Abstract
Aims:
To evaluate retention and outcomes of insured adults with prediabetes who enrolled or did not enroll in National Diabetes Prevention Programs (NDPPs).
Methods:
Between 2015 and 2019, 776 University of Michigan employees, dependents, and retirees with prediabetes and overweight or obesity enrolled in one-year NDPPs.
Results:
Enrollees attended a median of 18 sessions. Median retention was 38 weeks. Retention was associated with older age, greater initial weight loss, and physical activity. At both 1- and 2-years, body mass index, triglycerides, and HbA1c were significantly improved among enrollees. After adjusting for age group, sex, and race, the odds of developing diabetes based on HbA1c ≥6.5 % was 40 % lower at 1-year and 20 % lower at 2-years, and the odds of self-reported diabetes was 57 % lower at 1-year and 46 % lower at 2-years in enrollees compared to non-enrollees. Enrollees who disenrolled before completing the core curriculum had higher odds and enrollees who completed the NDPP had lower odds of developing diabetes that non-enrollees.
Conclusions:
In this population with prediabetes, NDPP retention was generally good, risk factors were improved, and diabetes was delayed or prevented for up to two years.
Keywords: Prospective observational study, Prediabetes, Type 2 diabetes prevention, Lifestyle intervention, Retention, Diabetes incidence
1. Introduction
In 2002, the Diabetes Prevention Program clinical trial demonstrated that an intensive behavioral lifestyle intervention that employed a low-fat, calorie-restricted diet and moderate physical activity reduced the incidence of type 2 diabetes by 58 % over 2.8 years in adults with overweight or obesity and impaired fasting glucose (IFG) and impaired glucose tolerance (IGT).1 Based upon these findings, the Centers for Disease Control and Prevention (CDC) launched the National DPP (NDPP) to provide high-quality lifestyle change programs to people with overweight or obesity and prediabetes to reduce their risk of type 2 diabetes and improve their overall health.2
Between 2012 and 2020, over 2000 CDC-recognized organizations enrolled over 450,000 adults in the 1-year NDPP.3 Enrollees represented approximately 0.5 % of the estimated 96 million adults with prediabetes and 2.5 % of the adults with prediabetes who reported being told by a health professional that they had this condition.4 While CDC has reported NDPP retention rates, the percent of enrollees achieving 5 % weight loss, and the percent meeting self-reported physical activity goals at 1-year,5 CDC has not compared the outcomes of NDPP enrollees to those who were eligible but did not enroll, has not described the incidence of diabetes in enrollees or non-enrollees, and has not reported outcomes beyond 1-year.
The purpose of this study was to describe retention and the 1- and 2-year clinical outcomes of individuals ≥18 years of age with prediabetes and overweight or obesity who enrolled in CDC-recognized NDPPs and individuals with prediabetes and overweight or obesity identified from the same employer population over the same time period who did not enroll in a NDPPs. The results are important to understand program uptake and retention and the short- and longer-term real-world benefits of NDPP enrollment.
2. Subjects
The University of Michigan (U-M) is a large public research university in Ann Arbor, Michigan with satellite campuses in Flint and Dearborn, Michigan. Beginning in 2015, the U-M offered the NDPP at no out-of-pocket cost to university employees, dependents, and retirees ≥18 years of age who had prediabetes and overweight or obesity and who belonged to the university’s self-funded health insurance program (Premier Care). Prediabetes was defined by either a health plan claims diagnosis of prediabetes or a hemoglobin A1c (HbA1c) level of 5.7 to 6.4 % in individuals without a history of diabetes mellitus. A history of diabetes was defined as at least one acute inpatient encounter or at least two outpatient encounters with a diagnosis of diabetes or at least one dispensing of an antihyperglycemic medication other than metformin on an ambulatory basis. Eligible subjects were offered the choice of four CDC-recognized NDPPs: two in-person classroom-based programs, one fitness-based program, and one on-line virtual program.
Of the 64,131 U-M employees, dependents, and retirees ≥18 years of age without diabetes insured through Premier Care, 8131 (12.7 %) were identified as having overweight or obesity and prediabetes. This study focused on the 776 people with prediabetes who enrolled in a NDPP (9.5 %) and the 7355 who did not enroll in a NDPP between 2015 and 2019.
With 500 enrollees and 500 non-enrollees, we estimated that we would have 90 % power to detect a change of 0.21 standard deviation in BMI and HbA1c between the groups using two-tailed t-tests with a 5 % level of significance.
This study was reviewed and approved by the University of Michigan Institutional Review Board for Human Research (HUM #00108065) and was granted a Waiver of Documented Informed Consent. Study participants were mailed Informed Consent documents with surveys. Return of a completed survey was considered to indicate consent.
