Abstract
This tutorial of the intrapartum management of shoulder dystocia utilizes drawings and videos of simulated and actual deliveries to illustrate the biomechanical principles of specialized delivery maneuvers and examine missteps associated with brachial plexus injury. It is intended to complement haptic, mannequin-based simulation training. Demonstrative explication of each maneuver is accompanied by specific examples of what not to do. Positive (prescriptive) instruction prioritizes early use of direct fetal manipulation and stresses the importance of determining the alignment of the fetal shoulders by direct palpation; before application of traction to the fetal head, the biacromial width is then manually adjusted to an oblique orientation within the pelvis. Negative (proscriptive) instructions include: to avoid more than usual and/or laterally-directed traction; only use episiotomy as a means to gain access to the posterior shoulder and arm; and to utilize a two-step procedure in which a 60-second hands-off period (“do not do anything”) is inserted between emergence of the head and any initial attempts at downward traction to allow for spontaneous rotation of the fetal shoulders. The tutorial presents an stepwise approach focused on the delivering clinician’s tasks, while including the role of assistive techniques, including McRoberts, Gaskin, and Sims positioning, suprapubic pressure and episiotomy. Video footage of actual deliveries involving shoulder dystocia and permanent brachial plexus injury demonstrate ambiguities in making the diagnosis of shoulder dystocia, risks of improper traction and torsion of the head, and over-reliance on repeating maneuvers that prove initially unsuccessful.
CONDENSATION
Management of shoulder dystocia requires equal attention to skillful execution of maneuvers and avoidance of missteps in order to lessen delivery force and reduce injury.
Since shoulder dystocia once it occurs is an emergency – and its treatment frequently involves internal manipulations that cannot be observed directly by learners – intrapartum management of shoulder dystocia is one of the earliest1 – and most common – obstetric scenarios used in simulation training. In the safe environment of simulation, preceptors observe one-on-one as trainees demonstrate their execution of shoulder dystocia maneuvers on a task trainer or mannequin; however, the opportunity to review and appraise critical injury-producing errors may or may not materialize for each simulation participant, unless deliberately included in the instructional content.
Indeed, a systematic review of original research comparing curricular content of shoulder dystocia simulation reveals several critical gaps: Prescriptive (i.e., positive, what to do) instruction that prioritizes maneuvers shown to decrease strain on the brachial plexus is inconsistently utilized. Proscriptive (i.e., negative, what not to do) instruction to avoid laterally-directed or torsional traction on the head is infrequently explicit.2
What follows is a technical and videographical tutorial about the intrapartum management of shoulder dystocia, utilizing drawings and videos of simulated3 and actual4 deliveries to illustrate the biomechanical principles of specialized delivery maneuvers and to examine missteps associated with brachial plexus injury.4 It is intended to complement haptic, mannequin-based simulation training.3
PATHOPHYSIOLOGY OF SHOULDER DYSTOCIA
Although maternal soft tissues may impede delivery to some degree, shoulder dystocia is fundamentally a problem of bony impaction – anterior shoulder against pubic bone or posterior shoulder against the sacral promontory, or both – and represents relative fetopelvic disproportion. Its resolution therefore depends upon the relief of the obstruction through a series of maneuvers designed to reestablish the physiologic orientation of the fetal biacromial dimension within the optimal oblique diameter of the maternal pelvic outlet (Figure 1).
Figure 1:
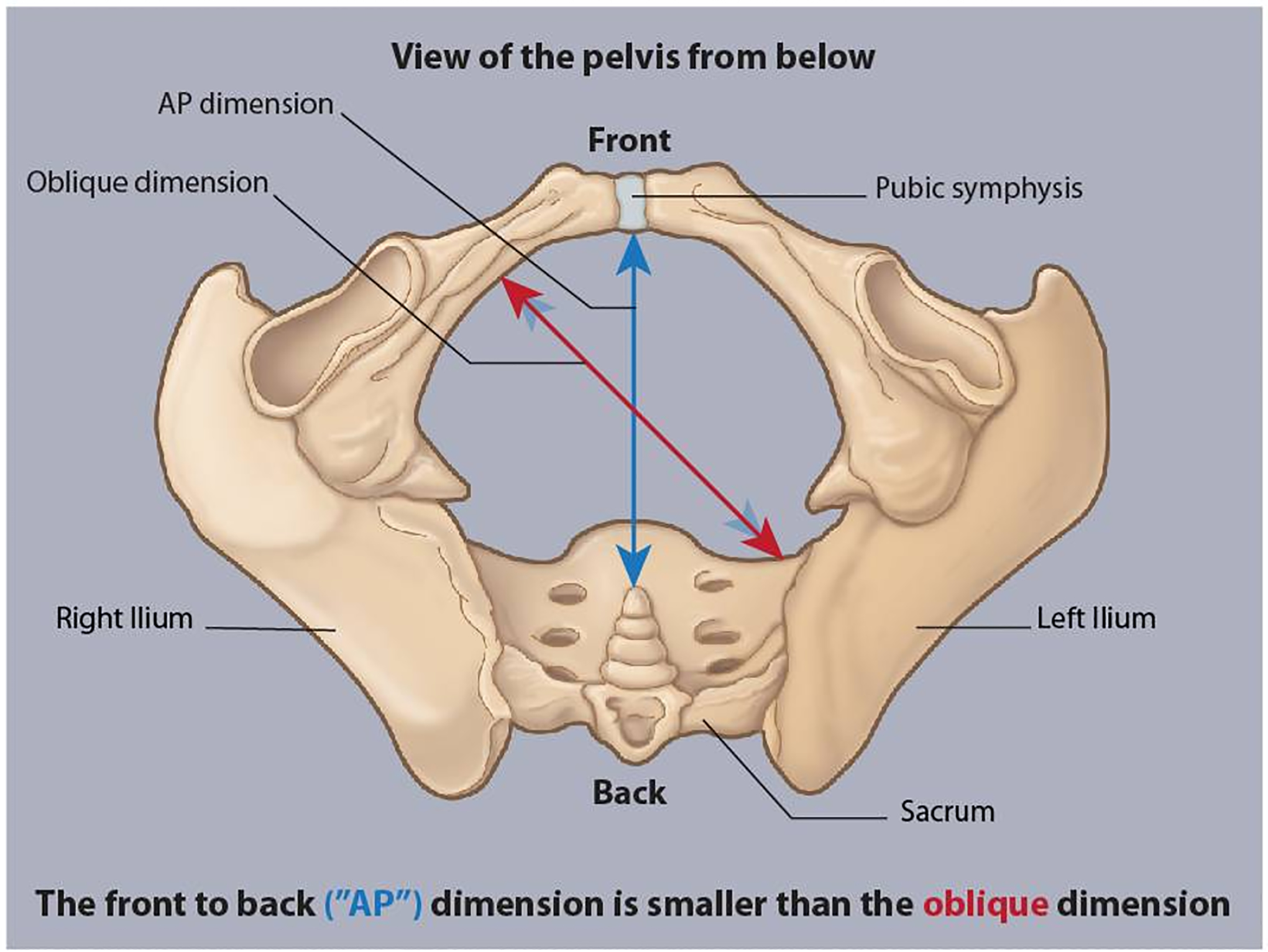
In the gynecoid pelvic outlet, as viewed in the transverse plane, the anterior-posterior dimension of the pelvic outlet (measured from the pubic symphysis to the tip of the coccyx) is about 10.5 cm in length. The oblique dimension is about 2 cm wider, measuring on average 12.5 cm in length. The latter dimension best accommodates the fetal shoulder width (biacromial diameter) during normal vaginal delivery.
As a result of human evolution to bipedalism (Figure 2A), the planes of the pelvic inlet and pelvic outlet are skew with respect to each other (giving the birth canal the shape of a bent rather than straight cylinder, [Figure 2B]).5 Therefore, during cephalic birth, the fetal head and the aftercoming body follow a winding motion, with fetal bony landmarks (e.g., the occiput and the acromion process, coming into contact with bony landmarks of the pelvis (e.g., the sacral promontory, the pubic symphysis and the coccyx) in a sequential rather than simultaneous fashion – as though progressing through the threads of a screw. During the cardinal movement of internal rotation, over the course of fetal descent through the pelvis, the fetal head undergoes a 90-degree realignment from the occiput transverse position in which it enters the pelvic inlet to the occiput anterior (or less commonly posterior) position adopted as it traverses the pelvic outlet.
Figure 2:
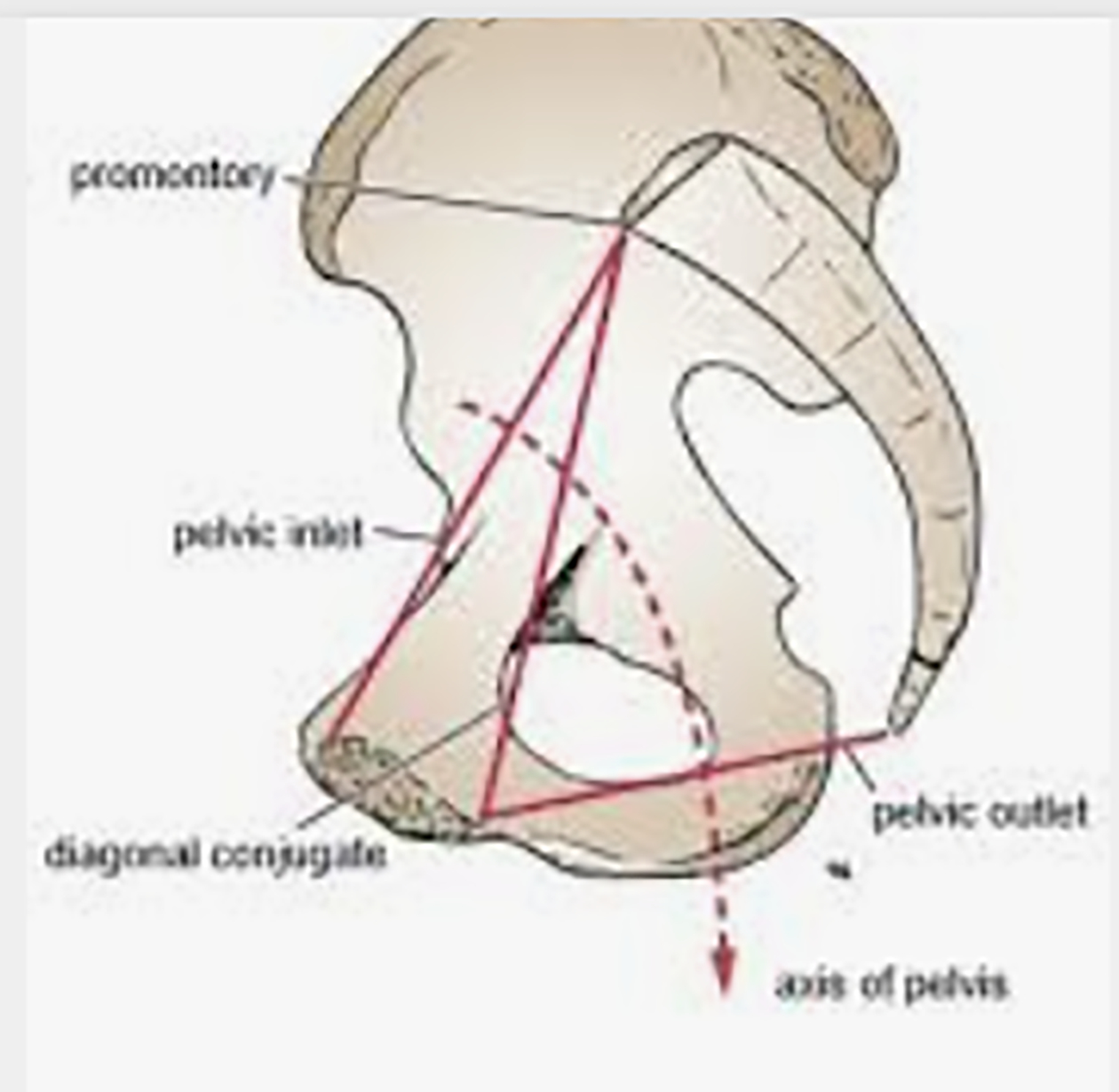
A: Sagittal CT of the pelvis in upright position illustrates that the pelvic inlet and pelvic outlet do not lie in parallel planes. B: The cavity of the true pelvis is comparable to bent cylinder. Note the curvature of the pelvic axis. As with the mechanical threads of a screw, which are aligned in skew orientation, a rotational motion at one end produces forward progression.
