Abstract
Purpose
The purpose of this study was to record the utilization of medicinal plants by the Oromo people in the Kofale District, Oromia Regional State, Ethiopia, to control human and animal health problems.
Methods
Data regarding the use of medicinal plants were collected using ethnobotanical methods from 84 traditional medicine practitioners and 304 general informants sampled employing purposive and systematic random sampling methods, respectively, in the Kofale District. Data were analyzed using different indices, including a preference ranking exercise, informant consensus factor (ICF), fidelity level (FL) and relative popularity level (RPL).
Results
In the district, 106 medicinal plants were claimed to be used for the treatment of 43 human and 18 livestock illnesses, of which 75 (71%) were used to manage human health problems, 23 (21.5%) were used to treat both human and livestock ailments and eight (7.5%) were utilized to treat manage livestock health problems. Most (76.4%) plants were harvested from the wild. Leaves were the most commonly used plant part (55.6%) in remedy preparations. Skin diseases scored the highest ICF value (0.97), followed by gastrointestinal disorders (ICF = 0.95), cancer (ICF = 0.93), and hemorrhoids (ICF = 0.91). Medicinal plants that record the highest fidelity level (FL) (100%) and rank order priority (ROP) (100%) values included Justicia schimperiana, Embelia schimperi, Ekebergia capensis and Datura stramonium, which have been used to treat liver disorders, tapeworm infections, babesiosis, and rabies, respectively. There were significant differences (p<0.05) in the mean numbers of medicinal plants claimed by different social groups: older, illiterate, and traditional medicine practitioners reported higher mean numbers of medicinal plants than younger, literate, and general informants, respectively.
Conclusion
This study indicated the richness of medicinal plant species in Kofale District. Medicinal plants with the highest FL and ROP values and those used to treat disease categories with the highest ICF values should be prioritized in future phytochemical and pharmacological investigations.
Keywords: ethnobotanical study, traditional medicine, traditional knowledge, herbal medicine practitioners
Introduction
World Health Organization (WHO) has reported that nearly 60% of people worldwide, and as far as 80% of the population in Africa, directly or indirectly, depend on traditional medicinal plants to solve their healthcare problem.1 The high reliance on medicinal plants is attributed to a number of claimed reasons that include easy accessibility, cultural acceptability, affordability (cheaper cost), fewer side effects,2 and the widespread availability of harmful pathogenic microorganisms that are resistant to existing modern drugs.3 Medicinal plants are valuable sources for the discovery of new therapeutics against different diseases,4 which may also have a wider therapeutic window than synthetic drugs, and thus prevent the development of drug resistance. Medicinal plants contain a diverse groups of phytochemical constituents such as flavonoids, triterpenoids, glycosides, saponins, carotenoids, volatile oils, amino acids, steroids, quinines, alkaloids5 and coumarins6 responsible for multifaceted biological effects.7 According to estimates, around 80% of the human population and 90% of the livestock population in Ethiopia rely on traditional medicinal plants for their day-to-day primary healthcare.8,9 Ethiopia is one of the most ethnically diverse countries in East Africa with the majority of its citizens living in rural areas and thus with limited access to modern healthcare services.10 Such condition has made the people blessed with rich traditional knowledge and practices on the use of medicinal plants, remedy preparations and administrations as well as illness diagnoses.8 Even though the majority of the populations in Ethiopia heavily depend on medicinal plants for their primary healthcare needs, very limited work has so far been done to record and analyze the associated knowledge, and validate the therapeutic values of the claimed plants.11,12 On the other hand, there is an ongoing rapid population increase, indiscriminate deforestation, overexploitation of natural resources, worldwide climate change, which has contributed to the depletion of useful medicinal plant resources and the associated indigenous knowledge.13 As a result, documenting and protecting medicinal plants and the associated knowledge is becoming a greater priority. A number of ethnobotanical studies conducted in different parts of Ethiopia have reported the common uses of medicinal and wild edible plants.12,14–27 However, only a few ethnobotanical studies have been conducted in the West-Arsi Zone of the Oromia Regional State Ethiopia28,29 which were conducted in the Negele Arsi and Nansebo districts, and no such study has been conducted in Kofale District. Like most Ethiopian communities, people in Kofale District are expected to practice traditional medicine, mainly associated with the use of medicinal plants to maintain their health, as well as that of their domestic animals. Therefore, this study was carried out to properly document traditional knowledge related to the use of medicinal plants to manage both human and livestock ailments by the people of the Kofale District, West-Arsi Zone, Oromia Regional State, Ethiopia.
Materials and Methods
Description of the Study Area
According to 2007 census conducted by the Population Census Commission (PCC) of Ethiopia, the West-Arsi Zone has a total population of 1,975,295.30 Most inhabitants in the zone belong to the Oromo ethnic group, constituting 88.52% of the total population. The Zone has 12 districts, one of which is Kofale District (Figure 1). Kofale District is geographically located between 6° 50ˈ-7° 9ˈN and 38° 38ˈ-39° 4ˈE, south of the capital Addis Ababa. According to Kofale District Healthcare Office (KDHCO), the district gets a mean annual rainfall of 1300 mm and a temperature of 10–24°C (KDHCO, 2022, unpublished data). The district has a total population of 179,508, of which 90,000 are men and 89,508 are women.30 People in the rural areas of the study district are mainly dependent on crop farming and livestock production for their livelihood. According to the Kofale District Agricultural Office (KDAO), there are 106,325 cattle heads, 112,570 sheep, 91,400 horses, 9784 goats, 9410 donkeys, and 35,901 chickens in the district (KDAO 2022, unpublished data). Based on data collected during a reconnaissance survey, the district has 43 kebeles (sub-districts) located at different distances from the administrative district center (Kofale town). The top-five human health problems in the district are dermatochalasis, gastrointestinal tract infections (diarrhea, typhoid, stomachache, abdominal pain, and internal parasite infestation), cancer, respiratory infections, and sexually transmitted diseases (KDHCO 2022, unpublished data), and the main livestock diseases in the study area include anthrax, black leg, pasteurellosis, dermatochalasis, tick infestations, equine glanders, leech infestation, and rabies (KDAO 2022, unpublished data).
