Abstract
Pain and frailty are closely linked. Chronic pain is a risk factor for frailty, and frailty is a risk factor for pain. People living with frailty also commonly have cognitive impairment, which can make assessment of pain and monitoring of pain management even more difficult. Pain may be sub-optimally treated in people living with frailty, people living with cognitive impairment and those with both these factors. Reasons for sub-optimal treatment in these groups are pharmacological (increased drug side effects, drug–drug interactions, polypharmacy), non-pharmacological (erroneous beliefs about pain, ageism, bidirectional communication challenges), logistical (difficulty in accessing primary care practitioners and unaffordable cost of drugs), and, particularly in cognitive impairment, related to communication difficulties. Thorough assessment and characterisation of pain, related sensations, and their functional, emotional, and behavioural consequences (“phenotyping”) may help to enhance the assessment of pain, particularly in people with frailty and cognitive impairment, as this may help to identify who is most likely to respond to certain types of treatment. This paper discusses the potential role of “digital phenotyping” in the assessment and management of pain in people with frailty. Digital phenotyping is concerned with observable characteristics in digital form, such as those obtained from sensing-capable devices, and may provide novel and more informative data than existing clinical approaches regarding how pain manifests and how treatment strategies affect it. The processing of extensive digital and usual data may require powerful algorithms, but processing these data could lead to a better understanding of who is most likely to benefit from specific and targeted treatments.
Key Points
| Pain can be challenging to assess and treat in older people living with frailty. |
| Pain assessment can be improved by collecting more information about features associated with pain that can be observed (phenotyping). |
| Digital methods may add value to the phenotyping of pain and may improve care for older people living with frailty and pain. |
What Makes Pain in Frail Older Adults Special?
Pain is a problem regardless of age [1]. For a young, fit, and healthy person, chronic pain is often a considerable challenge that both diminishes and draws upon the individual’s mental and physical reserves. With increasing age, mental and physical reserves are further diminished due to the accumulation of comorbidities and age-related decline; this is called frailty [2]. Frailty is closely linked to cognitive impairment; the presence of frailty significantly increases the risk of developing cognitive impairment and dementia [3–5]. Cognitive impairment itself, whether associated with frailty or not, also diminishes an individual’s reserves, such as the ability to apply self-management strategies to reduce pain.
Chronic pain and frailty are linked [6]. Pain is more prevalent in people living with frailty compared to robust older people [7]. The relationship between chronic pain and frailty is bidirectional; pain predicts the development of frailty, and frailty predicts the development or worsening of pain [8–11]. Multiple different processes, behaviours, and exposures are likely to drive both these relationships, including the immune-inflammatory response to stress, dysregulation of endocrine and immune processes, and reduced physical activity [12–16]. Due to the overlap between pain and frailty, we have argued that chronic pain itself may be an under-appreciated indicator of the frailty state; tools to identify frailty tend to focus upon muscular functioning and rarely include pain [17].
Older people living with frailty may have pain from multiple sources and sites, occasionally without a formal clinical diagnosis or clear evidence of a causative pathology. This can challenge clinicians aiming to provide targeted, tailored interventions for pain. A thorough assessment and characterisation of pain, related sensations, and their functional, emotional, and behavioural consequences (“phenotyping”) may help to enhance the assessment of pain, particularly in the complex states seen in people with frailty and cognitive impairment. Phenotyping includes assessing the type, severity, and sites of pain, aggravating and relieving factors, and associated factors and behaviours, alongside imaging, laboratory, and sensory function testing. Phenotyping is distinguished from an approach that considers pain more simplistically and tends to result in people with different pain phenotypes being offered the same treatment [18, 19].
Digital phenotyping is concerned with observable characteristics in digital form, more specifically those that are obtained from sensing-capable devices and other sensors, and may present deeper and novel information, adding to existing clinical approaches [20, 21]. Digital phenotyping is defined as the use of moment-to-moment quantitative and descriptive data that are automatically generated (for example, heart rate, blood pressure, skin conductance, and movement) and collected by technological devices such as wearables, mobile devices, or video cameras [22, 23]. The outcomes of digital phenotyping we designate as “digital biomarkers”, which are meant to complement traditional biomarkers (for example, non-specific autonomic, behavioural, and reflex responses) and can shed light on individualised descriptions of the complex, nonlinear, and heterogenous processes specific to the human body.
In this paper, we elaborate the challenges of the management of chronic pain in people with frailty and, hence, the additional complexity of pain phenotyping in these people. We also introduce the concept of digital phenotyping and its potential additional value.
Challenges of Pain Management in Older People Living with Frailty
Reasons for undertreatment of pain in frail older people are summarised in Figure 1.
Fig. 1.
