Abstract
Introduction and methods
Blood culturing has become one of the backbone investigations for septicemia, fever of unknown origin, etc. This study was conducted to test the effect of multimodal interventions on the practical skills of healthcare workers (HCWs), raise awareness regarding the importance of aseptic blood culture collection practices, and increase compliance with the specific steps to be followed. Hence, this current interventional study was aimed at comparing the rate of isolation of contaminants grown among the blood culture specimens, assessing the knowledge, attitude, and practice (KAP) of HCWs collecting the blood culture specimen on various aspects of sample collection, educating the nursing staff regarding blood sample collection using a structured, pre-formed checklist, and emphasizing best practices for blood culture collection. All of the study's objectives were successfully met within the time frame specified. Using a pre-formed checklist and a Google form for KAP analysis eased the calculation.
Results
On analysis, the blood culture contamination rate in the pre-interventional phase dropped drastically from 6.16% to 3.03% in the post-interventional phase. The educational sessions conducted are a paramount reason for the reduction in the contamination rate. The HCWs were the least compliant towards the eighth step in the checklist (regarding palpation of skin); however, that too increased from 66.93% and 64.51% to a whopping 82.25% and 83.06%, respectively, with a chi-square value of 0.03 and a p-value of 0.85 (not significant).
Conclusion
Implementation of interventional studies as an audit like this in tertiary care hospitals can result in a significant reduction in blood culture contamination rates and can also improve the compliance of HCWs with blood culture protocols. This, in turn, can overall improve the effectiveness of blood culture (BC) testing and reduce mortality and morbidity in tertiary care hospitals. Further research can be conducted to brainstorm more methods to increase the compliance of HCWs. Better monitoring strategies can also be set to ensure low contamination rates. Additionally, some other methods can be derived to locate the source of contamination within the hospital environment and thus eliminate it. Similar interventions can be conducted for a longer duration of time to further reduce the blood culture contamination rate below 3% (as per the recommendations).
Keywords: healthcare workers, kap analysis, multimodal interventions, septecemia, blood cultures
Introduction
Despite many advances in the healthcare system over the last decade, bloodstream infections (BSI) continue to remain a grueling conundrum responsible for high mortality and morbidity worldwide. Also, BSI is the major cause of mortality among patients admitted to intensive care units (ICUs) [1,2]. Hence, an accurate and rapid diagnosis of pathogens causing BSI can help in initiating appropriate antimicrobial therapy, which can improve the clinical outcome by reducing mortality and morbidity [2]. Blood cultures play an important role in the management of sepsis. Since BSI is a medical emergency, the application of accurate methodology in the collection of blood samples for culture is extremely crucial. Contaminated blood cultures can prove to be troublesome from a diagnostic point of view. Errors in blood culture (BC) collection may hamper the diagnosis and consequent treatment of the patient and may also increase the incidence of cross-contamination (if sterile practices are not implicated). Commonly grown contaminants include skin flora like Propionibacterium spp., CoNS (coagulase-negative staphylococci), alpha-hemolytic streptococci, and diphtheroids [2]. Therefore, it is of absolute importance that appropriate entities are well versed in the correct timing of BC collection, skin preparation, sample collection site and number, and the appropriate volume of blood. In other words, the quality of blood culture strongly depends upon the collection of the appropriate blood sample [2-4]. Contamination rates of less than 3% are universally accepted as per international standards [3,4]. In the last quarter's analysis, we found that the blood culture contamination rate in our institute is 12%, which is much above the accepted value. Many hospitals like ours do not have a trained phlebotomist for the collection of blood culture samples. Hence, the current study is aimed at determining the effectiveness of a multimodal intervention to improve blood culture collection in a tertiary care hospital situated in South India. This study will also aim to emphasize best practices like the collection of the specimen before starting the first dose of antimicrobial agent, adequate volume to be collected, site of collection of the sample (especially when patients are on the central and peripheral lines), transport of blood culture bottles to the laboratory, etc.