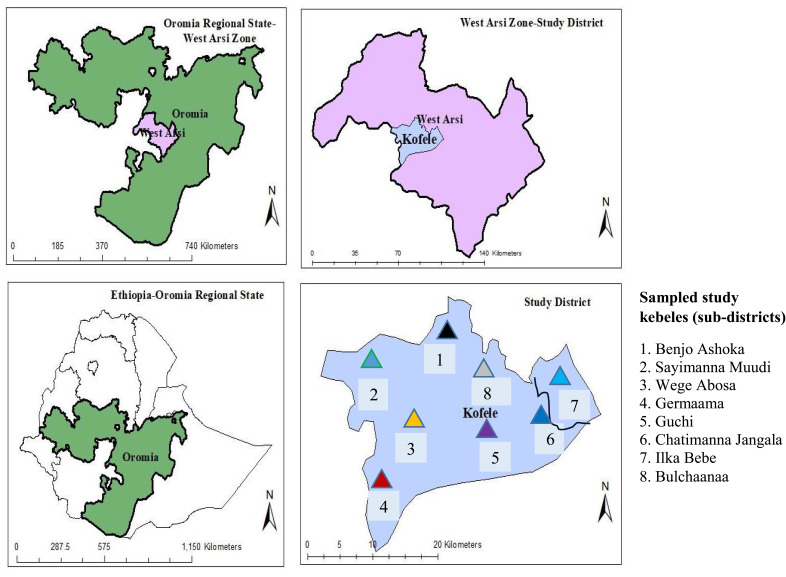
Figure 1.
Map of Kofale District, West-Arsi Zone, Oromia Regional State, Ethiopia.
Selection of Study Sites
A reconnaissance survey was conducted in Kofale District in January and February 2021 to select study kebeles and informants. Health and agricultural professionals in the district played key roles in the identification of herbal medicine practitioners. Of the 43 kebeles in the district, eight (Wege Abosa, Benjo Ashoka, Ilka Bebe, Sayimanna muudi, Chatimanna Jangala, Guchi, Bulchaana, and Garmaama) were purposively selected for the study, taking into consideration the history of use of traditional medicine and availability of practitioners in the area, less exposure of the community to modernization, and agro-ecological representation. Additional information regarding the sampled kebeles and traditional healers was gathered from kebele administration officers, knowledgeable elders, and other local inhabitants.
Study Design, Sample Size Determination and Sampling Techniques
A cross-sectional study design was adopted to conduct the ethnobotanical survey, and sample size was determined based on the total of household heads in the sampled kebeles30 using a standard sample size determination formula given below.31
n = N/(1+N(e)2), where n = sample size, N = total number of households in sample villages/kebeles (11,754), e = maximum variability or margin of error 5% (0.05) and 1 = the probability of event occurring
Based on this, the total sample size obtained was 388, of which 84 were locally recognized traditional health practitioners (THP) who were identified using purposive sampling method, and 304 were general informants that were sampled using a systematic random sampling method as described by Martin28 based on the total number of households each kebele (Table 1).
Table 1.
Number of Households and Informants in Each Sampled Kebele
| Kebeles | Altitude | Number of Households | Number of Informants | General Informants | Traditional Health Practitioners | ||||
|---|---|---|---|---|---|---|---|---|---|
| Total | M | F | Total | M | F | ||||
| Garmaama | 1500–2660 | 2726 | 88 | 69 | 65 | 4 | 19 | 18 | 1 |
| Benjo Ashoka | 1918–1945 | 1091 | 35 | 27 | 25 | 2 | 8 | 8 | |
| Sayimanna Muudi | 1938–1961 | 1148 | 37 | 29 | 26 | 3 | 8 | 8 | |
| Chatimanna Jangala | 1970–2500 | 1551 | 58 | 47 | 44 | 3 | 11 | 11 | |
| Bulchaana | 1989–2196 | 1298 | 42 | 33 | 31 | 2 | 9 | 9 | |
| Wege Abosa | 2190–2300 | 1721 | 56 | 43 | 40 | 3 | 13 | 12 | 1 |
| Guchi | 2200–2786 | 1262 | 41 | 32 | 36 | 2 | 9 | 8 | 1 |
| Ilka Bebe | 2605–2867 | 957 | 31 | 24 | 21 | 3 | 7 | 6 | 1 |
| Total | 11,754 | 388 | 304 | 282 | 22 | 84 | 80 | 4 | |
Ethnobotanical Data Collection
Ethnobotanical data were gathered from February 2022 to March 2023 through individual semi-structured interviews and guided field walks using the methods of Martin32 and Cotton.33 Data collected from informants during interviews included sociodemographic information, local name of each claimed medicinal plant, part used, condition of plant part used (fresh/dried), additive used (if any), preparation method, ailment treated, route of administration, dosage, side effects, and antidotes used. Additional data regarding habitat, abundance, and existing threats of medicinal plants were also gathered through guided field walks as described in Martin32 and Alexiades.34 Voucher specimens from all mentioned medicinal plants were collected, dried, identified by botanists at ALIPB and the National Herbarium, AAU using published volumes of the Flora of Ethiopian and Eritrea, and deposited for future reference.
Analysis of Data
Data were analyzed using quantitative tools, including preference ranking exercise, informant consensus factor (ICF), fidelity level index (FL), and rank order priority (ROP) value32,35–37 to identify the most important medicinal plants in the district. Analysis of variance (ANOVA) and t-tests were used to determine the effects of sociodemographic factors on respondents’ knowledge of traditional medicinal plants. Preference ranking exercises32 were conducted on seven medicinal plants with the highest number of informant citations to manage the most commonly reported human gastrointestinal complaints and skin diseases by ten traditional medicine practitioners sampled from those who were already involved in individual interviews. Informant consensus factor was computed to determine culturally important human and livestock ailment categories and, by doing so, identify potentially effective medicinal plant species within the respective disease categories using the formula ICF = (Nur − Nt)/(Nur − 1), where Nur is the number of use reports for each disease category and Nt is the number of species used in that category.36 Fidelity level index was computed to reveal the level of agreement among informants in selecting medicinal plants used to manage a specific ailment using the formula, FL = (Np/N) x100, where Np is the number of informants who cited or mentioned the use of a medicinal plant against a particular disease and N is the total number of informants who cited that plant for any other medical use.35 However, plants with similar FL values but known to different numbers of informants may vary in their healing potential. Thus, a correlation index known as relative popularity level (RPL) was additionally determined to compute the rank order priority (ROP) value, as given by Ali-Shtayeh et al37 by multiplying the FL value by RPL to differentiate the healing potential of plants with similar FL values.
