Abstract
Purpose
To compare perioperative, functional, and safety outcomes between thulium fiber laser enucleation of the prostate (ThuFLEP) and bipolar enucleation of the prostate performed by a single surgeon with use of propensity score (PS)-matched analysis.
Materials and Methods
Data were from 675 patients, 422 of whom underwent ThuFLEP and bipolar enucleation by a single highly experienced surgeon. ThuFLEP was performed with Fiberlase U1 (IRE Polus Ltd.). Perioperative parameters, safety, and functional outcomes, such as International Prostate Symptom Score (IPSS), quality of life (QoL), postvoid residual volume (PVR), and maximum urinary flow rate (Qmax) were assessed. To control for selection bias, a 1:1 PS-matched analysis was carried out using the following variables as covariates: total prostate volume, preoperative IPSS and early sphincter release.
Results
Of 422 patients, 370 (87.7%) underwent ThuFLEP and 52 (12.3%) underwent bipolar enucleation. Operation, enucleation, and morcellation time were comparable between groups before and after PS-matched analysis (p=0.954, p=0.474, p=0.362, respectively). Functional parameters (IPSS, QoL, PVR, Qmax) were also comparable between groups at every time point before and after PS matching. Significant improvements in IPSS, QoL score, Qmax, and PVR were observed during the 24-month follow-up period for both ThuFLEP and bipolar enucleation without any significant differences between groups. Early and late postoperative complications before and after PS-matched analysis were similar.
Conclusions
ThuFLEP was comparable to bipolar enucleation in perioperative characteristics, improvement in voiding parameters, and complication rates. Both procedures were shown to be effective and safe in the management of benign prostatic hyperplasia.
Keywords: Benign prostatic hyperplasia, Minimally invasive surgical procedure, Propensity score, Thulium
Graphical Abstract
INTRODUCTION
Benign prostatic hyperplasia (BPH) is one of the most common diseases in aging men. The disease results in lower urinary tract symptoms (LUTS) and low quality of life (QoL). Epidemiological studies have shown that BPH is present in approximately 8% of men in their fourth decade of life but in up to 90% of men in their 90s [1]. According to a population-based study, the prevalence of LUTS in men aged 40 to 69 years in Russia is 58.2% [2]. The incidence of moderate and severe LUTS progressively increases with age: from 15.3% to 26.2% [2].
When LUTS are refractory to conservative or medical treatment or patients already have absolute operation indications, the next step is surgical treatment. However, the choice of surgical techniques is one of the cornerstones of BPH management [3]. According to the 2023 European Association of Urology guidelines [3], the techniques include resection, enucleation, vaporization, alternative ablative techniques, and nonablative techniques. Enucleation is the most actively developing technique of BPH surgical treatment. Nowadays, enucleation of BPH is the procedure of choice for all prostate volumes starting from 30 cm3 even if it is not possible to stop anticoagulation or antiplatelet therapy [3].
Endoscopic enucleation of the prostate can be performed with different energies, such as bipolar/plasmakinetic, Tm:YAG laser (ThuLEP), Ho:YAG laser (HoLEP), diode laser, potassium-Titanyl-Phosphate, and the lithium triborate laser [3]. In editorial comments titled “Enucleation is enucleation is enucleation is enucleation” issued by Herrmann [4] in 2016, the author concluded that all enucleating techniques that have been demonstrated to perform anatomical enucleation should be summarized under the term ‘endoscopic enucleation of the prostate’ (EEP). The most recent systematic review and meta-analysis was published in 2023. That analysis showed that all variations of EEP improve symptoms and functional parameters with a low incidence of high-grade complications [5].
However, no one review has taken into account the newly invented thulium fiber laser (Tm-fiber), which can now be used for both enucleation and lithotripsy. Tm-fiber was developed in Russia and introduced into clinical practice in 2016 (IRE Polus Ltd.). The Tm-fiber laser technology combines the best features of Tm:YAG and Ho:YAG lasers: pulse periodic mode and wavelength (1.94 µm, whereas that for the Tm:YAG laser is more than 2 µm) [6]. A histologic analysis found greater tissue penetration with the Ho:YAG laser and different coagulation properties between the two lasers [7]. Such Tm-fiber laser features allow improved hemostasis without vaporization and optimize carbonation.
At the same time, studies devoted to comparing the results of enucleation performed with Tm-fiber and other energy sources are limited to several publications. To date, it has been shown that thulium fiber laser enucleation of the prostate (ThuFLEP) has some advantages over classic transurethral resection [8] and open adenomectomy [9], with the same effectiveness as ThuLEP [10] and HoLEP [11]. However, no work in the literature has compared ThuFLEP and the most economical and affordable bipolar enucleation. Therefore, the purpose of this study was to compare perioperative, functional, and safety outcomes between ThuFLEP and bipolar enucleation of the prostate performed by a single surgeon with use of propensity score (PS)-matched analysis.
MATERIALS AND METHODS
1. Study population
This study was approved by the Institutional Review Board (IRB) of Lomonosov Moscow State University (approval number: 04/22). Written informed consent was waived due to the retrospective nature of the study.
