Abstract
Background
Omega-3 polyunsaturated fatty acids (n-3 PUFA) have been suggested as a cognitive enhancing agent, though their effect is doubtful. We aimed to examine the effect of n-3 PUFA on the cognitive function of middle-aged or older adults without dementia.
Methods
We reviewed randomized controlled trials of individuals aged 40 years or older. We systematically searched PubMed/MEDLINE, EMBASE, CINAHL, PsycINFO, and Cochrane Library databases. We used the restricted cubic splines model for non-linear dose–response meta-analysis in terms of the standardized mean difference with 95% confidence intervals.
Results
The current meta-analysis on 24 studies (n 9660; follow-up 3 to 36 months) found that the beneficial effect on executive function demonstrates an upward trend within the initial 12 months of intervention. This effect is prominently observed with a daily intake surpassing 500 mg of n-3 PUFA and up to 420 mg of eicosapentaenoic acid (EPA). Furthermore, these trends exhibit heightened significance in regions where the levels of blood docosahexaenoic acid (DHA) + EPA are not very low.
Conclusions
Supplementation of n-3 PUFA may confer potential benefits to executive function among the middle-aged and elderly demographic, particularly in individuals whose dietary DHA + EPA level is not substantially diminished.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-024-03296-0.
Keywords: N-3 PUFA, Polyunsaturated fatty acids, Omega-3, Mild cognitive impairment, Cognitive function, Dose–response meta-analysis
Background
In 1971, Bang et al. [1] suggested a beneficial effect of the dietary n-3 polyunsaturated fatty acid (PUFA) such as docosahexaenoic acid (DHA) or eicosapentaenoic acid (EPA) on the incidence of ischemic heart disease. Since then, abundant epidemiological studies have explored its role on the cognitive function in human [2–4] under the assumption that the n-3 PUFA helps resolve inflammation and facilitate brain development [5], reduces accumulation of amyloid β [6], and increases the production of brain-derived neurotrophic factor (BDNF) [7].
Unfortunately, the efficacy of n-3 PUFAs on cognition has not been proven consistently in previous meta-analyses. In older adults aged 60 years or older with mild cognitive impairment (MCI), n-3 PUFAs were beneficial on mini-mental status examination (MMSE) (weighted mean difference = 0.85) [8]. Conversely, in adults aged 18 years or older, the impact of n-3 PUFA on MMSE was either negligible [9] or demonstrated very modest benefits at best resulting in less than 1% change in MMSE score [10]. Moreover, in younger adults aged between their 20 s and 30 s, no discernible influence of n-3 PUFA on cognition was identified [11, 12]. McCaddon and Miller asserted that to have any expectation of observing an effect of a nutritional intervention within a typical time frame of clinical trials from months to years, it is required that the participants should experience cognitive decline or on the verge of it during the study period [13]. These findings suggest that the inclusion of young adults in trials is unlikely to yield a significant effect of the intervention material on age-related cognitive trajectories [14]. Given that this age-related cognitive decline might commence as early as in 20 s to 30 s [15], it would be judicious to restrict the inclusion criteria to individuals aged 40 or older for meta-analyses. On the other hand, MCI represents a syndrome distinguished by cognitive impairment that deviates from the anticipated age-related trajectories, while daily functioning is not disturbed to qualify for the diagnosis of dementia [16]. Therefore, it would be meaningful to investigate the potential impact of n-3 PUFA with respect to the presence of MCI among the included studies.
Previous meta-analyses have primarily investigated the relationship between dose and response using linear models on subsets of included trials. However, this linear relationship could rarely be presumed in biological research [17], and subgroup analyses by categorizing trials could lead to a reduction in power and loss of information pertaining to the association to be examined [18, 19]. In this regard, the application of spline functions, which employ all available data points to explore the dose–response relationship between the intervention and the outcome, is capable of modeling intricate nonlinear associations [20, 21]. While several previous dose–response meta-analyses have already been conducted, they have either included, in their analyses, very young adults around the age of 30 [22], exclusively dealt with prospective cohort studies [23, 24], or were unable to conduct dose–response analyses due to data scarcity [8]. Furthermore, none of the preceding meta-analyses have investigated this association in relation to the nationwide blood levels of DHA + EPA, despite the potential influence of early-life or long-term exposure to n-3 PUFA on cognitive function [25].
Therefore, the objective of this study was to examine the impact of n-3 PUFAs on cognitive function in non-demented individuals, encompassing both cognitively normal older adults and those with MCI, belonging to the middle-aged or older age group (≥ 40 years old). This investigation employed restricted cubic splines models [26] on randomized controlled trials with subgroup analyses by the nation-wide blood level of DHA + EPA and by the presence of MCI.
Methods
This study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [27] and its protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO, registration number: CRD42020221943).
Criteria for study inclusion/exclusion
The selection of studies based on the Population, Intervention, Comparison, Outcomes, and Study Design (PICOS) criteria for this review is as follows: (1) inclusion of human subjects without dementia, aged 40 years or older; (2) incorporation of interventions involving n-3 PUFA, DHA, EPA, or alpha-linolenic acid (ALA); (3) administration of intervention supplements alone or in combination with other supplements, excluding B vitamins; (4) implementation of interventions lasting 3 or more months; (5) outcomes in the form of cognitive test scores; (6) availability of the mean difference of the test scores before and after the intervention, along with dispersion data such as standard deviation (SD), standard errors of the mean (SEM), confidence intervals, t statistics, P values, or F statistics; (7) structured as a randomized placebo-controlled clinical trial; and (8) studies published in any language.
Search strategy and study selection
Electronic searches of the PubMed/MEDLINE, EMBASE, CINAHL, PsycINFO, and Cochrane Library database were performed by SW Suh, E Lim, and KW Kim from inception to Sep 2023. Searches for the gray literature were also sought through the International Clinical Trials Registry Platform Search Portal. Search strategies for each database are presented in the Additional file 1: Table S1 which were built based on a previous literature.
From the search results, S-Y Burm and H Lee selected studies independently that fit the inclusion and exclusion criteria based on their titles followed by their abstracts. Subsequent full-text evaluation of the selected studies was conducted independently by SW Suh and E Lim. Non-English texts were translated into English using Google Translate. Disagreement of the selection results between two investigators that are not resolved by their discussion was settled by KW Kim and JW Han.
Outcomes
For the primary outcome, we used the standardized mean difference of the test scores on global cognitive function between baseline and follow-up assessments. For the secondary outcomes, we used the mean difference of the test scores on episodic memory, executive function, processing speed, attention, and visuospatial function between baseline and follow-up.
Data extraction and assessment of methodological quality
SW Suh and E Lim, working independently, extracted data on the study design, recruitment setting and location, sample size, baseline characteristics of participants such as age and sex ratio, intervention methods (ingredients, dosage, frequency, and duration), compliance to the intervention, funding sources, and the mean difference in the cognitive performance of participants before and after the intervention along with its corresponding SD or SEM. The mean difference was represented as standardized mean difference (SMD), factoring in the combined SD, with correction for small sample bias using Hedges’ g [28]. In instances where the dispersion data on the mean difference was not provided, it was computed in adherence to the Cochrane guidelines [29]. We grouped the cognitive tests by the cognitive domain they mainly represent based on a previous work [30]. If a study reported outcomes of multiple tests for a single cognitive domain, we chose the most frequently used test among the overall included studies to maximize the homogeneity of the outcome variable. If there were several scores of multiple time points for a given cognitive test under random-effects model, we used the one with the longest intervention period. Additionally, in case that a given study did not report numerical data of cognitive test scores, we approximated the means and measures of dispersion from figures, if available. For studies with a crossover design, we only used data prior to the crossover.
SW Suh and E Lim also evaluated risk of bias (RoB) of each included study using the RoB Tool from the Cochrane Handbook [29] in respect of the random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. We made summary assessments of the RoB by the order of priority of the following rules: (1) “high” for the high risk of one or more key domains; (2) “unclear” for the unclear risk of one or more key domains; and (3) “low” for the low risk of all key domains [29]. We determined the key domains to be the allocation concealment, blinding of participants and personnel, and blinding of outcome assessment because the outcome, cognitive test scores, could be critically affected by the preconception of the interviewer and/or interviewee. Disagreement between these two investigators about the extracted data or RoB that was not resolved by a discussion was settled by KW Kim and JW Han. We requested necessary information that was not available in the published article by e-mailing to the respective corresponding author.
Statistical analyses
We first synthesized data using standard inverse-variance random-effects model [31] for meta-analyses utilizing standardized mean differences (SMD) along with their corresponding 95% confidence intervals (CIs). This approach was adopted due to the diverse outcome measures employed by researchers in assessing cognitive function. We also conducted sensitivity analyses by eliminating one study at a time to examine the influence of each study on the results. We assessed the between-trial heterogeneity using I2 and τ2 values. Publication bias was ascertained by Egger’s test when at least 7 studies were included, as well as the visual inspection of the funnel plot.
