Abstract
OBJECTIVE:
To assess the efficacy and safety of extracorporeal shockwave therapy (ESWT) combined with sodium hyaluronate (HA) for the treatment of knee osteoarthritis (KOA).
METHODS:
PubMed, Embase, the Cochrane Library, Web of Science, China National Knowledge Infrastructure, Wanfang database, China Science and Technology Journal Database, and SinoMed were searched from inception to July 2020. The quality of the randomized controlled trials was evaluated independently by two reviewers according to the criteria in the Cochrane Collaboration for Systematic Reviews. The identified articles were then screened individually using EndnoteX9 for eligibility in this Meta-analysis. The heterogeneity among the articles was evaluated using I2.
RESULTS:
A total of 17 studies, comprising 2000 individuals, were included in this Meta-analysis. The results showed that a significant improvement was observed in knee pain and function based on the clinical efficacy of ESWT combined with HA. Statistical analysis of clinical efficacy showed that [relative risk (RR) = 1.21, 95% confidence interval (CI) (1.12, 1.30), P < 0.01]. Statistical analysis of visual analog scale showed that [standardized mean difference (SMD) = -2.84, 95%CI (-4.01, -1.66), P < 0.01]. Western Ontario and McMaster University osteoarthritis index statistical analysis showed that [SMD = -1.57, 95% CI (-2.52, -0.61), P < 0.01]. Lysholm score statistical analysis showed that [SMD = 1.71, 95% CI (0.98, 2.44), P < 0.01]. In addition, only minor side effects, such as redness and swelling of the skin, were observed.
CONCLUSIONS:
Medium to low quality evidence showed that ESWT combined with HA offers an inexpensive, well-tolerated, safe, and effective method to improve pain and functionality in patients with KOA. However, tightly controlled, randomized, large multicenter trials are warranted to validate the current findings.
Keywords: osteoarthritis, knee; randomized controlled trial; extracorporeal shockwave therapy; hyaluronic acid; Meta-analysis
1. INTRODUCTION
Knee osteoarthritis (KOA) is a common disease of the motor system occurring, manifested as local chronic pain, swelling, and stiffness. These findings can led to joint malformations, severely affecting the quality of life of some middle-aged and elderly people and also indicating a depressive predisposition.1,2 With an accelerated aging process of the population, the prevalence of KOA is about 50% in people > 60-years-old, mainly females.3,⇓-5
Currently, KOA is mostly treated with physical therapy and drug therapy in the early and middle stages, but the efficacy is not yet elucidated.1,6,7 In order to improve joint function, play a protective role, sodium hyaluronate (HA) was used clinically to inhibit immune injury and promote cartilage repair. However, the effects of HA alone are slow and often require adjuvant treatment with hormone peripheral nerve block.8,9 Extracorporeal shockwave therapy (ESWT) is a non-operative treatment between traditional physical therapy and surgical treatment that acts by producing and focusing shockwaves into a diseased region of the organization. It has a low risk for treating small body trauma, less complications and cost-effective.10,⇓-12 Originally, ESWT was used for the treatment of urinary calculi and then gradually extended for the treatment of musculoskeletal system diseases. It is also effective in the treatment of KOA, thereby providing another option for the KOA.13,⇓,⇓-16 Several studies demonstrated that ESWT combined with HA in the treatment of KOA was better than HA alone, but no systematic review is yet available.
Meta-analysis (MA) is a quantitative statistical analysis method that obtains comprehensive conclusions through statistical processing of data through quantitative synthesis.17,18 The systematic review and Meta-analyses are aimed to evaluate the efficacy and safety of ESWT combined with HA in the treatment of KOA to provide an evidence-based reference for clinical treatment.
2. MATERIAL AND METHODS
2.1. Search strategy
The systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Databases, such as PubMed, Embase, the Cochrane Library, Web of Science, China National Knowledge Infrastructure, Wanfang database, China Science and Technology Journal Database, and SinoMed, from inception to July 2021, were searched. All search algorithms were structured by Medical Subject Headings (MeSH) and free text terms as follows: “knee osteoarthritis”, “extracorporeal shock wave therapy”, “hyaluronate sodium”. In addition, the reference lists of the relevant articles and reviews were evaluated to identify the potentially eligible studies. The specific search strategy is presented in supplementary Text 1.