Using a database approved by the IRB, we retrospectively analyzed 675 patients hospitalized with a diagnosis of BPH (N40 according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision) between 2019 and 2021. A total of 422 patients were selected who underwent ThuFLEP and bipolar enucleation of the prostate for BPH by a single highly experienced surgeon and for whom information about the postoperative period was available. All patients had bladder outlet obstruction due to BPH with ineffective drug therapy. The choice of ThuFLEP or bipolar enucleation was according to the surgeon’s preference and the equipment available at the moment of operation. Exclusion criteria were a history of previous transurethral surgery before enucleation, urethral stricture or bladder neck sclerosis, prostate cancer, neurogenic bladder, and concomitant lower urinary tract surgery (optical urethrotomy and/or bladder lithotripsy).
All patients were evaluated for baseline characteristics. The preoperative level of prostate-specific antigen (PSA) and the total volume of the prostate gland were determined (using transrectal ultrasound). Before surgery and 1, 3, 6, 12, and 24 months after surgery, the International Prostate Symptom Score (IPSS) and QoL assessment, maximum urinary flow rate (Qmax), and postvoid residual volume (PVR) were evaluated. These variables were used as functional results. Intraoperative parameters were recorded in all patients, such as the technique of enucleation, the number of patients with early release of the sphincter, the operation time, and separately the enucleation time and the morcellation time. Early and long-term postoperative complications were also recorded. Urinary incontinence was defined as any leakage of urine that the patient reported during the observation period. Early and long-term postoperative complications, as well as anticoagulant/antiplatelet treatment before surgery were used as safety outcomes.
2. Surgical procedures
All operations were performed by one surgeon with enucleation experience of more than 2,000 cases. A Fiberlase U1 thulium fiber laser (IRE Polus Ltd.) with operating modes of 1.5 J and 40 Hz 60 W was used to perform the ThuFLEP. The fiber used was 550 microns. An irrigation resectoscope of the Iglessias type 27 Ch was used for fiber delivery (Olympus). Morcellation was performed using a Piranha rotary morcellator (Richard Wolf).
To perform bipolar enucleation, an Erbe Vio 3 (Erbe Elektromedizin) power unit was used with an effect of 2 for cutting and 3 for coagulation using a standard Olympus enucleation loop. Also used was an irrigation active resectoscope of the Iglessias type 27 Ch (Olympus). Morcellation was performed using a Piranha rotary morcellator (Richard Wolf).
The operation was performed by using a three-bladed, two-bladed, or en bloc technique, depending on the endoscopic anatomy of the prostate gland and its volume. In most cases, we used the two-lobe technique because for us it provides better visualization and better control of layers during enucleation. However, in some cases we had to employ threelobe or en bloc techniques. When we found the great mean lobe during cystoscopy, we used the three-lobe technique. When the en bloc technique began to be actively applied worldwide, we thought that we could use this technique in the same cases as the two-lobe technique, but only when total prostate volume was less than 120 cm3.
The first stage was carried out for all patients to introduce a layer in the area of the seminal tubercle. When an early apical dissection was performed, the mobilization of the lateral lobes occurred before the 4 and 8 o’clock positions, after which the dissection of the apical zone was performed. Subsequently, the operation techniques did not differ from the classic ones.
3. Statistical analysis
The statistical analysis was performed using Statistica 12 (StatSoft), IBM SPSS Statistics software version 22.0 (IBM Corp.), and jamovi version 2.2.5 (jamovi project). The Shapiro–Wilk’s and Kolmogorov–Smirnov’s tests were used to assess the normality of continuous data. All data had a nonnormal distribution and are represented as medians and interquartile ranges (IQRs). The numeric data between groups were compared with the Mann–Whitney U test. Categorical data are represented as number of patients (%). Categorical data were compared between groups by using Pearson’s chisquare test, Pearson’s chi-square test with Yates’s continuity correction, and one-tailed Fisher’s exact test. Comparison of multiple dependent variables was conducted with the Friedman test.
To control for selection bias and confounding factors, a 1:1 PS-matched analysis was carried out using a caliper width of 0.1. PSs were estimated by multivariable logistic regression using the following variables as covariates: total prostate volume, preoperative QoL, PVR, and early sphincter release. Absolute standardized mean differences (ASMDs) were used to examine the balance of covariate distribution between groups. Comparison after PS-matched analysis was conducted as described above. The statistical significance was set at p<0.05.
RESULTS
Table 1 shows the characteristics of the initial study cohort of 422 patients before and after they were matched according to the predefined criteria. Of these patients, 370 (87.7%) underwent ThuFLEP and 52 (12.3%) underwent bipolar enucleation. Before PS matching patients in bipolar enucleation group had less total prostate volume (median, 72.1 cm3 and 84.0 cm3 respectively; p=0.004), higher IPSS score (median, 29.5 and 26.0 respectively; p=0.014) and less often early sphincter release (76.9% and 90.5% respectively; p=0.007) compare to ThuFLEP. Other variables were similar. These variables were thus selected for PS-matched analysis as covariates. After PS matching, ASMDs for all preoperative covariates were <0.1 (Table 1), which suggested an absolute balance between covariates.
