Abstract
Objective:
This study aimed to examine variability in condom use trends by sexual risk behavior among US high school students.
Methods:
Data were from the 2003–2015 national Youth Risk Behavior Surveys conducted biennially among a nationally representative sample of students in grades 9 to 12. We used logistic regression to examine variability in trends of condom use during last sexual intercourse among female and male students by 4 sexual risk behaviors: drank alcohol or used drugs before last sexual intercourse, first sexual intercourse before age 13 years, 4 or more sex partners during their life, and 2 or more sex partners during the past 3 months.
Results:
Between 2003 and 2015, significant declines in self-reported condom use were observed among black female (63.6% in 2003 to 46.7% in 2015) and white male students (69.0% in 2003 to 58.1% in 2015). Among female students, declines in self-reported condom use were significant only among those who drank or use drugs before last sexual intercourse, had 4 or more sex partners during their life, or had 2 or more sex partners during the past 3 months. There was a significant interaction between trends in condom use and first sexual intercourse before age 13 years, suggesting more pronounced declines among female students who initiated first sexual intercourse before age 13 years compared with their female peers. Trends did not vary by sexual risk behavior for male students.
Conclusions:
Results suggest that declines in self-reported condom use have occurred among female students at greater risk for acquiring a sexually transmitted disease.
Consistent and correct condom use is an important sexually transmitted disease (STD) prevention strategy for sexually active adolescents.1–5 Both the American Academy of Pediatrics and the Centers for Disease Control and Prevention (CDC) recommend counseling adolescents on evidence-based STD prevention strategies including consistent and correct condom use.6,7 During adolescence, sexual relationships may be more transient and STD testing combined with mutual monogamy may not always be a feasible option.5 Although other contraceptive options are more effective for pregnancy prevention, condoms are the only available method for sexually active adolescents that offers protection against both unintended pregnancy and STDs.8 Trend data from the national Youth Risk Behavior Survey (YRBS) show that condom use during last sexual intercourse increased from 46.2% in 1991 to 56.9% in 2015 among sexually active high school students. However, from 2003 to 2015, condom use declined from 63.0% to 56.9%.9
Research is needed to better understand recent declines in self-reported condom use among adolescents, particularly because these declines may be occurring among youth at disproportionate risk for STD. Prior analyses of factors associated with condom use provide a useful starting point. Findings from the 2015 YRBS show that male students were more likely than female students to use condoms during last sexual intercourse with significant variation by both grade and race/ethnicity, with the highest prevalence among black male students and lowest among black or Hispanic female students.9 Analyses by grade suggested that self-reported condom use at last sex was significantly higher among students in 9th and 10th than students in 12th grade.
Furthermore, results from a longitudinal study of students at risk for high school dropout linked decreased condom use with increased frequency of sex and substance use, and increased condom use with increased number of sex partners.10,11 Other studies have found that earlier sexual initiation is associated with a decreased likelihood of condom use.12 Taken together, these findings suggest that other sexual risk behaviors, including sexual initiation, number of partners, and substance use, may be important to consider when interpreting declines in self-reported condom use during last sexual intercourse. Declines in self-reported condom use are particularly concerning if they are occurring predominately among young people engaging in other behaviors that increase risk for STDs.
No published literature has considered variability in condom use trends by sexual risk behaviors among adolescents. This study analyzed data from the national YRBS to examine whether declines in self-reported condom use between 2003 and 2015 varied as a function of 4 sexual risk behaviors, including whether students drank alcohol or used drugs before last sexual intercourse, had 4 or more sex partners during their life, had 2 or more sex partners during the past 3 months, or had first sexual intercourse before age 13 years. We hypothesize that declines in self-reported condom use will be more pronounced among students engaging in other sexual risk behaviors that increase STD risk. These results could help inform implementation of interventions to reduce the transmission of STDs, as well as identify groups disproportionately impacted by declining condom use for intervention.
METHODS
Study Design
Since 1991, the national YRBS has been conducted biennially as part of the Youth Risk Behavior Surveillance System developed by CDC. These surveys collect cross-sectional data from independently selected nationally representative samples of public and private school students in grades 9 to 12. Each national YRBS uses a similar 3-stage probability sampling methodology.13 Weighting factors are applied to each student’s record to adjust for varying probabilities of selection at each stage of sampling, student nonresponse, and the oversampling of black and Hispanic students. Questionnaires contain approximately 98 items and are administered in the classroom during a regular class period by trained data collectors. Responses are recorded directly on computer-scannable questionnaire booklets or answer sheets. Student participation in the survey is anonymous and voluntary, and local procedures are used to obtain parental permission. The national YRBS has been reviewed and approved by an institutional review board at the CDC. This study analyzes national YRBS data collected from 2003 to 2015. Overall response rates ranged from 60% in 2015 to 71% in 2009 and 2011.
