Abstract
Background:
General surgeons play an important role in the provision of trauma care in Canada and the current extent of their trauma experience during training is unknown. We sought to quantify the operative and nonoperative educational experiences among Canadian general surgery trainees.
Methods:
We conducted a multicentre retrospective study of major operative exposures experienced by general surgery residents, as identified using institutional trauma registries and subsequent chart-level review, for 2008–2018. We also conducted a site survey on trauma education and structure.
Results:
We collected data on operative exposure for general surgery residents from 7 programs and survey data from 10 programs. Operations predominantly occurred after hours (73% after 1700 or on weekends) and general surgery residents were absent from a substantial proportion (25%) of relevant trauma operations. The structure of trauma education was heterogeneous among programs, with considerable site-specific variability in the involvement of surgical specialties in trauma care. During their training, graduating general surgery residents each experienced around 4 index trauma laparotomies, 1 splenectomy, 1 thoracotomy, and 0 neck explorations for trauma.
Conclusion:
General surgery residents who train in Canada receive variable and limited exposure to operative and nonoperative trauma care. These data can be used as a baseline to inform the application of competency-based medical education in trauma care for general surgery training in Canada.
Abstract
Contexte:
Les chirurgiennes et chirurgiens généralistes jouent un rôle important dans la prestation de soins de traumatologie au Canada, et l’étendue actuelle de leur expérience en traumatologie durant la formation est inconnue. Nous avons voulu quantifier les expériences pédagogiques opératoires et non opératoires chez les stagiaires en chirurgie générale du Canada.
Méthodes:
Nous avons mené une étude rétrospective multicentrique sur les expositions opératoires majeures que vivent les résidentes et résidents en chirurgie générale, repérées dans les registres de traumatologie des établissements et dans le cadre d’un examen subséquent des dossiers, pour la période de 2008–2018. Nous avons aussi mené une enquête sur la formation en traumatologie et la structure de celle-ci.
Résultats:
Nous avons recueilli des données sur l’exposition opératoire des résidentes et résidents en chirurgie générale de 7 programmes ainsi que des données d’enquête de 10 programmes. Les interventions chirurgicales avaient principalement lieu en dehors des heures normales (73 % après 17 h ou la fin de semaine), et les résidentes et résidents étaient absents d’une proportion considérable (25 %) des interventions de traumatologie pertinentes. La structure de la formation sur le sujet était hétérogène entre les programmes, avec une importante variation d’un établissement à l’autre dans la participation des spécialités chirurgicales dans les soins de traumatologie. Durant leur formation, les résidentes et résidents en chirurgie générale qui terminaient leurs études avaient chacun participé à environ 4 laparotomies initiales de traumatologie, 1 splénectomie, 1 thoracotomie et 0 exploration du cou pour un trauma.
Conclusion:
Les résidentes et résidents en chirurgie générale formés au Canada sont exposés de façon variable et limitée aux soins de traumatologie opératoires et non opératoires. Ces données peuvent servir de valeur de référence pour orienter l’application d’une formation médicale fondée sur les compétences en traumatologie dans la formation en chirurgie générale au Canada.
Traumatic injury is the leading cause of death and disability for Canadians aged 1–44 years.1 Care for the trauma patient is provided by a multitude of providers, most notably by general surgeons, who have long been involved in the resuscitation and stabilization of severely injured trauma patients requiring surgical care.2,3 This is of particular importance outside of major trauma centres, as most severely injured trauma patients are initially cared for in community hospitals.4 The ongoing provision of this vital trauma care is grounded in successfully training general surgery residents to be competent in this field.
The evolving landscape of trauma care, with increasing use of nonoperative and less-invasive treatment strategies, has raised important questions about the adequacy of operative trauma training. Existing research in this field is limited and predominantly comes from the experience in the United States, but raises concerns about the ability to train providers competent in trauma care, given the current educational landscape.5,6 In the Canadian context, there is a dearth of published information on operative trauma training exposure and concerns are similarly being raised.7,8 In addition, the methods by which we train our trauma care providers are changing with the introduction of the Competence by Design (CBD) initiative by the Royal College of Physicians and Surgeons of Canada (RCPSC),9 as part of the global shift to competency-based medical education. Although several benefits of this education approach have been demonstrated, its optimal adaptation into each specialty and training experience is still under development and has not been fully determined for trauma care.
We sought to quantify exposure to specific trauma surgery operations during residency and to perform an environmental scan of the nonoperative clinical exposure and other formal and informal trauma education provided to general surgery residents across Canadian training programs.
Methods
Our study methodology has been published previously.10 We invited 22 Canadian trauma centres associated with the 17 RCPSC general surgery training programs to participate. We asked each participating centre to complete both components of the study. Data were collected from study sites from 2019 to 2021.
