Abstract
Objective:
We examined the association between utilization of care for a dental problem (utilization-DP) and parent-reported dental problem (DP) urgency among children with DP by type of health care insurance coverage.
Methods:
We used weighted 2008 National Health Interview Survey data from 2,834 children, aged 2–17 years with at least one DP within the 6 months preceding survey. Explanatory variables were selected based on Andersen’s model of healthcare utilization. Need was considered urgent if DP included toothache, bleeding gums, broken or missing teeth, broken or missing filling, or decayed teeth and otherwise as non-urgent. The primary enabling variable, insurance, had four categories: none, private health no dental coverage (PHND), private health and dental (PHD), or Medicaid/State Children’s Health Insurance Program (SCHIP). Predisposing variables included sociodemographic characteristics. We used bivariate and multivariate analyses to identify explanatory variables’ association with utilization-DP. Using logistic regression, we obtained adjusted estimates of utilization-DP by urgency for each insurance category.
Results:
In bivariate analyses, utilization-DP was associated with both insurance and urgency. In multivariate analyses, the difference in percent utilizing care for an urgent versus non-urgent DP among children covered by Medicaid/SCHIP was 32 percentage points; PHD, 25 percentage points; PHND, 12 percentage points; and no insurance, 14 percentage points. The difference in utilization by DP urgency was higher for children with Medicaid/SCHIP compared with either PHND or uninsured children.
Conclusion:
Expansion of Medicaid/SCHIP may permit children to receive care for urgent DPs who otherwise may not, due to lack of dental insurance.
Keywords: dental problem, utilization, dental care for children, health insurance, dental insurance, dental health services, Medicaid/SCHIP
Introduction
The burden of dental disease and factors associated with utilization of dental care for any reason among children, including the roles of dental insurance and sociodemographic characteristics, have been well documented (1–3). However, few studies have examined the role of health insurance – with or without dental coverage – in children’s utilization of dental care specifically for a dental problem, while also accounting for urgency of the dental problem for which care was sought and the influence of sociodemographic characteristics. Although oral health is considered an integral part of general health, almost one in six US children and adolescents aged 5–19 years have untreated dental decay (1). If left untreated, dental decay can lead to pain and infections and ultimately to problems in eating, playing, and learning (2). Routine use of dental services can both prevent the occurrence and progression of dental decay and contribute to maintaining a child’s overall health and well-being (3).
Utilization of health care including dental care, can be explained largely by a conceptual model developed by Andersen (4). This model hypothesizes that health care utilization is influenced by the presence of a) predisposing characteristics, e.g., sociodemographic characteristics that influence an individual’s valuation of health and knowledge of the benefits of health care; b) enabling resources such as those that support the individual to pursue and achieve good health, and c) the need for care, which is defined by the individual’s perceptions of necessary preventive interventions or treatments. Studies have confirmed the predictive power of these variables on dental utilization. For example, several studies have found that predisposing characteristics, such as oral health literacy, geographic location, higher parental education, and being non-Hispanic white, were associated with higher dental utilization among children (3,5–8). Studies have also documented that dental care utilization is higher in the presence of enabling characteristics such as higher family income and having dental or health insurance (7–9). The Rand Health Insurance Experiment, which randomly assigned families to a variety of insurance plans, found that the demand for dental services increased by reducing the level of cost-sharing. Participants whose insurance plan paid all of their dental care cost had 34 percent more visits, compared with enrollees whose plan paid only 5 percent of their dental costs (10). Because private dental insurance typically covers a higher share of cost for preventive services compared with restorative services (11,12), the influence of private dental insurance on dental utilization for a dental problem could, to the extent that patients can accurately predict their need for restorative care, vary by type of care needed. Medicaid/SCHIP on the other hand, covers 100 percent of the cost for medically necessary caries-related restorative procedures through the Early and Periodic Screening, Diagnostic, and Treatment Program, as well as preventive services (13).
While the impact of enabling and predisposing variables on dental utilization has been examined, less is known about the influence of need on utilization. The most recent study using data from the 2007 National Survey of Children’s Health found that children aged 3–17 years with a parent-reported dental need (toothache, decayed teeth or cavities, broken teeth, or bleeding gums) were more likely to have had a preventive dental visit in the past 12 months than were children without such need (14). By contrast, an analysis of data from the 1988–1994 National Health and Nutrition Examination Survey (NHANES) found that children aged 6–18 years with perceived dental needs (i.e., perceived by child or responsible adult) or normative dental need (clinically examined by dentist) were less likely to have had a previous-year dental visit than children with no needs had (15).