This interventional study will enable us to gauge the practical knowledge and skills of our healthcare workers (HCWs), figure out the discrepancies in the same, and therefore plan out an effective interventional method to correct their blood collection practices. We aspire to improve the quality of blood collection for culture to decrease the rate of growth of contaminants, thus allowing us to provide our patients with the best care possible. Hence, this current study aimed to compare the rate of isolation of contaminants grown among the blood culture specimens during the pre-and post-intervention period, to assess the knowledge, attitude, and practice (KAP) of HCW’s collecting the blood culture specimen on various aspects of sample collection during the pre-and post-intervention period, to educate the nursing staff regarding blood sample collection during the interventional phase of the study using a structured, pre-formed checklist, and to emphasize best practices for blood culture collection during the intervention period.
Materials and methods
The present study is an interventional study carried out for two months (from July 25, 2022, to September 18, 2022) in the adult medicine intensive care unit (MICU) of JSS Hospital, Mysore, Karnataka, India. The period of study is divided into three weeks of pre-intervention, two weeks of intervention, and three weeks of post-intervention. A total of 124 blood culture collection procedures from adult medicine ICUs were observed and recorded through a structured checklist. The study population included nursing staff, medical interns, and postgraduates posted to the adult medicine ICU. All blood culture procedures performed in the adult medicine ICU during a specific time of the day were included in the study. The study was divided into a pre-interventional phase, an interventional phase, and a post-interventional phase.
Pre-intervention phase (three weeks)
A blood culture sample collection audit was conducted daily for 1.5 hours by the direct observation method using a pre-formed structured checklist (Appendix 1), which was adopted from the ANTT (antiseptic non-touch technique). A well-structured knowledge, attitude, and practice (KAP) questionnaire survey regarding blood sample collection for culture were collected from nursing staff, medical interns, and postgraduates posted in the adult medicine ICU, and the data was analyzed. This method provided insight into the knowledge and practical skills of the HCWs and allowed for the preparation of an accurate plan to carry out the intervention. At the end of this phase, the rate of contaminants grown along with the blood culture specimens was analyzed using the following formula:
Blood culture contamination (BCC) rate = Number of contaminated cultures / Total cultures made x 100
Intervention phase (two weeks)
By utilizing the results of direct observation and the KAP survey, a strategic plan comprising multimodal strategies was created. Training and educational sessions were conducted during this period under the guidance of the infection control team. The specific steps mentioned in the checklist were explained to the HCWs, along with their proper sequence. The disadvantages of inaccurate collection of blood culture samples were also stressed. Also, posters related to blood sample collection for culture (Appendix 2) were displayed as visual reminders in the adult medicine ICU and the general medicine ward. The sessions were conducted with educational and linguistic barriers in mind. Additionally, on-site corrections were made daily through one-on-one interaction.
Post-intervention phase (three weeks)
The blood culture sample collection audit was done similarly to the pre-intervention phase. The rate of contaminants growing among blood culture specimens during this period was calculated using the same formula and compared with the pre-intervention period. Knowledge, attitude, and practice (KAP) questionnaire survey regarding blood sample collection for culture were collected from nursing staff, medical interns, and postgraduates posted in the adult medicine ICU, and the data was analyzed and compared with the pre-intervention period. This has enabled us to gauge the impact of the multimodal interventional strategies on the HCWs. All the data generated was entered in MS Excel (Microsoft Corporation, Redmond, Washington, United States) and analyzed using SPSS software (IBM Corp., Armonk, New York, United States). The rate of contaminants growing during pre-and post-intervention phases was calculated using the McNemar test. A P-value less than 0.05 was considered statistically significant.
Results
Blood culture sample collection was audited for six weeks, three weeks before the intervention, and three weeks after the intervention. Around 124 procedures were observed in the pre-intervention and post-intervention periods, respectively. Two samples from different sites were collected into two blood culture bottles as per the standard protocols. The audit was assessed in the pre-and post-interventional phases. Blood culture contamination rates were also determined during these phases. The contamination rates in the pre-and post-interventional phases were 6.16% and 3.03%, respectively. (Table 1). Overall, blood culture positivity in the pre-interventional phase was found to be 4.40% and 6.92% in the post-interventional phase, with a statistically significant reduction in contamination rates.