2.2. Inclusion and exclusion criteria
The studies were included in accordance with the following criteria: (a) The participants were diagnosed with KOA; (b) Intervention: intra-articular injection of HA combined with ESWT, and exclusion of different energies or modes (e.g. high energy vs low energy, focused vs diffuse) ESWT for comparison between clinical trials; (c) Control group: HA was injected into the joint cavity alone; (d) The primary outcomes were clinical efficacy, visual analog scale (VAS) and Western Ontario and McMaster University osteoarthritis index (WOMAC). The secondary outcomes were Lysholm score and incidence of adverse reactions; (e) Study design: randomized controlled trial (RCT).
Studies were excluded if they met the following criteria: (a) Studies with incomplete or unavailable data; (b) Studies that do not include any of the above outcome indicators; (c) Animal experiments; (d) Reviews, letters, conference papers, editorials, expert opinions, and comment protocols; (e) Languages other than Chinese and English.
2.3. Data extraction
Two researchers independently screened the literature and extracted experimental data. The discrepancies were settled through discussion or negotiation with a third investigator. After excluding duplicate literature through EndnoteX9 and manual screening, relevant data were extracted from the included articles, including author, year of publication, study design type, study sample size, basic patient characteristics (age, gender, and course of disease), intervention measures, treatment parameters, clinical efficacy, VAS, WOMAC, Lysholm score, and adverse events. If the articles did not provide detailed outcomes, the data were requested from the author via e-mail.
2.4. Assessment of risk of bias
Two researchers independently evaluated the risk of bias in the included study and cross-checked the results. The discrepancies could be resolved by discussion with a third investigator. The methodological quality of the RCT was assessed independently using the Cochrane Systematic Review Risk Assessment Tool18 with respect to randomization, concealment, blindness, data integrity, selective reporting, and other bias data. The risk of bias was determined to be low in the included literature. When one or more of the parameters are not described clearly, the risk of bias is considered unclear. When one or more of the parameters are missing, the risk of bias is high. The quality of evidence for each outcome was determined based on the risk of bias.
2.5. Data synthesis and analysis
Revman5.3 (Cochrane Collaboration, London, UK) and Stata 14.0 (StataCorp LP, Corpus Christi, TX, USA) statistical software were used for Meta-analysis. For continuous variables, mean difference (MD) or standardized mean difference (SMD) was used, while relative risk (RR) or odds ratio (OR) was used for categorical variables, and 95% confidence interval (CI) was provided for each effect.19 The heterogeneity between the results of the included studies was analyzed using χ 2 test, and the heterogeneity was determined by using I 2. I 2 < 50% was considered as no statistical heterogeneity between the results, and a fixed-effects model was used for Meta-analysis, otherwise the random-effects model was used. Significant clinical heterogeneity was treated by subgroup analysis or sensitivity analysis or by descriptive analysis only.20 On the other hand, sensitivity analysis explored the impact of individual studies by the sequential exclusion of each study.21 The test level for Meta-analysis was set as a = 0.05.
3. RESULTS
3.1. Study selection and characteristics
The current study generated 107 records from eights databases. The preliminary evaluation of the titles and abstracts identified 52 potentially eligible studies. Further screening of full texts excluded 35 articles, while 17 studies that met the eligibility criteria were included in the current Meta-analysis.22,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓-38 Table 1 shows the basic characteristics of the included studies. Table 2 shows the ESWT parameters of the included studies. The study selection process is shown in Figure 1.
Table 1.
