Abstract
Cardiovascular diseases (CVDs) remain the leading cause of death and disability worldwide. Digital health technologies are important public health interventions for addressing the burden of cardiovascular disease. In this article, we discuss the importance of translating digital innovations in research‐funded projects to low‐resource settings globally to advance global cardiovascular health equity. We also discuss current global cardiovascular health inequities and the digital health divide within and between countries. We present various considerations for translating digital innovations across different settings across the globe, including reciprocal innovation, a “bidirectional, co‐constituted, and iterative exchange of ideas, resources, and innovations to address shared health challenges across diverse global settings.” In this case, afferent reciprocal innovations may flow from high‐income countries toward low‐ and middle‐income countries, and efferent reciprocal innovations may be exported to high‐income countries from low‐ and middle‐income countries with adaptation. Finally, we discuss opportunities for bidirectional learning between local and global institutions and highlight examples of projects funded through the American Heart Association Health and Innovation Strategically Funded Research Network that have been adapted to lower‐resource settings or have the potential to be adapted to lower‐resource settings.
Keywords: cardiovascular disease, disparities, health equity, machine learning and artificial intelligence, translational studies
Subject Categories: Cardiovascular Disease, Machine Learning, Translational Studies, Disparities, Health Equity
Nonstandard Abbreviations and Acronyms
- ADD‐RHD
Active Case Detection and Decentralized Dynamic Registry to Improve the Uptake of Rheumatic Heart Disease Secondary Prevention
- DHI
digital health intervention
- GDMT
guideline‐directed medical therapy
- HICs
high‐income countries
- HCD
human‐centered design
- LMICs
low‐ and middle‐income countries
- RHD
rheumatic heart disease
Cardiovascular diseases (CVDs) remain the leading cause of death and disability worldwide. 1 In 2020, an estimated 523 million people had CVD; ≈32% of all global deaths were attributable to CVD. 1 , 2 The burden of CVD and barriers to its prevention and management are unequally distributed among various segments of populations within and between countries. For instance, in the United States, Black and Hispanic adults bear a disparate burden of CVD. 3 Globally, compared with high‐income countries (HICs), it is estimated that >80% of persons with CVD live in low‐ and middle‐income countries (LMICs), where more than three‐quarters of CVD deaths occur. 2
Digital health interventions (DHIs), including digital health technology, digital medicine, telemedicine, mobile health, remote monitoring, and wearable and consumer technologies, are important public health and clinical interventions for improving adherence, promoting lifestyle changes for preventing and treating CVD. 4 However, DHIs applied to cardiovascular health have a greater chance of success if equity is centered. Equity is the absence of unfair, avoidable, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, geographically, or by other dimensions of inequality. 5 DHIs can improve health care access, use, timeliness of care, and health outcomes and advance health equity by addressing barriers to care and facilitating evidence‐informed strategies such as team‐based care. 6
DHIs usher in great benefits but may expose, exacerbate, or drive inequities across multiple domains, including socioeconomic status, age, literacy, and geographic location. 7 To ensure equity in the development and use of DHIs and improvements in health and social determinants globally, particular attention must be devoted to the technology itself and aspects of design, technical development, integration of the technology into health care, and evaluation. This includes the digital health tools' relationship and interaction with various end users, including individual patients and with particular attention to historically excluded and marginalized populations globally, technology proprietors and developers, the health system, policymakers, governments, regional/international organizations and transnational organizations, and other stakeholders. 8
Global Cardiovascular Health Disparities
The burden of CVD in LMICs has dramatically increased recently due to rapid epidemiologic transitions, 9 characterized by changes in diet, tobacco use, sedentary lifestyle, and socioeconomic changes. At least three quarters of CVD deaths occur in LMICs. 9 Yet screening and surveillance systems and highly effective evidence strategies to control and prevent CVD, such as lifestyle interventions, blood pressure– and cholesterol‐lowering therapy, and novel therapeutics, have not been equally translated in LMICs. Moreover, the cardiovascular workforce needed to curb the increasing trend of CVD in LMICs is suboptimal. 10 Rapid innovations in diagnostic procedures and imaging modalities that facilitate accurate diagnosis and appropriate treatment of CVD have occurred in HICs. However, access to these innovative diagnoses and treatment procedures is not equitable across the globe, with LMICs experiencing these disparities on a larger scale. Factors driving these include disparity in broadband and Internet access across countries; despite the Internet spike experienced during the pandemic, about 2.7 million people (about a third of the work population) did not have Internet or high‐speed broadband access in 2022, 11 impacting DHI access. Gaps in digital literacy (competencies in using digital tools, processing information, and engaging with media) also present a major challenge; many education systems across the world are not equipped to teach digital skills due to lack of proper infrastructure, technological equipment, teacher training, curriculum, or learning benchmarks. 12 The digital divide, in which technology and Internet access and use patterns differ due to many of the factors mentioned above, extends beyond a divide between populations with access to the Internet or mobile devices and those without but includes overlapping divides in digital skills, digital use, quality of infrastructure, access to content, and so on. 11 Additionally, there are also gaps in translation, access, and adoption of DHIs and in conducting implementation of science‐based principles which may facilitate translation of DHI tools into practice.
