Abstract
Families of critically ill patients are predisposed to tremendous burdens when their relatives are admitted to the intensive care unit (ICU). Postintensive care syndrome family (PICS‐F) can be described as a devastated life, encompassing psychological, physical, and socioeconomical burdens that begin with the emotional impact experienced by the family when the patient is admitted to the ICU. PICS‐F was primarily proposed as a clinically significant psychological impairment, but it needs to be extended beyond the psychological impairment of the family to include physical and socioeconomical impairments in the future. The prevalence of physiological problems including depression, anxiety and post‐traumatic syndrome is 20–40%, and that of non‐physiological problems including fatigue is 15% at 6 months after the ICU stay. Assessment of PICS‐F was frequently conducted at 3‐ or 6‐month points, although the beginning of the evaluation was based on different assessment points among each of the studies. Families of ICU patients need to be given and understand accurate information, such as the patient's diagnosis, planned care, and prognosis. Prevention of PICS‐F requires a continuous bundle of multifaceted and/or multidisciplinary interventions including providing a family information leaflet, ICU diary, communication facilitators, supportive grief care, and follow‐up, for the patient and families from during the ICU stay to after discharge from the ICU. This is the first comprehensive review of PICS‐F to address the concept, risk factors, assessment tools, prevalence, and management to prevent PICS‐F to facilitate acute care physicians' understanding of PICS‐F.
Keywords: postintensive care syndrome family, prevention bundle, psychological, resilience
Postintensive care syndrome family (PICS‐F) is grave, which is a psychological, physical, and socioeconomic disorder of the family after the patient is admitted to the ICU that has a major impact on the quality of life of the families and the ability to support the recovery of ICU patients.
INTRODUCTION
Families of critically ill patients are predisposed to a tremendous burden when their relatives are admitted to the intensive care unit (ICU). 1 , 2 , 3 This burden has various effects on the patient's family, which is affected by the trajectories of the patient's recovery. 4 The cluster of psychological complications such as anxiety, depression, acute stress disorder, post‐traumatic stress disorder (PTSD), and complicated grief from exposure to critical care in families of patients is primarily called postintensive care syndrome family (PICS‐F), 5 , 6 and it might affect the family's ability to support the recovery of ICU patients. 7
Recently, narrative reviews of PICS including PICS‐F have been published; however, they were apparently focused on PICS, and no comprehensive summaries of PICS‐F have been published. 8 , 9 In addition, the description of PICS‐F in a previous review was limited to the classic definition of PICS‐F, that is psychological impairments in families of ICU patients, 5 but impairments of families usually develop beyond the psychological to affect quality of life, such as physical and socioeconomical impairments. 4 , 10 , 11 Thus, there is a strong need for a comprehensive review of PICS‐F to support families and improve recovery of ICU patients through family support.
The aim of this review was to clarify the concept, risk factors, assessment tools, prevalence, management to prevent PICS‐F, and facilitate acute care physicians' understanding of PICS‐F.
CONCEPTUALIZATION
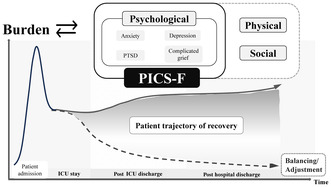
PICS‐F was primarily proposed as clinically significant psychological impairments including anxiety, depression, post‐traumatic stress disorder (PTSD), and complicated grief that developed in families of critically ill patients admitted to the ICU. 6 In addition to the psychiatric impairments, families actually experience physical impairments such as fatigue and sleep disturbances during the post‐ICU period, 12 , 13 and household financial insecurity due to the impact of patient care on their socioeconomic activities, such as sick leave, as well as work restrictions 14 , 15 (Figure 1).
FIGURE 1.
Conceptual diagram of PICS‐F. The horizontal axis shows the passage of time, and the vertical axis shows the amount of burden on the family. PICS‐F is triggered by the emotional burden experienced by the family when the patient is admitted to the ICU, which leads to the physical and socioeconomic burden. Furthermore, in the subsequent course, various factors, such as the patient's medical condition, the family's environment, and financial burden, are intricately related to the development of PICS‐F if families cannot adjust to these burdens. Psychological symptoms, which are classic symptoms of PICS‐F, are circled by solid lines, whereas physical and social problems, which are being expanded upon today as a new concept of PICS‐F, are circled by dotted lines. PICS‐F sometimes develops during a patient's ICU admission, and these symptoms may continue long after ICU discharge if families cannot adjust to the burden.
PICS‐F is triggered by the emotional burden of patient admission to the ICU, and a thorough understanding of the mechanism should be useful in overviewing the subsequent course of the disease. Families of critically ill patients experience significant and lasting effects not only on their mental health, but also on their physical and social wellbeing, and the family health condition may inversely impact the patient's recovery. 4 The entire trajectory of disease recovery of patients causes a wide range of family burden affecting their physical, socioeconomical, and emotional domains. 4 Recently, Kang 3 presented a comprehensive concept of PICS‐F as “being devastated by the critical illness journey in the family”. PICS‐F is largely associated with the decline of the family's quality of life as a result of a vicious cycle involving deteriorating physical health, rising psychological distress, social withdrawal, and family crisis. Furthermore, developing PICS‐F itself leads to an additional burden on the family.
In summary, PICS‐F can be described as a devastated life, encompassing psychological, physical, and socioeconomical burdens that begin with the emotional impact experienced by the family when the patient is admitted to the ICU. It is important to emphasize that PICS‐F needs to be extended beyond the psychological impairments of the families to include physical and socioeconomical impairments in the future.
RISK FACTORS FOR PSYCHOLOGICAL DISORDERS
Risk factors for PICS‐F (psychological disorders) were broadly categorized into patient‐related factors, family‐related factors, and protective factors. These risk factors are summarized in Table 1 for each period of PICS‐F assessment. The timing of PICS‐F evaluation is based on different assessment points, such as after ICU admission, after ICU discharge, and after hospital discharge. Therefore, in this review, although the assessment points are different, “months after ICU discharge” is generally used.
TABLE 1.
Risk factors for psychological disorders.