These two studies used data collected more than decade apart. Changes in oral health literacy or awareness in recent years could be one reason for their contrasting findings. However, one potential limitation of both of these studies was that the questions on dental need and dental utilization were asked in such a way that the timing of the dental visit relative to the onset of the dental problem was unknown. For example, if the dental visit occurred first and appropriate treatment services were received, then it would not be surprising that dental visits were associated with fewer unmet treatment needs. Alternatively, if the patient or caregiver became aware of the child’s treatment needs at an earlier dental visit, but treatment services were not received at that visit, then the dental visit may not be associated with fewer reported treatment needs. The 2008 National Health Interview Survey (NHIS) offers a unique opportunity to examine the association between dental need and utilization of care for a dental need, because NHIS first asks parents of participating children whether the children had any dental problems within the 6 months preceding the survey, and if yes, what types of dental problems and whether they obtained care for any of the reported problems.
In this study of children’s dental needs and utilization of care for dental needs, we first examined whether urgency of dental problem was associated with subsequent utilization of care for a reported problem, controlling for other factors. Second, we examined whether the association between dental problem urgency and utilization of care was modified by type of health insurance, and presence of dental coverage.
Methods
Data source
We used publically available data from the 2008 NHIS and its child oral health supplement, which was the first large scale dental supplement to the NHIS since 1989. Conducted by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention, the NHIS supports national estimates of health status and health care access and utilization for the civilian, non-institutionalized, US population (16). Data are collected annually through an in-person household interview. In the 2008 NHIS, a parent or adult household member responded for the sampled child. Family, person, and child files were merged to create the analysis dataset. The conduct of the NHIS was approved by the NCHS research ethics review board. This study used deidentified, publically released NHIS data and did not require separate institutional review board approval.
Study population
Our study population included children aged 2–17 years whose parents responded yes, that during the past 6 months the child had at least one of the following dental problems (DPs): toothache or sensitive teeth, pain in jaw joint, sores in mouth, bleeding gums, crooked teeth, broken, or missing teeth other than losing baby teeth, stained or discolored teeth, loose teeth not due to injury or losing baby teeth, decayed teeth or cavities, broken or missing fillings, bad breath, or dry mouth. Parents could report more than one DP for the child. A maximum of 12 DP per child were recorded in the data set. Children with no reported problems were excluded from the analysis.
Dependent variable
Our dependent variable was utilization of care for a dental problem (hereon referred to as utilization-DP). Parents who reported that their child had at least one dental problem (DP) within the last 6 months were asked, “During the past 6 months, did the ‘sample child’ see a dentist or a medical doctor for any problems with his/her mouth or teeth?”
Independent variables
We used Andersen’s predisposing, enabling, and need model of health care service use for selecting independent variables (4).
Need
We categorized a child as having an urgent need if reported DPs for that child included decayed teeth or cavities, toothache or sensitive teeth, bleeding gums, or broken or missing teeth or fillings, and otherwise, as non-urgent need (pain in jaw joint, sores in mouth, crooked teeth, stained or discolored teeth, loose teeth not due to injury or losing baby teeth, bad breath, or dry mouth). This categorization of DP urgency is consistent with the definition of “dental care need” and “acute dental care need” used in previous reports (14,15) and the urgent dental referral recommendation categories from NHANES (for example, tooth fracture, lost restoration, chronic pain, etc.) (17). Hereon, this variable will be referred to as urgency.
Enabling variables
We created four categories of health care insurance coverage: a) no insurance, b) private health but no dental (PHND), c) private health and dental (PHD), and d) Medicaid/State Children’s Health Insurance Program (SCHIP).
Children who had any type of health insurance other than Medicaid/SCHIP were considered to have private health insurance; presence of dental coverage was also assessed. Based on presence or absence of dental insurance, these children were categorized as having PHD or PHND. A question about single service plans that covered dental care (i.e., standalone dental insurance) was also asked. However, in our study sample, fewer than five children were reported to have standalone dental insurance but no health insurance and were excluded from the analysis.
Our second enabling variable was family income. We used the ratio of family income to the federal poverty level (FPL) divided into four categories: <100 percent FPL, 100–199 percent FPL, 200–299 percent FPL, and ≥300 percent FPL.