Digital Health Inequities
Digital health inequities permeate health care systems within and across countries. There are deeply rooted inequities in health care, and despite the technology ownership improvements, digital access continues to be low among underserved people. 13 Access to DHIs is often limited to various groups, such as people who live in rural areas, are low‐income, belong to racial and ethnic minority groups, have a disability, or are older. Linguistic and immigration barriers may also drive the digital divide within countries. Digital tools and smartphone applications are often designed for English speakers and can be exclusionary to immigrants, refugees, and people from other cultural backgrounds whose native language is not English. 14 People living in poverty typically reside in areas with limited Internet connectivity, broadband access, and access to computers and other digital devices. These populations may also experience limited digital literacy. Health system payment structures and regulatory hurdles also drive issues with access to and use of DHIs. For instance, in the United States, digital therapeutics are approved by the US Food and Drug Administration within the software‐as‐a‐medical‐device category, with some coverage through private insurance, federal and state programs like Medicaid and Veterans Affairs, and out‐of‐pocket spending. 15 To address this limited coverage, the Access to Prescription Digital Therapeutics Act of 2023 bill was recently introduced in the US Senate to expand Medicare coverage to prescription digital therapeutics. 16 There are also disparities in telehealth access, use, and coverage of telehealth visits. To further compound this, people who are not insured are additionally excluded. Eligibility restrictions that exclude segments of people, including undocumented individuals, from accessing health care also limit their access to digital health technologies.
Reciprocal Innovation
In global health partnerships, there is a tendency to assume and adopt a unidirectional flow of innovations, where DHIs developed in HICs are exported to LMICs. 10 This practice is rooted in a colonialist perspective that associates innovation with HICs while discounting the potential of LMICs to develop innovations that may benefit HICs. Thus, Sors and colleagues coined the term reciprocal innovation as the “bidirectional, co‐constituted, and iterative exchange of ideas, resources, and innovations to address shared health challenges across diverse global settings.” 17 From the LMIC perspective, afferent reciprocal innovations flow from HICs toward LMICs, and efferent reciprocal innovations may be exported to HICs with adaptation. A common category of efferent innovations is frugal innovations, which are cost‐effective technologies or strategies arising from LMICs out of the need to do more with fewer resources. 17 For instance, there is DHI diagnostic equipment developed and adjusted to LMICs, sometimes cheaper than their equivalent high‐end products, with high‐quality compliance for use not only in LMICs but also in HICs. Mobile health linked with team‐based care remote patient monitoring approaches, which have also been championed in many LMICs and are being adapted for use in HICs. 18 These frugal innovations have the potential to reduce health inequities in HICs at scale. Similarly, afferent digital innovations developed to reduce inequities in HICs may also have great potential for cost‐effective impact in LMICs by reducing the need for human resources that are so scarce and valuable in these settings (Figure). Reciprocal innovation has 3 main features 17 : (1) global health partnership, which is ingrained in the values of reciprocity, mutual learning, and equity across partner institutions in HICs and LMICs; (2) a bidirectional and co‐constituted approach to identifying shared health challenges across settings in long‐term engagements; and (3) identification of high‐quality innovations from global health partnerships for demonstration, replication, and dissemination in diverse settings.
Figure . Reciprocal innovations in digital health to advance global cardiovascular health equity.