Results
Socio-Demographic Status of Informants
In this study, 388 informants (84 traditional healers and 304 general informants) were involved, the majority (54.12%) of whom were between 41 and 60 years of age. Regarding educational status, 57.73% of informants were illiterate, and 42.27% were literate. Regarding the gender of the informants, 360 (92.79%) were males and 28 (7.22%) were females (Table 2).
Table 2.
Demographic Categories of Local Respondents
| Socio-Demographic Group | Number of Informants | Percentage | |
|---|---|---|---|
| Gender | Male | 360 | 92.79 |
| Female | 28 | 7.22 | |
| Age group | 20–40 years old (youngster) | 86 | 22.16 |
| 41–60 years old (middle aged) | 210 | 54.12 | |
| 61–89 years old (elder) | 92 | 23.71 | |
| Literacy | Illiterate | 224 | 57.73 |
| Literate | 164 | 42.27 | |
| Informant type | Traditional healer | 84 | 21.65 |
| General informant | 304 | 78.35 |
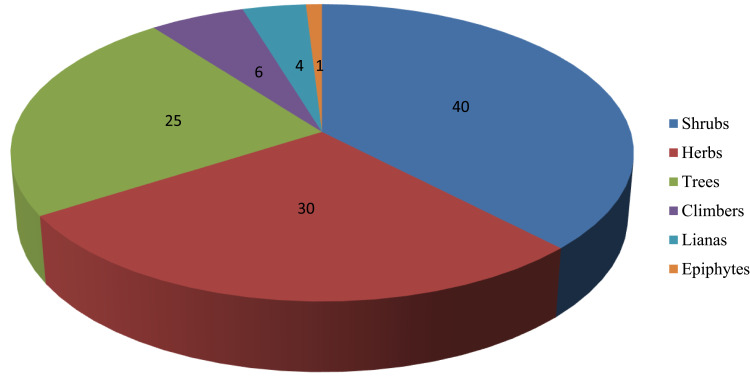
Diversity of Medicinal Plants Reported and Their Growth Forms
The study conducted in Kofale District recorded 106 medicinal plant species that belonged to 90 genera and 56 families, which were reported to treat 43 human illnesses and 18 livestock diseases (Table 3). Of these, 75 (71%) were used to manage human health problems, 23 (21.5%) to treat both human and livestock ailments, and eight (7.5%) to treat livestock diseases. The family Asteraceae was represented by nine species, Fabaceae and Solanaceae by seven species each, and Euphorbiaceae and Lamiaceae by five species each. Five families (Amaranthaceae, Myrsinaceae, Cucurbitaceae, Rosaceae, and Myrsinaceae) were represented by three species each and three families (Urticaceae, Meliaceae, and Rubiaceae) were represented by two species each. Each of the remaining families was represented by single species. Regarding the growth forms of medicinal plants, shrubs contributed the most (37.7%), followed by herbs (28.3%), trees (23.5%), herbaceous climbers (5.7%), lianas (3.7%), and epiphytes (0.9%) (Figure 2).
Table 3.
List of Medicinal Plants Used to Treat Human and Livestock Diseases in Kofale District
| Species Name | Family Name | Local Name | Habit | Part used | Disease Name Treated | Use | Mode of Preparation | Administration Route | Use citation | Voucher Number | Ailment Managed Elsewhere in Ethiopia |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Achyranthes sp. | Amaranthaceae | Qadara | Cl | Wh | Aspiration | Hu/Ls | Crushed with teeth | Nostrils | 12 | GN-120 | Wound infections,38 skin diseases39 |
| Acmella caulirhiza Delile | Asteraceae | Caanga | H | Wh | Headache | Hu | Crushed and squeezed | Nostril | 14 | GN-52 | Cancer-like symptoms,39,40 toothache41 |
| Adiantum sp. | Adiantaceae | Laaftuu | H | L | Wound | Crushed & squeezed | Topical | 5 | GN-72 | Wound treatment42 | |
| Agarista salicifolia (Comm.e.x. Lam.) Hook | Ericaceae | Sotra | T | Ba | Bone TB | Hu | Fresh bark is crushed and extract is applied | Dermal | 33 | GN-59 | Abdominal pain24 |
| Albizia gummifera (J.F.Gmel.) C.A.Sm. | Fabaceae | Qarcacee | T | Ba | Aspiration | Hu | Fresh bark is crushed and chewed | Oral | 34 | GN-16 | Anthrax28 |
| Albizia schimperiana Oliv. | Fabaceae | Sisaa | T | L/R | Liver disorder | Hu | Crush leaves and roots and mix them with water | Oral | 21 | GN-43 | Trypanosomiasis,43 helminthic infection,44 microbial infection,45 microbial infection46 |
| Cough | Ls | Fresh leaf is crushed and pounded | Oral | 49 | |||||||
| Hemorrhoids | Decoction | Topical | 16 | ||||||||
| Aloe sp. | Aloaceae | Hargisa | H | La | Hepatitis | Hu | Crushing the latex | Oral | 18 | GN-127 | Wounds and skin complaints, malaria, microbial infections, and complaints of the digestive system,47 malaria48 |
| L | Hemorrhoids | Hu | Crushing and squeezing | Anal | 260 | ||||||
| L | Abdominal pain | Hu | Crushing and squeezing | Oral | 80 | ||||||
| La | Dermatphilosisis, hair loss | Hu | Creaming | Topical | 78 | ||||||
| L | Blood pressure | Hu | Crushing | Oral | 103 | ||||||
| La | Eye ache | LS | Squeezing | Topical | 4 | ||||||
| Amaranthus dubius Mart ex Thell. | Amaranthaceae | Raafu qinxa | H | L | Anorexia | Hu | Fresh leaves are boiled | Oral | 8 | GN-33 | Diarrhea49 |
| L | Cancer | H | Crushed & squeezed | Oral | 52 | ||||||
| R | HIV-AIDS | H | Crush & mix juice produced with honey | Oral | 1 | ||||||
| Anethum graveolens L. | Apiaceae | Goomana | H | L | Constipation | Hu/LS | Fresh leaves are crushed and boiled | Oral | 23 | GN-171 | Stomachache50 |