Logically, the fetus’ shoulder width must follow similar rotations that the fetal head undergoes as it negotiates its passage through the birth canal.5 Early on in fetal descent, when the head enters the pelvic inlet in occiput transverse position, the shoulders are oriented in the anterior-posterior dimension. Thereafter, the head internally rotates and then extends to exit the vagina; at this moment, it as though the fetus has turned its head to look at its posterior shoulder. By the time of external rotation of the fetal head, after its emergence through the introitus (known as restitution), the head rotates from direct occiput anterior (or less commonly direct occiput posterior) position to adopt a more oblique-transverse position – either left or right occiput anterior (or posterior) position. Under usual physiologic circumstances, subsequent rotation of the head outside the vagina occurs as the aftercoming fetal shoulders are able to descend past the pelvic inlet – where they were oriented antero-posteriorly – and rotate within the birth canal to align within the oblique diameter of the pelvic outlet (perpendicular to the oblique diameter the head position now occupies), such the head has resumed its neutral position relative to the shoulders.6
In instances where either the fetal body is relatively large compared to the head (known as macrosomia) or the fetal body has been pulled further down into direct contact with the pubic symphysis during the process of an operative delivery or rapid descent, the fetal shoulders either rotate more slowly or have less time to rotate to the oblique during restitution of the head, and thus could remain in the anterior-posterior orientation at the pelvic inlet after the head restitutes, giving rise to the potential for shoulder dystocia to ensue.
RECOGNITION OF SHOULDER IMPACTION AND SELF-REGULATION OF APPLIED TRACTION
The most significant risk factors for the occurrence of shoulder dystocia are a prior history of shoulder dystocia;7 diabetes – especially when associated with accelerated fetal somatic growth compared to the fetal head; estimated fetal weight above 5,000 g (or 4,500 g for diabetic women)8 and operative – especially midpelvic9 – vaginal delivery.10,11 Either a prolonged or precipitous second stage of labor is a frequent antecedent of shoulder dystocia.12 Prepregnancy baseline maternal obesity, as well as excessive gestational weight gain, predispose to high birth weight and thus to shoulder dystocia.13 Nevertheless, women with risk factors – even if multiple – are more likely to have an uncomplicated delivery than to experience shoulder dystocia; whereas half the deliveries complicated by shoulder dystocia occur in the absence of any risk factors.14–17 Thus, the actual occurrence of shoulder dystocia, which complicates between 2–4%15,18 of term cephalic vaginal deliveries, remains largely unpredictable and therefore unpreventable. Consequently, every obstetric provider, regardless of discipline or specialty training, must be vigilant at each delivery and be able to manage this complication with alacrity and skill.
Management of shoulder dystocia begins with the prospective recognition of probable shoulder impaction. Slow fetal head expulsion, the need to coax the fetal brow and chin past the introitus with one’s fingers, and/or retraction of the fetal head against the perineum immediately following complete delivery of the head, are all variations of the “turtle sign.” However, this harbinger of shoulder dystocia is neither pathognomonic nor omnipresent. Therefore, probable shoulder impaction should be anticipated immediately upon the obstetric provider’s appreciation that more than the usual amount of traction would be required to complete the delivery of the fetus’ trunk after its head has emerged through the vaginal introitus. A confirmatory diagnosis of shoulder dystocia is based upon the clinician’s subjective appreciation that the anterior shoulder fails to deliver following application of customary traction only.
That delivering clinicians are capable of subjective self-assessment of their own applied delivery force has been demonstrated by Allen et al in simulated deliveries19 and by Mollberg et al in their series of prospectively followed live vaginal births.20 Yet, clinicians are more than 2.5 times as likely to distinguish a delivery “clinically complicated by some degree of shoulder impaction” than they are to use this criterion as a sole basis to diagnose shoulder dystocia.20,21 It is instructive that among the deliveries associated with brachial plexus injury in the Mollberg series, only 36.7% were given the diagnosis of shoulder dystocia; yet, 97.2% were identified as involving difficulty in delivering the shoulder.21
Video 1 is of a birth complicated by permanent brachial plexus injury. It is notable that the obstetrician included the diagnosis of shoulder dystocia in the medical record, despite not having used any standard shoulder dystocia maneuvers. While viewers of this video may debate whether shoulder dystocia actually occurred, nearly all will agree that more than customary traction was involved. Obstetric providers’ conscious awareness of -- and deliberate effort to – limit traction, as well as readiness to employ simple techniques to confirm and – if necessary – reestablish the physiologic orientation of the shoulders at every delivery is of greater importance in the prevention of brachial plexus injury than is the accuracy or certainty in ascertaining whether shoulder dystocia has occurred. A recent metanalysis of simulation-based training intervention to reduce brachial plexus injury found that simulation training is associated with an increase in the diagnosis of shoulder dystocia over time; and, that training with force measurement had a greater impact on this association.22 The occurrence of shoulder dystocia should not be regarded as evidence of poor obstetric management or even malpractice;16 neither should a higher rate of shoulder dystocia diagnoses at a given hospital be regarded as a poor key performance indicator. Indeed, clinicians are wise to maintain a high degree of suspicion and vigilance at every delivery, and to err toward rather than avoid making the diagnosis of shoulder dystocia.
Video 1:
Is it shoulder dystocia? Perhaps debatable. Is it “more than usual traction?” Most obstetric providers will agree that it is. Although the criteria for diagnosing shoulder dystocia depends on the provider’s (or researcher’s) definition, as a practical matter, if a clinician perceives that more than usual traction would be required to complete a delivery after the head has emerged through the vaginal introitus, maneuvers that lessen traction and reduce the risk of brachial plexus injury should be employed.
More than customary traction – and especially lateral (relative to the fetus’ vertebral axis) traction in the context of shoulder dystocia (Table 1) – is associated with permanent brachial plexus injury.21,23–29 Yet, the application of traction is needed for diagnosis and management of shoulder dystocia – and thus its active, conscious limitation is an important proscriptive element of instruction. The American College of Obstetricians and Gynecologists’ Task Force on Simulation advises the use of “appropriate” traction to diagnose shoulder dystocia.30 The Royal College of Obstetricians and Gynaecologists states: “Routine traction in an axial direction may be employed to diagnose shoulder dystocia, but any other traction should be avoided.”31 The third edition of Normal and Problem Pregnancies advises: “Gentle symmetric pressure on the fetal head will move the posterior shoulder into the hollow of the sacrum and encourage delivery of the anterior shoulder. Care should be taken not to “pry” the anterior shoulder out asymmetrically, as this might lead to trauma to the anterior brachial plexus.”32
Table 1:
Studies showing the near universal association of permanent brachial plexus injury with antecedent shoulder dystocia.
| Study | Year | # Deliveries | Injury (N) T – temporary P - permanent |
Association with Shoulder dystocia |
|---|---|---|---|---|
| Wolf | 2000 | 9,912 | T (56) P (16) |
88% 94% |
| Morrison | 1992 | 37,000 | T (75) P (7) |
100% 100% |
| Ouzounian | 1997 | 63 | P (63) | 96% |
| Ubachs | 1995 | 102 | P (102) | 100% |
| Allen | 2002 | 103 | P (103) | 94% |
Failure to follow these directives is evident in Video 2, another example of a shoulder dystocia delivery that resulted in a severe, permanent pan-plexus injury. Several learning points from this video include:
A clear turtle sign is exhibited at the beginning of the tape.
The delivering clinician has placed both hands atop the fetal head (rather than symmetrically balancing the hands above and below the head) and utilizes her entire body weight in a downward directed application of traction on the fetal head and neck. This action is repeated 11 times (!) over a head-to-body interval of 3 minutes’ duration. The risk of permanent brachial plexus injury increases with serially repeated unsuccessful maneuvers. Attempting a different maneuver at least every 30 seconds is associated with a lower incidence of permanent brachial plexus injury.33
Video 2:
Repeated, asymmetric, downward-directed traction on the head and neck during a three-minute shoulder dystocia resulted in a severe, pan-plexus injury.
In simulation training, the magnitude of delivery force applied by different types of clinicians during shoulder dystocia does not vary by provider experience, body weight or gender; however, forty percent of all clinicians apply more than 100 N34 (regarded as the threshold for brachial plexus injury35). Of note, observers – such as supervising attendings or simulation preceptors – are not able to visually estimate traction force with sufficient accuracy.36 Thus, it is incumbent upon the clinician to regulate his own applied traction at every delivery.
AWAITING THE NEXT CONTRACTION
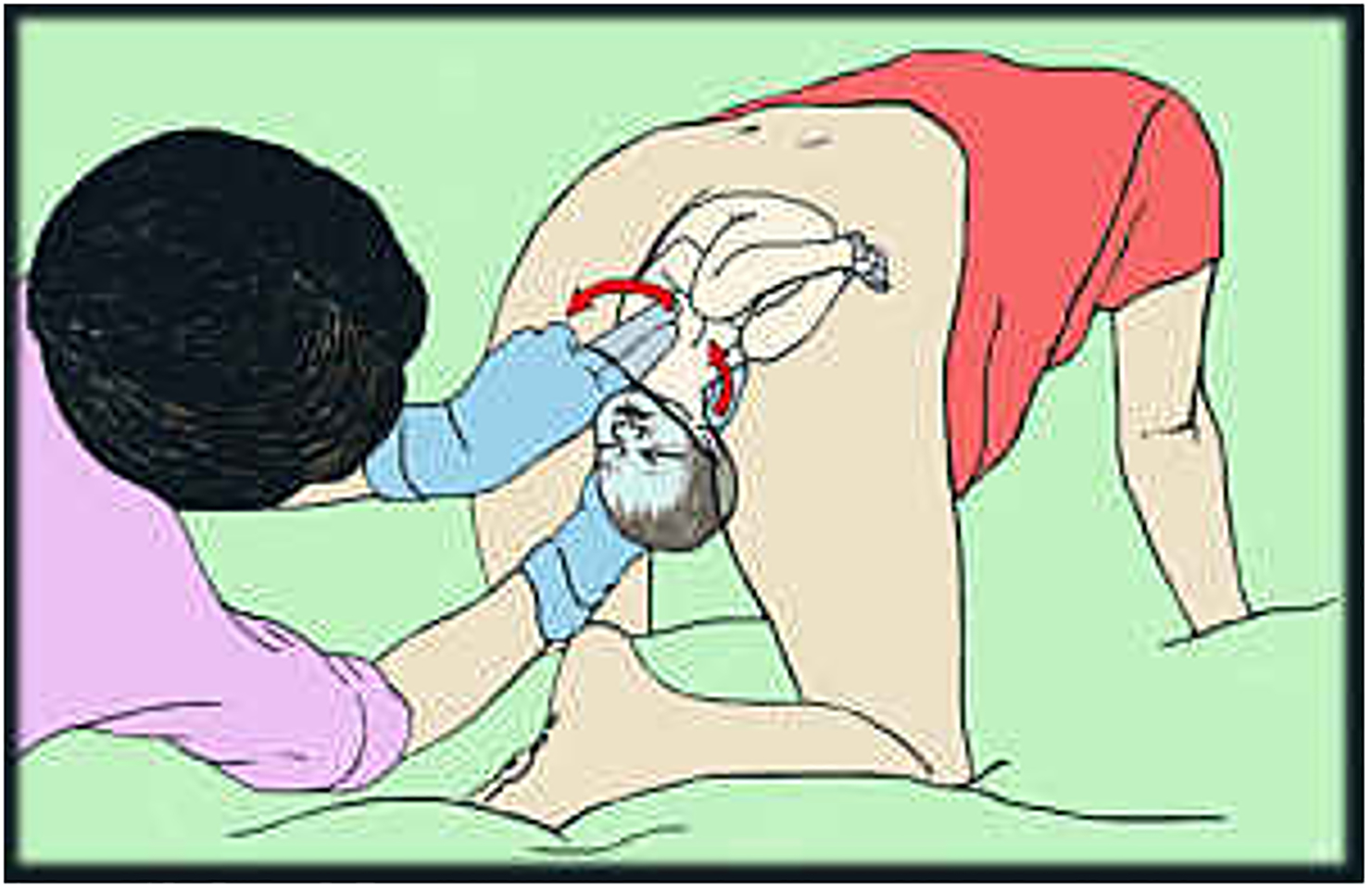
An appreciation of the aforementioned combination of static (fetopelvic) and dynamic (time-based) aspects of the pathophysiology of shoulder dystocia are vital to understanding the biomechanical and time-based approaches to its intrapartum management. Beall et al utilized an objective measure of head-to-body interval of 60 seconds or more to define shoulder dystocia, prospectively determining an incidence of 4% among term, cephalic vaginal deliveries based on this criterion.37 This suggests that allowing for a pause of just one minute, during which 96% of fetuses will spontaneously restitute to an unobstructed position that is optimal for delivery, can prevent shoulder dystocia occurring in the first place – as most fetuses will fully expel unimpeded before 60 seconds elapse. Indeed, Locatelli et al conducted a prospective observational study of awaiting the next contraction following delivery of the fetal head before application of traction and noted a marked reduction in shoulder dystocia (only 3 occurrences in 800 deliveries), without deleterious effects on neonatal outcome (e.g., low Apgar scores, fetal acidosis, or need for additional resuscitation).38 This time can be utilized instead to check for the presence of a nuchal cord and reduce it if possible, clear the oro- and nasopharynx with a bulb suction, and assess digitally the position of the shoulders within the pelvis (Figure 3).39,40 Inglis et al found that a deliberate “hands off” period, followed by checking the position of the fetal shoulders and then repositioning the biacromial dimension to the oblique position within the pelvic inlet (see explication of Rubin’s maneuver below) in response to shoulder dystocia was associated with a 66% reduction of brachial plexus injury, an increase in head-to-body interval of only 30 seconds and no difference in neonatal depression.41
Figure 3:

In the conduct of normal labor and delivery, the birth attendant should manually check the orientation of the shoulders using direct digital palpation, before applying initial traction on the head. Reprinted with permission.40
Video 3 is of another delivery complicated by a 70-second shoulder dystocia, which resulted in a permanent pan-plexus injury with multiple nerve root avulsions and phrenic nerve involvement. Several missteps are evident here and useful for demonstrating important proscriptive lessons (i.e., what not to do) in the intrapartum management of shoulder dystocia:
No time was allotted for spontaneous restitution. Furthermore, there was no confirmation of the true position of the head relative to the shoulders (i.e., determining which shoulder was in fact the anterior shoulder and thus which way the head should have been facing) before manually rotating the head. In fact, both obstetric42 and midwifery43 literature discuss the importance of assessing shoulder position before applying traction during the conduct of normal labor and delivery. By the end of the 70-second head-to-body interval in this delivery, it is evident that the fetus eventually rotated its left (anterior) shoulder to the oblique diameter on its own, having not been directly manipulated by the delivering clinician. Had the clinician only been patient, shoulder dystocia in this case could have been avoided.