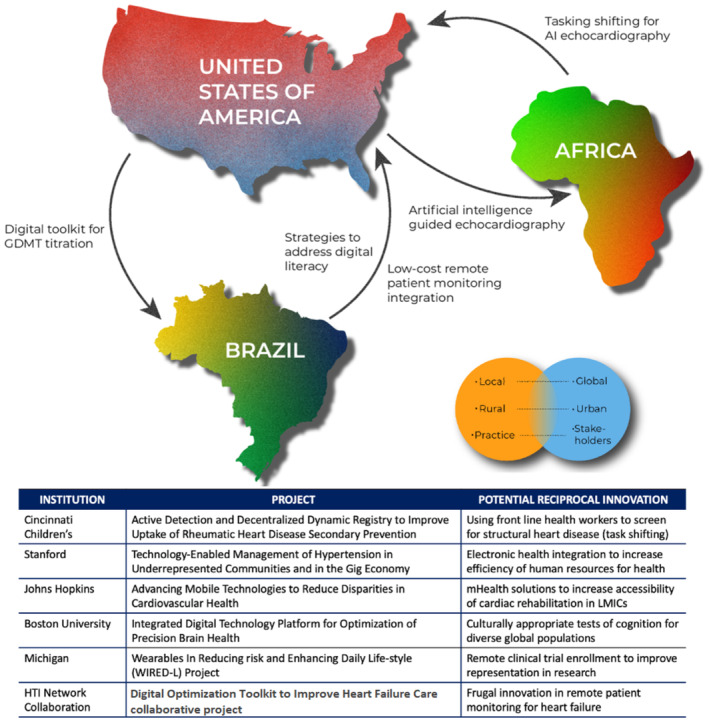
A, Two specific examples of afferent and efferent reciprocal innovation loops in the American Heart Association Health Technology and Innovation Strategically Focused Research Network. Cincinnati Children's is training nurses to screen for rheumatic heart disease using artificial intelligence‐assisted echocardiography acquisition. The team is adapting this approach to screen for structural heart disease at Indian Health Service sites in Arizona. The Digital Optimization Toolkit to Improve Heart Failure Care collaborative project is adapting a patient engagement application for patients with heart failure developed at Stanford for use in Brazil. The Brazil team is testing low‐cost remote patient monitoring solutions that could be useful in low‐resource settings of the United States. B, Reciprocal innovation can occur along multiple axes of context, for example, global to local, urban to rural, or academia to practice. C, Table showing potential reciprocal innovations of all AHA Health Technology and Innovation SFRN projects. AI indicates artificial intelligence; GDMT, guideline‐directed medical therapy; LMICs, low‐ and middle‐income countries; mHealth, mobile health; and HTI SFRN, American Heart Association Health Technology and Innovation Strategically Focused Research Network.
Translating Digital Innovations Across Different Settings
Translating DHIs between high‐ and low‐resource settings is crucial for advancing global cardiovascular health equity. Digital innovations have the potential to revolutionize health care delivery by improving access, delivery efficiency, and quality of care. 19 However, assessing the impact of the delivery of DHIs has often been limited to high‐resource settings, leaving low‐resource settings behind. It is essential to bridge this gap and ensure that digital innovations are accessible, can be applied across different settings, and can subsequently address the disparities in cardiovascular health outcomes.
Low‐resource settings often face significant health care delivery challenges. These challenges include limited health care infrastructure and resources and a shortage of health care professionals. However, by leveraging DHIs that high‐resource areas benefit from, low‐resource settings can overcome these barriers. This, in turn, can improve cardiovascular care delivery and outcomes. For example, telemedicine and mobile health applications can enable remote patient monitoring, timely consultations and referrals, and health education, thus reaching persons in remote or underserved areas.
Translating DHIs from high‐ to low‐resource settings also presents bidirectional learning opportunities between local and global institutions. While local institutions in the United States and many other HICs may have access to cutting‐edge technologies and research expertise, global institutions, particularly those in low‐resource settings, possess invaluable knowledge about their region's context, cultural norms, and healthcare challenges. By fostering collaboration and knowledge exchange, both sides can learn from each other and co‐create innovative solutions that are effective, culturally appropriate, and sustainable. This bidirectional learning approach ensures that DHIs are not simply imposed but are adapted and tailored to the global context and vice versa, increasing their chances of success and impact.
Several factors need to be considered to facilitate the successful translation of DHIs between settings. First, it is critical to involve local partners, including policymakers, regulatory bodies, health care providers, and patients, from the early stages of innovation development. Their input and feedback can guide the design and implementation of digital or other solutions that align with local needs and priorities. Second, capacity‐building and training programs should be established to ensure that health care professionals in low‐resource settings are equipped with the necessary skills to use digital innovations efficiently and maximize their benefits. Third, exploring and implementing DHIs prepared for offline use is expeditious, especially in areas without a reliable power supply and high‐speed Internet. Finally, infrastructure and resource limitations must be addressed. For example, to support the effective integration of DHIs into health care systems, it is important to ensure that reliable Internet connectivity, a sustainable power supply, and the access or ability to acquire affordable devices are available.
Partnering to Ensure Effective and Appropriate Implementation and Adaptation
Effective adaptation and uptake of DHIs between settings require careful consideration of the culture and context where the technology will be used. This is best achieved through partnership with the health intervention's target patient population and the team that will support the rollout of the technology locally. While strategies for stakeholder engagement can vary widely, there are some best practices for design and implementation and digital technology transfer that can help these technologies reach their full potential across settings.