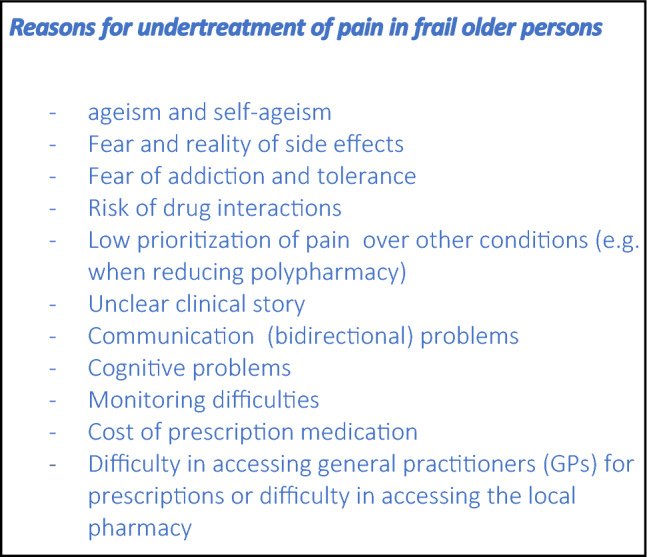
Reasons for undertreatment of pain in frail older people
Pharmacological Challenges
Pain is more than a nociceptive stimulus, and the way the pain is experienced, expressed, and understood is related to several biological, psychological, and social factors [24]. In most chronic pain management contexts, the first recommended line of treatment is with non-pharmacological interventions. These could include—but are not limited to—self-management strategies, maintenance of physical activity, and psychological therapies [25]. Pharmacological interventions can then follow if required. Non-pharmacological approaches should not be overlooked in acute pain contexts, such as the stabilisation of a fractured bone. In urgent and extreme cases, analgesic medication can be introduced alongside non-pharmacological interventions as first line.
Whilst older people living with frailty are most likely to receive medication because they often have multimorbidity, they are also the very people in whom drugs should be used with caution. This is primarily due to the fact that older people living with frailty are more vulnerable to drug side effects and more likely to suffer effects of polypharmacy [26]. Polypharmacy is the consumption of multiple medications, and is more common among older people, and especially those who live with frailty. This can potentiate the effect of undesirable side effects. In older people living with frailty, drug–drug interactions and cumulative effects such as anticholinergic burden are commonly encountered. An example of a drug–drug interaction is when buprenorphine is used concomitantly with antidepressants in people living with dementia, and can be poorly tolerated due to increased psychiatric and neurological side effects [27]. Moreover, many frequently prescribed drugs have weak anticholinergic properties that on their own are clinically not noticeable, but in polypharmacy, people may be taking several such drugs and the cumulative effect of them—the anticholinergic burden—can often be equivalent to the effect of a powerful anticholinergic drug. These concerns, in addition to concerns about age-related renal impairment, make clinicians wary of prescribing analgesics [28, 29].
Ageing-related changes in hepatic and renal function, muscle to fat ratios, and volumes of distribution will affect drug pharmacokinetics; the dose and interval of certain drugs may need to be adjusted accordingly. For example, after accounting for physiological changes, adjusted plasma concentrations of morphine in older people were similar to that of younger people [30]. However, adjusting doses and intervals to match each individual’s physiology is difficult to do because of the absence of sufficiently precise information about their physiological state, and dose adjustment can have an impact on drug effectiveness. Further, pharmacokinetic changes such as those a result of altered blood–brain permeability and pharmacodynamic changes such as altered target receptor density make the overall effectiveness of many drugs less predictable in older people than in younger people [31, 32].
A further challenge is a concern over the safety of long-term analgesic drug use, particularly where there is cognitive impairment [32]. A systematic review of trials in older people with dementia found sparse evidence for the tolerability of transdermal opioids, and also concluded that, although relatively safe, the risk of liver damage with long-term use of paracetamol was undetermined [33]. Both paracetamol and opioids are the most commonly used analgesic drugs used in older people, particularly in people living with dementia [34]. When considering whether to start or stop any of these drugs, these factors should be borne in mind.
Non-pharmacological Challenges
Non-pharmacological interventions for pain vary widely in type. This term refers to interventions to inform and educate patients or staff (typically about analgesic drug use), psychological interventions such as cognitive behavioural therapy, exercise, and sensory stimulation such as acupuncture [35–37]. The evidence for the efficacy of these interventions and in whom they are most effective is limited and unclear. One reason is that there is less research funding for such interventions compared to that for drugs. Further, people with frailty and those with cognitive impairment are often excluded from studies [38]. The lack of robust research makes it difficult for clinicians to advise such interventions, and their provision may be limited.
People living with frailty are also less likely to participate in active non-pharmacological pain management strategies that maintain normal function. They may see the onset of chronic pain as an inducement to become less active, believing that pain is an inevitable aspect of ageing. Older people often choose to adapt their daily living activities and stop doing previously valued activities altogether, findings that are explained in fear-avoidance models in chronic pain [39–41]. Clinicians may also encourage or impose this perspective on their patients. Older people living with frailty may also be less proactive and confident in trying new strategies and be reluctant to seek formal help [40, 42]. In addition, older people with cognitive impairment may experience apathy and a decreased ability to problem-solve, and the use of self-management strategies may be more difficult to carry out.
Ageism
Another important issue to account for in managing pain in older people is ageism and self-ageism. Although not all older people experience chronic pain, many people and older people themselves often believe that pain is a natural part of ageing [24]. This belief may lead the person to not complain or consult their clinician about pain, and is another important reason why pain in older people is not adequately assessed. There is evidence that this negative age stereotype and discrimination amongst older people is associated with lower intensity of analgesic management and increased development of chronic pain [43, 44]. Ageism is also present in many healthcare professionals, and may be overt or subconscious. Some healthcare professionals might stereotype older people as stoic, or be cognitively and perceptively impaired, with communication difficulties. They may conclude that these older people are unable to participate in pain management decisions [45, 46], thus impacting the care patients receive. Ageism is also endemic in drug licensing and medical research. Historically, eligibility for participation in clinical trials or for a drug often included arbitrary chronological age cut-offs. The evidence base for much of drug treatment may thus not apply well to current populations who are both older and have more comorbidities. These factors may affect how older people are offered, and make choices, about treatment options for pain.
