Abstract
Objectives:
To investigate resident-level, provider-type, nursing home (NH), and regional factors associated with feeding tube (FT) placement in advanced dementia.
Design:
Retrospective cohort study.
Setting and Participants:
NH residents in Texas with dementia diagnosis and severe cognitive impairment (N = 20,582).
Methods:
This study used 2011–2016 Texas Medicare data to identify NH residents with a stay of at least 120 days who had a diagnosis of dementia on Long Term Care Minimum Data Set (MDS) evaluation and severe cognitive impairment on clinical score. Multivariable repeated measures analyses were conducted to identify associations between FT placement and resident-level, provider-type, NH, and regional factors.
Results:
The prevalence of FT placement in advanced dementia in Texas between 2011 and 2016 ranged from 12.5% to 16.1% with a nonlinear trend. At the resident level, the prevalence of FT decreased with age [age > 85 years, prevalence ratio (PR) 0.60, 95% confidence interval (CI) 0.52–0.69] and increased among residents who are black (2.74, 95% CI 2.48–3.03) or Hispanic (PR 1.91, 95% CI 1.71–2.13). Residents cared for by a nurse practitioner or physician assistant were less likely to have an FT (PR 0.90, 95% CI 0.85–0.96). No facility characteristics were associated with prevalence of FT placement in advanced dementia. There were regional differences in FT placement with the highest use areas on the Texas-Mexico border and in South and East Texas (Harlingen border area, PR 4.26, 95% CI 3.69–4.86; San Antonio border area, PR 3.93, 95% CI 3.04–4.93; Houston, PR 2.17, 95% CI 1.87–2.50), and in metro areas (PR 1.36, 95% CI 1.22–1.50).
Conclusions and Implications:
Regional, race, and ethnic variations in prevalence of FT use among NH residents suggest opportunities for clinicians and policy makers to improve the quality of end-of-life care by especially considering other palliative care measures for minorities living in border towns.
Keywords: Dementia, feeding tube, nursing home, palliative care, border, Texas
Patients in the advanced stage of dementia have progressive difficulties with eating and swallowing, leading to recurrent aspiration, pneumonia and weight loss.1–3 These complications are a natural progression of dementia and contribute to the high rates of hospitalization and intensive care use in the last month of life.3,4 Clinical Practice Guidelines from AMDAeThe Society for Post-Acute and Long-Term Care Medicine, the American Geriatrics Society, and the Choosing Wisely Initiative list feeding tube (FT) insertion in advanced dementia as low-value care that should be avoided.5,6 The guidelines reflect a large body of evidence showing no association between FT use in advanced dementia and improvement in quality of life, prevention of aspiration, and increase in survival.1–3 Indeed, the median survival of nursing home (NH) residents with advanced dementia after FT insertion was 56 days, with a mean of 9.1 days of hospital stay in the year post tube insertion.3 For patients with advanced dementia who do not have an FT placed, hand feeding may continue as palliative care.5,6 Conversation with families early in the disease process about what to expect as dementia progresses to its terminal stage is an important part of end-of-life planning, and documentation of end-of-life wishes has been associated with decreased rates of FT placement.7
Nationally, the proportion of the NH residents with advanced dementia receiving an FT has decreased from 11.7% of patients in 2000 to 5.7% of patients in 2014, yet high rates of use persist in some areas.8–10 The persistence reflects discordance in perception of tube feeding benefits between residents’ surrogates and providers caring for patients with advanced dementia.2,7,11,12 This discordance is apparent at the provider level as rates of FT insertion vary substantially by type of attending physicians caring for hospitalized NH patients with dementia, with subspecialists having the highest rate of FT placement (11.0%) vs hospitalists (1.6%).12 As with providers, rates of FT placement vary by patient characteristics and at the NH level.13–15 For example, there is evidence that residents in NH with advanced practice providers (APPs) on staff are less likely to have FTs.13 APPs comprise nurse practitioners and physician assistants. This is important because data showed nurse practitioners spend more time on site in the nursing facilities and have more opportunities to address goals of care with the patients’ surrogate decision makers.16
Texas is among the top 3 states with the highest prevalence of dementia, making this discussion relevant to both residents and public health.15 The rate of FT use in dementia varies widely across the United States, with Texas having moderately high use.9 The variation continues at the local level, with discrete areas of Texas in which the rates of FT placement are lower or higher than the national average.10 The current study is an in-depth analysis of data collected on all NH patients with and without dementia who resided in Texas from January 1, 2011, through December 31, 2016. The study aims are to examine resident-level, provider-type, NH, and regional factors associated with FT placement in advanced dementia and discuss next steps in decreasing this low-value intervention. Understanding these complex relationships has potential to inform clinical practice and guide policy aimed at improving quality of end-of-life care for the growing number of NH residents.