| Patient | Family | Protective factors |
|---|---|---|
| ICU admission – <3 months after ICU discharge | ||
|
Demographic characteristics Younger, 16 , 17 , 18 , 19 Older, 20 Male, 21 Education level ≥12th grade, 21 Lower education or socioeconomic status 22 , Absence of chronic disease, 16 Clinical characteristics Severity of illness, 17 , 20 Delirium, 23 Anxiety or depression, 18 ICU length of stay, 24 , 25 , 26 , 27 , 28 Prolonged mechanical ventilation, 29 Presence of cancer metastasis, 29 Trauma diagnosis, 30 >3 day in ICU 25 Post‐hospital characteristics Death, 17 , 31 , 32 Readmission in the 2 months postdischarge, 33 Residing in institution post‐ICU 33 |
Demographic characteristics Younger, 34 , 35 Female, 16 , 27 , 28 , 29 , 31 , 33 , 36 Parent, 19 Spouse, 16 , 17 , 26 Child, 30 , 32 , 35 White, 37 Financial insufficiency, 24 Lower educational level, 22 , 30 Higher educational level, 27 Lower socioeconomic status, 26 , 35 , 38 Pain medication use, 24 Poor health status at enrollment, 33 Living alone, 36 Rural residence, 28 Perceived contradictions in the information provided by caregiver's 16 Religious and spiritual beliefs |
Communication and information Unsatisfactory communication in ICU, 17 , 28 Unsatisfactory communication with physician, 36 Help being received by general practitioner, 16 No regular nurse‐physician meetings, 16 No dedicated family meeting room, 16 Role incongruence in decision‐making, 31 Insufficient information about disease, prognosis, and treatment, 20 , 39 Contradictions in the information given 16 ,Desire for help from a psychologist 16 Family's experience at patient's death Present at death, 36 Difficult experience with dying and death 23 Resilience High resilience score 40 Caregiver support Participate in care, 41 Higher level of caregiving to patient, 42 Caregiver strain high, 43 Paid help for caregiver 44 Environment |
| 3–6 months after ICU discharge | ||
|
Demographic characteristics Congestive heart failure, 17 Cancer 17 Clinical characteristics Surgical procedure, 17 Severalty of illness, 17 Poor neurological outcome, 45 Post‐hospital characteristics |
Demographic characteristics Female, 17 , 46 Parent, 17 Child, 17 Hispanic, 46 Unemployment, 45 Lower educational level, 46 Used psychiatric medication 45 , 46 |
Communication and information Unsatisfactory communication in ICU, 17 Sharing in decisions in the ICU, 17 Involvement in ICU decisions, 17 Feeling that information was incomplete, 17 Family meeting conducted, 47 Time delay to get information from ICU staff, 45 Low perceived satisfaction with patient relationship, 48 Caregiver support Paid help for caregiver 44 Family's experience at patient's death End‐of‐life decision‐making, 17 Difficult experience with dying and death, 49 Witnessing cardiopulmonary resuscitation 45 |
| 6 months after ICU discharge | ||
|
Demographic characteristics Male 21 Clinical characteristics Tracheostomy, 21 Post‐hospital characteristics Residing in institution post‐ICU, 50 Functional dependency, 21 Poor health post‐ICU, 50 Higher depression score, Higher anxiety score, Higher PTSD score at 6 months, 51 Increased PTSD, 52 Higher PTSD score, 52 Increased anxiety, depression, PTSD 53 |
Demographic characteristics Younger, 11 , 54 Older, 44 Female 36 , 55 Parent, 54 Family surrogates, 47 Sick leave, 54 Comorbidity, 54 Recent personal experience of serious physical illness, 55 Living alone 36 |
Communication Poor communication between physicians and relatives, 36 Refusal of treatment by the patient, patient died while intubated 36 Family's experience at patient's death Present at death, 36 Relatives did not say goodbye to the patient 36 Caregiver support Paid help for caregiver, 44 Less social support 11 Caregiver mastery Less personal growth for caregiver, 11 Less sense of control over life, 11 Low level of hope 54 |
Abbreviations: ICU, intensive care unit; PTSD, post‐traumatic stress disorder.
Risk factors of patients associated with PICS‐F < 3 months after ICU discharge included younger age, 16 , 17 , 18 , 19 older age, 20 male sex, 21 and lower educational level 22 as demographic characteristics. Clinical characteristics of patients included severity of illness, 17 , 20 delirium, 23 and prolonged ICU stay 24 , 25 , 26 , 27 , 28 and mechanical ventilation. 29
Regarding family factors, demographic characteristics of family associated with increased risk of PICS‐F consistently included younger age, 11 , 34 , 35 , 54 female sex, 16 , 17 , 27 , 28 , 29 , 31 , 33 , 36 , 46 , 49 , 55 and parental status 17 , 19 , 54 across all time periods. Higher or lower educational level, 22 , 27 , 30 financial insufficiency, 24 lower socioeconomic status, 26 , 35 , 38 living alone, 36 and religious beliefs 29 , 35 were associated with an increased risk of PICS‐F < 3 months after ICU discharge.
Regarding protective factors, throughout all time periods, unsatisfactory communication with physicians and nurses, 16 , 17 , 28 , 36 and provision of information were associated with increased PICS‐F. 16 , 17 , 20 , 39 , 45 In addition, higher family resilience was associated with lower PICS‐F symptoms <3 months after ICU discharge. 40 At 3–6 months after ICU discharge, difficult experience with death and dying, 49 and witnessing cardiopulmonary resuscitation 45 were family experience at the time of the patient's death that were characteristic risk factor for PICS‐F. Involvement in decision‐making in the ICU was also a common risk factor for PICS‐F < 6 months after ICU discharge. 17 , 31 The PICS‐F protective factors more than 6 months after ICU discharge were related to the level of mastery as a caregiver; less personal growth for the caregiver, 11 less sense of control over life, 11 and low level of hope, 54 were associated with increased risk factors for PICS‐F.
Some of these risk factors for PICS‐F (psychological disorders) are invariant factors, such as age and gender, but others, such as unsatisfactory communication with physicians and nurses, are factors open to intervention. These protective factors should be the focus of future research, because they may be useful in the prevention of PICS‐F. Risk factors for PICS‐F other than psychological disorders, such as family physical symptoms and socioeconomic factors, remain unknown and also require further study. Of several risk factors, greater resilience and strong religious beliefs may reduce psychological symptoms; therefore, their details are further showed.
Resilience
Connor and Davidson reported that resilience suppresses PTSD and defined it as “the quality in individuals that makes them able to weather difficulties well, allowing them to develop from the experience”. 56 Resilience is the ability to accept traumatic events or stressful situations positively, and it is one of the psychological factors that protect against psychiatric symptoms such as PICS‐F. From around the 1950s, it was noted that some children who had been abused by their parents and lived in a harsh environment grew up to be adults who were healthy and did not suffer from mental illness. 57 The research into the psychological state of these adults was the background to the birth of this concept. After that, the word of resilience began to be used from the 1970s. In the 2000s, research on resilience began to be conducted targeting families of HIV patients 58 , 59 , dementia patients 60 , 61 , and families of palliative care patients 62 , 63 whose medical conditions are difficult to recover from. Several scales for measuring resilience have been developed, and the Conner‐Davidson Resilience Scale (CD‐RISC) is the scale that has been translated and developed into a Japanese version and used in PICS‐F research 56 ; it is a scale developed to be able to easily measure resilience in the general population and clinical settings. It consists of 25 items that are self‐administered and scored on a 5‐point scale (0–4), with higher scores indicating higher resilience. One study has clarified the relationship between PICS‐F and resilience using this CD‐RISC. 40
Religious beliefs
Religious beliefs are considered to be psychological coping, and several studies examined how religious beliefs affect psychological symptoms and behavioral patterns, targeting people with difficulties. 18 , 35 , 64 , 65 Since the late 2000s, studies clarifying the relationship between psychological states and religious beliefs in people with disease have examined the relationship between families' religious beliefs in patients with advanced cancer and gynecological cancer. 64 , 65 A study related to PICS‐F reported that PICS‐F decreased as the degree of family religious belief increased. 35 Since religious beliefs vary widely among religions and races, it is important to understand this when interpreting the results of a PICS‐F study.
ASSESSMENT OF PICS‐F
There are no universally accepted tools for assessing PICS‐F, and the assessment tools vary widely among studies (Table 2). Both anxiety and depression are commonly assessed using the Hospital Anxiety and Depression Scale (HADS). 76 , 77 Anxiety is also assessed using Patient Health Questionnaire (PHQ) 9 or PHQ 8, which omits suicide and hurting thought questions from PHQ 9. 67 CES‐D (Center for Epidemiologic Studies Depression) is also used to screen for depression. 69 PTSD can be assessed using the Impact of Event Scale (IES) or PTSD checklist (PCL). From the IES, IES‐R and IES‐6 are used to assess PTSD. The Society of Critical Care Medicine proposed the cutoff values of 1.6 and 1.75, the averages, for the IES‐R and IES‐6, respectively. 66 , 78 From the PCL, PCL‐5, PCL‐S, and PCL‐C are used to assess PTSD. It is important to note that PCL‐5 is based on DSM‐V criteria.
TABLE 2.