Experiments on cadavers demonstrate that the combination of torque (twist) with concomitant traction (elongation) is most injurious to the brachial plexus.44,45 This is consistent with the severe pan-plexus injury that resulted from this delivery, which included avulsions of the upper plexus. The latter is rare compared to avulsions of the lower plexus, unless there has been torque as well as elongation force applied.46
The episiotomy performed in this case was inadequate to increase access to the vagina to perform fetal manipulation. On its own, episiotomy will be insufficient to overcome the bony impaction that is shoulder dystocia, and thus the use of episiotomy should not be relied upon to relieve shoulder dystocia when initial maneuvers have failed. Rather, it should be utilized only when needed to gain access to vagina in order to perform direct fetal manipulation. In fact, in cases of severe shoulder dystocia where direct fetal manipulation was performed without the use of episiotomy, 50% emerged with an intact perineum.47
Video 3:
Manual rotation of the head without first determining the relative position of the fetal shoulders increases the risk that inappropriate torque will be placed on the neck. When combined with lateral traction, avulsions of the upper plexus can result, as occurred in this delivery. Failure to allow for spontaneous restitution following the delivery of the head increases the likelihood of shoulder dystocia.
CRITICAL FIRST RESPONSES
After allowing for spontaneous restitution, only a single attempt at delivery should be made by applying symmetric and axially-directed pressure and limited traction on the head, taking care to maintain the axial alignment of the neck with the spine. If the anterior shoulder fails to deliver, shoulder dystocia is confirmed. All action should immediately stop and both the team and the parturient must be informed of the diagnosis of shoulder dystocia. The labor nurse should mark the time and then call out every 30 second interval thereafter.48
Further delivery attempts without first employing ancillary maneuvers or techniques designed to relieve the obstruction will increase the risk of brachial plexus injury. However, there is a competing risk to consider: Since it is unknown how much, if any, of the umbilical cord may be compressed between the fetal body and the pelvic sidewalls, the “4-minute rule” – the head-to-body interval in which delivery should be accomplished in order to mitigate fetal asphyxia or death – should apply. Nevertheless, haste and adrenaline-mediated augmented forcefulness will prove counterproductive. It is important to maintain a calm demeanor, establish one’s leadership role, and avoid panicked and rushed actions. Try to maintain eye contact with the mother and ensure she is not attempting to push. Request additional assistance from available obstetric, pediatric, nursing and anesthesiology personnel. A coordinated approach to resolving the dystocia will be needed.
Suprapubic Pressure with Anterior Rubin’s Maneuver
Having assessed the fetus’ biacromial diameter to be in direct antero-posterior position, the primary goal should be to re-establish its physiologic position in the oblique diameter – as an initial approach.41 Rotating the shoulders to the oblique diameter of the pelvis may be accomplished externally by the application of suprapubic pressure – as described in Video 4 – or internally by applying pressure behind either the anterior or posterior shoulder’s scapula (also known as Rubin’s maneuver), as demonstrated in Video 5. However, it is best to coordinate rotation of the fetal shoulders to the oblique position with assistance from the labor nurse: First, apply pressure behind the anterior shoulder (rotating 30 degrees clockwise if the fetus’ left shoulder is anterior; counterclockwise if the right shoulder is anterior). Request the concomitant application of suprapubic pressure indicating from which side (from the mother’s right side pushing toward her left side if the fetus’ left shoulder is anterior; from the mother’s left side pushing toward her right side if the fetus’ right shoulder is anterior). Note that in Video 2 the suprapubic pressure was misapplied directly on top of rather than above the pubic bone and was not coordinated with an internal rotation of the anterior shoulder by the delivering clinician.
Video 4:
Correct application of suprapubic pressure is from the same side of the mother as the anterior shoulder’s scapula is located. Forward pressure toward the mother’s opposite side applied firmly with a fist or heel of the hand behind the anterior shoulder directs the shoulder off midline to an oblique orientation within the pelvis. The locus of pressure is directly above the pubic bone, neither fundal nor directly on the pubic bone; pressure is directly laterally and not vertically as the latter may lead to clavicle or ipsilateral humeral fractures. Since it is an indirect maneuver, suprapubic pressure should be coordinated with performance of Rubin’s maneuver on the anterior shoulder while a second obstetric assist completes the delivery by applying traction to the head.
Video 5:
The goal of Rubin’s maneuver, which involves the repositioning of the biacromial width to either oblique diameter, is to reestablish the physiologic orientation of the shoulders within the birth canal after the head has restituted. Rubin’s maneuver can be applied to either the anterior shoulder (in coordination with suprapubic pressure) or to the posterior shoulder (in coordination with McRoberts’ maneuver). It is the mechanically superior initial maneuver to use in response to shoulder dystocia, since it reduces the magnitude of subsequent traction applied to the head and is associated with less stretch of the brachial plexus compared to McRoberts’ maneuver utilized without concomitant rotation of the shoulders.
It is critical to verify which shoulder is the anterior shoulder by direct palpation of the scapula rather than relying on the direction the fetus appears to be facing (i.e., where the occiput is). Otherwise, inappropriate torque (as demonstrated in Video 3) may be applied inadvertently, increasing the risk of injury and rendering the application of suprapubic pressure ineffective.
Ideally, the concomitant application of direct pressure behind the anterior scapula should be maintained while a second obstetric provider attempts to deliver the fetus by repeating traction on the head using symmetric, axially-directed pressure. This coordinated technique can include the “ramp” maneuver, wherein the fingers of the hand applying pressure to the anterior scapula are guided between the acromion process and the pubic bone, creating a ramp to aid the extraction of the anterior shoulder from under the pubic symphysis. Although a similar effect can be achieved by inserting a curved blade (such as a Deaver retractor or one blade of an unfenestrated obstetric forceps pair), care is needed to avoid causing trauma to the urethra or bladder if an instrument is used.
McRoberts’ with Posterior Rubin’s Maneuver
In the event the coordination of pressure on the anterior shoulder (Rubin’s maneuver) combined with suprapubic pressure fails to overcome the obstruction – or if instead one intends to proceed directly to delivery of the posterior arm or to a corkscrew maneuver (discussed in more detail below) – the nurse should be explicitly instructed to discontinue the application of suprapubic pressure, as it will be counterproductive. Instead, nurses, or even lay support persons present in the delivery room, may assist by performing McRoberts’ maneuver (flexing the maternal thighs sharply against the abdomen as explained in Video 6) while rotation to the opposite oblique diameter is attempted by applying direct pressure on the posterior shoulder’s scapula (this time rotating counterclockwise if the right shoulder is posterior, clockwise if the left shoulder is posterior), again coordinated with the second assist’s delivery effort.
Video 6:
McRoberts’ maneuver is the sharp flexion of the maternal thighs against her abdomen, with her knees bent and directed toward the mother’s head (rather than toward her flanks), usually performed by nurses or lay support persons in attendance. Its goal is to lift and rotate the entire pelvis cephalad, thereby lifting the pubic bone over the anterior shoulder. As with suprapubic pressure, McRoberts’ maneuver is indirect, and should be accompanied by direct manipulation of the shoulders. Since McRoberts’ position also flattens the sacrum, its use assists the operator in grasping and shrugging the posterior shoulder, pulling it diagonally forward and into the hollow of the sacrum as either a posterior Rubin’s maneuver or before initiating delivery of the posterior arm or corkscrew maneuver.
The effectiveness of suprapubic pressure and McRoberts’ maneuver – each of which is an indirect manipulation of the fetal position relative to the mother’s pelvis – diminishes with increasing maternal obesity, especially with central adiposity. Thus, it is especially important to confirm that the fetus has rotated and/or the anterior shoulder has slipped under the pubic symphysis before applying traction to the fetal head.