Characteristics of the included RCTs
| Study | Sample size EG/CG |
Sex (M/F) | Age (years) | Duration of disease (years) | Intervention | Outcome | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EG | CG | EG | CG | EG | CG | EG | CG | |||||||
| Wang KT et al 202022 | 57/55 | 28/29 | 26/29 | 57.4±10.10 | 62.18±7.89 | 4.57±3.24 | 4.58±3.02 | ESWT+HA | HA | ①②⑤ | ||||
| Wang GR et al 201923 | 48/48 | 20/28 | 21/27 | 64.94±4.75 | 65.28±4.83 | 5.61±2.26 | 5.49±2.30 | ESWT+HA | HA | ④ | ||||
| Sun LM et al 201524 | 40/38 | 22/18 | 20/18 | 64.10±9.70 | 63.40±9.50 | 9.10±7.60 | 9.60±7.50 | ESWT+HA | HA | ②④⑤ | ||||
| Su WZ et al 201825 | 80/80 | 28/52 | 24/56 | 58.35±12.56 | 57.65±10.53 | 3.13±0.94 | 3.22±1.01 | ESWT+HA | HA | ①② | ||||
| Pan K et al 201826 | 25/25 | NA | NA | NA | NA | NA | NA | ESWT+HA | HA | ② | ||||
| Meng Y et al 201627 | 67/65 | NA | NA | NA | NA | NA | NA | ESWT+HA | HA | ①④ | ||||
| Li ZC et al 201728 | 39/39 | 18/21 | 15/24 | 65.31±7.56 | 64.55±8.38 | 5.52±2.28 | 5.49±3.45 | ESWT+HA | HA | ③④ | ||||
| Huang SX et al 202029 | 27/27 | 10/17 | 12/15 | 48.30±9.60 | 46.90±6.80 | NA | NA | ESWT+HA | HA | ④ | ||||
| Han FM et al 201730 | 38/38 | 20/18 | 19/19 | 59.71±11.87 | 61.39±11.57 | 1.47±2.06 | 1.59±2.14 | ESWT+HA | HA | ④ | ||||
| Duan JF et al 201631 | 49/49 | 18/31 | 12/37 | 68.13±5.89 | 68.13±5.75 | 5.14±1.14 | 5.49±3.45 | ESWT+HA | HA | ①③④ | ||||
| Ding YY et al 201532 | 50/50 | 19/31 | 21/29 | 68.20±5.90 | 67.30±6.60 | 3.30±2.40 | 3.10±2.20 | ESWT+HA | HA | ①③④ | ||||
| Chi X et al 201833 | 43/43 | 19/24 | 22/21 | 60.30±4.70 | 60.80±4.90 | 8.50±1.50 | 8.80±1.70 | ESWT+HA | HA | ①③④ | ||||
| Liu SC et al 201934 | 35/35 | 13/22 | 15/20 | 66.80±9.10 | 68.20±10.30 | 14.00±3.80 | 15.20±4.20 | ESWT+HA | HA | ①②⑤ | ||||
| Yin Q et al 201535 | 25/25 | 0/25 | 0/25 | 71.34±5.22 | 71.34±5.22 | 7.53±2.21 | 7.53±2.21 | ESWT+HA | HA | ⑤ | ||||
| Shi CA et al 202036 | 40/40 | 14/26 | 13/27 | 66.40±9.20 | 65.40±9.90 | 8.40±2.10 | 8.10±2.90 | ESWT+HA | HA | ①②⑤ | ||||
| Xi FF et al 201937 | 30/30 | 14/16 | 15/15 | 68.00±7.00 | 64.00±9.00 | 6.50±2.20 | 6.40±2.30 | ESWT+HA | HA | ①②⑤ | ||||
| Xu H et al 202038 | 310/310 | 156/154 | 150/160 | 63.20±2.60 | 64.20±2.80 | 4.50±0.60 | 5.10±0.70 | ESWT+HA | HA | ①③④ | ||||
Notes: data are presented as mean ± standard deviation. RCT: randomized controlled trial; EG: ESWT+HA; CG: HA; ESWT: extracorporeal shock wave combined with sodium hyaluronate; HA: sodium hyaluronate; M: male, F: female; NA: data not available. ①: visual analog scale, VAS; ②: Western Ontario and McMaster University osteoarthritis index, WOMAC; ③: Lysholm knee score; ④: total effective rate; ⑤: numeric rating scale, NRS.
Table 2.
Extracorporeal shock wave setting parameters
| Study | Type | Frequency | Time | Interval of treatment (days) | Intensity of pressure (bar) |
|---|---|---|---|---|---|
| Wang KT et al 202022 | Focused | 2500 | 5 | 7 | 1.5-2.5 |
| Wang GR et al 201923 | Focused | 1000 | 5 | 7 | 3.0 |
| Sun LM et al 201524 | Diffuse | 2000-3000 | 5 | 7 | 1.4-3.0 |
| Su WZ et al 201825 | Focused | 1000-2000 | 5 | 7 | 1.2-2.0 |
| Pan K et al 201826 | Focused | 1000 | 5 | 7 | 3.0 |
| Meng Y et al 201627 | NA | 3000-4000 | 4 | 2 | 1.5 |
| Li ZC et al 201728 | Diffuse | 2000 | 5 | 7 | 3.0 |
| Huang SX et al 202029 | NA | NA | 4 | 7 | NA |
| Han FM et al 201730 | NA | 2500 | 5 | 7 | 3.0 |
| Duan JF et al 201631 | NA | 2000 | 5 | 7 | 2.0-3.0 |
| Ding YY et al 201532 | NA | 2000 | 5 | 7 | 2.0-3.0 |
| Chi X et al 201833 | NA | 2000 | 10 | 7 | NA |
| Liu SC et al 201934 | NA | 4000 | 8 | 7 | 2.5 |
| Yin Q et al 201535 | NA | 2000 | 3 | 7 | 1.4-2.0 |
| Shi CA et al 202036 | Diffuse | 2000 | 5 | 7 | 3 |
| Xi FF et al 201937 | NA | 2000 | 5 | 7 | 2.5 |
| Xu H et al 202038 | Diffuse | 2000 | 4 | 7 | 2 |
Notes: NA: data not available.
