Abstract
Aims:
To examine enrollment in the National Diabetes Prevention Program (DPP) by insured adults with prediabetes according to domains of the Health Belief Model (HBM).
Methods:
Between 2015 and 2019, University of Michigan employees, retirees, and dependents with prediabetes were offered the National DPP at no out-of-pocket cost. Individuals with prediabetes were identified and mailed letters encouraging them to enroll. We surveyed those who enrolled and a random sample of those who did not using the HBM as a framework to examine factors associated with enrollment. Analyses were performed using multivariable logistic regression models.
Results:
Of 64,131 employees, retirees, and dependents, 8131 were identified with prediabetes and 776 (9.5%) enrolled in the National DPP. Of those surveyed, 532 of 776 National DPP enrollees and 945 of 2673 non-enrollees responded to the survey (adjusted response rates 74% and 43%, respectively). Among survey respondents, factors associated with National DPP enrollment included older age, female sex, higher BMI, prediabetes awareness, greater perceived benefits of health-protective action, and one or more cues to action.
Conclusions:
Optimizing National DPP enrollment among adults with prediabetes will require identifying individuals with prediabetes, increasing personal awareness of the diagnosis, increasing perceived benefits of enrollment, and providing strong cues to action.
Keywords: Beliefs, Lifestyle, Prevention, Type 2 diabetes, Workforce
1. Introduction
In 2018, 88 million U.S. adults, or 35% of the adult population, had prediabetes.1 Prediabetes confers higher risk for diabetes and cardiovascular disease. Up to 30% of adults with prediabetes develop diabetes over 5 years and up to 70% develop diabetes over their lifetimes.2 Intensive lifestyle interventions can delay or prevent type 2 diabetes, regardless of age, sex, or racial/ethnic background.3,4 In the Diabetes Prevention Program (DPP) clinical trial, the relative risk of developing type 2 diabetes was reduced by 58% over three years with the intensive lifestyle intervention.3 The Centers for Disease Control and Prevention has adapted the DPP intensive lifestyle intervention as the National DPP, a critical first step in targeted prevention of type 2 diabetes among high-risk individuals.5
Despite a decade's long effort to expand the reach of the National DPP, uptake has been low.6 Currently, the National DPP is offered by nearly 200 suppliers at more than 750 clinical and community locations across the country, and although a variety of delivery methods (individual, group, virtual/technology-based) are offered 7, fewer than 2.4% of eligible Americans with prediabetes have enrolled.8,9 Potential explanations for the low uptake among adults with prediabetes include prediabetes unawareness,1 misperceptions about diabetes risk and the effectiveness of interventions for reducing diabetes risk,10 and low rates of referrals from primary care providers.11 Prediabetes is asymptomatic and only about 13% of adults with prediabetes report ever having been told they have the condition.12 Even when individuals with prediabetes are aware of their diagnosis, fewer than 4% report having been referred to a lifestyle intervention program by their primary care provider, and fewer than 5% of them report ever having enrolled.13
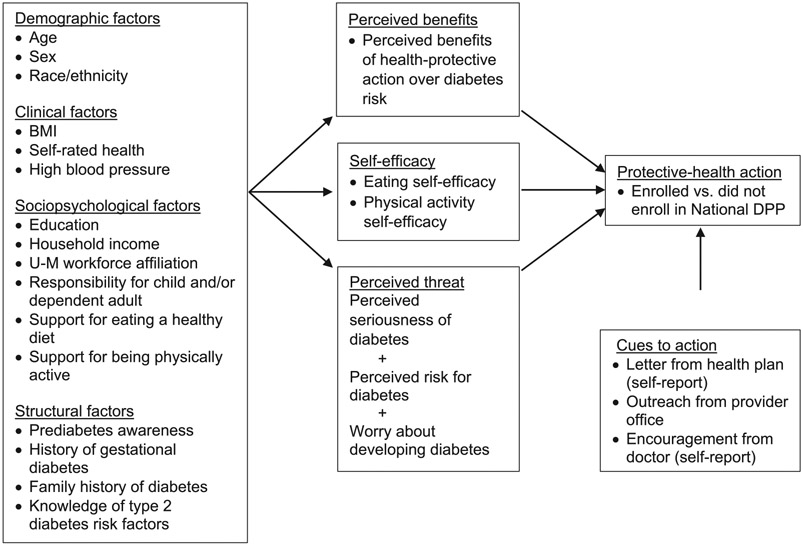
The Health Belief Model (HBM) (Fig. 1) provides a framework to understand health-protective action and to develop and refine interventions to optimize enrollment in the National DPP. According to the HBM, the likelihood that a person takes protective-health action is influenced by perceived benefits, self-efficacy, perceived threat, and internal or external events that may serve as cues to action (e.g., exposure to health information and encouragement from trusted sources).14,15 Protective-health actions are also influenced by demographic, clinical, sociopsychological, and structural factors.16
Fig. 1.
Theoretical framework based on the Health Belief Model.
BMI: Body Mass Index; DPP: Diabetes Prevention Program; U-M: University of Michigan.
Our aim was to examine relationships between domains of the HBM and National DPP enrollment to inform interventions to optimize enrollment in the National DPP to facilitate the primary prevention of type 2 diabetes among adults with prediabetes.
2. Subjects, materials and methods
Between 2015 and 2019, Premier Care, the employer-sponsored health insurance plan for University of Michigan (U-M) employees, retirees, and their dependents, offered the National DPP at no out-of-pocket cost to adults ≥18 years of age with prediabetes and overweight or obesity. Premier Care contracted four suppliers to provide the National DPP in clinical and community settings and online. Blue Care Network (BCN), the administrator of Premier Care, identified individuals with prediabetes based on absence of diabetes, administrative claims indicating prediabetes, and hemoglobin A1c (HbA1c) levels between 5.7% and 6.4%. BCN then mailed them letters encouraging them to enroll in the National DPP at no out-of-pocket cost. BCN also used a previously developed and validated algorithm17 to identify people at high risk for prediabetes and mailed them letters recommending that they be tested for prediabetes, and if diagnosed, enroll in the National DPP. To further publicize the opportunity to enroll, an email campaign was conducted to encourage U-M employees to self-screen for prediabetes using the American Diabetes Association screener.18 If positive, they were encouraged to get tested for prediabetes and if diagnosed, to enroll in the National DPP. The details of this multi-level strategy to identify individuals with prediabetes and to encourage them to enroll in the National DPP have been published.19
The U-M's policy decision to offer the National DPP at no out-of-pocket cost, to proactively identify potential participants, and to encourage enrollment provided a “natural experiment” to study relationships between National DPP enrollment and domains of the HBM.