ASSISTIVE SHOULDER DYSTOCIA MANEUVERS
Earlier versions of the American College of Obstetricians and Gynecologists’ Practice Bulletin entitled Shoulder Dystocia (originally published in 2002, reaffirmed in 2010) asserted that no maneuver is superior to another, and thus obstetric providers confronted with shoulder dystocia were encouraged to utilize the more intuitive and simpler technique of McRobert’s maneuver (Video 6) as a first line approach.49 However, compared to McRoberts’ maneuver, the direct adjustment of shoulder width by a 30-degree rotation to the either one of the oblique diameters of the pelvic outlet (i.e., Rubin’s maneuver, Video 5) restores the normal physiologic orientation that is optimal for delivery (Figure 4) and has similar efficacy to McRoberts’ maneuver in overcoming the initial impaction, but involves less traction force and less brachial plexus stretch (Table 2).50
Figure 4:
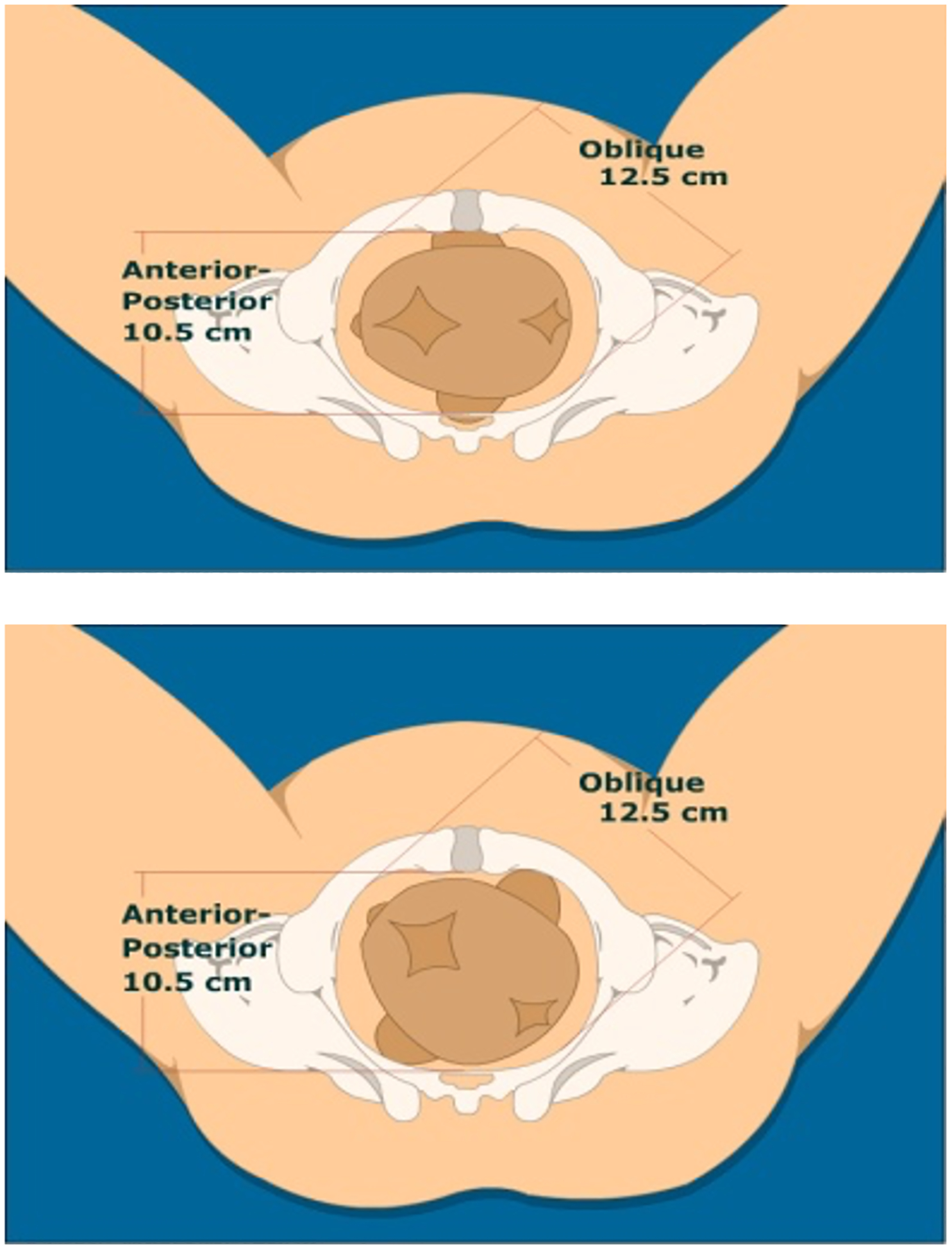
This schematic of posterior Rubin’s Maneuver – the 30-degree rotation/adduction of posterior shoulder to align with the oblique diameter of the pelvic inlet demonstrates its mechanical advantage in that it reestablishes the normal physiologic position, which is optimal for unobstructed vaginal delivery.
Table 2:
Comparing McRoberts’ and Rubin Maneuver As Initial Response to Shoulder Dystocia.
| McRoberts’ | Rubin’s | P value | |
|---|---|---|---|
| Traction force (lbs) | 16.2 ± 2.1 | 6.5 ± 1.8 | <0.0001 |
| Anterior BP stretch (mm) | 7.3 ± 2.5 | 2.9 ± 1.0 | 0.0003 |
| Posterior BP stretch (mm) | 2.3 ± 0.7 | 0.9 ± 0.1 | <0.0001 |
| Neck Rotation (degrees) | 14.5 ± 6.7 | 13.2 ± 3.3 | 0.09 |
BP: Brachial Plexus.
Adapted from Gurewitsch ED, Kim EJ, Yang JH, Outland KE, McDonald MK, Allen RH. (2005). Comparing McRoberts’ and Rubin’s maneuvers for initial management of shoulder dystocia: An objective evaluation. Am J Obstet Gynecol 2005:192(1):153–160.
Biomechanically, Rubin’s maneuver is more advantageous, in that it attains nearly 2 cm of additional space within the gynecoid pelvis for the shoulders to occupy. The anteroposterior dimension of the pelvic inlet in the majority of women who deliver vaginally is only 10.7 ± 0.9 cm, whereas the oblique diameter at the pelvic outlet, which is nearly round, is 12.1 ± 0.6 cm.51 On its own, McRoberts’ maneuver does not change the orientation of the shoulder width within the pelvis; rather it will lift the pubic symphysis one centimeter cephalad – up and over – the anterior shoulder.52 Given the mean biacromial diameter of term infants is 12.2 ± 1.0 cm,53 this explains why McRoberts’ maneuver as a single measure is only effective in 40% of deliveries complicated by shoulder dystocia.54 In instances where the shoulder width cannot be accommodated by lifting the pubic symphysis, McRoberts’ maneuver may displace the anterior shoulder further cephalad, increasing the risk of stretching the brachial plexus if combined with downward traction without first having also adjusted the orientation of the biacromial diameter to occupy an oblique position in the pelvis. This upper limit of effectiveness was confirmed in the original biomechanical study of McRoberts’ maneuver.55
Also noteworthy is that among the studies evaluating the clinical efficacy of simulation-based shoulder dystocia training for reducing the incidence of brachial plexus injury, those that did not yield a reduction in injury emphasized the use of McRoberts’ position as the initial response;56 whereas those that emphasized force measurement57 and prioritized direct fetal manipulation early in the algorithm41,58,59 showed a significant reduction in injuries over time.
Nevertheless, McRoberts’ positioning will flatten the sacrum, allowing the posterior shoulder that may be impinged on the sacral promontory to descend further into the hollow of the sacrum, facilitating the performance of posterior Rubin’s maneuver (as described above) or of more complex rotational maneuvers such as delivery of the posterior arm or corkscrew maneuver (explained in more detail below).52 A two-step procedure for adjusting the shoulders to the oblique diameter, wherein the posterior shoulder is first grasped and “shrugged” forward toward the hollow of the sacrum60 before attempting the rotation, can be combined with McRoberts’ maneuver. An instrumental variation of the shrug technique involves the use of a sling, fashioned from either suction tubing or a strong urinary catheter, threaded into the axilla of the posterior arm.61 Once again, caution is advised when using instruments in the setting of tight impactions within the birth canal, as injuries such as circumferential lacerations of the shoulder have been reported.62
Episiotomy
As discussed above, episiotomy should be thought of as an assistive maneuver, rather than a maneuver of its own: Episiotomy should be used only to facilitate gaining access to the hollow of the sacrum and thus to the posterior shoulder – if the provider is able to pass his full hand – including the thumb — up to the wrist without needing to cut soft tissue, the mother may be spared potential obstetric anal sphincter injuries associated with episiotomy.47
Gaskin’s Maneuver
Another assistive technique known as Gaskin’s maneuver involves having the mother assume an “all-fours” position (Figure 5). A less complicated repositioning to Sims position (Figure 6) may be more easily accomplished in situations where maternal mobility may be hampered by regional analgesia. Both these techniques can serve to dislodge and/or reorient the shoulder width from the anteroposterior to the oblique diameter of the pelvis; however, the provider still must confirm the oblique orientation of the shoulders or utilize Rubin’s or corkscrew maneuver to achieve it (Figure 5A). The birth attendant then performs downward traction on the head (Figure 5B), only now the top shoulder, which is the posterior shoulder, is delivered first.
Figure 5:
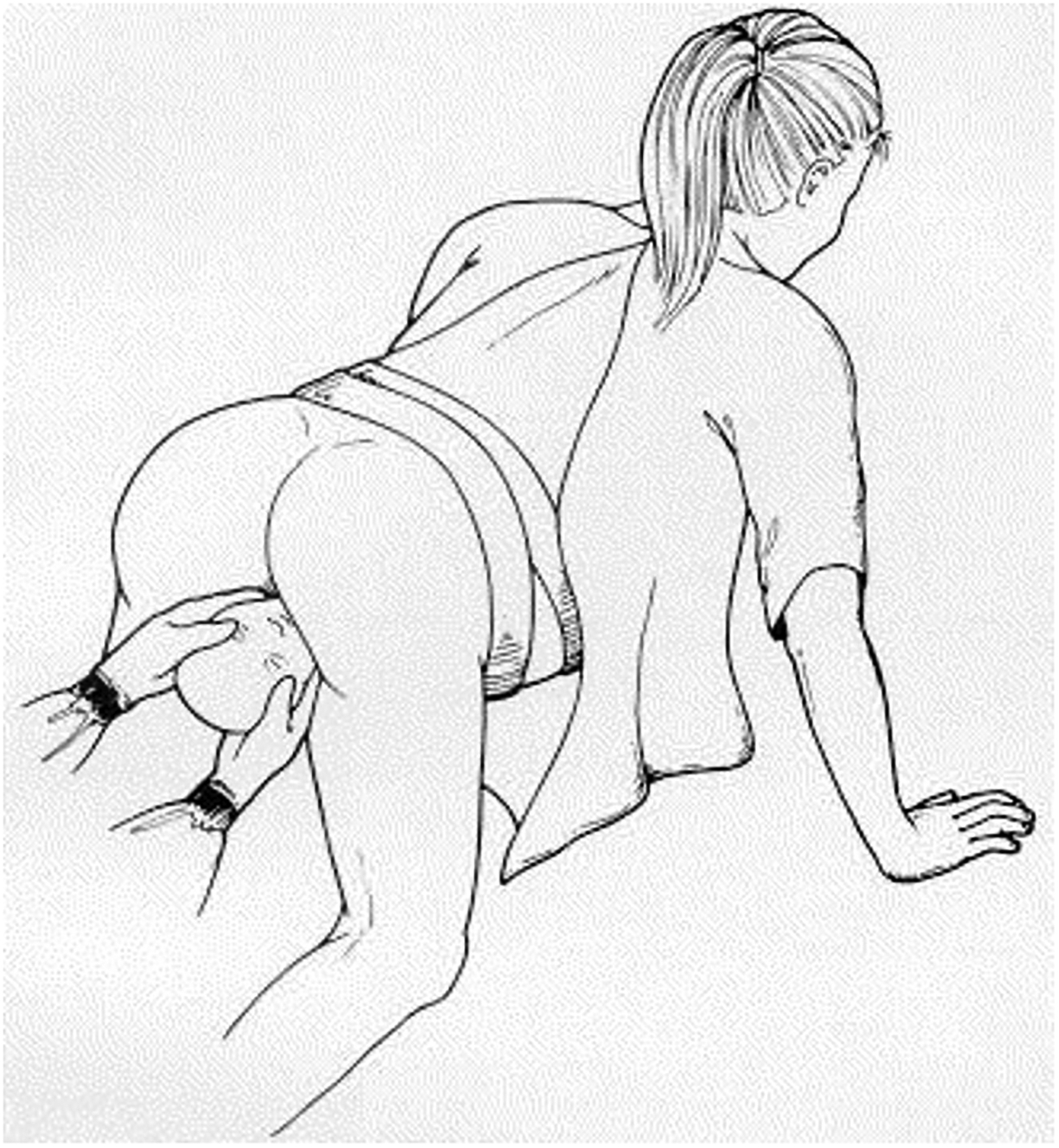
A: If the mother is able to support herself, turning to an all-fours position may dislodge or reorient the impacted anterior shoulder; however, the clinician must confirm this with direct palpation or rotation. B: Customary traction with symmetric pressure applied to the head with the mother on all fours delivers the posterior shoulder and thereby releases the obstructed anterior shoulder.
