen; therefore, to investigate the mechanisms of how tumour cells respond to nutrient insufficiency could provide promising therapeutic targets. Our previous study identified Stanniocalcin 2 (STC2) as one of the most upregulated genes upon Gln-/Glc- deprivation and hypoxia exposure1, 7, suggesting a critical role of STC2 in cellular response to nutrient insufficiency.
STC2 belongs to the secreted glycoprotein hormone family that was reported to lower intracellular calcium concentrations by attenuating Ca2+ influx8, 9. Under physiological conditions, STC2 is highly expressed in skeletal muscle, heart, testis and pancreas8, 10; while under pathological conditions, STC2 is upregulated in a plethora of human tumours, including hepatocellular carcinoma (HCC), cervical cancer, nasopharyngeal carcinoma, colorectal cancer, gastric cancer, esophageal squamous cell carcinoma, prostate cancer, renal cell carcinoma, etc.7, 8, 11, 12. Increased STC2 levels are strongly correlated with tumour development, progression and poor prognosis for most human tumours except breast cancer13.
The expression of STC2 is regulated at both transcriptional and post-transcriptional levels, particularly under stress conditions including ER stress, hypoxia, nutrient insufficiency and radiation-mediated stress1, 7, 8, 11, 14. Biologically, STC2 is involved in many biological processes in human tumours, such as cell survival, proliferation, migration and immune escape8, 15, 16, 17. However, the precise mechanisms underlying the stress-induced STC2 induction remain unclear.
Previous reports reveal hydrogen peroxide (H2O2) induces STC2 expression, and loss of STC2 impairs the tolerability of cells to oxidative stress18, 19, 20, suggesting a potential mechanism that links nutrient insufficiency to STC2 induction, redox homeostasis and cellular adaption. Current understanding is that aberrant metabolic activities of tumour cells result in an elevation of reactive oxygen species (ROS)21. Low to moderate levels of ROS may serve as a signaling mechanism to maintain cellular physiology; increased levels of ROS facilitate tumorigenesis by causing genetic alteration and oncogenic transformation; however, long-term and/or excessive ROS may trigger apoptosis22. In general, the glutathione (GSH) and nicotinamide adenine dinucleotide phosphate (NADPH) systems work coordinatively to maintain intracellular redox homeostasis23, 24. As for tumour cell metabolism, Gln serves as the major source of glutamate that functions as an important substrate for de novo GSH biosynthesis; hence, Gln-deprivation results in decreased GSH levels and ROS accumulation25, 26. Glc insufficiency may trigger oxidative stress via impaired NADPH production, because Glc is the substrate for pentose phosphate pathway, the major pathway to generate NADPH27. Moreover, hypoxia impairs the electron transport chain (ETC) activity and also enhances ROS production28, 29. Therefore, a deprivation of each of these major nutrients may trigger oxidative stress, and cells must overcome the oxidative stress to maintain survival. A better understanding of how STC2 regulates the adaptation of tumour cells to nutrient insufficiency and associated oxidative stress may provide new therapeutic targets.
In this study, we first confirm that STC2 protein is induced and secreted into the culture media by nutrient insufficiency. We next present data to define the cis-elements in the STC2 promoter that physically interact with activating transcription factor 4 (ATF4) and nuclear factor-kappa B p65 (p65/RelA) during nutrient insufficiency. We show that STC2 induction inhibits apoptosis but attenuates tumour cell proliferation during nutrient insufficiency. In addition, loss of STC2 leads to elevated ROS levels accompanied by apoptosis during nutrient insufficiency. We finally show that STC2 induction suppresses the expression of monoamine oxidase B (MAOB), a mitochondrial membrane-associated enzyme that produces ROS, and the administration of recombinant human STC2 to culture media is sufficient to suppress MAOB expression. Taken together, our findings indicate that STC2 serves as a key regulator of redox homeostasis that governs the survival of tumour cells during nutrient insufficiency.
Materials and methods
Ethical approval
Animal studies were performed according to the protocol approved by the Laboratory Animal Ethic Committee at the Tianjin Medical University Cancer Institute & Hospital (TUMCIH) (#: AE-2022036). This study has complied with all relevant ethical regulations for animal experiments. All efforts were made to minimize the numbers and suffering of experimental animals.
Human HCC tissue microarray (TMA) was purchased from the Shanghai Outdo Biotechnology (China) with an Internal Review Board approval (YB M-05–02). The clinical samples (23 HCC specimens) were collected from the Department of Pathology at the TMUCIH from January 1st 2018 to December 31st 2018. All patients were provided with informed consent and the study was conducted according to a protocol approved by the Internal Review Board at the TMUCIH (bc2021308).
Cell culture
Hep3B, HeLa, MCF-7, SK-BR-3, MDA-MB-453, MDA-MB-468 and HEK293T (ATCC) cells were maintained in DMEM with 10% fetal bovine serum (FBS) supplemented with Pen/Strep. All cells were cultured in a humidified incubator at 37 °C with 5% CO2. MM01 cells were established through extended culture of Hep3B cells in Gln-free DMEM supplemented with 10% dialyzed FBS (Atlantic Biologicals, dialyzed 10 kDa), 0.8 mM ammonia and Pen/Strep30. The culture media for MM01 cells were changed every 2 days and the cells were passed once reaching ~ 90% confluency. All cells were tested routinely to ensure mycoplasma-free using Polymerase Chain Reaction (PCR) methods.
Tumour xenografts
The NTG and athymic nude, nu/nu mice were purchased from SPF Biotechnology Co. (Beijing, China). For Hep3B xenografts, 24 NTG mice (male, age: 4 weeks old) were randomly allocated into three groups (6 per group). For HeLa xenografts, 24 athymic nude, nu/nu mice (female, age: 4 weeks old) were randomly allocated into three groups (six per group). In general, 5×106 Hep3B or HeLa cells were subcutaneously injected into each side of both flank regions. The xenografts were measured every three days to the completion of experiments. The growth curves were plotted with tumour sizes (calculated using the formula VT =0.5 × L × W2, mm3). After euthanization, dissected xenografts were weighted and recorded for further analysis. The mice were euthanized if the xenograft size became ≥ 20 mm in the long diameter, and the mice died prior to the completion of experiments were excluded for analysis.
Statistical analysis
Statistical analyses were performed using SPSS 27.0 software (IBM SPSS Statistics). The results of qRT-PCR, tumour weight, IHC staining score, and luciferase analysis were presented as average ± standard deviation; student t test or one-way ANOVA was performed to compare these results. The curves for cell proliferation and xenograft growth were compared using two-way ANOVA. Linear correlation was assessed using Spearman’s correlation analysis. Survival analysis was performed using the Log Rank test to estimate the survival probability, and p-value less than 0.05 was set as statistically significant.
Results
Nutrient insufficiency triggers STC2 induction and secretion
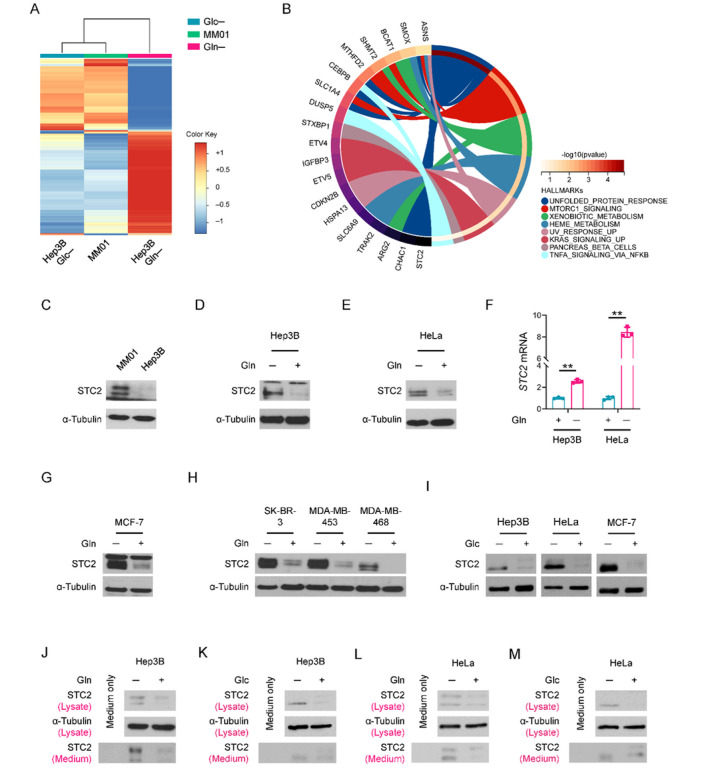
In previous work, we cultured Hep3B cells for long term in Gln-free media supplemented with NH4+ as an alternative nitrogen source and established a long-term Gln-deprived cell line, MM01, which maintains a slow proliferation phenotype30. In addition, we cultured Hep3B cells in Gln-/Glc- free media for short terms that served as a model for acute nutrient insufficiency. cDNA microarray analysis revealed that STC2 was among the most upregulated 58 genes shared by cells enduring acute Gln-/Glc- deprivation as well as long-term Gln-deprived condition (Fig. 1A,B & S1A), indicating the potential of STC2 in mediating cellular adaptation to nutrient insufficiency. Further functional analyses suggested that most of these 58 genes were related to amino acid metabolism (Fig. S1B & Supplementary Table 1). Moreover, our prior study found STC2 was also upregulated by hypoxia7, suggesting STC2 induction is a common phenomenon when tumour cells exposed to nutrient insufficiency. In accordance, elevated STC2 protein levels were confirmed in MM01 cells relative to that in Hep3B cells (Fig. 1C), and STC2 was remarkably induced by acute Gln-deprivation (Fig. 1D–F & S1C), whereas re-supplementation with Gln rapidly suppressed STC2 expression (Fig. S1D). Similar results were observed when Gln was added back to MM01 cells (Fig. S1E). To address whether STC2 upregulation is a common phenomenon in different tumour types enduring nutrient insufficiency, we exposed breast cancer cells to Gln-deprivation as well. We observed that STC2 was similarly induced in MCF-7, SK-BR-3, MDA-MB-453 and MDA-MB-468 cells by Gln-free media (Fig. 1G,H). In consistent with the cDNA microarray, Glc-deprivation also increased STC2 protein levels (Fig. 1I).