Table 1. Presenting the blood culture contamination rates in the pre-and post-intervention phases.
*p value <0.05 is considered to be statistically significant
| Total number of cultures | Contaminated cultures | Blood culture contamination rate | P-value | |
| Pre-intervention | 454 | 28 | 6.16% | 0.023* |
| Post-intervention | 462 | 14 | 3.30% |
It was observed that during the pre-interventional phase, 95.16% of the subjects performed hand hygiene before collecting the samples into two blood culture bottles, respectively, and 100% used sterile gloves, applied a tourniquet, palpated the vein, and marked the area. Of the subjects, 95.96% and 92.74% used 70% alcohol and rubbed the skin vigorously (5cm circle) before collecting blood in bottles one and two, respectively. Around 87.9% of the subjects waited for 30 seconds to allow the skin to dry completely, and 99.1% used chlorhexidine or povidone-iodine to disinfect the site concentrically inside out for bottles one and two. Around 85.48% and 83.87% of the subjects waited for two minutes to allow the skin to dry. It was observed that 66.93% and 64.51% of the subjects did not palpate skin again after disinfection for both bottles, and 100% of the subjects used an alcohol wipe to clean the bottle top for bottle one and 99.1% for bottle two. The same needle was used for blood collection and injection into the BACTEC bottle by 100% of the subjects. It was also observed that 88.7% of the subjects collected the ideal volume, i.e., 8-10 ml for adults and 1-3ml for pediatric or sterile fluid, into both bottles.
After the interventional phase and during the post-interventional phase, the percentage of adherence to following the steps showed a significant increase (Table 2).
Table 2. Presenting the observations while collecting blood for culture in the pre-and post-intervention phases.
| Steps | Pre-intervention | Post-intervention | ||
| Bottle 1 | Bottle 2 | Bottle 1 | Bottle 2 | |
| 1. Performed hand hygiene | 95.16% (118) | 95.16% (118) | 97.58% (121) | 97.58% (121) |
| 2. Used sterile gloves | 100% (124) | 100% (124) | 100% (124) | 100% (124) |
| 3. Applied tourniquet, palpated the vein and marked the area | 100% (124) | 100% (124) | 100% (124) | 100% (124) |
| 4. Used 70% alcohol and rubbed the skin vigorously (5cm circle) | 95.96% (119) | 92.74% (115) | 100% (124) | 98.38% (122) |
| 5. Waited for 30 sec (allow the skin to dry) | 87.9% (109) | 87.09% (108) | 95.96% (119) | 96.77% (120) |
| 6. Used chlorhexidine /povidone I2 to disinfect site concentric inside out | 99.1% (123) | 99.1% (123) | 100% (124) | 100% (124) |
| 7. Waited for two minutes (allow the skin to dry) | 85.48% (106) | 83.87% (104) | 96.77% (120) | 98.38% (122) |
| 8. Did not palpate skin again after disinfection | 66.93% (83) | 64.51% (80) | 82.25% (102) | 83.06% (103) |
| 9. Used an alcohol wipe to clean the bottle top | 100% (124) | 99.1% (123) | 100% (124) | 100% (124) |
| 10. Used the same needle for blood collection and injecting into the Bactec bottle | 100% (124) | 100% (124) | 100% (124) | 100% (124) |
| 11. Volume collected (Ideal: 8-10ml for adult, 1-3ml for pediatric/sterile fluid) | 88.7% (110) | 79.8% (99) | 95.96% (119) | 95.96% (119) |
During the pre-and post-interventional phases, two components were adopted that aimed at assessing the knowledge of blood sample collection among healthcare workers and others to assess their attitude and practice of blood sample collection for culture. The KAP survey had 54 HCWs participate in it. In the pre-interventional phase, 64.81% were aware that sample collection has to be done from two different venipuncture sites, 57.4% knew the correct technique of sterilizing the site for drawing blood, 42.59% palpated skin after disinfection, and 48.14% were aware of the WHO-assigned "My 5 Moments of Hand Hygiene." Of the participants, 53.79% knew about the minimum duration for which hand rub has to be performed; 75.92% were aware of the volume of blood to be collected in adults and pediatric cases/sterile fluids; 74.07% were aware of using an alcohol wipe to clean the bottle cap; and 72.22% knew the appropriate time for the collection of blood for culture. The post-interventional phase showed a significant variation in the knowledge-based questionnaire provided to the HCWs (Table 3).