Instruments to assess PICS‐F.
| Family after hospital discharge | Items | Score range | Cutoff | Features | |
|---|---|---|---|---|---|
| Anxiety or depression | HADS (Hospital Anxiety and Depression Scale) | 14 | 0–21 | ≥8 66 | |
| Depression | PHQ‐9 (Patient Health Questionnaire‐9) | 9 | 0–27 | ≥10 67 | Omitting suicide and hurting thought question |
| PHQ‐8 (Patient Health Questionnaire‐8) | 8 | 0–24 | ≥10 68 | ||
| CES‐D (Center for Epidemiologic Studies Depression) | 20 | 0–60 | ≥16 or 20 69 , 70 | ||
| PTSD | IES‐R (Impact of Event Scale‐Revised) | 22 | 0–4 (average) | >1.6 at average 66 | Based on DSM‐IV |
| IES‐6 (Impact of Event Scale‐6) | 6 | 0–4 (average) | >1.75 at average 66 | Short version of IES‐R | |
| PCL‐5 (PTSD Checklist‐5) | 20 | 0–80 | ≥28 or 37 71 | Based on DSM‐V | |
| PCL‐S or ‐C (PTSD Checklist for Specific or Civilian version) | 17 | 17–85 | ≥28 or 30 72 | PCL‐S asks symptoms related to a specified event | |
| Complicated grief | ICG (Inventory of complicated grief) | 19 | 0–76 | ≥25 or 30 73 | Internal consistency, convergent and criterion validity |
| Sleep | PSQI (Pittsburgh Sleep Quality Index) | 9 | 0–21 | > (sleep disturbance) 74 | Sleep quality, latency, duration, efficiency, disturbance, medication, daytime sleep dysfunction |
| Quality of life | SF‐36 (Short Form‐36) | 36 | 0–100 | NA | Usage fee required, physical, pain, general health, vitality, social, emotional, psychological |
| Quality of care | FS‐ICU 24 (Family Satisfaction in the ICU) | 24 | 0–100 | NA | Family's assessment of quality of patient's care in the ICU |
| Caregiver burden | Zarit‐12 (Zarit Burden Interview 12 items) | 12 | 0–48 | 13 75 | Social, psychological, physical burden of caregivers |
Abbreviations: DSM, Diagnostic and Statistical Manual of Mental Disorders; ICU, intensive care unit; NA, not applicable; PTSD, post‐traumatic stress disorder.
Other than the psychological problems of PICS‐F, families experience various difficult situations. It is important to assess various aspects of PICS‐F other than psychological problems. The complicated grief following a patient's death is objectively assessed using the Inventory of Complicated Grief (ICG). This hardness can cause sleep disturbance in families. The Pittsburgh Sleep Quality Index (PSQI) can assess sleep quality, latency, duration, efficiency, disturbance, medication, and daytime sleep dysfunction of families. Impaired of QOL can be generally assessed using SF‐36, as in a previous study. 10 For health care providers, it is important to understand the needs and expectations of families during their ICU stay. The family's experience in the ICU can be assessed using Family Satisfaction in the ICU (FS‐ICU). 79 One of the important aspects of PICS‐F is the assessment of the care burden of patients. It is important to note that families have a tremendous burden regarding patient care. This burden can be assessed using Zarit Burden Interview 12 items (Zarit‐12). 80
TIMING TO ASSESS PICS‐F
The timing of evaluations for PICS‐F is important in understanding and addressing the challenges faced by families of ICU patients. Evaluating PICS‐F at the optimal timing allows for comprehensive assessment and management of the family's needs. The Society of Critical Care Medicine recommended screening for PICS within 2–4 weeks of hospital discharge in ICU survivors, 66 but the timing of screening and follow‐up for PICS‐F is unclear. It is essential to align the evaluations with the patient’ trajectories. Evaluating PICS‐F too early during this period may not capture the full extent of the family's challenges. Furthermore, too‐late evaluation may miss the opportunity to manage those with PICS‐F. Because there are no organized criteria for evaluation timing, the timing of evaluation and the frequency of PICS‐F at the evaluation timing in previous studies are summarized in Table 3. According to this summary, the assessment was frequently conducted at 3‐month or 6‐month time points, although the beginning of the assessment varied among studies.
TABLE 3.
Timing to assess PICS‐F.
| <1 month | 1–2 months | 3 months | 3–6 months | 6 months | 12 months | |
|---|---|---|---|---|---|---|
| Anxiety | 62% 51 | 35% 51 | 49% 17 | 24% 51 | 32% 81 | |
| 42% 34 | 21% 34 | 67% 82 | 15% 34 | |||
| 22% 47 | 10% 83 , b | 3% 47 | ||||
| 9% 47 | 40% 81 | |||||
| 42% 81 | ||||||
| Depression | 31% 51 | 8% 34 | 20% 17 | 6% 34 | 27% 11 | |
| 16% 34 | 42% 47 | 56% 82 | 24% 11 | |||
| 53% 11 | 61% 35 | 29% 11 | 18% 84 , a | |||
| 27% 83 , b | 11.4% 47 | |||||
| 21% 47 | ||||||
| PTSD | 36% 85 | 33% 17 | 49% 51 | 24% 85 | ||
| 69% 82 | 35% 34 | |||||
| 10% 83 , b | 14% 84 , a | |||||
| 64% 46 | 48% 46 | |||||
| 25% 85 | 22% 85 | |||||
| 30%–34% 86 | ||||||
| Complicated Grief | 5% 83 , b | 46% 34 | ||||
| Fatigue | 53% 87 | 45% 87 | 50% 87 | |||
| Sleep disorder | 63% 88 | 55% 88 | 54% 88 | |||
| 54% 89 | 54% 89 |
Note: The beginning of follow‐up varies from ICU discharge, hospital discharge, and some research time point. However, within one month, the period during which the patient was admitted to the ICU is included.
Abbreviations: ICU = intensive care unit; PTSD, post‐traumatic stress disorder.
This study followed‐up for at least 6 months after a patient's death.
This study followed‐up at 3–12 months after a patient's death.
LONGITUDINAL OUTCOMES OF EACH PICS‐F COMPONENT
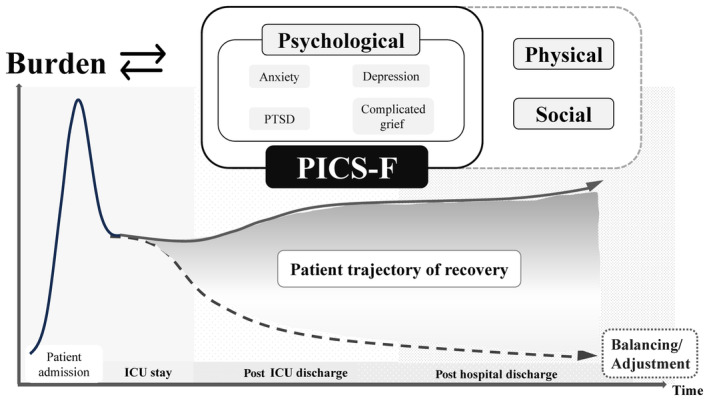
The longitudinal prevalence of PICS‐F divided into psychological and non‐psychological problems is presented in Figure 2.
FIGURE 2.
Longitudinal prevalence of PICS‐F problems. In the long term, the prevalence of PICS‐F has not changed. Non‐psychological problems refer to symptoms other than anxiety, depression, PTSD, and complicated grief, which were defined as symptoms of PICS‐F in the previous report in Critical Care Medicine in 2012.
With regard to psychological symptoms, Cameron et al. 11 reported a short‐term improvement within several months and a stable prevalence after that period in which depressive symptoms developed. Some studies examining trajectories of depressive symptoms found that a significant number of families experienced a persistently high degree of depressive symptoms over months to a year (16.4%–57.4%). 11 , 35 Similarly, Anderson et al. 34 reported a large reduction of the prevalence of anxiety symptoms for a relatively short period. Regarding post‐traumatic stress (PTS) symptoms, similar results were reported. In summary, the prevalence of psychological symptoms improves in a short period (e.g., during ICU stay to several months), and it remains almost unchanged (or sometimes even gets worse) after that period (e.g., several months to one year). This underscores the importance of early prevention and screening for high‐risk families, as well as long‐term psychological support for families with persistent symptoms. However, it might be difficult to prove the association between the event of a patient's ICU admission and the development of long‐term psychological symptoms. If the mental state of the family at the time of the patient's ICU admission can be assessed, PICS‐F could be diagnosed during long‐term follow‐up because changes in mental status of the family could be observed. Therefore, it is important to assess the family's mental status at the time of the patient's ICU admission in the diagnosis of long‐term PICS‐F. Studies examining whether the trajectories of psychological symptoms differ between symptoms (e.g., depression, anxiety, and PTS symptoms) are also required.