First, human‐centered design (HCD) may be adopted during technology development to develop and evaluate products alongside rather than for the likely end users. Done skillfully, HCD can save time and resources for the development team and results in products that are more creative, inclusive, and effective for the target population. HCD techniques have been increasingly used in the global health context, 20 and new monitoring and evaluation frameworks are being developed to capture these impacts. 21 First, during the technology development process, HCD is an approach that aims to develop and evaluate products alongside rather than for the likely end users. Done skillfully, HCD can save time and resources for the development team and results in products that are more creative, inclusive, and effective for the target population. HCD techniques have been increasingly used in the global health context and new monitoring and evaluation frameworks are being developed to capture these impacts. 21
Building on HCD is the equity‐centered design approach, which specifically aims to understand and account for variables that can lead to inequitable technology benefits among minoritized populations. 22 Equity‐centered design ensures that minoritized communities are engaged as codesigners to ensure solutions meet community needs and overcome systemic barriers to digital technology uptake. While HCD can encompass approaches emphasized in equity‐centered design, minority voices may not be adequately represented when combined with those in the majority.
There are best practices based on real‐life case studies of scaling digital health in LMICs and early implementation of DHIs in LMICs to address infectious disease. Five key focus areas identified as being critical for success include the following: 23 (1) The intrinsic characteristics of the DHI must offer tangible benefits to address an unmet need, with early end‐user input from the outset; (2) all stakeholders must be engaged, trained, and motivated to implement a new initiative; (3) the technical profile of the DHI should be driven by simplicity, interoperability, and adaptability; (4) The DHI should be aligned with the policy environment in which it is intended to function, including engaging the private sector; and (5) the extrinsic ecosystem should be considered, including the existence of appropriate infrastructure to support the DHI at scale.
Finally, when bringing proven technology to a new setting, there are also approaches that can ensure that the application of that technology is acceptable, feasible, and appropriate for a new population or context. Here, community‐based participatory research can be of benefit, empowering community voices and cultural perspectives that result in an authentic understanding of groups that are often underrepresented in research. 24 Just as importantly, roll out of any mobile health technology should include rigorous implementation of science measures as well as clinical outcomes measures to ensure scalability and sustainability of the new approach. 25 Some examples of academic and nonprofit‐led digital health interventions are provided below; there are several private sector–led DHIs, such as McKinsey and the Exemplars in Global Health, a research collaboration focused on assessing digital tools for primary health care in LMICs 26 ; a Novartis‐supported telemedicine project in Ghana; and the like. 23
Exemplar Digital Technology Projects Adaptable to Lower‐Resource Settings
Below are examples of projects funded through the American Heart Association Health Technologies and Innovation Strategically Focused Research Networks that have been adapted to lower‐resource settings or have the potential to adapt to lower‐resource settings.
Exemplar Project 1
Tele‐Visits Using Secure Health Insurance Portability and Accountability Act–Compliant Patient Mobile Video
Stroke is a leading cause of death and disability globally. 27 The burden of stroke globally is unevenly distributed. The burden of stroke globally is not evenly distributed. The timely and accurate diagnosis of stroke is a major public health challenge. Too many strokes are missed, misdiagnosed, or diagnosed too late. 28 Strokes are not misdiagnosed when they present with typical neurologic symptoms such as hemiparesis and aphasia; rather, they are missed when they present with atypical or nonspecific symptoms that mimic more benign disorders, such as isolated dizziness or vertigo. 29 It is estimated that roughly half of the >100 000 missed strokes each year in the United States occur in this clinical population. The Vestibular Neurology team at Johns Hopkins has developed innovative eye movement–based diagnostic approaches to diagnose stroke in these patients with greater accuracy than the gold standard of magnetic resonance imaging with diffusion‐weighted imaging. 29
This program involves designing a web‐based mobile application that connects patient‐recorded eye movement videos to a Health Insurance Portability and Accountability Act–secured TeleDizzy data warehouse known as Vision. This project is developing a smartphone application that accurately measures nystagmus velocity and direction. This project is part of the Johns Hopkins Center for Mobile Technologies to Reduce Disparities in Cardiovascular Health, which seeks to leverage mobile and wearable technologies that directly empower patients and providers to enhance quality, increase value, and reduce health disparities in the diagnosis and management of CVD and stroke.
Accurate eye movement evaluation is central to the timely diagnosis of vestibular strokes, often presenting with dizziness, thought to be innocuous by patients and caregivers. 30 However, the lack of expertise in evaluating eye movements and infrequent use of eye‐tracking technology in emergency departments and urgent care facilities hamper the accurate, timely diagnosis of vestibular strokes. 31 While more advanced medical centers could minimize the harm by using expert providers, lack of such human resources would render other medical centers, more specifically, rural hospitals and those located in areas of the world with a low neurologist‐to‐population ratio, to be more susceptible to adverse consequences of a delayed or inaccurate diagnosis of vestibular strokes.