Figure 1. Process of literature screening.
CNKI: China National Knowledge Infrastructure Database; VIP: China Science and Technology Journal Database; CBM: Chinese Biomedical Literature Database.
3.2. Risk of bias
Among all randomized studies, 7 trials22,24,25,27,35-37 explicitly proposed the method of random number table for random grouping, while the other articles only mentioned “random grouping” and did not report the generation method of random sequence. Only one trial23 mentioned the use of double-blind methods, while the other articles did not mention random occultation and blindness. Also, no dropouts or lost cases were described in any of the trials. In addition to the above methodological quality factors, no other bias was considered, and the risk of bias in the included study is shown in supplementary Figure 1. Overall, the studies were of medium-to-low quality.
3.3. Outcomes of the Meta-analysis
3.3.1. Clinical efficacy
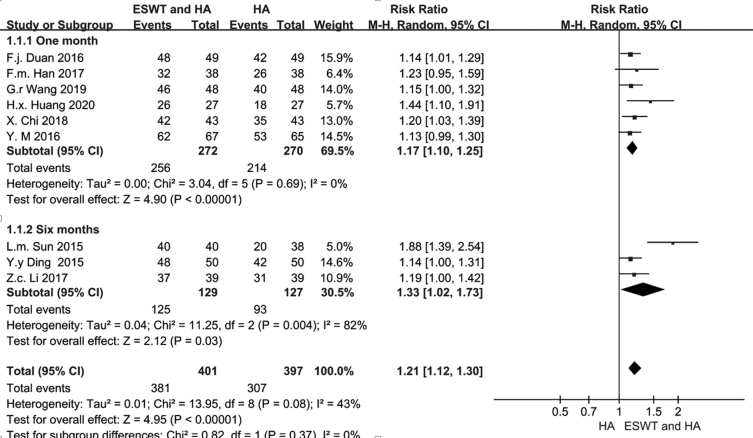
A total of 9 studies23,24,27-33 were included in this Meta-analysis, comprising 401 cases in the EXWT combined with HA group and 397 cases in the HA group alone. The Meta-analysis of the randomized effect model showed that the difference was statistically significant in the 1-month group23, 27, 29-31,33 of follow-up [RR =1.17, 95% CI (1.10, 1.25), P < 0.01] (Figure 2) and the difference was not statistically significant in the 6-months groups (24, 28, 32) of follow-up [RR = 1.33, 95% CI (1.02, 1.73), P = 0.03] (Figure 2). The efficacy of EXWT combined with HA in the treatment of KOA was significantly better than that of HA alone, but no significant advantage was recorded in long-term efficacy.
Figure 2. Meta-analysis of the effective rate of ESWT combined with HA treatment of KOA.
ESWT: extracorporeal shock wave combined with sodium hyaluronate; HA: sodium hyaluronate; CI: confidence interval.
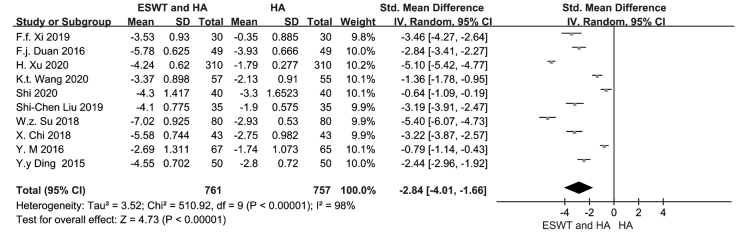
3.3.2. VAS
A total of 10 studies22,25,27,31-33,36-38 were included, comprising of 761 cases in the EXWT combined with HA group and 757 cases of the pure HA group. The results of the Meta-analysis of the randomized effect model showed that the differences were statistically significant [SMD = -2.84, 95% CI (-4.01, -1.66), P < 0.01] (Figure 3), and EXWT combined with HA was better than the pure HA group in relieving the pain of KOA.
Figure 3. Meta-analysis of the VAS of ESWT combined with HA treatment of KOA.
ESWT: extracorporeal shock wave combined with sodium hyaluronate; HA: sodium hyaluronate; CI: confidence interval.