For the nonlinear dose–response meta-analysis, we used a restricted cubic spline model applying weighted mixed-effects models [32] in accordance with the methodology demonstrated by Orsini et al. [26] with 3 knots at fixed percentiles (5, 50, and 95%). Estimates of the mixed-effects model were acquired by a restricted maximum likelihood method [32]. Through this, we evaluate the impact of key variables including the duration of the intervention (measured in months), daily intake of n-3 PUFA (in milligrams per day), cumulative PUFA consumption over the study period (in grams), daily intake of DHA (in milligrams per day), daily intake of EPA (in milligrams per day), and the ratio of DHA to EPA consumed. To ascertain nonlinearity, we conducted a Wald test [33]. In addition, we executed a linear dose–response meta-analysis, adhering to the approach elucidated by Greenland and Longnecker [34] and compared the goodness of fit, denoted by χ2, between the nonlinear and linear models. Furthermore, we visually examined the plot to facilitate the interpretation of the corresponding curve.
We performed a priori subgroup analyses for the primary outcome and for the secondary outcomes with significant nonlinear associations in the main analyses (1) by the nation-wide blood level of DHA + EPA (very low level with ≤ 4% such as USA, UK, Ireland, and Italy versus other countries with > 4% in erythrocyte equivalents) [35] and (2) by baseline cognitive function (normal cognition vs MCI). The blood level was defined as the percentage of DHA + EPA of total fatty acids in erythrocyte equivalents. All statistical analyses were executed using the R statistical software (version 4.3.1; R Foundation for Statistical Computing, Vienna, Austria) with a P-value of < 0.05 set as a statistical significance.
Results
Study selection
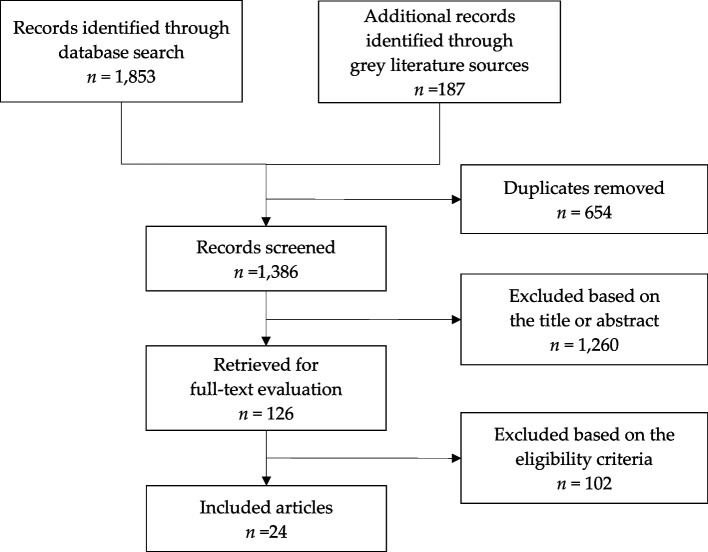
We retrieved 2040 articles and excluded 654 duplicates. Of the remaining 1386 articles, we excluded 1260 articles by screening the titles and abstracts. At this stage, we came to exclude all the non-English articles. Of the remaining 126 articles, we finally included 24 articles in the current systematic review after excluding 102 articles by full-text evaluation; 38 were not randomized or placebo-controlled, 11 had the intervention duration of less than 3 months, 17 included the participants under 40 years old, 10 included subjects who participated in other included studies, and 26 did not provide appropriate cognitive test results. We reached out to the corresponding authors but failed to get additional information on the missing data (Fig. 1).
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) diagram
Study characteristics
The characteristics of 24 individual trials are presented in Table 1. The sample size of them ranged from 29 to 2461, and the number of participants included in the current meta-analysis was 9660. Nine studies included the subjects with normal cognition only [36–44] while four studies composed only of people with MCI [45–48]. As for the intervention, three studies employed DHA only [36, 44, 49] and four studies employed ALA only [37, 39, 43, 50]. The length of intervention ranged from 3 to 36 months, and the daily dose of n-3 PUFA ranged from 230 to 4000 mg/day. Six studies were conducted in countries where the nationwide blood levels of DHA + EPA were notably low, measuring ≤ 4% in erythrocyte equivalents [36, 40, 44, 50–52].
Table 1.
Characteristics of included studies
| Study (year) | Country | Group | Age Mean (SD) |
Female (%) |
N | Duration (month) |
n-3 PUFA (mg/day) |
Cognitive measures used | Corresponding domain | Notes | Summary RoB |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Andrieu (2017) [53] | France | DHA, EPA | 75.6 (4.7) | 64 | 320 | 36 | 1025 | MMSE, FCSRT, CNT, DSST, TMT-A | GLO, MEM, EF, PS, ATT | Low | |
| Placebo | 75.1 (4.3) | 66 | 325 | ||||||||
| Arellanes (2020) [36] | USA | DHA | 68.5 (58,90)* | 89 | 15 | 6 | 2152 | MoCA, CVLT, TMT-B, TMT-A | GLO, MEM, EF, ATT | CN at baseline | Unclear |
| Placebo | 69 (58,79)* | 73 | 14 | ||||||||
| Bischoff-Ferrari (2020) [54] | Europe | DHA, EPA | 74.7 (4.3) | 62.3 | 1073 | 12, 24, 36 | 990 | MoCA | GLO | Low | |
| Placebo | 75.2 (4.6) | 61.2 | 1084 | ||||||||
| Bo (2017) [45] | China | DHA, EPA | 71.8 (5.68) | 40.9 | 44 | 6 | 1200 | BCAT, RM, MAE, PCT, SIE | GLO, MEM, EF, PS, VSF | MCI at baseline | Unclear |
| Placebo | 70.5 (6.82) | 40.5 | 42 | ||||||||
| Chew (2015) [51] | USA | DHA, EPA | 72.7 (7.7) | 58.8 | 1226 | 12 | 1000 | TICS | GLO | Low | |
| Placebo | 72.7 (7.8) | 56.2 | 1235 | ||||||||
| Dadova (2022) [55] | Czech Republic | DHA, EPA | 70.8 (3.6) | 100 | 27 | 4 | 230 | POBAV | MEM | Only women | Unclear |
| Placebo | 71.2 (4.0) | 100 | 25 | ||||||||
| Dangour (2010) [52] | UK | DHA, EPA | 74.7 (2.5) | 46.6 | 376 | 24 | 700 | GCF, CVLT, VF, SLM, DSF | GLO, MEM, EF, PS, ATT | Low | |
| Placebo | 74.6 (2.7) | 43.4 | 372 | ||||||||
| Geleijnse (2012) [56] | Netherlands | DHA, EPA | 69.2 (5.4) | 33 | 627 | 10 | 400 | MMSE | GLO | Low | |
| Placebo | 68.9 (5.4) | 20 | 638 | ||||||||
| Hashimoto (2016) [49] | Japan | DHA | 87.6 (3.3) | 88.4 | 39 | 6, 12 | 1720 | MMSE | GLO | Unclear | |
| Placebo | 89.6 (5.1) | 84.4 | 27 | ||||||||
| Hashimoto (2021) [37] | Japan | ALA | 71 (65, 83)* | 54.8 | 35 | 12 | 4000 | FAB | EF | CN at baseline | High |
| Placebo | 71 (64, 84)* | 51.5 | 24 | ||||||||
| Howe (2018) [57] | Australia | DHA, EPA | 63.2 (1.6) | 31.6 | 19 | 5 | 2000 | Corresponding Z scores (See Table S2) | GLO, EF, PS | Borderline hypertensive adults | Low |
| Placebo | 64.1 (2.3) | 31.6 | 19 | ||||||||
| Ichinose (2021) [38] | Japan | DHA, EPA | 69.1 (5.3) | 53.8 | 26 | 12 | 434 (297, 137) | MMSE | GLO | CN at baseline | Low |
| Placebo | 69.1 (4.9) | 55.6 | 27 | ||||||||
| Kuszewski (2020) [58] | Australia | DHA, EPA | 65.8 (1.4) | 53 | 26 | 4 | 2400 | RAVLT, Cognitive flexibility | MEM, EF | Low | |