The first component was the creation of a quantitative operative trauma exposure log by year of training, created using the institution’s trauma registry database. This identified all patients with trauma who underwent non-orthopedic, non-neurosurgical, and non-plastic surgical operations for injury during the study period (July 1, 2008, to June 30, 2018). Patient charts were abstracted to obtain details about the operations performed and the presence of trainees (residents and fellows). A comprehensive listing of general surgery residents in the residency program during the study period was created locally and used to cross-reference the operative reports to identify their postgraduate year of training at the time of each operation. In short, each site used their trauma registry to identify all patients who underwent operative treatment in the form of a neck exploration, thoracotomy or sternotomy, or laparotomy. These charts were then individually reviewed to extract the relevant operative details, as well as the details of which surgeons, fellows, and residents were present (using both the surgeon-dictated operative notes and the nursing-charted hospital operative records).
The second component was an environmental scan using a survey designed to elicit details regarding the typical general surgery resident’s clinical exposure to patients with trauma, as well as exposure to various forms of trauma teaching during residency. The survey was developed in an iterative fashion based on expert consensus by the members of the Canadian Collaborative on Urgent Care Surgery (CANUCS).11 It was pilot-tested, refined, and externally validated by representatives from multiple provinces. The full survey is available via the published study methodology.10
Our primary outcome was the volume and type of operative trauma cases to which general surgery residents were exposed throughout their postgraduate training in Canada. Secondary outcomes of interest included the timing of trauma operations and its relationship to resident participation, volume of trauma opportunities missed by residents, volume of operative trauma cases by type, and variability in experiences or exposure across participating sites, as well as comparison to existing minimums for operative trauma categories from the Accreditation Council for Graduate Medical Education (ACGME).12
Data analysis
We analyzed data using descriptive statistics, using frequencies and percentages for categorical variables and, for continuous varaibles, means and standard deviations (SDs) or medians with interquartile ranges (IQRs) for those with skewed distributions. We calculated 95% confidence intervals (CIs) where appropriate. We used the Cochran–Mantel–Haenszel test to examine the temporal trends in resident surgical involvement and time of day of the operation. We performed analyses using SPSS version 28.0 (IBM Corp.) and SAS software, version 9.4 (SAS Institute).
Ethics approval
Approval for the study was obtained from the Hamilton Integrated Research Ethics Board (REB), and each participating site obtained local REB approval. We implemented data sharing agreements with each site as required. The data from each study site were anonymized to conceal the identity of the site as specified by REBs and data sharing agreements. As per these agreements, not all data elements were able to be collected from all sites and some data have been presented in aggregate format only.
Results
Of the approached programs, 10 centres were able to complete the site survey on trauma education exposures. For the operative trauma exposure log, 8 centres contributed patient-record level data, although 1 centre could only provide data for 4 years of the 10-year study period, and another centre provided only descriptive statistics on the aggregate 10-year study period.
Participating institutions and their relevant characteristics regarding trauma exposure are presented in Table 1. The cohort for analysis included 528 individual residents contributing 1945 resident-years; 203 residents completed their general surgery residency during the study period. A total of 2151 abdominal, 510 thoracic, and 231 neck operations for trauma were performed during the study.
Table 1.
Trauma exposure characteristics by study site
| Characteristic | No. per study site* | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | J | K | Total | |
| Trauma centre characteristics, per annum† | |||||||||||
| Total trauma admissions | 471 | 856 | 503 | 265 | 554 | 913 | 509 | 850 | 800 | NR | 5617 |
| No. (%) of trauma admissions by ISS | |||||||||||
| ISS 9–12 | 208 (44.2) | 19 (22.2) | NR | 59 (22.3) | 129 (23.3) | 286 (31.3) | 76 (14.9) | 5 (0.6) | 91 (11.4) | NR | 1044 |
| ISS 13–15 | 54 (11.5) | 119 (13.9) | 175 (34.8) | 59 (22.3) | 87 (15.7) | 127 (13.9) | 73 (14.3) | 146 (17.0) | 128 (16.0) | NR | 968 |
| ISS 16–24 | 113 (24.0) | 265 (31.0) | 213 (42.3) | 84 (31.7) | 193 (34.8) | 235 (25.7) | 207 (40.7) | 413 (48.1) | 295 (36.9) | NR | 2018 |
| ISS ≥ 25 | 96 (20.4) | 282 (32.9) | 115 (22.9) | 63 (23.8) | 145 (26.2) | 265 (29.0) | 153 (30.1) | 286 (33.3) | 286 (35.6) | NR | 1691 |
| Total trauma team activations | 471 | 745 | 503 | 265 | 554 | 913 | 509 | 1114 | 800 | NR | 5874 |
| Resident characteristics | |||||||||||
| Total residents reported | 58 | 109 | NR | 49 | 78 | NR | 78 | 64 | 92 | NR | 528 |
| Total resident-years reported | 230 | 380 | NR | 181 | 295 | NR | 305 | 171 | 383 | NR | 1945 |
| Total graduating residents | 30 | 42 | NR | 20 | 35 | NR | 35 | NR | 41 | NR | 203 |
| Residents with 0 cases in cohort | 1 | 5 | NR | 1 | 1 | – | 2 | – | 0 | NR | 10 |
| Residents with > 0 cases in cohort | 29 | 37 | NR | 19 | 34 | – | 33 | – | 41 | NR | 193 |
| Trauma operation characteristics | |||||||||||
| Abdominal, any type | 136 | 422 | NR | 108 | 378 | NR | 265 | 326 | 516 | NR | 2151 |
| Thoracic, any type | 35 | 97 | NR | 11 | 96 | NR | 51 | 46 | 174 | NR | 510 |
| Neck, any type | 20 | 45 | NR | 17 | 44 | NR | 24 | 16 | 65 | NR | 231 |
ISS = Injury Severity Score; NR = not reported.
