Abstract
Objectives
To determine the impact of a pharmacist-led telephone outreach program among patients discharged from the emergency department (ED) to home.
Study Design
We conducted a randomized, controlled study from February to November 2019 at a tertiary care academic medical center.
Methods
At ED discharge, subjects were randomized to usual care (controls) or usual care plus the pharmacist’s review (intervention group). Eligible subjects included those being discharged from the ED to home with ≥ 8 medications. A pharmacist telephoned subjects in the intervention group within 48–96 hours after ED discharge. The medications in the patient’s record from the ED were compared to what the patient was taking at home. Discrepancies were communicated to the primary provider via fax or telephone. The primary outcomes included overall healthcare utilization including unplanned hospital readmissions or ED visits within 30 days of discharge. The effect of intervention on the number of acute events were analyzed using a Poisson regression model adjusting for relevant baseline characteristics.
Results
Of 90 eligible subjects, 45 patients were in the intervention and control groups. Twenty-six patients (58%) in the intervention group were reached and 56 interventions were provided by the pharmacists. There was no significant difference between groups for overall healthcare utilization (aRR, 1.01; 95% CI, 0.50, 2.06; p=0.96), hospitalizations (aRR, 0.20; 95% CI, 0.02, 2.18; p=0.19) and ED visits (RR: 1.24, 95% CI 0.56, 2.79; p=0.59).
Conclusions
A pharmacist-led telephone outreach program post-ED discharge was not associated with a change in healthcare utilization.
Introduction
When patients transition between care settings, they are at an increased risk of adverse drug events and unplanned readmissions, which can result in an annual estimated cost of over $26 billion.1 Studies have shown that adverse drug events (ADEs) are a significant contributor of emergency department (ED) visits to complications following a transition of care (TOC).2–4 Studies of consecutive discharges found that nearly 20% experience adverse drug events within 45 days of hospital discharge, and 66% of complications occurring within 3 weeks of discharge were from ADEs.5,6 As a result, there is increased interest from hospitals, health systems, and payers to implement various TOC programs aimed at reducing readmissions and overall healthcare utilization.
Pharmacists play a key role in TOC as part of an inter-professional healthcare team. A meta-analysis demonstrated that pharmacy-led medication reconciliations interventions were an effective strategy to reduce medication discrepancies.7 A recent systematic review on pharmacists’ impact at the TOC highlighted the crucial role pharmacists play promoting medication adherence and providing effective medication reconciliation.8 However, the review did not identify any one intervention to be the most effective in improving care transitions. Pharmacist involvement within care transitions is common for hospitalized patients being discharge or in ambulatory care settings following discharge.8–10 Despite the potential benefits pharmacists provides at care transitions, there are few reported pharmacist transition interventions occurring in the ED.
The ED plays a significant role in delivering healthcare services and providing care in medically underserved areas.11,12 Pharmacists could contribute to ED transitions by assessing medication reconciliation, ensuring medication access at discharge, and reviewing for contraindicated medications. 13 Hohner et al. reported a clinical pharmacist TOC program between the ED and ambulatory care pharmacists.14 This program provided patient-specific comprehensive medication review and education in the ED setting and ensured coordinated transition to the ambulatory care setting. Hohner and colleagues recruited 18 subjects and 5 were followed with a pharmacist on average 16 days after ED discharge. Pearson et al. described a pharmacist-led care transition intervention targeting high-risk older adults after an ED visit.15 This retrospective pilot study included a telephonic outreach and assessment by a clinical pharmacist. No differences were found in the primary outcomes of ED visit, hospitalization, or death within 30 days after ED discharge. Additional evidence is required to demonstrate that pharmacist TOC interventions in the ED can improve medication management and reduce healthcare utilization.
A pharmacist-led telephone call back program following ED care has the potential to improve medication adherence, and potentially reduce unneeded ED visits and hospital admissions. However, the literature on pharmacist-led ED transition programs is sparse and both reported studies are observational. Therefore, the objective of this study was to evaluate the impact of a pharmacist-led telephone outreach program among patients recently discharged from the ED.