Communication
A further challenging aspect of managing pain in the older person living with frailty can be communication. Communication challenges lead to suboptimal assessment of pain. When pain is not well assessed, its management will invariably be suboptimal [47]. Pain can be difficult to describe even in the absence of a communication deficit. Deafness, a common impairment in people living with frailty, makes history-taking more difficult, and yet a thorough assessment of pain is heavily dependent upon the history. This can often be largely overcome with training, time, and communication aids, but frequently, these are lacking [48]. Language or cultural differences between the patient and the clinician can make communication even more challenging. Multimorbidity may mean that patients have multiple different pains, in different sites, with different histories, aetiologies, and consequences. This adds to the challenge for patients when explaining their pain to a clinician.
Not only can it be difficult for the person with pain to express themselves, it is also difficult for the clinician to interpret and record what they hear. For example, a commonly used approach is to ask patients to provide a numerical value to their pain experience, but the validity of doing so has been challenged [49]. Multiple words can be substituted for pain (for example, soreness, hurt, stiffness), and a person may sometimes deny they are in pain but agree that they are sore. A narrative approach in which the patient is asked to tell their pain stories, with use of similes and metaphors, rather than posing direct questions, is likely to yield a better understanding of what pain is like for that older person, as well as how it impacts on their wellbeing [50]. However, this takes training, time, and patience to perform well.
People living with both frailty and cognitive impairment deserve special consideration. The presence of language and memory impairments makes it even more challenging to effectively communicate a complex pain experience or the effects of interventions. People living with cognitive impairment often have difficulty recalling the course of their pain or its relation to activities. They have trouble understanding and responding to self-report pain instruments, such as the numeric rating scale, visual analogue scale, or the verbal rating scale [51]. Where such deficits are marked, observational instruments that rely on non-verbal pain indicators such as vocalisations, body movements, and facial expressions are often used [52–54]. However, not all non-verbal pain indicators are specific for pain and may be expressions of distress due to unmet needs such as companionship or continence care. Further, implementation of these approaches into practice is inconsistent across hospital, community, and long-term care. There are also potential ethical issues. A person with cognitive impairment may not have the ability to understand the risks and benefits of treatment and weigh up these issues to come to an informed decision. There might also be a regular caregiver or advocate for the older person with cognitive impairment who can help in making decisions in the best interests of the patient, but they will have their own perspectives and potential biases, for example, about analgesic drugs, and these may influence how management decisions are made.
Phenotyping in Order to Enrich the Comprehensive Assessment of Pain
In reality, no matter how diligent the clinician is in history taking and how well pain is described, the mechanisms underlying an individual’s pain may be difficult to classify. Thus, the management of pain should not be focused solely on the direct aspects of pain (such as severity or site), but should also attend to understanding the complex psychosocial factors that are frequently associated with pain. These factors may sometimes be identified and measured (for example, depressive states or low mood), but the frequency, circumstances, and disease-specific states in which they occur in the context of pain are unclear. Pain management should include both sensory and emotional components, addressing problems experienced by the patient and also their caregivers and loved ones. Characterisation of observable, identifiable factors may provide discrete targets for intervention and improve overall pain management in older people living with frailty.
Phenotyping is defined as identifying observable characteristics of an organism, usually by means of biomarkers or other assessment outcomes, where specific aspects that make an individual more likely to respond to a certain treatment need to be identified in order for treatment to be most beneficial [55]. Phenotyping of pain can be done through clinical means: detailed analysis of pain quality and severity, associated symptoms, and identifiable features of non-verbal expressions or observable clinical signs that are specific for pain. In addition to clinical assessment, deep phenotyping of pain may be obtained using objective measures such as quantitative sensory testing and sensory profiling [19]. Psychosocial and sleep factors associated with pain are also core elements of pain phenotyping [56].
Digital Phenotyping in Frailty and Cognitive Impairment
Currently, digital phenotyping is a fertile front line of transdisciplinary research. New digital biomarkers are being designed through collaborative design and knowledge between engineering fields (computer or data science, systems engineering, applied mathematics) and clinical partners. Digital phenotyping may present new and valuable insight in older people living with frailty and cognitive impairment, which would overcome to some extent the recall and language required to express pain or functional impairment.
In practice, digital phenotyping implementation requires devices equipped with sensors to collect real-time data from the monitored person. The caregiver accessing these data would be able to estimate a longitudinal trajectory based on the digital biomarkers combined with other information, such as medication times, and then decide whether or not to change or continue with current treatment. Trajectories can then be measured that account for other factors such as diagnosis and context. This entire process allows for highly individualised longitudinal estimations to be made for the person receiving care in a timely manner.
For example, in Parkinson’s disease, research has been focused on designing wearable technology that documents gait and movement analysis in real time, to enable correlation with medication times and therefore a better understanding of treatment efficacy. This enables a more dynamic, temporal phenotyping of the movement disorder and identification of digital biomarkers to improve tracking of disease trajectories for clinical care and research [57]. Technology such as wearables and perhaps machine vision could give information from outside the clinical encounter. This could be helpful, for example, in revealing patterns and possible consequences in areas where the history is notoriously unrevealing, for example, sleep. This could augment the information available to clinicians in those with cognitive and memory impairment.
Digital Phenotyping in Pain
There remain few off-the-shelf solutions to estimate pain or precursors of pain using sensing devices specifically for groups marginalised by mainstream industry (for example, older people living with frailty) at the time of writing this article. However, international research efforts are dedicated to continuing to develop and validate these techniques for such groups [58–60].