Table 3. Presenting the responses to the knowledge-based questions during the pre-and post-intervention phases.
| Knowledge-based questions | Correct responses | |
| Pre-intervention | Post-intervention | |
| Collection of samples from two different venipuncture sites | 64.81% (35) | 83.33% (45) |
| Correct technique of sterilizing the site for drawing blood | 57.4% (31) | 88.88% (48) |
| Palpation of skin after disinfection | 42.59% (23) | 66.66% (36) |
| WHO-assigned "My 5 Moments of Hand Hygiene" | 48.14% (26) | 77.77% (42) |
| Minimum duration for which hand rub has to be performed | 53.7% (29) | 70.37% (38) |
| Volume of blood to be collected in adults and pediatric cases/ sterile fluids | 75.92% (41) | 90.74% (49) |
| Usage of an alcohol wipe to clean the bottle cap | 74.07% (40) | 85.18% (46) |
| Appropriate time for collection of blood for culture | 72.22% (39) | 83.33% (45) |
A questionnaire based on application and practice was provided to the HCWs as a part of the second component in the pre-and post-interventional phases, and it was observed that there is a significant change in the post-interventional phase compared to the pre-interventional phase (Table 4).
Table 4. Presenting the results of the application and practice-based questions during the pre-and post-interventional phases.
| AP1. Did you follow all the steps as per the SOP/poster for collecting the sample? | Pre-intervention | Post-intervention |
| Yes | 81.5% (44) | 92.59% (50) |
| Yes, partially | 18.5% (10) | 7.4% (4) |
| No | 0 | 0 |
| AP2. Which of the following aspects will help you to adhere to the correct method of blood sample collection? | ||
| Visual reminders like posters | 35.2% (19) | 40.74% (22) |
| Observing seniors | 16.7% (9) | 12.96% (7) |
| Educational sessions | 27.8% (15) | 24.07% (13) |
| Provision of a pre-formed checklist | 20.4% (11) | 22.22% (12) |
| AP3. What makes you not perform hand hygiene when required? | ||
| Inadequate availability of hand rub products | 9.25% (5) | 14.81% (8) |
| Forgetfulness | 88.88% (48) | 85.18% (46) |
| Lack of motivation | 1.85% (1) | 0 |
| Allergy to hand rub product | 0 | 0 |
| AP4. Your diagnosis is usually dependent on the blood culture? | ||
| Always | 33.3% (18) | 37.03% (20) |
| Sometimes | 66.7% (36) | 62.96% (34) |
| Never | 0 | 0 |
| AP5. Do you deliver the drawn blood into the culture bottle with the same needle used for venipuncture? | ||
| Always | 38.9% (21) | 72.22% (39) |
| Sometimes | 57.4% (31) | 25.92% (14) |
| Never | 3.2% (2) | 1.85% (1) |
| AP5. Are the standard precautions followed by you before and after collecting the sample for blood culture? | ||
| Always | 59.3% (32) | 75.92% (41) |
| Sometimes | 40.7% (22) | 24.07% (13) |
| Never | 0 | 0 |
Discussion
Bloodstream infections (BSIs) and septicemia are known to be significant causes of morbidity and mortality in a healthcare setting, and blood cultures play a vital role in their diagnosis [5]. Identification of the etiological agents and appropriate treatment plays a vital role in reducing mortality and morbidity [6]. Pre-analytical phase workflow, i.e., several factors such as the technique of specimen collection, volume of blood collected, number of BCs drawn, time of collection concerning antibiotic administration, and transport time of blood cultures by any process in the laboratory attribute to the quality of the final results and the outcome [7-11]. Healthcare workers working in tertiary care hospitals with huge patient loads and busy schedules can attribute this to the dereliction of the preanalytical workflow of blood culture tests. These will directly affect the outcome of the investigation, which will directly determine the treatment provided to the patients. Hence, a continuous monitoring system and education of the staff should exist to reduce such outcomes in a tertiary care hospital. Therefore, this study was carried out to develop a multimodal intervention and, subsequently, to evaluate its effectiveness in improving BC collection practices in a tertiary care hospital. According to the recommendations from the Clinical and Laboratory Standards Institute (CLSI), a blood culture contamination rate of less than 3% is acceptable [12]. As compared to the pre-(6.16%) and post-interventional phases (3.03%), the current study's contamination rates show a considerable decrease in the post-interventional phase. The current study involved a multimodal intervention, which included educational intervention and displaying standard protocols for blood sample collection for culture and sensitivity at the collection sites. This has majorly contributed to the significant reduction in contamination in the post-interventional phase. Concentrating on other groups like HCWs on rotational shifts, interns, resident doctors, and newly joined HCWs can even reduce the contamination further.