Methods
Trial Design and Participants
The study was a 1:1, prospective randomized controlled trial conducted from February to November 2019 at Erie County Medical Center (ECMC), approved by the University at Buffalo Investigational Review Board. The study followed Consolidated Standards of Reporting Trials (CONSORT) 2010 statement and CONSORT-Outcomes 2022 Extension.16 Patients were recruited from ECMC’s treatment area, and those taking ≥ 8 medications were approached to participate in the study. Inclusion and exclusion criteria for this study were summarized in Table S1 (in Appendix 1).17,18
Intervention Description & Sample size calculation
The intervention group received usual care and a pharmacist intervention via telephone 48–96 hours after ED discharge, while the control group received usual care only. Full descriptions of study procedures and interventions are documented in Appendix 2.
We aimed to screen all patients who had ED visit for potential inclusion. For our primary analysis, we employed a 2-side α of 0.05, and aimed for a power of 80%. The control group was expected to have a 30-day unplanned hospital utilization probability ranging from 25% to 40% based on previous literature.19–21 With the assumption that our intervention would result in a minimum reduction of 20% unplanned hospital utilization, we calculated a sample size requirement of 94 patients. Accounting for an estimated 20% loss follow-up, the adjusted sample size would be 112 patients (56 in the intervention group and 56 in the control group).
Outcomes and Covariates
The primary outcome was to evaluate the effectiveness of the pharmacist intervention in reducing unplanned hospital utilization within 30 days of ED discharge. The unplanned hospital utilization was defined as a composite of unexpected ED visits and/or hospital admissions. The study collected demographic and clinical variables during the interview, including knowledge of taking medications, adherence to the medications, barriers of access to medications, and confirmed follow-up appointments with the primary care provider (PCP). Full descriptions are available in Appendix 2.
Statistical analyses
Outcome measures were evaluated at the patient level between the intervention and control groups. Categorical variables were reported as percentages and compared using the chi-square test; continuous variables were reported as medians (interquartile ranges, IQR) and compared using the Mann-Whitney U test.