| Apodytes dimidiata E.Mey. ex Arn. | Icacinaceae | Odda badaa | T | Ba | Stomachache | Hu | Decoction | Oral | 23 | GN-66 | Stomachache, cough,28; child diarrheal disease, cholera, general health problem (low weight and compromised immunity of infants24 |
| Ba | Internal parasite infection | LS | Crushed & mixed with water | Oral | 9 | ||||||
| Arundinaria alpina K. Schum | Poaceae | Leman | Sh | Sh | Hemorrhoid, diarrhea | Hu | Leaves are pounded and squeezed and mixed with water | Oral | 12 | GN-48 | Neck tumour23 |
| Asparagus africanus Lam. | Asparagaceae | Sariiti | H | L | Breast cancer | Hu | Crush leaves and add honey | Oral | 59 | GN-2 | Malaria,51 erectile dysfunction,52 malaria53 |
| R | Anthrax | Ls | Crush fresh root and mix it with water | Oral | 6 | ||||||
| Blackleg | 5 | ||||||||||
| Bersama abyssinica Fresen. | Melianthaceae | Koraqa | Sh | L L L Ba |
Intestinal parasite Stomach ache, diarrhea Equine glanders Elephantiasis, itching |
Hu Hu Ls Hu |
Crush pounded and mix it with water Crush pounded and mix it with water Crush pounded and mix it with water Pounded and boiled |
Oral Oral Oral Dermal |
90 95 44 115 |
GN-1 | HIV-AIDS,54 diabetics,55,56 diarrhea57 |
| Brucea antidysenterica J.F. Mill | Simaroubaceae | Ciironta | Sh | L | Eczema | Hu | Crush pounded and mix it with water | Oral | 69 | GN-6 | Diarrhea,58 leishmaniasis59 |
| Sd | Amoeba/diarrhea | Hu | Dry, grind and mix it with water | Oral | 53 | ||||||
| Caesalpinia decapetala (Roth) Alston | Gorxa | La | L | Dermatophilosis | Hu | Fresh leaves are smashed, pounded and mixed with water | Oral | 3 | GN-35 | Spiritual use,59 Tonsillitis60 | |
| Calpurnia aurea (Aiton) Benth | Fabaceae | Ceekata | Sh | L | Tick infestation | Ls | Pounding and squeezing | Dermal | 87 | GN-143 | Malaria,61 snake poisoning,62 livestock external parasites63 |
| L | Rabies | Hu/Ls | Fresh leaves are crushed and squeezed | Oral | 21 | ||||||
| L | Liver disorders | Hu | Dried & ground and mix it with water | Oral | 76 | ||||||
| Carica papaya L. | Caricaceae | Papaya | Sh | Fr | Anemia | Hu | Crushed & squeezed | Oral | 7 | GN-174 | Malaria,64 |
| Carissa spinarum L. | Apocynaceae | Agamsa | Sh | Ba | Tumour | Hu | Fresh bark is crushed and squeezed | Oral | 17 | GN-23 | Evil eye,65,66 gonorrhea,67 bacterial infection,68 spiritual illness,59 accumulation of fluid in the body69 |
| R | Cancer | Hu | Root is crushed together with root of Euclea schimperi, pounded and boiled | Oral & dermal | 77 | ||||||
| R | Wound | Hu | Fresh bark is crushed and mixed with butter | Topical | 22 | ||||||
| Casimiroa edulis La Llave | Solanaceae | Koshimi | SH | R | Evil eye | Hu | Pounded & decocted for steam bath | Topical | 3 | GN-107 | Cancer70 |
| Catha edulis (Vahl) Forssk. Ex Endl. | Celastraceae | Caatii | H | L | Stomachache | Hu | Chewed | Oral | 4 | GN-108 | Jaundice,71 stomachache72 |
| Clematis hirsuta Perr. and Guill. | Ranunculaceae | Fiitii | La | L | Bone cancer Wound |
Hu Hu |
Pounded | Politice | 43 32 |
GN-76 | Blackleg,73 respiratory tract problem and cataract74 |
| Clerodendrum myricoides (Hochst.) R. Br. ex Vatke | Verbenaceae | Marachisa | T | Fr | Oedema | Hu | Dried & ground | Oral | 18 | GN-4 | Rheumatism, evil eye71 |
| L | Wound | Hu/Ls | Fresh leaves are crushed and mixed with water | Dermal | 16 | ||||||
| Coffee arabica L. | Rubiaceae | Buna | Sh | Fr | Diarrhea | Hu | Dried, ground and mixed with water | Oral | 13 | GN-178 | Diarrhea75 |
| Cordia africana Lam. | Borginaceae | Wodeessa | T | Ba | Cancer | Hu | Crushed while fresh and mixed with water | Oral | 13 | GN- | Pain, inflammation, microbial and viral infections, and fertility problem76 |
| Croton macrostachyus Hochst. ex Delile | Euphorbiaceae | Makanisa | T | Ba | Tumour | Hu | Bark is dried and ground | Topical | 55 | GN-25 | Malaria, abdominal pain, gonorrhea, wounds, ringworm infestation, hemorrhoids, ascariasis, venereal diseases, cough and rheumatism,77 malaria65 |
| Cynoglossum lanceolatum Forssk. | Borginaceae | Maxxanne | H | Wh | Febrile illnesses | Hu | Crushed & boiled | Oral | 2 | GN-98 | Fever,78 hemorrhoids79 |
| Datura stramonium L. | Solanaceae | Banji | H | Sd | Rabies | Hu | Seeds are roasted, ground and mixed with water | Oral | 76 | GN-9 | Bacterial infection,80 skin infections,81 head fungal infection,82 toothache,41 dermatological diseases61 |
| Sd | Head ache | Hu | Seeds are roasted | Nostril | 13 | ||||||
| Discopodium penninervum Hochst. | Solanacae | Maraaro | Sh | L | Pasteurollosis | Ls | Its leaves are crushed with leaves of Kalanchoe petitiana and mixed with water | Oral | 7 | GN-29 | Malaria, hemorrhoids, and anthrax in livestock28 |