There are many reasons for blood culture contamination, like patients' own skin commensal flora, HCWs being the source, and sometimes from the hospital environment [13-16]. The major limitation of this study is that the source of blood culture contamination was not assessed. Further, the compliance with the blood culture sample collection protocol, knowledge, and attitude of HCWs were evaluated using a pre-formed questionnaire. Compared to the pre-intervention group, there was a significant improvement in the compliance of HCWs to draw BCs in pairs. Several studies have documented that the collection of paired or multiple BCs results in improvements in pathogen isolation and also helps in differentiating contaminants from pathogens, and the results of our study also showed similar findings. Similarly, their knowledge of blood sample collection and attitude toward and practice of blood sample collection for blood culture showed a significant change in the post-interventional phase when compared to the pre-interventional phase.
Conclusions
For decades, blood cultures have been considered a potential tool for saving lives. However there are several problems during blood sample collection that in turn increase contamination rates and can directly affect the patients, for example: long hospital stays, increased diagnostic tests, prolonged antimicrobial exposure, and unnecessary usage of antibiotics. This can directly contribute to the morbidity and mortality of patients. Tertiary care hospitals with huge patient loads can attribute this to these parameters. Hence, we tried to implement a comprehensive multimodal interventional study that aimed at assessing blood culture contamination, assessing the knowledge, attitude, and practice of HCWs collecting the blood culture specimen on various aspects of sample collection during the pre-and post-intervention period, educating the nursing staff regarding blood sample collection during the interventional phase of the study, and using a structured, pre-formed checklist to emphasize best practices for blood culture collection during the intervention period. Through this, we found that implementing studies like these can result in a significant reduction of BC contamination rates and can also improve the compliance of HCWs with BC protocol. This, in turn, can overall improve the effectiveness of BC testing and reduce mortality and morbidity in tertiary care hospitals.
Appendices
Appendix 1
Table 5. Checklist for blood sample collection.