Specific to pain, digital phenotyping might usefully supplement the limited information available in those with communication, language, or memory deficits. For instance, facial expressions and vocalisations could be picked up by facial expressions scanners and artificial intelligence utilising natural language processing algorithms. Abnormal or reduced movement and other physiological cues such as change in heart rate and respiratory rate may be sensed by wearable technology and flag up early physiological changes in the person with cognitive impairment [61]. Some examples of technology that could be used in the digital phenotyping of pain that might help are listed in Table 1.
Table 1:
Examples of monitoring technologies that could be used in digital phenotyping of pain
| Types of digital technology modalities | Examples of digital technology modalities and data types | Observable features | Potential uses for pain assessment and management |
|---|---|---|---|
| Actigraphy | Wearable devices (often wrist-worn), from commercial brands, e.g. Garmin, Polar, Apple, that calculate e.g. step counts, MET scores | Movement, GPS tracking, MET tracking, step count | Data relating to assessment of consequences of pain, pain patterns, guided training |
| Personal sensing | Wearable devices, mobile phones, sensors embedded in clothing or beds (e.g. pressure mats, socks, gloves, jewellery); these are often equipped with sensors for EDA, temperature, heart rate and heart rate variability; text, voice and video sensing for mobile phones and tablets | Physiological parameters such as heart rate, respiratory rate, sleep/awake patterns | Differentiation between acute and chronic pain based on change in physiology, pain estimation based on behaviour. Accentuation of clinical assessment, for example, pressure mats inbuilt with sensors for people with pressure ulcers |
| Brain activity monitors | BIS, traditional EEGs and other technologies that use EEG electrodes, ECG, sEMG | Change in sleep patterns, brain wave activity | May be more suited to people who have very little speech (e.g. learning disability) or with low consciousness levels, e.g. ITU settings |
| Multi-modal systems | PSG and environmental sensors, wearable devices | Change in sleep patterns, change in activity and/or agitation levels, pacing patterns, activities of daily living estimation, reactions to medication | Assessment of pain during the night, assessment of sleep problems in relation to pain, assessment of motor and activity-related parameters in relation to pain, assessment of agitation |
| Non-contact monitoring systems | Video/facial expression analysis, infrared, radar | Sensing of subtle changes in facial expressions, sensing of pressure to skin or other bodily strain that might cause discomfort from people who are unable to communicate | Video and facial recognition algorithm-based apps already in use to supplement clinical assessment |
| Natural language processing | Language analysis: grammar, wording, word frequency; ontology-based analysis | Ability to extract significant and relevant terms from text | Summarising detailed accounts of pain experience where clinical time is short |
| Other technologies based on artificial intelligence (knowledge-based systems, neural network, Bayesian modelling, decision support systems, etc.) and based on formal methods (signal processing, system dynamics, nonlinear modelling, linear and nonlinear statistics, etc.) | Estimates of clinically relevant outcomes, which require clinical knowledge to design | All or most of the above | All or most of the above |
BIS bispectral index, ECG electrocardiography, EDA electrodermal activity, EEG electroencephalogram, GPS global positioning system, MET metabolic equivalent, PSG polysomnography, sEMG surface electromyogram, ITU intensive therapy unit
Digital pain phenotyping may also help with dissecting different components of pain in people with multiple pathologies, for example, whether an older person living with frailty has arthritis of multiple joints or multiple painful pathologies at once. Advanced data analysis (based on signal processing and/or artificial intelligence) could provide more sensitive and accurate information regarding the most prominent sources of pain in the body and the type and character of pain, thereby enabling more targeted biological treatment. Digital phenotyping may also help with providing feedback during therapy. For instance, if pain is associated with a specific gait deficit, improving the deficit might precede improvement in pain. This would encourage continuing therapy engagement if accompanied by early, sensitive digital information, which is not always clinically perceptible. Furthermore, people might exercise more effectively if digital technology can inform them that they are doing it as they should.
Personalisation of monitoring of the response to treatment is another potential benefit. For example, some people may become restless when in pain, others may develop a tachycardia or raise their blood pressure or breathing rate, whilst others might become less active. None of these biomarkers are specific for pain, as opposed to other forms of distress. With the help of digital phenotyping, clinicians might identify an individuals’ particular (digital) pain signal, and then use a digital monitor to assess change over time. In people who can self-report pain, change in digital biomarkers may be used to evaluate correlation with self-reported pain. While some work has been done in assessing the utility of digital phenotyping in cognitive impairment [61], future research questions should consider how the information gained might be more specific for pain rather than underlying distress from other causes, and also discriminate pain from other emotions. If pain can be assessed digitally, then the effects of pain treatments should also be able to be monitored in the same way. The challenge for the clinician would be to assimilate this knowledge into their clinical judgment to provide more holistic pain assessment and management.
Digital Phenotyping: Some Pitfalls
Although the use of digital technology and artificial intelligence in particular may have many potential benefits, there are some pitfalls to consider. There is currently reduced uptake of technology usage among older people compared to younger people, particularly if proactive use is required (for example, wearable devices). Reasons for this are multifactorial, and amongst other things, being of lower socioeconomic status, being older in age, and having no access to laptops or tablets is associated with reduced engagement [62, 63]. Older people living with frailty in particular have reduced uptake of digital technologies compared to older people who are more robust [64]. However, particularly since the coronavirus disease 2019 (COVID-19) pandemic, the percentage of older people engaging with digital technology has increased, and the narrowing digital divide between old and young should be seen as an opportunity [65, 66].