| Dodonaea viscosa subsp. angustifolia (L.f.) J.G. West | Sapindaceae | Ittacha | Sh | L | Herpes zoster | Hu | Crushed & squeezed | Dermal | 16 | GN-15 | Malaria,83 diarrhea, ulcer, microbial infection, diabetics, HIV-AIDS54 |
| Dermatochalasis | Hu | Crushing, pounding and powdering | Dermal | 27 | |||||||
| Wound | Hu | Decoction | Body shower | 42 | |||||||
| Dovalis abyssinica (A.Rich.)Warb. | Flacourtiaceae | Dhangago | Sh | Fr | Jaundice | Hu | Its fruits are mixed with root of Stephania abyssinica, crushed and mixed with water | Oral | 22 | GN-44 | Ascariasis84 |
| Drynaria volkensii Hieron. | Polypodiaceae | Kokoso | Sh | L | Tumour | Hu | Chewed & swallowed | Oral | 2 | GN-71 | Tooth ache41 |
| Echinops angustilobus S. Moore | Asteraceae | Anshokala | H | R | Evil eye | Hu | Dried, and ground | Nostrils | 5 | GN-153 | Bloating28 |
| Ekebergia capensis Sparrm | Miliaceae | Onoonuu | T | Ba | Babesiosis | Ls | Fresh bark is crushed and mixed with water | Oral | 73 | GN-55 | TB,28 weight loss in children, stabbing pain, bovine TB85 |
| Embelia schimperi Vatke | Myrsinaceae | Qaanqu | Sh | Fr | Tapeworm | Hu | Grind the dried fruit by mixing with Hagenia abyssinica dried flower | Oral | 197 | GN-73 | Helminthic infection,86 gastro-intestinal diseases in animals,87 helminthic infection88 |
| Englerina woodfordioides (Schweinf.) M Gilbert | Loranthaceae | Mukure | Epi | Wh | Liver disorders | Hu | Crushed & boiled | Oral | 19 | GN-36 | Earaches71 |
| Ensete ventricosum (Welw.) Cheesman | Musaceae | Worqe | Sh | L | Stomachache | Hu | Leaf petiole is crushed and fermented for weeks | Oral | 3 | GN-177 | Abdominal pain89 |
| Entada abyssinica Steud. Ex A. Rich | Fabaceae | Bobanqa | T | L | Skin diseases | Hu | Crushed, pounded and mixed with water | Dermal | 62 | GN-86 | Convulsion90 |
| Erica sp. | Ericaceae | Sato | Sh | L | Stomachache | LS | Fresh leaf is crushed and mixed with water | Oral | 11 | GN- 60 | Indigestion and bloating24 |
| Erythrina abyssinica Lam. ex DC. | Fabaceae | Woleena | Sh | Sh | Pasteurollosis | Ls | Fresh shoot is crushed and squeezed | Oral | 14 | GN-5 | Snakebites, malaria, sexual transmittable diseases such as syphilis and gonorrhoea, amoebiasis, cough, liver inflammation, stomachache, colic, measles, burns, ulcers and swellings,91 evil eye92 |
| L | Eye ache | LS | Crushed and squeezed | Topical | 33 | ||||||
| Eucalyptus camaldulensis Dehnh. | Myrtaceae | Bergamo diima | Sh | Ba | Febrile illness | Hu | Fresh part is crushed and squeezed | Topical | 8 | GN-169 | Bacterial infection93 |
| Eucalyptus globulus Labill. | Myrtaceae | Bargamo adii | T | L | Stomachache | Hu | Crushed & chewed | Oral | GN-162 | Stomachache,94 influenza,95 bacterial infection,96 respiratory tract infections,97 malaria57 | |
| Euclea schimperi (A.DC) Dandy | Ebenaceae | Mi’eesa | T | RB | Hemorrhoids | Hu | Its root bark and seeds of Solanum anguivi are dried, ground and mixed with butter Dried, pounded and mixed with butter |
Topical | 15 | GN-87 | Wound, teeth infections, eye disorders, head ache, pain, spasm98 |
| Dermatophilosis | Hu | Fresh leaf is crushed and mixed with water | Topical | 131 | |||||||
| L | Stomach ache | Hu | Oral | 50 | |||||||
| Euphorbia schimperiana Scheele | Euphorbiaceae | Guurii | H | Sp St |
Gonorrhea Hemorrhoid |
Hu HU |
Crushed & decocted Crushing & pounding |
Dermal Anal |
73 95 |
GN-6 | Proliferative activity,99 cancer,39 anthrax in livestock73 |
| Euphorbia tirucalli L. | Euphorbiaceae | Aananoo | Sh | La | Body swelling, gonorrhea | Hu | Crushed and squeezed | Dermal | 89 | GN-100 | Bacterial infection of urinary tract,100 urogenital disease,101 Stomachache28 |
| Ficus sycomorus L. | Moraceae | Qiltu | T | Ba | Diarrhea | Hu | Fresh bark is crushed and squeezed | Oral | 19 | GN-104 | Nausea and vomiting,49 ascariasis102 |
| Galiniera saxifraga (Hochst.) Bridson | Rubiaceae | Koralla | Sh | Ba Ba Ba Ba |
Babesiosis Liver disorders Jaundice Stomach ache |
LS Hu Hu Hu |
Crushed squeezed and mixed with water Fresh leaf is crushed and swallowed Fresh root is chewed and swallowed Decoction |
Oral Oral Oral |
14 73 31 63 |
GN-15 | Anthrax28 |
| Hagenia abyssinica (Bruce) J.F. Gmel. | Rosaceae | Heexo | T | Fr | Tapeworm | Hu | Crush its dried flower with bark of Croton macrostachyus and fruit of Embelia schimperi | Oral | 76 | GN-91 | Helminthic infections82 |
| Halleria lucida L | Scrophulariaceae | Muka dadhi | T | L | Body swelling | Hu | Decoction | Topical | 16 | GN-54 | Evil eye and kidney problem103 |
| Hypericum quartinianum A.Rich. | Hypericaceae | Garamba | Sh | L | Hepatitis | Hu | Its leaves and that of Junipers procera are crushed together and boiled | Oral | 85 | GN- | Stomachache for livestock104 |