Table 1. Preoperative and intraoperative patient characteristics.
| Parameter | Before PS matching | PS-matched patients | ASMD | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ThuFLEP (n=370) | Bipolar enucleation (n=52) | р-value | ThuFLEP (n=40) | Bipolar enucleation (n=40) | р-value | |||||
| Age (y) | 67.0 (61.0–72.0) | 70.0 (63.0–74.0) | 0.113 | 67.0 (59.0–74.0) | 69.0 (61.0–73.0) | 0.723 | -0.029 | |||
| ASA (score) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 0.153 | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 0.183 | 0.019 | |||
| Comorbid diseases | ||||||||||
| Hypertension | 245 (66.2) | 37 (71.2) | 0.479 | 23 (57.5) | 26 (65.0) | 0.491 | -0.075 | |||
| Coronary heart disease | 65 (17.6) | 12 (23.1) | 0.335 | 8 (20.0) | 10 (25.0) | 0.789 | -0.050 | |||
| Diabetes mellitus | 60 (16.2) | 10 (19.2) | 0.584 | 7 (17.5) | 9 (22.5) | 0.780a | -0.050 | |||
| Cerebrovascular diseases | 47 (12.7) | 8 (15.4) | 0.751 | 6 (15.0) | 34 (85.0) | >0.999a | -0.025 | |||
| Preoperative parameter | ||||||||||
| Total prostate volume (cm3) | 84.0 (60.0–117.0) | 72.1 (50.9–89.0) | 0.004* | 74.3 (58.6–100.5) | 69.5 (49.5–95.0) | 0.144 | 0.084 | |||
| IPSS (score) | 26.0 (22.0–31.0) | 29.5 (24.0–33.0) | 0.014* | 28.0 (23.5–32.5) | 25.5 (21.5–30.0) | 0.247 | 0.062 | |||
| QoL (score) | 5.0 (4.0–6.0) | 5.0 (4.0–5.0) | 0.176 | 5.0 (4.0–5.0) | 4.0 (3.0–5.0) | 0.087 | 0.087 | |||
| Qmax (mL/s) | 9.2 (7.3–11.9) | 9.5 (6.6–14.0) | 0.777 | 8.8 (7.2–11.7) | 9.8 (8.3–13.4) | 0.098 | -0.088 | |||
| PVR (mL) | 75.0 (47.0–112.0) | 87.5 (58.0–117.5) | 0.381 | 69.0 (37.0–100.0) | 69.0 (21.0–90.0) | 0.519 | 0.019 | |||
| PSA (ng/dL) | 4.0 (2.2–7.0) | 3.4 (1.7–5.8) | 0.223 | 3.7 (2.0–6.8) | 4.2 (1.7–5.6) | 0.604 | -0.012 | |||
| Indwelling catheter | 81 (21.9) | 12 (23.1) | 0.847 | 9 (22.5) | 9 (22.5) | >0.999 | 0.000 | |||
| Duration of indwelling catheter | 0.673 | 0.500a | 0.032 | |||||||
| Less than 6 months | 59 (72.8) | 10 (83.3) | 7 (77.8) | 8 (88.9) | ||||||
| 6 months and more | 22 (27.2) | 2 (16.7) | 2 (22.2) | 1 (11.1) | ||||||
| Intraoperative parameter | ||||||||||
| Early sphincter release | 335 (90.5) | 40 (76.9) | 0.007a* | 30 (75.0) | 29 (72.5) | 0.799 | 0.025 | |||
| Enucleation technique | 0.304 | 0.321 | -0.064 | |||||||
| 3-lobe | 15 (4.1) | 0 (0.0) | 2 (5.0) | 0 (0.0) | ||||||
| 2-lobe | 321 (86.8) | 48 (92.3) | 34 (85.0) | 37 (92.5) | ||||||
| En bloc | 34 (9.2) | 4 (7.7) | 4 (10.0) | 3 (7.5) | ||||||
| Operation time (min) | 75.0 (60.0–100.0) | 70.0 (55.0–90.0) | 0.257 | 70.0 (57.5–97.5) | 70.0 (55.0–90.0) | 0.954 | - | |||
| Enucleation time (min) | 55.0 (40.0–70.0) | 45.0 (35.0–62.5) | 0.069 | 50.0 (40.0–65.0) | 45.0 (32.5–62.5) | 0.474 | - | |||
| Morcellation time (min) | 25.0 (20.0–30.0) | 20.0 (20.0–35.0) | 0.508 | 25.0 (20.0–30.0) | 22.5 (20.0–32.5) | 0.362 | - | |||
| Anesthesia | 0.469 | 0.500b | -0.025 | |||||||
| General | 34 (9.2) | 7 (13.5) | 5 (12.5) | 36 (90.0) | ||||||
| Spinal | 336 (90.8) | 45 (86.5) | 35 (87.5) | 4 (10.0) | ||||||
Values are presented as median (interquartile range) or number (%).
PS, propensity score; ThuFLEP, thulium fiber laser enucleation of the prostate; ASMD, absolute standardized mean differences; ASA, American Society of Anesthesiologists; IPSS, International Prostate Symptom Score; QoL, quality of life; Qmax, maximum speed of urine flow; PVR, postvoid residual volume; PSA, prostate-specific antigen.
a:Pearson’s chi-square test with Yates’s continuity correction.
b:One-tailed Fisher’s exact test; without aPearson’s chi-square test.
*p<0.05.