Figure 1.
STC2 is upregulated under nutrient insufficient conditions. A The iDEP analysis was performed to compare the cDNA microarray data from cells cultured with Gln-/Glc- deprived media. A total of 5,783 genes are up-/down- regulated according to the criteria | log2(fold changes) | ≥ 1. B Circos plot shows the biological functions of the 58 most upregulated genes in cells exposed to nutrient insufficiency. STC2 is among the 58 most upregulated genes in MM01 cells and Gln-/Glc- deprived Hep3B cells. C–E STC2 is induced in MM01 cells (C), Hep3B (D) and HeLa (E) cells cultured in Gln-free media. F STC2 mRNA is induced by Gln-deprivation in Hep3B and HeLa cells. Data are shown as the mean ± SD; **, p<0.01, n=3. G, H STC2 is upregulated in human breast cancer cells when exposed to Gln-deprivation. IGlc-deprivation also upregulates STC2 in Hep3B, HeLa and MCF-7 cells. Note the loss of the high molecular weight band of STC2 in Glc-deprived cells (represents glycosylated STC2, unpublished data). J–M Nutrient insufficiency upregulates intracellular STC2 and its secretion into culture media. Both Hep3B and HeLa cells were cultured in Gln-free (J, L) or Glc-free (K, M) media, and the cell lysate and culture media were collected and analysed by Western blots.
To test whether STC2 is induced by the lack of Gln itself or by a lack of metabolic derivatives of Gln, we administered the glutaminase inhibitor, DON, to Hep3B cells. We observed that DON treatment efficiently induced STC2 expression in Gln-rich media (Fig. S1F,G), indicating that lack of Gln-derived metabolites is sufficient to trigger STC2 induction as well. As an inhibitor of protein secretion, BFA increased intracellular STC2 levels while decreased STC2 levels in the culture media (Fig. S1H), con rming STC2 as a secreted protein. To address whether increased STC2 levels in cells is the result of secretion inhibition, we analysed STC2 levels in cell lysate and their corresponding culture media. We observed that increased STC2 levels in both cell lysate and culture media in a proportional manner upon Gln-/Glc- deprivation, suggesting that increased intracellular STC2 levels are not a consequence of secretion inhibition (Fig. 1J–M). Taken together, these data suggest that nutrient insufficiency triggers STC2 induction and secretion, which represents a converging consequence in response to different nutrient insufficient conditions.
ATF4 and p65/RelA transcriptionally induce STC2 expression during nutrient insufficiency
Our previous studies indicated that STC2 mRNA levels were increased in cells under Gln-/Glc- deprived or hypoxic conditions1, 8, suggesting STC2 is transcriptionally upregulated by nutrient insufficiency. To further delineate the underlying mechanisms, we used ActD and CHX to block gene transcription and protein translation, respectively. ActD and CHX blocked STC2 expression at both mRNA and protein levels (Fig. S2A,B), demonstrating that STC2 transcription depends on de novo synthesis of a transcription factor. Additionally, to address whether Gln-deprivation affects STC2 protein stability, we performed CHX chase assay and found that after CHX treatment, STC2 showed a similar decay rate regardless of Gln levels (Fig. S2C,D), ruling out the possibility that Gln-deprivation stabilizes STC2 protein.
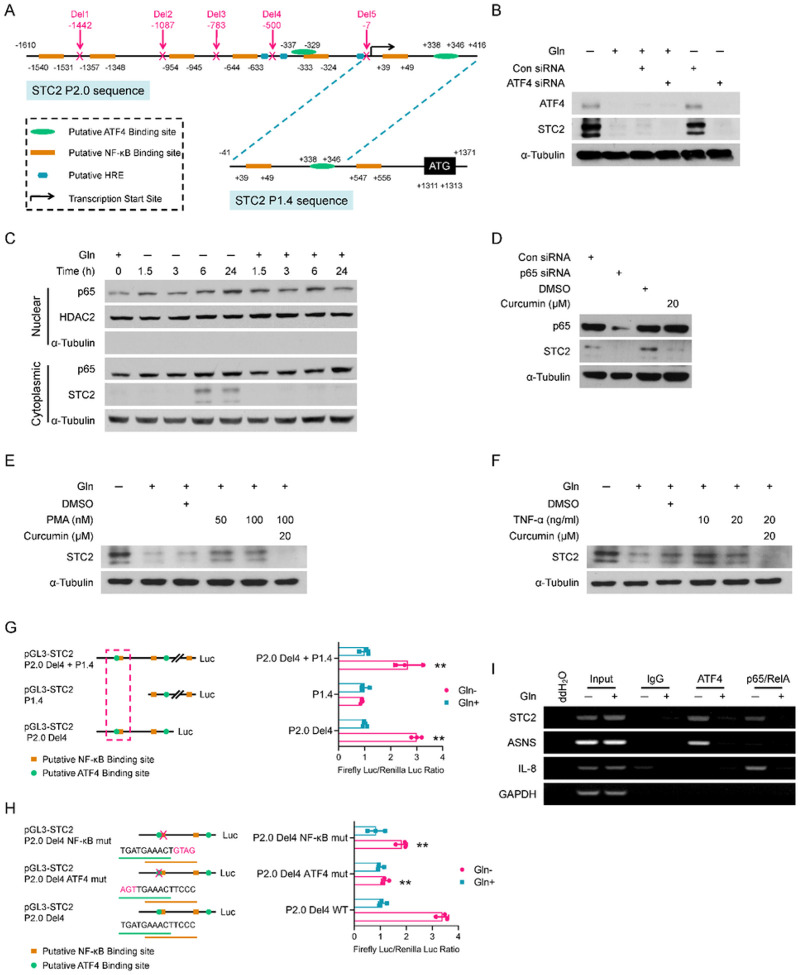
STC2 was reported to be induced by ER stress that is correlated with ATF4 activation. ATF4 is an important component of the integrated stress response system. Amino acid insufficiency leads to the accumulation of non-aminoacylated tRNAs, which promotes the activation of general control non-derepressible-2 (GCN2) and the phosphorylation of eIF2α, thereafter triggering the selective translation of ATF431, 32. To determine whether STC2 gene is a direct transcription target of ATF4, we performed bioinformatic analysis and found STC2 promoter contains multiple copies of putative ATF4, NF-κB and HIF-1 binding sites (HRE) (Fig. 2A). Next, we confirmed that Gln-deprivation enhanced eIF2α phosphorylation and ATF4 induction in our experimental setting (Fig. S2E,F). In addition, ATF4 knockdown effectively abolished STC2 induction in cells cultured in Gln-free media (Fig. 2B). Indeed, ER stress inducers like MG132 which blocks proteosome-dependent degradation of proteins or BFA which suppresses protein secretory pathway also induced STC2 expression; while ActD or CHX effectively blocked this induction (Fig. S2G–J), suggesting ER stress triggered STC2 induction also depends on de novo transcription and translation. Finally, glutaminase inhibitor, DON or Glc-deprivation also induced co-upregulation of ATF4 and STC2 (Fig. S2K,L).
Figure 2.
STC2 is transcriptionally upregulated by ATF4 and NF-κB. A Bioinformatic analysis suggests the presence of putative ATF4, NF-κB and HRE binding sites in STC2 promoter. B ATF4 knockdown abolishes STC2 induction upon Gln-deprivation. C p65/RelA is translocated into the nuclei in cells exposed to Gln-free media. D p65 knockdown or inhibition by curcumin effectively suppresses STC2 induction upon Gln-deprivation. E, F Curcumin effectively suppresses STC2 induction by the NF-κB signaling activators PMA (E) and TNF-α (F). G Luciferase reporter assays confirm the binding sites (located at nt[−337~−329] and nt[−333~−324] of STC2 promoter [NCBI Ref. #, NC_000005.10]) are required for STC2 induction by Gln-deprivation. H Mutation of either ATF4 or NF-κB binding sites impairs the response of STC2 promoter to Gln-deprivation. Data in Panels G & H are shown as the mean ± SD; **, p<0.01, n=3. I ChIP assays substantiates the direct binding of ATF4 or p65/RelA to the identified cis-elements on STC2 promoter. ASNS serves as a positive control for ATF4; IL-8 is used as a positive control for p65/RelA; GAPDH is used as a negative control.
