Abstract
Background
Telecommunicator CPR (T‐CPR), whereby emergency dispatch facilitates cardiac arrest recognition and coaches CPR over the telephone, is an important strategy to increase early recognition and bystander CPR in adult out‐of‐hospital cardiac arrest (OHCA). Little is known about this treatment strategy in the pediatric population. We investigated the role of T‐CPR and related performance among pediatric OHCA.
Methods and Results
This study was a retrospective cohort investigation of OHCA among individuals <18 years in King County, Washington, from April 1, 2013, to December 31, 2019. We reviewed the 911 audio recordings to determine if and how bystander CPR was delivered (unassisted or T‐CPR), key time intervals in recognition of arrest, and key components of T‐CPR delivery. Of the 185 eligible pediatric OHCAs, 23% (n=43) had bystander CPR initiated unassisted, 59% (n=109) required T‐CPR, and 18% (n=33) did not receive CPR before emergency medical services arrival. Among all cases, cardiac arrest was recognized by the telecommunicator in 89% (n=165). Among those receiving T‐CPR, the median (interquartile range) interval from start of call to OHCA recognition was 59 seconds (38–87) and first CPR intervention was 115 seconds (94–162). When stratified by age (≤8 versus >8), the older age group was less likely to receive CPR before emergency medical services arrival (88% versus 69%, P=0.002). For those receiving T‐CPR, bystanders spent a median of 207 seconds (133–270) performing CPR. The median compression rate was 93 per minute (82–107) among those receiving T‐CPR.
Conclusions
T‐CPR is an important strategy to increase early recognition and early CPR among pediatric OHCA.
Keywords: cardiac arrest, dispatch, pediatrics, prehospital
Subject Categories: Cardiopulmonary Resuscitation and Emergency Cardiac Care, Pediatrics
Nonstandard Abbreviations and Acronyms
- OHCA
out‐of‐hospital cardiac arrest
- T‐CPR
telecommunicator cardiopulmonary resuscitation
Clinical Perspective.
What Is New?
Although telecommunicator cardiopulmonary resuscitation (CPR) has been well studied in adult patients, this novel evaluation examines the role of the telecommunicator in delivery of bystander CPR in pediatric out‐of‐hospital cardiac arrest—a condition with unique circumstances and often different CPR goals, including ventilation delivery.
Leveraging 911 audio recordings to investigate bystander CPR performance, this study provides new insight into telecommunicator‐directed CPR performance in pediatric out‐of‐hospital cardiac arrest.
What Are the Clinical Implications?
Telecommunicators have the potential to play an important role in recognition of cardiac arrest and delivery of bystander CPR in pediatric out‐of‐hospital cardiac arrest.
Understanding the challenges associated with recognition of arrest and delivery of telecommunicator CPR in pediatric patients will help guide training efforts for communities seeking to improve pediatric telecommunicator CPR performance.
This study is the first large investigation to evaluate telecommunicator CPR performance in pediatric patients and thus may help inform pediatric‐specific performance standards for telecommunicator CPR.
Although less frequent among children than adults, out‐of‐hospital cardiac arrest (OHCA) among people <18 years has an estimated incidence of ~5 to 10 per 100 000 person‐years, 1 , 2 resulting in thousands of deaths in the United States alone each year. Although survival following pediatric OHCA is generally poor—ranging from 3% to 15% depending on age 1 , 3 —successful resuscitation is possible and relies on the links in the chain of survival. 4 As with adults, key determinants of positive outcomes among pediatric OHCA cases involve early arrest recognition and early bystander CPR. 5 Telecommunicator CPR (T‐CPR) or dispatcher‐assisted CPR, whereby emergency communication professionals facilitate OHCA identification and coach CPR over the telephone before emergency medical services (EMS) arrival, is an important strategy to increase early arrest recognition and bystander CPR and in turn is associated with a greater chance of survival. 5 , 6 , 7 , 8 This appreciation has produced initiatives to measure and improve T‐CPR using performance metrics that define timely arrest recognition, effective CPR coaching, and CPR performance. 9
Although the effect of T‐CPR on OHCA in adults has been investigated, little is known about T‐CPR in pediatric OHCA, an event with distinct circumstances and sometimes different CPR priorities. Current guidelines recommend the combination of ventilations and compressions as the optimal bystander T‐CPR approach among younger pediatric patients given the more common respiratory pathogenesis in the younger age group. We investigated the role of T‐CPR with regard to arrest recognition and bystander CPR performance to characterize if and how this strategy is used in pediatric OHCA.
METHODS
This study was approved by the University of Washington Institutional Review Board. The requirement for informed consent was waived due to the retrospective nature of this study. A subset of the data generated for this study is available upon request from the corresponding author with a specific data use agreement.