The perioperative parameters, such as the operation time, enucleation time, morcellation time and enucleation technique, were comparable between groups before as well as after PS matching (Table 1). Most patients had 2-lobe enucleation in both groups with no differences before or after PS matching (p=0.304 and p=0.321, respectively). The median operation time for ThuFLEP and bipolar enucleation was 75 minutes and 70 minutes, respectively (p=0.257). After PS matching it was 70 minutes for both ThuFLEP and bipolar enucleation, respectively (p=0.954). Median enucleation time for ThuFLEP and bipolar enucleation was 55.0 and 45.0, respectively (p=0.069). After PS matching it was 50.0 and 45.0 minutes, respectively (p=0.474). The same was found for morcellation time: it was 25.0 and 20.0 minutes for ThuFLEP and bipolar enucleation, respectively (p=0.508). After PS matching it was 25.0 and 22.5 minutes, respectively (p=0.362).
Table 2 shows postoperative functional outcomes of ThuFLEP and bipolar enucleation before and after PS-matched analysis. Before PS-matched analysis, ThuFLEP and bipolar enucleation had similar functional outcomes throughout the follow-up period from 1 to 24 months. After PS-matched analysis, the results were the same, which indicated a similar effectiveness of ThuFLEP and bipolar enucleation. At 24 months, we lost 92 patients (24.9%) to follow-up in the ThuFLEP group and 8 patients (15.4%) in the bipolar enucleation group. The number of losses at each time point are presented in Table 2.
Table 2. Postoperative functional outcomes.
| Parameter | Before PS matching | PS-matched patients | |||||
|---|---|---|---|---|---|---|---|
| ThuFLEP (n=370) | Bipolar enucleation (n=52) | p-value | ThuFLEP (n=40) | Bipolar enucleation (n=40) | p-value | ||
| 1 month | n=370 | n=52 | n=40 | n=40 | |||
| IPSS (score) | 9.0 (5.0–12.0) | 7.0 (4.0–13.0) | 0.622 | 8.0 (4.0–11.0) | 25.5 (21.5–30.0) | 0.313 | |
| QoL (score) | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) | 0.257 | 2.0 (1.5–3.0) | 4.0 (3.0–5.0) | 0.659 | |
| Qmax (mL/s) | 19.0 (15.0–22.0) | 20.0 (15.0–23.0) | 0.722 | 19.0 (15.5–22.5) | 9.75 (8.25–13.4) | 0.608 | |
| PVR (mL) | 24.0 (12.0–38.0) | 22.0 (0.0–32.0) | 0.078 | 19.5 (12.5–37.0) | 69.0 (21.0–90.0) | 0.521 | |
| 3 months | n=364 | n=52 | n=40 | n=40 | |||
| IPSS (score) | 6.0 (3.0–9.0) | 4.0 (2.0–9.0) | 0.549 | 5.0 (3.0–7.5) | 10.0 (5.0–13.0) | 0.904 | |
| QoL (score) | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) | 0.295 | 1.0 (0.0–2.0) | 2.0 (1.0–3.0) | 0.410 | |
| Qmax (mL/s) | 20.0 (16.0–24.0) | 22.0 (18.0–25.0) | 0.219 | 21.5 (16.0–24.5) | 21.0 (15.0–23.0) | 0.822 | |
| PVR (mL) | 23.0 (10.5–34.0) | 22.0 (0.0–32.0) | 0.377 | 14.5 (0.0–26.0) | 24.0 (0.0–32.0) | 0.568 | |
| 6 months | n=358 | n=51 | n=40 | n=40 | |||
| IPSS (score) | 7.0 (3.0–10.0) | 7.0 (2.0–10.0) | 0.403 | 8.0 (5.0–11.0) | 6.0 (2.0–10.0) | 0.198 | |
| QoL (score) | 1.0 (1.0–3.0) | 1.0 (0.0–2.0) | 0.497 | 1.0 (1.0–2.0) | 1.0 (0.0–2.0) | 0.487 | |
| Qmax (mL/s) | 21.0 (17.0–25.0) | 20.0 (17.0–26.0) | 0.949 | 20.0 (17.0–23.0) | 21.0 (17.0–26.0) | 0.334 | |
| PVR (mL) | 21.0 (11.0–30.0) | 19.0 (11.0–30.0) | 0.833 | 23.0 (13.0–27.0) | 19.0 (0.0–26.0) | 0.380 | |
| 12 months | n=347 | n=47 | n=40 | n=40 | |||
| IPSS (score) | 8.0 (4.0–12.0) | 9.0 (3.5–12.5) | 0.840 | 7.0 (4.0–11.0) | 9.0 (5.0–13.0) | 0.289 | |
| QoL (score) | 2.0 (1.0–3.0) | 2.0 (1.0–2.5) | 0.378 | 2.0 (2.0–2.0) | 2.0 (1.0–3.0) | 0.710 | |
| Qmax (mL/s) | 20.0 (16.0–24.0) | 20.0 (16.0–23.0) | 0.842 | 20.0 (18.0–22.0) | 20.0 (16.0–24.0) | 0.816 | |
| PVR (mL) | 18.0 (9.0–27.0) | 22.0 (9.5–29.0) | 0.420 | 15.0 (9.0–27.0) | 22.0 (9.0–28.0) | 0.672 | |
| PSA (ng/dL) | 1.8 (1.0–2.6) | 1.6 (1.1–2.7) | 0.985 | 1.4 (0.8–2.2) | 1.8 (1.2–2.7) | 0.104 | |
| 24 months | n=278 | n=44 | n=40 | n=40 | |||
| IPSS (score) | 7.0 (3.0–10.0) | 6.0 (3.0–9.0) | 0.515 | 5.5 (3.0–10.0) | 6.0 (3.0–10.0) | 0.697 | |
| QoL (score) | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) | 0.940 | 1.0 (1.0–2.0) | 1.0 (0.0–2.0) | 0.074 | |
| Qmax (mL/s) | 19.0 (16.0–21.0) | 19.5 (16.0–22.0) | 0.270 | 19.0 (15.5–21.0) | 20.0 (16.0–22.0) | 0.305 | |
| PVR (mL) | 28.0 (13.0–41.0) | 25.0 (11.0–37.0) | 0.348 | 33.5 (20.0–45.5) | 22.0 (11.0–34.0) | 0.027* | |
Values are presented as median (interquartile range).