Predisposing variables
These included age group (2–5, 6–11, and 12–17 years), sex, birthplace (US-born, foreign born), race/ethnicity [Hispanic, non-Hispanic white (NH white), non-Hispanic black (NH black), non-Hispanic Asian (NH Asian), non-Hispanic other (NH other)], and parents’ education level as the higher of either parent’s highest completed level of education [<high school (HS), HS graduate/General Educational Development (GED), some college, and college graduate or higher].
Region variable
The US regions of residence were categorized as Northeast, Midwest, West, and South. This variable captures the otherwise unmeasured effect of other predisposing (e.g., value placed on oral health) and enabling (e.g., supply of dental services, reimbursement rates and dental fees) variables that can vary by region and were not assessed in the 2008 NHIS survey or supplement.
Statistical analyses
All analyses were conducted using SAS-callable SUDAAN (Release 11.0, Research Triangle Institute, Research Triangle Park, NC) to account for survey weighting and to adjust the variance for the multistage, clustered survey design. Estimates calculated from fewer than 50 observations or with more than 30 percent relative standard error were considered statistically unstable.
We used a chi-square test of independence to examine whether urgency and utilization-DP differed by other independent variables. We used the Cochran-Mantel-Haenszel test to determine whether the association between utilization-DP and urgency varied among categories of each of the other independent variables. We also assessed whether or not urgent problems differed by insurance status, in unadjusted analyses and when adjusted for sociodemographic variables.
To examine the association between utilization-DP and urgency, simultaneously controlling for health insurance coverage, sociodemographic characteristics, and family income, we used logistic regression. In the regression, we included a term for interaction between insurance and urgency to examine if insurance modified this association. Wald F tests were used to assess whether explanatory variables were independently associated with the outcome in multivariable logistic regression models. We also tested for multicollinearity among variables using the Variance Inflation Factor (VIF) and tolerance statistic. The Hosmer-Lemeshow (HL) test was used to assess goodness of fit for the logistic regression model. Average marginal predictions of utilization-DP for various combinations of insurance coverage and urgency were also obtained from the regression model. To test for differences in the average marginal predictions, we used a t-test. Only statistically significant findings (P≤0.05) are reported unless stated otherwise.
Results
Study sample
The final study sample included 2,834 children aged 2–17 years with ≥1 DP who had complete data for utilization-DP and insurance. For multivariate analyses, only three race/ethnicity groups were included (non-Hispanic white, non-Hispanic black, and Hispanic) because the sample sizes were too small to produce reliable estimates for non-Hispanic Asian and non-Hispanic other groups. Multivariate analyses included data from 2,282 children.
Unadjusted analyses
Among children with at least one reported DP, 61.3 percent reported urgent DP (n=1,782). Among children with an urgent DP, a majority reported cavities (64 percent) or toothaches (52 percent), and among those with only non-urgent DP, more than half reported crooked teeth (55 percent) (Figure 1).When DP was stratified by insurance status among children with any urgent DP, the percentages of children with cavities ranged from 56.9 percent (PHND) to 69.6 percent (Medicaid/SCHIP) for cavities, and from 50 percent (PHD and PHND) to 58.2 percent (uninsured) (Figure 2). Overall, 54 percent of children with a DP utilized care within the 6 months preceding survey for a DP. Of those, 95.6 percent visited a dentist, 1.9 percent visited a medical provider, and 2.5 percent visited both a dentist and medical provider (data not shown). Children with urgent DP had higher utilization of dental care for all sociodemographic, income, and insurance groups compared to their counterparts with non-urgent DP (Table 1).
Figure 1.

Distribution of reported dental problems (DP) in the past six months among children aged 2–17 years with any urgent DP and only non-urgent DP – United States, 2008. Percentages do not sum to 100% because more than one DP could be reported for each child. Urgent DP – Children with at least one urgent problem reported. Non-urgent DP – Children with no urgent problems reported.
Figure 2.