In consistence with the existence of putative NF-κB binding sites in the STC2 promoter, GSEA analyses highlighted the upregulation of NF-κB targets under Gln-insufficient conditions (Fig. S3A & Supplementary Table 2). To evaluate the role of NF-κB in STC2 induction, we performed cell fractionation analysis and observed that Gln-deprivation triggered p65/RelA accumulation in the nuclear fraction (Fig. 2C), demonstrating the activation of p65/RelA signaling in Gln-deprived cells. Next, we applied chemical inhibitors or activators to test the importance of p65/RelA in mediating STC2 expression upon Gln-deprivation. We observed that NF-κB inhibitors, BAY11–7082 or curcumin, efficiently blocked STC2 upregulation (Fig. S3B–G). Furthermore, genetically suppressing p65/RelA by siRNA or IκBαSR attenuated STC2 induction by Gln-deprivation (Fig. 2D & S3H). On the other hand, broadly used NF-κB activators, PMA or TNF-α, induced STC2 that could be blocked by curcumin (Fig. 2E,F). Taken together, these data demonstrate that p65/RelA functions as another transcription activator for STC2 induction.
To define the cis-elements that regulate STC2 expression in response to Gln-deprivation, we cloned two promoter fragments into the pGL3-Luciferase reporter with a length of 2026bp (P2.0) and 1412bp (P1.4), respectively (Fig. 2A). Guided by the identified putative binding sites, a series of deletions were constructed and cloned into the pGL3-Luciferase reporter. Luciferase assays indicated a DNA region included in STC2-P2.0 but not in STC2-P1.4 is responsive to Gln-/Glc- deprivation or hypoxia (Fig. S4A–C). Further deletion assays narrowed down to Deletion4 (Del4) region that is indispensable for the response of STC2 promoter to nutrient insufficiency (Fig. 2G & S4D). Mutation of either ATF4 or NF-κB binding sites in this region decreased the stress response (Fig. 2H & S4E), further confirming that these binding sites are functionally important in regulating STC2 induction. Finally, ChIP assays confirmed the direct binding of ATF4 and p65/RelA to this region of STC2 promoter (Fig. 2I).
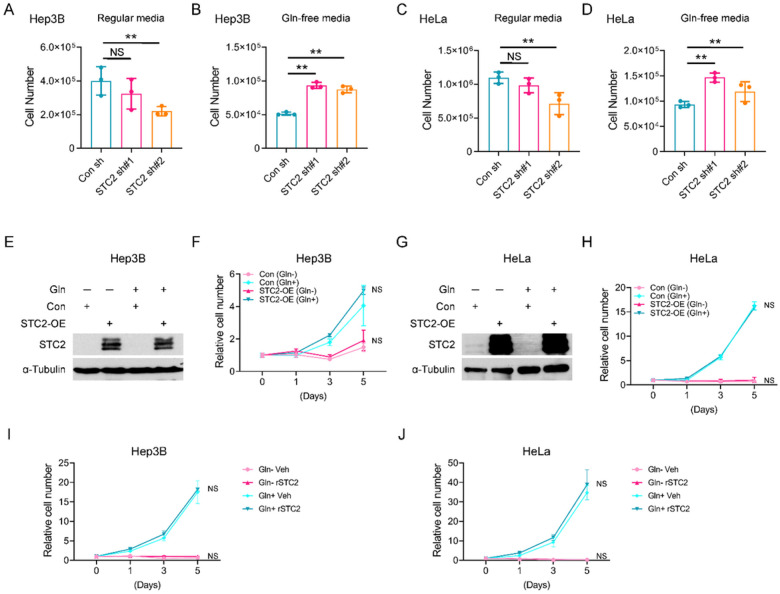
STC2 induction compromises tumour cell proliferation under nutrient insufficient conditions
Our previous study revealed that Gln-/Glc- deprivation caused cell cycle arrest, hence attenuating cell proliferation1. Since STC2 is induced by nutrient insufficiency, it is intriguing to investigate the role of STC2 in regulating cell proliferation under such conditions. We next focused on Gln-deprivation as a model to investigate the role of STC2 in regulating cell proliferation. In regular media, STC2 knockdown impaired the optimal proliferation of Hep3B and HeLa cells (Fig. 3A,C), while in Gln-free media, STC2 knockdown cells showed higher proliferation rates (Fig. 3B,D), indicating that basal levels of STC2 are required to maintain the optimal proliferation when cells cultured in nutrient rich media, whereas under nutrient insufficient conditions, elevated STC2 levels can suppress cell proliferation. Interestingly, overexpression of STC2 did not affect cell proliferation of cells cultured in either regular media or nutrient insufficient media (Fig. 3E–H). Furthermore, supplementing exogenous recombinant STC2 (rSTC2) to media didn’t affect cell proliferation under either conditions (Fig. 3I,J). Taken together, these data demonstrate that basal levels of STC2 are required to support cell proliferation under nutrient rich conditions; while endogenous STC2 gene can be induced by nutrient insufficiency, thereby attenuating cell proliferation and facilitating cellular adaptation to stress conditions.
Figure 3.
STC2 is required for optimal cell proliferation in normal culture media, but negatively regulates cell proliferation upon Gln-deprivation. A, B STC2 is needed for optimal proliferation of Hep3B cells in regular media (A) but suppresses cell proliferation in Gln-free media (B). C, D STC2 is needed for optimal proliferation of HeLa cells in regular media (C) but suppresses cell proliferation in Gln-free media (D). E–H Overexpression of STC2 has no apparent effects on the proliferation of Hep3B (E & F) and HeLa (G & H) cells. I, J Exogenous rSTC2 doesn’t affect the proliferation of Hep3B (I) and HeLa (J) cells. All data are shown as the mean ± SD; **, p<0.01; NS, not significant, n=3–6.
STC2 induction and secretion promote tumour cell survival during nutrient insufficiency
One common consequence of nutrient insufficiency and associated metabolic stress is apoptosis. We next focused on Gln-deprivation as a model to investigate whether STC2 induction played a role in maintaining cell survival during nutrient insufficiency. Western blot revealed STC2 knockdown increased PARP cleavage, a biomarker of apoptosis, under Gln-deprived conditions (Fig. 4A,B). In accordance, flow cytometry analysis also supported that cells with STC2 knockdown were more sensitive to apoptosis triggered by Gln-deprivation (Fig. 4C,D). On the other hand, overexpression of STC2 decreased apoptosis of cells exposed to Gln-free media (Fig. 4E–H). As a secretory protein, STC2 has been proposed to function as a signaling molecule or to function intracellularly as a calcium regulator9. To test whether STC2 protects cells from apoptosis triggered by Gln-deprivation in an autocrine/paracrine manner, we added rSTC2 to cell culture media and found that rSTC2 efficiently suppressed PARP cleavage as well as apoptosis of cells cultured in Gln-free media (Fig. 4I,J & S5). These data support that STC2 may function in an autocrine/paracrine manner to promote cell survival under nutrient insufficient conditions.
Figure 4.
STC2 reduces apoptosis of cells under Gln-deprived conditions. A, B STC2 knockdown leads to increased PARP cleavage in Hep3B (A) and HeLa (B) cells in Gln-deprived media. C, D Flow cytometry analyses show increased apoptosis in Hep3B (C) and HeLa (D) cells as assayed by Annexin V staining. E, F Overexpression of STC2 suppresses PARP cleavage in Hep3B (E) and HeLa (F) cells cultured with Gln-free media. G, H Flow cytometry analysis indicates overexpression of STC2 inhibits apoptosis of Hep3B (G) and HeLa (H) cells cultured in Gln-deprived media as measured by Annexin V staining. I, J rSTC2 effectively decreases STC2 knockdown-triggered PARP cleavage in Hep3B (I) and HeLa (J) cells cultured in Gln-free media.