Methods
Data Source
We analyzed a sample of Texas Medicare beneficiaries from Medicare claims and Long Term Care Minimum Data Set (MDS) from January 1, 2011, through December 31, 2016. Master Beneficiary Summary Files were used to check Medicare enrollment status. Medicare Provider Analysis and Review files were used to define skilled nursing facility stay. Outpatient Standard Analytic Files (Out-SAF) and Carrier claims were used to determine number of primary care visits and primary care provider type. MDS was used to identify the duration of NH stay, demographic factors, and assessment on active diagnoses, cognitive patterns, and nutritional approaches. Nursing Home Compare data were downloaded from Centers for Medicare & Medicaid Services (CMS) website to define facility characteristics in the corresponding study year.17 Health service region, metropolitan status, and border area by county data were downloaded from Texas Department of State Health Services Center for Health Statistics website.18
Study Population
We selected the beneficiaries with Fee-for-Service enrollment (Part A and B enrollment) and without health maintenance organization enrollment in whole calendar year, and with at least 120 days’ continuous stay in long-term care facility not including skilled nursing facility stay. Only subjects with Alzheimer’s disease or dementia and severe impairment on cognitive skills for daily decision making were included (Supplementary Table 1). Each beneficiary could contribute up to 6 years. Our final study cohort included 20,582 NH residents contributing 34,628 person-years, and 12,447 (60.47%) of them were eligible for only 1 year. Residents with only 1 year of eligibility were more likely to be older and die during study period (Supplementary Table 2).
Measurement
FT use was derived from MDS section K assessment (nutritional approach during the last 7 days). Demographic factors and comorbidity were identified from the first MDS assessment during observed episodes. Primary care visit and provider characteristics were defined from outpatient statistical analysis files and carrier files. Primary care visit was determined with Current Procedural Terminology code, and primary care provider was determined by CMS provider specialty codes and taxonomy code (Supplementary Table 3). In each calendar year, all primary care claims were selected to determine primary care provider type for each resident for the corresponding year. The residents with at least 2 visits in a year were assigned the provider type as physician or APP based on the provider type providing the majority of care or, in the case of a tie, the provider type that had the initial visit. For those with less than 2 visits, the provider type was unknown. The county of the facility was used to determine health service region, metropolitan status, and border area. The health service regions on the Texas-Mexico border were further divided into 2 regions (border and nonborder) for modeling.
Statistical Method
Continuous variables were described as mean and standard deviation (SD) and categorical variables were described as count and percentage. Chi-square test and t test were applied for group comparison on baseline characteristics in 2016. Generalized estimating equations (GEEs) with a logit link binomial distribution and first-order autoregression, AR(1), as correlation structure was used to estimate adjusted odds ratio (OR) of residents’ characteristics, provider-type, facility, and regional characteristics on FT insertion. Adjusted ORs was converted to prevalence ratios (PRs) with the following formula: PR = OR/[(1 – P0) (P0 × OR)]. P0 indicates the prevalence of FT use in the reference group.19 All analyses were performed with SAS, version 9.4 (SAS Inc., Cary, NC).
Results
The prevalence of FT use in all patients with advanced dementia in Texas ranged from 12.5% to 16.1% between 2011 and 2016 without a linear trend (Table 1). Table 2 showed the distribution of individual and facility characteristics among nursing home residents with advanced dementia in 2016, while Table 3 showed the PR estimation on feeding tube insertion for all NH residents, using all covariates in the multivariable model. For patients with an NH stay of 1 year or less, there was an overall decreasing trend of FT use between 2011 and 2016 [PR 0.71, 95% confidence interval (CI) 0.60–0.85]. For patients living in the NH more than 1 year, there was an increasing prevalence between 2011 and 2016 (PR 1.62, 95% CI 1.46–1.78) (Supplementary Table 4). Multivariable analysis of 2011–2016 data showed that prevalence of FT use decreased with age (age > 85 years, PR 0.60, 95% CI 0.52–0.69) and significantly increased among residents of black race or Hispanic ethnicity (non-Hispanic black, PR 2.74, 95% CI 2.48–3.03; Hispanic, PR 1.91, 95% CI 1.71–2.13). Residents with comorbid anemia (PR 1.19, 95% CI 1.12–1.27), heart failure (PR 1.13, 95% CI 1.03–1.23), urinary tract infection (PR 1.19, 95% CI 1.10–1.28), and diabetes (PR 1.36, 95% CI 1.25–1.47) had increased rates of FT use. Most significantly, residents with stroke had 1.67 higher prevalence of FT use (95% CI 1.55–1.80) (Table 3). In terms of provider characteristics, there was a decreased prevalence of FT use among patients primarily taken care of by an APP (PR 0.90, 95% CI 0.85–0.96). There were no associations found between FT placement and the facility characteristics of nonprofit status, registered nurse or total staffing, star quality ranking, and number of beds.
Table 1.
Feeding Tube Insertion From 2011 to 2016
| Year | All Subjects* | Only 1 Year Eligible | More Than 1 Year Eligible | |||
|---|---|---|---|---|---|---|
| n | With Feeding Tube, n (%) | n | With Feeding Tube, n (%) | n | With Feeding Tube, n (%) | |
| 2011 | 6234 | 852 (13.7) | 3124 | 441 (14.1) | 3110 | 411 (13.2) |
| 2012 | 6188 | 914 (14.8) | 1911 | 273 (14.3) | 4277 | 641 (15.0) |
| 2013 | 6599 | 1059 (16.0) | 1919 | 271 (14.1) | 4680 | 788 (16.8) |
| 2014 | 6282 | 1009 (16.1) | 1884 | 260 (13.8) | 4398 | 749 (17.0) |
| 2015 | 4750 | 592 (12.5) | 1463 | 144 (9.8) | 3287 | 448 (13.6) |
| 2016 | 4575 | 576 (12.6) | 2146 | 225 (10.5) | 2429 | 351 (14.5) |
Each resident could be eligible for 1 to 6 calendar years. There were 20582 residents contributing 34628 person-years. There were 60% residents with only 1 year of eligibility.