To assess differences between groups in the incidence rate of unplanned hospital utilization, a two-rate chi-square was initially used, followed by separate assessments of hospitalizations and ED visits. Poisson regression analysis was employed to evaluate the difference in healthcare utilization count between groups, with adjustment for age, gender, race, number of comorbidities, and medications. Main analysis and secondary analysis were performed to comprehensively evaluate the outcomes. Main analysis included all enrolled samples from the intervention and control groups after exclusion criteria were applied. In our secondary analysis, we excluded patients in the intervention group who were not successfully contacted by pharmacists. The analysis was performed using SAS version 9.4 (SAS Institute, Cary, NC). All hypothesis testing was 2-sided with a significance level set at p<0.05.
Results
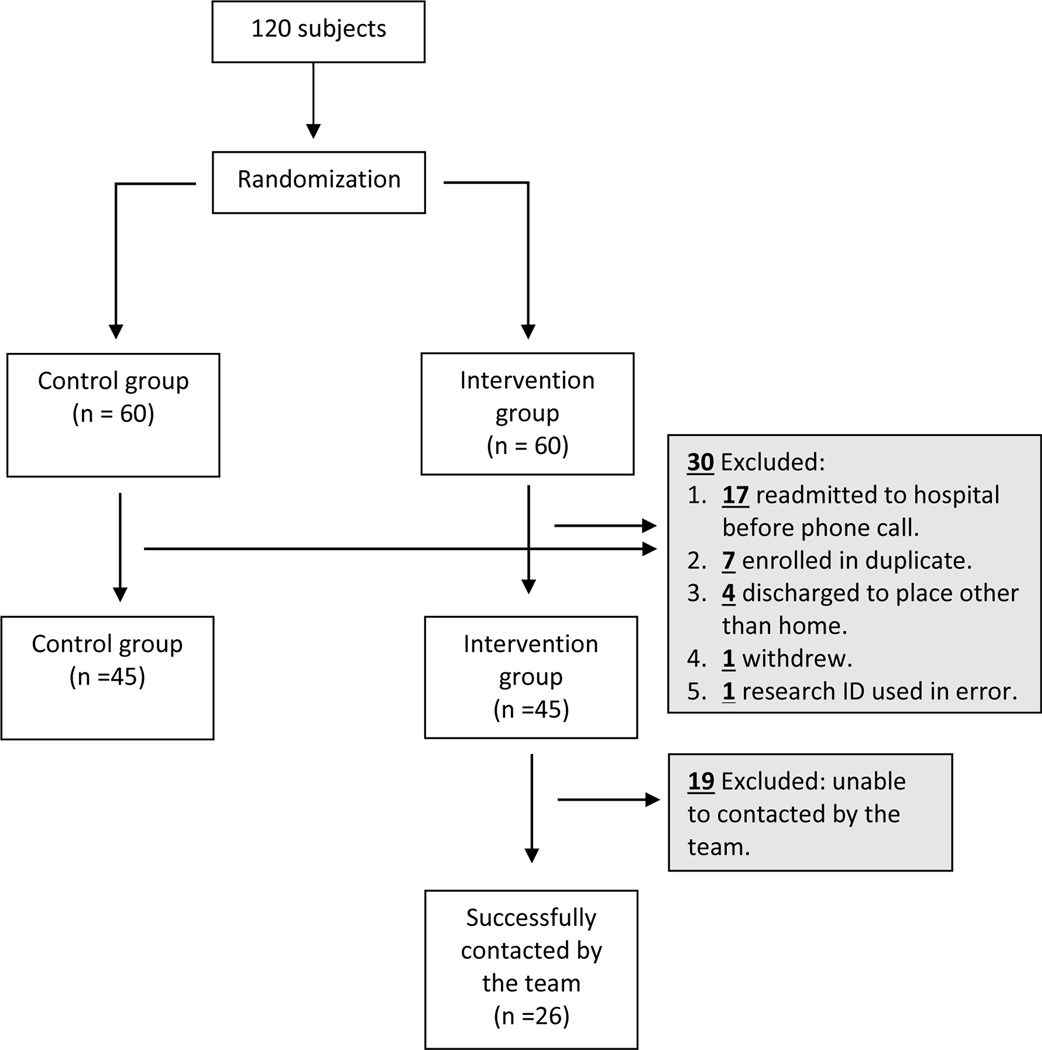
A total of 120 subjects were initially enrolled in the study. Of these, 30 subjects were subsequently eliminated as ineligible (Figure 1). The final study sample consisted of 90 subjects (29 males and 52 females) with a mean age at 58.2 years ± 12.1. These subjects were randomly assigned to either the intervention or control group, with 45 subjects in each group. However, only 57.8% of subjects in the intervention group were successfully contacted by a pharmacist.
Figure 1.
Study recruitment flow chart
Table S2 (in Appendix 6) showed that there were no significant differences in age, gender, or race between the two groups, but the intervention group had more comorbidities and medications. The top three comorbidities found were hypertension (n=14), hyperlipidemia (n=11), and diabetes (n=7). During telephone interviews, 56 interventions were provided, with the most frequent being general counseling and monitoring (n=13, Table S3, in Appendix 6). Medication discrepancies (n=68) were also identified, with 33 (48.5%) discrepancies relating to the number of medications reported at home and 35 (51.5%) relating to dosage or regimen. On average, the pharmacist spent a total of 62.5 minutes per case. This included 21.3 minutes reviewing the subject’s record before making the call, 16.2 minutes conducting the interview, and 25 minutes for documenting the call.
The incidence rate of unplanned hospital utilization within 30 days from the main analysis did not show a statistically significant difference between the intervention and control groups (p=0.61) (Table 1). There was also no significant difference in the rates of unexpected ED visits (p=0.34) and hospitalizations (p=0.45). The adjusted Poisson regression models did not demonstrate significant changes in overall unplanned hospital utilizations (adjusted Risk Ratio [aRR], 1.01; 95% confident interval [CI], 0.50, 2.06; p=0.96), ED visits (aRR, 1.42; 95%CI, 0.56, 2.79; p=0.59), or hospitalizations (aRR, 0.20; 95%CI, 0.02, 2.18; p=0.19) between the intervention and control groups (Table 1). The secondary analysis also showed similar findings.