3. Materials and methods
Beginning in 2015 and approximately every 6 months, the health plan sent letters to individuals identified with prediabetes encouraging them to enroll in a NDPP. The dates when enrollees attended a first NDPP session were used as their enrollment dates. Our ongoing analysis of enrollment data found that individuals with prediabetes who did not enroll in a NDPP within nine months of their invitation letters infrequently enrolled in the NDPP. Accordingly, they were classified as non-enrollees. Twenty individuals initially classified as non-enrollees subsequently enrolled in a NDPP and they were reclassified as enrollees. The dates non-enrollees were sent letters inviting them to enroll plus the median number of days to enrollment after the date of invitation letter for individuals from the same cohort who enrolled in a NDPP were used as the index dates for non-enrollees.
We used data provided by the contracted NDPP providers to assess retention in the NDPP among enrollees. For all enrollees and non-enrollees, we used data collected and provided by the health plan to describe the demographic, clinical, and laboratory characteristics of the subjects. We used the enrollment date for enrollees and the index date for non-enrollees to establish baseline, 1-year, and 2-year follow-up time windows. Baseline values of body mass index (BMI), blood pressure, lipids, and HbA1c were defined as the last measured value in the year before the enrollment or index date. One-year and 2-year follow-up values were defined as the last measured value in the interval between the enrollment or index date plus 365 days and between 365 days and 730 days, respectively. We used these values to assess changes in risk factor levels over time and the incidence of diabetes at 1- and 2-years follow-up. Using health plan data, we calculated the cumulative incidence of diabetes among enrollees and non-enrollees as the percentage of individuals who had HbA1c levels ≥6.5 % among those with HbA1c levels measured in the 1- and 2-year time intervals.
We also surveyed NDPP enrollees and non-enrollees with prediabetes to describe and compare the self-reported diagnosis of diabetes at 1- and 2-years follow-up. Progression to diabetes was assessed with the question “Have you been diagnosed with diabetes?”. We mailed surveys to 776 people who enrolled in a NDPP and to a random sample of 2892 people with prediabetes who did not enroll. We received 532 completed surveys (69 % crude response rate) from enrollees and 945 completed surveys from non-enrollees (35 % crude response rate). When we excluded those who had died, opted out of the research, or could not be contacted because of incorrect addresses, the adjusted response rates were 74 % for enrollees and 43 % for non-enrollees. We calculated the cumulative incidence of self-reported diabetes among enrollees and non-enrollees as the percentages of individuals with positive responses on the 1-year and the 2-year follow-up surveys.
We calculated the percentage of enrollees retained in the NDPP using the methods of Cannon et al..6 The percent retained through a given week of the NDPP was defined as the number of enrollees who remained in the program divided by the number of enrollees present during the first week of the program multiplied by 100. An enrollee was considered to be retained in the program at a given week if he or she attended a session that week or during a subsequent week. We considered the first session attended to be week 1 regardless of the session number. We truncated data on retention at week 44 because after week 44 the percent retention became unstable due to small sample sizes.
We further assessed retention by age group, sex, race, weight loss at week 3, and mean weekly reported minutes of physical activity. Mean weekly minutes of physical activity were calculated as the cumulative number of minutes reported by the enrollee divided by the number of weeks for which physical activity was reported. For this measure, we used only non-missing, non-zero reported minutes of physical activity. To compare differences in percent retention by age group, sex, race, weight loss at week 3, and mean minutes of physical activity per week, we used Cox proportional Hazards models with weeks until disenrolling as the time varying component and whether the enrollee disenrolled before or after 44 weeks as the survival indicator.
To compare characteristics and outcomes between individuals with prediabetes who enrolled and did not enroll in a NDPP, we used t-tests for continuous variables and chi-square tests for categorical variables. We also used independent continuous regression models to examine the mean changes in BMI, blood pressure, lipids, and HbA1c levels at one- and 2-years in enrollees vs. non-enrollees adjusting for age group (18–44, 45–54, 55–64, 65+ years), sex, race (Asian, Black, white, other), and baseline values of the risk factors.
Finally, we used logistic regression models to examine whether enrollment in a NDPP was associated with the odds of progression to diabetes at one- and 2-years after adjusting for age group, sex, and race. We also examined if enrollment and retention were associated with the odds of progression to diabetes (not enrolled, enrolled, enrolled but disenrolled before week 16, enrolled but disenrolled after week 16 but before week 44, enrolled and completed week 44 or more). All analyses were performed using SAS 9.4 (SAS Institute, Cary, North Carolina).
4. Results
Table 1 shows the baseline characteristics of U-M employees, dependents, and retirees ≥18 years of age with prediabetes and overweight or obesity overall and stratified by NDPP enrollment status. In general, individuals with prediabetes were middle-aged (51 ± 12 years, mean ± SD) and more likely to be women (57 %). Most (81 %) were white. Mean BMI was 32.3 ± 7.3 kg/m2. In general, blood pressure and lipid levels were well controlled. The mean HbA1c was 5.8 ± 0.5 %.