Measures
The analytic sample was restricted to currently sexually active students (i.e., students who had sexual intercourse during the past 3 months; n = 33,940), assessed with the question: “During the past 3 months, with how many people did you have sexual intercourse?” Response options were as follows: I have never had sexual intercourse; I have had sexual intercourse, but not during the past 3 months; 1 person; 2 people; 3 people; 4 people; 5 people; and 6 or more people. The outcome measure, condom use during last sexual intercourse, was assessed with the question: “The last time you had sexual intercourse, did you or your partner use a condom?” Response options were as follows: “I have never had sexual intercourse,” “yes,” and “no.” We created a dichotomous variable (yes vs. no) that excluded nonsexually experienced adolescents.
Four sexual risk behaviors were examined as potential moderators of declines in self-reported condom use. All study variables were dichotomized to be consistent with the standard reporting of YRBS data.9 Alcohol or drug use before last sexual intercourse was assessed with the question: “Did you drink alcohol or use drugs before you had sexual intercourse the last time?” A dichotomous (yes vs. no) variable was created. Number of lifetime sex partners was assessed with the question: “During your life, with how many people have you had sexual intercourse?” Response options were as follows: I have never had sexual intercourse, 1 person, 2 people, 3 people, 4 people, 5 people, and 6 or more people. Number of recent sex partners was assessed with the same response options; students were asked about number of sex partners during the prior 3 months. We created one variable for 4 or more sex partners during their life (≥4 people vs. <4 people) and another variable for 2 or more recent sex partners (≥2 people vs. 1 people). First sexual intercourse before the age of 13 years was assessed with the question: “How old were you when you had sexual intercourse for the first time?” Response options were as follows: I have never had sexual intercourse, 11 years or younger, 12 years old, 13 years old, 14 years old, 15 years old, 16 years old, and 17 years or older. Age of first sexual intercourse was dichotomized to create an indicator for early sexual initiation (first sexual intercourse before age 13 years vs. ≥13 years).
Demographics included race/ethnicity, sex, and grade. Race/ethnicity was a nominal variable with 4 categories: black non-Hispanic, white non-Hispanic, Hispanic, or other. Sex was assessed with the question: “What is your sex?” with the options “female” or “male.” Grade of enrollment was assessed with the question: “In what grade are you?” with the options “9th grade,” “10th grade,”“11th grade,”“12th grade,” or “ungraded or other grade.”
Data Analysis
Because the YRBS continuously used the same recruitment and sampling procedures, we were able to combine multiple year’s data into one analytic data set. Data from 7 surveys, conducted from 2003 to 2015, were analyzed using SUDAAN release 11.0.0 (Research Triangle Institute, Research Triangle Park, NC). All analyses were stratified by sex because of large differences in the prevalence of condom use among female and male students. First, using logistic regression with self-reported condom use at last sex as the dependent variable, we tested racial/ethnic and grade differences by examining interactions between linear contrast for survey year and race/ethnicity or grade. We used a similar approach for testing for variation in linear trends in self-reported condom use by self-reported drinking alcohol or using drugs before last sexual intercourse, having 4 or more sex partners during their life, having 2 or more recent sex partners, and having first sexual intercourse before age 13 years, controlling for race/ethnicity and grade. We controlled for race/ethnicity and grade because of the co-occurrence of racial/ethnic and grade differences between self-reported condom use and other sexual risk behaviors. For significant interactions, we stratified analyses by sexual risk behavior. Prevalence estimates with 95% confidence intervals were calculated using Taylor series linearization. Logistic regression t tests for linear trend β’s and Wald F statistics for interaction terms were considered statistically significant if P < 0.05. Cases with missing data were removed from the analysis (i.e., listwise deletion).