Figure 6:
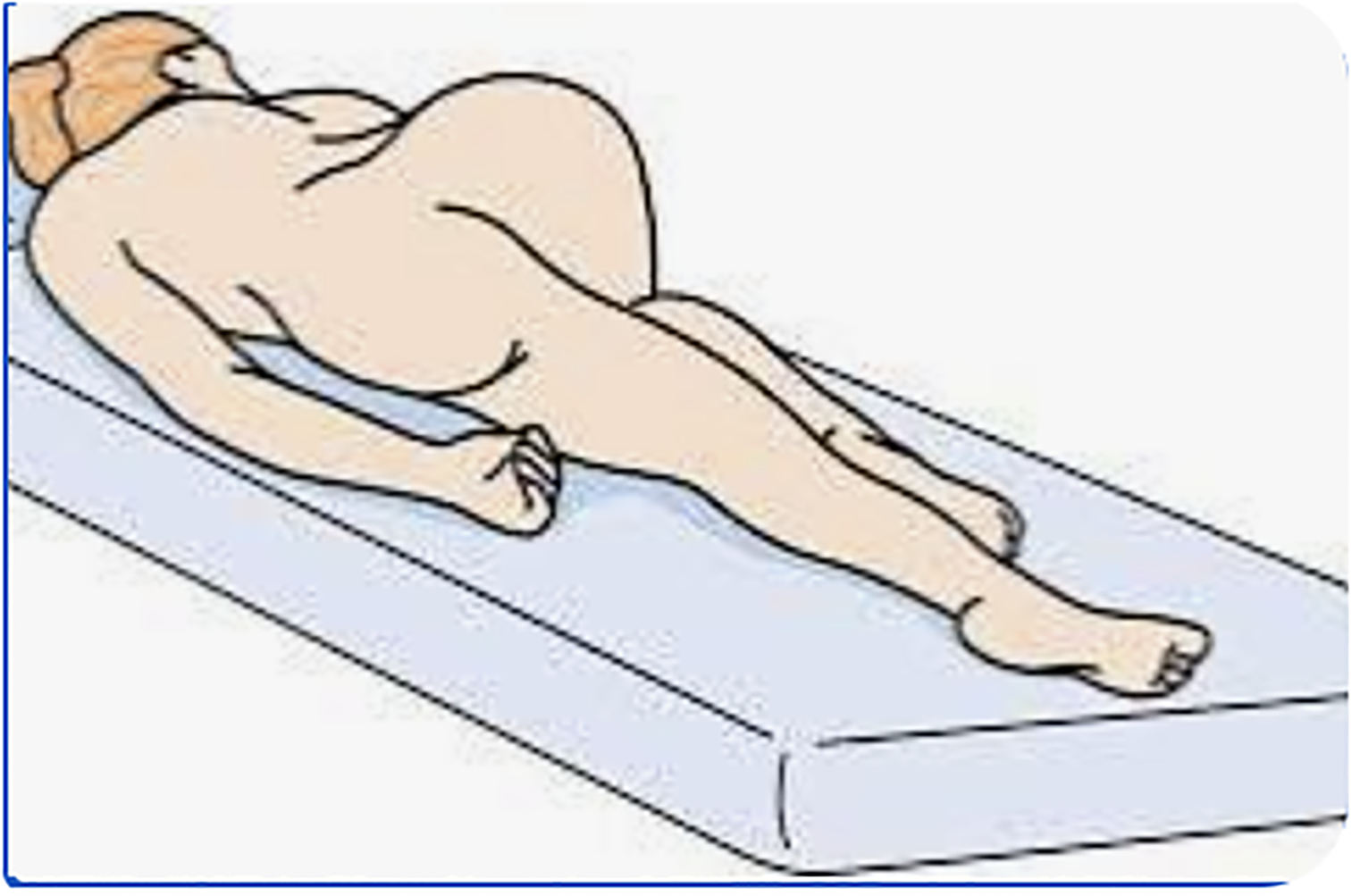
Sims position (as illustrated) may be used similarly to Gaskin’s maneuver when regional anesthesia hampers maternal mobility.
The following video (Video 7) demonstrates another misstep in management of shoulder dystocia: reversing direction and pulling upward on the head in an attempt to deliver the posterior shoulder before the anterior shoulder. Indeed, Allen et al demonstrated this phenomenon in a simulated setting, noting that traction levels of similar magnitude are often exerted in opposite directions (Figure 7) when clinicians are presented with shoulders that do not deliver in the anteroposterior dimension.19 This mechanism explains the occurrence of brachial plexus injuries even in posterior shoulders (as occurred in this video example) or during cesarean delivery,63 which involves upward traction on the fetal head after it is delivered through the hysterotomy. Aside: The incidence of permanent brachial plexus injury following cesarean section63 is a full order of magnitude less common than following shoulder dystocia.64 When faced with a difficult delivery of the trunk through the uterine incision during cesarean section, the surgeon should resort to delivery of the posterior arm (using the same technique described below) rather than applying forceful upward, laterally directed traction on the fetal head, which exerts the same mechanism of injury to the brachial plexus as downward-directed traction away from the anterior shoulder in the setting of shoulder dystocia.
Video 7:
Faced with obstructed delivery of the shoulders, a not uncommon misstep is to reverse direction and pull upward with equal force to the initial downward traction. Unless the obstruction is relieved, such reversal risks injury to the posterior brachial plexus.
Figure 7:
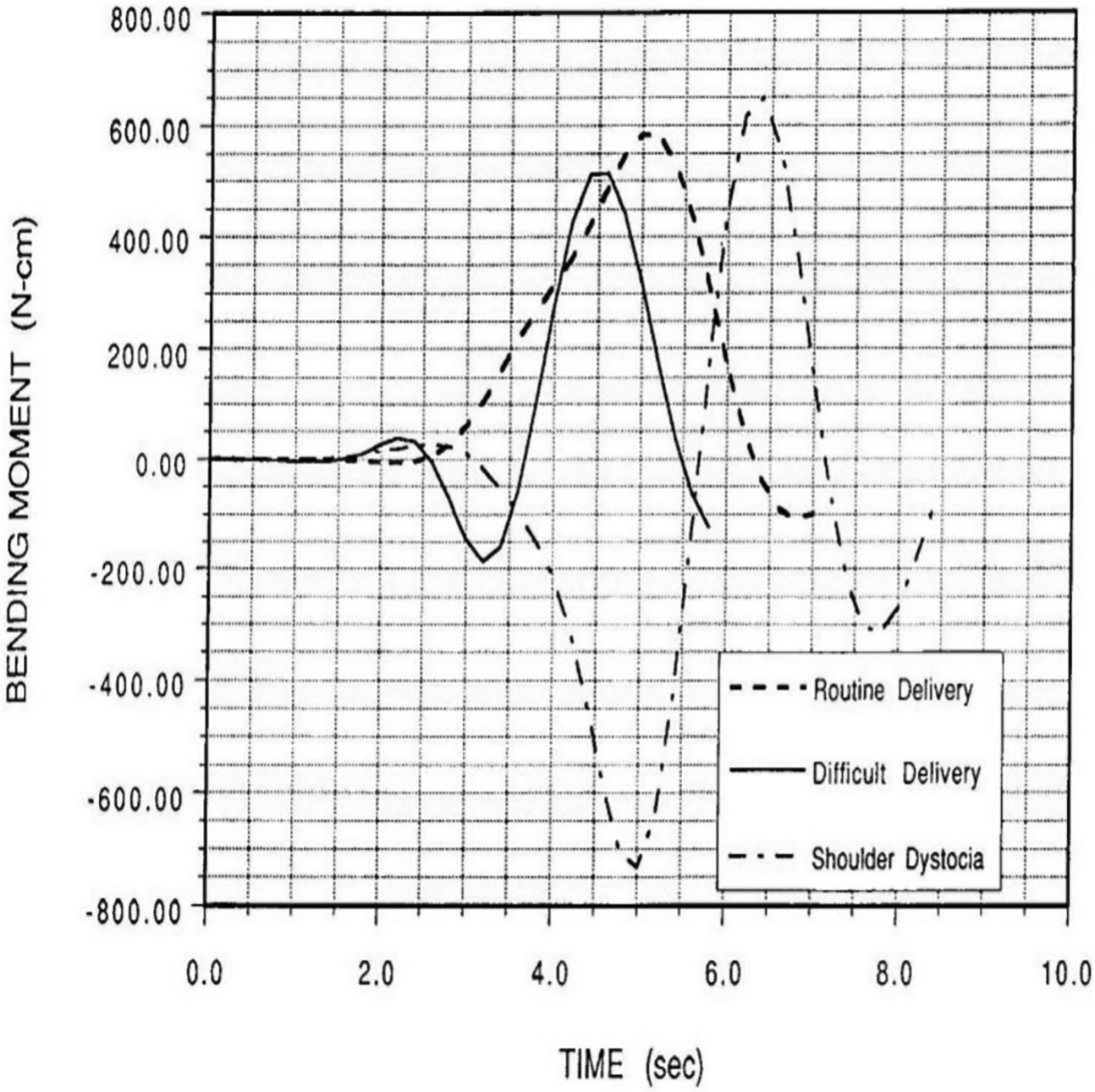
Presented with a simulated shoulder dystocia in which the fetus would not deliver, obstetrician participants reversed the direction of applied traction to the mannequin head. Reprinted with permission.18
COMPLEX ROTATIONAL MANEUVERS
Compared to the initial delivery techniques described above that still involve clinician-applied traction on the fetal head, immediate direct manipulation of the fetal trunk within the birth canal in response to shoulder dystocia decreases the magnitude of clinician-applied traction and the resultant brachial plexus stretch.50,65 Thus, every obstetric provider must become skilled in these techniques, which can be accomplished with regular rehearsal – repeated semi-annually or annually, depending upon initial competency – in a simulated setting.66 Ideally, simulation should include force measurement in order to provide objective feedback about skills acquisition, individual propensity for applying an injurious level of traction and to assess competency. The outset of obstetric training (e.g., during intern bootcamp), is the best time to review and teach the precepts of intrapartum management of shoulder dystocia, even before trainees begin to attend births on the Labor & Delivery unit.58
Delivery of the Posterior Arm
Proper technique for delivery of the posterior arm necessarily entails reaching into the vagina, beyond the delivered fetal head, bringing the posterior shoulder down and forward into the hollow of the sacrum and then into the oblique diameter (as in the beginning of a posterior Rubin’s maneuver, while simultaneously feeling for the antecubital fossa and flexing the elbow of the posterior arm. Then, by grasping the wrist, the arm is swept anteriorly across the fetal chest and out past the fetal head (Video 8). By substituting an acromio-axillary diameter for the biacromial diameter, yet another 2 cm of space is gained52 – in addition to the 2 cm obtained when the shoulder width is reoriented to occupy the oblique diameter of the pelvic outlet.
Video 8:
Delivery of the posterior arm involves rotating the posterior shoulder to the oblique diameter and then flexing the elbow and sweeping the arm across the fetal chest and face. It is the most successful maneuver to alleviate obstructed delivery of the fetal trunk (in the context of either shoulder dystocia or cesarean section) and can be the “go-to” initial maneuver for the proficient obstetric provider.
Delivery of the posterior arm is successful in over 96% of shoulder dystocia cases, and has recently been advocated as the maneuver to be prioritized early in the algorithmic response to shoulder dystocia.8 Indeed, the author advocates that experienced, proficient providers prioritize use of shoulder dystocia maneuvers that use the fetal body as the locus of direct manipulation by the birth attendant (e.g., corkscrew and delivery of the posterior arm) as their initial “go-to” maneuver over that of indirect maneuvers involving manipulation of the mother by assistants (e.g., McRoberts positioning and application of suprapubic pressure) while the birth attendant continues his delivery attempts.40,67–69 As explained above, assistive maneuvers should be combined with Rubin’s maneuver performed by the primary delivering clinician; repeated traction on the head during McRoberts’ and/or suprapubic to complete the delivery should be attempted only when a second obstetric assist is present and the primary assistant is simultaneously rotating the anterior shoulder.