2.1. Data collection
We used administrative data from BCN to describe the characteristics of the adults with prediabetes. We also merged residential address zip codes with data from the U.S. Census Bureau20 to describe neighborhood indicators of median household income, percent unemployment, and percent of families receiving Supplemental Nutrition Assistance Program (SNAP) benefits.
We mailed surveys to all the Premier Care members with prediabetes who enrolled in the National DPP and to a random sample of those who did not enroll. For Premier Care members with prediabetes who enrolled in the National DPP, the survey was mailed approximately 2 months after enrollment. For those who did not enroll, the survey was mailed at least 9 months after the initial invitation to enroll to ensure that those members with prediabetes had not enrolled. If we did not receive a completed survey or a postcard opting out of the survey, we mailed a reminder letter after 14 days, a second copy of the survey after 28 days, and a third copy of the survey after 42 days using Priority Mail. The study was reviewed and approved by the U-M Institutional Review Board and a waiver of written informed consent was granted. The informed consent document was mailed with the surveys and if a survey was returned, informed consent was implied.
2.2. Measurement of HBM domains
We used the survey to assess domains of the HBM including perceived benefits, self-efficacy, perceived threat, and cues to action (Fig. 1). We used a validated version21 of the Personal Control subscale from the Risk Perception Survey for Developing Diabetes (RPS-DD) to assess perceived benefits.22 Two items assess individuals' beliefs that people who make a good effort to control their risks of developing diabetes are much less likely to develop it, and that their personal efforts will help control their own risks for developing diabetes. Four response options are available for each question ranging from “strongly agree” (4) to “strongly disagree (1).” The subscale was scored as the average of the 2-items.
To assess eating self-efficacy, we used the sum of 6 items from the Weight Efficacy Lifestyle Questionnaire, which measure individuals' beliefs that they are in control of their eating and can control their desires to overeat.23 To assess physical activity self-efficacy, we used the sum of 5 items from the Self-Efficacy for Physical Activity scale, which measure peoples' beliefs that they can engage in regular physical activity.24 The items are rated on a 5-level Likert scale with 5 indicating strong agreement.
We conceptualized the domain of perceived threat as having three parts,16 perceived seriousness of diabetes, perceived risk for developing diabetes, and worry or concern about developing diabetes. We assessed perceived seriousness of diabetes using the item: “I think that diabetes is a serious health problem,” with 4 indicating strong agreement. To assess perceived risk for developing diabetes, we asked the question: “What do you think your risk is for getting diabetes over the next 5 years?” Respondents could select “almost no chance” (1), “slight chance” (2), “moderate chance” (3), or “high chance (4).” To assess worry or concern about developing diabetes, we used the Worry subscale from the RPS-DD,22 where each item had four response options ranging from “strongly agree” (4) to “strongly disagree (1).” Perceived threat of diabetes was calculated as the sum of the responses to the seriousness item, perceived risk item, and the worry subscale with a higher score indicating greater perceived threat.
Cues to action are events that can elicit health-protective actions or behaviors.16 We identified three cues to action to enrollment in the National DPP. First, survey respondents were asked if they recalled receiving a letter from BCN encouraging them to enroll in the National DPP (yes/no/not sure). “Yes” was interpreted as an affirmative response. Second, respondents were asked “Has anyone encouraged you to attend a Diabetes Prevention Program?” Selection of the response option, “Doctor,” was an event that we interpreted being a potential cue to action. Third, outreach was performed by some primary care offices in the form of a letter, portal message, or telephone call to patients with prediabetes encouraging them to enroll in the National DPP. We identified patients with prediabetes whose primary care offices engaged in such outreach.
We used the survey to assess demographic, clinical, sociopsychological, and structural factors.16 The demographic variables assessed were age, sex, and race. The clinical variables assessed were weight and height (used to calculate body mass index (BMI)), self-rated health (5 levels: Excellent = 1 to Poor = 5), and history of high blood pressure. The clinical values used were the most recent values in the year prior to the initial invitation from BCN to enroll in the National DPP. The sociopsychological variables assessed were educational attainment, household income, workforce affiliation, responsibility for caring for a child or dependent adult, support for eating a healthy diet, and support for being physically active. The structural variables assessed were prediabetes awareness, personal history of gestational diabetes, family history of diabetes, and knowledge of risk factors for type 2 diabetes. Prediabetes awareness was assessed by asking, “Do you have prediabetes?” The response options were “yes,” “no,” and “not sure.” Only an affirmative response was interpreted as awareness of prediabetes. We assessed knowledge of the risk factors for developing type 2 diabetes using the 11-item Diabetes Risk Knowledge test from the RPS-DD.22 Those who did not enroll in the National DPP were also presented a list of possible reasons for not enrolling and asked to check all that applied.
2.3. Data analysis
We used health plan administrative data and data on neighborhood indicators to compare respondents and non-respondents to the survey stratified by those who enrolled and did not enroll in the National DPP (Table A.1). Among those who enrolled and did not enroll in the National DPP, we found only small differences between respondents and non-respondents to the survey. We therefore examined associations between National DPP enrollment and domains from the HBM using data from the surveys.