Study Design, Population, and Setting
This investigation was a retrospective cohort study of nontraumatic OHCA in patients <18 years of age that occurred between April 1, 2013, and December 31, 2019. This study took place in King County, Washington, a mixed urban and suburban region with a population of approximately 2.3 million total individuals and 455 000 individuals <18 years. Cardiac arrest is determined if a patient is found to be pulseless by EMS or receives a shock by an automated external defibrillator before arrival of EMS. We included cases of confirmed nontraumatic OHCA in patients <18 years of age that occurred before the arrival of EMS and had a 911 audio recording available.
Dispatch Program and Protocol
Citizens activate professional emergency response by calling 911 to contact the emergency communication center. Telecommunicators use criteria‐based dispatch guidelines to provide prearrival instructions. After determining the address and location of the patient, telecommunicators use a 2‐question sequence designed to identify OHCA: “Is the patient conscious/awake?” and “Is the patient breathing normally?” If the caller answers no to both questions, then the telecommunicator proceeds to engage the caller in CPR instructions. Arrest recognition by the telecommunicator was inferred if the telecommunicator verbalized that the patient was in arrest or indicated that CPR needed to be performed.
The telecommunicator first instructs the caller to position the patient flat on their back on a hard surface. T‐CPR instructions for patients 0 to 8 years of age include instructions for compressions and ventilations at a ratio of 30:2, whereas instructions for patients 9 to 17 years of age are for compressions only with use of 2‐finger (<1 year), 1‐hand (1–8 years), or 2‐hand (≥9 years) to deliver compressions. In cases where a primary respiratory cause is suspected, telecommunicators may provide ventilation instructions in the older age group. Callers are encouraged to count out loud with each compression so that the telecommunicator can give feedback on appropriate rate and encourage ongoing CPR. The telecommunicator remains on the line until EMS arrives on scene in most cases.
Data Collection and Definitions
The EMS system maintains registries of OHCA organized according to the Utstein template. 10 Information about patient demographics (including date of birth), presentation, treatment, and outcome is systematically collected by trained data abstractors. Data classification is determined based on review of the dispatch audio recording, defibrillator electronic data, prehospital and hospital records, and death certificates.
Based on review of the dispatch audio recording, we stratified cases into 3 exclusive categories: (1) those for whom bystander CPR was spontaneously initiated (no telecommunicator instruction was needed), (2) those who required telecommunicator instruction to initiate CPR performance, and (3) those who did not receive bystander CPR before EMS arrival. We determined the timing of arrest recognition, onset of bystander CPR, and delays to CPR initiation. The start of the call was the time of 911 pick‐up. Caller verbalization that CPR was being performed, audible counting, audible delivery of compressions, or audible ventilations defined the CPR start time. The presence of agonal respirations required a description by the caller or audible gasps on the recording. For cases that received T‐CPR, rescuers more routinely verbalized their actions as directed by the telecommunicator; hence reviewers could better assess characteristics of the sequence, composition (chest compressions alone versus chest compressions plus ventilations), and quality (compression rate) of bystander CPR for this group. We were also able to assess the cause and timing of interruptions during bystander CPR for the T‐CPR cohort. This evaluation of CPR performance examined the interval from the onset of bystander CPR to arrival of EMS. A delay was defined by a deviation from the expected call sequence (address determination, assessment of consciousness and breathing, delivery of CPR instructions) lasting >5 seconds. An interruption in CPR performance was defined as any interval >5 seconds in which the bystander was not performing chest compressions or actions associated with delivery of ventilations.
We assessed interreviewer reliability of the key time intervals of arrest recognition and the start of bystander CPR in a subset of cases (n=10). Agreement required that the reviewers' interval be within 5 seconds of each other. Using this method, interreviewer agreement with regard to the timing of arrest recognition and the start of bystander CPR was 90%.
Statistical Analysis
We used descriptive statistics to present OHCA circumstances and CPR care overall and according to the prespecified CPR status groups (unassisted CPR, T‐CPR, and no CPR) and age (<1, 1–8, 9–17 years). Differences across groups were assessed with the Pearson chi‐square test. In the analyses stratified by age group, we sought to report sequence of CPR actions (compressions first or ventilations first), composition of CPR (compressions plus ventilations or compressions only), and quality (compression rate and frequency and duration of interruptions) as the guideline‐directed composition and potentially sequence may vary by age group. The assessment of CPR according to age was thus restricted to those receiving T‐CPR as ascertainment of the CPR sequence, composition, and quality could be readily ascertained for this group as described previously. Stata (version 16.0; StataCorp, College Station, TX) was used for statistical analysis.