There are fewer studies regarding non‐psychological problems including socioeconomic problems and physical symptoms than for psychological problems. A study that examined the substantial burden of families as caregivers at 2, 6, and 12 months after ICU admission showed significant lifestyle disruption and employment reduction of families, which persisted for a year. 44 Another study showed that 44.9% of families had to quit work at 1 month, and 36.7% of families had lost savings at 1 year. 90 Families of critically ill patients may need not only psychological support, but also socioeconomic intervention. Physical symptoms such as fatigue are important, but underreported components of PICS‐F. Choi et al. 87 reported that fatigue affected almost half of the families of critically ill patients during the ICU stay, and it persisted at 4 months after ICU discharge. Sleep quality also seems to be impaired in many families of critically ill patients. At 4 months after ICU admission, more than half of families still suffered from poor quality of sleep, as well as during the ICU stay. 88 Of note, these physical symptoms were reported to be correlated with their psychological symptoms. 87 , 89 These physical symptoms could be therapeutic targets in families with PICS‐F.
PREVENTION OF PICS‐F
Families of ICU patients need to be given and understand accurate information such as the patient's diagnosis, planned care, and prognosis. In addition, they need to inform others about their concerns, needs, and distress to relieve themselves. To address these issues, various communication tools, personnel, and support systems (teams) have been evaluated, and these studies have mainly been conducted in France. 52 , 86 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 More details on each are provided below.
Provide family information leaflet
One randomized, controlled trial (RCT) investigated whether providing a Family Information Leaflet improved anxiety and depression of families during ICU stays. 91 The leaflet provided general information on the ICU and hospital, the name of the ICU physician caring for the patient, a diagram of a typical ICU room with the names of all the devices, and a glossary of 12 terms commonly used in the ICU. Although the Family Information Leaflet did not significantly decrease symptoms of anxiety and depression of families during ICU stays, it significantly improved families' comprehension of the diagnosis and treatment. On the other hand, family satisfaction was not significantly associated with delivery of the leaflet, but among families with good comprehension those who received the leaflet had significantly better satisfaction scores than those who did not. These data suggest that comprehension is a foundation from which other benefits, such as better satisfaction, can arise. Azoulay et al. 92 conducted a prospective observational study to identify factors associated with poor comprehension by families of ICU patients. They found that failure to give the representative family member an information brochure was one of the factors associated with poor comprehension by families. More importantly, this leaflet both provided information and extended an invitation to talk with ICU caregivers. Therefore, the leaflet not only provides information from the ICU caregivers to the families, but it is also a tool to facilitate interactive communication between families and healthcare providers.
Intensive care unit diaries
The idea of keeping diaries for unconscious patients came initially from Denmark in 1984, where notes were made concerning events that had happened to the patients or in their personal environment, sometimes also noting what was happening in the world outside. 93 Since then, ICU diaries have long been used in Denmark, Norway, Sweden, Switzerland, and the United Kingdom for rebuilding the narrative of a life disrupted by illness with loss of patients' memory. 52 In recent years, the effectiveness of ICU diaries not only for patients, but also for their families has been examined. Three RCTs 86 , 94 , 95 and one before‐after study 52 examined the effects of ICU diaries written by nurses and families of patients on the psychological condition of relatives. One study reported no difference in families' PTSD, depression, and anxiety between the group that received or did not receive the ICU diary. 86 The remaining three studies showed a decrease in families' PTSD, 52 , 94 , 95 but depression and anxiety showed no improvement, except in the study of Garrouste et al. 52 A systematic review and meta‐analysis of the effect of ICU diaries on patients and families including the abovementioned four studies showed that there was no difference in the incidence of families' PTSD between those who received the ICU diary and those who did not. 96 Therefore, ICU diaries do not seem to have any beneficial effect on the families of ICU patients. However, ICU diaries provide families with information written in easily understandable terms and are available for review at any time during the ICU stay, and they are among the tools that can help improve communication between healthcare providers and families. 52
Communication facilitators
Facilitators, such as nurses and social workers trained to improve communication between the ICU team and family participate in family conferences and serve as a bridge between family members and physician communication by confirming the family's understanding and needs after the physician has explained the patient's medical condition. In addition, 24‐h follow‐up with the families may be provided after the patient's discharge from the ICU. 97 Curtis et al. 98 conducted an RCT in the USA that examined the usefulness of ICU communication facilitators. The facilitators received 2 days of special training from investigators who were experts in each component based on the evidence on clinician‐family communication. 98 They found that communication facilitators might be associated with decreased family depressive symptoms at 6 months after ICU discharge. In another study, Garrouste et al. 99 conducted an RCT to investigate family perceptions of having a nurse participating in family conferences and to assess the psychological symptoms of the families after ICU discharge. Although the participation of a nurse in the conferences did not significantly decrease symptoms of anxiety, depression, and PTSD 3 months after patient death or ICU discharge, it was considered positive by the families. Shelton et al. also conducted a nonrandomized, controlled trial, which included a prospective, observational study of ICU decision‐making and satisfaction (Phase I) and a controlled, clinical trial to test the intervention's effect (Phase II), to examine the effect of adding a full‐time family support coordinator to the surgical intensive care unit team on family satisfaction. 100 They found that the family support coordinator was associated with increases in family satisfaction with communication. Therefore, the intervention of facilitators trained in communication may be useful in increasing families' understanding and satisfaction with information in the ICU.
Support grief care with a condolence letter on grief/ bereavement brochure
In cases of dying or deceased ICU patients, caring for families by a condolence letter or the use of a bereavement brochure in the end‐of‐life conferences has been examined. 101 , 102 Kentish et al. 101 showed that handwritten condolence letters sent by physician and nurses 15 days after the patient's death might lead to increased symptoms of depression and PTSD in families. However, this study had an important limitation. Because the psychological status of the relatives at the time they received the condolence letter was not evaluated, it cannot be said that sending a condolence letter had a direct effect on the family's psychological state. This factor may have an influence on the effect of a condolence letter, and the kinetics of grieving remain unclear. Nancy et al. showed that the three‐step support strategy for families, including a family conference to prepare the relatives for the imminent death, an ICU room visit to provide active support, and a meeting after the patient's death to offer condolences and closure might be helpful to reduce prolonged grief symptoms of families. 103 The use of a condolence letter as part of a step‐by‐step communication process might have a positive effect. Lautrette et al. 102 showed that the use of a bereavement brochure in the end‐of‐life conference in the ICU might be helpful to reduce symptoms of anxiety, depression, and PTSD of families. However, the only criterion for inclusion in this study was the belief on the part of the physician in charge that death was inevitable and that a decision to forgo life‐sustaining treatment was in order; so in some cases, patients in such circumstances might survive, and it is possible that the evaluation lacks accuracy as grief care. Stephana et al. 104 also found that the evidence is modest in scope in a systematic review and narrative synthesis of RCTs evaluating bereavement interventions in adult ICUs targeting informal caregivers, and deeper understanding of which interventions are most effective, for whom, at what time, and in which contexts, is required. Therefore, several further studies of grief care are needed because of the strong limitations of previous reports.