We summarized data using mean ± standard deviation for continuous variables and frequency (percent) for categorical variables. We assessed differences between enrollees and non-enrollees using t-tests for continuous variables and chi-square tests for categorical variables. We tested if perceived benefits, eating and physical activity self-efficacy, perceived threat, and cues to action were associated with National DPP enrollment, first using independent logistic models, and then using a multivariable logistic regression model. Associations were also tested between the domains of the HBM and demographic, clinical, sociopsychological, and structural variables. Finally, we constructed fully-adjusted multivariate models predicting enrollment in the National DPP and used stepwise regression with p-value <0.05 for entry and > 0.05 for exit to identify the most parsimonious multivariate model. All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
3. Results
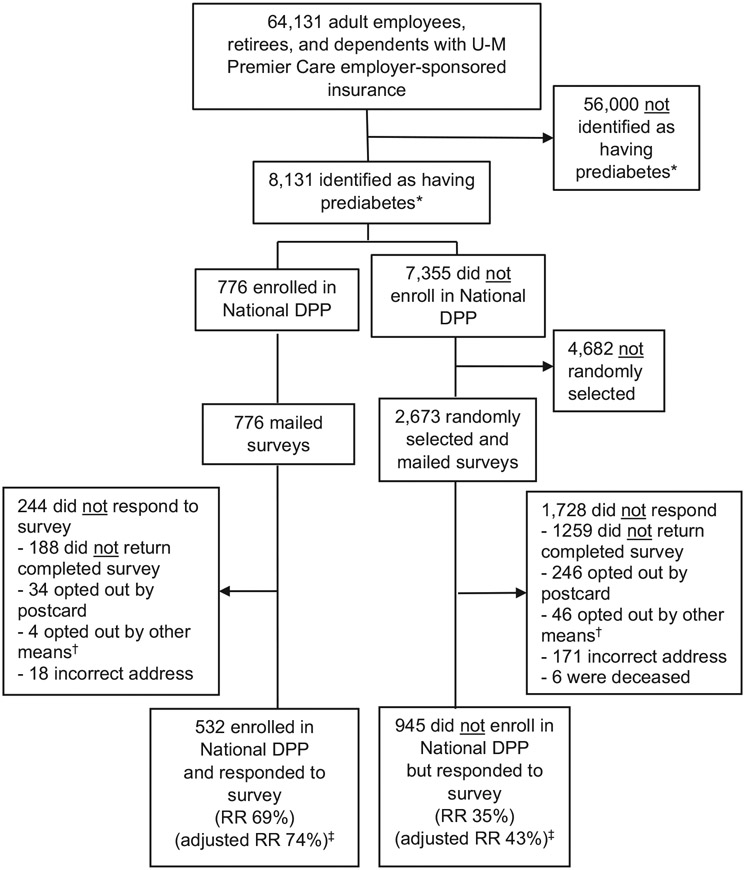
A total of 8131 adults with prediabetes were identified among the 64,131 adults with U-M Premier Care health insurance (Fig. 2). Their characteristics are shown in Table 1, in total and stratified by National DPP enrollment. Compared to the 7355 adults who did not enroll in the National DPP, the 776 adults (9.5%) who enrolled were older (53 ± 10 years vs. 50 ± 12 years) and more likely to be women (72% vs. 56%). Compared to National DPP non-enrollees, National DPP enrollees had higher BMI levels (34 kg/m22 vs. 32 kg/m22), were more likely to have claims diagnoses of overweight or obesity (46% vs. 33%), and less likely have claims diagnoses of smoking (2% vs. 7%). National DPP enrollees were more likely to have made at least one visit to a primary care provider (86% vs. 83%) or a specialist (70% vs. 65%) during the previous year and to live in a neighborhood with higher median household income ($71,287 vs. $69,588), a lower percentage of unemployment (34.4% vs. 35.0%), and a lower percentage of families receiving SNAP benefits (8.2% vs 8.7%). There were no differences between National DPP enrollees and non-enrollees with respect to race, blood pressure, cholesterol, claims diagnoses of hypertension or dyslipidemia, or pharmacy claims for blood pressure or lipid-lowering medications.
Fig. 2.
Study CONSORT flow diagram.
DPP: Diabetes Prevention Program, RR: Response Rate.
*Prediabetes determined using insurance claim and laboratory data.
†opted-out by phone or email.
‡Adjusted RR: Excludes individuals who opted out, for whom the address was incorrect, or who were deceased.
Table 1.
Characteristics of adult employees, retirees, and dependents with U-M Premier Care Health Insurance overall and those who were identified as having prediabetes, stratified by National DPP enrollment.
| Total | Prediabetes | Enrolled in National DPP | Did not enroll in National DPP | p-Value | |
|---|---|---|---|---|---|
| N (%) | 64,131 | 8131 | 776 (9.5%) | 7355 (90.5%) | – |
| Age (years) | 39 ± 14 | 50 ± 12 | 53 ± 10 | 50 ± 12 | <0.0001 |
| Sex | <0.0001 | ||||
| Men | 28,887 (45%) | 3482 (43%) | 219 (28%) | 3263 (44%) | |
| Women | 35,244 (55%) | 4649 (57%) | 557 (72%) | 4092 (56%) | |
| Race | 0.2804 | ||||
| White | 34,575 (84%) | 5254 (81%) | 538 (82%) | 4716 (81%) | |
| Asian | 3382 (8%) | 634 (10%) | 54 (8%) | 580 (10%) | |
| Black | 2688 (7%) | 532 (8%) | 49 (8%) | 483 (8%) | |
| Other | 651 (2%) | 85 (1%) | 12 (2%) | 73 (1%) | |
| BMI (kg/m2) | 28 ± 7 | 32 ± 7 | 34 ± 7 | 32 ± 7 | <0.0001 |
| Blood pressure (mmHg) | |||||
| Systolic | 120 ± 15 | 125 ± 15 | 125 ± 15 | 125 ± 15 | 0.5087 |
| Diastolic | 72 ± 10 | 75 ± 10 | 74 ± 10 | 75 ± 10 | 0.1705 |
| Cholesterol (mg/dL) | |||||
| Total cholesterol | 194 ± 38 | 194 ± 39 | 197 ± 38 | 194 ± 39 | 0.0851 |
| HDL | 55 ± 16 | 52 ± 15 | 53 ± 14 | 52 ± 15 | 0.0956 |
| Men | 48 ± 13 | 46 ± 12 | 45 ± 10 | 46 ± 12 | 0.1118 |
| Women | 61 ± 16 | 57 ± 15 | 57 ± 14 | 57 ± 16 | 0.3240 |
| Triglycerides | 129 ± 88 | 147 ± 94 | 147 ± 88 | 147 ± 95 | 0.9263 |
| LDL | 113 ± 32 | 114 ± 33 | 116 ± 33 | 114 ± 33 | 0.1905 |
| HbA1c (%) | 5.6 ± 0.6 | 5.8 ± 0.5 | 5.8 ± 0.3 | 5.8 ± 0.5 | 0.4364 |
| Claims diagnoses | |||||
| Overweight/obesity | 8598 (13%) | 2817 (35%) | 355 (46%) | 2462 (33%) | <0.0001 |
| Hypertension | 8108 (13%) | 3064 (38%) | 285 (37%) | 2779 (38%) | 0.5993 |
| Dyslipidemia | 6651 (10%) | 2733 (34%) | 282 (36%) | 2451 (33%) | 0.0815 |
| Cardiovascular disease | 1917 (3%) | 800 (10%) | 61 (8%) | 739 (10%) | 0.0517 |
| Smoking | 1737 (3%) | 530 (7%) | 17 (2%) | 513 (7%) | <0.0001 |
| Men | 887 (3%) | 274 (8%) | 8 (4%) | 266 (8%) | 0.0173 |
| Women | 850 (2%) | 256 (6%) | 9 (2%) | 247 (6%) | <0.0001 |
| Pharmacy prescription claims | |||||
| Antihypertensive medication | 8168 (13%) | 2865 (35%) | 265 (34%) | 2600 (35%) | 0.5378 |
| Lipid-lowering medication | 3619 (6%) | 1636 (20%) | 168 (21%) | 1468 (20%) | 0.2491 |
| Healthcare utilization | |||||
| ≥1 PCP visit in past year | 34,574 (54%) | 6789 (84%) | 663 (86%) | 6126 (83%) | 0.0459 |
| ≥1 Specialist visit in past year | 29,687 (46%) | 5323 (66%) | 539 (70%) | 4784 (65%) | 0.0060 |
| Neighborhood indicatorsa | |||||
| Median income ($) | 70,228 | 69,751 | 71,287 | 69,588 | 0.0133 |
| Percent unemployment | 35.3 ± 5.0 | 35.0 ± 4.7 | 34.4 ± 4.6 | 35.0 ± 4.8 | 0.0002 |
| Percent receiving SNAP benefits | 7.9 ± 6.0 | 8.7 ± 6.5 | 8.2 ± 6.0 | 8.7 ± 6.6 | 0.0136 |
BMI: Body Mass Index, HbA1c: Hemoglobin A1c, HDL: High-density lipoprotein cholesterol, LDL: Low-density lipoprotein cholesterol, DPP: Diabetes Prevention Program, PCP: Primary Care Provider, SNAP: Supplemental Nutrition Assistance Program.