RESULTS
During the study period, 230 individuals <18 years old experienced nontraumatic OHCA before EMS arrival. A total of 41 were missing the audio recording and 4 were born after the time of the 911 call, leaving 185 cases for the study cohort. Although there was no evidence of difference for most characteristics according to recording availability, bystander CPR was more frequent in the patients with an available recording (82% versus 63%, Table S1). Of the 185 reviewed cases, 23% received unassisted bystander CPR, 59% received T‐CPR, and 18% did not receive CPR before EMS arrival (Figure 1). Among those who did not receive bystander CPR, nonexclusive contributors preventing bystander CPR included lack of arrest recognition by the telecommunicator (n=11), no caller access to the patient (n=9), caller emotional distress (n=9), loss of phone contact (n=5), caller refusal of T‐CPR instructions (n=4), and language barrier (n=3).
Figure 1. Overview of the study population, cardiac arrest recognition by the telecommunicator, and bystander CPR delivery.
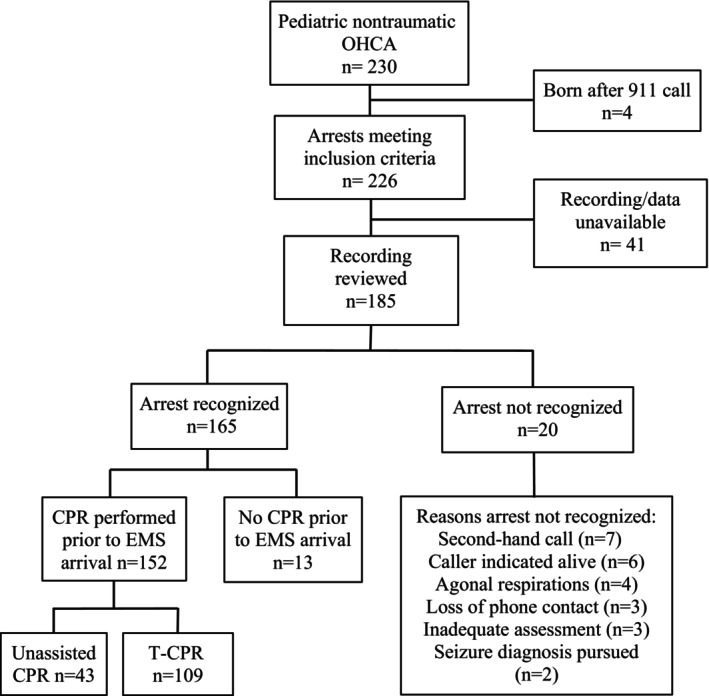
†Multiple factors may have contributed to lack of arrest recognition for each individual case. CPR indicates cardiopulmonary resuscitation; EMS, emergency medical services; OHCA, out‐of‐hospital cardiac arrest; and T‐CPR, telecommunicator cardiopulmonary resuscitation.
Table 1 presents Utstein characteristics overall and according to bystander CPR status. Overall, 41% (n=75) were women and median age was 1.0 years (0.2–11.5 years). Most pediatric OHCAs occurred in the home, had noncardiac pathogenesis, were not witnessed, had multiple bystanders, and presented with a nonshockable rhythm (Table 1). Overall, 14% survived to hospital discharge and 12% survived with favorable neurological status based on Cerebral Performance Category of 1 or 2. Compared with unassisted and no bystander CPR groups, the T‐CPR group was on average younger and more likely to have an unwitnessed, home location, nonshockable OHCA (Table 1). Arrest causes associated with challenges to patient access, such as hanging and drowning, occurred with greater frequency in patients who did not receive CPR compared with those who received unassisted CPR or T‐CPR (Table 1).
Table 1.