Table 2.
Distribution of Individual and Facility Characteristics Among Residents With Advanced Dementia in 2016
| Variable | Feeding Tube, n (%) | Without Feeding Tube, n (%) | P Value* |
|---|---|---|---|
| Residents’ characteristics | n = 576 | n = 3999 | |
| Age, y | <.001 | ||
| <65 | 75 (22.5) | 259 (77.5) | |
| 66–75 | 132 (17.9) | 606 (82.1) | |
| 76–85 | 197 (12.2) | 1417 (87.8) | |
| >85 | 172 (9.1) | 1717 (90.9) | |
| Gender | <.001 | ||
| Male | 180 (15.9) | 953 (84.1) | |
| Female | 396 (11.5) | 3046 (88.5) | |
| Race | <.001 | ||
| Non-Hispanic white | 186 (6.4) | 2709 (93.6) | |
| Non-Hispanic black | 138 (25.3) | 408 (74.7) | |
| Hispanic | 210 (21.5) | 769 (78.5) | |
| Other | 42 (27.1) | 113 (72.9) | |
| Marital status | <.001 | ||
| Married | 162 (13.0) | 1080 (87.0) | |
| Widowed | 238 (10.7) | 1995 (89.3) | |
| Other | 176 (16.0) | 924 (84.0) | |
| Type of provider† | .15 | ||
| MD | 355 (13.5) | 2274 (86.5) | |
| NP/PA | 166 (11.9) | 1227 (88.1) | |
| Active diagnosis at initial MDS | |||
| Anemia | |||
| Yes | 191 (15.9) | 1011 (84.1) | <.001 |
| No | 385 (11.4) | 2988 (88.6) | |
| Heart failure | |||
| Yes | 64 (11.9) | 476 (88.1) | .58 |
| No | 512 (12.7) | 3523 (87.3) | |
| Hypertension | |||
| Yes | 428 (13.0) | 2869 (87.0) | .20 |
| No | 148 (11.6) | 1130 (88.4) | |
| PVD or PAD | |||
| Yes | 58 (17.9) | 266 (82.1) | .003 |
| No | 518 (12.2) | 3733 (87.8) | |
| Urinary tract infection | |||
| Yes | 25 (13.2) | 165 (86.8) | .81 |
| No | 551 (12.6) | 3834 (87.4) | |
| Diabetes | |||
| Yes | 221 (19.5) | 914 (80.5) | <.001 |
| No | 355 (10.3) | 3085 (89.7) | |
| Thyroid Disorder | |||
| Yes | 44 (11.8) | 328 (88.2) | .64 |
| No | 532 (12.7) | 3671 (87.3) | |
| Arthritis | |||
| Yes | 33 (10.4) | 284 (89.6) | .23 |
| No | 543 (12.8) | 3715 (87.2) | |
| Osteoporosis | |||
| Yes | 20 (8.3) | 220 (91.7) | .041 |
| No | 556 (12.8) | 3779 (87.2) | |
| Stroke | |||
| Yes | 140 (25.5) | 408 (74.5) | <.001 |
| No | 436 (10.8) | 3591 (89.2) | |
| Anxiety | |||
| Yes | 176 (10.0) | 1590 (90.0) | <.001 |
| No | 400 (14.2) | 2409 (85.8) | |
| Depression | |||
| Yes | 254 (10.3) | 2223 (89.7) | <.001 |
| No | 322 (15.3) | 1776 (84.7) | |
| Asthma | |||
| Yes | 74 (15.6) | 401 (84.4) | .038 |
| No | 502 (12.2) | 3598 (87.8) | |
| Facility characteristics | n = 568 | n = 3974 | |
| Ownership | <.001 | ||
| Profit | 511 (13.6) | 3234 (86.4) | |
| Nonprofit or government | 57 (7.2) | 740 (92.8) | |
| Quality rank (1–5)‡ | .05 | ||
| 1–3 | 285 (11.6) | 2168 (88.4) | |
| >3 | 283 (13.5) | 1806 (86.5) | |
| RN staffing, adjusted hours per resident day‡,§ | .07 | ||
| ≤Median (0.326) | 304 (13.4) | 1966 (86.6) | |
| >Median (0.326) | 264 (11.6) | 2008 (88.4) | |
| Total staffing, adjusted hours per resident day‡,§ | .034 | ||
| ≤Median (3.457) | 307 (13.5) | 1959 (86.5) | |
| >Median (3.457) | 261 (11.5) | 2015 (88.5) | |
| Certified beds‡ | .022 | ||
| <100 | 133 (10.4) | 1151 (89.6) | |
| 100–200 | 410 (13.4) | 2652 (86.6) | |
| >200 | 25 (12.8) | 171 (87.2) | |
| Health service region | <.001 | ||
| Region 1 (Lubbock) | <15 (<10) | >167 (>90) | |
| Region 2/3 (Arlington) | 115 (9.3) | 1121 (90.7) | |
| Region 4/5N (Tyler) | 61 (10.4) | 528 (89.6) | |
| Region 6/5S (Houston) | 110 (17.2) | 530 (82.8) | |
| Region 7 (Temple) | 52 (7.6) | 632 (92.4) | |
| Region 8 (San Antonio) | 65 (11.7) | 490 (88.3) | |
| Region 9/10 (El Paso) | <11 (<5) | >180 (>95) | |
| Region 11 (Harlingen) | 145 (31.2) | 2652 (68.8) | |
| Metro area | <.001 | ||
| Metro county | 432 (14.0) | 2664 (86.0) | |
| Nonmetro county | 136 (9.4) | 1310 (90.6) | |
| Border area | <.001 | ||
| Border county | 141 (37.1) | 239 (62.9) | |
| Nonborder county | 427 (10.3) | 3735 (89.7) |
NP, nurse practitioner; PA, physician assistant; PAD, peripheral arterial disease; PVD, peripheral vascular disease; RN, registered nurse.