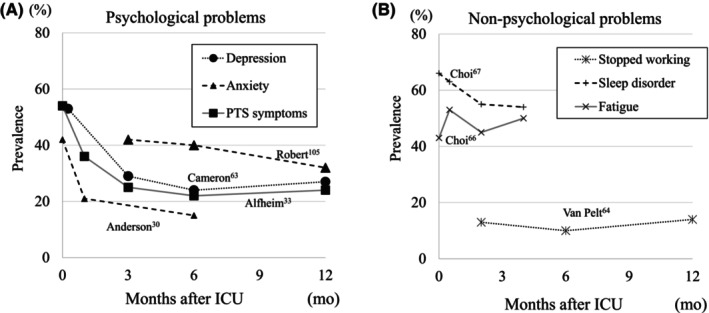
Bundle for PICS‐F prevention
Many of these interventions that are considered useful in the prevention of PICS‐F improve comprehension and satisfaction of families, and build good communication between ICU caregivers and families. However, these interventions may not work for all families. A condolence letter, for example, may be too strong a factor triggering painful memories for some families. Therefore, it may be important to make the tool one of proactive availability for families, rather than one‐way information from the ICU caregivers for the prevention of PICS‐F. The interventions described above can be divided mainly into those performed during the ICU stay and those performed after ICU discharge. Some of the interventions are initiated during the ICU stay and are continued after discharge from the ICU. Importantly, the effectiveness of a single intervention alone is limited. In addition, the patient's recovery process is also important for the family's psychological status. 105 Thus, prevention of PICS‐F requires a continuous bundle of multifaceted and/or multidisciplinary interventions for the patient and families from during the ICU stay to after discharge from the ICU 106 (Figure 3). The Guidelines published by the Society of Critical Care Medicine in 2007 and 2017 provided recommendations to improve the psychological status of families of patients admitted to the ICU, and they recommended relaxing restrictions on family visitation. 107 , 108 However, the studies that provided evidence for the recommendations were mainly derived from nonrandomized trials, so future large‐scale research is needed to establish recommendations for prevention and treatment of PICS‐F.
FIGURE 3.
The bundle for PICS‐F prevention. The prevention of PICS‐F requires a continuous bundle of multifaceted and/or multidisciplinary interventions for the patient and families from during the ICU stay to after discharge from the ICU. The elements of the bundle are arranged in chronological order from top to bottom. “Provide Leaflet” means that an informational booklet for families is given at the time of ICU admission. “ICU diary” is a daily record of events during the patient's stay in the ICU that the patients and families can look back on after leaving the ICU. “Communication facilitators” means persons to facilitate communication between the healthcare provider and the patient's family during ICU admission. “Support grief care” means support for grief care through a condolence letter on grief and bereavement brochure. “Follow‐up after ICU discharge” means that family follow‐up should be continued after discharge from the ICU to detect PICS‐F earlier.
LIMITATIONS
There were several limitations regarding the present review. First, symptoms of anxiety, depression, and PTSD were not evaluated at baseline in families, and it is difficult to compare them due to different assessment periods. Second, risk factors were only related to psychological symptoms of families. Third, there might be selection bias because this was not a systematic review. Fourth, the sample size of studies of references were small, and many of the studies were conducted in France. There have also been no studies discussing differences in PICS‐F depending on the type of ICU; therefore, these results could not be generalized, and more studies comparing international differences or ICUs are desired in the future.
CONCLUSIONS
PICS‐F has been described as a devastated life, encompassing psychological, physical, and socioeconomic burdens that begin with the emotional impact experienced by the family when the patient is admitted to the ICU. It is important to emphasize that PICS‐F needs to be extended beyond the psychological impairments of the families to the physical and socioeconomical impairments in the future, and the family health condition may adversely affect the patient's recovery.
PICS‐F can be prevented using a continuous bundle of multifaceted and/or multidisciplinary interventions for the patient and families from during the ICU stay to after discharge from the ICU. Further research will be needed to examine the efficacy of such interventions.
CONFLICT OF INTEREST STATEMENT
Nobuyuki Nosaka is working on the research about PICS‐F under funding from SHARP CORPORATION, but he has not received any direct support for the manuscript. Nobuyuki Nosaka is also working on the research about PICS and PICS‐F under funding from LIXIL Corporation, but he has not received any direct support for the manuscript. The remaining authors have disclosed that they do not have any potential conflicts of interest.
APPROVAL OF THE RESEARCH PROTOCOL
N/A.
INFORMED CONSENT
N/A.
REGISTRY AND THE REGISTRATION NO. OF THE STUDY/TRIAL
N/A.
ANIMAL STUDIES
N/A.
Shirasaki K, Hifumi T, Nakanishi N, Nosaka N, Miyamoto K, Komachi MH, et al. Postintensive care syndrome family: A comprehensive review. Acute Med Surg. 2024;11:e939. 10.1002/ams2.939
Kasumi Shirasaki and Toru Hifumi contributed equally to this work.
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- 1. Kentish‐Barnes N, Lemiale V, Chaize M, Pochard F, Azoulay E. Assessing burden in families of critical care patients. Crit Care Med. 2009;37(10 Suppl):S448–S456. [DOI] [PubMed] [Google Scholar]
- 2. Netzer G, Sullivan DR. Recognizing, naming, and measuring a family intensive care unit syndrome. Ann Am Thorac Soc. 2014;11(3):435–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kang J. Being devastated by critical illness journey in the family: a grounded theory approach of post‐intensive care syndrome‐family. Intensive Crit Care Nurs. 2023;78:103448. [DOI] [PubMed] [Google Scholar]
- 4. McPeake J, Auriemma CL, Harhay MO. Understanding the impact of critical illness on families: a call for standardization of outcomes and longitudinal research. Ann Am Thorac Soc. 2021;18(11):1783–1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome‐family. Crit Care Med. 2012;40(2):618–624. [DOI] [PubMed] [Google Scholar]
- 6. Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long‐term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40(2):502–509. [DOI] [PubMed] [Google Scholar]
- 7. Milton A, Schandl A, Larsson IM, Wallin E, Savilampi J, Meijers K, et al. Caregiver burden and emotional wellbeing in informal caregivers to ICU survivors‐a prospective cohort study. Acta Anaesthesiol Scand. 2022;66(1):94–102. [DOI] [PubMed] [Google Scholar]
- 8. Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, et al. Post‐intensive care syndrome: its pathophysiology, prevention, and future directions. Acute Med Surg. 2019;6(3):233–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hiser SL, Fatima A, Ali M, Needham DM. Post‐intensive care syndrome (PICS): recent updates. J Intensive Care. 2023;11(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lemiale V, Kentish‐Barnes N, Chaize M, Aboab J, Adrie C, Annane D, et al. Health‐related quality of life in family members of intensive care unit patients. J Palliat Med. 2010;13(9):1131–1137. [DOI] [PubMed] [Google Scholar]
- 11. Cameron JI, Chu LM, Matte A, Tomlinson G, Chan L, Thomas C, et al. One‐year outcomes in caregivers of critically ill patients. N Engl J Med. 2016;374(19):1831–1841. [DOI] [PubMed] [Google Scholar]