Unless indicated otherwise. All programs provided 10 years of data (2008–2018), except for program H, which provided 4 years of data (2014–2018).
As per most recent calendar year of trauma centre data available.
Overall volumes of trauma operation cases at each study site and the presence of general surgery residents at trauma operations are presented in Table 2. Presence of general surgery residents at abdominal operations ranged from 60.9%–97.2%, with a mean of 80.6%. For thoracic operations the range was 62.1%–82.9% with a mean of 67.1%, and for neck operations, the range was 20.0%–100% with a mean of 44.8%.
Table 2.
Trauma operation case volume and presence of general surgery resident by study site*
| Operation | A | B | D | E | G | H† | J | All sites | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
||||||||
| No. of available cases to attend | General surgery resident present, % | No. of available cases to attend | General surgery resident present, % | No. of available cases to attend | General surgery resident present, % | No. of available cases to attend | General surgery resident present, % | No. of available cases to attend | General surgery resident present, % | No. of available cases to attend | General surgery resident present, % | No. of available cases to attend | General surgery resident present, % | General surgery resident present, % | |
| Abdominal, any type | 136 | 91.9 | 422 | 91.9 | 108 | 97.2 | 378 | 96.3 | 265 | 88.5 | 326 | 91.7 | 516 | 60.9 | 80.6 |
|
| |||||||||||||||
| Thoracic, any type | 35 | 82.9 | 97 | 62.9 | 11 | 72.7 | 96 | 63.5 | 51 | 72.5 | 46 | 82.6 | 174 | 62.1 | 67.1 |
|
| |||||||||||||||
| Neck, any type | 20 | 20.0 | 45 | 37.8 | 17 | 88.2 | 44 | 54.5 | 24 | 41.7 | 16 | 100 | 65 | 37.8 | 44.8 |
Residency programs C, F, and K did not report these data.
Cohort from a 4-year study period.
The involvement of various surgical specialties according to operation type (abdominal, thoracic, or neck) is presented in Table 3, stratified by study site. For abdominal operations, the general surgery service was present at a mean of 98.5% of all cases (range 96.6%–100%), with the next most common specialty present being vascular surgery (mean 4.0%). For thoracic operations, the general surgery service was present a mean of 69.0% of all cases (range 17.1%–98.9%), with the next most common specialty present being thoracic surgery (mean 33.7%, range 0.6%–82.9%). For neck operations, the general surgery service was present a mean of 58.9% of all cases (range 10.0%–100%), with the next most common specialty present being ear, nose, and throat (ENT) or head and neck surgery (mean 32.5%, range 40.0%–68.9%).
Table 3.
Surgical specialty involvement in trauma operations*
| Operation | Study site | Total no. of operations | Presence of surgical specialties†, % | |||||
|---|---|---|---|---|---|---|---|---|
| General surgery | Vascular surgery | Thoracic surgery | Cardiac surgery | Head & neck or ENT surgery | Urology | |||
| Abdominal, any type | A | 136 | 97.1 | 2.9 | 2.2 | 0.0 | 0.0 | 5.1 |
| B | 422 | 98.6 | 6.9 | 2.1 | 1.2 | 0.7 | 5.5 | |
| D | 108 | 100 | 3.7 | 3.7 | 0.9 | 0.0 | 2.8 | |
| E | 378 | 96.6 | 7.4 | 6.1 | 0.0 | 0.0 | 2.4 | |
| G | 265 | 97.0 | 4.2 | 2.6 | 0.0 | 0.0 | 9.4 | |
| H | 326 | 99.7 | 1.2 | 0.6 | 0.0 | 0.0 | 4.6 | |
| J | 516 | 100 | 1.2 | 0.0 | 0.0 | 0.0 | 0.8 | |
| All sites | 2151 | 98.5 | 4.0 | 2.2 | 0.3 | 0.1 | 4.0 | |
| Thoracic, any type | A | 35 | 17.1 | 5.7 | 82.9 | 0.0 | 2.9 | 0.0 |
| B | 97 | 74.2 | 10.3 | 27.8 | 24.7 | 0.0 | 1.0 | |
| D | 11 | 45.5 | 18.2 | 45.5 | 9.1 | 0.0 | 0.0 | |
| E | 96 | 37.5 | 10.4 | 78.1 | 0.0 | 0.0 | 0.0 | |
| G | 51 | 33.3 | 9.8 | 56.9 | 0.0 | 0.0 | 2.0 | |
| H | 46 | 95.7 | 6.5 | 13.0 | 0.0 | 0.0 | 4.3 | |
| J | 174 | 98.9 | 2.3 | 0.6 | 0.0 | 0.0 | 0.0 | |
| All sites | 510 | 69.0 | 7.1 | 33.7 | 4.9 | 0.2 | 0.8 | |
| Neck, any type | A | 20 | 10.0 | 5.0 | 10.0 | 0.0 | 40.0 | 0.0 |
| B | 45 | 46.7 | 35.6 | 6.7 | 0.0 | 68.9 | 2.2 | |
| D | 17 | 47.1 | 17.6 | 11.8 | 0.0 | 0.0 | 0.0 | |
| E | 44 | 50.0 | 2.3 | 6.8 | 0.0 | 52.3 | 0.0 | |
| G | 24 | 20.8 | 33.3 | 4.2 | 0.0 | 54.2 | 0.0 | |
| H | 16 | 100 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| J | 65 | 95.4 | 4.6 | 0.0 | 0.0 | 0.0 | 0.0 | |
| All sites | 231 | 58.9 | 13.9 | 4.8 | 0.0 | 32.5 | 0.4 | |
ENT = ear, nose, and throat.