Chi-square tests were applied for group comparison.
Only determined for those subjects with at least 2 primary care visits.
Average of 4 quarterly nursing home comparison data reports in 2016.
Median was determined by assessment year.
Table 3.
Prevalence Ratio Estimation on Feeding Tube Insertion for All Subjects
| Variable | Univariate PR (95% CI) |
Multivariable* PR (95% CI) |
|---|---|---|
| Year of residency | ||
| 2011 | Ref | Ref |
| 2012 | 1.14 (1.08–1.20)† | 1.09 (1.03–1.16)† |
| 2013 | 1.23 (1.16–1.31)† | 1.19 (1.10–1.28† |
| 2014 | 1.30 (1.22–1.38)† | 1.19 (1.10–1.28)† |
| 2015 | 1.28 (1.19–1.37)† | 1.20 (1.10–1.30)† |
| 2016 | 1.30 (1.21–1.40)† | 1.28 (1.18–1.40)† |
| Age, y | ||
| <65 | Ref | Ref |
| 66–75 | 0.81 (0.72–0.90)† | 0.79 (0.69–0.89)† |
| 76–85 | 0.66 (0.58–0.74)† | 0.64 (0.56–0.73)† |
| >85 | 0.62 (0.55–0.69)† | 0.60 (0.52–0.69)† |
| Gender | ||
| Male | Ref | Ref |
| Female | 0.76 (0.71–0.81)† | 0.93 (0.86–1.01) |
| Race | ||
| Non-Hispanic white | Ref | Ref |
| Non-Hispanic black | 3.28 (3.00–3.58)† | 2.74 (2.48–3.03)† |
| Hispanic | 3.09 (2.87–3.33)† | 1.91 (1.71–2.13)† |
| Other | 2.09 (1.87–2.34)† | 1.86 (1.64–2.10)† |
| Marital status | ||
| Married | Ref | Ref |
| Widowed | 0.88 (0.81–0.95)† | 0.87 (0.79–0.95)† |
| Other | 1.17 (1.06–1.29)† | 0.95 (0.86–1.05) |
| Comorbidity | ||
| Without disease | Ref | Ref |
| Anemia | 1.20 (1.13–1.28)† | 1.19 (1.12–1.27)† |
| Heart failure | 1.16 (1.07–1.27)† | 1.13 (1.03–1.23)† |
| Hypertension | 1.11 (1.04–1.18)† | 1.01 (0.94–1.08) |
| PVD or PAD | 1.23 (1.11–1.35)† | 1.09 (0.98–1.22) |
| Urinary tract infection | 1.12 (1.06–1.20)† | 1.19 (1.10–1.28)† |
| Diabetes | 1.56 (1.43–1.70)† | 1.36 (1.25–1.47)† |
| Thyroid disorder | 1.07 (0.99–1.14) | 1.09 (0.99–1.19) |
| Arthritis | 0.98 (0.91–1.06) | 0.94 (0.84–1.04) |
| Osteoporosis | 1.06 (0.98–1.15) | 1.06 (0.95–1.17) |
| Stroke | 1.56 (1.44–1.68)† | 1.67 (1.55–1.80)† |
| Anxiety | 0.92 (0.88–0.97)† | 0.92 (0.87–0.97)† |
| Depression | 0.84 (0.79–0.88)† | 0.79 (0.75–0.84)† |
| Asthma | 1.12 (1.02–1.22)† | 1.12 (1.02–1.23)† |
| Provider type | ||
| MD | Ref | Ref |
| NP/PA | 0.97 (0.91–1.04) | 0.90 (0.85–0.96)† |
| Ownership‡ | ||
| Profit | Ref | Ref |
| Nonprofit or government | 0.97 (0.93–1.01) | 0.94 (0.89–1.00) |
| Quality§ | ||
| Rank 1–3 | Ref | Ref |
| Good (5-star rank >3) | 1.08 (1.04–1.13)† | 1.03 (0.98–1.08) |
| RN staffing§ | ||
| ≤Median | Ref | Ref |
| >Median | 1.00 (0.96–1.04) | 1.03 (0.99–1.08) |
| Total staffing§ | ||
| ≤Median | Ref | Ref |
| >Median | 0.99 (0.95–1.03) | 1.01 (0.97–1.06) |
| Certified beds§ | ||
| <100 | Ref | Ref |
| 100–200 | 1.12 (1.04–1.21)† | 1.07 (0.98–1.16) |
| >200 | 0.98 (0.83–1.14) | 0.98 (0.83–1.15) |
| Health service region | ||
| Temple | Ref | Ref |