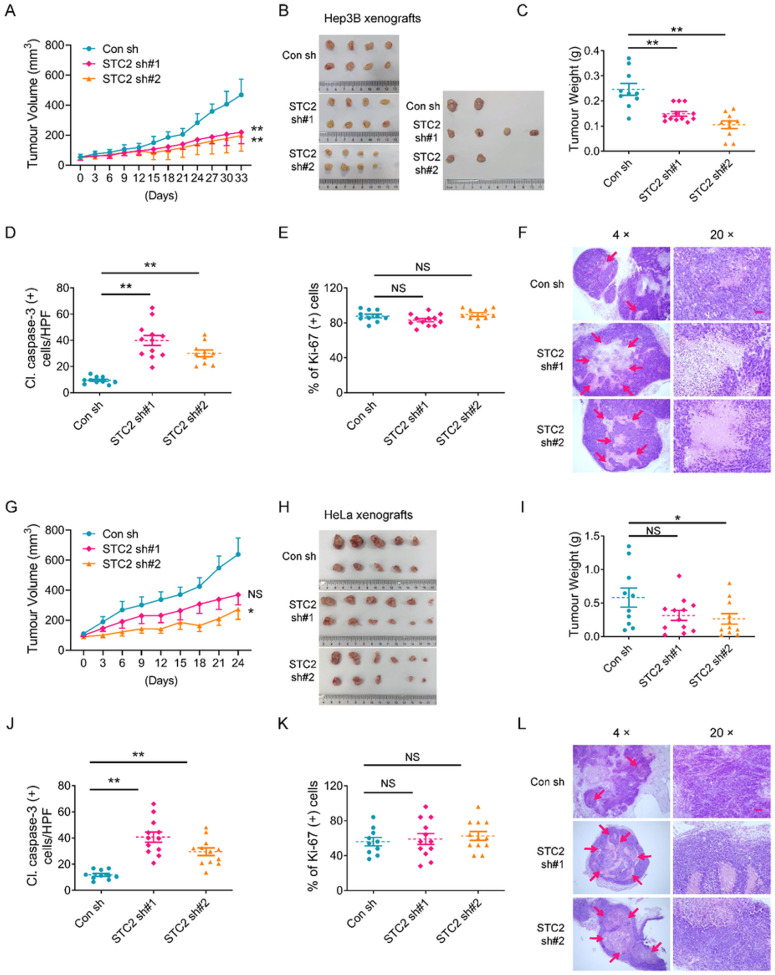
STC2 knockdown retards the growth of mouse xenografts
To evaluate the role of STC2 in a physiological context, we first run a large-scale Kaplan-Meier Plotter analyses and found that elevated STC2 levels were associated with poor prognosis in patients with a variety of tumours including HCC, cervical squamous cell carcinoma, thymoma, esophageal squamous cell carcinoma, renal papillary cell carcinoma, stomach adenocarcinoma, sarcoma, head and neck squamous cell carcinoma, bladder cancer and lung squamous cell carcinoma (Fig. S6). To confirm the role of STC2 induction in tumour progression in vivo, we established mouse xenografts by injecting 5×106 Hep3B or HeLa cells transfected with STC2 knockdown or control shRNAs independently. We found that STC2 knockdown tumours grew slower than control ones (Fig. 5A,B,G,H). Moreover, STC2 knockdown xenografts overall had lighter tumour weights compared to control counterparts (Fig. 5C,I). To further determine the role of STC2 in cell survival and proliferation in vivo, we examined the expression of cleaved caspase-3 and Ki-67 in the dissected xenografts by IHC staining as markers of apoptosis and proliferation, respectively. We found that loss of STC2 led to increased caspase-3 cleavage, suggesting STC2 induction is a favourable factor for cell survival in vivo (Fig. 5D,J & S7A), while there was no obvious difference in cell proliferation rates evaluated by Ki-67 IHC staining (Fig. 5E,K & S7B). More importantly, larger necrotic areas were observed in STC2 knockdown xenografts compared to control ones (Fig. 5F,L), suggesting a failed adaptation to insufficient blood supply during tumour progression, which is consistent with a previous report that STC2 was involved in tumour angiogenesis33. These data highlight that STC2 plays a critical role in preventing cell death during tumour progression in vivo.
Figure 5.
STC2 knockdown retards the growth of mouse xenografts. A STC2 knockdown slows down the growth of Hep3B xenografts. B The photographs of Hep3B tumour xenografts shown in the same scale. C Loss of STC2 reduces the tumour weight of Hep3B xenografts. D STC2 knockdown causes increased apoptosis (indicated by caspase-3 cleavage) in Hep3B xenografts. E STC2 knockdown did not affect cell proliferation rates in Hep3B xenografts as detected by Ki-67 IHC staining. F Loss of STC2 leads to increased necrosis in Hep3B xenografts. Red arrow, necrotic area. G STC2 knockdown slows down the growth of HeLa xenografts. H The photographs of HeLa tumour xenografts. I Loss of STC2 reduces the tumour weight of HeLa xenografts. JSTC2 knockdown causes increased apoptosis in HeLa xenografts indicated by caspase-3 cleavage. K STC2 knockdown doesn’t affect cell proliferation rates in HeLa xenografts evaluated by Ki-67 IHC staining. L Loss of STC2 leads to increased necrosis in HeLa xenografts. Red arrow, necrotic area. The representative IHC staining results in Panels D, E, J & K are put in Figure S7. All data are shown as the mean ± SD; *, p<0.05; **, p<0.01; NS, not significant; n=10–12. Scale bar, 50 mm.
STC2 knockdown results in ROS elevation in cells under nutrient insufficient conditions
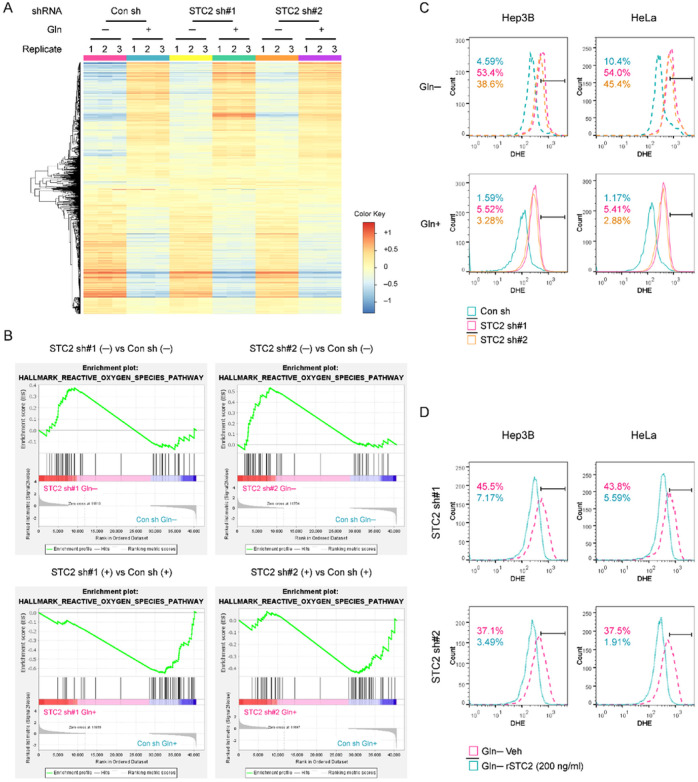
Next, we asked how STC2 protects tumour cells from nutrient insufficiency-induced apoptosis. To address this question, we first performed RNA-Seq analysis to search for alterations of signaling pathways in STC2 knockdown versus control cells cultured in Gln-free media (Fig. 6A). The analysis of the RNA-Seq data identified an alteration of genes related to “hallmark gene sets” (Fig. S8); particularly, both shRNAs targeting STC2 resulted in an elevation of genes related to redox homeostasis under Gln-deprived conditions (Fig. 6B). We next determined how STC2 status affected ROS levels in cells exposed to Gln-deprivation. Using dihydroethidium (DHE) staining combined with flow cytometry analyses, we observed that Gln-deprivation moderately increased ROS levels, and STC2 knockdown significantly intensified ROS accumulation (Fig. 6C). Moreover, the administration of rSTC2 to culture media obviously decreased ROS levels in STC2 knockdown cells (Fig. 6D). Taken together, these data indicate that STC2 induction and secretion are required to ameliorate ROS elevation triggered by nutrient insufficiency.
Figure 6.
STC2 knockdown alters the expression signature of genes participating in redox homeostasis and increases ROS levels in cells cultured in Gln-deprived media. A iDEP analysis shows the RNA-Seq data in STC2 knockdown versus control cells. This analysis was performed to identify the altered signaling pathways in STC2 knockdown cells in Gln-free media. B GSEA analysis highlights the enrichment of genes related to redox homeostasis in STC2 knockdown cells exposed to Gln-free media. C After dihydroethidium (DHE) staining, flow cytometry analyses were performed and the results indicate that Gln-deprivation increases ROS levels in both Hep3B and HeLa cells and STC2 knockdown further increases ROS levels. D rSTC2 treatment reduces ROS levels in Hep3B and HeLa cells in Gln-free media. The numbers in Panels C & D indicate the percentage of cells with elevated ROS levels.