Study sites C, F, and K did not report these data.
More than 1 surgical specialty could be present at a surgery.
For those general surgery residents who completed a full residency during the study period, the mean and range of their trauma operative exposure during their entire residency is presented in Table 4. Over a graduating resident’s entire residency experience, they were found to be present at any type of abdominal operation a mean of 6.0 (median 5.0) times, including index laparotomy a mean of 4.5 (median 4.0) times. For any type of thoracic operation, the mean was 1.1 (median 1.0) times, including emergency thoracotomy a mean of 0.1 (median 0) times. For any type of neck operations, the mean was 0.5 (median 0) times. The most common specific procedures that a graduating cohort resident was present for were splenectomy (mean 1.1, median 1) and bowel repair or resection (mean 2.1, median 2). All other procedures had mean and median values less than 1.
Table 4.
Trauma operative exposure among general surgery residents who completed a full residency during the study period
| Operation | Total no. of procedures with a graduating resident present (across all sites) | Overall mean | Overall median | Site range,* mean | Site range,* median |
|---|---|---|---|---|---|
| Abdominal operation | |||||
| Any type | 1208 | 6.0 | 5 | 3.8–9.6 | 3.5–9.0 |
| Index laparotomy | 914 | 4.5 | 4 | 1.9–7.2 | 2–7 |
| Second-look laparotomy | 200 | 1.0 | 1 | 0.0–1.7 | 0–1 |
| Index laparoscopy | 87 | 0.4 | 0 | 0.1–0.6 | 0–0 |
| Second-look laparoscopy | 0 | 0.0 | 0 | 0.0–0.0 | 0–0 |
| Laparoscopy converted to laparotomy | 7 | 0.04 | 0 | 0.0–0.1 | 0–0 |
| Thoracic operation | |||||
| Any type | 220 | 1.1 | 1 | 0.4–1.4 | 0.5–2 |
| ED thoracotomy | 28 | 0.1 | 0 | 0.1–0.2 | 0–0 |
| OR thoracotomy | 127 | 0.6 | 0 | 0.3–1.3 | 0–1 |
| OR sternotomy | 29 | 0.1 | 0 | 0.1–0.3 | 0–0 |
| OR VATS | 35 | 0.2 | 0 | 0.0–0.4 | 0–0 |
| OR VATS converted to thoracotomy | 1 | 0.0 | 0 | 0.0–0.0 | 0–0 |
| Neck exploration, any type | 101 | 0.5 | 0 | 0.1–0.8 | 0–1 |
| Specific procedures | |||||
| Splenectomy | 228 | 1.1 | 1 | 0.4–2.5 | 0–2 |
| Liver repair or resection | 129 | 0.6 | 0 | 0.2–1.3 | 0–1 |
| Bowel repair or resection | 427 | 2.1 | 2 | 1.1–4.1 | 1–4 |
| Diaphragm repair | 159 | 0.8 | 0 | 0.5–1.3 | 0–1 |
| Retroperitoneal exploration | 131 | 0.7 | 0 | 0.1–1.9 | 0–2 |
| Pancreas resection | 28 | 0.1 | 0 | 0.0–0.3 | 0–0 |
| Duodenal repair or resection | 49 | 0.2 | 0 | 0.1–1.0 | 0–1 |
| Renal repair or resection | 22 | 0.1 | 0 | 0.0–0.2 | 0–0 |
| Bladder repair or resection | 32 | 0.2 | 0 | 0.0–0.4 | 0–0 |
| Major abdominal vascular repair | 55 | 0.3 | 0 | 0.0–0.7 | 0–0 |
| Cardiac repair | 43 | 0.2 | 0 | 0.0–0.5 | 0–0 |
| Lung repair or resection | 47 | 0.2 | 0 | 0.0–0.5 | 0–0 |
| Major vascular repair | 16 | 0.1 | 0 | 0.0–0.2 | 0–0 |
ED = emergency department; OR = operating room; VATS = Video-Assisted Thoracoscopic Surgery.