RESULTS
Sample Characteristics for Currently Sexually Active High School Students
Table 1 contains sample characteristics and prevalence of risk behaviors. The percentage of currently sexually active students ranges from a high of 35.0% in 2007 to 30.1% in 2015. The percentage of black non-Hispanic students ranges from a high of 19.9% in 2007 to a low of 13.9% in 2015. The percentage of Hispanic students ranges from a high of 22.2% in 2015 to a low of 15.7 in 2005.
TABLE 1.
Point Prevalence for Demographic Characteristics and Sexual Risk Behaviors Among Currently Sexually Active Students*
| Year of Survey |
|||||||
|---|---|---|---|---|---|---|---|
| 2003 | 2005 | 2007 | 2009 | 2011 | 2013 | 2015 | |
|
| |||||||
| Sample size (n) after restricting to currently sexually active | 5218 | 4720 | 5066 | 5575 | 5158 | 4667 | 4304 |
| Sex | |||||||
| Male, % | 50.0 | 49.1 | 49.1 | 49.6 | 50.3 | 47.4 | 51.1 |
| Female, % | 50.0 | 50.9 | 51.0 | 50.5 | 49.7 | 52.7 | 48.9 |
| Race/ethnicity† | |||||||
| Black non-Hispanic, % | 18.4 | 18.0 | 19.9 | 18.0 | 16.5 | 17.0 | 13.9 |
| Hispanic, % | 18.6 | 15.7 | 17.7 | 18.9 | 19.3 | 21.2 | 22.2 |
| White non-Hispanic, % | 55.3 | 60.3 | 57.2 | 56.4 | 55.6 | 54.8 | 55.7 |
| Grade | |||||||
| 9th, % | 17.9 | 18.7 | 16.6 | 17.4 | 17.5 | 15.6 | 14.1 |
| 10th, % | 23.7 | 22.4 | 23.2 | 22.4 | 22.8 | 22.4 | 21.9 |
| 11th, % | 28.1 | 27.3 | 28.2 | 27.9 | 27.7 | 28.3 | 28.4 |
| 12th, % | 30.3 | 31.6 | 32.0 | 32.3 | 32.1 | 33.8 | 35.7 |
| Drank alcohol or used drugs during last sexual intercourse, % | 25.4 | 23.3 | 22.5 | 21.6 | 22.1 | 22.4 | 20.6 |
| 4 or more sex partners during their life, % | 37.8 | 37.2 | 38.2 | 36.4 | 40.1 | 39.4 | 33.6 |
| 2 or more sex partners during the last 3 months, % | 27.4 | 26.8 | 27.7 | 28.5 | 29.3 | 26.2 | 23.1 |
| Had first sexual intercourse before age 13 years, % | 15.5 | 12.9 | 14.0 | 12.6 | 13.3 | 11.9 | 9.3 |
Had sexual intercourse with at least one person during the 3 months before the survey.
Although racial/ethnic groups other than non-Hispanic black (“black”), non-Hispanic white (“white”), and Hispanic students (who might be of any race) were included in all analyses, their data were not presented because their sample size was insufficient for meaningful interpretation.
Prevalence and Trends in Condom Use
Overall, significant declines were observed in condom use during last sexual intercourse for sexually active female and male students between 2003 and 2015 (Table 2). Condom use during last sexual intercourse declined from 57.4% in 2003 to 52.0% in 2015 among female students (P = 0.01). Condom use during last sexual intercourse declined from 68.8% in 2003 to 61.5% in 2015 among male students (P = 0.001). However, variability in trends in condom use during last sexual intercourse was observed by race/ethnicity and by grade for both female and male students (Table 2). For female students, significant declines in self-reported condom use occurred only among black students (63.6% in 2003 to 46.7% in 2015; P < 0.01) and students in 9th (66.1% in 2003 to 56.7% in 2015; P < 0.01) and 10th grades (66.4% in 2003 to 54.0% in 2015; P = 0.02). For male students, significant declines in self-reported condom use occurred among white students (69.0% in 2003 to 58.1% in 2015; P < 0.01) and students in 9th (71.2% in 2003 to 63.3% in 2015; P = 0.03) and 12th grades (67.0% in 2003 to 57.4% in 2015; P = 0.01).
TABLE 2.