PS, propensity score; ThuFLEP, thulium fiber laser enucleation of the prostate; IPSS, International Prostate Symptom Score; QoL, quality of life; Qmax, maximum speed of urine flow; PVR, postvoid residual volume; PSA, prostate-specific antigen.
*p<0.05.
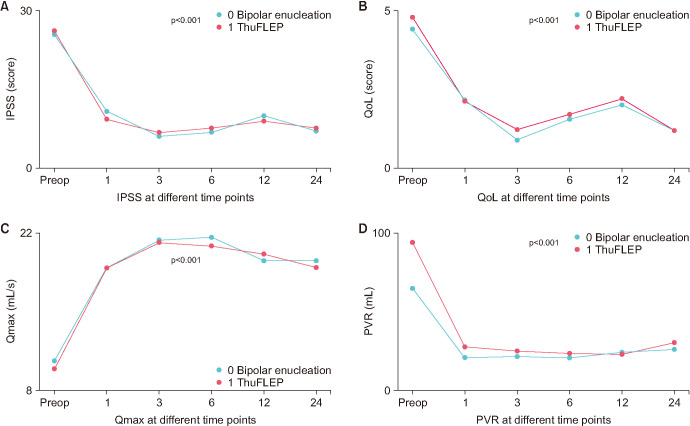
Significant improvements in IPSS, QoL score, Qmax, and PVR were observed during the 24-month follow-up period (Fig. 1) for both ThuFLEP and bipolar enucleation. Moreover, there were no significant differences in these parameters between the groups at any follow-up time point (p>0.05).
Fig. 1. Comparison of IPSS, QoL score, Qmax, and PVR before and after bipolar enucleation and ThuFLEP during 24 months of follow-up. Values are presented as mean. IPSS, International Prostate Symptom Score; QoL, quality of life; Qmax, maximum speed of urine flow; PVR, postvoid residual volume; preop, preoperative; ThuFLEP, thulium fiber laser enucleation of the prostate.
The safety outcomes of ThuFLEP and bipolar enucleation before and after PS-matched analysis are presented in Table 3. The same safety profile was found for ThuFLEP and bipolar enucleation. Median catheterization time before PS matching was 3.0 days and 2.0 days for ThuFLEP and bipolar enucleation, respectively (p=0.192). After PS matching, it still was similar with a median of 2.0 days for both ThuFLEP and bipolar enucleation, respectively (p=0.508). The same results were found for hospitalization time, with a median of 4.0 days for both ThuFLEP and bipolar enucleation before as well as after PS matching (p=0.326 and p=0.678, respectively).
Table 3. Safety outcomes.
| Parameters | Before PS matching | PS-matched patients | ||||||
|---|---|---|---|---|---|---|---|---|
| ThuFLEP (n=370) | Bipolar enucleation (n=52) | p-value | ThuFLEP (n=40) | Bipolar enucleation (n=40) | p-value | |||
| Catheterization time (d) | 3.0 (2.0–3.0) | 2.0 (2.0–3.0) | 0.192 | 2.0 (2.0–3.0) | 2.0 (2.0–3.0) | 0.508 | ||
| Hospitalization time (d) | 4.0 (3.0–5.0) | 4.0 (3.0–6.0) | 0.326 | 4.0 (4.0–5.0) | 4.0 (4.0–5.0) | 0.678 | ||
| Anticoagulant/antiplatelet treatments | 99 (26.8) | 15 (28.8) | 0.751 | 13 (32.5) | 10 (25.0) | 0.459 | ||
| Early postoperative complications | 22 (5.9) | 4 (7.7) | 0.847 | 1 (2.5) | 3 (7.5) | 0.374 | ||
| Acute urinary retention | 2 (0.5) | 1 (1.9) | 0 (0.0) | 1 (2.5) | ||||
| Rate of bleeding | 10 (2.7) | 2 (3.8) | 1 (2.5) | 0 (0.0) | ||||
| Prolonged irrigation due to hematuria | 7 (1.9) | 1 (1.9) | 0 (0.0) | 1 (2.5) | ||||
| Bleeding requiring repeated surgery | 4 (1.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||
| Urinary tract infection | 6 (1.6) | 1 (1.9) | 0 (0.0) | 1 (2.5) | ||||
| Cardiovascular complications | 2 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||
| Transfusion rate | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||
| Clavien–Dindo complications | 0.772 | 0.152 | ||||||
| I | 9 (2.4) | 2 (3.8) | 0 (0.0) | 2 (5.0) | ||||
| II | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||
| IIIa | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||
| IIIb | 4 (1.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||
| IV | 2 (0.5) | 2 (3.8) | 0 (0.0) | 0 (0.0) | ||||
| Urinary incontinence | 56 (15.1) | 9 (17.3) | 0.841 | 5 (12.5) | 6 (15.0) | >0.999a | ||
| Type of urinary incontinence | 30 (60.0) | 6 (66.7) | 0.415 | 4 (80.0) | 4 (66.7) | 0.231 | ||
| Stress | ||||||||
| Urge | 8 (16.0) | 0 (0.0) | 1 (20.0) | 0 (0.0) | ||||
| Mixed | 12 (24.0) | 3 (33.3) | 0 (0.0) | 2 (33.3) | ||||
| Duration of urinary incontinence | 23 (46.0) | 3 (33.3) | 0.582 | 3 (60.0) | 2 (33.3) | 0.392b | ||
| Up to 1 month | ||||||||
| From 1 to 3 months | 25 (50.0) | 5 (55.6) | 2 (40.0) | 4 (66.7) | ||||
| More than 3 months | 2 (4.0) | 1 (11.1) | - | - | ||||
| Kegel exercises | 43 (89.6) | 8 (88.9) | 0.662b | 4 (80.0) | 5 (83.3) | 0.727b | ||
| Incidental prostate cancer | 15 (4.1) | 2 (3.8) | 0.650b | 2 (5.0) | 2 (5.0) | 0.608b | ||
| Late postoperative complication | 8 (2.2) | 3 (5.8) | 0.163 | 1 (2.5) | 2 (5.0) | 0.223 | ||
| Urethral stricture requiring dilatation | 1 (0.3) | 2 (3.8) | 0 (0.0) | 1 (2.5) | ||||