| Ilex mitis (L.) Radlk | Rubiaceae | Amshiqa | T | Ba | Hemorrhoids | Hu | Fresh bark is crushed and boiled in water | Oral | 98 | GN-161 | Rheumatism71 |
| Juniperus procera Hochst.ex. Endl. | Cuperssaceae | Hidhesa ummama | T | Ba | Diarrhea | Hu | Fresh bark is crushed and squeezed and mixed with water | Oral | 35 | GN-14 | Stomachache105 |
| Justicia schimperiana (Hochst. ex Nees) T. Anderson | Acanthaceae | Dhumuuga | Sh | Sh | Hepatitis | Hu | Fresh shoot is pounded to make juice | Oral | 235 | GN-7 | Diabetes mellitus106 |
| Kalanchoe petitiana A. Rich | Rassulaceae | Hancuura | H | L L L L L |
Tonsillitis Bone fracture GIT disorders Pasteurellosis Anthrax |
Hu Hu Ls |
Crushed while fresh and squeezed Boiled while fresh Fresh leaf is chewed Crushed together with leaf of Disco podium penninervum |
Oral Dressing Oral Oral |
15 71 13 11 5 |
GN-18 | Evil eye, fractured bones and skin disorders,107 tissue proliferation,39 metacarpal bone fracture in livestock,91,108 anthrax28 |
| Lagneria sp. | Cucurbitaceae | Buqe arba | Sh | St | Hepatitis | Hu | Crushed & sap produced is collected | Oral | 87 | GN-66 | Gonorrhea,16 cancer109 |
| Lippia adoensis Hochst. | Verbenaceae | Sukayi | H | L | Stomachache | HU | Crushed & chewed | Oral | 22 | GN-37 | Severe headache,25 pain,110 harm on body by free radicals,111 fungal infection,112 repelling Anopheles arabiensis and Aedes aegypti,113 bacterial and fungal infection,114 stomach pain71 |
| Maesa Lanceolata Forssk. | Myrsinaceae | Abbayii | T | Ba Ba |
Liver disorders Dermatophilosis |
Hu Hu/Ls |
Its bark is mixed with leaves of Discopodium penninervum and boiled Dried & boiled |
Oral Dermal |
97 62 |
GN-142 | Mastitis,28 malaria,115 ovicidal and larvicidal activity,116 Snakebites81 |
| Mangifera indica L. | Anacardiaceae | Mango | Sh | Fr | Blood pressure | Hu | Squeezed | Oral | 4 | GN-110 | Harm on body by free radicals117 |
| Maytenus addat (Looes.) Sebsebe | Celastraceae | Kombolcha | Sh | Ba | Diarrhea | Hu | Fresh bark is crushed and mixed with water | Oral | 10 | GN-53 | Parasites infections28 |
| Millettia ferruginea (Hochst.) Bak. | Fabaceae | Dhadhatu | T | Fr | Leech infestation | Ls | Crushed & pounded | Nostril | 72 | GN-90 | ‘Mujele’ (infection caused by an insect present in the soil)118 |
| Moringa stenopetala (Bak.f.) Cuf. | Moringaceae | Shifera | Sh | L | Blood pressure | Hu | Crushed, dried and ground | Oral | 44 | GN-126 | Anthrax28 |
| Myrsine melanophlous (L.) R.Br. | Myrsinaceae | Tuula | Sh | L Ba |
Child emaciation Stomachache |
Hu Hu |
Fresh leaf is pounded and boiled Decoction |
Oral & body shower Oral |
57 69 |
GN-41 | Stomach problem28 |
| Nicotiana tabacum L. | Solanaceae | Tambo | H | R L |
Leech infestation Tooth ache |
Hu/Ls HU |
Chewed & spit into the mouth of the sick animal Dried & powdered |
Oral Topical |
48 14 |
GN-176 | Leech repulsion78 |
| Nuxia congesta R. Br. ex Fresen. | Loganiaceae | Bixana | Anthrax | Ls | Crushed, squeezed and mixed with water | Oral | 11 | GN-47 | Malaria,119 calf pneumonia,120 anthrax28 | ||
| Ocimum gratissimum L | Lamiaceae | Cabbicha | H | L | Rheumatism, headache, eye disease, allergic reaction | Hu | Crushed & squeezed | Oral & nostril | 31 | GN-80 | Skin infections121 |
| Oenanthe palustris (Chiov.) Norman | Apiaceae | Goonde | H | L | Bone cancer | Hu/ Ls | Fresh leaves are crushed | Topical | 13 | GN-42 | Tooth ache41 |
| Olinia rochetiana A. Juss. | Oliniaceae | Gunaa | T | L | Bone TB Diarrhea |
Hu Hu |
Fresh leaf is crushed and macerated with water Fresh leaf is crushed and macerated with water |
Dermal Oral |
79 133 |
GN-17 | Stabbing pain,73 colds and chest related condition122 |
| Physalis peruviana L. | Solanaceae | Mujulo | H | Wh | Indigestion | Hu | Crushed & boiled in water | Oral | 3 | GN-111 | Medicinal value95 |
| Phytolacca dodecandra L’Her. | Phytolaccaceae | Handoode | H | L L R |
Jaundice External parasite, dermatophilosis Rabies |
Hu LS Hu/LS |
Fresh leaves are crushed and juice diluted in water Fresh leaf is crushed Fresh root is crushed and mixed with water |
Oral Dermal Oral |
8 64 92 |
GN-93 | Molluscicidal properties,123 used for abortion118 |
| Pittosporum abyssinicum Del. | Pittosporaceae | Aaraa | T | L Ba |
Cancer Blackleg |
Hu | Fresh leaves are crushed and mixed with water Crushed & mixed with water |
Oral Oral |
22 6 |
GN-50 | Coughing, Pneumonia, TB, and Abdominal pain,24 cancer,124 intestinal problems, internal parasites, urine problems, diarrhea, swelling of gland, ascariasis, diarrhea, and vomiting125 |