The ethics of obtaining information without informed consent, for example, with machine vision, needs to be deliberated prior to use. The privacy and data security of vulnerable older people living with frailty must be protected. In addition, a wealth of information does not mean that all information is useful or that positive signals pertain to the clinical question (i.e. non-specificity). Increased information may be overwhelming for older people and their loved ones, and may lead to the person and the clinician being over-anxious. In addition, some older people may also not accept or be fully compliant with the technology, which influences accuracy of the measurements, and while this issue is mitigated by swapping wearable sensors with environment-based, unobtrusive devices, the latter cannot follow patients outside their residence. Moreover, some techniques pertaining to artificial intelligence carry over substantial bias from the dataset used during training. The information used in creating the algorithm might not represent the true underlying population of older adults with frailty and calls into question the generalisability of data being collected. Furthermore, obtaining collateral information through digital technology to accentuate the pain phenotype is desirable, but future research should set out to determine whether they improve outcomes compared to standard care.
In addition, the clinician will need to maintain clinical skills in assessment and clinical reasoning, whilst harnessing the potential of digital technology as a tool and not regard it as a substitute diagnostician. Over-reliance on digital technology can de-skill clinicians, change the clinician–patient relationship, and reduce trust in clinical judgment. The clinician may also be less likely to treat a person on a symptomatic basis, simply because a machine does not give the expected signals. All these issues should be borne in mind when embracing the benefits that digital technology has to offer.
Future Directions
Digital solutions for tasks and problems are becoming more and more ingrained into daily life, and are likely to be a significant part of the future of healthcare. Compared to robust individuals, older people with frailty and cognitive impairment may benefit more from technological advances that enable early recognition and characterisation of pain and monitoring of treatment efficacy. The pain phenotype of the individual will then be analysed alongside evidence of organ dysfunction, multimorbidity, and the patient’s psychosocial and functional status in order to have a fuller and richer picture of pain in individual contexts. More comprehensive data collection through digital phenotyping might enable powerful algorithms and tailoring of treatment options and a better understanding of who benefits from specific and targeted treatments.
Declarations
Funding
No direct funding is declared for this article. JTC is funded by the National Institute of Health and Care Research (NIHR). BSH and MP would like to thank the GC Rieber Foundation and the Norwegian Government for supporting their work at the Centre for Elderly and Nursing Home Medicine, University of Bergen, Norway.
Conflict of interest
Jemima T. Collins, David A. Walsh, John R.F. Gladman, Monica Patrascu, Bettina S. Husebo, Esmee Adam, Alison Cowley, Adam L. Gordon, Giulia Ogliari, Hanneke Smaling, and Wilco Achterberg declare that they have no conflicts of interest that might be relevant to the contents of this article.
Ethics approval
This review does not require ethics approval.
Consent (participation and publication)
Not applicable.
Authors contributions
WA: Lead for article conception, design, and draft and revision editing. JTC: Article conception and design, structuring of article, overall editing of drafts, revisions, and submission. MP and BSH: draft editing and revisions (overall and, in particular, digital phenotyping and technology contributions). DAW and JRFG: Draft editing and revisions (overall and, in particular, non-pharmacological and pharmacological challenges in assessment of pain contributions). EA, AC, ALG, GO and HS contributed to the structuring, designing, drafting and editing of the original and revised manuscript. All authors read and approved the final manuscript.
Data availability statement
Not applicable.
Code availability
Not applicable.
References
- 1.Owiredua C, Flink I, Vixner L, Äng BO, Tseli E, Boersma K. The context matters: a retrospective analysis of life stage at chronic pain onset in relation to pain characteristics and psychosocial outcomes. J Pain Res. 2020;23(13):2685–2695. doi: 10.2147/JPR.S263035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clegg A, Young J, Iliffe S, Rikkert MO. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng L, Nyunt MS, Gao Q, Feng L, Lee TS, Tsoi T, Chong MS, Lim WS, Collinson S, Yap P, Yap KB, Ng TP. Physical frailty, cognitive impairment, and the risk of neurocognitive disorder in the Singapore longitudinal ageing studies. J Gerontol A Biol Sci Med Sci. 2017;72(3):369–375. doi: 10.1093/gerona/glw050. [DOI] [PubMed] [Google Scholar]