Table 1.
Baseline characteristics of employees, dependents, and retirees ≥18 years of age with overweight or obesity and prediabetes: overall and stratified by NDPP enrollment status.
| Overall | Enrolled in NDPP | Not enrolled in NDPP | p-Value | |
|---|---|---|---|---|
| N (%) | 8131 | 776 (10 %) | 7355 (90 %) | – |
| Age (years) | 51 ± 12 | 53 ± 10 | 50 ± 12 | <0.001 |
| Sex | <0.001 | |||
| Women | 4649 (57 %) | 557 (72 %) | 4092 (56 %) | |
| Men | 3482 (43 %) | 219 (28 %) | 3263 (44 %) | |
| Race | 0.280 | |||
| Asian | 634 (10 %) | 54 (8 %) | 580 (10 %) | |
| Black | 532 (8 %) | 49 (8 %) | 483 (8 %) | |
| White | 5254 (81 %) | 538 (82 %) | 4716 (81 %) | |
| Other | 85 (1 %) | 12 (2 %) | 73 (1 %) | |
| BMI (kg/m2) | 32.3 ± 7.3 | 34.1 ± 7.0 | 32.1 ± 7.3 | <0.001 |
| Blood pressure (mmHg) | ||||
| Systolic | 125 ± 15 | 126 ± 15 | 125 ± 15 | 0.136 |
| Diastolic | 75 ± 10 | 74 ± 10 | 75 ± 10 | 0.233 |
| Lipids (mg/dl) | ||||
| Total cholesterol | 194 ± 39 | 196 ± 39 | 194 ± 39 | 0.176 |
| HDL-c | 52 ± 15 | 53 ± 14 | 52 ± 15 | 0.194 |
| Triglycerides | 146 ± 94 | 147 ± 96 | 146 ± 94 | 0.676 |
| LDL-c | 113 ± 32 | 113 ± 32 | 113 ± 32 | 0.929 |
| HbA1c (%) | 5.8 ± 0.5 | 5.9 ± 0.3 | 5.8 ± 0.5 | 0.002 |
Data are expressed as N(%) or mean ± SD.
Compared to individuals with prediabetes who did not enroll in a NDPP, enrollees were older and more likely to be women. The racial distribution of enrollees did not differ from that of non-enrollees. Enrollees had significantly higher BMI and HbA1c levels than non-enrollees. Blood pressure and lipid levels did not differ between enrollees and non-enrollees (Table 1).
For enrollees, median retention was 38 weeks. The median number of sessions attended was 18. In general, attrition was low during the first 16 weeks of the core curriculum but increased somewhat thereafter during the maintenance phase (Fig. 1a). Retention was consistently greater among older enrollees. Compared to enrollees 55 years of age and older, the hazard ratio for retention was 0.40 (95 % CI 0.23–0.68) for enrollees 18 to 29 years of age, 0.55 (0.43–0.70) for those 30 to 44 years of age, and 0.78 (0.62–0.97) for those 45 to 54 years of age (Fig. 1b). Retention did not differ by sex (men vs. women, HR 0.96 (0.78–1.18)) (Fig. 1c). Retention did not differ between Asians vs. whites (HR 0.79 (0.56–1.11)), Blacks vs. whites (HR 0.74 (0.51–1.08)), or other races vs. whites (HR 0.59 (0.30–1.14)) (Fig. 1d). Initial weight loss and mean weekly self-reported physical activity were strongly associated with retention. Enrollees who lost no weight vs. any weight at week 3 were less likely to be retained (HR 0.80 (0.65–0.97)) (Fig. 1e). Enrollees with lower levels of self-reported physical activity were less likely to be retained than enrollees with higher levels of physical activity (HR 0.37 (0.30–0.47) for <60 min vs. ≥150 min; HR 0.79 (0.63–0.99) for 60–149 min vs. ≥150 min) (Fig. 1f).
Fig. 1.