Range of means or medians from each individual site.
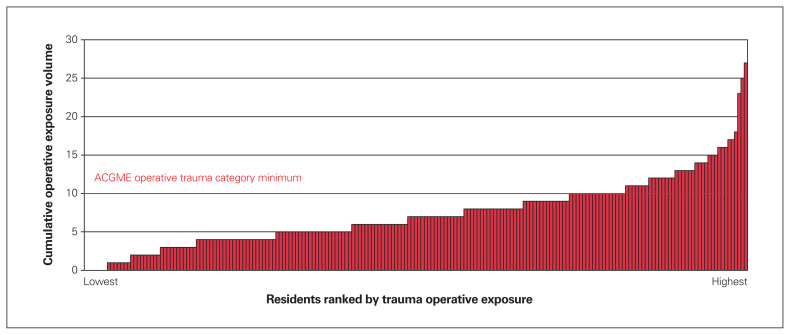
The volume of operative trauma exposure during residency among the 203 residents who completed their residency during the study period is displayed graphically in Figure 1, in the context of the ACGME minimums for operative trauma12 of 10 trauma operative cases. Fewer than one-third of graduating Canadian general surgery residents met this standard.
Fig. 1.
Distribution of total operative trauma exposure during residency among graduating general surgery residents, including 203 general surgery graduating residents ranked according to cumulative trauma operative exposure. Each bar represents 1 of the 203 graduate residents. ACGME = Accreditation Council for Graduate Medical Education.
The environmental scan results for the trauma training settings of the study sites are summarized in Table 5. In addition to the tabular results for trauma education for residents, sites also reported the occurrence of weekly or biweekly trauma rounds (e.g., morbidity and mortality conferences, case presentations, didactic session), informal trauma topic discussion on the trauma service, cadaveric trauma laboratory sessions, trauma simulation events, trauma journal clubs, and resuscitative endovascular balloon occlusion of the aorta (REBOA) training. Sites reported that, for surgeons providing trauma care, a range of 0%–100% had formal trauma fellowship training. Eight of 10 sites reported participation of their trauma surgeons in the call schedule of trauma team leaders. Nine of 10 sites reported the rotation of junior general surgery residents on the trauma service, with all sites reporting their participation in trauma team activations. All sites reported a senior resident on-call for trauma patients at all times, and 9 of 10 sites reported the senior resident attending all trauma team activations. All sites reported mandatory completion of the Advanced Trauma Life Support (ATLS) program as a first-year resident, and 5 of 9 reporting completion of one of the Advanced Trauma Operative Management (ATOM), Advanced Surgical Skills for Exposure in Trauma (ASSET), or Definitive Surgical Trauma Care (DSTC) courses as a senior resident.
Table 5.
Environmental scan of trauma education characteristics by study site*
| Characteristic | A | B | C | D | E | F | G | H1 | H2 | J | Summary |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Staff surgeons on trauma or combined trauma and ACS service | |||||||||||
| No. of surgeons in the pool that rotate on trauma and ACS services | 13 | 7 | 5 | 3 | 5 | 11 | 11 | 5 | 6 | 6 | Range 3–13 |
| No. (%) of surgeons who have completed a trauma fellowship | 1 (8) | 3 (43) | 3 (60) | 0 | 5 (100) | 3 (27) | 0 | 3 (60) | 5 (83) | 5 (83) | Range 0–5 |
| No. of surgeons who have completed a critical care fellowship | 0 | 1 | 4 | 1 | 4 | 1 | 2 | 3 | 3 | 4 | Range 0–4 |
| No. of surgeons who participate in TTL call schedule | 0 | 6 | 0 | 3 | 5 | 5 | 1 | 5 | 6 | 6 | Range 0–6 |
| General surgery resident rotation on trauma service | |||||||||||
| Junior resident rotation on trauma or combined trauma and ACS service | Y | Y | Y | Y | Y | Y | Y | Y | 8 of 9 | ||
| On-call resident formally scheduled as TTL or sub-TTL | Y | Y | 2 of 9 | ||||||||
| ≥ 1 senior resident on call for trauma patients at all times | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 of 9 | |
| Trauma service on-call coverage model | |||||||||||
| Junior resident on-call every night, home call | Y | 1 of 10 | |||||||||
| Junior resident on-call every night, in-house | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 of 10 | |
| Junior resident attends trauma activations | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 of 10 |
| Senior resident on-call every night, home call | Y | Y | Y | Y | Y | 5 of 10 | |||||
| Senior resident on-call every night, in-house | Y | Y | Y | Y | Y | 5 of 10 | |||||
| Senior resident attends trauma activations | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 of 10 | |
| Emergency medicine residents rotate on trauma service† | 8 of 9 | ||||||||||
| Orthopedic surgery residents rotate on trauma service† | 7 of 9 | ||||||||||
| Neurosurgery residents rotate on trauma service† | 6 of 9 | ||||||||||
| Plastic surgery residents rotate on trauma service† | 6 of 9 | ||||||||||
| On-call staff TTL roster filled 100% of time | Y | Y | Y | Y | Y | Y | Y | 7 of 10 | |||
| Trauma education for medical students | |||||||||||
| Formal preclinical teaching about trauma care | Y | Y | Y | Y | Y | 5 of 9 | |||||
| Formal clerkship teaching about trauma care | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 of 9 | |
| Trauma education for residents | |||||||||||
| No. of academic half-days dedicated to trauma | 3 | 1 | 4 | 3 | Y | 3 | Y | 4 | 1 | Range 1–4 | |
| Ssessions taught by a trauma fellowship–trained surgeon | Y | Y | Y | Y | Y | Y | Y | 7 of 9 | |||
| Mandatory completion of ATLS during PGY-1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 of 9 | |