- 4.Petermann-Rocha F, Lyall DM, Gray SR, et al. Associations between physical frailty and dementia incidence: a prospective study from UK Biobank. Lancet Health Longev. 2020;1(2):e58–e68. doi: 10.1016/S2666-7568(20)30007-6. [DOI] [PubMed] [Google Scholar]
- 5.Grande G, Haaksma ML, Rizzuto D, Melis RJF, Marengoni A, Onder G, Welmer AK, Fratiglioni L, Vetrano DL. Co-occurrence of cognitive impairment and physical frailty, and incidence of dementia: systematic review and meta-analysis. Neurosci Biobehav Rev. 2019;107:96–103. doi: 10.1016/j.neubiorev.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Guerriero F, Reid MC. Linking persistent pain and frailty in older adults. Pain Med. 2020;21(1):61–66. doi: 10.1093/pm/pnz174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown L, Young J, Clegg A, Heaven A. Pain in older people with frailty. Rev Clin Gerontol. 2015;25(3):159–171. doi: 10.1017/S0959259815000143. [DOI] [Google Scholar]
- 8.Rodríguez-Sánchez I, García-Esquinas E, Mesas AE, Martín-Moreno JM, Rodríguez-Mañas L, Rodríguez-Artalejo F. Frequency, intensity and localization of pain as risk factors for frailty in older adults. Age Ageing. 2019;48(1):74–80. doi: 10.1093/ageing/afy163. [DOI] [PubMed] [Google Scholar]
- 9.Chiou JH, Liu LK, Lee WJ, Peng LN, Chen LK. What factors mediate the inter-relationship between frailty and pain in cognitively and functionally sound older adults? A prospective longitudinal ageing cohort study in Taiwan. BMJ Open. 2018;8(2):e018716. doi: 10.1136/bmjopen-2017-018716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wade KF, Marshall A, Vanhoutte B, Wu FC, O'Neill TW, Lee DM. Does pain predict frailty in older men and women? Findings from the English longitudinal study of ageing (ELSA) J Gerontol A Biol Sci Med Sci. 2017;72(3):403–409. doi: 10.1093/gerona/glw226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saraiva MD, Suzuki GS, Lin SM, de Andrade DC, Jacob-Filho W, Suemoto CK. Persistent pain is a risk factor for frailty: a systematic review and meta-analysis from prospective longitudinal studies. Age Ageing. 2018;47(6):785–793. doi: 10.1093/ageing/afy104. [DOI] [PubMed] [Google Scholar]
- 12.Generaal E, Vogelzangs N, Macfarlane GJ, Geenen R, Smit JH, Penninx BW, Dekker J. Reduced hypothalamic-pituitary-adrenal axis activity in chronic multi-site musculoskeletal pain: partly masked by depressive and anxiety disorders. BMC Musculoskelet Disord. 2014;9(15):227. doi: 10.1186/1471-2474-15-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanabria-Mazo JP, Colomer-Carbonell A, Carmona-Cervelló M, Feliu-Soler A, Borràs X, Grasa M, Esteve M, Maes M, Edo S, Sanz A, Luciano JV. Immune-inflammatory and hypothalamic-pituitary-adrenal axis biomarkers are altered in patients with non-specific low back pain: a systematic review. Front Immunol. 2022;2(13):945513. doi: 10.3389/fimmu.2022.945513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clegg A, Hassan-Smith Z. Frailty and the endocrine system. Lancet Diabetes Endocrinol. 2018;6(9):743–752. doi: 10.1016/S2213-8587(18)30110-4. [DOI] [PubMed] [Google Scholar]
- 15.Gupta D, Morley JE. Hypothalamic-pituitary-adrenal (HPA) axis and aging. Compr Physiol. 2014;4(4):1495–1510. doi: 10.1002/cphy.c130049. [DOI] [PubMed] [Google Scholar]
- 16.Niederstrasser NG, Attridge N. Associations between pain and physical activity among older adults. PLoS One. 2022;17(1):e0263356. doi: 10.1371/journal.pone.0263356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chaplin WJ, McWilliams DF, Millar BS, Gladman JRF, Walsh DA. The bidirectional relationship between chronic joint pain and frailty: data from the Investigating Musculoskeletal Health and Wellbeing cohort. BMC Geriatr. 2023;23(1):273. doi: 10.1186/s12877-023-03949-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quintner JL, Cohen ML, Buchanan D, Katz JD, Williamson OD. Pain medicine and its models: helping or hindering? Pain Med. 2008;9(7):824–834. doi: 10.1111/j.1526-4637.2007.00391.x. [DOI] [PubMed] [Google Scholar]
- 19.Edwards RR, Dworkin RH, Turk DC, et al. Patient phenotyping in clinical trials of chronic pain treatments: IMMPACT recommendations. PAIN Rep. 2021;6(1):e896. doi: 10.1097/PR9.0000000000000896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vahia IV, et al. Motion mapping in humans as a biomarker for psychiatric disorders. Neuropsychopharmacol. 2019;44(1):231–232. doi: 10.1038/s41386-018-0205-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Torous J, Keshavan M. A new window into psychosis: the rise digital phenotyping, smartphone assessment, and mobile monitoring. Schizophr Res. 2018;197:67–68. doi: 10.1016/j.schres.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Husebo BS, Heintz HL, Berge LI, Owoyemi P, Rahman AT, Vahia IV. Sensing technology to monitor behavioral and psychological symptoms and to assess treatment response in people with dementia. A systematic review. Front Pharmacol. 