| Placebo | 65.8 (1.4) | 56 | 26 | ||||||||
| Lee (2013) [46] | Malaysia | DHA, EPA | 66.4 (5.1) | 82.4 | 17 | 6, 12 | 1750 | Corresponding Z scores (see Table S2) | MEM, EF, PS, VSF | MCI at baseline | Low |
| Placebo | 63.5 (3.0) | 72.2 | 18 | ||||||||
| Macpherson (2022) [59] | Australia | DHA, EPA | 70.0 (6.3) | 70 | 69 | 6 | 1500 | MoCA, TMT-B, CPF-z, TMT-A | GLO, EF, PS, ATT | Intervened only 6 months. Next 6 months was without n-3 PUFA | Low |
| Placebo | 70.5 (5.9) | 70 | 72 | ||||||||
| Mengelberg (2022) [47] | New Zealand | DHA, EPA | 72.3 (6.2) | 53 | 30 | 12 | 1842 | RTot, RDM, TMT-B, DSF, RVC | GLO, MEM, EF, ATT, VSF | Low | |
| Placebo | 734. (7.0) | 63 | 30 | ||||||||
| Ogawa (2023) [39] | Japan | ALA | 71.9 (3.7) | 46.7 | 30 | 3 | 2200 | MMSE, WMSR-VM, LF, WAIS-PSI, WMSR-AC, WAIS-PRI | GLO, MEM, EF, PS, ATT, VSF | Low | |
| Placebo | 72.1 (4.3) | 53.3 | 30 | ||||||||
| Power (2022) [40] | Ireland | DHA, EPA | 69.0 (4.4) | 56.7 | 28 | 24 | 520 | RTot, SWM, SRT, | GLO, EF, PS | CN at baseline | Low |
| Placebo | 69.8 (3.7) | 70.0 | 22 | ||||||||
| Sala-Vila (2020) [50] | USA | ALA | 69.4 (3.8) | 67.4 | 324 | 6 | 1206 | RAVLT, SF, SDMT, TMT-A, block design | MEM, EF, PS, ATT, VSF |
Constituents were determined by FoodData Central** CN at baseline |
High |
| Placebo | 68.9 (3.5) | 68.5 | 312 | ||||||||
| Sinn (2012) [48] | Australia | DHA | 74.2 (7.0) | 28 | 16 | 6 | 1950/1830 | ILFC | EF | MCI at baseline | Unclear |
| EPA | 74.9 (5.1) | 18 | 13 | ||||||||
| Placebo | 73.0 (4.0) | 53 | 15 | ||||||||
| Tokuda (2020) [42] | Japan | DHA, EPA | 67.8 (0.8) | 66.7 | 27 | 6 | 400 | WMS-verbal delayed, VF, TMT-A | MEM, EF, ATT | CN at baseline | Low |
| Placebo | 67.7 (1.1) | 52.38 | 21 | ||||||||
| Valls-Pedret (2015) [43] | Spain | ALA | 66.7 (5.3) | 48.2 | 112 | 36 | 402.225 | MMSE, RAVLT, VF, DSF | GLO, MEM, EF, ATT |
Constituents were determined by FoodData Central** CN at baseline |
Unclear |
| Placebo | 67.9 (5.4) | 52.8 | 127 | ||||||||
| van de Rest (2008) [60] | Netherlands | DHA, EPA | 69.9 (3.4) | 45 | 96 | 3.25, 6.5 | 400, 1800 | Corresponding Z scores (see Table S2) | MEM, EF, ATT | Low | |
| Placebo | 70.1 (3.7) | 44 | 103 | ||||||||
| Yurko-Mauro (2010) [44] | USA | DHA | 70 (9.3) | 23.14 | 219 | 6 | 300 | MMSE, VRM, SOC | GLO, MEM, EF | CN at baseline | Unclear |
| Placebo | 70 (8.7) | 24.69 | 218 |
ATT attention, ALA alpha-linolenic acid, BCAT Basic Cognitive Aptitude Test, CN cognitively normal, CNT Category Naming Test, CPF-z Z score of Cogstate psychomotor function, CVLT California Verbal Learning Test, DHA docosahexaenoic acid, DSB Digit Span Backward, DSF Digit Span Forward, DSST Digit Symbol Substitution Test, EF executive function, EPA eicosapentaenoic acid, FAB frontal assessment battery, FCSRT Free and Cued Selective Reminding Test, GLO global cognition, GCF Global Cognition Function, ILFC Initial Letter Fluency Change, LM lexical fluency, MAE Mental Arithmetic Efficiency, MCI mild cognitive impairment, MEM episodic memory, MMSE Mini-Mental State Examination, MoCA Montreal Cognitive Assessment, PCT Perceptual Speed, POBAV Pojmenování OBrázků A jejich Vybavení (Picture naming and their recall), PS Processing Speed, RAVLT Rey Auditory Verbal Learning Test, RBANS Repeatable Battery for the Assessment of Neuropsychological Status, RDM delayed memory of RBANS, RM recognition memory, RVC visuospatial/constructional of RBANS, SDMT Symbol Digit Modalities Test, SF semantic fluency, SIE Space Imagery Efficiency, SLM Symbol Letter Modality, SOC Stockings of Cambridge, SRT simple reaction time, SWM spatial working memory, RTot total score of RBANS, TICS Telephone Interview for Cognitive Status, TMT-A Trail Making Test-A, TMT-B Trail Making Test-B, VF verbal fluency, VRM Verbal Recognition Memory, WAIS-PRI Wechsler Adult Intelligence Scale-perceptual reasoning index, WAIS-PSI Wechsler Adult Intelligence Scale-processing speed index, WMS Wechsler memory scale, WMSR-AC Wechsler memory scale revised-attention/concentration, WMSR-VM Wechsler memory scale revised-verbal memory
*median (min, max); **From U.S. Department of Agriculture (https://fdc.nal.usda.gov/)
Cognitive measures employed in the trials are presented in Additional file 1: Table S2. The most frequently employed measurement was the Mini-Mental State Examination (MMSE) for global cognition [38, 39, 43, 44, 46, 49, 53, 56], the delayed recall test from Rey Auditory Verbal Learning Test (RAVLT) for episodic memory [43, 46, 50, 58], verbal fluency test for executive function [42, 43, 50–53, 60], digit symbol substitution test for processing speed [39, 46, 53], trail making test A (TMT-A) for attention [36, 42, 50, 59, 60] and block design test for visuospatial function [39, 50].
Methodological quality
In terms of blindness and/or allocation concealment, two studies were at high risk of bias. Sala-Vila et al. acknowledged that the participants were not blinded because the intervention group was given a whole food while the placebo group was told to abstain from walnuts [50]. Hashimoto et al. also pointed out that the participants might be able to distinguish the type of intervention by odor or taste [37]. Other studies did not have a high risk of bias regarding key domains (Table 1). Supporting evidence for judging the RoB of individual trials is presented in Additional file 1: Table S3.
Efficacy of n-3 PUFA
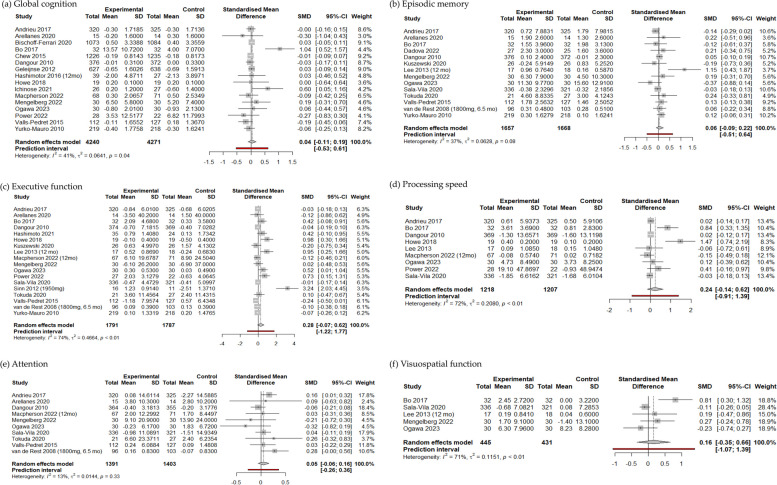
In the random-effects models, the intake of n-3 PUFA was not associated with the changes in global cognition (SMD [95% CI] = 0.0411 [− 0.1078, 0.1899]) and five other cognitive domains (Fig. 2). Statistical heterogeneity among the trials was substantial for the executive function (I2 = 74%, τ2 = 0.466), processing speed (I2 = 72%, τ2 = 0.208), and visuospatial function (I2 = 71%, τ2 = 0.115) [29].
Fig. 2.