| Mandatory completion of ATOM during PGY3–5 | Y | Y | Y | 3 of 9 | |||||||
| Mandatory completion of ASSET during PGY-5 | Y | 1 of 9 | |||||||||
| Mandatory completion of DSTC during PGY-5 | Y | 1 of 9 | |||||||||
| Formal FAST training during residency | Y | Y | Y | Y | 5 of 9 | ||||||
| Fellowship training | |||||||||||
| Local presence of a trauma care, trauma surgery, or traumatology fellowship program | Y | Y | Y | 3 of 10 | |||||||
| No. of residents pursuing trauma fellowship after residency during study period | 4 | 2 | 4 | 4 | 7 | 2 | 4 | 7 | 3 | Range 2–7 | |
ACS = Acute Care Surgery; ASSET = Advanced Surgical Skills for Exposure in Trauma; ATLS = Advanced Trauma Life Support; ATOM = Advanced Trauma Operative Management; DSTC = Definitive Surgical Trauma Care; FAST = Focused Assessment with Sonography in Trauma; REB = research ethics board; TTL = trauma team leader; Y = yes.
No data reported for Site K because of local research ethics board limitations. One of the residency programs (H) has 2 sites of trauma service; where appropriate, that residency program has been represented by either a single response or separate response according to the details of each site, hence the variable denominator of 9 residency programs or 10 trauma service sites.
Only aggregate information is provided, as per REB requirements.
In terms of the distribution of the start times for trauma operations across all sites, 26.8% were on weekdays (0700–1659, Monday through Friday), 43.3% were on weekends (Friday at 1700 until Monday at 0659), and 29.9% were on weeknights (1700–0659 Monday through Thursday). We did not observe any statistically significant variation between individual study years.
Discussion
Our study demonstrates that general surgery residency training in Canada is variable, with limited exposure to operative trauma care.
Training programs had inherent differences in the volumes of trauma patients they treated and differences in how they provided trauma care exposure in the training of their residents. Indeed, involvement of different surgical specialties in operative trauma care varied considerably by site and likely has a substantial impact on the opportunities available for general surgery residents. Although resident rotation on the trauma service and on-call exposure to trauma patients showed some consistent approaches, there is a lack of uniformity.
Trauma operations predominantly occurred after hours (73%), and general surgery residents attended only a portion of these learning opportunities, with 81% attendance at abdominal trauma operations and lower attendance at those operations involving the thorax (67%) or neck (45%). Exposure to body cavity and procedure-specific trauma operations were both relatively limited, with the average graduating general surgery resident being present for 4 index trauma laparotomies; the average procedural experience was 2 bowel resections for trauma and 1 trauma splenectomy. On average, only 1 of 7 graduating residents was present at an emergency thoracotomy and 1 of 2 was present for a neck exploration.
The relationship between nonoperative trauma education opportunities and operative experiences at each site was complex. At least 1 site appeared to exhibit some alignment of increased operative volume with nonoperative exposures, as well as a preponderance of fellowship-trained trauma surgeons. One possible explanation is that sites with higher volumes of clinical trauma have a dedicated cadre of trauma-focused surgeons that generate a strong program of trauma education and nonoperative learning opportunities and mandatory trauma courses (e.g., ATOM, ASSET, DSTC). Another possibility is that sites with lower volumes of clinical trauma recognize their limitations and thus invest more heavily in simulation-based trauma exposure and other nonoperative trauma education strategies. Still another possibility is that there exists both a deficiency in operative and nonoperative exposures, as well as a limited number of faculty dedicated to trauma care and education. Although we cannot make such determinations, these results clearly demonstrate substantial variability across training sites that begs further exploration.
The evolving landscape of trauma care, with increasing use of nonoperative and less-invasive treatment strategies, has raised important questions about the adequacy of operative trauma training. Existing research in this field comes from the US and raises concerns about the ability to train competent trauma care providers in the current conditions.5,6 A recent publication found that current postgraduate general surgery training in trauma in Canada is perceived to be inadequate by both educators and trainees.8 Our findings on trauma training across sites provide a baseline understanding of clinical exposure to trauma care, which, in the context of the evolving educational paradigm of CBD, is essential in identifying current performance, as well as opportunities for additional exploration, focus, and improvement.