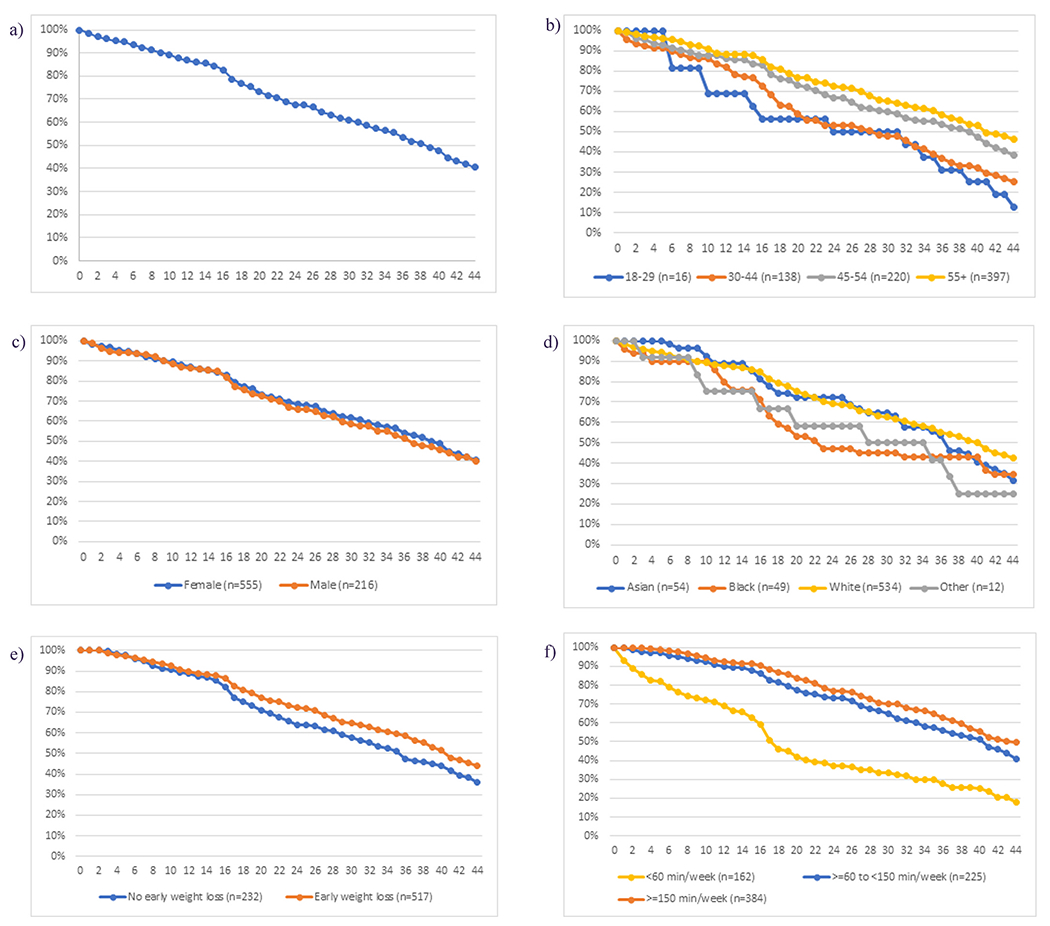
NDPP retention by program week.
a) Overall percent retention among enrollees.
b) Percent retention by age group.
c) Percent retention by sex.
d) Percent retention by race.
e) Percent retention by weight loss at 3 weeks.
f) Percent retention by mean physical activity minutes per week.
At 1-year follow-up, reductions in BMI were significantly greater in enrollees compared to non-enrollees (−1.2 ± 2.4 vs. −0.1 ± 2.4 kg/m2, p < 0.001). At 1-year, reductions in systolic and diastolic blood pressure, total cholesterol, triglycerides, and HbA1c were all significantly greater in enrollees compared to non-enrollees (Table 2). At 2-years, the differences in clinical outcomes between enrollees and non-enrollees were attenuated but the reductions in BMI (−0.6 ± 2.7 vs. −0.1 ± 2.9 kg/m2, p < 0.001), triglycerides (−27 ± 103 vs. −6 ± 87 mg/dl, p = 0.004), and HbA1c (0.0 ± 0.5 vs. 0.1 ± 0.6 %, p = 0.039) remained significantly greater among enrollees (Table 2).
Table 2.