Patient Characteristics, Arrest Recognition, and Key Time Intervals According to Type of CPR Delivered
| Unassisted CPR (n=43) | T‐CPR (n=109) | No CPR (n=33) | All cases (n=185) | |
|---|---|---|---|---|
| Utstein characteristics | ||||
| Age, % (n)* | ||||
| <1 y | 42% (18) | 60% (65) | 21% (7) | 48% (89) |
| 1–8 y | 14% (6) | 20% (22) | 21% (7) | 19% (36) |
| 9–17 y | 44% (19) | 20% (22) | 55% (18) | 32% (59) |
| Female sex, % (n) | 37% (16) | 46% (50) | 27% (9) | 41% (75) |
| Witnessed, % (n) | 49% (21) | 24% (26) | 48% (16) | 34% (63) |
| ≥2 bystanders present, % (n) | 88% (38) | 70% (76) | 70% (23) | 74% (137) |
| Home location, % (n) | 70% (30) | 92% (100) | 67% (22) | 82% (152) |
| Noncardiac cause, % (n) | 70% (30) | 70% (76) | 79% (26) | 71% (132) |
| Response interval in minutes, median (IQR) | 4.28 (3.32–5.45) | 4.47 (3.83–5.13) | 4.88 (3.88–6.33) | 4.48 (3.80–5.45) |
| Initial rhythm shockable, %, (n) | 14% (6) | 6% (7) | 9% (3) | 9% (16) |
| PAD used, %, (n)† | 16% (7) | 6% (6) | 9% (3) | 9% (16) |
| Status at end of emergency medical services care, %, (n) | ||||
| Died in field | 37% (16) | 61% (67) | 42% (14) | 52% (97) |
| Ongoing CPR | 16% (7) | 16% (17) | 30% (10) | 18% (34) |
| Alive at emergency department arrival | 47% (20) | 23% (25) | 27% (9) | 29% (54) |
| Outcomes at hospital discharge, % (n) | ||||
| Survived | 21% (9) | 11% (12) | 12% (4) | 14% (25) |
| Cerebral Performance Category 1–2 | 16% (7) | 10% (11) | 12% (4) | 12% (22) |
| Arrest recognition | ||||
| Arrest recognized, % (n) | 100% (43) | 100% (109) | 39% (13) | 89% (165) |
| Key time intervals from start of call in seconds, median (IQR) | ||||
| Interval to address confirmation | 23 (19–33) | 30 (21–38) | 35 (21–51) | 30 (21–40) |
| Interval to recognition of arrest | 47 (30–86) | 59 (38–87) | 64 (62–101) | 58 (37–87) |
| Interval to first CPR intervention | 102 (39–154) | 115 (94–162) | … | 114 (91–161) |
| Delays‡ and complicating factors in recognition or delivery of CPR instructions | ||||
| Agonal respirations present, % (n) | 9% (4) | 18% (20) | 15% (5) | 16% (29) |
| Initial complaint described, % (n) | ||||
| Hanging | 12% (5) | 4% (4) | 12% (4) | 7% (13) |
| Drowning | 7% (3) | 3% (3) | 15% (5) | 6% (11) |
| Cases with ≥1 delay, % (n) | 58% (25) | 92% (100) | 82% (27) | 82% (152) |
| Delay time, sec, median (IQR) | 42 (14–74) | 35 (21–63) | 151 (58–263) | 44 (22–91) |
CPR indicates cardiopulmonary resuscitation; IQR, interquartile range; PAD, public access defibrillator; and T‐CPR, telecommunicator cardiopulmonary resuscitation.
Exact age could not be determined in 1 case.
PAD applied after the call was terminated in the no CPR group.
Delay is defined as any deviation from the expected call sequence lasting >5 seconds that occurred before initiation of CPR.
Arrest Recognition
The most common patient conditions initially reported by the caller were absent or abnormal breathing (49%), unconsciousness (12%), and hanging (7%). Agonal respirations were heard or described in 16% (n=29) of all cases and 19% (n=12) among witnessed OHCAs. The arrest was recognized by the telecommunicator in 89.2% (n=165) of cases, including 39% (n=13) of cases in the no bystander CPR group. When restricted to calls in which the bystander could respond to questions about consciousness and breathing (ie, those with the bystander on scene and maintained phone contact), the arrest was recognized in 94.5% (165/176). Among all cases where the arrest was recognized (n=165), the median (interquartile range) interval from call initiation to arrest recognition was 58 (37–87) seconds, increasing from 47 (30–86) seconds among unassisted CPR, 59 (38–87) seconds among the T‐CPR group, and 64 (62–101) seconds among the no bystander CPR group.
CPR Initiation
Overall, 82% (n=152) of patients received bystander CPR before EMS arrival. Bystander CPR was initiated without telecommunicator assistance (unassisted CPR) in 23% (n=43), though 28% (12/43) of these cases still received coaching on 1 or more aspects of CPR, including rate (n=9), depth or hand placement (n=3), instructions on ventilations (n=2), and ratio of compressions to ventilations (n=8). With regard to CPR performance, the interval from call receipt to the caller report of the start of bystander CPR was 102 seconds (39–154) among those receiving unassisted CPR and 115 seconds (94–162) among those requiring T‐CPR to initiate bystander CPR.