Table 1.
Rate of unplanned hospital utilization and outcomes among patients with or without the pharmacist telephone intervention
| Intent-to-treat analysis | Case (n=45) | Control (n=45) | ||||
|---|---|---|---|---|---|---|
| Total | ED | Admission | Total | ED | Admission | |
| No. of healthcare event within 30 days (%) | 18 (100) | 16 (88.9) | 2 (11.1) | 15 (100) | 11 (73.3) | 4 (26.7) |
| Rate of healthcare event per 100 persons (95% CI) | 40 (23.7, 63.2) | 35.6 (20.3, 57.7) | 4.4 (0.5, 16.1) | 33.3 (18.6, 55.0) | 24.4 (12.2, 43.7) | 8.9 (2.4, 22.8) |
| Rate difference between groups (95% CI) | 6.67 (−18.4, 31.7) | 11.1 (−11.5, 33.7) | −4.4 (−15.1, 6.2) | |||
| p=0.61 | p=0.34 | p=0.45 | ||||
| Per-protocol analysis | Case (n=26) | Control (n=45) | ||||
| Total | ED | Admission | Total | ED | Admission | |
| No. of healthcare event within 30 days (%) | 10 (100) | 8 (80.0) | 2 (20.0) | 15 (100) | 11 (73.3) | 4 (26.7) |
| Rate of healthcare event per 100 persons (95% CI) | 38.5 (18.4, 70.7) | 30.8 (13.3, 60.6) | 7.7 (0.9, 27.8) | 33.3 (18.6, 55.0) | 24.4 (12.2, 43.7) | 8.9 (2.4, 22.8) |
| Rate difference between groups (95% CI) | 5.1 (−24.1, 34.3) | 6.3 (−19.4, 32.1) | −1.2 (−15.0, 12.6) | |||
| p=0.72 | p=0.62 | p=0.90 | ||||
| Intent-to-treat analysis | ||||||
| Intervention vs. control | Unadjusted model | Adjusted a model | ||||
| Poisson regression model | Total | ED | Admission | Total | ED | Admission |
| Risk Ratio (95%CI) | 1.20 (0.60, 2.38) | 1.45 (0.68, 3.13) | 0.50 (0.09, 2.73) | 1.01 (0.50, 2.06) | 1.24 (0.56, 2.79) | 0.20 (0.02, 2.18) |
| P-value | 0.60 | 0.34 | 0.42 | 0.96 | 0.59 | 0.19 |
| Per-protocol analysis | ||||||
| Intervention vs. control | Unadjusted model | Adjusted a model | ||||
| Poisson regression model | Total | ED | Admission | Total | ED | Admission |
| Risk Ratio (95%CI) | 1.15 (0.52, 2.57) | 1.26 (0.51, 3.13) | 0.86 (0.16, 4.72) | 1.08 (0.47, 2.50) | 1.27 (0.49, 3.29) | 0.38 (0.03, 4.96) |
| P-value | 0.73 | 0.62 | 0.87 | 0.85 | 0.62 | 0.46 |
Adjusted for age, gender, race, number of medications, and number of comorbidities
Abbreviation: CI, confident interval; ED, emergency department
Discussion
In this trial, a pharmacist-led telephone outreach program following ED discharge was not associated with a change in 30-day ED revisits or hospitalizations. Pharmacists were able to follow up with subjects after ED discharge and perform a medication reconciliation interview with the subject or caregiver. This led to numerous interventions related to medication list discrepancies at discharge, medication access issues, and counseling on appropriate medication administration for high-risk drugs such as insulin. In some instances, the pharmacists followed up directly with the subject’s primary care provider as they deemed the identified medication-related problems time-sensitive. These recommendations are viewed as a study strength and supports the value of a pharmacy-led outreach program after ED discharge.