1- and 2-year changes in risk factors overall and for NDPP enrollees and non-enrollees, and adjusted change in risk factors among NDPP enrollees and non-enrollees.a
| Overall | Enrollees | Non-enrollees | p-Value | N used in model | Adjusted mean change in risk factor among enrolleesa (95 % CI) | Adjusted mean change in risk factor among non-enrolleesa (95 % CI) | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Number (N) | 8131 | 776 | 7355 | – | – | – | – | – |
| One-year changes | ||||||||
| BMI (kg/m2) | −0.2 ± 2.5 | −1.2 ± 2.4 | −0.1 ± 2.4 | <0.001 | 5145 | −1.1 (−1.3 to −0.8) | −0.1 (−0.3 to 0.1) | <0.001 |
| Blood pressure (mmHg) | ||||||||
| Systolic | 0 ± 16 | −2 ± 15 | 0 ± 16 | 0.002 | 4910 | −2 (−3 to 0) | 0 (−1 to 1) | 0.003 |
| Diastolic | 0 ± 11 | −1 ± 11 | 0 ± 11 | 0.0325 | 4910 | −1 (−2 to 0) | 0 (−1 to 1) | 0.002 |
| Lipids (mg/dl) | ||||||||
| Total cholesterol | −2 ± 30 | −6 ± 32 | −1 ± 30 | 0.032 | 1952 | −8 (−12 to −3) | −3 (−6 to 0) | 0.022 |
| HDL-c | 0 ± 8 | 1 ± 8 | 0 ± 8 | 0.561 | 1947 | 1 (−1 to 2) | 0 (0 to 1) | 0.881 |
| Triglycerides | −8 ± 89 | −27 ± 103 | −6 ± 87 | 0.004 | 1936 | −30 (−42 to −18) | −10 (−18 to −2) | <0.001 |
| LDL-c | −2 ± 26 | −4 ± 25 | −2 ± 26 | 0.091 | 2537 | −5 (−9 to −2) | −3 (−5 to −1) | 0.100 |
| HbA1c (%) | 0.0 ± 0.6 | −0.1 ± 0.4 | 0.0 ± 0.6 | <0.001 | 2382 | −0.1 (−0.2 to 0.0) | 0.0 (0.0 to 0.1) | <0.001 |
| Two-year changes | ||||||||
| BMI (kg/m2) | −0.1 ± 2.9 | −0.6 ± 2.7 | −0.1 ± 2.9 | <0.001 | 4760 | −0.5 (−0.8 to −0.2) | −0.2 (−0.4 to 0.0) | 0.009 |
| Blood pressure (mmHg) | ||||||||
| Systolic | 1 ± 16 | 0 ± 16 | 1 ± 16 | 0.151 | 4556 | −1 (−2 to 1) | 0 (−1 to 1) | 0.084 |
| Diastolic | −1 ± 11 | −1 ± 11 | 0± 11 | 0.129 | 4556 | −1 (−2 to 0) | 0 (−1 to 0) | 0.010 |
| Lipids (mg/dl) | ||||||||
| Total cholesterol | −1 ± 33 | −2 ± 31 | −1 ± 33 | 0.718 | 1536 | −4 (−10 to 2) | −2 (−6 to 1) | 0.586 |
| HDL-c | 1 ± 8 | 1 ± 7 | 0 ± 8 | 0.155 | 1553 | 1 (−1 to 3) | 1 (0 to 1) | 0.534 |
| Triglycerides | −8 ± 89 | −27 ± 103 | −6 ± 87 | 0.004 | 1936 | −30 (−42 to −18) | −10 (−17 to −2) | <0.001 |
| LDL-c | −3 ± 28 | −4 ± 28 | −3 ± 29 | 0.302 | 2461 | −6 (−10 to −2) | −4 (−6 to −1) | 0.169 |
| HbA1c (%) | 0.1 ± 0.6 | 0.0 ± 0.5 | 0.1 ± 0.6 | 0.039 | 2293 | 0.0 (−0.1 to 0.1) | 0.1 (0.0 to 0.1) | 0.219 |
Adjusted for baseline age group, sex, race, and value of the risk factor.
Table 2 also shows the changes in risk factors by NDPP enrollment status adjusted for baseline age group, sex, race, and value of the risk factor. At 1-year, the mean changes in BMI, systolic blood pressure, diastolic blood pressure, total cholesterol, triglycerides, and HbA1c were significantly greater in enrollees than non-enrollees. At 2-years, the changes in BMI, diastolic blood pressure, and triglycerides remained significantly greater in enrollees than non-enrollees.
At 1- and 2-years, the incidence of diabetes was lower among enrollees than non-enrollees based on HbA1c ≥6.5 % (8 % vs. 12 % at 1-year, p = 0.003 and 11 % vs. 15 % at 2-years, p = 0.022) and self-report (3 % vs. 7 % at 1-year, p = 0.004 and 6 % vs. 11 % at 2-years, p = 0.009) (Table 3). When enrollees were stratified by retention, those who disenrolled before week 16 had greater incidences of diabetes by both the HbA1c criterion and self-report, and those who completed the program through week 44 had significantly lower incidences of diabetes at both 1- and 2-years compared to non-enrollees (Table 3). In multivariable models adjusting for age group, sex, and race, the odds of developing diabetes based on HbA1c ≥6.5 % was 40 % lower at 1-year for enrollees compared to non-enrollees (OR = 0.60, 95 % CI (0.41–0.86), p = 0.005) and 20 % lower at 2-years although the difference at 2-years was not statistically significant (OR = 0.80, 95 % CI (0.60–1.05), p = 0.108) (Table 3). The adjusted odds of self-reported diabetes was 57 % lower in enrollees compared to non-enrollees at 1-year (OR 0.43, 95 % CI 0.22–0.83, p = 0.013) and 46 % lower at 2-years (OR 0.54, 95 % CI 0.32–0.91, p = 0.021) (Table 3).
Table 3.