Forest plots concerning the effect of n-3 polyunsaturated fatty acids on six cognitive domains using randomized controlled trials
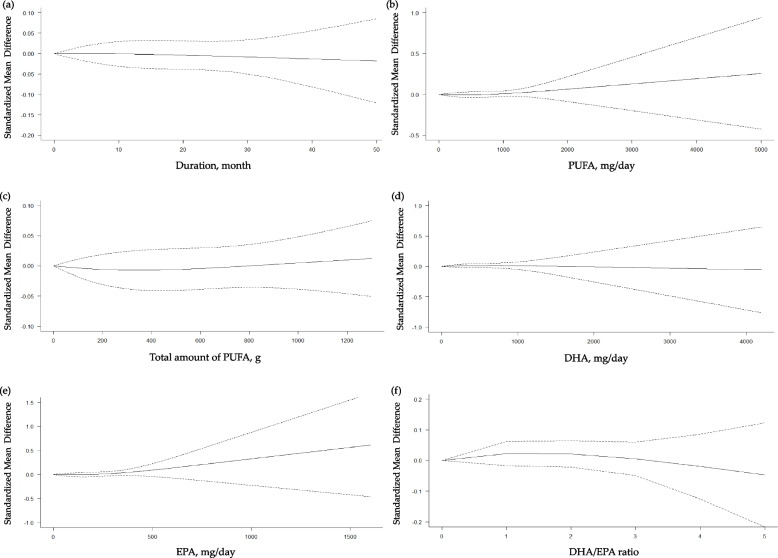
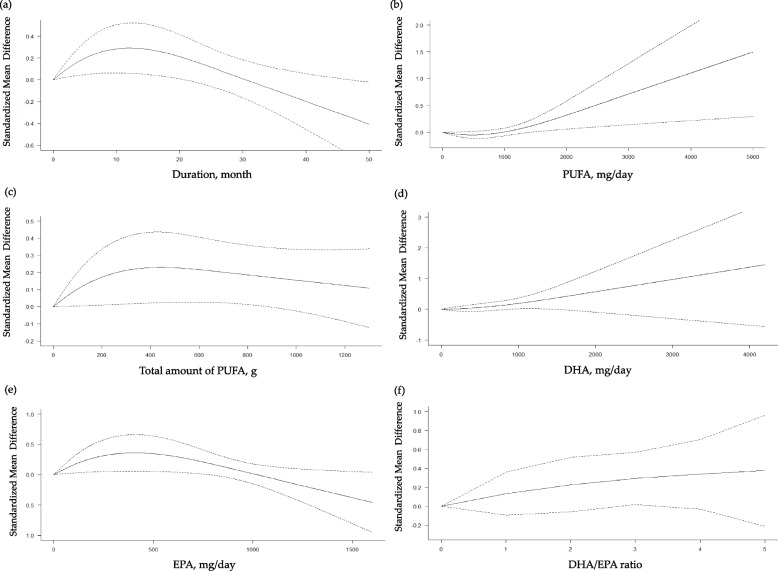
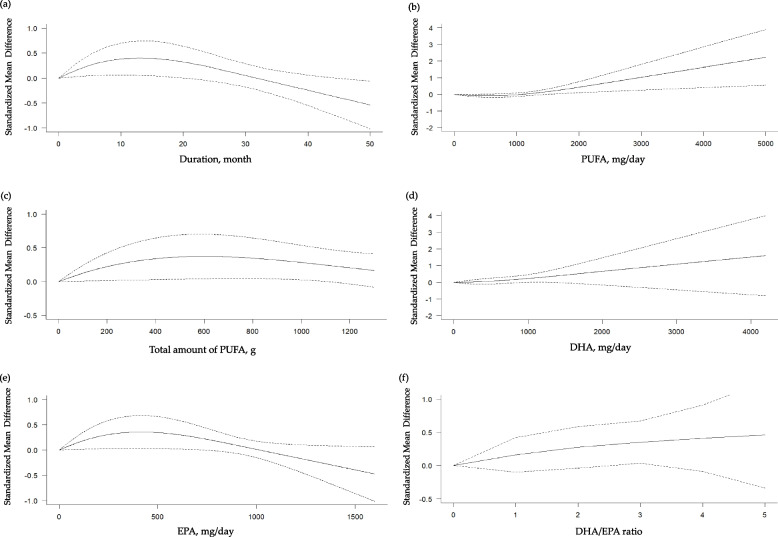
In the subsequent restricted cubic splines models, we did not find significant non-linear dose–response relationships in terms of the duration of intervention, daily and total dose of n-3 PUFA, daily dose of DHA or EPA and the ratio of DHA to EPA with the global cognition (Fig. 3), episodic memory (Additional file 1: Fig. S1), processing speed (Additional file 1: Fig. S2), attention (Additional file 1: Fig. S3), and visuospatial function (Additional file 1: Fig. S4). On the other hand, as shown in Fig. 4a, there was a increasing beneficial effect of n-3 PUFA on the executive function up to 12 months of intervention (coefficient [95% CI] = 0.0449 [0.0101, 0.0796], pcoefficient = 0.0114) with a significant negative curve afterwards (coefficient [95% CI] = − 0.1896 [− 0.3326, − 0.0465], pcoefficient = 0.0094; goodness of fit: χ2nonlinear = 6.941 versus χ2linear = 4.726; pnonlinearity = 0.031). We also found a significantly positive curve for the executive function after 500 mg/d of PUFA intake (coefficient [95% CI] = 0.0013 [0.0002, 0.0025], pcoefficient = 0.0249; goodness of fit: χ2nonlinear = 5.715 versus χ2linear = 3.492; pnonlinearity = 0.057) (Fig. 4b). In addition, there was an increasing beneficial effect on the executive function up to 420 mg/d of EPA (coefficient [95% CI] = 0.0017 [0.0003, 0.0031], pcoefficient = 0.0196) with a negative curve thereafter (coefficient [95% CI] = − 0.0077 [− 0.0143, − 0.0012], pcoefficient = 0.0209; goodness of fit: χ2nonlinear = 5.822 versus χ2linear = 3.819; pnonlinearity = 0.054) (Fig. 4e). Based on these findings, we determined to conduct subgroup analyses on the global cognition, our primary outcome, and the executive function which demonstrated significant nonlinear relationships.
Fig. 3.
Dose–response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the global cognition. a Duration of intervention; b daily intake of n-3 PUFA; c total amount of n-3 PUFA taken during the study period; d daily intake of docosahexaenoic acid (DHA); e daily intake of eicosapentaenoic acid (EPA); f ratio of DHA to EPA taken
Fig. 4.
Dose–response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the executive function. a Duration of intervention; b daily intake of n-3 PUFA; c total amount of n-3 PUFA taken during the study period; d daily intake of docosahexaenoic acid (DHA); e daily intake of eicosapentaenoic acid (EPA); f ratio of DHA to EPA taken
Subgroup analysis on the efficacy of n-3 PUFA by the populational blood level of DHA and EPA
In the countries where the blood level of DHA and EPA was very low, the beneficial effects of n-3 PUFA were not significant for the global cognition (Additional file 1: Fig. S5) and executive function (Additional file 1: Fig. S6).
However, in case of the countries where the blood level of DHA and EPA was not very low with > 4% in erythrocyte equivalents, an increasing beneficial effect on the executive function was observed up to 12 months of intervention (coefficient [95% CI] = 0.0621 [0.0138, 0.1105], pcoefficient = 0.0117) followed by a descending curve (coefficient [95% CI] = − 0.2918 [− 0.5123, − 0.0713], pcoefficient = 0.0095; goodness of fit: χ2nonlinear = 7.278 versus χ2linear = 4.950; pnonlinearity = 0.026;) (Fig. 5a). A significant ascending curve was also found for the executive function after 500 mg/d of PUFA intake (coefficient [95% CI] = 0.0016 [0.0003, 0.0029], pcoefficient = 0.0158; goodness of fit: χ2nonlinear = 6.854 versus χ2linear = 3.824; pnonlinearity = 0.033) (Fig. 5b). An incremental beneficial effect on the executive function was also observed up to 420 mg/d of EPA (coefficient [95% CI] = 0.0016 [0.0001, 0.0031], pcoefficient = 0.0323) with a negative curve thereafter (coefficient [95% CI] = − 0.0071 [− 0.0138, − 0.0005], pcoefficient = 0.0340; goodness of fit: χ2nonlinear = 4.584 versus χ2linear = 3.345; pnonlinearity = 0.101) (Fig. 5e). In regions where the level of n-3 PUFA is not very low, no substantial non-linear correlation was observed between the use of n-3 PUFA and global cognition (Additional file 1: Fig. S7).
Fig. 5.