Data are n (%) or mean ± standard deviation. P-values indicate significance between those who enrolled and those who did not enroll in National DPP.
Neighborhood indicators determined by merging residential zip codes with data reported from U.S. Census Bureau.
All the health plan members identified with prediabetes who enrolled in the National DPP, and a random sample of the health plan members identified with prediabetes who did not enroll were invited to participate in the survey (n = 3449). The characteristics of the 1477 adults with prediabetes who responded to the survey are shown in Table 2. Of the 776 adults with prediabetes who enrolled in the National DPP and were mailed a survey, 532 responded (crude response rate 69%). When we excluded individuals who opted out or for whom the address was incorrect, the adjusted response rate was 74%. Among the 2673 adults with prediabetes who did not enroll in the National DPP and were mailed surveys, 945 responded (crude response rate 35%). When we excluded individuals who opted out, for whom the address was incorrect, or who were deceased, the adjusted response rate was 43%. Overall, people with prediabetes who responded to the survey were 53 ± 11 years old (mean ± SD), 63% were women, 83% were non-Hispanic white. BMI was 31 ± 7 kg/m2 (mean ± SD). Slightly fewer than a third (30%) reported having high blood pressure. Nearly two-thirds (64%) had 4-year college degrees or higher and a similar proportion (63%) reported that their yearly household income was $75,000 or greater. The majority (61%) were affiliated with the U-M workforce as current employees.
Table 2.
Characteristics of adult employees, retirees, and dependents with U-M Premier Care Health Insurance who were identified as having prediabetes and responded to the survey, stratified by National DPP enrollment, and results of multivariate modeling.
| Prediabetes | Enrolled in National DPP |
Did not enroll in National DPP |
p-value | Fully-adjusted Multivariate model OR (95% CI) |
Most parsimonious Multivariate model OR (95% CI) |
|
|---|---|---|---|---|---|---|
| N (%) | 1477 | 532 (36%) | 945 (64%) | – | 1359 | 1359 |
| Demographic factorsa | ||||||
| Age (years) | 53 ± 11 | 54 ± 10 | 53 ± 11 | 0.0249 | 1.014 (1.001–1.027) | 1.013 (1.000–1.026) |
| Sex | <0.0001 | |||||
| Men | 540 (37%) | 150 (28%) | 390 (41%) | reference | reference | |
| Women | 937 (63%) | 382 (72%) | 555 (59%) | 1.720 (1.300–2.276) | 1.699 (1.290–2.238) | |
| Race | 0.5194 | – | – | |||
| White | 1027 (83%) | 654 (83%) | 373 (83%) | |||
| Asian | 114 (9%) | 76 (10%) | 38 (8%) | |||
| Black | 78 (6%) | 44 (6%) | 34 (8%) | |||
| Other | 15 (1%) | 10 (1%) | 5 (1%) | |||
| Clinical factors | ||||||
| BMI (kg/m2) | 31 ± 7 | 32 ± 7 | 31 ± 7 | 0.0526 | 1.032 (1.012–1.053) | 1.027 (1.007–1.046) |
| Self-rated health | 3.7 ± 0.8 | 3.4 ± 0.8 | 3.3 ± 0.9 | 0.0037 | – | – |
| High blood pressure | 443 (30%) | 155 (29%) | 288 (30%) | 0.5893 | – | – |
| Domains from Health Belief Model | ||||||
| Perceived benefits of health-protective action over diabetes risk (possible range 1 to 4) | 3.3 ± 0.6 | 3.4 ± 0.6 | 3.2 ± 0.6 | <0.0001 | 1.650 (1.318–2.066) | 1.668 (1.334–2.085) |
| Eating self-efficacy (possible range 6 to 30) | 21.1 ± 5.3 | 20.8 ± 5.0 | 21.3 ± 5.4 | 0.0609 | – | – |
| Physical activity self-efficacy (possible range 4 to 20) | 11.1 ± 4.3 | 11.1 ± 4.2 | 11.1 ± 4.3 | 0.9264 | – | – |
| Perceived threat of developing diabetes (possible range 3 to 12) | 8.6 ± 1.4 | 8.8 ± 1.4 | 8.4 ± 1.4 | <0.0001 | 0.980 (0.882–1.088) | – |
| “Cues to action” | <0.0001 | |||||
| None | 708 (48%) | 107 (20%) | 601 (64%) | reference | reference | |
| Letter from health plan (self-report)b | 276 (19%) | 175 (33%) | 101 (11%) | 6.475 (4.495–9.327) | 6.429 (4.469–3.407) | |
| Encouragement from doctor (self-report)c or outreach from clinicd | 267 (18%) | 104 (20%) | 163 (17%) | 2.389 (1.657–3.442) | 2.369 (1.657–3.407) | |
| Both letter from health plan and encouragement from doctor or outreach from clinic | 226 (15%) | 146 (27%) | 80 (8%) | 5.861 (3.919–8.763) | 5.818 (3.898–8.684) | |
| Sociopsychological factors | ||||||
| Education | 0.0058 | – | ||||
| ≤Some college | 517 (35%) | 158 (30%) | 359 (38%) | reference | ||
| 4-year college graduate | 340 (23%) | 126 (24%) | 214 (23%) | 1.473 (1.038–2.091) | ||
| >4-year college graduate | 600 (41%) | 238 (46%) | 362 (39%) | 1.377 (1.008–1.879) | ||
| Annual income | 0.9662 | – | – | |||
| <$75,000 | 518 (37%) | 184 (37%) | 334 (37%) | |||
| ≥$75,000 | 884 (63%) | 315 (63%) | 569 (63%) | 0.0560 | ||
| UM workforce affiliation | 0.0560 | – | – | |||
| Employee | 857 (61%) | 334 (65%) | 523 (58%) | |||
| Retiree | 156 (11%) | 51 (10%) | 105 (12%) | |||
| Dependent | 398 (28%) | 130 (25%) | 268 (30%) | |||
| Caring for child or dependent adult | 418 (28%) | 149 (28%) | 269 (29%) | 0.8586 | – | – |
| Support for eating a healthy diet or being physically active | 292 (20%) | 103 (19%) | 189 (20%) | 0.7672 | 1.035 (0.742–1.444) | – |
| Structural factors | ||||||
| Prediabetes awareness | 734 (50%) | 403 (76%) | 331 (35%) | <0.0001 | 2.559 (1.882–3.480) | 2.568 (1.917–3.441) |
| History of GDM or family history of diabetes | 814 (55%) | 308 (58%) | 506 (53%) | 0.1066 | 1.006 (0.767–1.321) | – |
| Knowledge of type 2 diabetes risk factors (possible range 0 to 11) | 6.5 ± 2.1 | 6.9 ± 2.1 | 6.3 ± 2.1 | <0.0001 | – | – |
BMI: Body Mass Index, HbA1c: Hemoglobin A1c, DPP: Diabetes Prevention Program, OR: Odds Ratio.