Incidence of diabetes defined by HbA1c ≥6.5 % and by self-report at 1- and 2-years stratified by NDPP enrollment and retention, and adjusted odds of progression to diabetes.a
| Total N | No diabetes | Diabetes | p-Value | Adjusted odds ratio (95 % CI) compared to the reference groupa | p-Value | |
|---|---|---|---|---|---|---|
| 1-year outcome | ||||||
| Diabetes by HbA1c criterion | ||||||
| Not enrolled | 3548 | 3112 | 436 (12 %) | 0.003 | (reference) | |
| Enrolled | 546 | 503 | 43 (8 %) | 0.60 (0.41–0.86) | 0.005 | |
| Disenrolled before week 16 | 73 | 62 | 11 (15 %) | 0.007 | 1.37 (0.69–2.74) | 0.371 |
| Disenrolled after week 16 but before week 44 | 220 | 198 | 22 (10 %) | 0.73 (0.44–1.22) | 0.229 | |
| Completed through week 44 | 251 | 241 | 10 (4 %) | 0.29 (0.14–0.59) | 0.006 | |
| Self-report of diabetes | ||||||
| Not enrolled | 699 | 648 | 51 (7 %) | 0.004 | (reference) | |
| Enrolled | 439 | 425 | 14 (3 %) | 0.43 (0.22–0.83) | 0.013 | |
| Disenrolled before week 16 | 33 | 28 | 5 (15 %) | <0.001 | 2.40 (0.85–6.77) | 0.100 |
| Disenrolled after week 16 but before week 44 | 168 | 162 | 6 (4 %) | 0.39 (0.13–1.10) | 0.075 | |
| Completed through week 44 | 235 | 232 | 3 (1 %) | 0.20 (0.06–0.64) | 0.007 | |
| 2-year outcome | ||||||
| Diabetes by HbA1c criterion | ||||||
| Not enrolled | 4717 | 4033 | 684 (15 %) | 0.022 | (reference) | |
| Enrolled | 653 | 580 | 73 (11 %) | 0.80 (0.60–1.05) | 0.108 | |
| Disenrolled before week 16 | 92 | 73 | 19 (21 %) | 0.002 | 1.65 (0.95–2.87) | 0.075 |
| Disenrolled after week 16 but before week 44 | 268 | 238 | 30 (11 %) | 0.75 (0.49–1.15) | 0.189 | |
| Completed through week 44 | 290 | 267 | 23 (8 %) | 0.58 (0.36–0.91) | 0.018 | |
| Self-report of diabetes | ||||||
| Not enrolled | 664 | 591 | 73 (11 %) | 0.009 | (reference) | |
| Enrolled | 402 | 377 | 25 (6 %) | 0.54 (0.32–0.91) | 0.021 | |
| Disenrolled before week 16 | 28 | 22 | 6 (21 %) | <0.001 | 1.80 (0.64–5.06) | 0.266 |
| Disenrolled after week 16 but before week 44 | 159 | 147 | 12 (8 %) | 0.60 (0.29–1.25) | 0.173 | |
| Completed through week 44 | 214 | 207 | 7 (3 %) | 0.33 (0.15–0.75) | 0.008 |
Adjusted for age group, sex, and race.
5. Discussion
In this real world study, we found that after adjustment for baseline age group, sex, race, and value of the risk factor, the mean improvement in BMI, systolic blood pressure, diastolic blood pressure, total cholesterol, triglycerides, and HbA1c at 1-year was significantly greater among NDPP enrollees than non-enrollees. At 2-years, the improvement in BMI, diastolic blood pressure, and triglycerides remained significantly greater in enrollees compared to non-enrollees. When we defined diabetes by HbA1c ≥ 6.5 % at follow-up, the incidence of diabetes was significantly lower in NDPP enrollees than non-enrollees at 1-year (8 % vs. 12 %, p = 0.003) and at 2-years (11 % vs. 15 %, p = 0.022). In a multivariate model adjusting for age group, sex, and race that was stratified by enrollment and retention, we found that the odds of developing diabetes based on HbA1c criteria was 40 % lower for enrollees at 1-year (p = 0.005) and 20 % lower at 2-years (p = 0.108). Adjusted rates of self-reported diabetes were 57 % lower in enrollees compared to non-enrollees at 1-year (p = 0.013) and 46 % lower at 2-years (p = 0.021). The DPP clinical trial demonstrated the efficacy of an intensive lifestyle intervention to delay or prevent diabetes in carefully selected individuals with overweight or obesity and both IFG and IGT.1 Compared to the placebo intervention, the intensive lifestyle intervention reduced the incidence of diabetes from 11.0 cases per 100 person-years to 4.8 cases per 100 person-years at 2.8 years (a 58 % relative risk reduction).1
The real-world effectiveness of intensive lifestyle interventions to delay or prevent the development of diabetes in individuals with prediabetes has been less clear. A meta-analysis of 19 randomized trials that tested a variety of lifestyle interventions in adults with prediabetes defined by IFG, IGT, or both reported that the incidence of diabetes was reduced from 11.4 cases per 100 person-years in control participants to 7.4 cases per 100 person-years in lifestyle intervention participants at 2.6 years (a 39 % relative risk reduction).7 A second meta-analysis of 23 trials that used less rigorous eligibility criteria found that lifestyle interventions were associated with a 22 % relative risk reduction.8 A third meta-analysis of 63 real world lifestyle modification programs to prevent diabetes reported that only 14 reported the numbers of participants who developed diabetes.9 In the 7 controlled studies, diabetes cumulative incidence was 8.5 per 100 person years in control participants and 6.0 per 100 person years in intervention participants. The relative risk of diabetes among participants receiving the intervention was 29 % lower (relative risk 0.71 (95 % CI 0.58–0.88)).9
Previously, we demonstrated that using insurance records and targeted screening, we were able to identify as many as 42 % of all employees, dependents, and retirees with prediabetes and overweight or obesity in the U-M workforce.10 We further demonstrated that people with prediabetes who enrolled in the NDPP were older, more likely to be women, to have received medical care in the past year, and to live in neighborhoods with higher household incomes, lower rates of unemployment, and lower percentages of families receiving Supplemental Nutrition Assistance Program (SNAP) benefits.10 When we examined the domains of the Health Belief Model, we also found that enrollees perceived greater benefits of health-protective action and were more likely to receive cues to action than non-enrollees.11