Point Prevalence for Condom Use During Last Sexual Intercourse Among Students Who Had Sexual Intercourse During the Past 3 Months by Sex, Race/Ethnicity, and Grade, 2003–2015 National YRBS
| Year of Survey |
Linear Trend P Value | |||||||
|---|---|---|---|---|---|---|---|---|
| 2003 | 2005 | 2007 | 2009 | 2011 | 2013 | 2015 | ||
|
| ||||||||
| Female students (n = 17,170) | ||||||||
| Overall | 57.4 (54.3–60.4) | 55.9(53.1–58.7) | 54.9 (51.8–58.0) | 53.9 (51.4–56.4) | 53.6 (50.7–56.4) | 53.1 (49.6–56.7) | 52.0 (49.0–55.1) | 0.01 |
| Black | 63.6 (58.2–68.6) | 62.1 (55.9–68.0) | 60.1 (53.7–66.2) | 51.8 (47.6–55.9) | 53.8 (47.2–60.2) | 55.3 (49.2–61.2) | 46.7 (38.9–54.6) | 0.00 |
| Hispanic | 52.3 (43.9–60.5) | 49.8(45.5–54.1) | 52.1 (45.5–58.7) | 48.0 (43.8–52.3) | 53.0 (48.6–57.3) | 50.7 (45.8–55.6) | 48.3 (41.6–55.1) | 0.79 |
| White | 56.5 (52.8–60.2) | 55.6(52.3–58.8) | 53.9 (48.8–59.0) | 56.1 (52.3–59.9) | 53.4 (49.3–57.4) | 53.2 (48.1–58.2) | 55.9 (51.3–60.3) | 0.57 |
| 9th grade | 66.1 (56.3–74.7) | 71.5 (65.4–76.9) | 61.0 (54.3–67.3) | 57.7 (51.2–63.9) | 56.3 (49.4–63.0) | 56.5 (47.7–65.0) | 56.7 (49.5–63.7) | 0.00 |
| 10 th grade | 66.4 (59.6–72.5) | 57.2 (52.0–62.2) | 59.5 (52.8–65.9) | 63.5 (58.4–68.2) | 56.7 (50.2–63.0) | 55.5 (47.7–63.0) | 54.0 (47.2–60.7) | 0.02 |
| 11th grade | 55.5 (49.9–60.9) | 57.8 (52.1–63.2) | 55.1 (50.2–60.0) | 54.0 (50.2–57.8) | 55.5 (51.9–59.0) | 54.8 (49.9–59.5) | 52.9 (46.9–58.9) | 0.31 |
| 12th grade | 48.5 (43.5–53.4) | 46.1 (42.2–49.9) | 49.9 (45.0–54.8) | 46.3 (41.2–51.4) | 48.9 (44.8–52.9) | 48.4 (44.8–52.1) | 48.8 (44.1–53.5) | 0.59 |
| Male students (n = 16,655) | ||||||||
| Overall | 68.8 (66.1–71.3) | 70.0 (66.8–72.9) | 68.5 (65.5–71.4) | 68.6 (66.0–71.1) | 67.0 (63.5–70.2) | 65.8 (62.5–69.0) | 61.5 (57.6–65.3) | 0.00 |
| Black | 81.2 (77.1–84.7) | 75.5 (70.8–79.6) | 74.0 (69.9–77.7) | 72.5 (65.7–78.4) | 75.4 (70.1–80.0) | 73.0 (66.6–78.6) | 73.6 (63.9–81.5) | 0.11 |
| Hispanic | 62.5 (57.7–67.2) | 65.3 (57.7–73.2) | 69.9 (65.4–74.0) | 61.7 (57.8–65.5) | 63.4 (57.0–69.4) | 66.5 (61.0–71.6) | 62.5 (57.3–67.5) | 0.87 |
| White | 69.0 (65.1–72.7) | 70.1 (66.3–73.8) | 66.4 (62.2–70.3) | 71.0 (67.6–74.3) | 66.3 (61.3–71.0) | 61.8 (57.2–66.3) | 58.1 (52.9–63.2) | 0.00 |
| 9th grade | 71.2 (62.7–78.5) | 77.1 (69.9–82.9) | 75.8 (69.0–81.5) | 69.9 (63.9–75.4) | 67.0 (60.2–73.1) | 69.5 (63.0–75.3) | 63.3 (55.0–70.9) | 0.03 |
| 10th grade | 71.8 (66.1–76.9) | 74.4 (67.9–80.0) | 73.2 (67.8–78.1) | 71.9 (66.6–76.6) | 69.9 (64.3–75.0) | 69.3 (60.9–76.6) | 65.6 (58.0–72.5) | 0.07 |
| 11th grade | 66.7 (59.7–73.0) | 66.0(60.0–71.5) | 69.3 (63.1–74.8) | 68.9 (64.3–73.1) | 67.0 (63.1–70.6) | 70.6 (65.1–75.5) | 62.5 (56.1–68.5) | 0.74 |
| 12 th grade | 67.0 (61.9–71.7) | 65.8(60.2–71.0) | 59.6 (55.3–63.8) | 65.0 (61.1–68.8) | 64.7 (58.1–70.8) | 58.1 (53.0–62.9) | 57.4 (51.8–62.8) | 0.01 |
Linear trend P values reflect adjustment for demographic characteristics (race/ethnicity, and grade).