- 12. Choi J, Lingler JH, Donahoe MP, Happ MB, Hoffman LA, Tate JA. Home discharge following critical illness: a qualitative analysis of family caregiver experience. Heart Lung. 2018;47(4):401–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Verceles AC, Corwin DS, Afshar M, Friedman EB, McCurdy MT, Shanholtz C, et al. Half of the family members of critically ill patients experience excessive daytime sleepiness. Intensive Care Med. 2014;40(8):1124–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. van Beusekom I, Bakhshi‐Raiez F, de Keizer NF, Dongelmans DA, van der Schaaf M. Reported burden on informal caregivers of ICU survivors: a literature review. Crit Care. 2016;20:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stayt LC, Venes TJ. Outcomes and experiences of relatives of patients discharged home after critical illness: a systematic integrative review. Nurs Crit Care. 2019;24(3):162–175. [DOI] [PubMed] [Google Scholar]
- 16. Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, et al. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision‐making capacity. Crit Care Med. 2001;29(10):1893–1897. [DOI] [PubMed] [Google Scholar]
- 17. Azoulay E, Pochard F, Kentish‐Barnes N, Chevret S, Aboab J, Adrie C, et al. Risk of post‐traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987–994. [DOI] [PubMed] [Google Scholar]
- 18. Fumis RR, Ranzani OT, Martins PS, Schettino G. Emotional disorders in pairs of patients and their family members during and after ICU stay. PloS One. 2015;10(1):e0115332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kose I, Zincircioglu C, Ozturk YK, Çakmak M, Güldoğan EA, Demir HF, et al. Factors affecting anxiety and depression symptoms in relatives of intensive care unit patients. J Intensive Care Med. 2016;31(9):611–617. [DOI] [PubMed] [Google Scholar]
- 20. Rusinova K, Kukal J, Simek J, Cerny V, Group DSW . Limited family members/staff communication in intensive care units in the Czech and Slovak republics considerably increases anxiety in patients relatives – the DEPRESS study. BMC Psychiatry. 2014;14:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Van Pelt DC, Schulz R, Chelluri L, Pinsky MR. Patient‐specific, time‐varying predictors of post‐ICU informal caregiver burden: the caregiver outcomes after ICU discharge project. Chest. 2010;137(1):88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Paparrigopoulos T, Melissaki A, Efthymiou A, Tsekou H, Vadala C, Kribeni G, et al. Short‐term psychological impact on family members of intensive care unit patients. J Psychosom Res. 2006;61(5):719–722. [DOI] [PubMed] [Google Scholar]
- 23. Rosgen BK, Krewulak KD, Davidson JE, Ely EW, Stelfox HT, Fiest KM. Associations between caregiver‐detected delirium and symptoms of depression and anxiety in family caregivers of critically ill patients: a cross‐sectional study. BMC Psychiatry. 2021;21(1):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tang ST, Huang CC, Hu TH, Chou WC, Chuang LP, Chiang MC. Course and predictors of posttraumatic stress‐related symptoms among family members of deceased ICU patients during the first year of bereavement. Crit Care. 2021;25(1):282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Andresen M, Guic E, Orellana A, Diaz MJ, Castro R. Posttraumatic stress disorder symptoms in close relatives of intensive care unit patients: prevalence data resemble that of earthquake survivors in Chile. J Crit Care. 2015;30(5):1152.e7–11. [DOI] [PubMed] [Google Scholar]
- 26. Celik S, Genc G, Kinetli Y, Asiliogli M, Sari M, Madenoglu KM. Sleep problems, anxiety, depression and fatigue on family members of adult intensive care unit patients. Int J Nurs Pract. 2016;22(5):512–522. [DOI] [PubMed] [Google Scholar]
- 27. Chui WY, Chan SW. Stress and coping of Hong Kong Chinese family members during a critical illness. J Clin Nurs. 2007;16(2):372–381. [DOI] [PubMed] [Google Scholar]
- 28. Belayachi J, Himmich S, Madani N, Abidi K, Dendane T, Zeggwagh AA, et al. Psychological burden in inpatient relatives: the forgotten side of medical management. QJM. 2014;107(2):115–122. [DOI] [PubMed] [Google Scholar]
- 29. Fumis RR, Deheinzelin D. Family members of critically ill cancer patients: assessing the symptoms of anxiety and depression. Intensive Care Med. 2009;35(5):899–902. [DOI] [PubMed] [Google Scholar]
- 30. Pillai L, Aigalikar S, Vishwasrao SM, Husainy SM. Can we predict intensive care relatives at risk for posttraumatic stress disorder? Indian J Crit Care Med. 2010;14(2):83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Smith OM, Metcalfe K, Puts M, McDonald E, Sue‐Chee S, Friedrich JO. Role incongruence and psychological stress symptoms in substitute decision makers of intensive care patients. Am J Crit Care. 2020;29(4):301–310. [DOI] [PubMed] [Google Scholar]
- 32. Petrinec AB, Mazanec PM, Burant CJ, Hoffer A, Daly BJ. Coping strategies and posttraumatic stress symptoms in post‐ICU family decision makers. Crit Care Med. 2015;43(6):1205–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Douglas SL, Daly BJ, O'Toole E, Hickman RL Jr. Depression among white and nonwhite caregivers of the chronically critically ill. J Crit Care. 2010;25(2):364.e11–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Anderson WG, Arnold RM, Angus DC, Bryce CL. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med. 2008;23(11):1871–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Choi J, Sherwood PR, Schulz R, Ren D, Donahoe MP, Given B, et al. Patterns of depressive symptoms in caregivers of mechanically ventilated critically ill adults from intensive care unit admission to 2 months postintensive care unit discharge: a pilot study. Crit Care Med. 2012;40(5):1546–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kentish‐Barnes N, Chaize M, Seegers V, Legriel S, Cariou A, Jaber S, et al. Complicated grief after death of a relative in the intensive care unit. Eur Respir J. 2015;45(5):1341–1352. [DOI] [PubMed] [Google Scholar]
- 37. Athavale AM, Callahan CM, Sachs GA, Wocial LD, Helft PR, Monahan PO, et al. Communication quality predicts psychological well‐being and satisfaction in family surrogates of hospitalized older adults: an observational study. J Gen Intern Med. 2018;33(3):298–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kao YY, Chen CI, Chen FJ, Lin YH, Perng SJ, Lin HY, et al. Effects of resourcefulness on sleep disturbances, anxiety, and depressive symptoms in family members of intensive care unit patients. Arch Psychiatr Nurs. 2016;30(5):607–613. [DOI] [PubMed] [Google Scholar]
- 39. Zimmerli M, Tisljar K, Balestra GM, Langewitz W, Marsch S, Hunziker S. Prevalence and risk factors for post‐traumatic stress disorder in relatives of out‐of‐hospital cardiac arrest patients. Resuscitation. 2014;85(6):801–808. [DOI] [PubMed] [Google Scholar]
- 40. Sottile PD, Lynch Y, Mealer M, Moss M. Association between resilience and family member psychologic symptoms in critical illness. Crit Care Med. 2016;44(8):e721–e727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Azoulay E, Pochard F, Chevret S, Arich C, Brivet F, Brun F, et al. Family participation in care to the critically ill: opinions of families and staff. Intensive Care Med. 2003;29(9):1498–1504. [DOI] [PubMed] [Google Scholar]
- 42. Im K, Belle SH, Schulz R, Mendelsohn AB, Chelluri L, Investigators Q‐M. Prevalence and outcomes of caregiving after prolonged (> or =48 hours) mechanical ventilation in the ICU. Chest. 2004;125(2):597–606. [DOI] [PubMed] [Google Scholar]