Improving access to advanced eye movement evaluation and timely stroke diagnosis is the prevailing vision in developing the EyePhone application. Eliminating the need for expensive devices and expert clinicians to obtain accurate measurements of different eye examination components expands this technology's global reach. Currently, the data regarding the proof of the concept and the accuracy and precision of different measurements of the application have been published. The data regarding the accuracy of nystagmus measurements, as an important component in stroke diagnosis, are published in this issue of the Journal of the American Heart Association (JAHA), indicating a high correlation between EyePhone measurements and standard reference in 10 healthy volunteers. This technology is currently being tested on different patient populations with an array of eye movement abnormalities, providing real‐world measures of the application's performance. Moreover, the team behind the application is constantly evaluating its technical and usability aspects to maximize its usability in a wide range of clinical settings.
Exemplar Project 2
Active Case Detection and Decentralized Dynamic Registry to Improve the Uptake of Rheumatic Heart Disease Secondary Prevention
Rheumatic heart disease (RHD), the result of autoimmune response to recurrent untreated group A streptococcal infection, affects ≈40.5 million people worldwide and results in ≈305 000 deaths annually. 32 , 33 However, the distribution of RHD is inequitable, with the highest prevalence in LMICs and marginalized populations in HICs. 32 RHD is a progressive disease, and patients often present late in the disease process with severe valvular dysfunction, heart failure, and stroke. 34 Echocardiographic screening can identify RHD before development of clinical symptoms (latent period), but LMICs often lack the resources and trained experts to implement widespread screening echocardiography.
ADD‐RHD (Active Case Detection and Decentralized Dynamic Registry to Improve the Uptake of Rheumatic Heart Disease Secondary Prevention) is a multipronged program using novel technologies to increase RHD detection and improve RHD management in Uganda. 35 One strategy uses echocardiographic artificial intelligence to further latent RHD detection. 36 Designed in the United States, software integrated into hand‐held devices (Caption Health) aids users in image acquisition and automated diagnosis. This approach aided novice providers in Uganda to successfully obtain screening echocardiograms for RHD after minimal training (efferent reciprocal innovation). 36 With anticipated success from this approach, there is a high potential to scale use of echocardiographic artificial intelligence to more rural settings in Uganda and to adapt this technology for diagnoses and management of other CVD and chronic conditions. This addresses barriers of transportation to specialist facilities, inability to see a specialist due to shortages of health care professionals, and so on.
Within the United States, American Indian populations have been found to have rates of RHD 7 times that of the general population, 37 and a recent study within an American Indian population in eastern Arizona found rates of invasive group A Streptococcus over 30 times higher than those in the general population. 38 This same American Indian population faces multiple barriers to care, 39 including geographic isolation with limited transportation, with patients often having to travel 3 or 4 hours for echocardiograms and cardiology care. In an effort to improve access to echocardiography for American Indians, the American Indian Structural Heart Disease Partnership adapted approaches such as task‐shifting 40 , 41 and artificial intelligence used by ADD‐RHD to integrate echocardiographic screening into the primary care setting. The American Indian Structural Heart Disease Partnership used methods effective in LMICs to develop a low‐cost strategy to address a resource gap within the United States (afferent reciprocal innovation).
Exemplar Project 3
The Digital Optimization Toolkit to Improve Heart Failure Care
Heart failure is a rapidly increasing public health problem, primarily due to aging populations globally. 42 Guideline‐directed medical therapy (GDMT) for heart failure with reduced ejection fraction reduces morbidity and death, yet there is a gap in implementing GDMT in clinical practice, with stark disparities in GDMT use across diverse global populations. 43 Shared barriers to GDMT optimization in HICs and LMICs are an opportunity to codevelop DHIs to promote GDMT implementation. Barriers include(1) reduced access to care, (2) clinician inertia, and (3) patients' inadequate knowledge about the disease and treatment. 42
The Digital Optimization Toolkit to Improve Heart Failure Care toolkit was first developed for the United States and consists of a patient engagement application integrated with a clinician‐facing dashboard. Core elements of the toolkit were developed using HCD 44 and include assessment of patients' health status, medication adherence, and vitals through remote monitoring tools (Bluetooth‐enabled scale and blood pressure cuff). When communicated efficiently to clinicians, these data may promote timely and safe GDMT optimization and patient empowerment, which has increased GDMT optimization by nearly 20% in prior studies. 45
Building on a previous heart failure intervention in Brazil, 46 the Digital Optimization Toolkit to Improve Heart Failure Care toolkit was adapted using HCD. New context‐specific challenges to GDMT optimization in Brazil were considered, including (1) lower income, education, and digital literacy of the Brazilian population; (2) restricted access to specialty care (cardiologists) and newer drugs (sodium‐glucose cotransporter‐2 inhibitors and angiotensin receptor–neprilysin inhibitor); and (3) cultural specificities. Some clinician tasks were shifted to nurses, and centralized cardiology consultations were integrated into the workflow. To address digital literacy, videos were developed for caregivers, and a chat function was added to promote human interaction.