| Checklist for blood sample collection | ||
| Name: Age: Sex: | ||
| Hospital No: | ||
| Department: Unit: | ||
| Date and time of blood culture sent | ||
| Blood culture sent: a. Before starting antibiotics b. After starting antibiotics | ||
| Provisional diagnosis: | ||
| Site: CL/PL/V (Central line/Peripheral line/Venipuncture) | 1st Bottle | 2nd Bottle |
| 1. Performed hand hygiene | ||
| 2. Used sterile gloves | ||
| 3. Applied tourniquet, palpated the vein and marked the area | ||
| 4. Used 70% alcohol and rubbed the skin vigorously (5cm circle) | ||
| 5. Waited for 30 sec (allow the skin to dry) | ||
| 6. Used chlorhexidine/povidone iodine to disinfect site concentric inside out | ||
| 7. Waited for two mins (allow the skin to dry) | ||
| 8. Did not palpate skin again after disinfection | ||
| 9. Used alcohol wipe to clean the bottle top | ||
| 10. Used the same needle for blood collection and injecting to Bactec bottle/blood culture bottle | ||
| 11. Adequate volume collected (Ideal: 8-10 ml for adults, 1-3 ml for Pediatric/ sterile fluids) | ||
Appendix 2
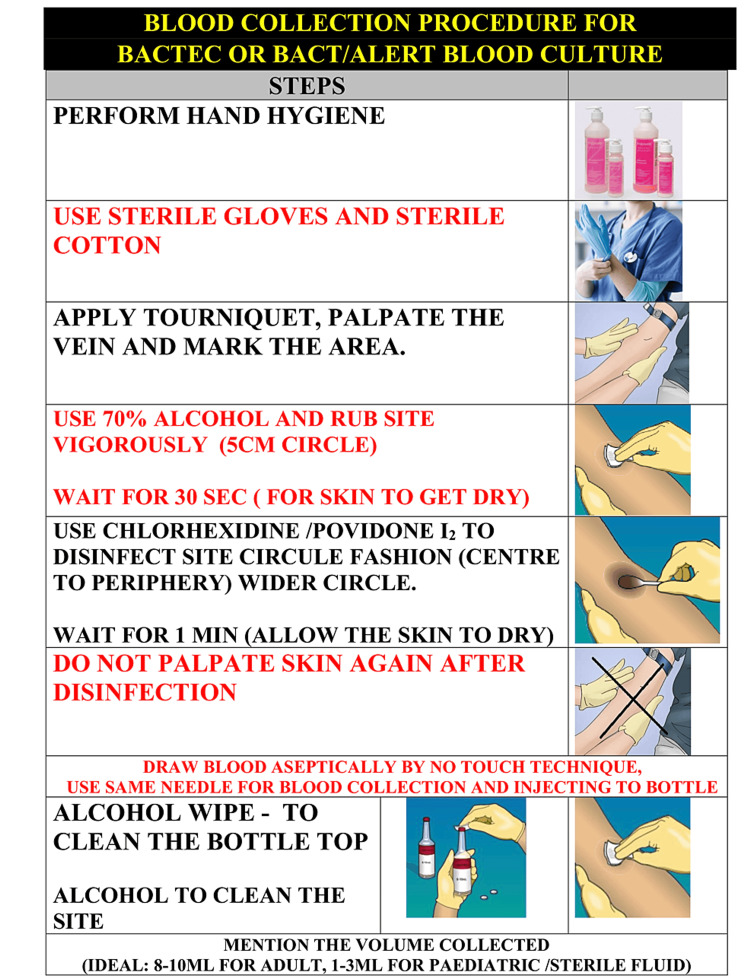
Figure 1. Blood culture collection poster.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Krishna Karthik, Isha Kumthekar , Tejashree Urs, Deepashree Rajashekar
Acquisition, analysis, or interpretation of data: Krishna Karthik, Isha Kumthekar , Tejashree Urs, Deepashree Rajashekar
Drafting of the manuscript: Krishna Karthik, Isha Kumthekar , Tejashree Urs, Deepashree Rajashekar
Critical review of the manuscript for important intellectual content: Krishna Karthik, Tejashree Urs, Deepashree Rajashekar
Supervision: Krishna Karthik, Tejashree Urs, Deepashree Rajashekar
Human Ethics
Consent was obtained or waived by all participants in this study. JSS Medical College, JSS Academy of Higher Education and Research issued approval SSMC/IEC/050722/24/NCT/2022-23. Institutional ethics committee approval was obtained before initiation of the study (JSSMC/IEC/050722/24/NCT/2022-23, dated 08.07.2022)
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2018 update by the Infectious Diseases Society of America and the American Society for Microbiology. Miller JM, Binnicker MJ, Campbell S, et al. Clin Infect Dis. 2018;67:0. doi: 10.1093/cid/ciy584. [DOI] [PubMed] [Google Scholar]
- 2.ANTT: an essential tool for effective blood culture collection. Rowley S, Clare S. Br J Nurs. 2011;20:S9-10, S12-4. doi: 10.12968/bjon.2011.20.Sup7.S9. [DOI] [PubMed] [Google Scholar]
- 3.Sepsis: definition, epidemiology, and diagnosis. Lever A, Mackenzie I. BMJ. 2007;335:879–883. doi: 10.1136/bmj.39346.495880.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clinical and Laboratory Standards Institute. Procedures for Collection of Diagnostic Blood Specimens by Venipuncture; Approved Standard- Sixth Edition. Wayne, PA: CLSI document H3-A6; 2007. Procedures for Collection of Diagnostic Blood Specimens by Venipuncture; Approved Guideline. CLSI Document H3-A6. [Google Scholar]