Data are N (percent) or mean ± standard deviation. P-values indicate significance between those who enrolled and those who did not enroll in National DPP.
Reported from insurance claims data.
Self-report of receipt of letter from the health plan that encouraged National DPP enrollment.
Self-report of encouragement from a “doctor” to enroll in the National DPP.
Outreach (letter, portal message, or telephone call) from primary care clinic that encouraged National DPP enrollment.
Compared to non-enrollees, National DPP enrollees were significantly older, more likely to be women, had higher BMIs and better self-rated health (Table 2). Enrollees reported greater perceived benefits, greater perceived threat, and were more likely to have experienced one or more cues to action. There were no differences between non-enrollees and enrollees with respect to eating self-efficacy or physical activity self-efficacy. In the first multivariate logistic model, we simultaneously examined the HBM domains to determine which were independently associated with National DPP enrollment (data not shown). Perceived benefits, perceived threat, and cues to action remained significant in the multivariate model.
We used a second set of logistic models to examine how perceived benefits and perceived threat were associated with demographic, clinical, sociopsychological, and structural variables. Greater perceived benefits were associated with higher self-rated health, higher level of educational attainment, higher income level, and greater knowledge of risk factors for type 2 diabetes. Lower perceived benefits were associated with higher BMI and having support for eating a healthy diet or for being physically active. Greater perceived threat was associated with female sex, lower self-rated health, higher BMI, not having support for eating a healthy diet or for being physically active, prediabetes awareness, history of gestational diabetes mellitus or family history of type 2 diabetes, and greater knowledge of risk factors for type 2 diabetes (data not shown).
In the third set of logistic models, we examined whether perceived benefits, perceived threat, and cues to action were independently associated with National DPP enrollment after demographic, clinical, sociopsychological, and structural variables were included in the model (Table 2). In the most descriptive fully-adjusted model, older age, female sex, higher BMI, higher educational attainment, prediabetes awareness, greater perceived benefits, and one or more cues to action were all associated with enrollment. Perceived threat was no longer independently associated with enrollment. When we used stepwise regression to find the most parsimonious model, all of the variables except education remained in the model. Both perceived benefits of health-protective action over diabetes risk (odds ratio 1.668, 95% CI 1.334–2.085) and cues to action (ORs 2.369 to 6.429) were significantly associated with National DPP enrollment.
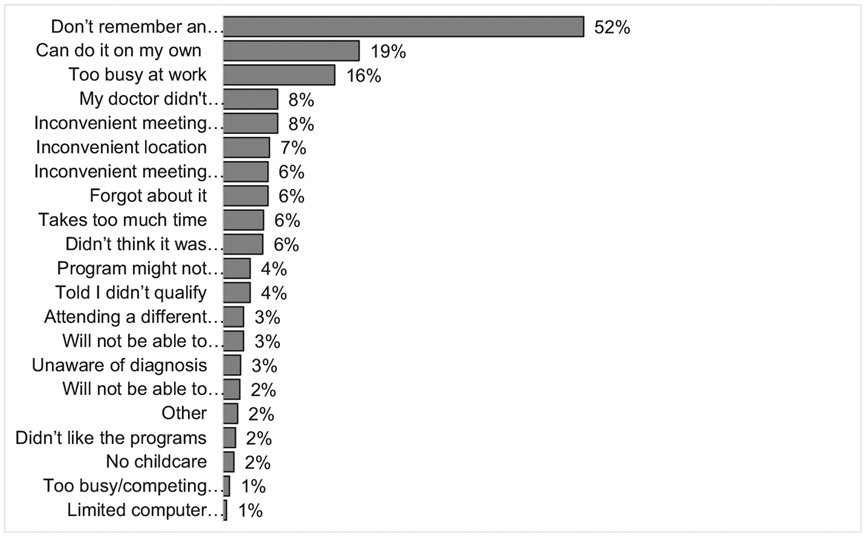
When survey respondents who did not enroll in the National DPP were presented with a list of potential reasons for not participating, more than half (52%) indicated that they did not remember being invited to participate in the National DPP. Some (19%) reported that they could “do it on their own”. Other common responses were “too busy at work” (16%), “my doctor didn't recommend it” (8%), and inconvenient meeting location (7%), time (8%), or day (6%). The list of reasons for not participating and the frequency of responses is presented in Fig. A.1.
4. Discussion
Fewer than 10% of insured adults who were identified with prediabetes and encouraged to enroll in the National DPP enrolled. Although this rate of enrollment is more than twice that reported in comparable studies,25,26 it remains disappointingly low. We found that compared to those who did not enroll, those who enrolled in the National DPP were older and more likely to be women, to have a diagnosis of overweight or obesity, to have received medical care from a primary care provider or a specialist during the past year, and to live in neighborhoods with higher household incomes, lower rates of unemployment, and lower percentages of families receiving SNAP benefits.