3.3.3. WOMAC
A total of 7 studies22,24-26,34,36,37 were included, consisting of 307 cases of EXWT combined with HA group and 303 cases of the pure HA group. The results of the random-effects model showed statistically significant differences [SMD = -1.5, 95% CI (-2.52, -0.61), P = 0.001] (Figure 4), and EXWT combined with HA relieved swelling and recovered the joint function better than pure HA in the treatment of KOA.
Figure 4. Meta-analysis of WOMAC of ESWT combined with HA treatment of KOA.
ESWT: extracorporeal shock wave combined with sodium hyaluronate; HA: sodium hyaluronate; CI: confidence interval.
3.3.4. Lysholm knee score, LKS
A total of 5 studies28,31-33,38 were included, comprising 491 cases in EXWT combined with HA group and 481 of the pure HA group. The results of Meta-analysis of the randomized effect model showed statistically significant differences [SMD = 1.71, 95% CI (0.98, 2.44), P < 0.001]. The EXWT combined with HA in the treatment of KOA was better than pure HA.
3.3.5. Adverse effects (AE)
A total of 4 studies22,34,36,37 reported AEs, such as aggravated symptoms or local subcutaneous ecchymosis, during the experiment. No AE reported in 2 studies,24,35 while the remaining studies did not report such reactions. No serious AEs were described. Among these, 227 cases comprised the EXWT combined with HA group and 223 in the pure HA group. Meta-analysis of the fixed effects model showed that the differences were not statistically significant [OR = 0.84, 95% CI (0.44, 1.62), P = 0.61]. Therefore, no significant difference was observed in the incidence of adverse reactions between EXWT combined with HA and pure HA in the treatment of KOA.
3.4. Sensitivity analysis
Due to the obvious heterogeneity in VAS, WOMAC, and Lysholm scores, sensitivity analysis was conducted to determine the source of heterogeneity. After sequential exclusion of the studies, statistical analysis data did not show any directional change, indicating the credibility of the results.
4. DISCUSSION
KOA is a degenerative joint disease with an irreversible process, and the treatment of the early disease could be effectuated via pharmacological (oral and topical use of Traditional Chinese Medicine and nonsteroidal anti-inflammatory drugs) and non-pharmacological methods (acupuncture and massage, functional exercise, and joint cleaning) to relieve symptoms or delay the disease.1,6,7 The late KOA often uses artificial knee joint replacement. ESWT was initially used to treat urinary calculi but has been extended to treat musculoskeletal disorders and has shown promising clinical results. Further studies indicated that ESWT could relieve joint pain, protect the cartilage, promote bone remodeling, and release soft tissue.10,⇓-12 The synergistic effect of various mechanisms alleviated the pain and stiffness of the knee joint and improved the joint function in a short duration.39,⇓-41 Its clinical efficacy was better than the traditional treatment methods, such as NSAIDs, blocking therapy, and cartilage protectants. In addition, some studies have also shown that ESWT has a good therapeutic effect on severe KOA patients.42,43 The original studies have shown that the clinical effect of ESWT combined with HA in the treatment of KOA is better than HA alone.22,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓,⇓-38 However, clinical evidence of ESWT combined with HA in the treatment of KOA is yet lacking, and the efficacy and safety of ESWT combined with HA have not been verified.
In this study, the systemic review was used to search for the major medical databases used commonly. The screening process and criteria were developed according to the PRISMA principle, and a total of 15 articles were included to evaluate the efficacy and safety of ESWT combined with HA in the treatment of KOA. Although the number included in this analysis was small, all of the references were clinical RCTs. The quality was evaluated in accordance with the bias risk assessment tools recommended by the Cochrane Guidelines to minimize the errors and reduce various biases.