- 5.Effectiveness of a novel specimen collection system in reducing blood culture contamination rates. Bell M, Bogar C, Plante J, Rasmussen K, Winters S. J Emerg Nurs. 2018;44:570–575. doi: 10.1016/j.jen.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Economic health care costs of blood culture contamination: a systematic review. Dempsey C, Skoglund E, Muldrew KL, Garey KW. Am J Infect Control. 2019;47:963–967. doi: 10.1016/j.ajic.2018.12.020. [DOI] [PubMed] [Google Scholar]
- 7.Reducing blood culture contamination in the emergency department: an interrupted time series quality improvement study. Self WH, Speroff T, Grijalva CG, et al. Acad Emerg Med. 2013;20:89–97. doi: 10.1111/acem.12057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Factors impacting the pre-analytical quality of blood cultures-analysis at a tertiary medical center. Romann L, Werlen L, Rommers N, et al. PLoS One. 2023;18:0. doi: 10.1371/journal.pone.0282918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Practical guidance for clinical microbiology laboratories: a comprehensive update on the problem of blood culture contamination and a discussion of methods for addressing the problem. Doern GV, Carroll KC, Diekema DJ, Garey KW, Rupp ME, Weinstein MP, Sexton DJ. Clin Microbiol Rev. 2019;33 doi: 10.1128/CMR.00009-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The effectiveness of interventions to reduce peripheral blood culture contamination in acute care: a systematic review protocol. Hughes JA, Cabilan CJ, Williams J, Ray M, Coyer F. Syst Rev. 2018;7:216. doi: 10.1186/s13643-018-0877-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reduction in blood culture contamination through use of initial specimen diversion device. Rupp ME, Cavalieri RJ, Marolf C, Lyden E. Clin Infect Dis. 2017;65:201–205. doi: 10.1093/cid/cix304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reducing blood culture contamination in community hospital emergency departments: a multicenter evaluation of a quality improvement intervention. Self WH, Mickanin J, Grijalva CG, et al. Acad Emerg Med. 2014;21:274–282. doi: 10.1111/acem.12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reduction of blood culture contamination rates after implementation of a phlebotomist team. Foggiato GF, Tuon FF, Becker G, et al. https://www.ajicjournal.org/article/S0196-6553(17)30149-9/pdf. Am J Infect Control. 2017;45:698–699. doi: 10.1016/j.ajic.2017.02.028. [DOI] [PubMed] [Google Scholar]
- 14.Impact of blood cultures drawn by phlebotomy on contamination rates and health care costs in a hospital emergency department. Gander RM, Byrd L, DeCrescenzo M, Hirany S, Bowen M, Baughman J. J Clin Microbiol. 2009;47:1021–1024. doi: 10.1128/JCM.02162-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Frequently Asked Questions on Bloodstream Infection (BSI) Events. [ May; 2023 ]. 2021. https://www.cdc.gov/nhsn/faqs/faq-bsi.html https://www.cdc.gov/nhsn/faqs/faq-bsi.html
- 16.Significance of coagulase negative Staphylococcus from blood cultures: persisting problems and partial progress in resource constrained settings. Sidhu SK, Malhotra S, Devi P, Tuli AK. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5420390/ Iran J Microbiol. 2016;8:366–371. [PMC free article] [PubMed] [Google Scholar]