We explored whether National DPP enrollment was associated with domains of the Health Belief Model. We found that perceived benefits of protective-health action over diabetes risk and cues to action were both independently associated with National DPP enrollment. Individuals' sense of self-efficacy, that they could control eating or engage in regular physical activity, and perceived threat of developing diabetes were not associated with National DPP enrollment after adjusting for demographic, clinical, sociopsychological, and structural variables. Adults with prediabetes who reported that people who make a good effort to control their risks of developing diabetes are much less likely to develop diabetes and that their personal efforts would help control their own risk of developing diabetes were significantly more likely to enroll in the National DPP. These results highlight the importance of educating individuals with prediabetes about the compelling evidence for the effectiveness of intensive lifestyle interventions for diabetes prevention regardless of age, sex, race/ethnicity, and baseline risk. There is an urgent need to better communicate the benefits of lifestyle interventions to delay or prevent the onset of type 2 diabetes and provide clear and actionable information about the programs that are available.
Recently, we conducted a study examining factors associated with the use of metformin in the same population.27 In that study, we found that compared to those who did not use metformin, those who used metformin were younger and more likely to have experienced one or more cues to action. Compared to those who did not use metformin, those who used metformin were no more likely to perceive the benefits of diet and physical activity on diabetes risk. These findings suggest that older individuals with prediabetes who have fewer competing demands on their time and who perceive greater benefits of diet and physical activity might be more likely to choose the National DPP. Interventions are needed to promote shared decision-making and might support providers' ability to discuss metformin and the National DPP in a manner that allows patients to make decisions that are informed and consistent with their health beliefs and preferences.
Cues to action were also very important determinants of National DPP enrollment. Clear information about the diagnosis of prediabetes and decision support for joining a lifestyle intervention, especially from a trusted health care provider, are critical. Among people with prediabetes who did not enroll in the National DPP, 39% indicated that they were unaware that they had prediabetes, and 26% indicated that they were unsure whether they had prediabetes. Additionally, 64% indicated that they were unaware that they were invited to join the DPP. Data from the National Health and Nutrition Examination Survey (NHANES) indicate only about 13% of American adults with screen-detected prediabetes report ever having been told by a health care provider that they have prediabetes1, suggesting that the diagnosis is not being made or if it is being made, it is not being communicated to people in ways that are understandable and actionable. Heath care providers' comfort and expertise with diagnosing prediabetes and discussing the benefits of the National DPP are also limited.28 In one study, fewer than one-quarter of primary care providers reported ever having made a referral to the National DPP.29
Fortunately, there are policy changes underway at the Centers for Disease Control and Prevention and the Centers for Medicare and Medicaid Services that will increase the number of National DPP suppliers and reduce some of the barriers to participation.31 Yet questions remain about the lack of demand for the DPP among adults with prediabetes.7,11 Health care provider advice and decision support are key motivators for health-protective action and behavior change.32 Although physicians face challenges with providing counseling regarding weight loss including a lack of training, tools, reimbursement, staffing, and time, and a lack confidence in their own abilities to help patients implement weight loss strategies,32 simply inviting patients to enroll in the National DPP might substantially increase enrollment. Data from the 2016 National Health Interview Survey indicated that only 4.2% of eligible adults reported ever being referred to the National DPP.30
Our findings of sex differences in enrollment in the National DPP among adults with prediabetes are not novel. Unfortunately, men have been underrepresented in the National DPP across age and race/ethnicity groups.33 A possible explanation for the lower enrollment among men is that men are less likely to have accurate weight perception and weight dissatisfaction.34 Additional explanations include health care providers not communicating the benefits of National DPP enrollment and not addressing the stigma that men might perceive regarding seeking help to address their diabetes risk.33
In a pragmatic weight management trial performed in England, younger people, men, and those from poorer socioeconomic areas were significantly less likely to participate in a behavioral weight-loss program. Inequalities regarding who was offered the referral and who accepted the referral accounted for lower participation among men. When letters publicizing the opportunity to participate in the behavioral weight loss program were sent to all eligible patients and patients were offered a variety of interventions, the proportion of men who participated more than doubled.35
There are several limitations to our study. While the U.S. health system must take action to improve equity in type 2 diabetes prevention36, the U-M workforce was not representative of the educational, economic, or racial and ethnic diversity of the prediabetes population in the US. Among the cohort of insured adults with prediabetes identified in this study, the largest portion was non-Hispanic White (81%), followed by Asian (10%), and non-Hispanic Black (8%). In addition, the study was designed to examine associations. Cause-and-effect relationships cannot be inferred. Because the National DPP was offered at no out-of-pocket cost, we were unable to assess the role of financial barriers to enrollment. Finally, we recognize that some people may have chosen to enroll in alternative lifestyle programs. We conducted a sensitivity analysis and identified individuals with prediabetes who attended other programs or who tried to enroll but were told they did not qualify. Using this broader definition of participation, the results were the same (data not shown) indicating that the intrinsic and extrinsic motivation for enrolling in the National DPP or another program are the same.
4.1. Conclusions
Although there are almost 100 million U.S. adults with prediabetes who are at risk for type 2 diabetes, participation in the National DPP has been low. Therefore, effective approaches to increase enrollment and reduce disparities are urgently needed. The results of this study suggest that to optimize enrollment in the National DPP, it will be important to increase awareness of prediabetes and the benefits of DPP enrollment for patients with prediabetes and to increase the degree to which primary care providers make the diagnosis of prediabetes, communicate about prediabetes with patients, and invite them to join the National DPP.
Acknowledgements
The authors thank Marsha Manning, Manager, Medical Benefits and Strategy at the University of Michigan, Ashley Weigl, Associate Director, MHealthy, and Marc D. Keshishian, MD and Dawn Beaird, Blue Cross Blue Shield of Michigan for their contributions to this project.
Funding
This work was supported by National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases [grant R01 DK109995].
Appendix
Table A.1.