- 43. McPeake J, Devine H, MacTavish P, Fleming L, Crawford R, Struthers R, et al. Caregiver strain following critical care discharge: an exploratory evaluation. J Crit Care. 2016;35:180–184. [DOI] [PubMed] [Google Scholar]
- 44. Van Pelt DC, Milbrandt EB, Qin L, Weissfeld LA, Rotondi AJ, Schulz R, et al. Informal caregiver burden among survivors of prolonged mechanical ventilation. Am J Respir Crit Care Med. 2007;175(2):167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Metzger K, Gamp M, Tondorf T, Hochstrasser S, Becker C, Luescher T, et al. Depression and anxiety in relatives of out‐of‐hospital cardiac arrest patients: results of a prospective observational study. J Crit Care. 2019;51:57–63. [DOI] [PubMed] [Google Scholar]
- 46. Amass T, Van Scoy LJ, Hua M, Ambler M, Armstrong P, Baldwin MR, et al. Stress‐related disorders of family members of patients admitted to the intensive care unit with COVID‐19. JAMA Intern Med. 2022;182(6):624–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tang ST, Huang CC, Hu TH, Lo ML, Chou WC, Chuang LP, et al. End‐of‐life‐care quality in ICUs is associated with family Surrogates' severe anxiety and depressive symptoms during their first 6 months of bereavement. Crit Care Med. 2021;49(1):27–37. [DOI] [PubMed] [Google Scholar]
- 48. Wintermann GB, Weidner K, Strauss B, Rosendahl J, Petrowski K. Predictors of posttraumatic stress and quality of life in family members of chronically critically ill patients after intensive care. Ann Intensive Care. 2016;6(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kentish‐Barnes N, Seegers V, Legriel S, Cariou A, Jaber S, Lefrant JY, et al. CAESAR: a new tool to assess relatives' experience of dying and death in the ICU. Intensive Care Med. 2016;42(6):995–1002. [DOI] [PubMed] [Google Scholar]
- 50. Douglas SL, Daly BJ. Caregivers of long‐term ventilator patients: physical and psychological outcomes. Chest. 2003;123(4):1073–1081. [DOI] [PubMed] [Google Scholar]
- 51. Jones C, Skirrow P, Griffiths RD, Humphris G, Ingleby S, Eddleston J, et al. Post‐traumatic stress disorder‐related symptoms in relatives of patients following intensive care. Intensive Care Med. 2004;30(3):456–460. [DOI] [PubMed] [Google Scholar]
- 52. Garrouste‐Orgeas M, Coquet I, Perier A, Timsit JF, Pochard F, Lancrin F, et al. Impact of an intensive care unit diary on psychological distress in patients and relatives*. Crit Care Med. 2012;40(7):2033–2040. [DOI] [PubMed] [Google Scholar]
- 53. Rosendahl J, Brunkhorst FM, Jaenichen D, Strauss B. Physical and mental health in patients and spouses after intensive care of severe sepsis: a dyadic perspective on long‐term sequelae testing the actor‐partner interdependence model. Crit Care Med. 2013;41(1):69–75. [DOI] [PubMed] [Google Scholar]
- 54. Alfheim HB, Hofso K, Smastuen MC, Toien K, Rosseland LA, Rustoen T. Post‐traumatic stress symptoms in family caregivers of intensive care unit patients: a longitudinal study. Intensive Crit Care Nurs. 2019;50:5–10. [DOI] [PubMed] [Google Scholar]
- 55. Lee RY, Engelberg RA, Curtis JR, Hough CL, Kross EK. Novel risk factors for posttraumatic stress disorder symptoms in family members of acute respiratory distress syndrome survivors. Crit Care Med. 2019;47(7):934–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Connor KM, Davidson JR. Development of a new resilience scale: the Connor‐Davidson resilience scale (CD‐RISC). Depress Anxiety. 2003;18(2):76–82. [DOI] [PubMed] [Google Scholar]
- 57. Rutter M, Tizard J, Yule W, Graham P, Whitmore K. Research report: Isle of Wight studies, 1964‐1974. Psychol Med. 1976;6(2):313–332. [DOI] [PubMed] [Google Scholar]
- 58. Bunupuradah T, Puthanakit T, Kosalaraksa P, Kerr SJ, Kariminia A, Hansudewechakul R, et al. Poor quality of life among untreated Thai and Cambodian children without severe HIV symptoms. AIDS Care. 2012;24(1):30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nichols S, Mahoney EM, Sirois PA, Bordeaux JD, Stehbens JA, Loveland KA, et al. HIV‐associated changes in adaptive, emotional, and behavioral functioning in children and adolescents with hemophilia: results from the hemophilia growth and development study. J Pediatr Psychol. 2000;25(8):545–556. [DOI] [PubMed] [Google Scholar]
- 60. Dias R, Simoes‐Neto JP, Santos RL, Sousa MF, Baptista MA, Lacerda IB, et al. Caregivers' resilience is independent from the clinical symptoms of dementia. Arq Neuropsiquiatr. 2016;74(12):967–973. [DOI] [PubMed] [Google Scholar]
- 61. Haley WE, Bergman EJ, Roth DL, McVie T, Gaugler JE, Mittelman MS. Long‐term effects of bereavement and caregiver intervention on dementia caregiver depressive symptoms. Gerontologist. 2008;48(6):732–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Giesbrecht M, Wolse F, Crooks VA, Stajduhar K. Identifying socio‐environmental factors that facilitate resilience among Canadian palliative family caregivers: a qualitative case study. Palliat Support Care. 2015;13(3):555–565. [DOI] [PubMed] [Google Scholar]
- 63. Sanderson C, Lobb EA, Mowll J, Butow PN, McGowan N, Price MA. Signs of post‐traumatic stress disorder in caregivers following an expected death: a qualitative study. Palliat Med. 2013;27(7):625–631. [DOI] [PubMed] [Google Scholar]
- 64. McCoubrie RC, Davies AN. Is there a correlation between spirituality and anxiety and depression in patients with advanced cancer? Support Care Cancer. 2006;14(4):379–385. [DOI] [PubMed] [Google Scholar]
- 65. Boscaglia N, Clarke DM, Jobling TW, Quinn MA. The contribution of spirituality and spiritual coping to anxiety and depression in women with a recent diagnosis of gynecological cancer. Int J Gynecol Cancer. 2005;15(5):755–761. [DOI] [PubMed] [Google Scholar]
- 66. Mikkelsen ME, Still M, Anderson BJ, Bienvenu OJ, Brodsky MB, Brummel N, et al. Society of Critical Care Medicine's international consensus conference on prediction and identification of Long‐term impairments after critical illness. Crit Care Med. 2020;48(11):1670–1679. [DOI] [PubMed] [Google Scholar]
- 67. Levis B, Sun Y, He C, Wu Y, Krishnan A, Bhandari PM, et al. Accuracy of the PHQ‐2 alone and in combination with the PHQ‐9 for screening to detect major depression: systematic review and meta‐analysis. Jama. 2020;323(22):2290–2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shin C, Lee SH, Han KM, Yoon HK, Han C. Comparison of the usefulness of the PHQ‐8 and PHQ‐9 for screening for major depressive disorder: analysis of psychiatric outpatient data. Psychiatry Investig. 2019;16(4):300–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Wada K, Tanaka K, Theriault G, Satoh T, Mimura M, Miyaoka H, et al. Validity of the Center for Epidemiologic Studies Depression Scale as a screening instrument of major depressive disorder among Japanese workers. Am J Ind Med. 2007;50(1):8–12. [DOI] [PubMed] [Google Scholar]
- 70. Radloff LS. The CES‐D scale: a self‐report depression scale for research in the general population. Appl Psychol Measur. 1977;1(3):385–401. [Google Scholar]
- 71. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM‐5 (PCL‐5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. [DOI] [PubMed] [Google Scholar]
- 72. Weathers F, Litz B, Herman D, Huska JA, Keane T. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper Presented at the Annual Convention of the International Society for Traumatic Stress Studies . 1993.