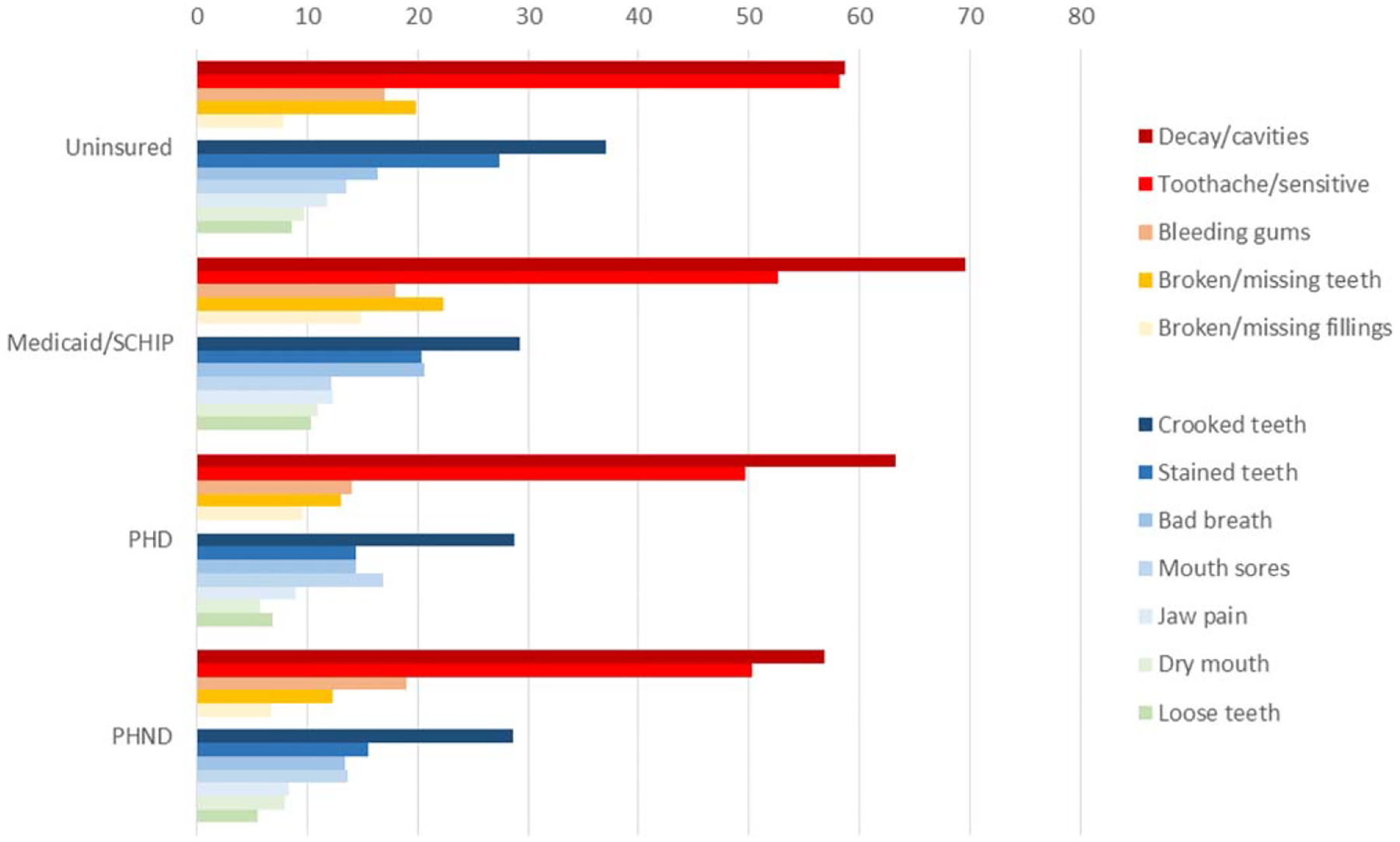
Percentage of children aged 2–17 years with specific types of dental problems (DP) in the past six months among children with at least one urgent DP, by type of insurance – United States, 2008. Percentages do not sum to 100% because more than one DP could be reported for each child. Urgent DP – cavities/decay, toothache, bleeding gums, broken/missing teeth, broken/missing restoration.
Table 1.