Sources of Funding
LCCB is supported in part by CNPq (307329/2022‐4).
Disclosures
None.
This manuscript was sent to Mahasin S. Mujahid, PhD, MS, FAHA, Associate Editor, for review by expert referees, editorial decision, and final disposition.
For Sources of Funding and Disclosures, see page 6.
References
- 1. Muthiah V, Mensah GA, Varieur TJ, Valentin F, Roth GA. The global burden of cardiovascular diseases and risk. J Am Coll Cardiol. 2022;80:2361–2371. doi: 10.1016/j.jacc.2022.11.005 [DOI] [PubMed] [Google Scholar]
- 2. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker‐Smith CM, Beaton AZ, Boehme AK, Buxton AE, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation. 2023;147:e93–e621. doi: 10.1161/CIR.0000000000001123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hernandez MF, Rodriguez F. Health techequity: opportunities for digital health innovations to improve equity and diversity in cardiovascular care. Curr Cardiovasc Risk Rep. 2023;17:1–20. doi: 10.1007/s12170-022-00711-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization (WHO) . Health Equity. Accessed September 13, 2023. https://www.who.int/health‐topics/healthequity#tab=tab_1
- 6. Xiong S, Lu H, Peoples N, Duman EK, Najarro A, Ni Z, Gong E, Yin R, Ostbye T, Palileo‐Villanueva LM, et al. Digital health interventions for non‐communicable disease management in primary health care in low‐and middle‐income countries. NPJ Digit Med. 2023;6:12. doi: 10.1038/s41746-023-00764-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Economic Impact . The Intersection of Digital Health and Equity. 2022. Accessed September 12, 2023. https://impact.economist.com/perspectives/sites/default/files/ei241_va_report_v3_illustration.pdf.
- 8. Lawrence K. Digital health equity. In: Linwood SL, ed. Digital Health. Exon Publications; 2022. Accessed September 12, 2023. https://pubmed.ncbi.nlm.nih.gov/35605078/ [PubMed] [Google Scholar]
- 9. World Health Organization . Cardiovascular Diseases (CVDs). 2021. Accessed September 12, 2023. https://www.who.int/news‐room/fact‐sheets/detail/cardiovascular‐diseases‐(cvds).
- 10. Ahadzi D, Gaye B, Commodore‐Mensah Y. Advancing the cardiovascular workforce in Africa to tackle the epidemic of cardiovascular disease: the time is now. Global Heart. 2023;18:20. doi: 10.5334/gh.1197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Signé L. Fixing the global digital divide and digital access gap. Brookings. 2023. Accessed September 12, 2023. https://www.brookings.edu/articles/fixing‐the‐global‐digital‐divide‐and‐digital‐access‐gap/#:~:text=While%20this%20growth%20indicates%20that,of%20compounding%20negative%20effects%20in
- 12. Bandura, Romina ML Elena I . The Digital Literacy Imperative. Center for Strategic and International Studies (CSIS) . Accessed September 12, 2023. https://www.csis.org/analysis/digital‐literacy‐imperative
- 13. Dolcini MM, Canchola JA, Catania JA, Song Mayeda MM, Dietz EL, Cotto‐Negrón C, Narayanan V. National‐level disparities in internet access among low‐income and Black and Hispanic youth: current population survey. J Med Int Res. 2021;23:e27723. doi: 10.2196/27723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hong YA, Juon H‐S, Chou W‐YS. Social media apps used by immigrants in the United States: challenges and opportunities for public health research and practice. mHealth. 2021;7:52. doi: 10.21037/mhealth-20-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mantovani A, Leopaldi C, Nighswander CM, Di Bidino R. Access and reimbursement pathways for digital health solutions and in vitro diagnostic devices: current scenario and challenges. Front Med Technol. 2023;5:1101476. doi: 10.3389/fmedt.2023.1101476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Access to Prescription Digital Therapeutics Act of 2023 . H.R.1458. 2023. Accessed September 12, 2023. https://www.congress.gov/bill/118th‐congress/housebill/1458.