Effect Modification by Sexual Risk Behaviors
Among female students, interaction analyses suggested that trends in self-reported condom use varied significantly depending on other sexual risk behaviors, including drank alcohol or used drugs before last sexual intercourse (Wald F = 6.4, P = 0.01), had 4 or more sex partners during their life (Wald F = 8.2, P < 0.01), had 2 or more sex partners during the past 3 months (Wald F = 4.7, P = 0.03), or had their first sexual intercourse before age 13 years (Wald F = 4.6, P = 0.03; data not shown). Among male students, trends in condom use during last sexual intercourse did not significantly vary by involvement in other sexual risk behaviors.
Table 2 presents condom use trends for female students, stratified by other sexual risk behaviors. Across 3 risk behaviors (drank alcohol or used drugs before last sexual intercourse, 4 or more sex partners during their life, and 2 or more sex partners during the past 3 months), condom use decreased significantly only among female students who engaged in the risk behavior. Condom use decreased significantly for female students regardless of early sexual initiation, but the decreases were more pronounced among those who initiated sexual activity before the age 13 years compared with those who did not initiate sex before age 13 years. These findings are presented graphically in Figure 1.
Figure 1.
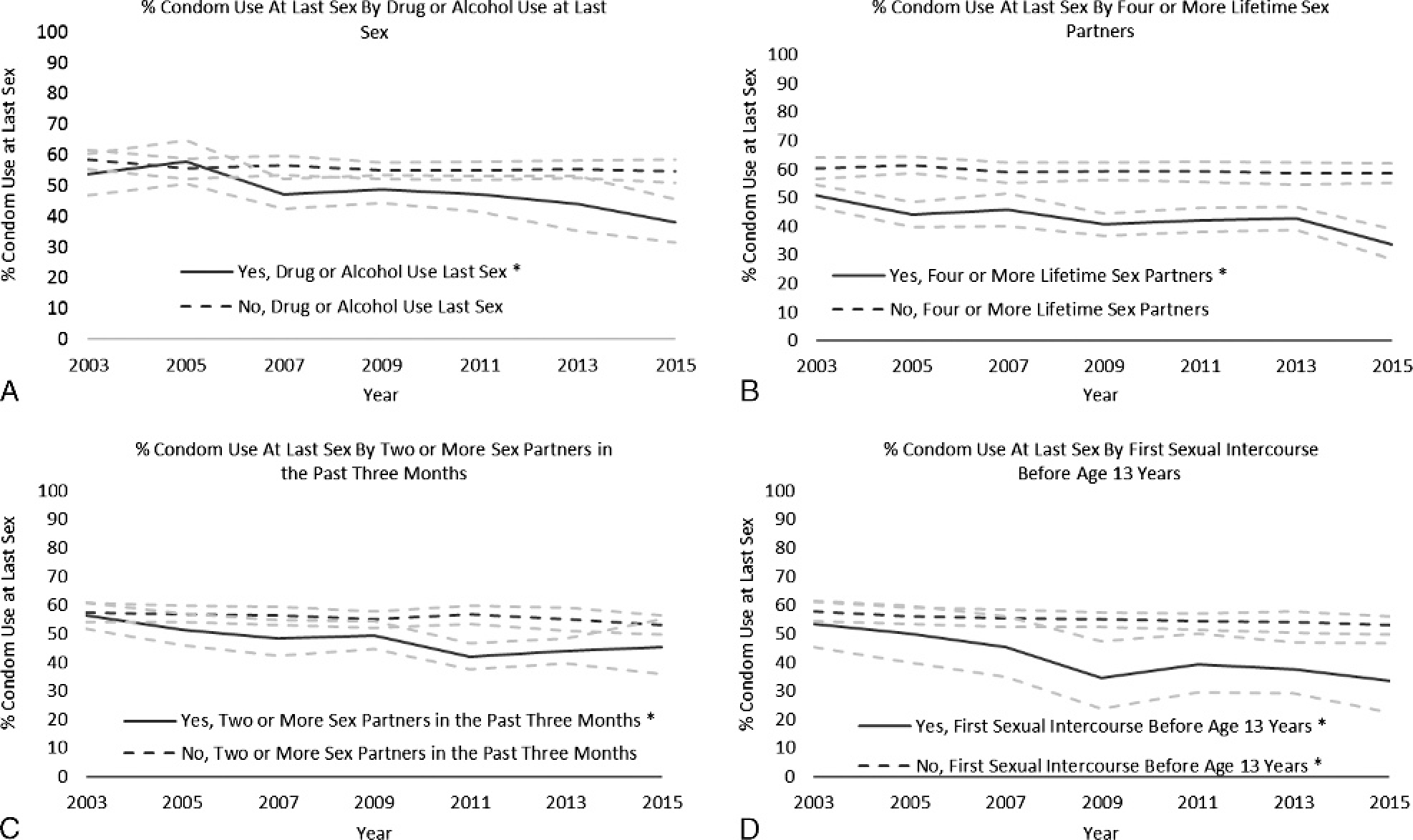
Plots for trends in self-reported condom use during last sexual intercourse among female students, with findings stratified by drank alcohol or used drugs before last sexual intercourse (A), 4 or more sex partners during their life (B), 2 or more sex partners during the past 3 months (C), and first sexual intercourse before age 13 years (D). Trends significant at P < 0.05 are indicated with an asterisk. Ninety-five percent confidence bands are in gray.
DISCUSSION
This study uses nationally representative data to describe recent trends in self-reported condom use among sexually active female and male high school students. We sought to examine whether declines varied by sexual risk behavior, with important variations identified for female students but not male students. Specifically, we found that declines in self-reported condom use have disproportionately occurred among female students whose other sexual behaviors place them at increased risk for STD. We also found substantial differences by race/ethnicity and grade, independent of variation by sexual risk behavior.