Dose–response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the executive function based on the studies from countries where the blood level of docosahexaenoic acid (DHA) + eicosapentaenoic acid (EPA) is not very low. a Duration of intervention; b daily intake of n-3 PUFA; c total amount of n-3 PUFA taken during the study period; d daily intake of DHA; e daily intake of EPA; f ratio of DHA to EPA taken
Subgroup analysis on the efficacy of n-3 PUFA by the presence of MCI
As for trials composed only of people with MCI, we identified two studies [36, 47] that examined the global cognition, thus preventing us to conduct any meaningful meta-analysis. For those studies that analyzed executive function, we encountered an absence of statistically significant effects attributable to n-3 PUFA (Additional file 1: Fig. S8).
In the people with normal cognition, the beneficial effects of n-3 PUFA on global cognition and the executive function were not different by the duration of intervention, daily and total doses of n-3 PUFA, and daily doses of DHA and EPA (Additional file 1: Fig. S9 and Additional file 1: Fig. S10).
Sensitivity analyses and publication bias
When we eliminated one study at a time in a stepwise fashion, we did not observe any significant effect of an individual study on the overall estimates. However, we found that several trials have an influence on the statistical heterogeneity of the overall studies. Exclusion of the study by Bo et al. [45] led to a decrease in statistical heterogeneity concerning both global cognition and visuospatial function (Additional file 1: Table S4). Elimination of the studies by Lee et al. [46], Sinn et al. [48], and Howe et al. [57] correspondingly resulted in the reduction of statistical heterogeneity associated with episodic memory, executive function, and processing speed, respectively (Additional file 1: Table S4).
Egger’s test demonstrated that the degree of the funnel asymmetry was not significant in five random-effects models (between n-3 PUFA and the global cognition, p = 0.467; episodic memory, p = 0.226; executive function, p = 0.078; processing speed, p = 0.694; attention, p = 0.841) (Additional file 1: Fig. S11).
Discussion
To the best of our knowledge, this is the first dose–response meta-analysis examining the link between n-3 PUFA intake and cognitive function in non-demented individuals exclusively of middle age or older. This study found that the beneficial effect on executive function demonstrates an upward trend within the initial 12 months of intervention. This effect is prominently observed with a daily intake surpassing 500 mg of n-3 PUFA and up to 420 mg of EPA. We also identified a descending curve following 12 months of n-3 PUFA intervention, and when the dosage of EPA exceeded 420 mg/d. Furthermore, these trends exhibit heightened significance in regions where the levels of blood DHA + EPA are not very low.
Our finding regarding the beneficial effect on the executive function is in line with a recent dose–response meta-analysis [22] and previous cross-sectional studies that suggested higher fasting plasma DHA + EPA levels [61] were associated with better executive function in dementia-free elderly individuals. The cognitive advantages attributed to n-3 polyunsaturated fatty acids (PUFA) are believed to be mediated by their influence on synaptic plasticity and neurogenesis in brain regions susceptible to oxidative stress [62]. Intriguingly, in the healthy adult population, it has been posited that vulnerability to oxidation follows a caudal-cranial gradient, with the highest vulnerability in the frontal cortex and the lowest in the spinal cord [63]. Given that executive function is primarily associated with the frontal cortex, it could elucidate why supplementation with n-3 PUFA exclusively benefits executive function. Furthermore, some scholars have suggested that the positive impact on executive function may be mediated through a reduction in the cerebrovascular lesion [64].
We identified that the beneficial effect on the executive function was not apparent for the individuals from the countries where the blood DHA + EPA level was reportedly very low with ≤ 4% in erythrocytes equivalents. It has long been suggested that this blood level is well correspond to the dietary intakes of DHA + EPA [65], and showed a similar distribution to the data obtained by nutrition surveys [66]. Researchers contend that cognitive processes cannot be singularly attributed to the accumulation of n-3 PUFA in the neural membrane; rather, the activation of various genes by dietary n-3 PUFA and their resultant products may also play a crucial role in facilitating its beneficial effects [67]. These phenomena may take place as early as conception to perinatal period characterized by an inherently gradual progression [25]. Therefore, it is tempting to propose that a habitual, long-term exposure to the n-3 PUFA might be a prerequisite to expect any beneficial effect from a high dose intake of n-3 PUFA though, from these analyses, we were unable to confirm the isolated effect of life-long intake of n-3 PUFA on the cognitive function.
Our analyses also indicated that detrimental effects to the executive function might be possible when taking n-3 PUFA for longer than 12 months or EPA for more than 420 mg/d, respectively. Several previous studies indeed suggested that a high n-3 PUFA intake might actually be associated with a low-density lipoprotein (LDL)-cholesterol-raising effect [68, 69] or a decline in the platelet count [70, 71], though their evidence is controversial [72]. Further studies on the tolerable upper limit of daily intake of n-3 PUFA, especially EPA, are needed to clarify this issue.
The current recommended guidelines for adequate n-3 PUFA intake among the adult or elderly population propose a daily intake of DHA + EPA at levels specified as follows: 250 mg according to the European Food Safety Authority [73] and Poland [74], 450 mg in the Netherlands [75], 500 mg in France [76] and Switzerland [77], between 250 and 500 mg in Belgium [78], and between 250 and 2000 mg according to the Food and Agriculture Organization of the United Nations/World Health Organization [79]. Our investigation reveals that a majority of these guidelines employ certain criteria to formulate specific recommendations, primarily focusing on the mitigation of cardiovascular diseases or the prevention of clinical deficiencies. Should subsequent research validate our findings, we posit that our results could enhance existing recommendations by incorporating cognitive perspectives. Notably, a daily n-3 PUFA intake exceeding 500 mg may warrant consideration in the refinement of these guidelines.
There are several limitations that warrant comments. Firstly, multiple cognitive tests were utilized to represent a single cognitive domain. However, efforts were made to reduce this heterogeneity by prioritizing the most commonly used cognitive test for analysis. Conversely, certain cognitive tests were found to lack specificity for the designated cognitive domain. Nonetheless, the overall results demonstrated robustness even after reassigning the test to an alternative domain (data not shown). Secondly, in several instances, the intervention material of trials claiming to be focused on n-3 PUFA did not exclusively consist of it. Minor amounts of other components such as vitamins, protein, or minerals were also mixed in. To ensure the generalizability of our analyses, we opted to exclude only those studies explicitly stating the inclusion of B vitamins in the intervention material but not in the placebo, as these were reported to be linked with cognitive benefits in certain studies [80]. Thirdly, we observed that four studies [45, 46, 48, 57] have significantly contributed to the overall statistical heterogeneity. We postulated that the utilization of distinctive cognitive assessments, such as the Basic Cognitive Aptitude Test, Initial Letter Fluency Change, or Z scores, might have exacerbated the heterogeneity, though sensitivity analyses for each of these studies showed robustness.
Conclusions
In conclusion, supplementation of n-3 PUFA may offer potential advantages for executive function in the middle-aged and elderly population, particularly in individuals whose dietary DHA + EPA level is not substantially diminished.
Supplementary Information
Additional file 1: Table S1. Search strategies by data sources. Table S2. Cognitive tests employed in each trial by their corresponding cognitive domain. Table S3. Detailed description of the risk of bias (RoB) for the individual studies. Table S4. Sensitivity analyses for each of the six cognitive domains. Fig. S1. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the episodic memory. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S2. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the processing speed. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S3. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the attention. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S4. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the visuospatial function. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S5. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the global cognition based on the studies from countries where the blood level of DHA + EPA is very low. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S6. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the executive function based on the studies from countries where the blood level of DHA + EPA is very low. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S7. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the global cognition based on the studies from countries where the blood level of DHA + EPA is not very low. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S8. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the executive function of the people with mild cognitive impairment. (a) daily intake of n-3 PUFA; (b) total amount of n-3 PUFA taken during the study period; (c) daily intake of docosahexaenoic acid (DHA); (d) daily intake of eicosapentaenoic acid (EPA); (e) ratio of DHA to EPA taken. Fig. S9. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the global cognition of the cognitively normal individuals. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S10. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the executive function of the cognitively normal individuals. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S11. Funnel plots of meta-analyses between n-3 polyunsaturated fatty acids and the (a) global cognition, (b) episodic memory, (c) executive function, (d) processing speed, (e) attention, and (f) visuospatial function.
Acknowledgements
Not applicable.