2019;10:1699. doi: 10.3389/fphar.2019.01699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torrado JC, Husebo BS, Allore HG, Erdal A, Fæø SE, Reithe H, Førsund E, Tzoulis C, Patrascu M. Digital phenotyping by wearable-driven artificial intelligence in older adults and people with Parkinson's disease: protocol of the mixed method, cyclic ActiveAgeing study. PLoS One. 2022;17(10):e0275747. doi: 10.1371/journal.pone.0275747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walsh DA, Rathbone J, Akin-Akinyosoye K, Fernandes GS, Valdes AM, McWilliams DF, Zhang W, Doherty M, Hancox JE, Vedhara K, das Nair R, Ferguson E. How people with knee pain understand why their pain changes or remains the same over time: a qualitative study. Osteoarthr Cartil Open. 2023;5:100345. doi: 10.1016/j.ocarto.2023.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.NICE Guidelines NG193. Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain. https://www.nice.org.uk/guidance/ng193/chapter/recommendation. Accessed 7 Apr 2021. [DOI] [PMC free article] [PubMed]
- 26.Zhang M, Holman CDJ, Preen DB, Brameld K. Repeat adverse drug reactions causing hospitalization in older Australians: a population-based longitudinal study 1980–2003. Br J Clin Pharmacol. 2007;63:163–170. doi: 10.1111/j.1365-2125.2006.02839.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erdal A, Flo E, Aarsland D, Selbaek G, Ballard C, Slettebo DD, Husebo BS. Tolerability of buprenorphine transdermal system in nursing home patients with advanced dementia: a randomized, placebo-controlled trial (DEP.PAIN.DEM) Clin Interv Aging. 2018;13:935–946. doi: 10.2147/CIA.S161052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rodger KT, Greasley-Adams C, Hodge Z, et al. Expert opinion on the management of pain in hospitalised older patients with cognitive impairment: a mixed methods analysis of a national survey. BMC Geriatr. 2015;15:56. doi: 10.1186/s12877-015-0056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Ojik AL, Jansen PA, Brouwers JR, van Roon EN. Treatment of chronic pain in older people: evidence-based choice of strong-acting opioids. Drugs Aging. 2012;29(8):615–625. doi: 10.2165/11632620-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 30.Schlender JF, Meyer M, Thelen K, Krauss M, Willmann S, Eissing T, Jaehde U. Development of a whole-body physiologically based pharmacokinetic approach to assess the pharmacokinetics of drugs in elderly individuals. Clin Pharmacokinet. 2016;55(12):1573–1589. doi: 10.1007/s40262-016-0422-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57(1):6–14. doi: 10.1046/j.1365-2125.2003.02007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reeve E, Trenaman SC, Rockwood K, Hilmer SN. Pharmacokinetic and pharmacodynamic alterations in older people with dementia. Expert Opin Drug Metab Toxicol. 2017;13(6):651–668. doi: 10.1080/17425255.2017.1325873. [DOI] [PubMed] [Google Scholar]
- 33.Erdal A, Ballard C, Vahia IV, Husebo BS. Analgesic treatments in people with dementia—how safe are they? A systematic review. Expert Opin Drug Saf. 2019;18(6):511–522. doi: 10.1080/14740338.2019.1614166. [DOI] [PubMed] [Google Scholar]
- 34.Tevik K, Benth JŠ, Aarøen M, Lornstad MT, Bergh S, Helvik AS. Prevalence and persistent use of analgesic drugs in older adults receiving domiciliary care at baseline—a longitudinal study. Health Sci Rep. 2021;4(3):e316. doi: 10.1002/hsr2.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tang SK, Tse MMY, Leung SF, et al. The effectiveness, suitability, and sustainability of non-pharmacological methods of managing pain in community-dwelling older adults: a systematic review. BMC Public Health. 2019;19:1488. doi: 10.1186/s12889-019-7831-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liao YJ, Parajuli J, Jao YL, Kitko L, Berish D. Non-pharmacological interventions for pain in people with dementia: a systematic review. Int J Nurs Stud. 2021;124:104082. doi: 10.1016/j.ijnurstu.2021.104082. [DOI] [PubMed] [Google Scholar]
- 37.Soares Fonseca L, Pereira Silva J, Bastos Souza M, et al. Effectiveness of pharmacological and non-pharmacological therapy on pain intensity and disability in older people with chronic nonspecific low back pain: a systematic review with meta-analysis. Eur Spine J. 2023;32:3245–3271. doi: 10.1007/s00586-023-07857-4. [DOI] [PubMed] [Google Scholar]
- 38.Hempenius L, Slaets JP, Boelens MA, van Asselt DZ, de Bock GH, Wiggers T, van Leeuwen BL. Inclusion of frail elderly patients in clinical trials: solutions to the problems. J Geriatr Oncol. 2013;4(1):26–31. doi: 10.1016/j.jgo.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 39.Blomqvist K, Edberg A. Living with persistent pain: experiences of older people receiving home care. J Adv Nurs. 2002;40(3):297–306. doi: 10.1046/j.1365-2648.2002.02371.x. [DOI] [PubMed] [Google Scholar]
- 40.Schofield P. Pain in older adults: epidemiology, impact and barriers to management. Rev Pain. 2007;1(1):12–14. doi: 10.1177/204946370700100104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Larsson C, Ekvall Hansson E, Sundquist K, et al. Impact of pain characteristics and fear-avoidance beliefs on physical activity levels among older adults with chronic pain: a population-based, longitudinal study. BMC Geriatr. 2016;16:50. doi: 10.1186/s12877-016-0224-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schofield PA, Clarke A, Faulkner M, et al. University of Sheffield ISBN 1-902411-40-4. 2005.