Delays
In 82% (152/185) of cases there was at least 1 delay to recognition of arrest or the start of CPR. Among these 152 cases, the most common (nonexclusive) causes were pauses in the interaction between the caller and telecommunicator in 57% (n=86), with a median associated time of 17 seconds (11–41), unnecessary information requested by the telecommunicator in 42% (n=64), with a median associated delay of 17 seconds (9–53), caller emotional distress in 34% (n=51), with a median associated time delay of 21 seconds (10–66), and unnecessary information provided by the caller in 24% (n=37), with a median associated delay of 12 seconds (8–15). The longest median delay of 108 seconds (47–189) was associated with language barrier and occurred in 4% of cases (n=6).
Age Groups
Among the total pediatric cohort with OHCA (n=185), 49% (n=90) were <1 year old, 19% (n=35) were 1 to 8 years old, and 32% (n=59) were 9 to 17 years old. Among patients <1 year old, 13% (n=12) were <1 day old, 13% (n=12) were 1 to 28 days old, and 72% (n=66) were 29 days to 364 days old. The proportion of patients who received CPR decreased as age group increased: 92% among <1 year, 80% among 1 to 8 years, and 68% among 9 to 17 years (P=0.002). The decrease in overall CPR performance in the oldest age group is directly related to the lower frequency of T‐CPR in this cohort (Figure 2).
Figure 2. Proportion of patients who received CPR according to age group.
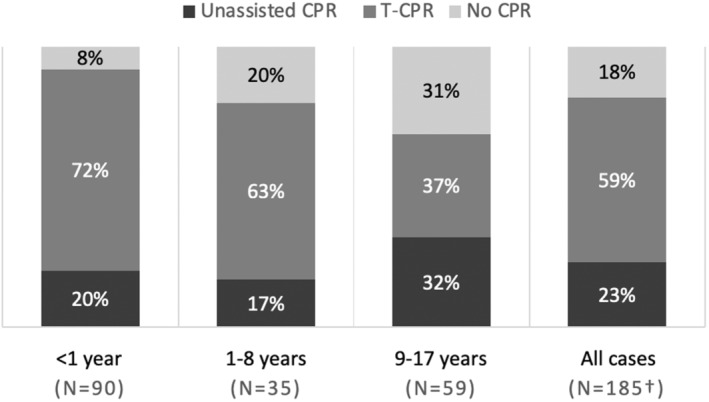
†Exact age could not be determined in one case. CPR indicates cardiopulmonary resuscitation; and T‐CPR, telecommunicator cardiopulmonary resuscitation.
T‐CPR Performance According to Age Group
Among the T‐CPR cohort (n=109), the large majority (95%) of the younger age groups received compressions and ventilations, most often using the compression‐airway‐breathing sequence (Table 2). Conversely, the large majority (95%) of the 9‐ to 17‐year age group received chest compressions only bystander CPR. The interval from the start of the call to initiation of CPR (first compression or ventilation) was 115 seconds (94–162) overall and increased according to age group: 109 seconds (87–146) among the <1 year group, 123 seconds (99–168) among the 1 to 8 year group, and 149 seconds (103–195) among the 9 to 17 year age group. The compression‐airway‐breathing sequence delivered the first compression in 110 seconds and the first ventilation in 161 seconds. The airway‐breathing‐compression sequence delivered the first compression in 155 seconds and the first ventilation in 123 seconds. Among cases receiving ventilations (n=84), callers described difficulty with delivery of ventilations in 25% (n=21), with the most common challenges related to fluid, secretions, or blood in the airway (n=17). The median compression rate was 93 per minute (82–107) overall and did not differ across the age groups. Table 3 shows the proportion of CPR time spent on compressions, ventilations, interruptions, and unknown actions by type of CPR performed.
Table 2.