- 73. Szuhany KL, Malgaroli M, Miron CD, Simon NM. Prolonged grief disorder: course, diagnosis, assessment, and treatment. Focus (American Psychiatric Publishing). 2021;19(2):161–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L, et al. Relationships between the Pittsburgh sleep quality index (PSQI), Epworth sleepiness scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4(6):563–571. [PMC free article] [PubMed] [Google Scholar]
- 75. Gratão ACM, Brigola AG, Ottaviani AC, Luchesi BM, Souza ÉN, Rossetti ES, et al. Brief version of Zarit burden interview (ZBI) for burden assessment in older caregivers. Dementia Neuropsychol. 2019;13(1):122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Rabiee A, Nikayin S, Hashem MD, Huang M, Dinglas VD, Bienvenu OJ, et al. Depressive symptoms after critical illness: a systematic review and meta‐analysis. Crit Care Med. 2016;44(9):1744–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Nikayin S, Rabiee A, Hashem MD, Huang M, Bienvenu OJ, Turnbull AE, et al. Anxiety symptoms in survivors of critical illness: a systematic review and meta‐analysis. Gen Hosp Psychiatry. 2016;43:23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders‐fifth edition (PCL‐5) in veterans. Psychol Assess. 2016;28(11):1379–1391. [DOI] [PubMed] [Google Scholar]
- 79. Wall RJ, Engelberg RA, Downey L, Heyland DK, Curtis JR. Refinement, scoring, and validation of the family satisfaction in the intensive care unit (FS‐ICU) survey. Crit Care Med. 2007;35(1):271–279. [DOI] [PubMed] [Google Scholar]
- 80. Zarit SH, Reever KE, Bach‐Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649–655. [DOI] [PubMed] [Google Scholar]
- 81. Robert R, Le Gouge A, Kentish‐Barnes N, Cottereau A, Giraudeau B, Adda M, et al. Terminal weaning or immediate extubation for withdrawing mechanical ventilation in critically ill patients (the ARREVE observational study). Intensive Care Med. 2017;43(12):1793–1807. [DOI] [PubMed] [Google Scholar]
- 82. Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, et al. A communication strategy and brochure for relatives of patients dying in the ICU. New England J Med. 2007;356(5):469–478. [DOI] [PubMed] [Google Scholar]
- 83. Siegel MD, Hayes E, Vanderwerker LC, Loseth DB, Prigerson HG. Psychiatric illness in the next of kin of patients who die in the intensive care unit. Crit Care Med. 2008;36(6):1722–1728. [DOI] [PubMed] [Google Scholar]
- 84. Gries CJ, Engelberg RA, Kross EK, Zatzick D, Nielsen EL, Downey L, et al. Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest. 2010;137(2):280–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Alfheim HB, Hofsø K, Småstuen MC, Tøien K, Rosseland LA, Rustøen T. Post‐traumatic stress symptoms in family caregivers of intensive care unit patients: a longitudinal study. Intensive Critical Care Nurs. 2019;50:5–10. [DOI] [PubMed] [Google Scholar]
- 86. Garrouste‐Orgeas M, Flahault C, Vinatier I, Rigaud JP, Thieulot‐Rolin N, Mercier E, et al. Effect of an ICU diary on posttraumatic stress disorder symptoms among patients receiving mechanical ventilation: a randomized clinical trial. Jama. 2019;322(3):229–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Choi J, Tate JA, Hoffman LA, Schulz R, Ren D, Donahoe MP, et al. Fatigue in family caregivers of adult intensive care unit survivors. J Pain Symptom Manage. 2014;48(3):353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Choi J, Hoffman LA, Schulz R, Tate JA, Donahoe MP, Ren D, et al. Self‐reported physical symptoms in intensive care unit (ICU) survivors: pilot exploration over four months post‐ICU discharge. J Pain Symptom Manage. 2014;47(2):257–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Choi J, Tate JA, Donahoe MP, Ren D, Hoffman LA, Chasens ER. Sleep in family caregivers of ICU survivors for two months post‐ICU discharge. Intensive Crit Care Nurs. 2016;37:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Swoboda SM, Lipsett PA. Impact of a prolonged surgical critical illness on patients' families. Am J Crit Care. 2002;11(5):459–466. [PubMed] [Google Scholar]
- 91. Azoulay E, Pochard F, Chevret S, Jourdain M, Bornstain C, Wernet A, et al. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients a multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med. 2002;165:438–442. [DOI] [PubMed] [Google Scholar]
- 92. Azoulay E, Chevret S, Leleu G, Pochard F, Barboteu M, Adrie C, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28:3044–3049. [DOI] [PubMed] [Google Scholar]
- 93. Ingegerd Bergbom CS, Berggren E, Kamsula M. Patients' and relatives' opinions and feelings about diaries kept by nurses in an intensive care unit: pilot study. Intensive and Critical Care Nursing. 1999;15:185–191. [DOI] [PubMed] [Google Scholar]
- 94. Nielsen AH, Angel S, Egerod I, Lund TH, Renberg M, Hansen TB. The effect of family‐authored diaries on posttraumatic stress disorder in intensive care unit patients and their relatives: a randomised controlled trial (DRIP‐study). Aust Crit Care. 2020;33(2):123–129. [DOI] [PubMed] [Google Scholar]
- 95. Jones C, Backman C, Griffiths RD. Intensive care diaries and relatives' symptoms of posttraumatic stress disorder after critical illness: a pilot study. Am J Crit Care. 2012;21(3):172–176. [DOI] [PubMed] [Google Scholar]
- 96. Barreto BB, Luz M, Rios MNO, Lopes AA, Gusmao‐Flores D. The impact of intensive care unit diaries on patients' and relatives' outcomes: a systematic review and meta‐analysis. Crit Care. 2019;23(1):411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Curtis JR, Ciechanowski PS, Downey L, Gold J, Nielsen EL, Shannon SE, et al. Development and evaluation of an interprofessional communication intervention to improve family outcomes in the ICU. Contemp Clin Trials. 2012;33(6):1245–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Curtis JR, Treece PD, Nielsen EL, Gold J, Ciechanowski PS, Shannon SE, et al. Randomized trial of communication facilitators to reduce family distress and intensity of end‐of‐life care. Am J Respir Crit Care Med. 2016;193(2):154–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Garrouste‐Orgeas M, Max A, Lerin T, Grégoire C, Ruckly S, Kloeckner M, et al. Impact of proactive nurse participation in ICU family conferences: a mixed‐method study. Crit Care Med. 2016;44(6):1116–1128. [DOI] [PubMed] [Google Scholar]
- 100. Burns JP, Mello MM, Studdert DM, Puopolo AL, Truog RD, Brennan TA. Results of a clinical trial on care improvement for the critically ill. Crit Care Med. 2003;31:2107–2117. [DOI] [PubMed] [Google Scholar]
- 101. Kentish‐Barnes N, Chevret S, Champigneulle B, Thirion M, Souppart V, Gilbert M, et al. Effect of a condolence letter on grief symptoms among relatives of patients who died in the ICU: a randomized clinical trial. Intensive Care Med. 2017;43(4):473–484. [DOI] [PubMed] [Google Scholar]
- 102. Lautrette A, Darmon A, Megarbane B, Joly LM, Chevret S, Adrie C, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356:469–478. [DOI] [PubMed] [Google Scholar]
- 103. Kentish‐Barnes N, Chevret S, Valade S, Jaber S, Kerhuel L, Guisset O, et al. A three‐step support strategy for relatives of patients dying in the intensive care unit: a cluster randomised trial. Lancet. 2022;399(10325):656–664. [DOI] [PubMed] [Google Scholar]
- 104. Moss SJ, Wollny K, Poulin TG, Cook DJ, Stelfox HT, Ordons AR, et al. Bereavement interventions to support informal caregivers in the intensive care unit: a systematic review. BMC Palliat Care. 2021;20(1):66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Bohart S, Egerod I, Bestle MH, Overgaard D, Christensen DF, Jensen JF. Recovery programme for ICU survivors has no effect on relatives' quality of life: secondary analysis of the RAPIT‐study. Intensive Crit Care Nurs. 2018;47:39–45. [DOI] [PubMed] [Google Scholar]
- 106. Zante B, Camenisch SA, Schefold JC. Interventions in post‐intensive care syndrome‐family: a systematic literature review. Crit Care Med. 2020;48(9):e835–e840. [DOI] [PubMed] [Google Scholar]
- 107. Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, et al. Clinical practice guidelines for support of the family in the patient‐centered intensive care unit: American College of Critical Care Medicine Task Force 2004‐2005. Crit Care Med. 2007;35(2):605–622. [DOI] [PubMed] [Google Scholar]
- 108. Davidson JE, Aslakson RA, Long AC, Puntillo KA, Kross EK, Hart J, et al. Guidelines for family‐centered Care in the Neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45(1):103–128. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