| Lubbock | 0.61 (0.45–0.84)† | 0.89 (0.64–1.22) |
| Arlington | 1.26 (1.09–1.45)† | 1.27 (1.09–1.48)† |
| Tyler | 1.35 (1.15–1.58)† | 1.59 (1.33–1.89† |
| Houston | 2.41 (2.12–2.72)† | 2.17 (1.87–2.50)† |
| San Antonio (border) | 3.33 (2.54–4.20)† | 3.93 (3.04–4.93)† |
| San Antonio (not border) | 1.54 (1.31–1.81)† | 1.49 (1.24–1.77)† |
| El Paso (border) | 2.33 (1.85–2.88)† | 1.98 (1.50–2.57)† |
| El Paso (not border) | 0.63 (0.45–0.86)† | 0.69 (0.47–1.01) |
| Harlingen (border) | 4.58 (4.16–4.99)† | 4.26 (3.69–4.86)† |
| Harlingen (not border) | 1.95 (1.56–2.41)† | 2.01 (1.60–2.51)† |
| Metro county | 1.60 (1.47–1.74)† | 1.36 (1.22–1.50)† |
NP, nurse practitioner; PA, physician assistant; PAD, peripheral arterial disease; PVD, peripheral vascular disease; Ref, referent; RN, registered nurse.
Multivariable was a full mode with all covariates in the model.
P < .05.
Ownership status in corresponding study year.
Average of 4 quarterly assessments in corresponding study year. For 2013, the facility without quarterly report was determined by average of 6 monthly assessments (July-December).
On the larger scale, patients residing in southern and eastern heath service regions in Texas were more likely to have an FT placed in advanced dementia; however, between 2011 and 2016, the trends in FT placement between regions did not vary significantly (Figure 1). In terms of absolute percentage, in 2016, more than 30% of residents with advanced dementia in the Harlingen service region had an FT compared to less than 5% of residents in the El Paso service region (Table 2). The multivariate prevalence ratio of FT placement for residents with advanced dementia was the highest in the Harlingen service region border area, at 4.26 times that of the Temple region (95% CI 3.69–4.86). Within the Harlingen service region, along with the other regions on the border, the prevalence was higher within 100 km of the border. For example, the El Paso region excluding the border had a PR of 0.69 (95% CI 0.47–1.01), the lowest in this study, but the border of the El Paso region had a PR of 1.98 (95% CI 1.50–2.57). Not including the border, the Houston (PR 2.17, 95% CI 1.87–2.50) and Harlingen (PR 2.01, 95% CI 1.60–2.51) service regions had the highest prevalence of FT placement. Residents in metropolitan areas had 1.36 times the prevalence of residents in rural areas (95% CI 1.22–1.50).18
Fig. 1.
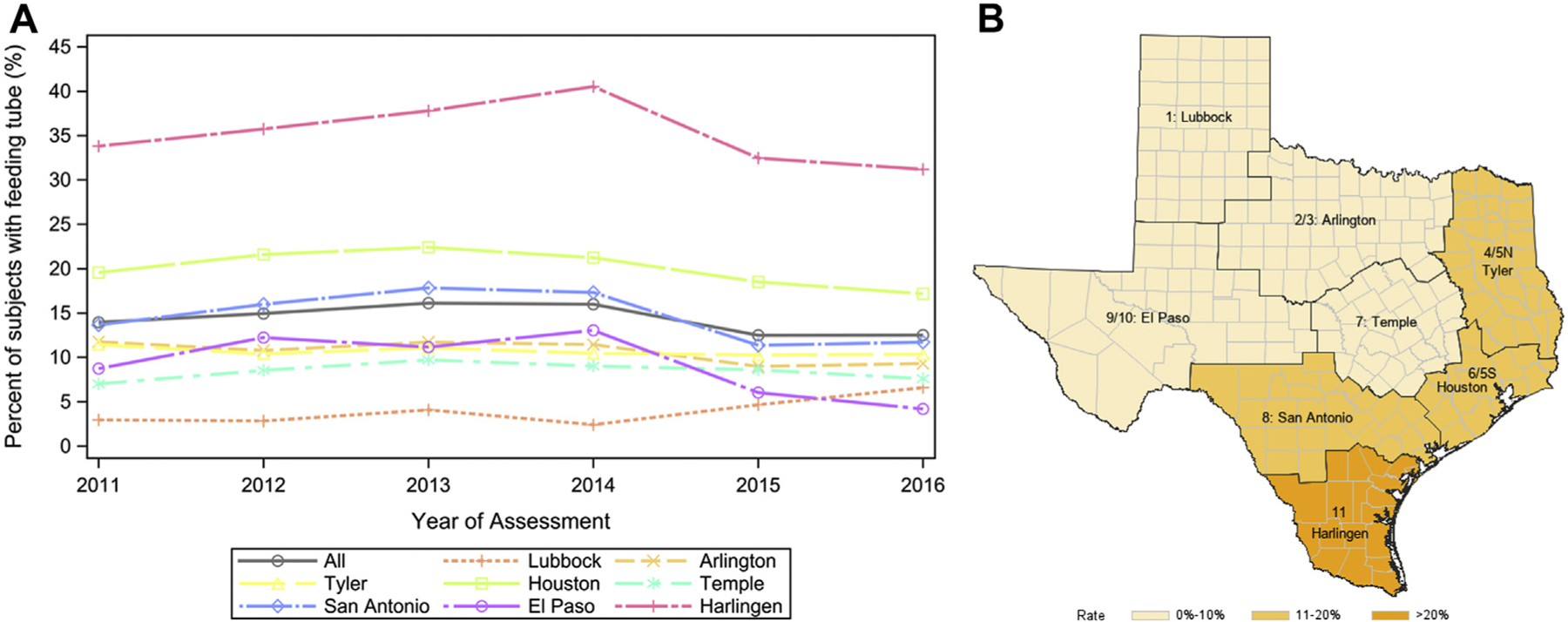
Percentage of nursing home residents with feeding tube insertion (A) for all residents with facility characteristics measured from 2011 to 2016 stratified by 8 health service regions and (B) for residents in 2016 (n = 4542) by health service region with the percentage categorized into 3 levels: low (0%–10%), middle (11%–20%), and high (>20%).