- 17. Sors TG, O'Brien RC, Scanlon ML, Bermel LY, Chikowe I, Gardner A, Kiplagat J, Lieberman M, Moe SM, Morales‐Soto N, et al. Reciprocal innovation: a new approach to equitable and mutually beneficial global health partnerships. Global Public Health. 2022;1–13. doi: 10.1080/17441692.2022.2102202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sarkar S, Mateus S. Doing more with less–how frugal innovations can contribute to improving healthcare systems. Soc Sci Med. 2022;306:115127. doi: 10.1016/j.socscimed.2022.115127 [DOI] [PubMed] [Google Scholar]
- 19. Senbekov M, Saliev T, Bukeyeva Z, Almabayeva A, Zhanaliyeva M, Aitenova N, Toishibekov Y, Fakhradiyev I. The recent progress and applications of digital technologies in healthcare: a review. Int J Telemed Appl. 2020;2020:8830200. doi: 10.1155/2020/8830200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Blynn E, Harris E, Wendland M, Chang C, Kasungami D, Ashok M, Ayenekulu M. Integrating human‐centered design to advance global health: lessons from 3 programs. Global Health Sci Pract. 2021;9:S261–S273. doi: 10.9745/GHSP-D-21-00279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Heller C, LaFond A, Murthy L. Methods and benefits of measuring human‐centered design in global health. Global Health Sci Pract. 2021;9:S274–S282. doi: 10.9745/GHSP-D-21-00207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Stiles‐Shields C, Cummings C, Montague E, Plevinsky JM, Psihogios AM, Williams KDA. A call to action: using and extending human‐centered design methodologies to improve mental and behavioral health equity. Front Digit Health. 2022;4:4. doi: 10.3389/fdgth.2022.848052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Labrique AB, Wadhwani C, Williams KA, Lamptey P, Hesp C, Luk R, Aerts A. Best practices in scaling digital health in low‐ and middle‐income countries. Global Health. 2018;14:103. doi: 10.1186/s12992-018-0424-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Marrone NL, Nieman CL, Coco L. Community‐based participatory research and human‐centered design principles to advance hearing health equity. Ear Hear. 2022;43:33S–44S. doi: 10.1097/AUD.0000000000001183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shaw J, Agarwal P, Desveaux L, Palma DC, Stamenova V, Jamieson T, Yang R, Bhatia RS, Bhattacharyya O. Beyond “implementation”: digital health innovation and service design. NPJ Digital Med. 2018;1:48. doi: 10.1038/s41746-018-0059-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bode M, Goodrich T, Kimeu M, Okebukola P, Wilson M. COVID‐19 led many healthcare systems in lower‐ and middle‐income countries to adapt digital‐healthcare platforms. McKinsey & Company. 2021. Accessed September 1, 2023. https://www.mckinsey.com/industries/healthcare/our‐insights/unlocking‐digital‐healthcare‐in‐lower‐and‐middle‐income‐countries [Google Scholar]
- 27. Katan M, Luft A. Global burden of stroke. Seminars Neurol. 2018;38:208–211. doi: 10.1055/s-0038-1649503 [DOI] [PubMed] [Google Scholar]
- 28. Wallace EJC, Liberman AL. Diagnostic challenges in outpatient stroke: stroke chameleons and atypical stroke syndromes. Neuropsychiatric Dis Treat. 2021;17:1469–1480. doi: 10.2147/NDT.S275750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Newman‐Toker DE, Saber Tehrani AS, Mantokoudis G, Pula JH, Guede CI, Kerber KA, Blitz A, Ying SH, Hsieh Y‐H, Rothman RE, et al. Quantitative video‐oculography to help diagnose stroke in acute vertigo and dizziness: toward an ECG for the eyes. Stroke. 2013;44:1158–1161. doi: 10.1161/STROKEAHA.111.000033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kattah JC, Talkad AV, Wang DZ, Hsieh Y‐H, Newman‐Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three‐step bedside oculomotor examination more sensitive than early MRI diffusion‐weighted imaging. Stroke. 2009;40:3504–3510. doi: 10.1161/STROKEAHA.109.551234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ohle R, Montpellier R‐A, Marchadier V, Wharton A, McIsaac S, Anderson M, Savage D. Can emergency physicians accurately rule out a central cause of vertigo using the HINTS examination? A systematic review and meta‐analysis. Acad Emerg Med. 2020;27:887–896. doi: 10.1111/acem.13960 [DOI] [PubMed] [Google Scholar]
- 32. Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, Forouzanfar MH, Longenecker CT, Mayosi BM, Mensah GA, et al. Global, regional, and national burden of rheumatic heart disease, 1990‐2015. N Eng J Med. 2017;377:713–722. doi: 10.1056/NEJMoa1603693 [DOI] [PubMed] [Google Scholar]
- 33. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd‐Allah F, Abdela J, Abdelalim A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zühlke L, Engel ME, Karthikeyan G, Rangarajan S, Mackie P, Cupido B, Mauff K, Islam S, Joachim A, Daniels R, et al. Characteristics, complications, and gaps in evidence‐based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study). Eur Heart J. 2015;36:1115–1122a. doi: 10.1093/eurheartj/ehu449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Reach. Reach Partners with Cincinnati Children's Hospital on RHD Secondary Prevention Research Project. 2020. Accessed Septmber 1, 2023. https://www.stoprhd.org/news/reach‐partners‐cincinnati‐childrens‐hospital‐rhdsecondary‐prevention‐researchproject#:~:text=Reach%20is%20partnering%20with%20the,(ADD%2DRHD)%20project.