When we compare our results to those reported by Strumwasser and colleagues,5 we see that Canadian trainees have trauma operative exposures that are, by and large, inferior to those in the US, and only 27% (54 of 203) of graduating general surgery residents would meet the ACGME minimum standard in trauma operations.12 Strumwasser and colleagues5 reported that a recent graduating general surgery resident in the US would have been exposed to 1.3 neck explorations, 2.3 thoracotomies, and 6.4 laparotomies (all types), compared with 0.5, 1.1, and 5.5, respectively, in our study.
Admittedly, exclusive reliance on case-logs as the sole assessment of operative exposure and competency is not supported by modern educational theory and does not represent the entire picture of training. One cannot even determine what role the trainee may have had in the operation (e.g., primary operator, first assistant, pure observer). Also, the role the resident takes in an operation is often perceived differently by their attending surgeon13 and the educational impact of the encounter is variable. However, most surgeons would consider a certain level of first-hand experience necessary and expected in future performance of a procedure.14
We also identified important differences in training environments. Consistent elements across sites included junior residents doing in-house call and responding to trauma activations, senior residents responding to trauma activations, mandatory completion of ATLS as a first-year resident, and trauma education within formal residency academic curricula. Notable elements of variability and exception across sites included a mix of in-house and home call among senior residents at the trauma centres; all but 1 centre reported that senior residents attended trauma activations, and only 2 centres reported formal trauma team leader exposure.
Addressing the gaps in trauma education is complex. Certainly, operative simulation training has an important role to play;15 rotations to high-volume trauma centres outside Canada may also be important.16 New approaches will likely be necessary, some of which are outlined by Mador and colleagues,17 who have developed a new conceptual framework in trauma training that highlights the key elements of institutional context and transferability of curricular components as part of the search for unconventional training opportunities.
The goals of trauma training within general surgery residency must also be evaluated. The clinical evolution in trauma care has been paralleled by an evolution in the training of trauma experts.5 Although post-residency trauma fellowship training has existed for decades, the advancement in clinical trauma care has driven trauma fellowship training to become formalized and accredited by national bodies within the US18 and Canada19 (e.g., Trauma General Surgery Diplomate designation from the RCPSC). The training duration and exposure required to achieve a level of expertise that was once within the domain of general surgery, now resides within formal fellowship training at a higher level. The interface between the objectives of training for trauma care within general surgery residency and training experiences that have been promoted to postresidency fellowship training in trauma is not impermeable. What may have been achievable with regard to trauma training exposure during residency in the past may not be achievable in the future, and identification of this changing goalpost is important both in standard setting, as well as in considering the role of simulation-based clinical education and in developing opportunities to capitalize on training exposures with comparable or transferral value.
As the CBD program for general surgery training evolves, the degree of inclusion of training in trauma care and the competencies that may reasonably be achieved within residency will need to be explored, affirmed, and demonstrated objectively, and not merely reflexively attested to. Prospective, comprehensive, and transparent reporting of objective operative learning experiences should be considered as part of the quality assurance and quality improvement aspects of surgical competency-based medical education in Canada.
Limitations
We used chart-level data abstraction from multiple sources to improve accuracy and a multicentre study including sites across 6 provinces, but as such, limitations included those inherent in chart documentation, especially in the sometimesfrenzied environment of the emergency department. Only 9 training programs of 17 participated and only 7 provided operating case-log data; some centres provided only portions of their data or permitted presentation of only aggregate data. Identified barriers to future participation include variable REB approval practices, absence of a functional local trauma registry, local lack of access to medical records for the purposes of research, and lack of local resources to participate. As per the REB and data sharing agreements with all sites, not all data elements could be collected from all sites and some data have been presented in aggregate format only. The lack of a single national database with residency case-log information severely hindered our ability to collect and analyze such data in a timely fashion.
Conclusion
In our study, we quantified the operative trauma exposure of general surgery residents in Canada and collected important information on the organization and format of other nonoperative trauma education experiences across Canada. Overall, general surgery residents who train in Canada have variable and limited exposure to operative and nonoperative trauma care. This information can be used as a baseline to inform future efforts to improve trauma education within general surgery residency training.
Footnotes
Competing interests: Paul Engels and Kelly Vogt sit on the board of the Trauma Association of Canada. Markus Ziessman reports honoraria from the American College of Surgeons. No other competing interests were declared.
Contributors: Paul Engels, Qian Shi, Angela Coates, Kelly Vogt, and Timothy Rice contributed to study conception and design. Paul Engels, Qian Shi, Angela Coates, Laura Allen, Fran Priestap, Bradley Moffat, Kelly Vogt, Emily Joos, Samuel Minor, Mylene Marchand, Erin Williams, Chris Evans, Brett Mador, Sandy Widder, Markus Ziessman, Jacinthe Lampron, Chad Ball, and Timothy Rice acquired data. Paul Engels, Angela Coates, Qian Shi, Laura Allen, Fran Priestap, Bradley Moffat, Kelly Vogt, and Timothy Rice contributed to data analysis and interpretation. Paul Engels, Qian Shi, Angela Coates, and Timothy Rice drafted the article. All of the authors revised the article for critically important intellectual content, gave final approval for the version to be published, and agreed to act as guarantor of the work.