Return visits to the ED and hospital are costly on health systems and the ED discharge process is typically a high-stress encounter with patients. Medication-related problems including adverse events, medication access, and incorrect medication lists are common following ED discharge.22,23 Implementation of a pharmacy telephone outreach program after discharge is an innovative approach towards reducing medication related problems. This is the first RCT to evaluate a pharmacist-led outreach program after ED discharge and we were successfully able to implement the program within a medically unserved area. Numerous medication interventions were completed, yet we found no statistical differences in return ED visits or hospitalizations. Two previous studies have evaluated similar pharmacist-led interventions and found no significant differences in 30- or 90-day repeat ED visits or hospitalizations.14,15 Post ED discharge outreach or callback programs are receiving broad attention across the U.S. as it represents an opportunity to improve care and is used as a quality metric. However, most studies focus on physician or nurse outreach post-discharge and are unable to demonstrate improvement in patient outcomes.24,25 The optimal location and time for medication reconciliation during a care transition has not been identified.8 Given the complexities at ED discharge it will be a priority to further explore pharmacist-led interventions either within the ED or directly after discharge.
The pharmacist interview led to numerous medication-related interventions which supports the value provided by the program. Currently, there is a lack of economic data to support pharmacist-led care transition programs and the value provided to the healthcare system. Although we did not perform a formal economic analysis, the estimated pharmacist costs based on current salary data was ~$38 per subject with an overall cost of $1,724.26 As health care shifts towards value-based payment systems there will be pharmacists’ opportunities to provide transition interventions within different parts of the care continuum. Most pharmacist-led care transition interventions occur within the hospital, yet care transition pharmacists and interventions are expanding into primary care, community, and long-term care settings.8,27–29 Despite pharmacist role expansion into the TOC process, there is still insufficient evidence for the most effective pharmacist-led intervention for improving the continuity of care. Moving forward, studies should include both clinical and economic outcomes with a priority on using rigorous study designs. This will provide best practices and identify pharmacist-led TOC services that improve care and are cost-effective.
One potential approach to enhance the outcomes of pharmacist-led intervention programs is through collaborative efforts among providers, patients, and pharmacists. For example, Taber et al. developed and implemented an mobile app and web portal to consolidate patient-level data.30 This system aimed to monitor the occurrence and severity of medication errors in kidney transplant recipients.30,31 By using this technology, pharmacists could receive automatic notifications from patients regarding medication changes through the app. They could then take necessary actions, such as scheduling tele-visits with patients or contacting physicians for recommendations to prevent medication errors. Report showed that the participants who received this intervention demonstrated a significant reduction in medication errors (incident risk ratio, 0.39, p<0.001).32 In future studies, it is recommended to adopt a similar automated workflow to provide pharmacists with comprehensive patient-level data and enable the capture of a broader range of cases.
There are several important limitations to consider when interpreting the findings of our study. First, our data analysis was based solely on information obtained from ED discharge summaries and charts. his limited our ability to access vital patient information, such as living situations, previous ED visits, and inpatient admissions. While we were able to determine patient insurance status, we could not determine the specific plan or coverage, potentially affecting the validity of our results. Future studies should aim to collect more comprehensive patient data to ensure the accuracy of their findings. Second, our post-ED outreach call was primarily focused on medication, and other factors that could contribute to ED revisits and hospitalizations, such as communication between providers and patients, and socio-economic status, were not fully considered. This lack of information may limit the generalizability of our results, and future research should explore these aspects to validate our findings. Third, we excluded patients in the intervention group from the analysis who were readmitted prior to receiving an outreach call, which may have created a selection bias. Future studies should take this into consideration to minimize the potential for a selection bias. Fourth, our final sample was underpowered after exclusion criteria were applied, and we were only able to contact 58% of the patients in the intervention group, which could have introduced bias into our results. Future research with powered samples should be conducted to evaluate the effect of pharmacist-led TOC intervention program. To improve contact and participation rates, future studies may need to explore alternative strategies, such as offering incentives or compensation to patients. Taken together, these limitations underscore the need for caution when interpreting our findings, and future research must address them to enhance the validity and generalizability of their results.