Abbreviations
- ALA
Alpha linolenic acid
- BDNF
Brain-derived neurotrophic factor
- CI
Confidence interval
- DHA
Docosa hexaenoic acid
- EPA
Eicosa pentaenoic acid
- LDL
Low-density lipoprotein
- MCI
Mild cognitive impairment
- MMSE
Mini-Mental Status Examination
- N-3 PUFA
Omega 3 polyunsaturated fatty acids
- RAVLT
Rey Auditory Verbal Learning Test
- RoB
Risk of bias
- SD
Standard deviation
- SMD
Standardized mean difference
- TMT-A
Trail making test A
Authors’ contributions
SWS, EL, JBB, JWH, and KWK conceived and designed this study. SWS, EL, SYB, and HL conducted the study selection and data extraction. SWS conducted the statistical analyses and participated in the interpretation of the data, SWS and EL drafted the manuscript. All authors critically reviewed the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by a funding from the Research and Publication Projects of Ottogi Ham Taiho Foundation, Seoul, Republic of Korea, and the Korea Dementia Research Project through the Korea Dementia Research Center (KDRC), funded by the Ministry of Health & Welfare and Ministry of Science and ICT, Republic of Korea (grant number: HU20C0015). Dr. Ej Lim, Dr. Bae, Dr. Han, and Dr. Kim have received research support by a grant from the Korean Health Technology Research and Development Project of the Ministry of Health, Welfare, and Family Affairs, Republic of Korea (grant number A092077).
Availability of data and materials
The datasets utilized and/or analyzed throughout the present study are obtainable from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Seung Wan Suh and Eunji Lim contributed equally to this work.
References
- 1.Bang H, Dyerberg J, Nielsen AB. Plasma lipid and lipoprotein pattern in Greenlandic West-coast Eskimos. Lancet. 1971;297:1143–1146. doi: 10.1016/S0140-6736(71)91658-8. [DOI] [PubMed] [Google Scholar]
- 2.Kyle D, Schaefer E, Patton G, Beiser A. Low serum docosahexaenoic acid is a significant risk factor for Alzheimer's dementia. Lipids. 1999;34:S245. doi: 10.1007/BF02562306. [DOI] [PubMed] [Google Scholar]
- 3.Barberger-Gateau P, Letenneur L, Deschamps V, Pérès K, Dartigues J-F, Renaud S. Fish, meat, and risk of dementia: cohort study. BMJ. 2002;325:932–933. doi: 10.1136/bmj.325.7370.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris MC, Evans DA, Tangney CC, Bienias JL, Wilson RS. Fish consumption and cognitive decline with age in a large community study. Arch Neurol. 2005;62:1849–1853. doi: 10.1001/archneur.62.12.noc50161. [DOI] [PubMed] [Google Scholar]
- 5.Saini RK, Keum Y-S. Omega-3 and omega-6 polyunsaturated fatty acids: Dietary sources, metabolism, and significance—A review. Life Sci. 2018;203:255–267. doi: 10.1016/j.lfs.2018.04.049. [DOI] [PubMed] [Google Scholar]
- 6.Teng E, Taylor K, Bilousova T, Weiland D, Pham T, Zuo X, et al. Dietary DHA supplementation in an APP/PS1 transgenic rat model of AD reduces behavioral and Aβ pathology and modulates Aβ oligomerization. Neurobiol Dis. 2015;82:552–560. doi: 10.1016/j.nbd.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hjorth E, Zhu M, Toro VC, Vedin I, Palmblad J, Cederholm T, et al. Omega-3 fatty acids enhance phagocytosis of alzheimer's disease-related amyloid-β 42 by human microglia and decrease inflammatory markers. J Alzheimers Dis. 2013;35:697–713. doi: 10.3233/JAD-130131. [DOI] [PubMed] [Google Scholar]
- 8.Zhang X, Han H, Ge X, Liu L, Wang T, Yu H. Effect of n-3 long-chain polyunsaturated fatty acids on mild cognitive impairment: a meta-analysis of randomized clinical trials. Eur J Clin Nutr. 2020;74:548–554. doi: 10.1038/s41430-019-0544-4. [DOI] [PubMed] [Google Scholar]
- 9.Alex A, Abbott KA, McEvoy M, Schofield PW, Garg ML. Long-chain omega-3 polyunsaturated fatty acids and cognitive decline in non-demented adults: a systematic review and meta-analysis. Nutr Rev. 2020;78:563–578. doi: 10.1093/nutrit/nuz073. [DOI] [PubMed] [Google Scholar]
- 10.Brainard JS, Jimoh OF, Deane KH, Biswas P, Donaldson D, Maas K, et al. Omega-3, Omega-6, and polyunsaturated fat for cognition: systematic review and meta-analysis of randomized Trials. J Am Med Dir Assoc. 2020;21:1439–50. doi: 10.1016/j.jamda.2020.02.022. [DOI] [PubMed] [Google Scholar]
- 11.Giles GE, Mahoney CR, Urry HL, Brunyé TT, Taylor HA, Kanarek RB. Omega-3 fatty acids and stress-induced changes to mood and cognition in healthy individuals. Pharmacol Biochem Behav. 2015;132:10–19. doi: 10.1016/j.pbb.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 12.Jackson PA, Deary ME, Reay JL, Scholey AB, Kennedy DO. No effect of 12 weeks' supplementation with 1 g DHA-rich or EPA-rich fish oil on cognitive function or mood in healthy young adults aged 18–35 years. Br J Nutr. 2012;107:1232–1243. doi: 10.1017/S000711451100403X. [DOI] [PubMed] [Google Scholar]
- 13.McCaddon A, Miller JW. Assessing the association between homocysteine and cognition: reflections on Bradford Hill, meta-analyses, and causality. Nutr Rev. 2015;73:723–735. doi: 10.1093/nutrit/nuv022. [DOI] [PubMed] [Google Scholar]
- 14.Rutjes AW, Denton DA, Di Nisio M, Chong LY, Abraham RP, Al-Assaf AS, et al. Vitamin and mineral supplementation for maintaining cognitive function in cognitively healthy people in mid and late life. Cochrane Database Syst Rev. 2018;12:CD011906. doi: 10.1002/14651858.CD011906.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salthouse TA. When does age-related cognitive decline begin? Neurobiol Aging. 2009;30:507–514. doi: 10.1016/j.neurobiolaging.2008.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund LO, et al. Mild cognitive impairment–beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Int Med. 2004;256:240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- 17.Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29:1037–1057. doi: 10.1002/sim.3841. [DOI] [PubMed] [Google Scholar]
- 18.Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332:1080. doi: 10.1136/bmj.332.7549.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greenland S. Avoiding power loss associated with categorization and ordinal scores in dose-response and trend analysis. Epidemiol. 1995;6:450–454. doi: 10.1097/00001648-199507000-00025. [DOI] [PubMed] [Google Scholar]
- 20.Greenland S. Dose-response and trend analysis in epidemiology: alternatives to categorical analysis. Epidemiol. 1995;6:356–365. doi: 10.1097/00001648-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Govindarajulu US, Spiegelman D, Thurston SW, Ganguli B, Eisen EA. Comparing smoothing techniques in Cox models for exposure–response relationships. Stat Med. 2007;26:3735–3752. doi: 10.1002/sim.2848. [DOI] [PubMed] [Google Scholar]
- 22.Kosti RI, Kasdagli MI, Kyrozis A, Orsini N, Lagiou P, Taiganidou F, et al. Fish intake, n-3 fatty acid body status, and risk of cognitive decline: a systematic review and a dose–response meta-analysis of observational and experimental studies. Nutr Res Rev. 2022;80:1445–1458. doi: 10.1093/nutrit/nuab078. [DOI] [PubMed] [Google Scholar]
- 23.Zeng L-F, Cao Y, Liang W-X, Bao W-H, Pan J-K, Wang Q, et al. An exploration of the role of a fish-oriented diet in cognitive decline: a systematic review of the literature. Oncotarget. 2017;8:39877–39895. doi: 10.18632/oncotarget.16347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang Y, Chen J, Qiu J, Li Y, Wang J, Jiao J. Intakes of fish and polyunsaturated fatty acids and mild-to-severe cognitive impairment risks: a dose-response meta-analysis of 21 cohort studies–3. Am J Clin Nutr. 2015;103:330–340. doi: 10.3945/ajcn.115.124081. [DOI] [PubMed] [Google Scholar]
- 25.Joffre C, Nadjar A, Lebbadi M, Calon F, Laye S. n-3 LCPUFA improves cognition: the young, the old and the sick. Prostaglandins Leukot Essent Fatty Acids. 2014;91:1–20. doi: 10.1016/j.plefa.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175:66–73. doi: 10.1093/aje/kwr265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;151:264–69. [PMC free article] [PubMed] [Google Scholar]
- 28.Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. J Educ Stat. 1981;6:107–128. doi: 10.3102/10769986006002107. [DOI] [Google Scholar]
- 29.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. 2. Oxford: Blackwell Science; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCleery J, Abraham RP, Denton DA, Rutjes AW, Chong LY, Al-Assaf AS, et al. Vitamin and mineral supplementation for preventing dementia or delaying cognitive decline in people with mild cognitive impairment. Cochrane Database Syst Rev. 2018;11:CD011905. doi: 10.1002/14651858.CD011905.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 32.Orsini N. Weighted mixed-effects dose–response models for tables of correlated contrasts. Stata J. 2021;21:320–347. doi: 10.1177/1536867X211025798. [DOI] [Google Scholar]