Utilization of Care for a Reported Dental Problem (DP) Among Children 2–17 Years of Age by Problem Urgency and Selected Characteristics – United States, 2008
| Characteristics | Percentage of children with DP who utilized care for a DP | ||||
|---|---|---|---|---|---|
| Overall % SE | P * | Urgent DP % SE | Non-urgent DP % SE | P † | |
| Total | 54.0 1.2 | 62.2 1.4 | 41.0 1.9 | <0.001 | |
| Age (years) | 0.171 | ||||
| 2–5 | 50.5 2.7 | 64.2 3.4 | 27.0 4.0 | ||
| 6–11 | 53.3 1.8 | 61.6 2.3 | 38.8 3.0 | ||
| 12–17 | 56.2 1.7 | 61.9 2.1 | 48.5 2.7 | ||
| Sex | 0.615 | <0.001 | |||
| Male | 53.4 1.6 | 62.7 1.9 | 40.1 2.6 | ||
| Female | 54.6 1.6 | 61.7 1.9 | 42.1 2.6 | ||
| Place of birth | 0.168 | <0.001 | |||
| US born | 54.3 1.2 | 62.6 1.5 | 41.4 1.9 | ||
| Foreign born | 46.2 5.5 | 53.2 6.0 | 30.4 7.8 | ||
| Region | 0.080 | <0.001 | |||
| Northeast | 58.6 2.6 | 62.6 3.0 | 52.2 4.9 | ||
| Midwest | 50.3 2.4 | 57.0 3.1 | 39.9 3.9 | ||
| South | 56.0 1.9 | 65.0 2.3 | 41.8 3.0 | ||
| West | 52.2 2.4 | 63.4 2.9 | 34.1 3.9 | ||
| Race/Ethnicity | 0.519 | <0.001 | |||
| Hispanic | 51.6 2.2 | 58.5 2.6 | 37.3 3.4 | ||
| NH‡ white | 53.9 1.6 | 62.8 2.1 | 42.5 2.4 | ||
| NH black | 56.1 2.8 | 64.2 3.1 | 36.9 5.4 | ||
| NH Asian | 57.9 5.3 | 64.4 6.8 | 45.2 7.9 | ||
| NH all other race§ | 62.7 12.2 | 69.4 12.0 | 45.7 21.6 | ||
| Parent’s education | <0.001 | <0.001 | |||
| <HS | 44.8 3.1 | 48.9 3.6 | 34.3 5.5 | ||
| HS/GED | 47.2 2.6 | 54.8 3.3 | 34.6 4.1 | ||
| Some college | 53.7 2.0 | 61.6 2.4 | 41.4 3.2 | ||
| College or higher | 62.5 1.8 | 75.1 2.4 | 46.6 3.0 | ||
| Family income | <0.001 | <0.001 | |||
| <100% | 46.0 3.0 | 53.0 3.3 | 29.3 5.6 | ||
| 100–199% | 47.8 2.5 | 55.4 3.1 | 31.3 4.1 | ||
| 200–299% | 55.5 3.1 | 67.5 3.5 | 35.8 4.7 | ||
| ≥300% | 60.9 1.7 | 71.0 2.2 | 49.9 2.8 | ||
| Insurance status | <0.001 | <0.001 | |||
| No insurance | 26.8 3.1 | 30.3 3.8 | 17.9 4.4 | ||
| PHND | 55.7 2.8 | 60.3 3.8 | 49.2 4.3 | ||
| PHD | 57.6 1.6 | 68.2 2.1 | 44.8 2.7 | ||
| Medicaid/SCHIP | 56.4 2.2 | 66.4 2.5 | 33.3 3.8 | ||
SCHIP, State Children’s Health Insurance Program; PHD, Private health insurance and private dental insurance; PHND, Private health insurance and no private dental insurance.
Chi-square test of independence.
Cochran-Mantel-Haenszel test of homogeneity of association among strata.
Non-Hispanic.
Estimate is statistically unstable (RSE >30 percent or denominator n <50).
Adjusted analyses
The odds of having cavities, toothache, or any of the other urgent problems, were not associated with insurance category after adjustment for sociodemographic characteristics. Multicollinearity among selected predisposing and enabling variables included in the multivariable logistic regression model was low (VIF<2), thus all variables were retained in the full model (Table 2). In this adjusted model, utilization-DP was associated with urgency, however, the strength of the association varied by insurance category. Urgency was strongly associated with utilization-DP among children with Medicaid/SCHIP [odds ratio (OR)=4.28, 95 percent confidence interval (CI)=2.73–6.71], followed by those with PHD (OR=3.00, 95 percent CI=2.13–4.23). (Table 2).
Table 2.