STC2 knockdown leads to MAOB dysregulation and redox imbalance during nutrient insufficiency
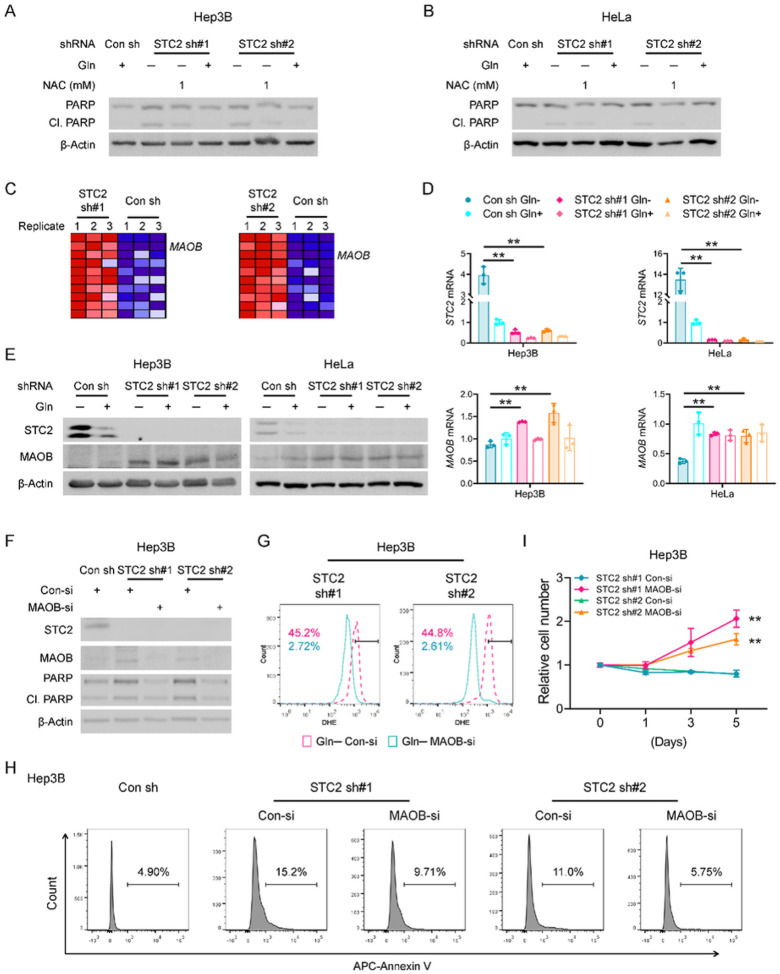
To confirm a causative relationship between ROS accumulation and apoptosis in our experimental model, we administered NAC, an ROS scavenger, to STC2 knockdown cells. Not surprisingly, NAC suppressed apoptosis of STC2 knockdown cells enduring Gln-deprivation (Fig. 7A,B & S5), indicating increased ROS is a bona fide mediator of apoptosis in our experimental setting. To explore the molecular mechanism underlying the protective effects of STC2 in response to nutrient insufficiency, we mined the RNA-Seq data and found MAOB, a mitochondrial membrane associated enzyme that directly participates in ROS production, was among the genes most upregulated by STC2 knockdown (Fig. 7C & Supplementary Table 3). Subsequent qRT-PCR and western blot assays further demonstrated that STC2 knockdown increased MAOB expression under Gln-deprived conditions (Fig. 7D,E & S9A), whereas we didn’t detect significant alteration of other genes related to ROS generation in two independent STC2 knockdown cell lines; particularly, no signal was detected for NADPH oxidase (NOX) family genes in both STC2 knockdown cell lines (Fig. S9B–E).
Figure 7.
Loss of STC2 leads to MAOB dysregulation and redox imbalance when exposed to Gln-free media. A, B ROS scavenger NAC decreases PARP cleavage in Hep3B (A) and HeLa (B) cells in Gln-free media. C Blue-Pink O’ Gram in the Space of the analysed Gene Set, the comparison of redox metabolic genes between STC2 knockdown and control cells cultured in Gln-free media. MAOB is one of the genes most significantly upregulated in STC2 knockdown cells. Detailed genes are listed in Supplementary Table 3. D qRT-PCR validates the upregulation of MAOBmRNA in STC2 knockdown Hep3B and HeLa cells cultured in Gln-free media. Data are shown as the mean ± SD; **, p<0.01; n=3. E Western blot confirms that MAOB levels are higher in STC2 knockdown Hep3B and HeLa cells cultured in Gln-free media. F MAOB knockdown reduces PARP cleavage in STC2 knockdown Hep3B cells cultured in Gln-free media. G MAOB knockdown decreases ROS levels in STC2 knockdown Hep3B cells in Gln-free media. The numbers indicate the percentage of cells with elevated ROS levels. H MAOB knockdown prevents Gln-deprivation-triggered apoptosis of STC2 knockdown Hep3B cells. I MAOB knockdown rescues the proliferation of STC2 knockdown Hep3B cells cultured in Gln-free media. Data are shown as the mean ± SD; **, p<0.01; n=4.
To further explore the regulatory relationship between STC2 and MAOB, we applied rSTC2 to cells with STC2 knockdown. We observed that rSTC2 effectively decreased MAOB expression in STC2 knockdown cells in Gln-free media (Fig. S10). To substantiate the biological importance of MAOB expression to ROS levels and cell survival, we used siRNA pool to knockdown MAOB, or specific inhibitors to suppress MAOB activity in STC2 knockdown cells. We observed that MAOB knockdown efficiently decreased ROS levels in STC2 knockdown cells cultured in Gln-free media (Fig. 7F,G & S11A,B). In addition, MAOB knockdown not only suppressed apoptosis but also rescued cell proliferation (Fig. 7H,I & S11C,D). To further evaluate whether MAOB is associated with STC2 loss, we employed two specific MAOB inhibitors, Rasagiline and Selegiline. Consistently, both inhibitors effectively attenuated ROS production and apoptosis in STC2 knockdown cells cultured in Gln-free media (Fig. S12A–D), thereby rescuing cell proliferation (Fig. S12E,F). Taken together, these findings indicate that under nutrient insufficient conditions, STC2 induction maintains redox homeostasis by suppressing MAOB expression, hence reducing intracellular ROS levels and maintaining cell survival.
The expression levels of STC2 and MAOB are negatively correlated, and elevated STC2 is associated with tumour progression in vivo
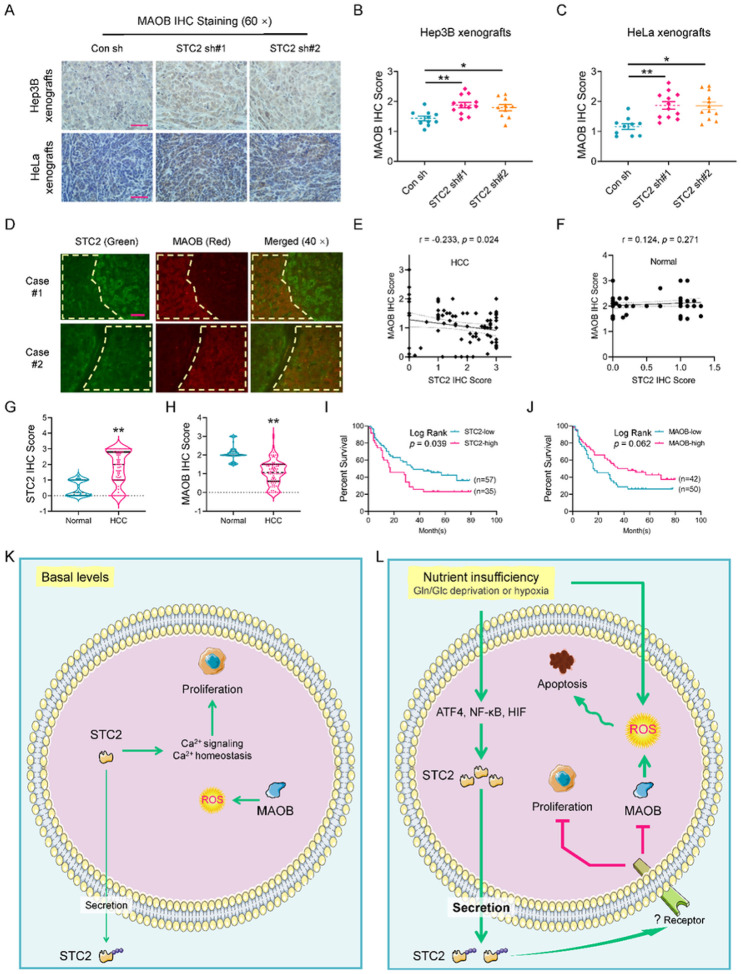
To address whether the observation in cell culture is relevant to tumour progression in vivo, we first performed IHC staining and confirmed the elevated expression of MAOB in STC2 knockdown xenografts (Fig. 8A–C). Furthermore, DepMap analyses suggested a reverse correlation between STC2 and MAOB expression in a series of human tumour cells (Fig. S13A). Other bioinformatic analyses also revealed a negative correlation between STC2 and MAOB expression in human tumours (Fig. S13B–F).
Figure 8.
The expression levels of STC2 and MAOB are negatively correlated, and elevated STC2 is associated with tumour progression. A Elevated MAOB levels are revealed in STC2 knockdown xenografts by IHC staining. Scale bar, 50 mm. B, C The xenografts from cells with STC2 knockdown show higher MAOB IHC staining score. All data are shown as the mean ± SD; *, p<0.05; **, p<0.01; n=10–12. D The immunofluorescent staining indicates the reverse correlation between STC2 (green) and MAOB (red) expression in HCC specimens. Yellow line encircled area with low STC2 expression but high MAOB levels. Scale bar, 50 mm. E, F TMA IHC staining reveals a reverse correlation between STC2 and MAOB expression in HCC but not normal samples. G, H Elevated STC2 (G) and decreased MAOB (H) levels are detected in human HCC versus normal samples. **, p<0.01. I, J High STC2 expression is significantly correlated with poor prognosis in patients with HCC. K, L Schematic illustration of the proposed role of STC2 signaling in tumour cell adaptation to nutrient insufficiency. Under normal conditions, basal levels of STC2 performs its biological functions mainly by affecting intracellular targets, for example, maintaining Ca2+ homeostasis to facilitate cell proliferation. Under nutrient insufficient conditions, stress-triggered ATF4 and NF-κB activation upregulates STC2 expression. STC2 is secreted out of the cells to function in an autocrine/paracrine manner to prevent apoptosis through the alleviation of oxidative stress and to conserve nutrients by attenuating cell proliferation.