Characteristics of adult employees, retirees, and dependents with U-M Premier Care Health Insurance who were identified as having prediabetes and surveyed, stratified by enrollment in the National DPP and if they responded to the survey or did not respond to the survey.
| Enrolled in National DPP |
Did not enroll in National DPP |
|||||
|---|---|---|---|---|---|---|
| Responded to the survey |
Did not respond to the survey |
p-Value | Responded to the survey |
Did not respond to the survey |
p-Value | |
| N (%) | 532 (74%) | 188 (26%) | – | 945 (43%) | 1259 (57%) | – |
| Age (years) | 54 ± 10 | 49 ± 10 | <0.0001 | 53 ± 11 | 49 ± 11 | <0.0001 |
| Sex | 0.8902 | |||||
| Men | 150 (28%) | 54 (29%) | 390 (41%) | 613 (49%) | ||
| Women | 382 (72%) | 134 (71%) | 555 (59%) | 646 (51%) | ||
| Race | 0.2257 | 0.0208 | ||||
| White | 373 (83%) | 132 (83%) | 654 (83%) | 840 (82%) | ||
| Asian | 38 (8%) | 9 (6%) | 76 (10%) | 78 (8%) | ||
| Black | 34 (8%) | 14 (9%) | 44 (6%) | 94 (%) | ||
| Other | 5 (1%) | 5 (3%) | 10 (1%) | 13 (1%) | ||
| BMI (kg/m2) | 34 ± 7 | 35 ± 7 | 0.0145 | 32 ± 7 | 34 ± 7 | <0.0001 |
| Blood pressure (mmHg) | ||||||
| Systolic | 126 ± 16 | 126 ± 13 | 0.8956 | 126 ± 16 | 127 ± 16 | 0.2314 |
| Diastolic | 74 ± 10 | 76 ± 9 | 0.0452 | 75 ± 10 | 76 ± 10 | 0.0004 |
| Cholesterol (mg/dL) | ||||||
| Total cholesterol | 197 ± 39 | 196 ± 36 | 0.7400 | 190 ± 36 | 193 ± 39 | 0.1401 |
| HDL | 54 ± 15 | 51 ± 12 | 0.0456 | 53 ± 15 | 50 ± 14 | <0.0001 |
| Men | 45 ± 11 | 43 ± 10 | 0.4673 | 46 ± 11 | 45 ± 12 | 0.2431 |
| Women | 58 ± 14 | 54 ± 11 | 0.0251 | 58 ± 16 | 55 ± 14 | 0.0011 |
| Triglycerides | 145 ± 92 | 149 ± 76 | 0.6278 | 134 ± 77 | 153 ± 101 | 0.0001 |
| LDL | 115 ± 33 | 115 ± 31 | 0.9152 | 111 ± 31 | 114 ± 33 | 0.1318 |
| HbA1c (%) | 5.8 ± 0.3 | 5.8 ± 0.3 | 0.7586 | 5.8 ± 0.5 | 5.8 ± 0.6 | 0.1793 |
| Claims diagnoses | ||||||
| Overweight/obesity | 228 (43%) | 97 (52%) | 0.0358 | 332 (34%) | 486 (39%) | 0.0290 |
| Hypertension | 204 (38%) | 63 (34%) | 0.2381 | 390 (41%) | 515 (41%) | 0.8634 |
| Dyslipidemia | 198 (37%) | 65 (35%) | 0.5176 | 359 (38%) | 428 (34%) | 0.0528 |
| Cardiovascular disease | 50 (9%) | 9 (5%) | 0.0475 | 118 (12%) | 124 (10%) | 0.0500 |
| Smoking | 10 (2%) | 7 (4%) | 0.1524 | 61 (6%) | 123 (10%) | 0.0054 |
| Men | 4 (3%) | 4 (8%) | 0.1238 | 38 (10%) | 67 (11%) | 0.5497 |
| Women | 6 (2%) | 3 (2%) | 0.6112 | 23 (4%) | 56 (9%) | 0.0016 |
| Pharmacy claims | ||||||
| Antihypertensive medication | 194 (36%) | 58 (31%) | 0.1653 | 368 (39%) | 505 (40%) | 0.5785 |
| Lipid-lowering medication | 123 (23%) | 35 (19%) | 0.1997 | 215 (23%) | 252 (20%) | 0.1199 |
| Healthcare utilization | ||||||
| ≥1 PCP visit in past year | 462 (88%) | 157 (84%) | 0.2857 | 831 (88%) | 1046 (83%) | 0.0017 |
| ≥1 Specialist visit in past year | 385 (73%) | 117 (63%) | 0.0102 | 680 (72%) | 804 (64%) | <0.0001 |
| Neighborhood indicatorsa | ||||||
| Median income ($) | 72,118 | 68,582 | 0.0154 | 70,786 | 69,064 | 0.0271 |
| Percent unemployment | 34 ± 5 | 34 ± 4 | 0.8933 | 35 ± 5 | 35 ± 4 | 0.2375 |
| Percent receiving SNAP benefits | 8 ± 6 | 8 ± 6 | 0.5688 | 8 ± 7 | 9 ± 7 | 0.0042 |
BMI: Body Mass Index, HbA1c: Hemoglobin A1c, HDL: High-density lipoprotein cholesterol, LDL: Low-density lipoprotein cholesterol, NDPP: National Diabetes Prevention Program, PCP: Primary Care Provider, SNAP: Supplemental Nutrition Assistance Program.
Data are N (percent) or mean ± standard deviation.
Neighborhood indicators determined by merging zip codes with data reported from U.S. Census Bureau.
Fig. A.1.
Reasons cited by adult employees, retirees, and dependents with U-M Premier Care Health Insurance who were identified with prediabetes and who responded to the survey but did not enroll in the National DPP for not enrolling (N = 945).
DPP: Diabetes Prevention Program; PA: physical activity.
Respondents could select more than one response.