Conclusions
ED discharge poses significant difficulties for healthcare systems and can cause distress for patients. Despite this, our study found that implementing a pharmacist-led telephone outreach program after ED discharge did not result in a decrease in the number of ED revisits or hospitalizations within 30 days. Nevertheless, pharmacists were able to address medication-related problems such as incorrect medication lists and medication access issues. The effectiveness of pharmacist-led interventions during the TOC process in the ED discharge process requires further investigation.
Supplementary Material
Précis to appear on the table of contents:
Pharmacist roles in transitions of care continue to evolve. Evaluation of pharmacist interventions as patients transition from emergency department to home is needed.
Take-Away Points:
In this analysis of pharmacist’s telephone interventions as patients transition from emergency department to home, a clear benefit on unplanned hospital utilization was not identified
Pharmacists made a number of interventions that potentially affect unplanned hospital utilization
Despite not finding a statistical difference a trend towards beneficial impact on unplanned hospital utilization was seen in the intervention group
Telephone interventions may not be an ideal method of reaching patients as only 57.8% of patients in the intervention group could be successfully contacted.
Acknowledgments:
DMJ is supported by the National Institutes of Health (NIH)/National Heart, Lung, and Blood Institute Award No. K23HL153582. Research reported in this publication was supported by the National Center for Advancing Translational Services of the NIH under Award No. ULTR001412 to the University at Buffalo.
Funding sources:
This project was supported by the American Society of Health-System Pharmacists Research and Education Foundation (ASHP Foundation) New Investigator Award.
Contributor Information
Terry E. Dunn, State University of New York at Buffalo, School of Pharmacy and Pharmaceutical Sciences.
Kalpesh J. Desai, State University of New York at Buffalo, School of Pharmacy and Pharmaceutical Sciences.
Michael P. Krajewski, State University of New York at Buffalo, School of Pharmacy and Pharmaceutical Sciences.
David M. Jacobs, State University of New York at Buffalo, School of Pharmacy and Pharmaceutical Sciences.
Chi-Hua Lu, State University of New York at Buffalo, School of Pharmacy and Pharmaceutical Sciences.
Sucharita Paul, State University of New York at Buffalo, Department of Emergency Medicine, Jacobs School of Medicine.
Joseph A. Paladino, State University of New York at Buffalo, School of Pharmacy and Pharmaceutical Sciences.
References.
- 1.Centers for Medicare and Medicaid Services. Community-based care transitions program. Available at: https://innovation.cms.gov/initiatives/CCTP/. Accessed March 15, 2023. [Google Scholar]
- 2.Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. Mar 5 2003;289(9):1107–16. doi: 10.1001/jama.289.9.1107 [DOI] [PubMed] [Google Scholar]
- 3.American College of Clinical P, Kirwin J, Canales AE, et al. Process indicators of quality clinical pharmacy services during transitions of care. Pharmacotherapy. Nov 2012;32(11):e338–47. doi: 10.1002/phar.1214 [DOI] [PubMed] [Google Scholar]
- 4.American Pharmacists A, American Society of Health-System P, Steeb D, Webster L. Improving care transitions: optimizing medication reconciliation. J Am Pharm Assoc (2003). Jul-Aug 2012;52(4):e43–52. doi: 10.1331/JAPhA.2012.12527 [DOI] [PubMed] [Google Scholar]