To investigate the potential of using the reciprocal STC2-MAOB expression as a prognostic indicator, we first performed immunofluorescent staining to examine their expression correlation in human HCC specimens. In consistency with cell culture findings, we confirmed an obviously negative correlation between STC2 and MAOB levels in the same HCC samples (Fig. 8D). IHC staining also verified a reverse correlation between STC2 and MAOB expression in human HCC tissues but not in normal counterparts (Fig. 8E–H & S14). Importantly, clinicopathological analyses revealed that elevated STC2 expression was significantly associated with poor prognosis in patients with HCC, whereas increased MAOB levels were likely correlated with a favourable prognosis with a log-rank p value of 0.062 (Fig. 8I,J). Taken together, these data strongly indicate that STC2 negatively regulates MAOB expression via an un-characterized mechanism (Fig. 8K,L), and a combined analysis of both STC2 and MAOB levels is a potential approach in assessing the prognosis of patients with HCC.
Discussion
Rapid proliferation of tumour cells demands increased supply of nutrients to support proliferation and active biosynthesis, while defective blood vessel system often fails to support solid tumour cells with sufficient blood supply, leading to nutrient insufficiency and subsequently oxidative stress during tumour progression. Our previous study revealed that STC2 is one of the most upregulated genes under Gln-/Glc-deprived and hypoxic conditions1. With these data in context, our study focuses on addressing how STC2 is upregulated by nutrient insufficiency, and the biological roles of STC2 in the adaptation of tumour cells to nutrient insufficiency.
We presented data to conclude that ATF4 and p65/RelA are activated by nutrient insufficiency that in turn transactivates STC2 gene. Previous studies reported that STC2 was upregulated upon ATF4 activation8, 18, but it was unclear whether ATF4 directly transactivates STC2 gene, or indirectly regulates its expression. Our current study identifies the cis-elements of the STC2 gene and demonstrates that these elements are indispensable for STC2 induction upon nutrient deprivation. It is well known that eIF2α-ATF4 axis represents the core of an integrated stress response mechanism34. Under various stress conditions, cells utilize multiple kinases to phosphorylate eIF2α. Phosphorylation of eIF2α results in a global translation inhibition but a selective translation of stress related genes exemplified by ATF4. As a stress responsive transcription factor, ATF4 transcribes several functional groups of genes including ER chaperones that are involved in protein folding, ER-associated degradation of terminally damaged proteins, and apoptosis. In addition to ATF4, NF-κB is another transcription factor ubiquitously involved in cellular stress response. It was suggested that Gln-deprivation activated NF-kB signaling35. Consistent with that report, our findings demonstrate that p65/RelA, a member of NF-κB family, directly transactivates STC2 gene by a physical interaction with identified cis-elements upon activation. Considering NF-κB is activated by various cell injury, pathogen infection and inflammatory signaling, we deduce that STC2 could also be induced by a variety of stress including cell injury and inflammatory factors.
Elevated ROS is a common result of many cellular stress and disease status, and is a major contributor to oxidative stress imbalance. ROS is mainly generated in the mitochondria as a byproduct of oxidative phosphorylation, or in the cytosol from reactions catalyzed by oxidoreductases such as NOX36. To some extent, ROS possesses beneficial effects for tumour cells, driving cell proliferation, genetic instability and metastasis37. However, excessive and/or long-term ROS may lead to the damage of macromolecules, and eventually cell death. From the nutrient point of view, Gln and Glc play critical roles in the intracellular counter-oxidative stress processes25, 26. Gln is the direct precursor of glutamate; both Gln and glutamate play central roles as a nitrogen donor in the biosynthesis of non-essential amino acids including cysteine and glycine. Glutamate, cysteine and glycine are the direct substrates for GSH biosynthesis. Indeed, we observed that Gln-/Glc- deprivation altered the amino acid metabolic pathway (Fig. S1B), reflecting a feedback response to global amino acid insufficiency that directly impair the biosynthesis of GSH and possibly other antioxidants. Our data revealed that tumour cells exposed to Gln-free media have elevated ROS levels, and STC2 knockdown further increases ROS levels, suggesting that STC2 plays a role in maintaining redox homeostasis. RNA-Seq analyses also revealed that the change of ROS metabolic signature is one of the most affected pathways in STC2 knockdown cells upon Gln-deprivation, further providing additional evidence to our hypothesis.
Previous studies indicated a connection between oxidative stress and STC2 induction. For example, H2O2 treatment leads to STC2 upregulation, and loss of STC2 causes cell death when challenged with oxidative stress18, 19, 20. We note that a variety of cell stress, including nutrient insufficiency, may trigger oxidative stress and ER stress. Accordingly, as a primary or a secondary alteration, oxidative stress itself may be sufficient to independently activate ATF4 and NF-kB, hence upregulating STC2.
Whereas STC1 has been reported to regulate redox homeostasis by promoting the expression of uncoupling protein 2, thus compromising the ETC-related ROS production38, 39, our findings in this study suggest that STC2 utilizes a novel mechanism to maintain the cellular redox homeostasis during nutrient insufficiency, i.e., STC2 induction by nutrient insufficiency suppresses MAOB expression to decrease ROS production. MAOB belongs to the family of monoamine oxidase (MAO) enzymes that localize in the outer mitochondrial membrane to catalyze the oxidation of various monoamines.40. MAOB is mainly expressed in liver, heart, duodenum, lung and brain41. Under physiological conditions, there is a clear increase of MAOB expression in aging or inflammatory brains42, 43. The reaction catalyzed by MAOB is regarded as a source of H2O2 that is involved in ROS-mediated cellular injury in neurological and cardiac disorders44, 45, 46, 47. In consistent with these literatures, our data indicate that STC2 suppresses MAOB expression, whereas loss of STC2 leads to MAOB induction, which coincides with elevated ROS levels and cell death upon Gln-deprivation, highlighting the role of MAOB as a redox regulator during nutrient insufficiency. Therefore, although MAOB is not a major ROS producer in regular metabolism, its activity in ROS generation may serve as a critical regulator of the redox balance in cells enduring stress.
Besides its functions in catalyzing monoamine, it remains unclear whether MAOB directly affects the activity of ETC, the major source of ROS production. A previous study reported that MAOA, another member of the MAO family, is involved in regulating mitochondrial bioenergetics, and MAOA specific inhibitor, clorgyline, enhances mitochondrial ROS production at high concentrations by increasing cellular respiration48.
Importantly, this study found the administration of rSTC2 can efficiently block Gln-deprivation-induced apoptosis, suggesting STC2 may perform its biological functions in an autocrine/paracrine manner. Till now, the majority of investigations have focused on utilizing the genetically overexpressing systems to investigate the biological functions of STC2 to establish its role in regulating cell proliferation, migration, invasion and apoptosis8. But as a secreted glycoprotein, overexpression of STC2 leads to increased secretion when it has its own signal peptide (our unpublished data). Therefore, it’s unreasonable to simply attribute the biological effects of STC2 overexpression to its intracellular functions49. Our study found rSTC2 efficiently blocks MAOB induction, resulting in reduced ROS production and apoptosis under Gln-deprived conditions. These findings strongly suggest STC2 works in an autocrine/paracrine manner to regulate cellular processes. A recent study found the administration of rSTC2 promotes epithelial-mesenchymal transition by inducing the expression of snail family transcription repressor 2 and matrix metalloproteinases16. Recently, several clinicopathological studies have identified serum STC2 levels are elevated in patients with HCC, gastric cancer and colorectal cancer, and particularly high serum STC2 levels are associated with poor prognosis20, 50, 51, 52, indicating secreted STC2 could perform its biological functions through an endocrine mechanism at organism levels. It has been reported that the cation-independent mannose-6-phosphate receptor/IGF2R interacts with STC1 and may serve as a receptor53. Whether STC2 shares the same receptor or uses a different surface protein as a receptor remains to be investigated.
Although a plethora of clinicopathological investigations indicate that STC2 expression is correlated with tumour size, disease stage and prognosis of various human tumours that is also demonstrated by the bioinformatic analyses of the TCGA data in our study8, it remains unclear how STC2 induction could biologically benefit tumour growth. This study provides new insights into our understanding of the role of STC2: serving as a critical regulator to coordinate cell survival and proliferation under nutrient insufficient conditions. Specifically, STC2 is required to support optimal cell proliferation under normal conditions, indicating basal levels of intracellular STC2 facilitate cell proliferation, which might be attributed to its function in maintaining intracellular calcium homeostasis (Fig. 8K,L). Under nutrient insufficient conditions, STC2 slows down cell proliferation that might be more beneficial for tumour cells by allocating limited resources to fulfill their basic demands, such as maintaining cell survival. A potential explanation might be that various types of cellular stress triggers STC2 induction and secretion into the culture media; and the secreted STC2 serves as a ligand to activate downstream signaling, which subsequently slows down cell proliferation (Fig. 8K,L). Therefore, STC2 serves as a switch of cell priority: under normal conditions, basal levels of STC2 facilitate maintaining normal cell biology and functions; under stress conditions, STC2 is upregulated and secreted, thereby triggering a stress response that shifts cellular priority to survival.