Patient Characteristics, CPR Sequence Performed, and Key Time Intervals for Patients Who Received CPR Stratified By Age
| <1 year (n=65) | 1–8 years (n=22) | 9–17 years (n=22) | All T‐CPR cases (n=109) | |
|---|---|---|---|---|
| Utstein characteristics | ||||
| Female sex, % (n) | 46% (30) | 50% (11) | 41% (9) | 46% (50) |
| Witnessed, % (n) | 17% (11) | 27% (6) | 41% (9) | 24% (26) |
| ≥2 bystanders present, % (n) | 69% (45) | 55% (12) | 86% (19) | 70% (76) |
| Home location, % (n) | 97% (63) | 91% (20) | 77% (17) | 92% (100) |
| Noncardiac cause, % (n) | 71% (46) | 77% (17) | 59% (13) | 70% (76) |
| First unit response interval in minutes, median (IQR) | 4.48 (3.83–5.13) | 4.35 (4.00–4.82) | 4.48 (3.47–5.67) | 4.47 (3.83–5.13) |
| Initial rhythm shockable, %, (n) | 2% (1) | 9% (2) | 18% (4) | 6% (7) |
| Public access defibrillator used, %, (n) | 3% (2) | 9% (2) | 9% (2) | 6% (6) |
| Status at end of emergency medical services care, %, (n) | ||||
| Died in field | 75% (49) | 41% (9) | 41% (9) | 61% (67) |
| Ongoing CPR | 14% (9) | 32% (7) | 5% (1) | 16% (17) |
| Alive at emergency department arrival | 11% (7) | 27% (6) | 55% (12) | 23% (25) |
| Outcomes at hospital discharge, % (n) | ||||
| Survived | 5% (3) | 14% (3) | 27% (6) | 11% (12) |
| Cerebral Performance Category 1–2 | 5% (3) | 9% (2) | 23% (5) | 10% (11) |
| CPR sequence performed | ||||
| CAB | 77% (50) | 50% (11) | 5% (1) | 57% (62) |
| ABC | 22% (14) | 36% (8) | … | 20% (22) |
| Compressions only | 2% (1) | 14% (3) | 95% (21) | 23% (25) |
| Time intervals to first CPR intervention* in seconds, median (IQR) | ||||
| Start of call to intervention | 109 (87–146) | 123 (99–168) | 149 (103–195) | 115 (94–162) |
| Start of assessment to intervention | 81 (64–103) | 88 (68–140) | 112 (69–186) | 85 (64–125) |
| Recognition of arrest to intervention | 58 (41–79) | 64 (36–74) | 68 (44–106) | 58 (41–81) |
| Time interval from start of call to first compression in seconds, median (IQR) | ||||
| CAB | 109 (85–142) | 111 (91–160) | 186† | 110 (91–144) |
| ABC | 148 (115–254) | 174 (134–212) | … | 155 (121–224) |
| Compression only | 220* | 140 (114–256) | 142 (113–195) | 142 (114–219) |
| Time interval from start of call to first ventilation in seconds median (IQR) | ||||
| CAB | 158 (133–186) | 175 (138–186) | 234† | 161 (135–186) |
| ABC | 120 (96–206) | 124 (106–174) | … | 123 (99–206) |
ABC indicates airway‐breathing‐compression CPR sequence; CAB, compression‐airway‐breathing CPR sequence; CPR, cardiopulmonary resuscitation; IQR, interquartile range; and T‐CPR, telecommunicator cardiopulmonary resuscitation.
First CPR intervention is the first ventilation or compression, whichever occurred first.
IQR not reported for single observations.
Table 3.
Compression Rate and Fraction of Total CPR Interval Spent on Compressions, Ventilations, and Other Activities by Type of CPR Among Patients Who Received Telecommunicator CPR
| 30:2 Compressions and ventilations | Compression only | All cases | |
|---|---|---|---|
| Total CPR interval* in seconds, median (IQR) | 211 (143–258) | 206 (107–294) | 207 (133–270) |
| Compression fraction, mean (SD) | 43% (19) | 88% (25) | 54% (28) |
| Ventilation fraction, mean (SD) | 25% (14) | … | 20% (16) |
| Interruption fraction†, mean (SD) | 14% (16) | 6% (17) | 12% (17) |
| Unknown action fraction‡, mean (SD) | 17% (22) | 6% (17) | 15% (21) |
| Compressions/minute, median (IQR) | 92 (82–106) | 100 (86–109) | 93 (82–107) |
Total CPR interval begins with first compression or ventilation, whichever occurs first, and ends with last compression, ventilation, or the end of the 911 call.
Interruptions in CPR were defined as any interval ≥5 seconds in which the bystander was heard performing activities other than ventilations or compressions.
Unknown actions were defined as any interval ≥5 seconds in which the action of the caller could not be determined from the 911 audio.
CPR indicates cardiopulmonary resuscitation; and IQR, interquartile range.
DISCUSSION
Summary
In this cohort investigation of pediatric OHCAs, 82% (n=152) of patients received bystander CPR, the majority (n=109) as a consequence of T‐CPR identification and coaching. Nearly 90% (n=165) of OHCAs were recognized by the telecommunicator, with 92% (152/165) of the recognized group receiving bystander CPR. Among those requiring T‐CPR, the median interval from call initiation to OHCA recognition was 59 seconds and from arrest recognition to start of bystander CPR was 58 seconds, producing a combined median interval from call initiation to the start of bystander CPR of 115 seconds. Most of the T‐CPR period was spent providing CPR, though the distribution and timing of compressions and ventilations was determined in part by the specific algorithm (compressions only versus compressions plus ventilations). A mix of logistical, caller, and telecommunicator factors contributed to delays and interruptions in timely OHCA recognition and CPR performance.