- 33.Shim SR, Lee J. Dose-response meta-analysis: application and practice using the R software. Epidemiol Health. 2019;41:e2019006. doi: 10.4178/epih.e2019006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135:1301–1309. doi: 10.1093/oxfordjournals.aje.a116237. [DOI] [PubMed] [Google Scholar]
- 35.Stark KD, Van Elswyk ME, Higgins MR, Weatherford CA, Salem N., Jr Global survey of the omega-3 fatty acids, docosahexaenoic acid and eicosapentaenoic acid in the blood stream of healthy adults. Prog Lipid Res. 2016;63:132–152. doi: 10.1016/j.plipres.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 36.Arellanes IC, Choe N, Solomon V, He X, Kavin B, Martinez AE, et al. Brain delivery of supplemental docosahexaenoic acid (DHA): a randomized placebo-controlled clinical trial. EBioMedicine. 2020;59:102883. doi: 10.1016/j.ebiom.2020.102883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hashimoto M, Matsuzaki K, Hossain S, Ito T, Wakatsuki H, Tanabe Y, et al. Perilla seed oil enhances cognitive function and mental health in healthy elderly Japanese individuals by enhancing the biological antioxidant potential. Foods. 2021;10:1130. doi: 10.3390/foods10051130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ichinose T, Matsuzaki K, Kato M, Tanabe Y, Tachibana N, Morikawa M, et al. Intake of docosahexaenoic acid-enriched milk beverage prevents age-related cognitive decline and decreases serum bone resorption marker levels. J Oleo Sci. 2021;70:1829–1838. doi: 10.5650/jos.ess21195. [DOI] [PubMed] [Google Scholar]
- 39.Ogawa T, Sawane K, Ookoshi K, Kawashima R. Supplementation with flaxseed oil rich in alpha-linolenic acid improves verbal fluency in healthy older adults. Nutrients. 2023;15:1499. doi: 10.3390/nu15061499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Power R, Nolan JM, Prado-Cabrero A, Roche W, Coen R, Power T, et al. Omega-3 fatty acid, carotenoid and vitamin E supplementation improves working memory in older adults: a randomised clinical trial. Clin Nutr. 2022;41:405–414. doi: 10.1016/j.clnu.2021.12.004. [DOI] [PubMed] [Google Scholar]
- 41.Sala-Vila A, Arenaza-Urquijo EM, Sánchez-Benavides G, Suárez-Calvet M, Milà-Alomà M, Grau-Rivera O, et al. DHA intake relates to better cerebrovascular and neurodegeneration neuroimaging phenotypes in middle-aged adults at increased genetic risk of Alzheimer disease. Am J Clin Nutr. 2021;113:1627–1635. doi: 10.1093/ajcn/nqab016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tokuda H, Ito M, Sueyasu T, Sasaki H, Morita S, Kaneda Y, et al. Effects of combining exercise with long-chain polyunsaturated fatty acid supplementation on cognitive function in the elderly: a randomised controlled trial. Sci Rep. 2020;10:1–12. doi: 10.1038/s41598-020-69560-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Valls-Pedret C, Sala-Vila A, Serra-Mir M, Corella D, De la Torre R, Martínez-González MÁ, et al. Mediterranean diet and age-related cognitive decline: a randomized clinical trial. JAMA Intern Med. 2015;175:1094–1103. doi: 10.1001/jamainternmed.2015.1668. [DOI] [PubMed] [Google Scholar]
- 44.Yurko-Mauro K, McCarthy D, Rom D, Nelson EB, Ryan AS, Blackwell A, et al. Beneficial effects of docosahexaenoic acid on cognition in age-related cognitive decline. Alzheimers Dement. 2010;6:456–464. doi: 10.1016/j.jalz.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 45.Bo Y, Zhang X, Wang Y, You J, Cui H, Zhu Y, et al. The n-3 polyunsaturated fatty acids supplementation improved the cognitive function in the Chinese elderly with mild cognitive impairment: a double-blind randomized controlled trial. Nutrients. 2017;9:54. doi: 10.3390/nu9010054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee LK, Shahar S, Chin A-V, Yusoff NAM. Docosahexaenoic acid-concentrated fish oil supplementation in subjects with mild cognitive impairment (MCI): a 12-month randomised, double-blind, placebo-controlled trial. Psychopharmacol. 2013;225:605–612. doi: 10.1007/s00213-012-2848-0. [DOI] [PubMed] [Google Scholar]
- 47.Mengelberg A, Leathem J, Podd J, Hill S, Conlon C. The effects of docosahexaenoic acid supplementation on cognition and well-being in mild cognitive impairment: A 12-month randomised controlled trial. Int J Geriatr Psychiatry. 2022;37:5707. doi: 10.1002/gps.5707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sinn N, Milte CM, Street SJ, Buckley JD, Coates AM, Petkov J, et al. Effects of n-3 fatty acids, EPA v. DHA, on depressive symptoms, quality of life, memory and executive function in older adults with mild cognitive impairment: a 6-month randomised controlled trial. Br J Nutr. 2012;107:1682–93. doi: 10.1017/S0007114511004788. [DOI] [PubMed] [Google Scholar]
- 49.Hashimoto M, Kato S, Tanabe Y, Katakura M, Mamun AA, Ohno M, et al. Beneficial effects of dietary docosahexaenoic acid intervention on cognitive function and mental health of the oldest elderly in Japanese care facilities and nursing homes. Geriatr Gerontol Int. 2016;17:330–337. doi: 10.1111/ggi.12691. [DOI] [PubMed] [Google Scholar]
- 50.Sala-Vila A, Valls-Pedret C, Rajaram S, Coll-Padrós N, Cofán M, Serra-Mir M, et al. Effect of a 2-year diet intervention with walnuts on cognitive decline. The Walnuts And Healthy Aging (WAHA) study: a randomized controlled trial. Am J Clin Nutr. 2020;111:590–600. doi: 10.1093/ajcn/nqz328. [DOI] [PubMed] [Google Scholar]
- 51.Chew EY, Clemons TE, Agrón E, Launer LJ, Grodstein F, Bernstein PS. Effect of omega-3 fatty acids, lutein/zeaxanthin, or other nutrient supplementation on cognitive function: the AREDS2 randomized clinical trial. JAMA. 2015;314:791–801. doi: 10.1001/jama.2015.9677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dangour AD, Allen E, Elbourne D, Fasey N, Fletcher AE, Hardy P, et al. Effect of 2-yn− 3 long-chain polyunsaturated fatty acid supplementation on cognitive function in older people: a randomized, double-blind, controlled trial. Am J Clin Nutr. 2010;91:1725–1732. doi: 10.3945/ajcn.2009.29121. [DOI] [PubMed] [Google Scholar]
- 53.Andrieu S, Guyonnet S, Coley N, Cantet C, Bonnefoy M, Bordes S, et al. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): a randomised, placebo-controlled trial. Lancet Neurol. 2017;16:377–389. doi: 10.1016/S1474-4422(17)30040-6. [DOI] [PubMed] [Google Scholar]
- 54.Bischoff-Ferrari HA, Vellas B, Rizzoli R, Kressig RW, da Silva JA, Blauth M, et al. Effect of vitamin d supplementation, omega-3 fatty acid supplementation, or a strength-training exercise program on clinical outcomes in older adults: The DO-HEALTH Randomized Clinical Trial. JAMA. 2020;324:1855–1868. doi: 10.1001/jama.2020.16909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Daďová K, Petr M, Tufano JJ, Sontáková L, Krauzová E, Štěpán M, et al. Calanus oil supplementation does not further improve short-term memory or brain-derived neurotrophic factor in older women who underwent exercise training. Clin Interv Aging. 2022;17:1227–36. doi: 10.2147/CIA.S368079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Geleijnse JM, Giltay EJ, Kromhout D. Effects of n-3 fatty acids on cognitive decline: a randomized, double-blind, placebo-controlled trial in stable myocardial infarction patients. Alzheimers Dement. 2012;8:278–287. doi: 10.1016/j.jalz.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 57.Howe PR, Evans HM, Kuszewski JC, Wong RH. Effects of long chain omega-3 polyunsaturated fatty acids on brain function in mildly hypertensive older adults. Nutrients. 2018;10:1413. doi: 10.3390/nu10101413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kuszewski JC, Howe PR, Wong RH. Evaluation of cognitive performance following fish-oil and curcumin supplementation in middle-aged and older adults with overweight or obesity. J Nutr. 2020;150:3190–3199. doi: 10.1093/jn/nxaa299. [DOI] [PubMed] [Google Scholar]
- 59.Macpherson H, Brownell S, Harris E, Duckham RL, O’Connell S, Meyer BJ, et al. Effects of a 6-Month Multifaceted Diet and Exercise Intervention on Cognition in Older Adults at Risk of Cognitive Decline: The PONDER Double-Blind, Placebo-Controlled Randomized Trial. J Alzheimers Dis. 2022;89:247–263. doi: 10.3233/JAD-220234. [DOI] [PubMed] [Google Scholar]