We found that the uptake of the NDPP was low among eligible U-M employees, dependents, and retirees (9.5 %) but was nearly 4-fold higher than has been observed among U.S. adults with prediabetes who reported being told by a health professional that they had the condition (2.5 %). Despite the low uptake, we have now demonstrated that overall retention was good among U-M NDPP enrollees (median number of sessions attended 18, median retention 38 weeks with 77 % retention through 18 weeks and 40 % retention through 44 weeks). Cannon et al. reported that between 2016 and 2017, the median number of sessions attended by NDPP enrollees nationwide was 16 and median retention was 28 weeks.6 Sixty-three percent of enrollees were retained in the program through eighteenth weeks and 32 % through 44 weeks.6 Among the approximately 15,000 people enrolled in the NDPP between 2012 and 2016, 87 % attended four or more sessions and of them, only 70 % attended at 16 weeks and 22 % attended at 10 months or more.5 Like Cannon, we found that attrition increases between weeks 16 and 18 when session frequency typically transitions from weekly to monthly.6 We also found that retention among enrollees was greater among older age groups and among enrollees with greater initial weight loss and self-reported minutes of physical activity.6
Our finding that the incidence of diabetes was higher in enrollees who disenrolled from the NDPP before completing the core curriculum than in non-enrollees suggests that enrollees were at higher baseline risk for diabetes than non-enrollees. The older age of enrollees and higher BMI and HbA1c levels at baseline supports this hypothesis. The higher baseline risk of enrollees compared to non-enrollees but the lower incidence of diabetes among enrollees compared to non-enrollees also highlights the effectiveness of the NDPP among program completers.
Because of the relatively small sample size and low uptake of the NDPP among U-M employees, dependents, and retirees with prediabetes, we were unable to demonstrate a change in the incidence of diabetes at a population level as was demonstrated by McManus et al. who assessed the population health impact of systematically implementing the National Health System Diabetes Prevention Programme (NHSDPP) on the incidence of diabetes in England12 Over 271,000 of the 513,000 eligible individuals with HbA1c levels between 6.0 and 6.4 % or fasting glucose levels between 100 and 125 mg/dl attended an initial assessment (52.8 %) and over 101,000 (19.7 %) attended at least 60 % of NHSDPP sessions. Using a difference-in-differences methodology, the authors demonstrated that the incidence of type 2 diabetes was reduced by approximately 7 % on a population basis.
Together, our results suggest that among NDPP enrollees with prediabetes proactively identified from a large and diverse employer group and diagnosed with prediabetes on the basis of HbA1c and/or medical claims criteria, retention was good, risk factors were improved, and diabetes was delayed or prevented for up to 2-years when assessed by self-report. Longer-term follow-up of the DPP clinical trial cohort and simulation modeling have both demonstrated that preventing or delaying the onset of type 2 diabetes and reducing cumulative glycemic exposure are associated with a lower risk of complications.13,14 The clinical and public health challenge is to increase the diagnosis and awareness of prediabetes at the population level and to ensure that at-risk individuals are referred to effective programs.15 Of the approximately 14.6 million U.S. adults with diagnosed prediabetes and elevated body mass index, ~300,000 (2 %) reported having been referred to a type 2 diabetes prevention program in 2016–2017.3 Potential barriers to NDPP uptake include low rates of screening and diagnosis of prediabetes, inadequate healthcare professional communication with at-risk patients, confusion as to who should be screened and referred, lack of CDC-recognized programs, and insufficient insurance coverage.16
There are a number of limitations to our study. First, NDPP uptake was low although higher than reported for the U.S. as a whole. Second, enrollees were more socioeconomically advantaged and probably more highly motivated that non-enrollees. Offering the NDPP at no out-of-pocket cost likely increased uptake and financial incentives provided to contracted NDPP providers for enrollee retention may have increased retention and improved outcomes. Nevertheless, enrollees were at higher baseline risk based on older age, higher BMI, and higher HbA1c and enrollment reduced the incidence of type 2 diabetes. Because most study subjects had information on HbA1c levels available through the health plan but only a sample of non-enrollees had survey data, we were unable to assess incident diabetes based on both laboratory criteria and self-report for the entire population. Despite these limitations, our results are encouraging.