| Podocarpus falcatus (Thunb.) R.B. ex Mirb. | Podocarpaceae | Birbirsa | T | L | Epilepsy Cancer |
Hu Hu |
Its leaves together with leaves of Carissa spinarum are crushed and boiled Fresh leaves are crushed and boiled in water |
Oral Oral |
50 17 |
GN-8 | Wound of both human and livestock126 |
| Polycarpon tetraphyllum (L.) L. | Caryophyllaceae | Laalessa | CL | R | Toothache | Hu | Crushed & kept between teeth | Topical | 4 | GN-172 | Lung diseases and menstrual problem71 |
| Prunus africana (Hook.f.) Kalkman | Rosaceae | Sukee | T | L Sh Ba |
GIT cancer Stomachache Skin diseases, wound |
Hu Hu/Ls |
Fresh leaves are boiled in water Crushed & squeezed |
Oral Dermal |
21 73 76 |
GN-27 | Cancer, respiratory disorders, bad breath, diarrhea, gonorrhea, tuberculosis, and ear problems28 |
| Psidium guajava L. | Myrtaceae | Zeeytuna | Sh | Sd | Hepatitis | Hu | Dried, powdered and mixed with water | Oral | 7 | GN-175 | Damage on body by free radicals and bacterial infection127,128 |
| Ranunculus multifidus Forssk. | Ranunculaceae | Siifa | H | L | Cancer | Hu | Fresh leaf is crushed and mixed with water | Oral | 12 | GN-51 | Oedema129 |
| Rhamnus prinoides L’Hér | Rhamnaceae | Geesho | H | Wh | Stomach ache | Ls | Pounded & mixed with water | Oral | 6 | GN-170 | Tonsillitis71 |
| Rhus tenuinervis Engl. | Anacardiaceae | Kolaassa | Sh | L | Cough | Hu/Ls | Dried, ground and boiled in water | Oral | 3 | GN-22 | Stomach bloating in livestock28 |
| Ricinus communis L. | Euphorbiaceae | Qoboo | Sh | Sd | Infertility | Hu/LS | Seeds are dried, powdered and boiled | Oral | 44 | GN-92 | Erectile dysfunction,52 antimicrobial infection,130 coughing, constipation and swelling and anthrax94 |
| Rosmarinus officinalis L. | Lamiaceae | Wodi fooni | H | L | Diabetes | Hu | Crushed & boiled | Oral | 31 | GN-99 | Bacterial infection,110,131,132 |
| Rubus steudneri Schweinf. | Rosaceae | Gora | La | L | Wound | Hu/LS | Dried & ground | Dermal | 5 | GN-40 | Bacterial infection,87 damage on body by free radicals116 |
| Rumex abyssinica Jacq. | Polygonaceae | Shoshira | Sh | L | Gonorrhea, diarrhea | Hu | Crushed, pounded and boiled | Oral | 10 | GN-74 | Damage on body by free radicals and inflammation,133 diabetes mellitus134 |
| Rumex nepalensis Spreng. | Polygonaceae | Shaabee | H | R | Hemorrhoids | Hu | Dried, ground and mixed with sugar | Oral | 78 | GN-9 | Gastrointestinal infection,74 diarrhoea73 |
| L | Goiter | Hu | Crushed & mixed with water | Oral | 10 | ||||||
| Diarrhea | LS | Fresh leaf crushed and mixed with water | Oral | 77 | |||||||
| Ruta chalepensis L | Rutaceae | Caarota | H | L | Stomachache, abdominal pain, gastritis | Hu | Crushed and chewed | Oral | 6 | GN-97 | Stomachache28 |
| Rytigynia neglecta (Hiem) Robyns | Rubiaceae | Gaaloo | Sh | R | Pneumonia | Hu | Fresh root is crushed and boiled in water | Oral | 13 | GN-20 | TB135 |
| Saliva nilotica Juss. ex Jacq. | Lamiaceae | Hulageb | H | L | Snakebites | Hu | Crushed, dried and mixed with butter | Dermal | 27 | GN-173 | Skin diseases28 |
| Schefflera abyssinica Hochst. ex A. Rich.) Harms | Araliaceae | Gatame | T | Ba | Tonsillitis | Hu | Inner part of the bark is chewed | Oral | 13 | GN-151 | Anthrax28 |
| Schefflera volkensii (Engl). Harms | Araliaceae | Anshaa | T | L | Anthrax | Ls | Its leaves are crushed with leaves of Hypericum quartinianum and mixed with water | Oral | 28 | GN-161 | Head ache73 |
| Sedum baleensis M. Gilbert | Crassulaceae | Buri | H | R | Eczema | Hu/LS | Fresh leaves are crushed | Dermal | 4 | GN-68 | Eczema71 |
| Senecio myriocephalus Sch. Bip. ex A. Rich. | Asteraceae | Agadena | T | R | Stomachache | Fresh root is crushed, squeezed and mixed with water | Oral | 24 | GN-163 | Evil eye,118 herpes Zoster71 | |
| Sida schimperiana Hochst. ex A. Rich | Malvaceae | Kotte jabeesa | H | L | Evil eye | Hu | Leaf is dried and ground | Tie on the neck | 12 | GN-152 | Prenatal abortion,67 microbial infection136 |
| Solanecio gigas (Vatke) C. Jeffrey | Asteraceae | Taruura | Sh | Ba | Babesiosis | Hu/LS | Crushed & mixed with water | Oral | 4 | GN-172 | Bacterial infection137 |
| Solanum adoense Hochst ex. A.Rich. | Solanaceae | Hiddi oromoo | Sh | L | Nose bleed | Hu | Fresh leaves are smashed | Nostril | 11 | GN-10 | Malaria138 |
| Solanum anguivi Lam | Solanaceae | Xoshine | H | L | Blood pressure | Hu | Dried, ground and boiled | Oral | 51 | GN-65 | Trypanosomiasis,139 diabetes and atherosclerosis140 |
| Solanum benderianum Schimp. ex Engl. | Solanaceae | Galimo | T | R | Stomachache | Hu | Root is crushed, dried and boiled | Oral | 3 | GN-69 | Hypertension141 |