- 60.van de Rest O, Geleijnse JM, Kok FJ, van Staveren WA, Dullemeijer C, OldeRikkert MG, et al. Effect of fish oil on cognitive performance in older subjects: a randomized, controlled trial. Neurol. 2008;71:430–438. doi: 10.1212/01.wnl.0000324268.45138.86. [DOI] [PubMed] [Google Scholar]
- 61.Bowman GL, Silbert L, Howieson D, Dodge H, Traber M, Frei B, et al. Nutrient biomarker patterns, cognitive function, and MRI measures of brain aging. Neurol. 2012;78:241–249. doi: 10.1212/WNL.0b013e3182436598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Crupi R, Marino A, Cuzzocrea S. n-3 fatty acids: role in neurogenesis and neuroplasticity. Curr Med Chem. 2013;20:2953–2963. doi: 10.2174/09298673113209990140. [DOI] [PubMed] [Google Scholar]
- 63.Naudí A, Cabré R, Dominguez-Gonzalez M, Ayala V, Jové M, Mota-Martorell N, et al. Region-specific vulnerability to lipid peroxidation and evidence of neuronal mechanisms for polyunsaturated fatty acid biosynthesis in the healthy adult human central nervous system. Biochim Biophys Acta Mol Cell Biol Lipids. 2017;1862:485–495. doi: 10.1016/j.bbalip.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 64.Shinto L, Lahna D, Murchison CF, Dodge H, Hagen K, David J, et al. Oxidized products of omega-6 and omega-3 long chain fatty acids are associated with increased white matter hyperintensity and poorer executive function performance in a cohort of cognitively normal hypertensive older adults. J Alzheimers Dis. 2020;74:65–77. doi: 10.3233/JAD-191197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Metherel A, Armstrong J, Patterson A, Stark K. Assessment of blood measures of n-3 polyunsaturated fatty acids with acute fish oil supplementation and washout in men and women. Prostaglandins Leukot Essent Fatty Acids. 2009;81:23–29. doi: 10.1016/j.plefa.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 66.Micha R, Khatibzadeh S, Shi P, Fahimi S, Lim S, Andrews KG, et al. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys. BMJ. 2014;348:g2272. doi: 10.1136/bmj.g2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kitajka K, Puskás LG, Zvara Á, Hackler L, Barceló-Coblijn G, Yeo YK, et al. The role of n-3 polyunsaturated fatty acids in brain: modulation of rat brain gene expression by dietary n-3 fatty acids. Proc Natl Acad Sci. 2002;99:2619–2624. doi: 10.1073/pnas.042698699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fumeron F, Brigant L, Ollivier V, De Prost D, Driss F, Darcet P, et al. n− 3 Polyunsaturated fatty acids raise low-density lipoproteins, high-density lipoprotein 2, and plasminogen-activator inhibitor in healthy young men. Am J Clin Nutr. 1991;54:118–122. doi: 10.1093/ajcn/54.1.118. [DOI] [PubMed] [Google Scholar]
- 69.Harris WS. Fish oils and plasma lipid and lipoprotein metabolism in humans: a critical review. J Lipid Res. 1989;30:785–807. doi: 10.1016/S0022-2275(20)38310-3. [DOI] [PubMed] [Google Scholar]
- 70.Goodnight SH, Jr, Harris WS, Connor WE, Illingworth D. Polyunsaturated fatty acids, hyperlipidemia, and thrombosis. Arteriosclerosis. 1982;2:87–113. doi: 10.1161/01.ATV.2.2.87. [DOI] [PubMed] [Google Scholar]
- 71.Dyerberg J, Bang H. Haemostatic function and platelet polyunsaturated fatty acids in Eskimos. Lancet. 1979;314:433–435. doi: 10.1016/S0140-6736(79)91490-9. [DOI] [PubMed] [Google Scholar]
- 72.Eritsland J. Safety considerations of polyunsaturated fatty acids. Am J Clin Nutr. 2000;71(Suppl):197–201. doi: 10.1093/ajcn/71.1.197S. [DOI] [PubMed] [Google Scholar]
- 73.EFSA Panel on Dietetic Products N, Allergies Scientific opinion on dietary reference values for fats, including saturated fatty acids, polyunsaturated fatty acids, monounsaturated fatty acids, trans fatty acids, and cholesterol. EFSA J. 2010;8:1461. [Google Scholar]
- 74.Dobrzańska A, Charzewska J, Weker H, Socha P, Mojska H, Książyk J, et al. Normy żywienia zdrowych dzieci w 1.–3. roku życia–stanowisko Polskiej Grupy Ekspertów. Część II–Omówienie poszczególnych składników odżywczych. Pediatr Pol. 2013;88:97–102. doi: 10.1016/j.pepo.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 75.Westerterp-Plantenga W, IJedema M, Wijckmans-Duijsens N. 78 Dietary reference intakes: energy, proteins, fats, and digestible carbohydrates. Dietary Ref Intakes. 2001;70:78. [Google Scholar]
- 76.Agence nationale de sécurité sanitaire de l'alimentation dleedt . Actualisation des apports nutritionnels conseillés pour les acides gras: rapport d'expertise collective: anses. 2011. [Google Scholar]
- 77.Bundesamt für Gesundheit. Fette in der Ernährung-Aktualisierte Empfehlungen der Eidgenössischen Ernährungskommission. Suppl. zum Expert. Fette der Ernährung mit den Aktual. Empfehlungen. Zürich: Eidgenössische Ernährungskommission; 2012. https://www.blv.admin.ch/dam/blv/de/dokumente/das-blv/organisation/kommissionen/eek/fette-in-der-ernaehrung-2013/empfehlung-fette-ernaehrung.pdf.download.pdf/3_EEK_Revision_Fettempfehlungen_2012_FINAL_D.pdf.
- 78.Sioen I, van Lieshout L, Eilander A, Fleith M, Lohner S, Szommer A, et al. Systematic review on n-3 and n-6 polyunsaturated fatty acid intake in European countries in light of the current recommendations-Focus on specific population groups. Ann Nutr Metab. 2017;70:39–50. doi: 10.1159/000456723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.FAO J . Fats and fatty acids in human nutrition. Report of an expert consultation. 2010. [PubMed] [Google Scholar]
- 80.Suh SW, Kim HS, Han JH, Bae JB, Oh DJ, Han JW, et al. Efficacy of vitamins on cognitive function of non-demented people: a systematic review and meta-analysis. Nutrients. 2020;12:1168. doi: 10.3390/nu12041168. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Search strategies by data sources. Table S2. Cognitive tests employed in each trial by their corresponding cognitive domain. Table S3. Detailed description of the risk of bias (RoB) for the individual studies. Table S4. Sensitivity analyses for each of the six cognitive domains. Fig. S1. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the episodic memory. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S2. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the processing speed. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S3. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the attention. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S4. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the visuospatial function. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S5. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the global cognition based on the studies from countries where the blood level of DHA + EPA is very low. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S6. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the executive function based on the studies from countries where the blood level of DHA + EPA is very low. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S7. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the global cognition based on the studies from countries where the blood level of DHA + EPA is not very low. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S8. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the executive function of the people with mild cognitive impairment. (a) daily intake of n-3 PUFA; (b) total amount of n-3 PUFA taken during the study period; (c) daily intake of docosahexaenoic acid (DHA); (d) daily intake of eicosapentaenoic acid (EPA); (e) ratio of DHA to EPA taken. Fig. S9. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the global cognition of the cognitively normal individuals. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S10. Dose-response meta-analyses for the association between n-3 polyunsaturated fatty acids (PUFA) and the executive function of the cognitively normal individuals. (a) duration of intervention; (b) daily intake of n-3 PUFA; (c) total amount of n-3 PUFA taken during the study period; (d) daily intake of docosahexaenoic acid (DHA); (e) daily intake of eicosapentaenoic acid (EPA); (f) ratio of DHA to EPA taken. Fig. S11. Funnel plots of meta-analyses between n-3 polyunsaturated fatty acids and the (a) global cognition, (b) episodic memory, (c) executive function, (d) processing speed, (e) attention, and (f) visuospatial function.
Data Availability Statement
The datasets utilized and/or analyzed throughout the present study are obtainable from the corresponding author upon reasonable request.