Acknowledgments
The authors thank Marsha Manning, former Manager, Medical Benefits and Strategy at U-M; Ashley Weigl, Associate Director, MHealthy; and Dr. Marc D. Keshishian and Dawn Beaird, Blue Cross Blue Shield of Michigan, for their contributions to this project.
Funding
This work was supported by National Institutes of Health, National Institute of Diabetes, Digestive, and Kidney Diseases grant number R01 DK109995.
Footnotes
CRediT authorship contribution statement
W.H.H. researched the data, wrote the manuscript, and reviewed and edited the manuscript. K.L.J. and C.V. contributed to the discussion and reviewed and edited the manuscript. L.N.M. researched the data, performed statistical analyses, assisted in writing the manuscript, contributed to the discussion, and reviewed and edited the manuscript. W.H.H is the guarantor of this work and as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis.
Declaration of competing interest
No potential conflicts of interest were reported.
References
- 1.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes prevention program research group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albright AL, Gregg EW. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am J Prev Med. 2013;44:S346–S351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cannon MJ, Ng BP, Lloyd K, Reynolds J, Ely EK. Delivering the National Diabetes Prevention Program: assessment of enrollment in in-person and virtual organizations. J Diabetes Res. 2022;2022:2942918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Diabetes Statistics Report website. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed January 31, 2023.
- 5.Ely EK, Grass SM, Luman ET, Gregg EW, Ali MK, Nhim K, et al. A national effort to prevent type 2 diabetes: participant-level evaluation of CDC’s national diabetes prevention program. Diabetes Care. 2017;40:1331–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cannon MJ, Masalovich S, Ng BP, Soler RE, Jabrah R, Ely EK, et al. Retention among participants in the National Diabetes Prevention Program Lifestyle Change Program, 2012-2017. Diabetes Care. 2020;43:2042–2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haw JS, Galaviz KI, Straus AN, Kowalski AJ, Magee MJ, Weber MB, et al. Long-term sustainability of diabetes prevention approaches: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2017;177:1808–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jonas DE, Crotty K, Yun JDY, Cook Middleton J, Feltner C, Taylor-Phillips S, et al. Screening for prediabetes and type 2 diabetes mellitus: an evidence review for the U.S. Preventive Services Task Force [internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2021. (Aug. Evidence Synthesis, No. 207.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK574057/. Accessed November 29, 2022 (Aug. Evidence Synthesis, No. 207.) Available from:. [PubMed] [Google Scholar]
- 9.Galaviz KI, Weber MB, Straus A, Haw JS, Narayan KMV, Ali MK. Global diabetes prevention interventions: a systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose. Diabetes Care. 2018;41:1526–1534. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herman WH, Joiner KL, Hurst T, McEwen LN. The effectiveness of a proactive, three-level strategy to identify people with prediabetes in a large workforce with employer-sponsored health insurance. Diabetes Care. 2021;44:1532–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joiner KL, McEwen LN, Hurst TE, Adams MP, Herman WH. Domains from the health belief model predict enrollment in the National Diabetes Prevention Program among insured adults with prediabetes. J Diabetes Complicat. 2022;36:108220. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McManus E, Meacock R, Parkinson B, Sutton M. Population level impact of the NHS diabetes prevention programme on incidence of type 2 diabetes in England: an observational study. Lancet Regional Health Europe. 2022;19, 100420 [Published Online May 29]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the diabetes prevention program outcomes study. Lancet Diabetes Endocdnol. 2015;3:866–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herman WH, Hoerger TJ, Brandle M, Hicks K, Sorensen S, Zhang P, et al. The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med. 2005;142:323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herman WH, Schillinger D, Bolen S, Boltri JM, Bullock A, Chong W, et al. The National Clinical Care Commission Report to Congress: recommendations to better leverage federal policies and programs to prevent and control diabetes. Diabetes Care: In press; 2023. [In press]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ali MK, McKeever Bullard K, Imperatore G, Benoit SR, Rolka DB, Albright AL, et al. Reach and use of diabetes prevention services in the United States, 2016-2017. JAMA Netw Open. 2019;2, el93160. [DOI] [PMC free article] [PubMed] [Google Scholar]