Adjusted Odds Ratio for Utilization for a Reported Dental Problem (DP) Among Children Aged 2 to 17 Years with a DP in Past 6 Months – United States, 2008
| Full model with interaction term Variables | Odds ratio | 95% confidence interval | P* |
|---|---|---|---|
| Combined effect of Insurance status and dental problem urgency | |||
| No insurance, Urgent versus Non-urgent DP | 2.07 | 0.96–4.46 | 0.064 |
| PHND, Urgent versus Non-urgent DP | 1.69 | 1.00–2.84 | 0.049 |
| PHD, Urgent versus Non-urgent DP | 3.00 | 2.13–4.23 | <0.001 |
| Medicaid/SCHIP, Urgent versus Non-urgent DP | 4.28 | 2.73–6.71 | <0.001 |
| Age (years) | 0.054 | ||
| 2–5 | Reference | ||
| 6–11 | 0.98 | 0.73–1.31 | |
| 12–17 | 1.26 | 0.96–1.66 | |
| Sex | 0.691 | ||
| Male | Reference | ||
| Female | 0.96 | 0.78–1.18 | |
| Place of birth | 0.754 | ||
| US born | Reference | ||
| Foreign born | 0.92 | 0.54–1.57 | |
| Region | 0.020 | ||
| South | Reference | ||
| Northeast | 1.07 | 0.77–1.48 | |
| Midwest | 0.75 | 0.58–0.98 | |
| West | 0.70 | 0.52–0.95 | |
| Race/Ethnicity | 0.238 | ||
| Hispanic | Reference | ||
| NH† white | 0.80 | 0.62–1.04 | |
| NH black | 0.94 | 0.68–1.29 | |
| Parental education | 0.004 | ||
| <HS | Reference | ||
| HS/GED | 1.00 | 0.68–1.47 | |
| Some college | 1.31 | 0.90 −1.88 | |
| College or higher | 1.70 | 1.13–2.56 | |
| Family income | <0.001 | ||
| <100% | Reference | ||
| 100–199% | 1.26 | 0.89–1.79 | |
| 200–299% | 1.72 | 1.17–2.52 | |
| ≥300% | 2.29 | 1.55–3.39 |
SCHIP, State Children’s Health Insurance Program; PHD, Private health insurance and private dental insurance; PHND, Private health insurance and no private dental insurance.
P values from Wald F test.
Non-Hispanic.
Based on the regression model, the percent of children with only non-urgent DPs who utilized care was lower among those with no insurance (22.9 percent) compared with those covered by PHND (47.4 percent), Medicaid/SCHIP (41.8 percent) or PHD (37.8 percent); however, differences between PHND, PHD, and Medicaid/SCHIP were not statistically significant (Figure 3). Utilization-DP for urgent DPs was higher among Medicaid/SCHIP (73.9 percent) enrolled children compared with their counterparts who had no insurance (37.2 percent), PHND (59.6 percent) or PHD (63.2 percent) (Figure 3). Utilization-DP for urgent DPs was also higher among children with PHND and PHD compared with uninsured children (Figure 3).
Figure 3.

Utilization for a dental problem (utilization-DP) among children with any urgent dental problem (DP) and only non-urgent DP by insurance category – United States, 2008. SCHIP, State Children’s Health Insurance Program; PHD, Private health insurance and private dental insurance; PHND, Private health insurance and no private dental insurance; Urgent DP, Children with at least one urgent problem reported; Non-urgent DP, Children with no urgent problems reported. *Difference in utilization between urgent and non-urgent dental problem, T test≤0.05 for all insurance categories. Among children with an urgent dental problem, T test P≤0.05 for no insurance vs Medicaid/SCHIP, PHD or PHND, and PHND or PHD versus Medicaid/SCHIP. Among children with a non-urgent dental problem, T test P≤0.05 for no insurance vs Medicaid/SCHIP, PHD or PHND. Difference in difference of utilization between urgent and non-urgent dental problem, T test≤0.05 for Medicaid/SCHIP vs no insurance (32.1%–14.3%) or PHND (32.1–12.2%).
Among children with Medicaid/SCHIP, the percentage of children with an urgent DP who utilized care was 32.1 percentage points higher than among those with only non-urgent DP, 25.3 percentage points higher among PHD, 12.2 percentage points higher among PHND, and 14.3 percentage points higher among uninsured children (Figure 3). This difference in utilization-DP by urgency was almost 20 percentage points greater among children with Medicaid/SCHIP compared with children with PHND or no insurance (32.1 versus 12.2 and 14.3 percentage points, respectively). The difference by urgency was 13 percentage points higher among children with PHD compared with those with PHND (25.3 versus 12.2 percentage points) but was not statistically significant (P=0.073) (Figure 3).
Children with a college-educated parent were 1.7 times more likely to utilize care for a DP than their counterparts whose parents had less than a HS education. Compared with children living in a family with income below 100 percent FPL, those living in families with incomes ≥300 percent FPL (OR=2.29) or between 200–299 percent FPL (OR=1.73) were more likely to utilize care for a DP.