Discussion
Of all the resident-level findings, the most significant was the higher prevalence of FT use in residents who are black or Hispanic. This finding has been widely reported elsewhere.8,13 Nursing home residents in Texas with advanced dementia who are black had 2.74 times the prevalence (95% CI 2.48–3.03) and Hispanic residents had 1.91 times the prevalence (95% CI 1.71–2.13) of FT use compared with non-Hispanic white residents. Interestingly, though the overall rate of FT placement in the USA decreased between 2000 and 2014, the rate fell more sharply for residents who are black, from 37.5% in 2000 to 17.5% in 2014, compared with a decrease of 5.5% among white residents.8 That said, patient-centered research is needed, especially among the nonwhite population, to assess if the changing rates in FT use reflect a change in access to care or shifts in preferences of patients, their surrogate decision makers or families, or increasing awareness of the Choosing Wisely initiative on the futility of FT use in advanced dementia.5,6
Also consistent with prior research, our study found variation in FT placement by comorbid conditions.8,13 FT use in advanced dementia was associated with comorbid diagnoses of anemia, diabetes, urinary tract infection, and stroke. Past research showed most FT are placed during hospitalizations, thus explaining, at least in part, the relationship between exacerbations of chronic illnesses (eg, diabetes) or new onset of severe acute illness (eg, urinary tract infection) leading to hospitalizations, and subsequent FT placement.7 As expected, chronic conditions (eg, osteoporosis and arthritis) with low risk of severe exacerbations are associated with a lower prevalence of FT placement.
Outside of patient-level characteristics, resident FT use varied by provider-type (APP vs physician), with patients cared for a majority of the time by APPs having a lower prevalence of FT use (PR 0.90, 95% CI 0.85–.096) even after adjusting for factors like NH for-profit status and star quality ranking. An increasing proportion of APPs devote most or all of their time to NH care, and research showed that the higher the proportion of time providers devote to NH care, the lower the likelihood of hospitalizations of the NH residents.16,20 In other studies, APP nursing home providers had an increased presence in the NH and more resident visits compared with physicians who may have additional sites of care.16,20,21 In the state of Texas, APPs work collaboratively with physicians and, by state law, are overseen by physicians but, by Medicare regulations, APPs are able to alternate visits with physicians for skilled nursing residents and perform two-thirds of the visits for those living in long-term care.22
Contrary to other studies, our analysis found no relationship between NH characteristics (nonprofit status, registered nurse or total staffing, star quality ranking, number of beds) and prevalence of FT use in advanced dementia. Past analyses, one of which used nationwide MDS data, however, found relationships between increased use of FT and larger NH size and for-profit ownership.13,23 It is unclear if our findings represent a regional difference or a larger national trend.
There are known regional differences in FT placement in advanced dementia with at least a 10-fold variation across the United States.9,10 Among health service regions in Texas, those in the south and east have the highest rates of FT placement in advanced dementia. Apart from communities on the Texas-Mexico border, the Houston (PR 2.19, 95% CI 1.78–2.67) and Harlingen (PR 1.96, 95% CI 1.43–2.63) service regions had the highest prevalence of FT placement, and the El Paso region the lowest (PR 0.69, 95% CI 0.47–1.01). Of note, prior studies have shown a high rate of general overuse of medical interventions, regardless of indications, in the town of McAllen in the Harlingen health service region compared with El Paso.24,25 Our study supports those findings. The strongest regional association with FT placement in advanced dementia was being within 100 km of the Texas-Mexico border, an area defined as the border region by the La Paz agreement.26 Within 100 km of the border, the prevalence of FT placement was more than double the prevalence in the rest of the border regions even after adjusting for resident characteristics associated with FT use like race and ethnicity. A more detailed study of the border area would be helpful in understanding what factors (eg, culture of resource overutilization, less adoption of advance directive, density of “proceduralists,” family preference) account for the high rate of FT use and in determining trends of use. Cross-border health care was fairly common along the Texas-Mexico border and was more common among urban area residents.27 Our findings of metro county residents having a prevalence 1.36 times of that of rural residents (95% CI 1.22–1.50) suggest a need for cross-national study of twin cities along the Texas-Mexico border, like McAllen and Reynosa; such study can potentially benefit USA and Mexico by identifying factors associated with use of low-value care.