Overall, condom use declined significantly among both female and male students from 2003 to 2015. These declines are in contrast to data suggesting increases in condom use during the past 2 decades, which may be explained by increases from 1991 to 2003.9 It is unclear what accounts for more recent declines, yet there are several potential explanations. Findings from the School Health Policies and Practices Study suggest that there is decreasing emphasis on teaching STD prevention, with the percentage of schools in which students are required to receive instruction on STD prevention declining from 48.6% in 2000 to 38.2% in 2014.14 In addition, increases in the uptake of more effective contraceptive methods—which has been shown to be increasing among high school students nationally—may contribute to declines in self-reported condom use.9,15,16 Finally, there may be changes in sociocultural influences and norms regarding sexual behavior (e.g., condom use–related stigma) that may be contributing to declining condom use.17
One important finding was that declining condom use among female students primarily occurred among young women engaging in other sexual risk behaviors, suggesting that these adolescents are especially at risk for STDs. Significant declines were only observed among female students who drank alcohol or used drugs before last sexual intercourse, had 4 or more sex partners during their life, or had 2 or more sex partners during the past 3 months. No statistically significant declines were found among female students who did not engage in these behaviors. Although declines were observed regardless of age of sexual initiation, they were more pronounced among female students who initiated sexual activity before age 13 years compared with their female peers who initiated later. This effect modification by sexual risk behavior suggests that the declines in self-reported condom use observed among female students in the national YRBS may be primarily explained by changes in the condom use of females engaging in the other 4 risk behavior examined. These findings are not entirely surprising given existing theory and empirical evidence indicating that adolescent risk behaviors tend to co-occur because of shared social determinants and risk factors.18,19 However, the co-occurrence of risk behaviors documented in this study is particularly important given that declines in self-reported condom use occurring primarily among young females engaging in other sexual risk behaviors potentially contribute to increasing STD rates.