Discussion
After controlling for covariates, we found that for both categories of urgency, children with some type of health insurance, either medical and/or dental, were more likely to utilize care compared with children with no insurance. Utilization-DP was higher among children with an urgent DP versus non-urgent DP for all insurance categories. Among insured children with urgent DP, utilization-DP varied by type of insurance – children with Medicaid/SCHIP had higher utilization than those with PHND or PHD. Finally, we found that the difference in utilization by urgency was larger for children covered by Medicaid/SCHIP compared with children with no dental insurance (i.e., non-insured and those with private health but no dental insurance).
The types of DPs in the urgent category were more commonly caries-related compared with those in the non-urgent category where orthodontic needs were the most frequently reported. For caries-related urgent problems, it is likely that Medicaid/SCHIP would be the most enabling (i.e., no copayment), followed by PHD, then PHND, and finally no insurance (12,13). To the extent that non-urgent problems represented orthodontic needs, it is likely that PHD would be more enabling (e.g., some copayment or discounted fee for orthodontics) than the other three insurance categories in which patients usually must pay the full cost of orthodontic services, if they are not considered medically necessary (12,18). This may be why the difference in utilization-DP by urgency was greater for Medicaid/SCHIP than for PHND and no insurance – Medicaid was most enabling among children with urgent DP and only about as enabling as PHD and PHND among children with a non-urgent DP.
Our findings suggest that among children with a DP, urgency of need can increase utilization of dental care and enabling resources can modify utilization significantly. Insurance can be enabling in two ways. First, dental insurance lowers the price that patients pay because it reduces their out-of-pocket expenses. Studies have confirmed that demand for dental care is sensitive to price (10,19). Second, the lower out-of-pocket cost for dental and medical services, due to having dental and health insurance, results in families having more discretionary income (10,19). Medicaid/SCHIP was found to be more enabling than PHD for urgent DP. Previous studies have also shown that dental utilization increases in the presence of either dental or health insurance (7,8,11). The current study may be the first to use child-level data to document the combined influence of need and enabling resources. It also may be the first to show the difference in utilization of dental care for a dental problem between two types of dental insurance – Medicaid/SCHIP and PHD
Our finding that children with one or more urgent DPs are more likely to utilize care when provided enabling resources may have implications for estimating demand for dental services. An earlier study noted that having an urgent DP is not uncommon (27 percent) (14), and the cost of providing care typically increases as needs become more urgent (20). Not taking these factors – urgency and costs of care – into account could result in underestimation of changes in short-run utilization attributable to expanding insurance coverage. Getting more children with urgent dental needs into care, however, could save resources in the long run, as delay in treatment could result in higher treatment costs per child and more emergency visits among those with no dental insurance. The most common non-traumatic conditions for emergency dental visits are caries related such as those mentioned in our urgent dental problem category (21). Our results found that utilization-DP among children without dental insurance (no insurance or PHND) was low suggesting that these children could benefit from dental benefits received through Medicaid expansion.
Another interesting finding was that predisposing variables, with the exception of parent education equaling college or greater, were not associated with utilization-DP among children with a reported DP. Previous studies have found an association between dental utilization and predisposing characteristics such as age, race/ethnicity, sex, and birthplace (2,5,6) for preventive or routine care. It may be that parents, regardless of sociodemographic characteristics, are “predisposed” to take their child with an urgent DP to the dentist and thus, in the presence of urgent need, enabling resources may be the most important drivers of dental utilization.
A limitation of this study was that the dental problem used to define urgency was parent-reported, and thus could be underreported relative to dentist-assessed treatment needs if parents were not fully aware of their child’s oral health status (22). Even though the questions used in this study were designed to measure dental utilization for a reported dental problem, we cannot assess if the parent correctly identified the dental problems nor whether the parents became aware of the problems from an earlier dental visit. Also, utilization of dental care in the past six months for a dental problem may not be accurately reported because of recall and social desirability biases, biases that may be shared in other parent-reported indicators of health status and health care utilization (23,24). Lastly, hypothesis tests were not adjusted for multiple comparisons. Future research may describe types and patterns of reported dental problems, and assess barriers to care among those who reported a dental problem but did not seek care, or sought but did not receive care.
Our study findings indicate that insurance modifies the relationship between dental problem urgency and utilization of care, and suggest that expansion of Medicaid/SCHIP may permit children to receive care for urgent DPs who otherwise may not, due to lack of dental insurance.
Acknowledgments
We acknowledge excellent suggestions provided by Dr. Barbara Gooch with the Division of Oral Health at the Centers for Disease Control and Prevention.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and prevention.