Crofts et al reviewed several common errors in gaining access to the vagina for delivery of the posterior arm in their series of 450 simulations70 and encouraged the deliverer to insert the entire hand, including the thumb, to at least the level of the wrist. To this the author adds her observation that clinicians tend to rely on their dominant hand to perform delivery of the posterior arm, regardless of the relative position of the fetal head and shoulders. In the circumstance where the fetal head position is left occiput transverse, with the infant’s back to the maternal left, a right-handed provider is better advised to use her left hand (Figure 8) to initiate the clockwise rotation of the posterior shoulder into the oblique position and then continue with delivery of the posterior arm. Although initially somewhat awkward, this facilitates the use of the full 180 arc available by optimizing the range of motion of the provider’s arm as it crosses the midline, 6-o’clock position of the clockwise rotation, without having to interrupt and switch hands to complete; if the dominant hand (right hand in this instance) were to be used, once the posterior shoulder has crossed the midline, the provider’s range of motion is restricted from continuing the clockwise arcing motion. Another observation is that some clinicians will attempt to deliver the posterior arm from directly underneath the fetal trunk (similar to pulling on one end of a wishbone) rather than sweeping the arm across the chest. This improper form fails to take advantage of the increased space in the oblique diameter and is likely to result in fracture of the humerus from forcing its midshaft against resistance posteriorly.
Figure 8:


A: A common misstep in beginning internal rotational maneuvers is the clinician inserting her dominant hand, regardless of fetal position. Note the clinician is using her right hand to deliver the posterior (left) arm in this simulated delivery. B: Instead, in a shoulder dystocia where the head in left occiput anterior position and the fetus’ back is on the maternal left, the clinician preparing to deliver the posterior arm or perform a corkscrew maneuver is advised to begin with the left hand as pictured (regardless of hand dominance). Although initially awkward, once the posterior shoulder is rotated in clockwise fashion (adducting the shoulder toward the fetal chest) and the clinician’s arm reaches the 7 o’clock position, she has the full range of motion of the left arm to complete either the sweep of the posterior arm across the chest or the full 180-degree clockwise rotation to the anterior position in front of the pubic bone.
Corkscrew (Modified Woods’ Screw) Maneuver
In the less common instance where the posterior arm is fully extended, and possibly pinned between the body and the sacral promontory, often this circumstance is more responsive to use of the corkscrew maneuver then to flexion of the elbow and delivery of the posterior arm. First described by Woods in 1943, the corkscrew maneuver has been modified to eliminate any use of concomitant fundal pressure (shown to be associated with a higher incidence of brachial plexus injury12 and to proceed with adduction rather than abduction of the shoulder. Corkscrew maneuver involves placing simultaneous pressure on each shoulder and rotating the shoulders a complete 180 degrees in a winding rather than planar rotary motion (Video 9). Given the skew position of the pelvic outlet relative to the pelvic inlet, the posterior shoulder that was initially more cephalad (behind) relative to the anterior shoulder is wound through the “threads of the screw”(from above or just in front of the coccyx), and then and ends up in front of the pubic bone in its new anterior position; no longer impeded anteriorly by the pubic bone, the trunk immediately delivers.
Video 9:
The Modified Wood’s corkscrew maneuver requires adduction of the posterior shoulder and a 180-degree rotation, bringing the posterior shoulder to an anterior position, only it is now in front instead of behind the pubic symphysis. With the obstruction thus relieved, the remainder of the trunk delivers easily.
HEROIC MANEUVERS OF LAST RESORT
It is important to mention the maneuvers of last resort to be utilized once all other techniques have been attempted unsuccessfully. Earlier maneuvers can be repeated (although not by repeating the same maneuver immediately after it had failed, especially those that still include traction on the head,33 as critiqued in Video 2) until the head-to-body interval has extended beyond 8 minutes’ duration.71 These maneuvers of last resort include cephalic replacement (Zavanelli maneuver) (Video 10); intentional cleidotomy (fracturing or cutting the clavicle with scissors); symphysiotomy (dividing the anterior symphyseal ligament utilizing a scalpel from above while protecting the catheterized urethra and displacing it laterally from midline with a finger from below, Figure 9); and abdominal rescue, wherein a cesarean section is performed, and the operator pushes the impacted anterior shoulder laterally and underneath the pubic bone from above, while a second assist completes the delivery from below.
Video 10:
Cephalic replacement, also known as Zavanelli’s maneuver, is a heroic maneuver of last resort, once other complex maneuvers have been tried and failed.
Figure 9:
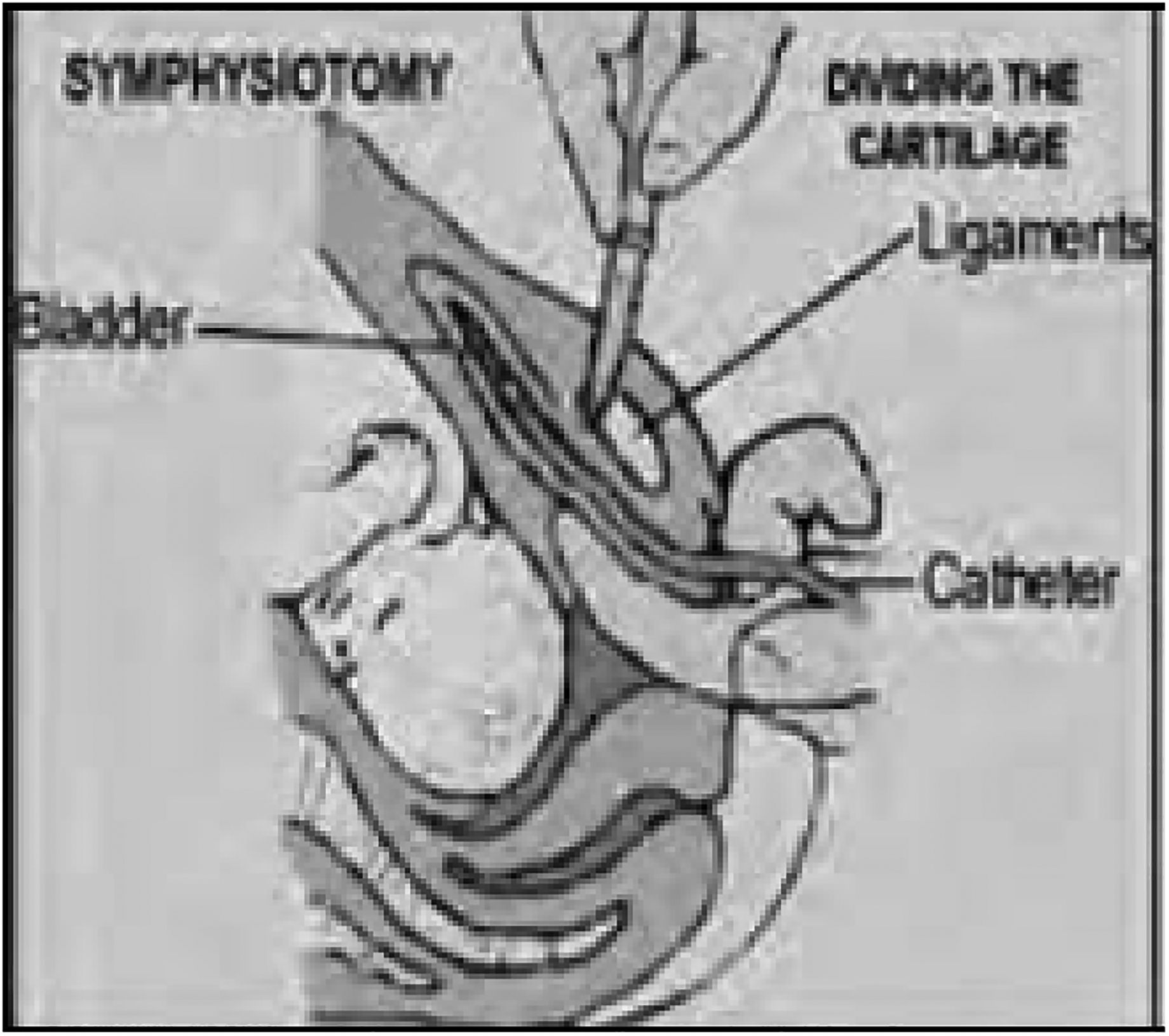
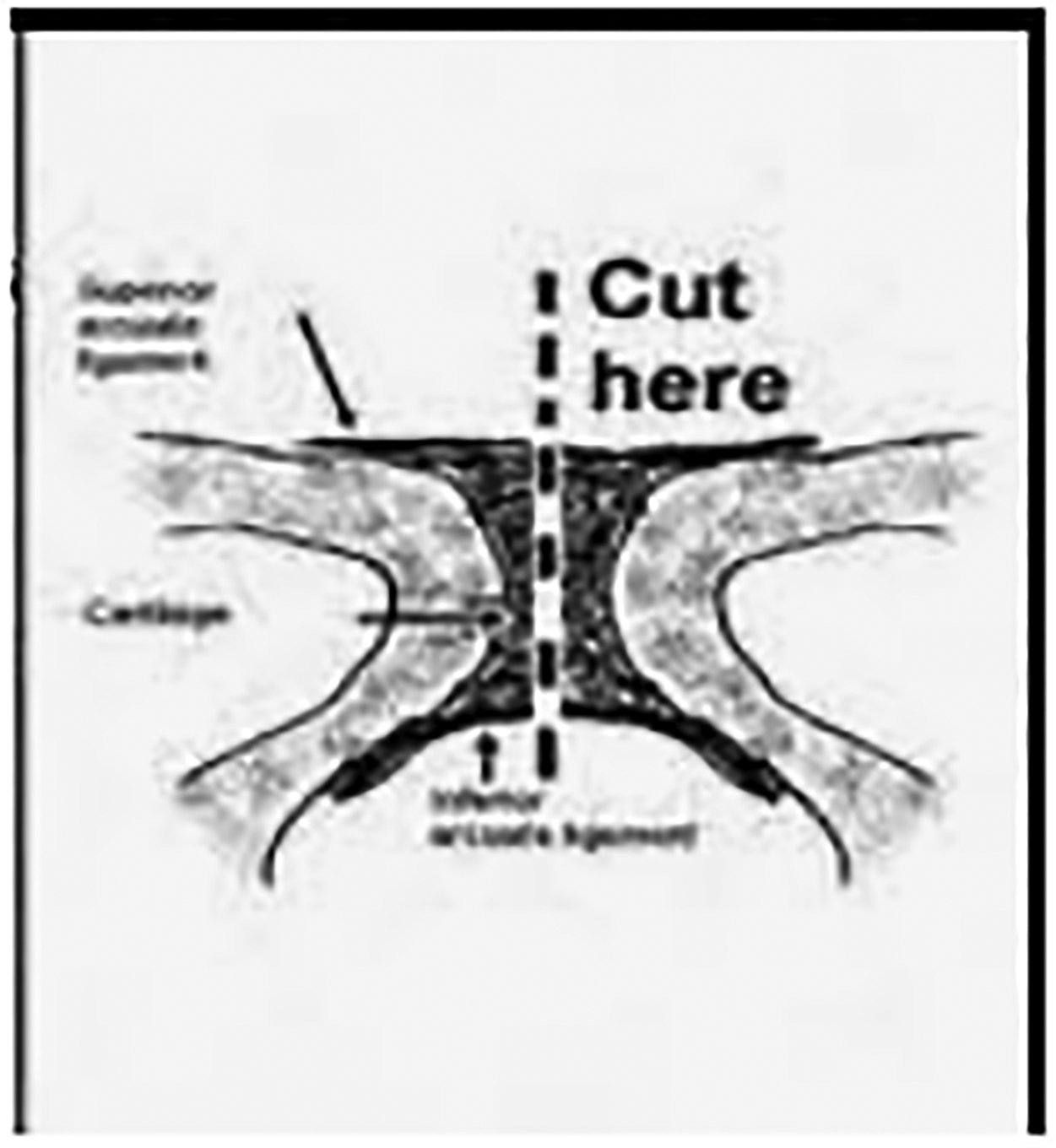
Symphysiotomy is a surgical procedure resorted to when catastrophic obstructed labors (e.g., head entrapment in breech deliveries or shoulder dystocia refractory to all other maneuvers) occur in resource-poor settings. A: A urinary catheter is placed in the urethra and one finger of one hand displaces the urethra off midline while the other hand utilizes a scalpel anteriorly and above to incise the ligament between the two pubic rami, B: as shown.