| Urethral strictures requiring urethrotomy | 1 (0.3) | 1 (1.9) | ||||||
| Bladder neck contracture | 5 (1.4) | 0 (0.0) | 0 (0.0) | 1 (2.5) | ||||
| Repeated surgery for BPH | 1 (0.3) | 0 (0.0) | 1 (2.5) | 0 (0.0) | ||||
Values are presented as median (interquartile range) or number (%).
PS, propensity score; ThuFLEP, thulium fiber laser enucleation of the prostate; BPH, benign prostatic hyperplasia.
a:Pearson’s chi-square test with Yates’s continuity correction.
b:One-tailed Fisher’s exact test; without aPearson’s chi-square test.
Two patients from the ThuFLEP group (0.5%) had major cardiovascular complications (acute myocardial infarction and pulmonary embolisms), but these complications were successfully resolved. A total of 5.9% of patients in the ThuFLEP group and 7.7% in the bipolar enucleation group had early postoperative complications (p=0.847). Urinary incontinence was observed in 15.1% and 17.3% of patients, respectively (p=0.841); urinary incontinence persisted for more than 3 months in only 3 patients. After histological examination, 4.1% of patients from the ThuFLEP group and 3.8% from the bipolar enucleation group were found to have incidental prostate cancer. Patients were under active surveillance without progression.
Late postoperative complications included urethral strictures (0.5% for ThuFLEP and 5.8% for bipolar enucleation), bladder neck contracture (1.4% for ThuFLEP), and repeated surgery for BPH (0.3% for ThuFLEP). All complication rates before as well as after PS-matched analysis were comparable, which indicated that the effectiveness of these procedures was similar.
DISCUSSION
Publications comparing ThuFLEP with other enucleation techniques are limited in open sources. ThuFLEP has been compared with HoLEP, monopolar enucleation, open simple prostatectomy, and transurethral resection the prostate (TURP), but no studies have compared ThuFLEP with classic bipolar enucleation. However, this was the aim of our study, which was the first to compare perioperative, functional, and safety outcomes between ThuFLEP and bipolar enucleation of the prostate performed by a single surgeon by use of PS-matched analysis.
Some studies have compared ThuFLEP with other modalities, but none have compared ThuFLEP and bipolar enucleation. Perioperative parameters such as operation time, enucleation time, and morcellation time are similar between ThuFLEP and other enucleation methods. According to Bozzini et al. [10], mean operation time for ThuFLEP was 70.7 minutes, which was comparable with ThuLEP. In the study by Enikeev et al. [9], operation time was 103.2 minutes, which may be related to the large total prostate volume (127 cm3) or early step of enucleation. In 2019 Enikeev et al. [8] reported about 46.6 minutes for ThuFLEP with mean prostate volume of 63.3 cm3. We obtained similar data in our study with a median operation time for ThuFLEP of 75 minutes with median prostate volume of 84 cm3. Operation time, enucleation time, and morcellation time were comparable between ThuFLEP and bipolar enucleation as well as before and after PS matching.
According to Petov et al. [12], ThuFLEP is considered an effective and safe method of endoscopic enucleation characterized by improvement of all functional parameters (IPSS, QoL, PVR, Qmax) after surgery (p<0.05) with durable improvement lasting for up to 3 years of follow-up. Similar results were reported by Bozzini et al. [10] with 3 months of follow-up. Similar data are observed in all studies about ThuFLEP, indicating the good functional results and effectiveness of this procedure [8,11]. A systematic review of Tm-fiber was published in 2021 under the guidance of Rice and Somani [13]. That study showed a significant improvement in IPSS, Qmax, QoL score, and PVR [13], which was also confirmed in our study. According to the Friedman test, significant improvements in IPSS, QoL score, Qmax, and PVR were observed during the 24-month follow-up period for both ThuFLEP and bipolar enucleation. Moreover, there were no significant differences in these parameters between the groups at any follow-up time point (p>0.05).