This analysis showed that the clinical efficacy of ESWT combined with HA in the treatment of KOA was better than pure HA. Due to the varied follow-up time in the included studies, the subgroup analysis was conducted on the 1-month and the 6-months groups. The results showed that the efficacy of EXWT combined with HA in the treatment of KOA was significantly better than pure HA, but there was no significant advantage detected in the long-term efficacy. Also, VAS score analysis showed that ESWT combined with HA in the treatment of KOA was better than HA alone in alleviating joint pain. Ding et al 32 demonstrated that ESWT combined with HA in the treatment of KOA was better than HA alone in alleviating joint pain and improving joint function, with a faster curative effect and longer duration, which was consistent with the results of the present study. According to the WOMAC score, Lysholm scale, and adverse reaction analysis, ESWT combined with HA was better than HA alone in relieving pain and swelling of the joint and improving the joint function and quality of life in patients with no obvious adverse reactions. ESWT combined with HA has the advantages of simple operation, working fast, less injury, high safety, low cost, and no requirement of anesthesia. The follow-up clinical applications widely use ESWT combined with HA therapy for the conservative treatment of patients with KOA. In addition, one study compared the clinical effects of ESWT combined with HA, ESWT alone, and HA alone.25 The results showed that the combined treatment was better than ESWT alone and HA alone in improving the clinical effect and reducing the VAS and WOMAC scores and no obvious adverse reactions. Therefore, to improve the effectiveness and shorten the course of clinical treatment, ESWT could be combined with other treatment methods to achieve a better therapeutic effect. Shi et al 36 compared the clinical effects of ESWT combined with HA and HA alone in the treatment of KOA in elderly women. The results showed that ESWT combined with HA had an exact and lasting effect in the treatment of KOA, with improved knee joint function and no obvious adverse reactions, which was consistent with the results of the present study. Also, obvious heterogeneity was detected in this Meta-analysis, which might be related to the gender and age differences of the included samples. Yin et al 35 assessed the efficacy and safety of ESWT combined with HA in females with KOA. Simultaneously, the heterogeneity could be increased due to the inconsistency of treatment parameters in the experimental group and different follow-up periods of each included study. Chi et al 33 showed that the interval of ESWT was only 1 d, which was significantly different from other studies with an interval of 7 d. In future studies, the sample size would be increased to reduce the heterogeneity in the analysis.
Nevertheless, the present study has some limitations in this Meta-analysis: (a) Only Chinese and English literature were included, which may have morbidity bias; (b) The included studies were from China, which might affect the generalizability of the results; (c) Most of the included studies did not report randomized methods, allocation concealment, and blinding, which might have a high risk of selectivity and measurement bias; (d) There is a lack of a unified standard for the specifications and frequency of shock wave and hyaluronic acid in various studies that resulted in significant heterogeneity; (e) The evaluation indicators were scores, and the lack of imaging indicators or other significant cytokine-related data made it difficult to determine the clinical applications accurately.
In conclusion, it was rare that the efficacy and safety of ESWT combined with HA for the treatment of KOA were assessed using a systematic review and Meta-analysis. The results suggested that using ESWT combined with HA for treatment of KOA has a beneficial effect on pain relief, physical function, and quality of life, and only minor complications occurred after ESWT combined with HA treatment, which can be a clinical priority.
5. ACKNOWLEDGMENTS
The authors would like to thank all the members of the Center for Evidence-Based Medicine, Lanzhou University, for their help with this study.
6. SUPPORTING INFORMATION
Supporting data to this article can be found online at http://journaltcm.cn.
Contributor Information
Kehu YANG, Email: kehuyangebm2006@126.com.
Shenghua LI, Email: Medicweich@163.com.
References