- 5.Kanaan AO, Donovan JL, Duchin NP, et al. Adverse drug events after hospital discharge in older adults: types, severity, and involvement of Beers Criteria Medications. J Am Geriatr Soc. Nov 2013;61(11):1894–9. doi: 10.1111/jgs.12504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. Feb 4 2003;138(3):161–7. doi: 10.7326/0003-4819-138-3-200302040-00007 [DOI] [PubMed] [Google Scholar]
- 7.Mekonnen AB, McLachlan AJ, Brien JA. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open. Feb 23 2016;6(2):e010003. doi: 10.1136/bmjopen-2015-010003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bethishou L, Herzik K, Fang N, Abdo C, Tomaszewski DM. The impact of the pharmacist on continuity of care during transitions of care: A systematic review. J Am Pharm Assoc (2003). Jan-Feb 2020;60(1):163–177 e2. doi: 10.1016/j.japh.2019.06.020 [DOI] [PubMed] [Google Scholar]
- 9.Rodrigues CR, Harrington AR, Murdock N, et al. Effect of Pharmacy-Supported Transition-of-Care Interventions on 30-Day Readmissions: A Systematic Review and Meta-analysis. Ann Pharmacother. Oct 2017;51(10):866–889. doi: 10.1177/1060028017712725 [DOI] [PubMed] [Google Scholar]
- 10.Slazak E, Cardinal C, Will S, Clark CM, Daly CJ, Jacobs DM. Pharmacist-led transitions-of-care services in primary care settings: Opportunities, experiences, and challenges. J Am Pharm Assoc (2003). May-Jun 2020;60(3):443–449. doi: 10.1016/j.japh.2019.11.016 [DOI] [PubMed] [Google Scholar]
- 11.Duong HV, Herrera LN, Moore JX, et al. National Characteristics of Emergency Medical Services Responses for Older Adults in the United States. Prehosp Emerg Care. Jan-Feb 2018;22(1):7–14. doi: 10.1080/10903127.2017.1347223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bazargan M, Smith JL, Cobb S, et al. Emergency Department Utilization among Underserved African American Older Adults in South Los Angeles. Int J Environ Res Public Health. Apr 2 2019;16(7)doi: 10.3390/ijerph16071175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farmer BM, Hayes BD, Rao R, Farrell N, Nelson L. The Role of Clinical Pharmacists in the Emergency Department. J Med Toxicol. Mar 2018;14(1):114–116. doi: 10.1007/s13181-017-0634-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hohner E, Ortmann M, Murtaza U, et al. Implementation of an emergency department-based clinical pharmacist transitions-of-care program. Am J Health Syst Pharm. Aug 1 2016;73(15):1180–7. doi: 10.2146/ajhp150511 [DOI] [PubMed] [Google Scholar]
- 15.Pearson SM, Tandon A, Fixen DR, et al. Pharmacist-Led Transition of Care Pilot Targeting Older People After Emergency Department Discharge. Sr Care Pharm. Jun 1 2020;35(6):273–282. doi: 10.4140/TCP.n.2020.273 [DOI] [PubMed] [Google Scholar]
- 16.Butcher NJ, Monsour A, Mew EJ, et al. Guidelines for Reporting Outcomes in Trial Reports: The CONSORT-Outcomes 2022 Extension. JAMA. Dec 13 2022;328(22):2252–2264. doi: 10.1001/jama.2022.21022 [DOI] [PubMed] [Google Scholar]
- 17.Ibrahim IA, Kang E, Dansky KH. Polypharmacy and possible drug-drug interactions among diabetic patients receiving home health care services. Home Health Care Serv Q. 2005;24(1–2):87–99. doi: 10.1300/J027v24n01_07 [DOI] [PubMed] [Google Scholar]
- 18.Bauer S, Nauck MA. Polypharmacy in people with Type 1 and Type 2 diabetes is justified by current guidelines--a comprehensive assessment of drug prescriptions in patients needing inpatient treatment for diabetes-associated problems. Diabet Med. Sep 2014;31(9):1078–85. doi: 10.1111/dme.12497 [DOI] [PubMed] [Google Scholar]
- 19.Sanchez GM, Douglass MA, Mancuso MA. Revisiting Project Re-Engineered Discharge (RED): The Impact of a Pharmacist Telephone Intervention on Hospital Readmission Rates. Pharmacotherapy. Sep 2015;35(9):805–12. doi: 10.1002/phar.1630 [DOI] [PubMed] [Google Scholar]