It was shown in 2018 that patients treated with ThuFLEP had a significant improvement in the IIEF-5 (5-item International Index of Erectile Function) score compared with TURP at 6 months after surgery [14]. The authors suggested that this was due to a lower penetration depth of the Tm-fiber, allowing safer incisions with less risk of surgical capsule penetration and, therefore, less damage to the neurovascular bundles at the posterolateral surface of the prostate [14].
According to Petov et al. [12], ThuFLEP has a low incidence of complications after 3 years of follow-up. Stress urinary incontinence was observed in 1.2% of patients, urethral stricture in 1.1%, and bladder neck contracture in 0.9% of patients [12]. This is similar to our data, but we had an even lower percentage of late complications: only 2 patients (0.5% of total) from the ThuFLEP group had stress urinary incontinence lasting more than 3 months. Urethral stricture and bladder neck contracture occurred in 2 patients (0.5% of total) and 5 patients (1.4% of total), respectively, which also confirms Petov et al.’s data [12] about the safety of ThuFLEP. In 2023 ThuFLEP was compared with ThuLEP by Bozzini et al. [10]. During 3 months of follow-up, the theoretical advantages of Tm-fiber such as a shallower penetration depth and improved vaporization capacity, did not translate into relevant perioperative outcomes or clinical differences [10].
In a randomized study conducted in 2019, ThuFLEP was compared with monopolar TURP in patients with smaller-sized prostates of less than 80 cm3 [8]. Short-term stress urinary incontinence was observed in 7 patients (13.7% of total), but at 6 and 12 months of follow-up, these percentages were 1.9% and 1.9%, respectively. Clot retention occurred in 5.8% of patients, but no patients required surgical revision. Acute urinary retention was found in 1.9% of patients and urinary tract infection in 3.9%. Among late postoperative complications, urethral stricture with no bladder neck contracture occurred in 1.9% of patients. The same level of postoperative complications was observed for monopolar TURP [8]. Complication rates were similar in our study.
A further randomized prospective trial compared ThuFLEP with HoLEP. No differences were found in number of postoperative complications, catheterization time, or hospital stay [11]. These data were also confirmed by a large analysis from the REAP Registry. In that analysis, early and delayed outcomes of enucleation with ThuFLEP were comparable to those with high-powered HoLEP, with similar improvements in micturition parameters and IPSS [15]. The same data were observed in our study, but for ThuFLEP and bipolar enucleation: ThuFLEP was associated with a low level of early and late postoperative complications that were comparable with bipolar enucleation despite the physical benefits of Tm-fiber.
As for cost effectiveness, there are no comparative trials available, but multiple factors make ThuFLEP a cost-effective procedure. According to Wani et al. [16], the cost of Tm-fiber is about 400 pounds each, which is comparable to other laser systems; in contrast, however, Tm-fiber can be used many times, which amounts to negligible running costs.
Therefore, ThuFLEP is characterized by high efficiency and safety comparable with classic bipolar enucleation, as was proved in our present study. As previously found, ThuFLEP is also comparable with ThuLEP, HoLEP, and monopolar enucleation and has some advantages over open simple prostatectomy and TURP. It also seems to be a cost-effective procedure with a good influence on erectile function because of its physical characteristics. These data confirmed the early expectations of Kronenberg and Traxer [6], who wrote that Tm-fiber is “the laser of the future”; but at the same time: “Enucleation is enucleation is enucleation is enucleation” [4].
The main limitation of our study is the retrospective design, but we attempted to exclude potential bias by using the PS-matched analysis. One potential bias is the single surgeon; however, we believe that this fact allows us to avoid the inaccuracy of various manual aspects during the operation and can be considered a strength of our work. Still, the present study is the first trial with comparison of ThuFLEP and bipolar enucleation.
CONCLUSIONS
ThuFLEP was comparable to bipolar enucleation in terms of perioperative characteristics, improvement in voiding parameters, and complication rates. Operation time, enucleation time, morcellation time, postoperative IPSS, QoL, Qmax, and PVR during follow-up showed no significant differences. Thus, both procedures have been shown to be effective and safe in the management of BPH.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING: The study was conducted under the state task (number: 0908.003.006) force of the Medical Research and Educational Center of Lomonosov Moscow State University.
- Research conception and design: Nikolay Ivanovich Sorokin and Armais Albertovich Kamalov.
- Data acquisition: Nikolay Ivanovich Sorokin, Vitaly Kazichanovich Dzitiev, and Andrey Alekseevich Strigunov.
- Statistical analysis: Olga Yurevna Nesterova.
- Data analysis and interpretation: Nikolay Ivanovich Sorokin, Andrey Alekseevich Strigunov, and Olga Yurevna Nesterova.
- Drafting of the manuscript: Andrey Alekseevich Strigunov, Olga Yurevna Nesterova, and Ilya Vladimirovich Bondar.