Data sharing statement: In compliance with the existing Research Ethics Board and data sharing agreements that pertain to this study, data from our study are not available for use by other researchers.
Disclosure: Paul Engels is an associate editor and Chad Ball is co–editor-in-chief of CJS. They were not involved in the review or decision to accept this manuscript for publication.
Funding: This study was funded by the McMaster Surgical Associates Education Research Grant.
References
- 1.Cost of Injury in Canada. Toronto: Parachute; 2023. Available: https://parachutecanada.org/en/professional-resource/cost-of-injury-in-canada/ (accessed 2023 Jan. 6). [Google Scholar]
- 2.Resources for optimal care of the injured patient. Chicago: American College of Surgeons. Available: https://www.facs.org/quality-programs/trauma/quality/verification-review-and-consultation-program/standards/ (accessed 2023 Jan. 6). [Google Scholar]
- 3.Evans DC. From trauma care to injury control: a people’s history of the evolution of trauma systems in Canada. Can J Surg 2007; 50:364–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Hameed SM, Schuurman N, Razek T, et al. Access to trauma systems in Canada. J Trauma 2010;69:1350–61. [DOI] [PubMed] [Google Scholar]
- 5.Strumwasser A, Grabo D, Inaba K, et al. Is your graduating general surgery resident qualified to take trauma call? A 15-year appraisal of the changes in general surgery education for trauma. J Trauma Acute Care Surg 2017;82:470–80. [DOI] [PubMed] [Google Scholar]
- 6.Musonza T, Todd SR, Scott B, et al. Trends in resident operative trauma: How to train future trauma surgeons? Am J Surg 2019;218:1156–61. [DOI] [PubMed] [Google Scholar]
- 7.Engels PT, Bradley NL, Ball CG. The current state of resident trauma training: are we losing a generation? Can J Surg 2018;61:153–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan JF, Murphy PB, Mador B. A needs assessment of Canadian general surgery postgraduate trauma training. Injury 2021;52:2534–42. [DOI] [PubMed] [Google Scholar]
- 9.Competency by design: Canada’s model for competency-based medical education. Ottawa: The Royal College of Physicians and Surgeons of Canada. Available: https://www.royalcollege.ca/rcsite/cbd/what-is-cbd-e (accessed 2023 Jan. 6). [Google Scholar]
- 10.Shi Q, Coates A, Engels PT, et al. Trauma Resident Exposure in Canada and Operative Numbers (TraumaRECON): a study protocol for a national multicenter study of operative, non-operative, and structured educational exposures in Canada. CMAJ Open 2020;8:E715–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canadian Collaborative on Urgent Care Surgery (CANUCS). Available: https://canucs.ca (accessed 2023 Jan. 6).
- 12.Defined category minimum numbers for general surgery residents and credit role: Review Committee for Surgery. Chicago: Accreditation Council for Graduate Medical Education; 2019. Available: www.acgme.org/Portals/0/DefinedCategoryMinimumNumbersforGeneralSurgeryResidentsandCreditRole.pdf (accessed 2023 Jan. 6). [Google Scholar]
- 13.Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg 2013;258:440–9. [DOI] [PubMed] [Google Scholar]
- 14.Stoller J, Jamil T. The path to surgical autonomy: a return to apprenticeship. Available: https://www.generalsurgerynews.com/Opinion/Article/11-21/The-Path-to-Surgical-Autonomy-A-Return-to-Apprenticeship/65226 (accessed 2023 Jan. 6).
- 15.Lee S, Buck JR, Ledgerwood AM, et al. Nonoeprative management (NOM) of most liver injuries impairs the mastery of intraoperative hemostasis. Am J Surg 2020;219:462–4. [DOI] [PubMed] [Google Scholar]
- 16.Barmparas G, Navsaria PH, Dhillon NK, et al. The gap in operative exposure in trauma surgery: quantifying the benefits of an international rotation. Surg Open Sci 2019;2:46–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mador B, Kim M, White J, et al. Development of a novel conceptual framework for curriculum design in Canadian postgraduate trauma training. Can Med Educ J 2020;11:e62–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Acute care surgery. Chicago: American Association for the Surgery of Trauma, Acute Care Surgery Fellowship Program. Available: https://www.aast.org/acute-care-surgery-overview (accessed 2023 Jan. 6). [Google Scholar]
- 19.Competency Training Requirements for the Area of Focussed Competence in Trauma General Surgery. Ottawa: Royal College of Physicians and Surgeons of Canada. Available: https://www.royalcollege.ca/rcsite/documents/ibd/trauma-general-surgery-ctr-e (accessed 2023 Jan. 6). [Google Scholar]