In summary, as a secreted glycoprotein, STC2 is quickly and remarkably transactivated by ATF4 and p65/RelA in cells enduring nutrient insufficiency. As a signaling molecule, secreted STC2 functions as a ligand in an autocrine/paracrine manner to promote cell survival by alleviating oxidative stress. One possible mechanism is that STC2 suppresses MAOB expression at transcriptional level, thus decreasing ROS production. Although the receptor of STC2 and its downstream signaling remain to be dissected, our current findings support a model that STC2 switches cancer cells’ priority from proliferation to survival, hence facilitating cellular adaptation to nutrient insufficiency. Therefore, STC2 can be regarded as a prognostic biomarker and a promising therapeutic target for cancer treatment.
ACKNOWLEDGEMENTS
The authors thank Drs. J. Jiang and E. Fisher (Drexel University) for their kind assistance in flow cytometry analysis. The authors also thank Dr. F. Elefant for helpful discussion in chromatin immunoprecipitation assay.
FUNDING
This work is supported by the grant R01-CA129494 (N.S.) from NIH/NCI and a research contract fund from Lipogen (N.S.), the National Natural Science Foundation of China (S.Q., 82373360), the Tianjin Municipal Education Commission Key Project Program (S.Q., 2022ZD065), the Tianjin Medical University Cancer Institute and Hospital Talent Program and Start-up Grant for Doctors (S.Q., B2102), the Start-up funding from the Tianjin Medical University Cancer Institute and Hospital (S.Q., 2021-1-7), and the Tianjin Key Medical Discipline (Pathology) Construction Project (TJYXZDXK-012A).
Funding Statement
This work is supported by the grant R01-CA129494 (N.S.) from NIH/NCI and a research contract fund from Lipogen (N.S.), the National Natural Science Foundation of China (S.Q., 82373360), the Tianjin Municipal Education Commission Key Project Program (S.Q., 2022ZD065), the Tianjin Medical University Cancer Institute and Hospital Talent Program and Start-up Grant for Doctors (S.Q., B2102), the Start-up funding from the Tianjin Medical University Cancer Institute and Hospital (S.Q., 2021-1-7), and the Tianjin Key Medical Discipline (Pathology) Construction Project (TJYXZDXK-012A).
Footnotes
COMPETING INTERESTS
The authors declare no competing interests.
ETHICS STATEMENT
The protocol was approved by the Laboratory Animal Ethic Committee at the Tianjin Medical University Cancer Institute & Hospital (TUMCIH) (#: AE-2022036). This study has complied with all relevant ethical regulations for animal experiments. Every effort was made to minimize the numbers and suffering of the included animals.
Human HCC tissue microarray (TMA) was purchased from the Shanghai Outdo Biotechnology with an Internal Review Board approval (YB M-05–02). Twenty-three cases of HCC specimens were also collected from the Department of Pathology at the TMUCIH. The inpatient time was from January 1st 2018 to December 31st 2018. All patients provided informed consent and this study was conducted according to the guidelines of the Internal Review Board at the TMUCIH (bc2021308).
ADDITIONAL INFORMATION
The online version contains Supplementary information available at
Supplementary Files
Contributor Information
Shuo Qie, Tianjin Medical University Cancer Institute and Hospital.
Haijuan Xiong, Tianjin Medical University Cancer Institute and Hospital.
Yaqi Liu, Tianjin Medical University Cancer Institute and Hospital.
Chenhui Yan, Tianjin Medical University Cancer Institute and Hospital.
Yalei Wang, Tianjin Tumor Hospital.
Lifeng Tian, Kimmel Cancer Center, Thomas Jefferson University.
Chenguang Wang, Kimmel Cancer Center, Thomas Jefferson University.
Nianli Sang, Drexel University.
DATA AVAILABILITY
All datasets generated are included in the maintext and its Supplementary Information files. Additional data are available from the corresponding authors upon reasonable request.
References
- 1.Qie S, Liang D, Yin C, Gu W, Meng M, Wang C, et al. Glutamine depletion and glucose depletion trigger growth inhibition via distinctive gene expression reprogramming. Cell Cycle 2012, 11(19): 3679–3690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qie S, Chu C, Li W, Wang C, Sang N. ErbB2 activation upregulates glutaminase 1 expression which promotes breast cancer cell proliferation. J Cell Biochem 2014, 115(3): 498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qie S, Yoshida A, Parnham S, Oleinik N, Beeson GC, Beeson CC, et al. Targeting glutamine-addiction and overcoming CDK4/6 inhibitor resistance in human esophageal squamous cell carcinoma. Nat Commun 2019, 10(1): 1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qie S, Diehl JA. Glutamine addiction: an Achilles heel in esophageal cancers with dysregulation of CDK4/6. Mol Cell Oncol 2019, 6(4): 1610257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qie S, He D, Sang N. Overview of Glutamine Dependency and Metabolic Rescue Protocols. Methods Mol Biol 2019, 1928: 427–439. [DOI] [PubMed] [Google Scholar]
- 6.Wu S, Fukumoto T, Lin J, Nacarelli T, Wang Y, Ong D, et al. Targeting glutamine dependence through GLS1 inhibition suppresses ARID1A-inactivated clear cell ovarian carcinoma. Nat Cancer 2021, 2(2): 189–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He H, Qie S, Guo Q, Chen S, Zou C, Lu T, et al. Stanniocalcin 2 (STC2) expression promotes post-radiation survival, migration and invasion of nasopharyngeal carcinoma cells. Cancer Manag Res 2019, 11: 6411–6424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qie S, Sang N. Stanniocalcin 2 (STC2): a universal tumour biomarker and a potential therapeutical target. J Exp Clin Cancer Res 2022, 41(1): 161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zeiger W, Ito D, Swetlik C, Oh-hora M, Villereal ML, Thinakaran G. Stanniocalcin 2 is a negative modulator of store-operated calcium entry. Mol Cell Biol 2011, 31(18): 3710–3722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hernandez Cordero AI, Gonzales NM, Parker CC, Sokolof G, Vandenbergh DJ, Cheng R, et al. Genome-wide Associations Reveal Human-Mouse Genetic Convergence and Modifiers of Myogenesis, CPNE1 and STC2. Am J Hum Genet 2019, 105(6): 1222–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin S, Guo Q, Wen J, Li C, Lin J, Cui X, et al. Survival analyses correlate stanniocalcin 2 overexpression to poor prognosis of nasopharyngeal carcinomas. J Exp Clin Cancer Res 2014, 33: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bu Q, Deng Y, Wang Q, Deng R, Hu S, Pei Z, et al. STC2 is a potential biomarker of hepatocellular carcinoma with its expression being upregulated in Nrf1alpha-deficient cells, but downregulated in Nrf2-deficient cells. Int J Biol Macromol 2023, 253(Pt 8): 127575. [DOI] [PubMed] [Google Scholar]
- 13.Chatterji S, Krzoska E, Thoroughgood CW, Saganty J, Liu P, Elsberger B, et al. Defining genomic, transcriptomic, proteomic, epigenetic, and phenotypic biomarkers with prognostic capability in male breast cancer: a systematic review. Lancet Oncol 2023, 24(2): e74–e85. [DOI] [PubMed] [Google Scholar]
- 14.Jiang K, Yin X, Zhang Q, Yin J, Tang Q, Xu M, et al. STC2 activates PRMT5 to induce radioresistance through DNA damage repair and ferroptosis pathways in esophageal squamous cell carcinoma. Redox Biol 2023, 60: 102626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhong Q, Chu H, Wang G, Zhang C, Li R, Guo F, et al. Structural insights into the covalent regulation of PAPP-A activity by proMBP and STC2. Cell Discov 2022, 8(1): 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yun EJ, Kim D, Hsieh JT, Baek ST. Stanniocalcin 2 drives malignant transformation of human glioblastoma cells by targeting SNAI2 and Matrix Metalloproteinases. Cell Death Discov 2022, 8(1): 308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen X, Liu Q, Huang W, Cai C, Xia W, Peng Y, et al. Stanniocalcin-2 contributes to mesenchymal stromal cells attenuating murine contact hypersensitivity mainly via reducing CD8(+) Tc1 cells. Cell Death Dis 2018, 9(5): 548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ito D, Walker JR, Thompson CS, Moroz I, Lin W, Veselits ML, et al. Characterization of stanniocalcin 2, a novel target of the mammalian unfolded protein response with cytoprotective properties. Mol Cell Biol 2004, 24(21): 9456–9469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joshi AD, Carter DE, Harper TA, Jr., Elferink CJ. Aryl hydrocarbon receptor-dependent stanniocalcin 2 induction by cinnabarinic acid provides cytoprotection against endoplasmic reticulum and oxidative stress. J Pharmacol Exp Ther 2015, 353(1): 201–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang FY, Wong DK, Mak LY, Cheung TT, Seto WK, Yuen MF. Hepatitis B virus X protein promotes hepatocarcinogenesis via the activation of HMGA2/STC2 signaling to counteract oxidative stress-induced cell death. Carcinogenesis 2022, 43(7): 671–681. [DOI] [PubMed] [Google Scholar]