References
- 1.Dye BA, Li X, Beltran-Aguilar ED. Selected oral health indicators in the united states, 2005–2008. NCHS Data Brief 2012;96:1–8. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. Oral health in America: a report of the surgeon general. Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- 3.Institute of Medicine and National Research Council. Improving access to oral health care for vulnerable and underserved populations. Washington, DC: National Academic Press; 2011. [Google Scholar]
- 4.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995;36(1):1–10. [PubMed] [Google Scholar]
- 5.Edelstein BL, Chinn CH. Update on disparities in oral health and access to dental care for America’s children. Acad Pediatr 2009;9(6):415–9. [DOI] [PubMed] [Google Scholar]
- 6.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics 2008;121(2):e286–98. [DOI] [PubMed] [Google Scholar]
- 7.Lewis C, Mouradian W, Slayton R, Williams A. Dental insurance and its impact on preventive dental care visits for US children. J Am Dent Assoc (1939) 2007; 138(3):369–80. [DOI] [PubMed] [Google Scholar]
- 8.Decker SL. Medicaid payment levels to dentists and access to dental care among children and adolescents. J Am Med Assoc 2011;306(2):187–93. [DOI] [PubMed] [Google Scholar]
- 9.Kenney MK, Kogan MD, Crall JJ. Parental perceptions of dental/oral health among children with and without special health care needs. Ambul Pediatr 2008;8(5):312–20. [DOI] [PubMed] [Google Scholar]
- 10.Manning WG, Bailit HL, Benjamin B, Newhouse JP. The demand for dental care: evidence from a randomized trial in health insurance. J Am Dent Assoc 1985;110(6):895–902. [DOI] [PubMed] [Google Scholar]
- 11.Meyerhoefer CD, Zuvekas SH, Manski R. The demand for preventive and restorative dental services. Health Econ 2014;23(1):14–32. [DOI] [PubMed] [Google Scholar]
- 12.Dental D. Plans & pricing options: delta dental of Idaho; 2015. [cited 2015 Oct 05]. Available from: https://secure.deltadentalid.com/IndividualPlan/plans.aspx
- 13.Centers for Medicare and Medicaid Services. Dental Care for Medicaid and CHIP Enrollees. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Benefits/Dental-Care.html
- 14.Bell JF, Huebner CE, Reed SC. Oral health need and access to dental services: evidence from the national survey of children’s health, 2007. Matern Child Health J 2012;16 Suppl 1:S27–34. [DOI] [PubMed] [Google Scholar]
- 15.Vargas CM, Ronzio CR. Relationship between children’s dental needs and dental care utilization: united states, 1988–1994. Am J Public Health 2002;92(11):1816–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NCHS C, National Center for Health Statistics Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. Data File Documentation. 2008 National Health Interview Survey, (NHIS) public use data release. Hyattsville, MD: NCHS; 2009. [Google Scholar]
- 17.CDC/National Center for Health Statistics. 2013–2014 National Health and Nutrition Examination Survey (NHANES). Oral Health Examiners Manual; 2014. [Google Scholar]
- 18.Blue Cross Blue Shield of Alabama. Dental Plans; 2015. Available from: https://www.ibcbsal.com/sales/compare-plans.
- 19.Liu S, Chollet D. Price and income elasticity of the demand for health insurance and health care services: a critical review of the literature. No. dbf03ba11863430593b0b825 fb48acc2. Mathematica Policy Research, Inc.; 2006. [Google Scholar]
- 20.Guay AH. The differences between dental and medical care: implications for dental benefit plan design. J Am Dent Assoc 2006;137(6):801–6. [DOI] [PubMed] [Google Scholar]
- 21.Lewis C, Lynch H, Johnston B. Dental complaints in emergency departments: a national perspective. Ann Emerg Med 2003;42(1):93–9. [DOI] [PubMed] [Google Scholar]
- 22.Weyant RJ, Manz M, Corby P, Rustveld L, Close J. Factors associated with parents’ and adolescents’ perceptions of oral health and need for dental treatment. Community Dent Oral Epidemiol 2007;35(5):321–30. [DOI] [PubMed] [Google Scholar]
- 23.Romaire MA, Bell JF, Huebner CE. Variations in children’s dental service use based on four national health surveys. Pediatrics 2012;130(5):e1182–e9. [DOI] [PubMed] [Google Scholar]
- 24.Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev 2006;63(2):217–35. [DOI] [PubMed] [Google Scholar]