We did not observe variations in condom use decline by other sexual risk behaviors among male students. Rather, condom use declined regardless of risk behavior. It remains unclear what accounts for the fact that significant effects of sexual risk behavior on trends in condom use were observed for female but not male students. One potential explanation is that there are underlying sex differences in the interpersonal processes and motivations that underpin adolescent condom use. Past research has found sex differences in adolescent relationships and condom use in adolescent sexual relationships.20–22 The YRBS does not collect information on relationship type or sex partner characteristics; the influence of these factors as well as other potential explanations for differences by biological sex should be explored in future research on condom use trends.
In addition, variations in trends by race/ethnicity and grade emerged from our analyses. This variation by race/ethnicity suggests that the overall decline may be explained by decline among black female students and white male students. These racial/ethnic differences may reflect sociocultural differences in the correlates of adolescent sexual risk behavior and condom use.23 Similarly, the findings of variability by grade may suggest that the overall decline is explained by decline among students in 9th and 10th grades for female students and 9th and 12th grades for male students. These results suggest that just focusing on overall trends may overlook differences by sex, grade, and race/ethnicity which carry important programmatic implications.
This study has several limitations. These data are based solely on self-report, the validity of which may be influenced by social desirability biases or other response errors; in particular, some studies using biological outcomes have suggested that self-reported condom use may not accurately reflect condom use. However, systematic reviews have supported the validity of self-reported risk behaviors.24 In addition, the YRBS has shown good test–retest reliability in psychometric studies.13 That said, the potential limitations of self-reported data should be considered when interpreting the findings. For example, observed declines may reflect changes in factors that influence the self-reporting of condom use (e.g., stigma); however, we do not have evidence to suggest this is likely. Although the data are nationally representative, findings from the YRBS are only generalizable to students enrolled in US high schools. However, according to a 2012 report, only 3% of adolescent aged 16 to 17 years were not currently enrolled in a high school program or had completed high school.25
Public Health Implications
This study not only extends what is known about recent declines in self-reported condom use among adolescents but also points to the need for future research to explain underlying drivers, variation by sexual risk behavior among female students, and differential effects by sex. Longitudinal data that explore developmental trajectories in condom use could be particularly useful. Qualitative studies to better understand motivations, barriers, and facilitators to using condoms among male and female students from racially diverse groups could also provide insight into declines in self-reported condom use. Such research could help identify strategies for strengthening sexual risk reduction programs, ensuring maximum reach and effectiveness for all adolescents, including those at highest risk.
These results demonstrate that public health and clinical efforts to increase condom use among young people are warranted. Many sexual risk reduction interventions have been found to increase condom use, and these can be implemented in a variety of settings including schools, community-based organizations, and clinics.6 Evidence also exists that provider counseling is associated with increased condom use, which suggests that an additional avenue for increasing condom use may be to improve adolescents’ access to quality sexual health and reproductive health services.26 Increasing access to care also provides an opportunity for providers to promote STD prevention strategies for sexually active adolescents in addition to condom use, such as STD/HIV testing and human papillomavirus vaccination.7 Given that adolescent receipt of preventive counseling during adolescent well-visits is low, provider training to ensure adherence to existing guidelines may be important.27,28 Ultimately, a combination of individual- and systems-level approaches will be needed to increase condom use among sexually active adolescents.
Footnotes
Conflict of Interest and Sources of Funding: None declared.
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC). Condoms and STDs: Fact Sheet for Public Health Personnel. Available at: http://www.cdc.gov/condomeffectiveness/latex.htm.