Footnotes
CRediT authorship contribution statement
Kevin Joiner: Conceptualization, Methodology, Formal Analysis, Investigation, Data Curation, Writing – Original Draft, Writing – Review & Editing. Laura N. McEwen: Conceptualization, Methodology, Formal Analysis, Investigation, Data Curation, Writing – Original Draft, Writing – Review & Editing, Funding Acquisition. Thomas Hurst: Writing – Original Draft, Writing – Review & Editing. Mackenzie Adams: Writing – Original Draft, Writing – Review & Editing. William Herman: Conceptualization, Methodology, Investigation, Data Curation, Writing – Original Draft, Writing – Review & Editing, Funding Acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: U.S. Department of Health and Human Services; 2020. [Google Scholar]
- 2.Zhang X, Gregg EW, Williamson DF, Barker LE, Thomas W, Bullard KM, et al. A1C level and future risk of diabetes: a systematic review. Diabetes Care. 2010;33:1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. [DOI] [PubMed] [Google Scholar]
- 5.Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am J Prev Med. 2013;44:S346–S351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grass SM, Nhim K, Gregg E, Bell M, Luman E, Albright A. Public health approaches to type 2 diabetes prevention: the U.S. National Diabetes Prevention Program and beyond. Curr Diab Rep. 2019;19:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoerger TJ, Jacobs S, Romaire M, Liu Y, Neuwahl S, Casoglos A. Evaluation of the Medicare diabetes prevention program: first annual report [article online]. Available from https://innovation.cms.gov/data-and-reports/2021/mdpp-firstannevalrpt; 2021. Accessed August 11, 2021. [Google Scholar]
- 8.Ely EK, Grass SM, Luman ET, Gregg EW, Ali MK, Nhim K, et al. A national effort to prevent type 2 diabetes: participant-level evaluation of CDC's national diabetes prevention program. Diabetes Care. 2017;40:1331–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sinclair-White B, Nett B, Ilagan L, Cacal SL, Vu U, Ching LK, et al. Insights in public health: development, implementation, and evaluation of the prevent diabetes, Hawai' i campaign. Hawaii J Health Soc Welf. 2020;79:86–90. [PMC free article] [PubMed] [Google Scholar]
- 10.Tseng E, Greer RC, O'Rourke P, Yeh HC, McGuire MM, Albright AL, et al. National survey of primary care physicians' knowledge, practices, and perceptions of prediabetes. J Gen Intern Med. 2019;34:2475–2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ackermann RT, O'Brien MJ. Evidence and challenges for translation and population impact of the diabetes prevention program. Curr Diab Rep. 2020;20:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gopalan A, Lorincz IS, Wirtalla C, Marcus SC, Long JA. Awareness of prediabetes and engagement in diabetes risk-reducing behaviors. Am J Prev Med. 2015;49:512–519. [DOI] [PubMed] [Google Scholar]
- 13.Gopalan A, Kellom K, McDonough K, Schapira MM. Exploring how patients understand and assess their diabetes control. BMC Endocr Disord. 2018;18:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Becker MH. The health belief model and personal health behavior. Health Educ. 1974;2:324–508. [Google Scholar]
- 15.Rosenstock IM, Strecher VJ, Becker MH. The health belief model and HIV risk behavior change. In: DiClemente RJ, Peterson JL, eds. Preventing AIDS: Theories and methods of behavioral interventions. Boston, MA, Springer: US; 1994:5–24. [Google Scholar]
- 16.West R, Godinho CA, Bohlen LC, Carey RN, Hastings J, Lefevre CE, et al. Development of a formal system for representing behaviour-change theories. Nat Hum Behav. 2019;3:526–536. [DOI] [PubMed] [Google Scholar]
- 17.Ali MK, McKeever Bullard K, Imperatore G, Benoit SR, Rolka DB, Albright AL, et al. Reach and use of diabetes prevention services in the United States, 2016–2017. JAMA Netw Open. 2019;2, e193160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Diabetes Association. 3. Prevention or delay of type 2 diabetes: standards of medical care in diabetes-2021. Diabetes Care. 2021;44:S34–S39. [DOI] [PubMed] [Google Scholar]
- 19.Herman WH, Joiner K, Hurst T, McEwen LN. The effectiveness of a proactive, three-level strategy to identify people with prediabetes in a large workforce with employer-sponsored health insurance. Diabetes Care. 2021;44:1532–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Explore Census Data. Article online. Available from https://data.census.gov/cedsci/; 2021. Accessed August 11, 2021.
- 21.Rochefort C, Baldwin AS, Tiro J, Bowen ME. Evaluating the validity of the risk perception survey for developing diabetes scale in a safety-net clinic population of English and Spanish speakers. Diabetes Educ. 2020;46:73–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walker EA, Mertz CK, Kalten MR, Flynn J. Risk perception for developing diabetes: comparative risk judgments of physicians. Diabetes Care. 2003;26:2543–2548. [DOI] [PubMed] [Google Scholar]
- 23.Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59:739–744. [DOI] [PubMed] [Google Scholar]
- 24.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63:60–66. [DOI] [PubMed] [Google Scholar]
- 25.Kullgren JT, Knaus M, Jenkins KR, Heisler M. Mixed methods study of engagement in behaviors to prevent type 2 diabetes among employees with pre-diabetes. BMJ Open Diabetes Res Care. 2016;4, e000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zigmont VA, Shoben AB, Kaye GL, Snow RJ, Clinton SK, Harris RE, et al. An evaluation of reach for a work site implementation of the National Diabetes Prevention Program focusing on diet and exercise. Am J Health Promot. 2018;32:1417–1424. [DOI] [PubMed] [Google Scholar]
- 27.McEwen LN, Hurst TE, Joiner KJ, Herman WH. Health beliefs associated with metformin use among insured adults with prediabetes. Diabetes Care. 2022. (under review April 2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tseng E, Greer RC, O’Rourke P, Yeh H-C, McGuire MM, Albright AL, et al. National survey of primary care physicians’ knowledge, practices, and perceptions of prediabetes. J Gen Intern Med. 2019;34:2475–2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nhim K, Khan T, Grass SM, Wozniak G, Kirley K, Schumacher P, et al. Primary care providers' prediabetes screening, testing, and referral behaviors. Am J Prev Med. 2018;55:e39–e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Venkataramani M, Pollack CE, Yeh H-C, Marathur NM. Prevalence and correlates of diabetes prevention program referral and participation. AmJ Prev Med. 2019;56:452–457. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Medicare &, Medicaid Services. Proposed policies for the Medicare Diabetes Prevention Program (MDPP) expanded model for the calendar year 2022 medicare physician fee schedule [article online], https://www.cms.gov/newsroom/fact-sheets/proposed-policies-medicare-diabetes-prevention-program-mdpp-expanded-model-calendar-year-2022; 2021. Accessed August 11, 2021.
- 32.Rose SA, Poynter PS, Anderson JW, Noar SM, Conigliaro J. Physician weight loss advice and patient weight loss behavior change: a literature review and meta-analysis of survey data. Int J Obes (Lond). 2013;37:118–128. [DOI] [PubMed] [Google Scholar]
- 33.Jackson MC, Dai S, Skeete RA, Owens-Gary M, Cannon MJ, Smith BD, et al. An examination of gender differences in the National Diabetes Prevention Program's lifestyle change program. Diabetes Educ. 2020;46:580–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsai SA, Lv N, Xiao L, Ma J. Gender differences in weight-related attitudes and behaviors among overweight and obese adults in the United States. Am J Mens Health. 2016;10:389–398. [DOI] [PubMed] [Google Scholar]
- 35.Ahern AL, Aveyard P, Boyland EJ, Halford JC, Jebb SA, WRAP trial team. Inequalities in the uptake of weight management interventions in a pragmatic trial: an observational study in primary care. Br J Gen Pract. 2016;66:e258–e263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care. 2020:dci200053. [DOI] [PMC free article] [PubMed] [Google Scholar]