- 1. Kolasinski SL, Neogi T, Hochberg MC, et al. . 2019 American College of Rheumatology/Arthritis Foundation Guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2020; 72: 149-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Madaleno FO, Santos BA, Araújo VL, Oliveira VC, Resende RA. . Prevalence of knee osteoarthritis in former athletes: a systematic review with Meta-analysis. Braz J Phys Ther 2018; 22: 437-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim JH, Kim JY, Choi CM, et al. . The dose-related effects of extracorporeal shock wave therapy for knee osteoarthritis. Ann Rehabil Med 2015; 39: 616-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cisternas MG, Murphy L, Sacks JJ, Solomon DH, Pasta DJ, Helmick CG. . Alternative methods for defining osteoarthritis and the impact on estimating prevalence in a US population-based survey. Arthritis Care Res (Hoboken) 2016; 68: 574-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Richmond J, Hunter D, Irrgang J, et al. . American academy of orthopaedic surgeons clinical practice guideline on the treatment of osteoarthritis (OA) of the knee. J Bone Joint Surg Am 2010; 92: 990-3. [DOI] [PubMed] [Google Scholar]
- 6. Birch S, Lee MS, Robinson N, Alraek T. . The U.K. 2014 guidelines for osteoarthritis of the knee: lessons learned in a narrative review addressing inadvertent limitations and bias. J Altern Complement Med 2017; 23: 242-6. [DOI] [PubMed] [Google Scholar]
- 7. Wang YC, Huang HT, Huang PJ, Liu ZM, Shi CL. . Efficacy and safety of extracorporeal shockwave therapy for treatment of knee osteoarthritis: a systematic review and Meta-analysis. Pain Med 2020; 21: 822-35. [DOI] [PubMed] [Google Scholar]
- 8. Maheu E, Avouac B, Dreiser RL, Bardin T. . A single intra-articular injection of 2.0% non-chemically modified sodium hyaluronate vs 0.8% hylan G-F 20 in the treatment of symptomatic knee osteoarthritis: a 6-month, multicenter, randomized, controlled non-inferiority trial. PLoS One 2019; 14: e0226007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jüni P, Hari R, Rutjes AW, et al. . Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 2015: Cd005328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Simplicio CL, Purita J, Murrell W, Santos GS, Dos Santos RG, Lana J. . Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. J Clin Orthop Trauma 2020; 11: S309-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang CJ. . Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res 2012; 7: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xie X, Zhu J, Zhang H. . Effects of extracorporeal shock wave therapy in patients with knee osteoarthritis: a cohort study protocol. Medicine (Baltimore) 2020; 99: e21749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liao CD, Tsauo JY, Liou TH, Chen HC, Huang SW. . Clinical efficacy of extracorporeal shockwave therapy for knee osteoarthritis: a systematic review and Meta-regression of randomized controlled trials. Clin Rehabil 2019; 33: 1419-30. [DOI] [PubMed] [Google Scholar]
- 14. Schnurrer-Luke-Vrbanić T, Avancini-Dobrović V, Sosa I, Cvijanovic O, Bobinac D. . Effect of radial shock wave therapy on long bone fracture repair. J Biol Regul Homeost Agents 2018; 32: 875-9. [PubMed] [Google Scholar]
- 15. Mackert GA, Schulte M, Hirche C, et al. . Low-energy extracorporeal shockwave therapy (ESWT) improves metaphyseal fracture healing in an osteoporotic rat model. PLoS One 2017; 12: e0189356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lizis P, Kobza W, Manko G. . Extracorporeal shockwave therapy vs kinesiotherapy for osteoarthritis of the knee: a pilot randomized controlled trial. J Back Musculoskelet Rehabil 2017; 30: 1121-8. [DOI] [PubMed] [Google Scholar]
- 17. Yang KH. . Evidence-based social science: the origin, development and prospects. Libr Inf 2018; 3: 1-10. [Google Scholar]
- 18. Yang KH, Li XX, Bai ZG. . Research methods of Evidence-based social science:systematic review and Meta-analysis. Lanzhou: Lanzhou University Press, 2018: 20- 32. [Google Scholar]
- 19. Pan B, Ge L, Xun YQ, et al. . Exercise training modalities in patients with type 2 diabetes mellitus: a systematic review and network Meta-analysis. Int J Behav Nutr Phys Act 2018; 15: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Huang D, Song X, Cui Q, Tian J, Wang Q, Yang K. . Is there an association between aircraft noise exposure and the incidence of hypertension? A Meta-analysis of 16784 participants. Noise Health 2015; 17: 93-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li X, Wei L, Shang W, et al. . Trace and evaluation systems for health services quality in rural and remote areas: a systematic review. J Public Health 2018; 26: 127-35. [Google Scholar]
- 22. Wang KT, Wu Q, Zhang L. . Observation on the clinical efficacy of intra-articular injection of sodium hyaluronate combined with shock wave in the treatment of knee osteoarthritis. Zhong Guo Xian Dai Yi Sheng 2020; 58: 77-80. [Google Scholar]