- 36. Peck D, Rwebembera J, Nakagaayi D, Minja NW, Ollberding NJ, Pulle J, Klein J, Adams D, Martin R, Koepsell K, et al. The use of artificial intelligence guidance for rheumatic heart disease screening by novices. J Am Soc Echocardiograph. 2023;36:724–732. doi: 10.1016/j.echo.2023.03.001 [DOI] [PubMed] [Google Scholar]
- 37. Schaffer WL, Galloway JM, Roman MJ, Palmieri V, Liu JE, Lee ET, Best LG, Fabsitz RR, Howard BV, Devereux RB. Prevalence and correlates of rheumatic heart disease in American Indians (the Strong Heart Study). Am J Cardiol. 2003;91:1379–1382. doi: 10.1016/S0002-9149(03)00338-2 [DOI] [PubMed] [Google Scholar]
- 38. Sutcliffe C, Close R, Davidson A, Reid A, Quay D, Nicolet K, Brown L, Grant L, Weatherholtz R, McAuley J, et al. 453. High burden of invasive and severe group A Streptococcus disease among native Americans on the White Mountain Apache tribal lands. Open Forum Infect Dis. 2019;6:S223. doi: 10.1093/ofid/ofz360.526 [DOI] [Google Scholar]
- 39. Galloway JM. Cardiovascular health among American Indians and Alaska Natives: successes, challenges, and potentials. Am J Prevent Med. 2005;29:11–17. doi: 10.1016/j.amepre.2005.07.023 [DOI] [PubMed] [Google Scholar]
- 40. Scheel A, Ssinabulya I, Aliku T, Bradley‐Hewitt T, Clauss A, Clauss S, Crawford L, DeWyer A, Donofrio MT, Jacobs M, et al. Community study to uncover the full spectrum of rheumatic heart disease in Uganda. Heart. 2019;105:60–66. doi: 10.1136/heartjnl-2018-313171 [DOI] [PubMed] [Google Scholar]
- 41. Ubels J, Sable C, Beaton AZ, Nunes MCP, Oliveira KKB, Rabelo LC, Teixeira IM, Ruiz GZL, Rabelo LMM, Tompsett AR, et al. Cost‐effectiveness of rheumatic heart disease echocardiographic screening in Brazil: data from the PROVAR+ study: cost‐effectiveness of RHD screening in Brazil. Global Heart. 2020;15:18. doi: 10.5334/gh.529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e895–e1032. doi: 10.1161/CIR.0000000000001063 [DOI] [PubMed] [Google Scholar]
- 43. Joseph P, Roy A, Lonn E, Störk S, Floras J, Mielniczuk L, Rouleau J‐L, Zhu J, Dzudie A, Balasubramanian K, et al. Global variations in heart failure etiology, management, and outcomes. JAMA. 2023;329:1650–1661. doi: 10.1001/jama.2023.5942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Isakadze N, Molello N, MacFarlane Z, Gao Y, Spaulding EM, Commodore Mensah Y, Marvel FA, Khoury S, Marine JE, Michos ED, et al. The virtual inclusive digital health intervention design to promote health equity (iDesign) framework for atrial fibrillation: co‐design and development study. JMIR Hum Factors. 2022;9:e38048. doi: 10.2196/38048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Allen LA, Venechuk G, McIlvennan CK, Page RL II, Knoepke CE, Helmkamp LJ, Khazanie P, Peterson PN, Pierce K, Harger G, et al. An electronically delivered patient‐activation tool for intensification of medications for chronic heart failure with reduced ejection fraction: the EPIC‐HF trial. Circulation. 2021;143:427–437. doi: 10.1161/CIRCULATIONAHA.120.051863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ribeiro EG, Brant L, Rezende LC, Teixeira RA, Parreiras LC, Franco TB, Ribeiro A, Malta D. Effectiveness of telemedicine in reducing hospitalizations in patients discharged from the hospital due to heart failure: a randomized clinical trial protocol. Int J Cardiovasc Sci. 2022;35:635–642. doi: 10.36660/ijcs.20210131 [DOI] [Google Scholar]