- 2.Weller SC, Davis-Beaty K. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev 2002; (1):CD003255. [DOI] [PubMed] [Google Scholar]
- 3.Winer RL, Hughes JP, Feng Q, et al. Condom use and the risk of genital human papillomavirus infection in young women. N Engl J Med 2006; 354:2645–2654. [DOI] [PubMed] [Google Scholar]
- 4.Crosby RA, DiClemente RJ, Wingood GM, et al. Value of consistent condom use: A study of sexually transmitted disease prevention among African American adolescent females. Am J Public Health 2003; 93:901–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matson PA, Adler NE, Millstein SG, et al. Developmental changes in condom use among urban adolescent females: Influence of partner context. J Adolesc Health 2011; 30;48:386–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Brien RF, Warner L, Blythe MJ, et al. Condom use by adolescents. Pediatrics 2013; 132:973–981. [DOI] [PubMed] [Google Scholar]
- 7.Workowski K, Bolan G. Sexually transmitted diseases treatment guidelines, 2015. MMWR Reccomm Rep 2015; 64:1–138. [PMC free article] [PubMed] [Google Scholar]
- 8.Kost K, Singh S, Vaughan B, et al. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception 2008; 77:10–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kann L Youth risk behavior surveillance—United States, 2015. MMWR Surveill Summ 2016; 65:1–174. [DOI] [PubMed] [Google Scholar]
- 10.Elkington KS, Bauermeister JA, Zimmerman MA. Psychological distress, substance use, and HIV/STI risk behaviors among youth. J Youth Adolesc 2010; 39:514–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bauermeister JA, Zimmerman MA, Caldwell CH. Neighborhood disadvantage and changes in condom use among African American adolescents. J Urban Health 2011; 88:66–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lowry R, Dunville R, Robin L. Early sexual debut and associated risk behaviors among sexual minority youth. Am J Prev Med 2016. In press. [DOI] [PubMed] [Google Scholar]
- 13.Brener ND, Kann L, Shanklin S, et al. Methodology of the Youth Risk Behavior Surveillance System—2013. MMWR Recomm Rep 2013; 62:1–20. [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Fact Sheet: School Health Policies and Practices Study, Trends Over Time: 2000–2014. Available at: https://www.cdc.gov/healthyyouth/data/shpps/pdf/2014factsheets/trends_shpps2014.pdf.
- 15.Sayegh MA, Fortenberry JD, Shew M, et al. The developmental association of relationship quality, hormonal contraceptive choice and condom non-use among adolescent women. J Adolesc Health 2006; 39:388–395. [DOI] [PubMed] [Google Scholar]
- 16.Goldstein RL, Upadhyay UD, Raine TR. With pills, patches, rings, and shots: who still uses condoms? A longitudinal cohort study. J Adolesc Health 2013; 52:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarkar NN. Barriers to condom use. Eur J Contracept Reprod Health Care 2008; 13:114–122. [DOI] [PubMed] [Google Scholar]
- 18.Jessor R Risk behavior in adolescence: A psychosocial framework for understanding and action. J Adolesc Health 1991; 12:597–605. [DOI] [PubMed] [Google Scholar]
- 19.Jessor R Problem Behavior Theory: A half century of research on adolescent behavior and development. In: Lerner RM, Peterson AC, Sibereisen RK, eds. The Developmental Science of Adolescence: History Through Autobiography. New York: Psychology Press, 2014. [Google Scholar]
- 20.Lescano CM, Vazquez EA, Brown LK, et al. Condom use with “casual” and “main” partners: What’s in a name? J Adolesc Health 2006; 39:443. e1–443.e7. [DOI] [PubMed] [Google Scholar]
- 21.Gebhardt WA, Kuyper L, Greunsven G. Need for intimacy in relationships and motives for sex as determinants of adolescent condom use. J Adolesc Health 2003; 33:154–164. [DOI] [PubMed] [Google Scholar]
- 22.Tschann JM, Adler NE, Millstein SG, et al. Relative power between sexual partners and condom use among adolescents. J Adolesc Health 2002; 31:17–25. [DOI] [PubMed] [Google Scholar]
- 23.Zimmer-Gembeck MJ, Helfand M. Ten years of longitudinal research on US adolescent sexual behavior: Developmental correlates of sexual intercourse, and the importance of age, gender and ethnic background. Dev Rev 2008; 28:153–224. [Google Scholar]
- 24.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. J Adolesc Health 2003; 33:436–457. [DOI] [PubMed] [Google Scholar]
- 25.Stark P, Noel AM. Trends in High School Dropout and Completion Rates in the United States: 1972–2012 (NCES 2015–015). US Department of Education. Washington, DC: National Center for Education Statistics, 2015. Available at: http://nces.ed.gov/pubs2015/2015015.pdf. Accessed on March 3, 2016. [Google Scholar]
- 26.Morroni C, Heartwell S, Edwards S, et al. The impact of oral contraceptive initiation on young women’s condom use in 3 American cities: missed opportunities for intervention. PLoS One 2014; 9:e101804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peddecord KM, Wang W, Wang L, et al. Adolescents’ self-reported recall of anticipatory guidance provided during well-visits at nine medical clinics in San Diego, California, 2009–2011. J Adolesc Health 2016; 58:267–275. [DOI] [PubMed] [Google Scholar]
- 28.American Academy of Pediatrics. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. Elk Grove Village, IL: American Academy of Pediatrics, 2008. [Google Scholar]