Our study had several limitations including using only 1 year of data for 60% of residents. Also person-years were used in analysis, with some subjects living the entire 5 years of the study. Of the subjects with 1 year of data, a higher percentage were older and died during the study period. Our study found that the overall prevalence of FT placement in patients with only 1 year of data decreased between 2011 and 2016, suggesting a possible trend of decreasing FT use in high-risk patients. On the converse, in the analysis of data containing multiple patient-years, the odds of having an FT increased between 2011 and 2016. Of all the comorbid conditions studied, residents with history of stroke had the strongest association with FT use (PR 1.67, 95% CI 1.55–1.80). It is hypothesized that patients with cognitive impairment and/or dysphagia due to stroke or other causes outside of dementia likely had an effect on calculation of the prevalence of FT use in patients with advanced dementia. Also, our study did not capture people in long-term care who died before 120 days in the facility. The 30-day mortality post-FT placement has been estimated at 54% for patients with advanced dementia.28 Therefore, in our analysis, we likely missed a number of patients who received FT but died from dementia within 3 months of the procedure.
In sum, our most significant findings are the higher prevalence of FT use in residents who are black or Hispanic and in residents who live on the Texas-Mexico border, suggesting underuse of the AMDA-endorsed alternative (hand feedingd—a form of palliative care) to FT placement in NH residents with advanced dementia.5,6 There are known disparities among people of black race or Hispanic ethnicity in access to palliative care, with studies showing implicit bias underpinning the lower referral rates and access to timely palliative care in racial and ethnic minorities.8,13,29–31 Written advance directives, reflecting the preferences and values of the residents, are associated with lower rates of FT insertion.7 One approach to ensure adherence to patient’s end-of-life preferences is by education of patient’s surrogates with validated clinical decision aides.32 Such approach has been shown to reduce burdensome and low-value interventions such as FT insertion in patients with advanced dementia.32 Another approach is to discuss at every clinical encounter the need to execute a Physician Order for Life Sustaining Treatment (POLST) document and advance directives, especially at the early stage of dementia when patients still have decisional capacity. In Texas, the Medical Orders for Scope of Treatment document outlines preference for or against medically assisted nutrition and, though not codified, can guide providers and the patients’ caregivers to choose interventions that are consistent with the patients’ values and end-of-life preferences.33
Conclusions and Implications
Both AMDA—The Society for Post-Acute and Long-Term Care Medicine and the American Geriatrics Society recommend against FT placement in advanced dementia and encourage hand feeding.5,6 The prevalence of FT use in advanced dementia was nearly 2 to 3 times greater in nursing home residents who were black and/or Hispanic. Regionally, nursing home residents living on the Texas-Mexico border had more than double the prevalence of FT use. Though further studies are needed to examine the factors underlying these racial and ethnic and regional variation, our research findings along with the known racial and ethnic disparities in access to palliative care underscore the need for policy mandating incorporation of advanced care planning process into routine operation of all nursing homes. Such policy is key toward providing high-quality end-of-life care by decreasing the use of potentially harmful procedures such as FT placement in advanced dementia.
Supplementary Material
Acknowledgments
This work was supported by grants R01-HS020642 from the Agency for Healthcare Research and Quality, and P30-AG024832 from the National Institutes of Health. V.S. is funded by the Texas Alzheimer’s Research and Care Consortium.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Sampson EL, Candy B, Jones L. Enteral tube feeding for older people with advanced dementia. Cochrane Database Syst Rev; 2009:CD007209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mitchell SL. Clinical practice. Advanced dementia. N Engl J Med 2015;372: 2533–2540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuo S, Rhodes RL, Mitchell SL, et al. Natural history of feeding-tube use in nursing home residents with advanced dementia. J Am Med Dir Assoc 2009;10: 264–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen C, Downer B, Chou LN, et al. End-of-Life healthcare utilization of older Mexican Americans with and without a diagnosis of Alzheimer’s disease and related dementias. J Gerontol A Biol Sci Med Sci 2020;75:326–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.AMDAeThe Society for Post-Acute and Long-Term Care Medicine. Ten things physicians and patients should question. Available at: https://www.choosingwisely.org/societies/amda-the-society-for-post-acute-and-long-term-care-medicine/. Accessed April 12, 2020.
- 6.American Geriatrics Society. Choosing WiselydPromoting conversations between providers and patients. Available at: https://www.choosingwisely.org/clinician-lists/american-geriatrics-society-percutaneous-feeding-tubes-in-patients-with-dementia/. Accessed April 12, 2020.