Each of these heroic measures is fraught with potential for serious maternal or fetal complications: Cephalic replacement may cause uterine rupture and should be accompanied by pharmacologically induced uterine relaxation (e.g., nitroglycerin or a halogenated inhalational anesthetic). Cleidotomy can cause lacerations of the subclavian vasculature and/or puncture a lung underneath. Therefore, intentional fracture of the clavicle, whether performed digitally (usually with a thumb) or sharply (with scissors) should be directed from behind the midshaft of the clavicle in an upward and outward direction. Symphysiotomy is a highly morbid procedure whose orthopedic repair and subsequent rehabilitation is lengthy and arduous. It is best reserved for resource poor settings where an abdominal surgical approach is unavailable. The original description of abdominal rescue by O’Leary72 was a case in which cephalic replacement had failed, required general anesthesia and the infant received low Apgars and suffered neonatal seizures. Fortunately, the need for these techniques is exceedingly rare. Most clinicians – even those who deliver thousands of babies over many years and encounter shoulder dystocia with some regularity – will never need to use them.
AFTERMATH OF SHOULDER DYSTOCIA
Upon delivery following shoulder dystocia, it is important that the infant is evaluated immediately by pediatric providers in attendance. After any necessary resuscitation is complete, the infant should be examined in the delivery room for the presence of crepitus over the clavicles, asymmetric Moro reflex, symmetry of grasp reflex, other possible skeletal fractures (especially of the humerus on the contralateral side to the arm that was anterior) and evidence of a Horner’s sign. The chest wall should be observed for symmetric breathing. If any of these abnormalities are found, avoid making any prognostications in the immediate aftermath of the delivery. Rather, ensure that the infant will undergo serial evaluations over the next few days until discharge from the hospital, after which the prognosis for recovery may be discussed. It is best if a dedicated team of interdisciplinary specialists in brachial plexus injury are involved before discharge from the hospital – and if there is incomplete resolution of the findings, that close follow-up after discharge is arranged. The obstetric provider is advised to maintain contact with the family and make regular inquiries about the infant’s progress.
While the evaluation of the neonate is occurring, communication with the parents about the events of the delivery is paramount, even if no injury is evident. The mother must understand that the occurrence of shoulder dystocia is a significant part of her obstetric history and that caretakers of her future pregnancies will rely on her reporting of the complication, as this may be the only prompt for the clinician to review records from the previous delivery.
The events should be extensively documented in the medical record, including the specific diagnosis of shoulder dystocia, as well as the details of the head-to-body interval; the sequence of techniques attempted and which provider (if more than one) performed which maneuver; which shoulder was anterior; which shoulder ultimately delivered first and by what final maneuver; and that the occurrence of shoulder dystocia was specifically discussed with the mother. The obstetric provider is advised to limit documentation of pediatric findings – and if discussed at all, should indicate their source (e.g, “decreased movement of the right arm noted by pediatric team in attendance”). Similarly, neither the nurses nor the pediatric team should document their observed management of shoulder dystocia; rather, they should document only those actions they undertook themselves; and otherwise note that the delivery record should be consulted for details of additional obstetric procedures.
Finally, after either a simulated and actual delivery complicated by shoulder dystocia, a non-judgmental and supportive debriefing of the events should take place as close in real time to the event as possible. Debrief sessions enhance the culture of safety on Labor & Delivery, provide the opportunity for the team to review what went well, what could have gone better and what might be done differently in future events; and to mutually support learning and resilience after responding to this obstetric emergency.
SUMMARY PEARLS AND PITFALLS
Shoulder dystocia is an unpreventable emergency that occurs unpredictably. The time for obstetric providers to practice its safe management is before it is encountered clinically. The combination of visual and haptic learning in a simulated environment increases skill and reduces injury.
Every obstetric provider should be vigilant at every delivery and willingly inclined to recognize when there may be impacted shoulders. Direct palpation of the anterior fetal scapula is a simple yet critical technique by which to confirm the orientation of the biacromial diameter before initial traction is applied.
Slow down! After the head has completely emerged from the vaginal introitus, mark the time and await the next contraction. A pause of 60 seconds’ duration allows for spontaneous restitution of the aftercoming shoulders – or for the clinician to manually adjust the shoulders before applying traction to the head. In most cases, this two-step method will mitigate the occurrence of shoulder dystocia.
Clinicians must consciously limit their own initial traction when confirming the diagnosis of shoulder dystocia, as observers and supervising physicians may not appreciate the magnitude of force applied. The head should be grasped with both hands, one on either side, and symmetric pressure applied to maintain the axial alignment of the fetal neck with its vertebral column during pull.
Obstetric providers are advised to use maneuvers in which they are most proficient. However, initial maneuvers should incorporate a minimum rotation of 30 degrees off the anteroposterior axis by directly manipulating the shoulder. Seasoned clinicians may proceed directly to complex rotational maneuvers such as corkscrew (Modified Woods’) or delivery of the posterior arm.
If initial maneuvers are to be followed by application of traction on the head, they must be verbally coordinated with additional providers’ assistive maneuvers such as suprapubic pressure, McRoberts’ or Gaskin’s positioning. The goal of a team approach is to achieve simultaneous reorientation of the shoulders to the oblique position as subsequent traction is applied.
Delivery of the posterior arm is a rotational maneuver that begins with shrugging the posterior shoulder diagonally into the hollow of the sacrum before attempting to flex the elbow. Avoid lateral displacement of the upper arm, which can lead to humeral fracture; instead, sweep the posterior arm across the chest and extend the forearm by grasping the wrist and delivering it past the fetal head.
The corkscrew maneuver takes mechanical advantage of the skew orientation between the planes of the pelvic inlet and outlet. The 180-degree rotational motion is winding in nature (i.e., combined with forward progression rather than planar), wherein the posterior shoulder is brought from behind the more cephalad coccyx to an anterior position in front of the pubic bone. When the posterior arm is extended and there is difficulty flexing the elbow, the corkscrew maneuver is often successful.
Persistent repetition of unsuccessful traction-based maneuvers increases the risk of permanent brachial plexus injury. A different technique should be attempted at least every 30 seconds, limiting the number of pulls exerted on the head. However, earlier maneuvers should be repeated after subsequent complex maneuvers prove unsuccessful, before resorting to heroic measures.
Every shoulder dystocia occurrence should be debriefed with all providers – and most importantly with the mother, regardless of the occurrence of injury. Early, interdisciplinary care of an infant who suffers an injury is critical to optimal recovery.
Skills of shoulder dystocia management should be reviewed and rehearsed at least annually.
Supplementary Material
Disclosure Statement:
The author is currently funded by the Agency for Healthcare Research & Quality (AHRQ) Grant #1R18HA026689 entitled “Virtual Reality Enhanced Haptic Simulation to Improve Self-Regulation of Applied Delivery Force During Shoulder Dystocia.” The opinions expressed herein are those of the author only based on her extensive research, clinical experience and review of litigated cases of shoulder dystocia-associated brachial plexus injuries; and do not necessarily represent the opinions of the AHRQ or the Department of Obstetrics, Gynecology & Women’s Health of the Albert Einstein College of Medicine/Montefiore Medical Center.
REFERENCES
- 1.Deering S, Poggi S, Macedonian C, Gherman R, Satin AJ. Improving resident competency in the management of shoulder dystocia with simulation training. Obstet Gynecol 2004;103(6);1224–1228. [DOI] [PubMed] [Google Scholar]
- 2.Gurewitsch Allen ED. Simulation of shoulder dystocia for skill acquisition and competency assessment: a systematic review and gap analysis. Simul Healthc 2018;13(4):268–283. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalves A, Verhaeghe C, Bouet PE, Gillard P, Descamps P, Legendre G. Effect of the use of a video tutorial in addition to simulation in learning the maneuvers for shoulder dystocia. J Gynecol Obstet Hum Reprod 2018;47(4):151–155. [DOI] [PubMed] [Google Scholar]
- 4.Kimmich N, Zimmermann R, Kreft M. Video analysis for the evaluation of vaginal birth: a prospective observational study. Swiss Med Wkly 2018;148:w14634. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg K, Trevathan W. Birth, obstetrics and human evolution. Br J Obstet Gynaecol 2002;109(11):1199–1206. [DOI] [PubMed] [Google Scholar]
- 6.Bamberg C, Rademacher G, Güttler F, Teichgräber U, Cremer M, Bührer C, et al. Human birth observed in real-time open magnetic resonance imaging. Am J Obstet Gynecol 2012;206(6):505.e1–6. [DOI] [PubMed] [Google Scholar]
- 7.Gurewitsch Allen ED. Recurrent shoulder dystocia: Risk factors and counseling. Clin Obstet Gynecol 2016;59(4):803–812. [DOI] [PubMed] [Google Scholar]
- 8.American College of Obstetricians & Gynecologists. Practice Bulletin No. 178: Shoulder Dystocia. Obstet Gynecol 2017;129(5):e123–e133. [DOI] [PubMed] [Google Scholar]
- 9.Benedetti TJ, Gabbe SG. Shoulder dystocia: a complication of fetal macrosomia and prolonged second stage of labor with midpelvic delivery. Obstet Gynecol 1978;52(5):526–9. [PubMed] [Google Scholar]
- 10.Bofill JA, Rust OA, Devidas M, Roberts WE, Morrison JC, Martin JN. Shoulder dystocia and operative vaginal delivery. J Mat Fet Med. 1997;6(4);220–224. [DOI] [PubMed] [Google Scholar]
- 11.Mollberg M, Hagberg H, Bager B, Lilja H, Ladfors L. Risk factors for obstetric brachial plexus palsy among neonates delivered by vacuum extraction. Obstet Gynecol 2005;106(5 Pt 1):913–8. [DOI] [PubMed] [Google Scholar]
- 12.Gross SJ, Sokol RJ, Shime J, Farine D. Shoulder dystocia: Predictors and outcome – a five-year review. Am J Obstet Gynecol 1987;156(2):334–336. [DOI] [PubMed] [Google Scholar]
- 13.Ouzounian JG, Hernandez G, Korst LM, Montoro MM, Battista LR, Walden C, et al. Pre-pregnancy weight and excess weight gain are risk factors for macrosomia in women with gestational diabetes. J Perinatol 2011;31:717–721. [DOI] [PubMed] [Google Scholar]
- 14.Acker DB, Sachs BP, Friedman EA. Risk factors for shoulder dystocia. Obstet Gynecol 1985;66(6):762–768. [PubMed] [Google Scholar]
- 15.Acker DB, Sachs BP, Friedman EA. Risk factors for shoulder dystocia in the average-weight infant. Obstet Gynecol 1986;67(5), 614–618. [DOI] [PubMed] [Google Scholar]