- Critical revision of the manuscript: Nikolay Ivanovich Sorokin and Armais Albertovich Kamalov.
- Obtaining funding: Armais Albertovich Kamalov.
- Administrative, technical, or material support: Nikolay Ivanovich Sorokin and Armais Albertovich Kamalov.
- Supervision: Nikolay Ivanovich Sorokin and Armais Albertovich Kamalov.
- Approval of the final manuscript: all authors.
References
- 1.Langan RC. Benign prostatic hyperplasia. Prim Care. 2019;46:223–232. doi: 10.1016/j.pop.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Apolihin OI, Sivkov AV, Zolotuhin OV, Shaderkin IA, Voytko DA, Prosyannikov MY, et al. [Prevalence of lower urinary tractsymptoms in men according to the results of population research] Eksp Klin Urol. 2018;(1):4–12. Russian. [Google Scholar]
- 3.European Association of Urology. EAU guidelines. EAU Guidelines Office; 2023. [Google Scholar]
- 4.Herrmann TR. Enucleation is enucleation is enucleation is enucleation. World J Urol. 2016;34:1353–1355. doi: 10.1007/s00345-016-1922-3. [DOI] [PubMed] [Google Scholar]
- 5.Ortner G, Pang KH, Yuan Y, Herrmann TRW, Biyani CS, Tokas T. Peri- and post-operative outcomes, complications, and functional results amongst different modifications of endoscopic enucleation of the prostate (EEP): a systematic review and meta-analysis. World J Urol. 2023;41:969–980. doi: 10.1007/s00345-023-04308-z. [DOI] [PubMed] [Google Scholar]
- 6.Kronenberg P, Traxer O. The laser of the future: reality and expectations about the new thulium fiber laser-a systematic review. Transl Androl Urol. 2019;8(Suppl 4):S398–S417. doi: 10.21037/tau.2019.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doizi S, Germain T, Panthier F, Compérat E, Traxer O, Berthe L. Comparison of holmium:YAG and thulium fiber lasers on soft tissue: an ex vivo study. J Endourol. 2022;36:251–258. doi: 10.1089/end.2021.0263. [DOI] [PubMed] [Google Scholar]
- 8.Enikeev D, Netsch C, Rapoport L, Gazimiev M, Laukhtina E, Snurnitsyna O, et al. Novel thulium fiber laser for endoscopic enucleation of the prostate: a prospective comparison with conventional transurethral resection of the prostate. Int J Urol. 2019;26:1138–1143. doi: 10.1111/iju.14115. [DOI] [PubMed] [Google Scholar]
- 9.Enikeev D, Okhunov Z, Rapoport L, Taratkin M, Enikeev M, Snurnitsyna O, et al. Novel thulium fiber laser for enucleation of prostate: a retrospective comparison with open simple prostatectomy. J Endourol. 2019;33:16–21. doi: 10.1089/end.2018.0791. [DOI] [PubMed] [Google Scholar]
- 10.Bozzini G, Berti L, Maltagliati M, Besana U, Micali S, Roche JB, et al. Thulium: YAG vs continuous-wave thulium fiber laser enucleation of the prostate: do potential advantages of thulium fiber lasers translate into relevant clinical differences? World J Urol. 2023;41:143–150. doi: 10.1007/s00345-022-04201-1. [DOI] [PubMed] [Google Scholar]
- 11.Enikeev D, Taratkin M, Babaevskaya D, Morozov A, Petov V, Sukhanov R, et al. Randomized prospective trial of the severity of irritative symptoms after HoLEP vs ThuFLEP. World J Urol. 2022;40:2047–2053. doi: 10.1007/s00345-022-04046-8. [DOI] [PubMed] [Google Scholar]
- 12.Petov V, Babaevskaya D, Taratkin M, Chuvalov L, Lusuardi L, Misrai V, et al. Thulium fiber laser enucleation of the prostate: prospective study of mid- and long-term outcomes in 1328 patients. J Endourol. 2022;36:1231–1236. doi: 10.1089/end.2022.0029. [DOI] [PubMed] [Google Scholar]
- 13.Rice P, Somani BK. A systematic review of thulium fiber laser: applications and advantages of laser technology in the field of urology. Res Rep Urol. 2021;13:519–527. doi: 10.2147/RRU.S233979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Enikeev D, Glybochko P, Rapoport L, Okhunov Z, O'Leary M, Potoldykova N, et al. Impact of endoscopic enucleation of the prostate with thulium fiber laser on the erectile function. BMC Urol. 2018;18:87. doi: 10.1186/s12894-018-0400-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gauhar V, Nedbal C, Castellani D, Fong KY, Sofer M, Socarrás MR, et al. Comparison between thulium fiber laser and high-power holmium laser for anatomic endoscopic enucleation of the prostate: a propensity score-matched analysis from the REAP registry. Eur Urol Focus. 2023 Jul 04; doi: 10.1016/j.euf.2023.06.009. [Epub] [DOI] [PubMed] [Google Scholar]
- 16.Wani MM, Sriprasad S, Bhat T, Madaan S. Is Thulium laser enucleation of prostate an alternative to Holmium and TURP surgeries - a systematic review? Turk J Urol. 2020;46:419–426. doi: 10.5152/tud.2020.20202. [DOI] [PMC free article] [PubMed] [Google Scholar]