- 7.Teno JM, Mitchell SL, Gozalo PL, et al. Hospital characteristics associated with feeding tube placement in nursing home residents with advanced cognitive impairment. JAMA 2010;303:544–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell SL, Mor V, Gozalo PL, et al. Tube feeding in US nursing home residents with advanced dementia, 2000–2014. JAMA 2016;316:769–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teno JM, Mor V, DeSilva D, et al. Use of feeding tubes in nursing home residents with severe cognitive impairment. JAMA 2002;287:3211–3212. [DOI] [PubMed] [Google Scholar]
- 10.Bynum J, Meara E, Chang CH, et al. Our parents, ourselves: Health care for an aging population. Dartmouth Atlas Project. 2016;1:38–39. Available at: https://www.dartmouthatlas.org/%20downloads/reports/Our_Parents_Ourselves_021716.pdf. Accessed November 23, 2020. [PubMed] [Google Scholar]
- 11.Day LW, Nazareth M, Sewell JL, et al. Practice variation in PEG tube placement: Trends and predictors among providers in the United States. Gastrointest Endosc 2015;82:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teno J, Meltzer DO, Mitchell SL, et al. Type of attending physician influenced feeding tube insertions for hospitalized elderly people with severe dementia. Health Aff (Millwood) 2014;33:675–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mitchell SL, Teno JM, Roy J, et al. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. JAMA 2003;290:73–80. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell SL, Kiely DK, Jones RN, et al. Advanced dementia research in the nursing home: the CASCADE study. Alzheimer Dis Assoc Disord 2006;20: 166–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koller D, Bynum JP. Dementia in the USA: State variation in prevalence. J Public Health (Oxf) 2015;37:597–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuo YF, Raji MA, Goodwin JS. Association between proportion of provider clinical effort in nursing homes and potentially avoidable hospitalizations and medical costs of nursing home residents. J Am Geriatr Soc 2013;61: 1750–1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. Research, statistics, data & systems. CMS.gov. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Research-Statistics-Data-and-Systems. Accessed April 17, 2020. [Google Scholar]
- 18.Texas Health and Human Services. Texas metropolitan status by county. Available at: https://dshs.texas.gov/chs/info/current-msa.shtm?terms=metro. Accessed April 23, 2020.
- 19.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 1998;280: 1690–1691. [DOI] [PubMed] [Google Scholar]
- 20.Teno JM, Gozalo PL, Trivedi AN, et al. Temporal trends in the numbers of skilled nursing facility specialists from 2007 through 2014. JAMA Intern Med 2017; 177:1376–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aigner MJ, Drew S, Phipps J. A comparative study of nursing home resident outcomes between care provided by nurse practitioners/physicians versus physicians only. J Am Med Dir Assoc 2004;5:16–23. [PubMed] [Google Scholar]
- 22.Hamilton T Physician delegation of tasks in skilled nursing facilities (SNFs) and nursing facilities (NFs). cms.gov.2013. Available at: https://wwhttps://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-13-15-.pdf. Accessed June 12, 2020. [Google Scholar]
- 23.Mitchell SL, Kiely DK, Gillick MR. Nursing home characteristics associated with tube feeding in advanced cognitive impairment. J Am Geriatr Soc 2003;51: 75–79. [PubMed] [Google Scholar]
- 24.Gawande A The cost conundrum. The New Yorker 2009;1:36–44. Available at: https://www.newyorker.com/magazine/2009/06/01/the-cost-conundrum. Accessed April 24, 2020. [Google Scholar]
- 25.Franzini L, Mikhail OI, Skinner JS. McAllen And El Paso revisited: Medicare variations not always reflected in the under-sixty-five population. Health Aff (Millwood) 2010;29:2302–2309. [DOI] [PubMed] [Google Scholar]
- 26.Office of Global Affairs. The U.S.-Mexico border region. hhs.gov. Available at: https://www.hhs.gov/about/agencies/oga/about-oga/what-we-do/international-relations-division/americas/border-health-commission/us-mexico-border-region/index.html. Accessed June 12, 2020. Published 2017. [Google Scholar]
- 27.Su D, Pratt W, Salinas J, et al. Rural-urban differences in health services utilization in the US-Mexico border region. J Rural Health 2013;29: 215–223. [DOI] [PubMed] [Google Scholar]
- 28.Goldberg LS, Altman KW. The role of gastrostomy tube placement in advanced dementia with dysphagia: a critical review. Clin Interv Aging 2014;9: 1733–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lopez RP, Amella EJ, Strumpf NE, et al. The influence of nursing home culture on the use of feeding tubes. Arch Intern Med 2010;170:83–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agency for Healthcare Research and Quality. Chartbook on person and family centered care: End-of-life care measures. Available at: https://www.ahrq.gov/research/findings/%20nhqrdr/chartbooks/personcentered/measures5.html. Accessed April 23, 2020.
- 31.Yancu CN, Farmer DF, Leahman D. Barriers to hospice use and palliative care services use by African American adults. Am J Hosp Palliat Med 2010;27: 248–253. [DOI] [PubMed] [Google Scholar]
- 32.Hanson LC, Carey TS, Caprio AJ, et al. Improving decision-making for feeding options in advanced dementia: A randomized, controlled trial. J Am Geriatr Soc 2011;59:2009–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Texas Medical Orders for Scope of Treatment. Texasmost.com. 2018. Available at: http://texasmost.com/wp-content/uploads/2019/01/MOSTform92818.pdf. Accessed June 12, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