- 20.Budiman T, Snodgrass K, Komatsu Chang A. Evaluation of Pharmacist Medication Education and Post-discharge Follow-up in Reducing Readmissions in Patients With ST-Segment Elevation Myocardial Infarction (STEMI). Ann Pharmacother. Feb 2016;50(2):118–24. doi: 10.1177/1060028015620425 [DOI] [PubMed] [Google Scholar]
- 21.Tedesco GW, McConaha JL, Skomo ML, Higginbotham SK. A Pharmacist’s Impact on 30-Day Readmission Rates When Compared to the Current Standard of Care Within a Patient-Centered Medical Home: A Pilot Study. J Pharm Pract. Aug 2016;29(4):368–73. doi: 10.1177/0897190014568671 [DOI] [PubMed] [Google Scholar]
- 22.Caglar S, Henneman PL, Blank FS, Smithline HA, Henneman EA. Emergency department medication lists are not accurate. J Emerg Med. Jun 2011;40(6):613–6. doi: 10.1016/j.jemermed.2008.02.060 [DOI] [PubMed] [Google Scholar]
- 23.Nymoen LD, Flatebo TE, Moger TA, Oie E, Molden E, Viktil KK. Impact of systematic medication review in emergency department on patients’ post-discharge outcomes-A randomized controlled clinical trial. PLoS One. 2022;17(9):e0274907. doi: 10.1371/journal.pone.0274907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harrison PL, Hara PA, Pope JE, Young MC, Rula EY. The impact of postdischarge telephonic follow-up on hospital readmissions. Popul Health Manag. Feb 2011;14(1):27–32. doi: 10.1089/pop.2009.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shuen JA, Wilson MP, Kreshak A, et al. Telephoned, Texted, or Typed Out: A Randomized Trial of Physician-Patient Communication After Emergency Department Discharge. J Emerg Med. Oct 2018;55(4):573–581. doi: 10.1016/j.jemermed.2018.07.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pharmacists. U.S. Bureau of Labor Statistics. Available at: https://www.bls.gov/ooh/healthcare/pharmacists.htm. Accessed on March 20, 2023. [Google Scholar]
- 27.Lussier ME, Evans HJ, Wright EA, Gionfriddo MR. The impact of community pharmacist involvement on transitions of care: A systematic review and meta-analysis. J Am Pharm Assoc (2003). Jan-Feb 2020;60(1):153–162 e5. doi: 10.1016/j.japh.2019.07.002 [DOI] [PubMed] [Google Scholar]
- 28.Melody KT, McCartney E, Sen S, Duenas G. Optimizing care transitions: the role of the community pharmacist. Integr Pharm Res Pract. 2016;5:43–51. doi: 10.2147/IPRP.S87947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Birtwell K, Planner C, Hodkinson A, et al. Transitional Care Interventions for Older Residents of Long-term Care Facilities: A Systematic Review and Meta-analysis. JAMA Netw Open. May 2 2022;5(5):e2210192. doi: 10.1001/jamanetworkopen.2022.10192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taber DJ, Pilch NA, McGillicuddy JW, Mardis C, Treiber F, Fleming JN. Using informatics and mobile health to improve medication safety monitoring in kidney transplant recipients. Am J Health Syst Pharm. Jul 18 2019;76(15):1143–1149. doi: 10.1093/ajhp/zxz115 [DOI] [PubMed] [Google Scholar]
- 31.Fleming JN, Treiber F, McGillicuddy J, Gebregziabher M, Taber DJ. Improving Transplant Medication Safety Through a Pharmacist-Empowered, Patient-Centered, mHealth-Based Intervention: TRANSAFE Rx Study Protocol. JMIR Res Protoc. Mar 2 2018;7(3):e59. doi: 10.2196/resprot.9078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gonzales HM, Fleming JN, Gebregziabher M, et al. Pharmacist-Led Mobile Health Intervention and Transplant Medication Safety: A Randomized Controlled Clinical Trial. Clin J Am Soc Nephrol. May 8 2021;16(5):776–784. doi: 10.2215/cjn.15911020 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.