- 21.Sies H, Belousov VV, Chandel NS, Davies MJ, Jones DP, Mann GE, et al. Defining roles of specific reactive oxygen species (ROS) in cell biology and physiology. Nat Rev Mol Cell Biol 2022, 23(7): 499–515. [DOI] [PubMed] [Google Scholar]
- 22.Badgley MA, Kremer DM, Maurer HC, DelGiorno KE, Lee HJ, Purohit V, et al. Cysteine depletion induces pancreatic tumor ferroptosis in mice. Science 2020, 368(6486): 85–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Son J, Lyssiotis CA, Ying H, Wang X, Hua S, Ligorio M, et al. Glutamine supports pancreatic cancer growth through a KRAS-regulated metabolic pathway. Nature 2013, 496(7443): 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hayes JD, Dinkova-Kostova AT, Tew KD. Oxidative Stress in Cancer. Cancer Cell 2020, 38(2): 167–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang B, Zhang J, Zhao G, Liu M, Hu J, Lin F, et al. Filamentous GLS1 promotes ROS-induced apoptosis upon glutamine deprivation via insufficient asparagine synthesis. Mol Cell 2022, 82(10): 1821–1835. [DOI] [PubMed] [Google Scholar]
- 26.Li M, Thorne RF, Shi R, Zhang XD, Li J, Li J, et al. DDIT3 Directs a Dual Mechanism to Balance Glycolysis and Oxidative Phosphorylation during Glutamine Deprivation. Adv Sci (Weinh) 2021, 8(11): e2003732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang C, Li B. Maintaining proton homeostasis is an essential role of the Warburg effect in proliferating cells. Cancer Biol Med 2019, 16(3): 391–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee P, Chandel NS, Simon MC. Cellular adaptation to hypoxia through hypoxia inducible factors and beyond. Nat Rev Mol Cell Biol 2020, 21(5): 268–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martinez-Reyes I, Diebold LP, Kong H, Schieber M, Huang H, Hensley CT, et al. TCA Cycle and Mitochondrial Membrane Potential Are Necessary for Diverse Biological Functions. Mol Cell 2016, 61(2): 199–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meng M, Chen S, Lao T, Liang D, Sang N. Nitrogen anabolism underlies the importance of glutaminolysis in proliferating cells. Cell Cycle 2010, 9(19): 3921–3932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bader DA, Hartig SM, Putluri V, Foley C, Hamilton MP, Smith EA, et al. Mitochondrial pyruvate import is a metabolic vulnerability in androgen receptor-driven prostate cancer. Nat Metab 2019, 1(1): 70–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tameire F, Verginadis II, Leli NM, Polte C, Conn CS, Ojha R, et al. ATF4 couples MYC-dependent translational activity to bioenergetic demands during tumour progression. Nat Cell Biol 2019, 21(7): 889–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Law AY, Wong CK. Stanniocalcin-1 and −2 promote angiogenic sprouting in HUVECs via VEGF/VEGFR2 and angiopoietin signaling pathways. Mol Cell Endocrinol 2013, 374(1–2): 73–81. [DOI] [PubMed] [Google Scholar]
- 34.Kartha N, Gianopulos JE, Schrank Z, Cavender SM, Dobersch S, Kynnap BD, et al. Sirtuin 6 is required for the integrated stress response and resistance to inhibition of transcriptional cyclin-dependent kinases. Sci Transl Med 2023, 15(694): eabn9674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bobrovnikova-Marjon EV, Marjon PL, Barbash O, Jagt DLV, Abcouwer SF. Expression of angiogenic factors vascular endothelial growth factor and interleukin-8/CXCL8 is highly responsive to ambient glutamine availability: Role of nuclear Factor-kappa B and activating protein-1. Cancer Research 2004, 64(14): 4858–4869. [DOI] [PubMed] [Google Scholar]
- 36.Kong H, Reczek CR, McElroy GS, Steinert EM, Wang T, Sabatini DM, et al. Metabolic determinants of cellular fitness dependent on mitochondrial reactive oxygen species. Sci Adv 2020, 6(45): eabb7272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kong N, Zhang H, Feng C, Liu C, Xiao Y, Zhang X, et al. Arsenene-mediated multiple independently targeted reactive oxygen species burst for cancer therapy. Nat Commun 2021, 12(1): 4777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ohkouchi S, Block GJ, Katsha AM, Kanehira M, Ebina M, Kikuchi T, et al. Mesenchymal stromal cells protect cancer cells from ROS-induced apoptosis and enhance the Warburg effect by secreting STC1. Mol Ther 2012, 20(2): 417–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ono M, Ohkouchi S, Kanehira M, Tode N, Kobayashi M, Ebina M, et al. Mesenchymal stem cells correct inappropriate epithelial-mesenchyme relation in pulmonary fibrosis using stanniocalcin-1. Mol Ther 2015, 23(3): 549–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tripathi RKP, Ayyannan SR. Monoamine oxidase-B inhibitors as potential neurotherapeutic agents: An overview and update. Med Res Rev 2019, 39(5): 1603–1706. [DOI] [PubMed] [Google Scholar]
- 41.Costa-Machado LF, Garcia-Dominguez E, McIntyre RL, Lopez-Aceituno JL, Ballesteros-Gonzalez A, Tapia-Gonzalez A, et al. Peripheral modulation of antidepressant targets MAO-B and GABAAR by harmol induces mitohormesis and delays aging in preclinical models. Nat Commun 2023, 14(1): 2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Clarke LE, Liddelow SA, Chakraborty C, Munch AE, Heiman M, Barres BA. Normal aging induces A1-like astrocyte reactivity. Proc Natl Acad Sci U S A 2018, 115(8): E1896–E1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Park JH, Ju YH, Choi JW, Song HJ, Jang BK, Woo J, et al. Newly developed reversible MAO-B inhibitor circumvents the shortcomings of irreversible inhibitors in Alzheimer’s disease. Sci Adv 2019, 5(3): eaav0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaludercic N, Carpi A, Nagayama T, Sivakumaran V, Zhu G, Lai EW, et al. Monoamine oxidase B prompts mitochondrial and cardiac dysfunction in pressure overloaded hearts. Antioxid Redox Signal 2014, 20(2): 267–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu Z, Xia Y, Wang Z, Su Kang S, Lei K, Liu X, et al. C/EBPbeta/delta-secretase signaling mediates Parkinson’s disease pathogenesis via regulating transcription and proteolytic cleavage of alpha-synuclein and MAOB. Mol Psychiatry 2021, 26(2): 568–585. [DOI] [PubMed] [Google Scholar]
- 46.Gabilondo AM, Hostalot C, Garibi JM, Meana JJ, Callado LF. Monoamine oxidase B activity is increased in human gliomas. Neurochem Int 2008, 52(1–2): 230–234. [DOI] [PubMed] [Google Scholar]
- 47.Yang YC, Chien MH, Lai TC, Su CY, Jan YH, Hsiao M, et al. Monoamine Oxidase B Expression Correlates with a Poor Prognosis in Colorectal Cancer Patients and Is Significantly Associated with Epithelial-to-Mesenchymal Transition-Related Gene Signatures. Int J Mol Sci 2020, 21(8): 2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kalimon OJ, Vekaria HJ, Gerhardt GA, Sullivan PG. Inhibition of monoamine oxidase-a increases respiration in isolated mouse cortical mitochondria. Exp Neurol 2023, 363: 114356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jepsen MR, Kloverpris S, Mikkelsen JH, Pedersen JH, Fuchtbauer EM, Laursen LS, et al. Stanniocalcin-2 inhibits mammalian growth by proteolytic inhibition of the insulin-like growth factor axis. J Biol Chem 2015, 290(6): 3430–3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu Z, Cheng H, Liu J, Zhang S, Zhang M, Liu F, et al. The Oncogenic and Diagnostic Potential of Stanniocalcin 2 in Hepatocellular Carcinoma. J Hepatocell Carcinoma 2022, 9: 141–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fang Z, Tian Z, Luo K, Song H, Yi J. Clinical significance of stanniocalcin expression in tissue and serum of gastric cancer patients. Chin J Cancer Res 2014, 26(5): 602–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li H, Zhou X, Zhang H, Jiang J, Fu H, Wang F. Combined Efficacy of CXCL5, STC2, and CHI3L1 in the Diagnosis of Colorectal Cancer. J Oncol 2022, 2022: 7271514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wan HT, Ng AH, Lee WK, Shi F, Wong CK. Identification and characterization of a membrane receptor that binds to human STC1. Life Sci Alliance 2022, 5(11): e202201497. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All datasets generated are included in the maintext and its Supplementary Information files. Additional data are available from the corresponding authors upon reasonable request.