- 43.Levy BR, Pietrzak RH, Slade MD. Societal impact on older persons' chronic pain: roles of age stereotypes, age attribution, and age discrimination. Soc Sci Med. 2023;323:115772. doi: 10.1016/j.socscimed.2023.115772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Achterberg WP. How can the quality of life of older patients living with chronic pain be improved? Pain Manag. 2019;9(5):431–433. doi: 10.2217/pmt-2019-0023. [DOI] [PubMed] [Google Scholar]
- 45.Yates P, Dewar A, Fentiman B. Pain: the views of elderly people living in long-term residential care settings. J Adv Nurs. 1995;21:667–674. doi: 10.1046/j.1365-2648.1995.21040667.x. [DOI] [PubMed] [Google Scholar]
- 46.Brown D. A literature review exploring how healthcare professionals contribute to the assessment and control of postoperative pain in older people. J Clin Nurs. 2004;13(2):74–90. doi: 10.1111/j.1365-2702.2004.01047.x. [DOI] [PubMed] [Google Scholar]
- 47.Collins JT, Harwood RH, Cowley A, et al. Chronic pain in people living with dementia: challenges to recognising and managing pain, and personalising intervention by phenotype. Age Ageing. 2023;52(1):afac06. doi: 10.1093/ageing/afac306. [DOI] [PubMed] [Google Scholar]
- 48.Lichtner V, Dowding D, Allcock N, Keady J, Sampson EL, et al. The assessment and management of pain in patients with dementia in hospital settings: a multi-case exploratory study from a decision making perspective. BMC Health Serv Res. 2016;16(1):427. doi: 10.1186/s12913-016-1690-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gooberman-Hill R, Woolhead G, MacKichan F, Ayis S, Williams S, Dieppe P. Assessing chronic joint pain: lessons from a focus group study. Arthrit Care Res. 2007;57(4):666–671. doi: 10.1002/art.22681. [DOI] [PubMed] [Google Scholar]
- 50.Clarke A, Anthony G, Gray D, et al. “I feel so stupid because I can’t give a proper answer…” How older adults describe chronic pain: a qualitative study. BMC Geriatr. 2012;12:78. doi: 10.1186/1471-2318-12-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pautex S, Michon A, Guedira M, Emond H, Le Lous P, Samaras D, Michel JP, Herrmann F, Giannakopoulos P, Gold G. Pain in severe dementia: self-assessment or observational scales? J Am Geriatr Soc. 2006;54(7):1040–1045. doi: 10.1111/j.1532-5415.2006.00766.x. [DOI] [PubMed] [Google Scholar]
- 52.Husebo BS, Ostelo R, Strand LI. The MOBID-2 pain scale: reliability and responsiveness to pain in patients with dementia. Eur J Pain. 2014;18(10):1419–1430. doi: 10.1002/ejp.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kunz M, Scharmann S, Hemmeter U, et al. The facial expression of pain in patients with dementia. Pain. 2007;133(1):221–228. doi: 10.1016/j.pain.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 54.Smith TO, Harvey K. Psychometric properties of pain measurements for people living with dementia: a COSMIN systematic review. Eur Geriatr Med. 2022;13:1029–1045. doi: 10.1007/s41999-022-00655-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Robinson JR, Wei WQ, Roden DM, Denny JC. Defining phenotypes from clinical data to drive genomic research. Annu Rev Biomed Data Sci. 2018;1:69–92. doi: 10.1146/annurev-biodatasci-080917-013335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Edwards RR, Dworkin RH, Turk DC, et al. Patient phenotyping in clinical trials of chronic pain treatments: IMMPACT recommendations. Pain. 2016;157(9):1851–1871. doi: 10.1097/j.pain.0000000000000602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Espay AJ, Bonato P, Nahab FB, Maetzler W, Dean JM, et al. Movement Disorders Society Task Force on Technology. Technology in Parkinson's disease: challenges and opportunities. Mov Disord. 2016;31(9):1272–1282. doi: 10.1002/mds.26642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vahia IV, Kabelac Z, Hsu CY, et al. Radio signal sensing and signal processing to monitor behavioral symptoms in dementia: a case study. Am J Geriatr Psych. 2020;28(8):820–825. doi: 10.1016/j.jagp.2020.02.012. [DOI] [PubMed] [Google Scholar]
- 59.Husebo BS, Vislapuu M, Cyndecka M, et al. Understanding pain and agitation through system analysis algorithms in people with dementia. A novel explorative approach by the DIGI. PAIN Study. Front Pain Res. 2020;3:847578. doi: 10.3389/fpain.2022.847578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cook DJ, Strickland M, Schmitter-Edgecombe M. Detecting smartwatch-based behavior change in response to a multi-domain brain health intervention. ACM Trans Comput Healthc (HEALTH) 2022;3(3):1–18. doi: 10.1145/3508020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hoti K, Atee M, Chivers P, Vahia I, Hughes J. Technology-guided assessment of vocalisations and their diagnostic value as pain indicators for people living with dementia. Age Ageing. 2023;52(6):afad088. doi: 10.1093/ageing/afad088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gordon NP, Crouch E. Digital information technology use and patient preferences for internet-based health education modalities: cross-sectional survey study of middle-aged and older adults with chronic health conditions. JMIR Aging. 2019;2(1):e12243. doi: 10.2196/12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Begde A, Jain M, Goodwin M, et al. Exploring factors influencing willingness of older adults to use assistive technologies: evidence from the cognitive function and ageing study II. Inf Commun Soc. 2023 doi: 10.1080/1369118X.2023.2205915. [DOI] [Google Scholar]
- 64.Lee DR, Lo JC, Ramalingam N, Gordon NP. Understanding the uptake of digital technologies for health-related purposes in frail older adults. J Amer Geriatric Soc. 2021;69(1):269–272. doi: 10.1111/jgs.16841. [DOI] [PubMed] [Google Scholar]
- 65.Age UK Briefing Paper. Digital inclusion and older people—how have things changed in a COVID-19 world? https://www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/active-communities/digital-inclusion-in-the-pandemic-final-march-2021.pdf. Accessed March 2021.
- 66.Yao Y, Zhang H, Liu X, et al. Bridging the digital divide between old and young people in China: challenges and opportunities. Lancet Health Longev. 2021;2(3):e125–e126. doi: 10.1016/S2666-7568(21)00032-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