- 23. Wang GR. . Effect of extracorporeal shock wave combined with sodium hyaluronate intra-articular injection on osteoarthritis of knee Joint. Zhong Wai Yi Xue Yan Jiu 2019; 17: 141-2. [Google Scholar]
- 24. Sun LM, Lyu K, Zhu H. . Efficacy of dispersive shock wave combined with intra-articular injection of sodium hyaluronate in the treatment of knee osteoarthritis. Huai Hai Yi Yao 2015; 33: 548-9. [Google Scholar]
- 25. Su WZ, Lin YG, Wang GW. . Therapeutic efficacy of extracorporeal shock wave therapy combined with sodium hyaluronate injection on knee osteoarthritis. Zhong Hua Jie Pou Yu Lin Chuang 2018; 23: 418-21. [Google Scholar]
- 26. Pan K, Qi W, Liu Y. . Efficacy research of extracorporeal shock wave combined with sodium hyaluronate injection in the treatment of knee osteoarthriti. Zhong Guo Shi Yong Yi Yao 2018; 13: 25-7. [Google Scholar]
- 27. Meng Y, Wu M, Wang HP. . Application of shock wave combined with intra-articular injection in the treatment of knee osteoarthritis. Zhong Guo Teng Tong Yi Xue 2016; 22: 638-9. [Google Scholar]
- 28. Li ZC. . Intra-articular injection of sodium hyaluronate combined with extracorporeal shock wave therapy for the treatment of elderly patients with knee osteoarthritis. Dang Dai Yi Yao Lun Cong 2017; 15: 87-8. [Google Scholar]
- 29. Huang SX, Wei X, Tang DC. . Efficacy of pneumatic ballistic extracorporeal shock wave combined with sodium hyaluronate in the treatment of knee osteoarthritis. Yunnan Yi Yao 2020; 41: 156-8. [Google Scholar]
- 30. Han FM, Li ZL, Zhang WJ, et al. . Efficacy of extracorporeal shock wave combined with sodium hyaluronate injection in the treatment of knee osteoarthritis. An Mo Yu Kang Fu Yi Xue 2017; 8: 52-3. [Google Scholar]
- 31. Duan JF, Wang BW, Zhang XB, et al. . Effect of sodium hyaluronate combined with pneumatic ballistic extracorporeal shock wave therapy on knee osteoarthritis. Zhong Guo Shi Yong Yi Kan 2016; 43: 41-3. [Google Scholar]
- 32. Ding YY, Yao P. . Efficacy of pneumatically ballistic extracorporeal shockwave combined with sodium hyaluronate on knee osteoarthritis. Shi Yong Yao Wu Yu Lin Chuang 2015; 18: 799-803. [Google Scholar]
- 33. Chi X, Lin SJ, Tang JY, et al. . Efficacy of electromagnetic shock wave combined with sodium hyaluronate in the treatment of knee osteoarthritis. Psychology Monthly 2018; 10: 255. [Google Scholar]
- 34. Liu SC, Qiao XF, Tang QX, et al. . Therapeutic efficacy of extracorporeal shock wave combined with hyaluronic acid on knee osteoarthritis. Medicine (Baltimore) 2019; 98: e14589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yin Q, Shen W, Yuan Y, et al. . Clinical observation of extracorporeal shock wave combined with knee injection in the treatment of elderly women with knee arthritis. Zhong Wai Nyu Xing Jian Kang Yan Jiu 2015: 193-4. [Google Scholar]
- 36. Shi CA, Liu L, Wang JW. . Clinical observation of extracorporeal shock wave combined with hyaluronic acid in the treatment of knee osteoarthritis. Zhong Guo Gu Yu Guan Jie 2020; 9: 632-5. [Google Scholar]
- 37. Xi FF, Li J, Zhao FL. . Clinical observation of periprosthetic pain point extracorporeal shock wave for the treatment of knee osteoarthritis pain. Zhong Guo Teng Tong Yi Xue 2019; 25: 924-7. [Google Scholar]
- 38. Xu H, Zhang HY, Su GC. . Clinical application of electromagnetic shock wave combined with evanescent extracorporeal shock wave in the treatment of osteoarthritis of the knee. Jian Kang Guan Li 2020; 6: 44. [Google Scholar]
- 39. Chen L, Ye L, Liu H, Yang P, Yang B. . Extracorporeal shock wave therapy for the treatment of osteoarthritis: a systematic review and Meta-analysis. Biomed Res Int 2020; 2020: 1907821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vetrano M, Ranieri D, Nanni M, et al. . Hyaluronic Acid (HA), Platelet-rich plasm and extracorporeal shock wave therapy (ESWT) promote human chondrocyte regeneration in vitro and ESWT-mediated increase of CD 44 expression enhances their susceptibility to HA treatment. PLoS One 2019; 14: e0218740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yu L, Liu S, Zhao Z, et al. . Extracorporeal shock wave rebuilt subchondral bone in vivo andactivated Wnt5a/Ca(2+) signaling in vitro. Biomed Res Int 2017; 2017: 1404650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Xu Y, Wu K, Liu Y, et al. . The effect of extracorporeal shock wave therapy on the treatment of moderate to severe knee osteoarthritis and cartilage lesion. Medicine (Baltimore) 2019; 98: e15523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Li W, Pan Y, Yang Q, Guo ZG, Yue Q, Meng QG. . Extracorporeal shockwave therapy for the treatment of knee osteoarthritis: a retrospective study. Medicine (Baltimore) 2018; 97: e11418. [DOI] [PMC free article] [PubMed] [Google Scholar]