Role of Telecommunicator and T‐CPR in Pediatric OHCA
Approaches to improve outcomes following OHCA highlight early recognition and early CPR. Among adults, T‐CPR is a proven strategy that can increase bystander CPR and is associated with greater survival. T‐CPR can double or even triple the proportion of adult patients experiencing OHCA who receive bystander CPR. 11 , 12 , 13 We observed a similar and important role for T‐CPR in pediatric OHCAs, where telecommunicator involvement was integral in upwards of three‐quarters of cases that received bystander CPR, facilitating both cardiac arrest recognition and CPR performance. Importantly, even if CPR was initially started by the bystanders unassisted, the telecommunicator provided important coaching in multiple instances. Thus T‐CPR appears to be a viable and promising strategy to improve pediatric OHCA outcomes. Bystander CPR among pediatric OHCAs was substantially more common in our study community compared with other North American systems, suggesting an opportunity for public health benefit by increasing early CPR with broad‐based implementation of T‐CPR. 1
T‐CPR Performance Metrics
The investigation provides real‐world experience that can be used to inform T‐CPR performance metrics for pediatric OHCA resuscitation. Among adults, these metrics related to arrest recognition, CPR, and their timing provide useful process goals for individual and organizational performance, and in turn can provide an operational means to improve care and outcome. We observed telecommunicator OHCA recognition in approximately 90% of all pediatric OHCA cases and successful start of bystander CPR in a similar proportion of recognized OHCAs (even when excluding those cases who received unassisted bystander CPR). Median interval to recognition was 59 seconds and to start of CPR was 115 seconds, mirroring best practices goals among adult OHCAs. 9 The study results provide support for the 2‐question approach for identification of pediatric OHCA and can inform performance goals as the field of resuscitation seeks to operationalize scientific understanding into best clinical practices. Moreover, the identified causes for delay and interruptions provide a useful framework for training and quality improvement aimed at advancing bystander and telecommunicator OHCA care.
Differences by Age
Pediatric resuscitation after OHCA presents a special challenge for lay individuals given the diverse age‐related circumstances and the potential goal to incorporate ventilations as part of bystander CPR. We observed age group differences in the likelihood of bystander CPR performance and composition. Although two‐thirds of the 9‐ to 17‐year‐old group received bystander CPR, this oldest age group was less likely to receive bystander CPR compared with younger groups even though compression‐only CPR is seemingly simpler to instruct and subsequently perform. The decrease in CPR among the oldest age group appeared to be a function of a lower frequency of T‐CPR, despite telecommunicator attempts to deliver instructions regardless of age. Patients in the 9‐ to 17‐year age group more frequently presented with hanging and drowning than their younger counterparts (22% versus 4%), causes that create patient access and patient positioning challenges, which may influence CPR performance. Whether specific training can address this opportunity to improve T‐CPR in older pediatric patients is unclear, though challenges with cause‐specific patient access likely influence the rate of T‐CPR delivery in this group.
The study has limitations. The investigation was conducted in a large metropolitan region with a mature EMS system that includes a coordinated T‐CPR program and a relatively favorable neurologically intact survival outcome. Although the patient characteristics (ie, distribution of age and proportion with a shockable rhythm) are similar to other pediatric cohorts with OHCA, the system and outcome characteristics may indicate that T‐CPR in the current investigation may represent a relatively more practiced or expert performance, a feature that could limit generalizability. Audio recordings were not available in 17.8% (n=41). We did not have an a priori hypothesis that missingness of the recording was related to CPR measures. However, we did observe bystander CPR was somewhat less common among the missing group, though this may simply be due to the more limited information sources to ascertain bystander CPR status when a recording is not available. The use of the audio recording to ascertain key information is helpful but can present challenges. For example, the details of bystander CPR performance and onset of first CPR intervention required verbalization. However, when CPR was unassisted, there was less verbalization and hence the onset of unassisted CPR may have occurred earlier, making the reported interval to CPR an overestimate of true performance among the unassisted CPR group. Finally, the investigation was not designed to evaluate survival outcome relationships. Such a study would require a larger sample size to support multivariable regression to understand the independent outcome relationships with bystander CPR and specifically T‐CPR.
CONCLUSIONS
In this cohort of pediatric OHCAs, T‐CPR was an important strategy to achieve timely arrest recognition and bystander CPR performance. Measurement and consequent performance metrics can support efforts aimed at improving bystander CPR and in turn pediatric OHCA survival.
Sources of Funding
None.
Disclosures
None.
Supporting information
Table S1
Acknowledgments
We want to acknowledge the dedicated efforts of the telecommunicators and EMS professionals of King County and their ongoing efforts to improve the care delivered to the communities they serve.