- 16.Gross TL, Sokol RJ, Williams T, Thompson K. Shoulder dystocia: a fetal-physician risk. Am J Obstet Gynecol 1987;156(6):1408–18. [DOI] [PubMed] [Google Scholar]
- 17.Morrison JC, Sanders JR, Magann EF, Wiser WL. The diagnosis and management of dystocia of the shoulder. Surg Gynecol Obstet 1992;175(6):515–22. [PubMed] [Google Scholar]
- 18.Spong CY, Beall M, Rodrigues D, Ross MG. An objective definition of shoulder dystocia: prolonged head-to-body delivery intervals and/or the use of ancillary obstetric maneuvers. Obstet Gynecol 1995;86(3):433–6. [DOI] [PubMed] [Google Scholar]
- 19.Allen RH, Bankoski BR, Butzin CA, Nagey DA. Comparing clinician-applied loads for routine, difficult, and shoulder dystocia deliveries. Am J Obstet Gynecol, 1994;171(6):1621–1627. [DOI] [PubMed] [Google Scholar]
- 20.Mollberg M, Wennergren M, Bager B, Ladfors L, Hagberg H. Obstetric brachial plexus palsy: A prospective study on risk factors related to manual assistance during the second stage of labor. Acta Obstet Gynecol Scand, 2007;86(2):198–204. [DOI] [PubMed] [Google Scholar]
- 21.Mollberg M, Lagerkvist AL, Johansson U, Bager B, Johansson A, Hagberg H. Comparison in obstetric management on infants with transient and persistent obstetric brachial plexus palsy. J Child Neurol, 2008;23(12):1424–1432. [DOI] [PubMed] [Google Scholar]
- 22.Wagner SM, Bell CS, Gupta M, Mendez-Figueroa H, Ouellette L, Blackwell SC, Chauhan SP. Interventions to decrease complications after shoulder dystocia: a systematic review and Bayesian meta-analysis. Am J Obstet Gynecol 2021;225(5),484.e1–484.e33. [DOI] [PubMed] [Google Scholar]
- 23.Sever JW. Obstetric paralysis: Its etiology, clinical aspects and treatment, with a report of four hundred and seventy cases. Arch Pediatr Adolesc Med 1916;12:541–7. [Google Scholar]
- 24.Sunderland S, Bradley KC. Stress-strain phenomena in human peripheral nerve trunks. Brain 1961;84(1):102–119. [Google Scholar]
- 25.Volpe JJ. Injuries of extracranial, cranial, intracranial, spinal cord and peripheral nervous system structures. In Neurology of the Newborn. St Louis: WB Saunders, 1995, pp. 769–92. [Google Scholar]
- 26.Ubachs JMH, Sloof ACJ, Peeters LLH. Obstetric antecedents of surgically treated obstetric brachial plexus injuries. BJOG Int J Obstet Gynaecol 1995;102:10:813–817. [DOI] [PubMed] [Google Scholar]
- 27.Ouzounian JG, Korst LM, Phelan JP. Permanent Erb palsy: a traction-related injury? Obstet Gynecol 1997;89(1):139–41. [DOI] [PubMed] [Google Scholar]
- 28.Wolf H, Hoeksma AF, Oei SL, Bleker OP. Obstetric brachial plexus injury: risk factors related to recovery. Eur J Obstet Gynecol Reprod Biol 2000;88(2):133–8 [DOI] [PubMed] [Google Scholar]
- 29.Singh A, Lu Y, Chen C, Cavanaugh JM. Mechanical properties of spinal nerve roots subjected to tension at different strain rates. J Biomechanics 2006;39(9):1669–1676. [DOI] [PubMed] [Google Scholar]
- 30.American College of Obstetricians & Gynecologists. Emergencies in Clinical Obstetrics. In ACOG Simulations. Accessed February 27, 2022 from https://www.acog.org/education-and-events/simulations/eco. [Google Scholar]
- 31.Royal College of Obstetricians & Gynaecologists. Shoulder dystocia: green top guideline no. 42. In: rcog.org. Accessed February 27,2022 from https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg42. [Google Scholar]
- 32.Seeds JW, Walsh M. “Intrapartum care: Malpresentations,” ch 16 In: Obstetrics: Normal and Problem Pregnancies (3rd ed.) Gabbe SG, Niebyl JR, Simpson JL. (eds) New York:Churchill Livingston, 1996, p. 492. [Google Scholar]
- 33.Gurewitsch E, Stallings S, Tam W, Allen R. Does maneuver rate affect shoulder dystocia outcome? Am J Obstet Gynecol 2004;191(6):S66. [Google Scholar]
- 34.Deering SH, Weeks L, Benedetti T. Evaluation of force applied during deliveries complicated by shoulder dystocia using simulation. Am J Obstet Gynecol 2011;204:234.e1–5. [DOI] [PubMed] [Google Scholar]
- 35.Allen R, Sorab J, Gonik B. Risk factors for shoulder dystocia: an engineering study of clinician-applied forces. Obstet Gynecol 1991;77(3):352–5. [PubMed] [Google Scholar]
- 36.Walters M, Eubanks A, Weissbrod E, Fischer J, Staat B, Deering S. Visual estimation of force applied during simulated deliveries complicated by shoulder dystocia. AJP Rep 2018;8(4):e206–e211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beall MH, Spong C, McKay J, Ross MG. Objective definition of shoulder dystocia: A prospective evaluation. Am J Obstet Gynecol 1998;179(4):934–937. [DOI] [PubMed] [Google Scholar]
- 38.Locatelli A, Incerti M, Ghidini A, Casario G, Ferrini S, & Strobelt N Head-to-body delivery interval using ‘two-step’ approach in vaginal deliveries: Effect on umbilical artery pH. J Mat Fet Neonatal Med 2011;24(6):799–803. [DOI] [PubMed] [Google Scholar]
- 39.Bottoms SF, Sokol RJ (1981) Mechanism and conduct of labor. In: Iffy L, Kaminetzky HA (eds) Principles and Practice of Obstetrics & Perinatology. New York:Wiley, 1981, pp 815–838. [Google Scholar]
- 40.Allen RH, Gurewitsch ED. Shoulder dystocia, 2015. In: Emedicine.medscape.com. Accessed April 3 2016 from http://emedicine.medscape.com/article/1602970-overview#a8. [Google Scholar]
- 41.Inglis SR, Feier N, Chetiyaar JB, Naylor MH, Sumersille M, Cervellione KL, et al. Effects of shoulder dystocia training on the incidence of brachial plexus injury. Am J Obstet Gynecol 2011;204(4):322.e1–322.e6. [DOI] [PubMed] [Google Scholar]
- 42.Reid DE. Conduct of normal labor and the puerperium. In Reid DE (ed.) Textbook of Obstetrics. Philadelphia, PA: W.B. Saunders Company, 1962, pp. 448–449. [Google Scholar]
- 43.Mortimore VR, McNabb M. A six-year retrospective analysis of shoulder dystocia and delivery of the shoulders. Midwifery 1998;14(3);162–173. [DOI] [PubMed] [Google Scholar]
- 44.Metaizeau JP, Gayet C, Plenat F. Les lesions obstetricales due plexus brachial [brachial plexus birth injuries. an experimental study]. Chirurgie Pediatrique, 1979;20(3):159–163. [PubMed] [Google Scholar]
- 45.Morris W Shoulder dystocia. J Obstet Gynaecol Br Emp 1955;62(2):302–6. [Google Scholar]
- 46.Zapałowicz K, Radek M. The distribution of brachial plexus lesions after experimental traction: a cadaveric study. J Neurosurg Spine 2018;29(6):704–710. [DOI] [PubMed] [Google Scholar]
- 47.Gurewitsch ED, Donithan M, Stallings SP, Moore PL, Agarwal S, Allen LM, Allen RH. Episiotomy verses fetal manipulation in managing severe shoulder dystocia: A comparison of outcomes. Am J Obstet Gynecol 2004;191:911–916. [DOI] [PubMed] [Google Scholar]
- 48.Grobman WA, Miller D, Burke C, Hornbogen A, Tam K, Costello R. Outcomes associated with introduction of a shoulder dystocia protocol. Am J Obstet Gynecol, 2011;205(6):513–517. [DOI] [PubMed] [Google Scholar]
- 49.American College of Obstetricians & Gynecologists. Technical Bulletin No. 40: Shoulder Dystocia. Obstet Gynecol 2002;100(5):1045–50.12434783 [Google Scholar]
- 50.Gurewitsch ED, Kim EJ, Yang JH, Outland KE, McDonald MK, Allen RH. Comparing McRoberts’ and Rubin’s maneuvers for initial management of shoulder dystocia: An objective evaluation. Am Obstet Gynecol 2005;192(1):153–160. [DOI] [PubMed] [Google Scholar]
- 51.Salk I, Cetin M, Salk S, Cetin A. Determining the incidence of gynecoid pelvis using three-dimensional computed tomography in nonpregnant multiparous women. Med Princ Pract 2016;25(1):40–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Poggi SH, Spong CY, Allen RH. Prioritizing posterior arm delivery during severe shoulder dystocia. Obstet Gynecol 2003;101(5 Pt 2):1068–1072. [DOI] [PubMed] [Google Scholar]
- 53.Verspyck E, Goffinet F, Hellot MF, Milliez J, Marpeau L. Newborn shoulder width: A prospective study of 2222 consecutive measurements. Br J Obstet Gynaecol 1999;106(6):589–593. [DOI] [PubMed] [Google Scholar]
- 54.Gherman RB, Goodwin TM, Souter I, Neumann K, Ouzounian JG, Paul RH. The McRoberts’ maneuver for the alleviation of shoulder dystocia: how successful is it? Am J Obstet Gynecol 1997;176(3):656–661. [DOI] [PubMed] [Google Scholar]
- 55.Gonik B, Allen R, Sorab J. Objective evaluation of the shoulder dystocia phenomenon: effect of maternal pelvic orientation on force reduction. Obstet Gynecol 1989;74(1):44–8. [PubMed] [Google Scholar]
- 56.Walsh JM, Kandamany N, Ni Shuibhne N, Power H, Murphy JF, O’Herlihy C. Neonatal brachial plexus injury: comparison of incidence and antecedents between 2 decades. Am J Obstet Gynecol 2011;204(4):324.e1324–e3246. [DOI] [PubMed] [Google Scholar]
- 57.Crofts JF, Lenguerrand E, Bentham GL, Tawfik S, Claireaux HA, Odd D, et al. Prevention of brachial plexus injury-12 years of shoulder dystocia training: An interrupted time-series study. Br J Obstet Gynaecol 2015;123(1):111–118. [DOI] [PubMed] [Google Scholar]
- 58.Gurewitsch Allen ED, Brown Will SE, Allen RH. Improving shoulder dystocia management and outcomes with a targeted quality assurance program. Am J Perinatol, 2017;34:1088–1096. [DOI] [PubMed] [Google Scholar]
- 59.Dahlberg J, Nelson M, Dahlgren MA, Blomberg M. Ten years of simulation-based shoulder dystocia training- impact on obstetric outcome, clinical management, staff confidence, and the pedagogical practice - a time series study. BMC Pregnancy Childbirth 2018;18(1):361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sancetta R, Khanzada H, Leante R. Shoulder shrug maneuver to facilitate delivery during shoulder dystocia. Obstet Gynecol 2019;133(6):1178–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cluver CA, Hofmeyr GJ. Posterior axilla sling traction: a technique for intractable shoulder dystocia. Obstet Gynecol 2009;113(2 Pt 2):486–488. [DOI] [PubMed] [Google Scholar]
- 62.McCarter AR, Theiler RN, Rivera-Chiauzzi EY. Circumferential shoulder laceration after posterior axilla sling traction: a case report of severe shoulder dystocia. BMC Pregnancy Childbirth 2021;21(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gherman RB, Goodwin TM, Ouzounian JG, Miller DA, Paul RH. Brachial plexus palsy associated with cesarean section: An in utero injury? Am J Obstet Gynecol 1997;177(5):1162–1164. [DOI] [PubMed] [Google Scholar]
- 64.Nath RK, Kumar N, Avila MB, Nath DK, Melcher SE, Eichhorn MG, Somasundaram C. Risk factors at birth for permanent obstetric brachial plexus injury and associated osseous deformities. ISRN Pediatr 2012;2012:307039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grimm M, Costello R, Gonik B. Effect of clinician-applied maneuvers on brachial plexus stretch during a shoulder dystocia event: Investigation using a computer simulation model. Am J Obstet Gynecol 2010;203(4):339. [DOI] [PubMed] [Google Scholar]
- 66.Crofts JF, Bartlett C, Ellis D, Hunt LP, Fox R, Draycott TJ. Management of shoulder dystocia: skill retention 6 and 12 months after training. Obstet Gynecol 2007;110(5):1069–74. [DOI] [PubMed] [Google Scholar]
- 67.Gurewitsch ED, Allen RH. Fetal manipulation for management of shoulder dystocia. Fet Mat Med Rev 2006;17(3):239–280. [Google Scholar]
- 68.Gurewitsch ED. Optimizing shoulder dystocia management to prevent birth injury. Clin Obstet Gynecol 2007;50:592–606. [DOI] [PubMed] [Google Scholar]
- 69.Gurewitsch ED, Allen RH. Reducing the risk of shoulder dystocia and associated brachial plexus injury. Special Issue: Practical Approaches to Controversies in Obstetric Care. Blackwell SC, Saade GR, eds. Obstet Gynecol Clin North Am 2011;38:247–269 [DOI] [PubMed] [Google Scholar]
- 70.Crofts JF, Fox R, Ellis D, Winter C, Hinshaw K, Draycott TJ. Observations from 450 shoulder dystocia simulations: Lessons for skills training. Obstet Gynecol 2008;112(4):906–912. [DOI] [PubMed] [Google Scholar]
- 71.Poggi SH, Stallings SP, Ghidini A, Spong CY, Deering SH, Allen RH. Intrapartum risk factors for permanent brachial plexus injury. Am J Obstet Gynecol 2003;189(3):725–9. [DOI] [PubMed] [Google Scholar]
- 72.O’Leary JA, Cuva A. Abdominal rescue after failed cephalic replacement. Obstet Gynecol 1992;80(3 Pt 2):514–6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