This article was sent to Dianne L. Atkins, MD, Guest Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.123.031740
For Sources of Funding and Disclosures, see page 9.
References
- 1. Atkins DL, Everson‐Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, Berg RA; The Resuscitation Outcomes Consortium Investigators . Epidemiology and outcomes from out‐of‐hospital cardiac arrest in children: the resuscitation outcomes consortium Epistry—cardiac arrest. Circulation. 2009;119:1484–1491. doi: 10.1161/CIRCULATIONAHA.108.802678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fink EL, Prince DK, Kaltman JR, Atkins DL, Austin M, Warden C, Hutchinson J, Daya M, Goldberg S, Herren H, et al. Unchanged pediatric out‐of‐hospital cardiac arrest incidence and survival rates with regional variation in North America. Resuscitation. 2016;107:121–128. doi: 10.1016/j.resuscitation.2016.07.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker‐Smith CM, Beaton AZ, Boehme AK, Buxton AE, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation. 2023;147:e93–e621. doi: 10.1161/CIR.0000000000001123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL, Lasa JJ, Lavonas EJ, Levy A, Mahgoub M, et al. Part 4: Pediatric Basic and Advanced Life Support: 2020 guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S469–S523. doi: 10.1542/peds.2020-038505D [DOI] [PubMed] [Google Scholar]
- 5. Goto Y, Maeda T, Goto Y. Impact of dispatcher‐assisted bystander cardiopulmonary resuscitation on neurological outcomes in children with out‐of‐hospital cardiac arrests: a prospective, nationwide, population‐based cohort study. J Am Heart Assoc. 2014;3:e000499. doi: 10.1161/JAHA.113.000499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Akahane M, Ogawa T, Tanabe S, Koike S, Horiguchi H, Yasunaga H, Imamura T. Impact of telephone dispatcher assistance on the outcomes of pediatric out‐of‐hospital cardiac arrest. Crit Care Med. 2012;40:1410–1416. doi: 10.1097/CCM.0b013e31823e99ae [DOI] [PubMed] [Google Scholar]
- 7. Bobrow BJ, Spaite DW, Vadeboncoeur TF, Hu C, Mullins T, Tormala W, Dameff C, Gallagher J, Smith G, Panczyk M. Implementation of a regional telephone cardiopulmonary resuscitation program and outcomes after out‐of‐hospital cardiac arrest. JAMA Cardiol. 2016;1:294–302. doi: 10.1001/jamacardio.2016.0251 [DOI] [PubMed] [Google Scholar]
- 8. Rea TD, Eisenberg MS, Culley LL, Becker L. Dispatcher‐assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation. 2001;104:2513–2516. doi: 10.1161/hc4601.099468 [DOI] [PubMed] [Google Scholar]
- 9. Kurz MC, Bobrow BJ, Buckingham J, Cabanas JG, Eisenberg M, Fromm P, Panczyk MJ, Rea T, Seaman K, Vaillancourt C. On behalf of the American Heart Association advocacy coordinating committee. Telecommunicator cardiopulmonary resuscitation: a policy statement from the American Heart Association. Circulation. 2020;141:e686–e700. doi: 10.1161/CIR.0000000000000744 [DOI] [PubMed] [Google Scholar]
- 10. Perkins GD, Jacobs IG, Nadkami VM, Berg RA, Bhanji F, Biarent D, Bossaert LL, Brett SJ, Chamberlain D, de Caen AR, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out‐of‐hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association emergency cardiovascular care committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132:1286–1300. [DOI] [PubMed] [Google Scholar]
- 11. Culley LL, Clark JJ, Eisenberg MS, Larsen MP. Dispatcher‐assisted telephone CPR: common delays and time‐standards for delivery. Ann Emerg Med. 1991;20:362–366. doi: 10.1016/S0196-0644(05)81655-5 [DOI] [PubMed] [Google Scholar]
- 12. Fujie K, Nakata Y, Yasuda S, Mizutani T, Hashimoto K. Do dispatcher instructions facilitate bystander‐initiated cardiopulmonary resuscitation and improve outcomes in patients with out‐of‐hospital cardiac arrest? A comparison of family and non‐family bystanders. Resuscitation. 2014;85:315–319. doi: 10.1016/j.resuscitation.2013.11.013 [DOI] [PubMed] [Google Scholar]
- 13. Song KJ, Shin SD, Park CB, Kim JY, Kim DK, Kim CH, Ha SY, Eng Hock Ong M, Bobrow BJ, McNally B. Dispatcher‐assisted bystander cardiopulmonary resuscitation in a metropolitan city: a before—after population‐based study. Resuscitation. 2014;85:34–41. doi: 10.1016/j.resuscitation.2013.06.004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