| Solanum benderianum Shimper ex Damme | Solanaceae | Galimo | CL | Ba | Stomachache | Hu | Dried, ground and boiled | Oral | 3 | GN- 69 | Calf diarrhea142 |
| Stephania abyssinica (Dillon & A. Rich.) Walp. | Menispermaceae | Kalaala | Cl | L | Jaundice | Hu | Leaf dried, ground and boiled in water | Oral | 31 | GN-11 | Malaria,143 gastrointestinal diseases,144 external cancer91 |
| Syzygium guineense (Willd.) DC. | Myrtaceae | Baddeesa | T | Ba | Kidney infection Diarrhea Tonsillitis |
Hu Hu |
Fresh leaf is crushed, squeezed and mixed with water Fresh leaf is chewed and ingested |
Oral Oral |
20 133 13 |
GN-62 | Stomachache, diarrhea,28 hypertension,145 Malaria,100 cancer.146 |
| Teclea nobilis Del. | Rutaceae | Hadhesa | Sh | L | Blackleg | Ls | Leaves are pounded and mixed with water | Oral | 10 | GN-30 | Blackleg89 |
| Toddalia asiatica (L) Lam. | Rutaceae | Gaawo | Sh | Fr | Stomach ache, wound | Hu/ Ls | Fruit is crushed, pounded and mixed with water | Oral | 7 | GN-28 | External body swelling147 |
| Urera hypselodendron (Hochst. ex A. Rich.) Wedd. | Urticaceae | Haliila | CL | Ba | Internal parasite | Leaves are crushed and mixed with water | Oral | 66 | GN-31 | Anthrax17 | |
| Urtica simensis Steudel. | Urticaceae | Doobii | H | L | Constipation & gastritis Bloat |
Hu Ls |
Leaves are washed and boiled in water Leaves are washed and boiled in water |
Oral | 35 16 |
GN-95 | Damage on body by free radicals,92 stomach ulcer,144 wound,148 malaria149 |
| Verbascum sinaiticum Benth. | Scrophulariaceae | Gurra harree | Sh | L | Hepatitis | Hu | Fresh/dry leaves are crushed and mixed in water | Oral | 8 | GN- | Hepatitis,150 blood pressure151 |
| Vernonia amygdalina Del. | Asteraceae | Ebicha | Sh | Ba L L L |
Bone TB Skin diseases Diarrhea Goiter |
Hu Hu Hu/Ls Hu |
Fresh root is crushed and mixed with honey Decoction Decoction Fresh leaf is crushed and squeezed |
Oral Dermal Oral Oral |
7 81 84 15 |
GN-12 | Malaria152 |
| Vernonia auriculifera Hiern | Asteraceae | Reejii | Sh | L | Bloat | Ls | Leaves are crushed and macerated in water | Oral | 16 | GN-13 | Wound,153 bacterial infection,154 pain and inflammation, wound155 |
| Vernonia sp. | Asteraceae | Kalaqicha | Sh | L | Diarrhea | Hu | Crushed & squeezed | Oral | 7 | GN-70 | Mlaria64 |
| St | Ringworm | Hu | Stem is crushed | Dermal | 12 | ||||||
| Withania somnifera (L.) Dunal | Solanaceae | Baala ajo | Sh | L/R | Evil eye | Hu | Dried, ground and mixed with water | Oral & nostril | 78 | GN-84 | Trypanosomiasis,156 evil eye,157 enteric bacteria infection83 |
| L | Diarrhea | Leaf is crushed and squeezed | Oral | 65 |
Abbreviations: T, tree, Sh, shrub, H, herb, Fr, fruit, Sa, sap, La, liana, Cl, climbers, ep, epiphyte, Hu, human, Ls, livestock, Hu/Ls, human and livestock, L, leaf, Ba, bark, R, root, Se, seed, St, stem, Wh, whole plant, Sh, shoot, Lt, latex, L/R, leaf and root, GIT, gastro-intestinal tract, TB, tuberculosis.
Figure 2.
Proportions of medicinal plants growth forms in percent.
Habitat of Medicinal Plants
Most medicinal plants (76.4%) used in traditional medicine in the district were uncultivated that were harvested from forests, riverbanks, grasslands, roadsides, life fences, and school compounds. Some were grown in homestead gardens (15%), and a few were harvested from both wild and homestead gardens (8.6%).
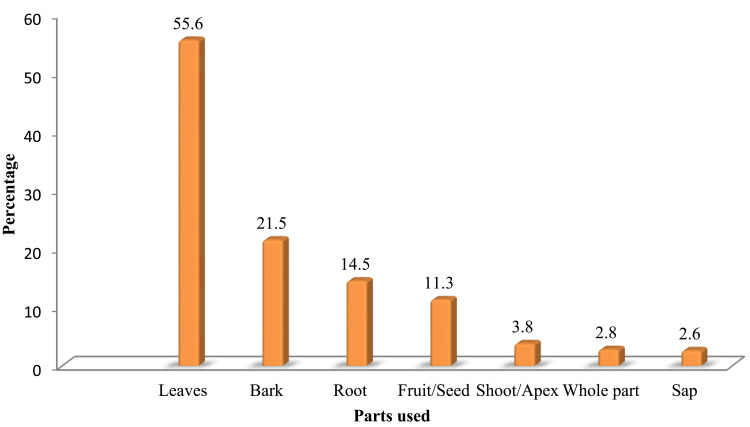
Medicinal Plant Parts Used in Remedy Preparations
The leaves were the most commonly used medicinal plant parts (55.6%) in the preparation of plant-based remedies in the district, followed by the bark (21.6%), root (14.15%), fruit/seed (11.3%), shoot/apex (3.8%), whole parts (2.8%), and sap (2.6%) (Figure 3).
Figure 3.
Proportions in percent of plant parts used for the treatment of human and livestock diseases in Kofale District, Oromia Regional State, Ethiopia.
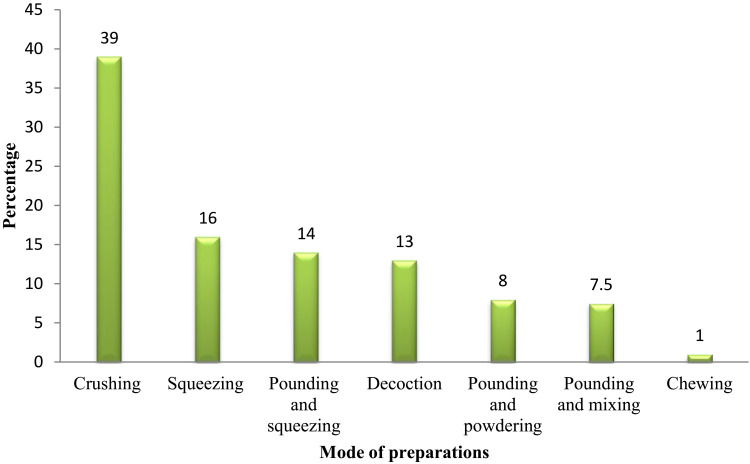
Conditions of Plant Parts Used and Preparation Methods
The majority (75.8%) of the medicinal plant parts were claimed to be used in their fresh form, whereas some others were used in their dry (14.15%) and dry or fresh (10.65%) forms. The highest proportion (39%) of remedies was prepared by crushing (39%), followed by squeezing (16%), pounding and squeezing (14.5%), decoction (13%), pounding and powdering (9%), pounding and mixing (7.5%), and chewing (1%) (Figure 4).
Figure 4.
Percentages of different methods of remedy preparations.
Administration Routes of Remedies
Oral was the most frequently cited route of remedy administration in the district (61.3%), followed by topical/dermal (26.3%), nasal (4.7%), and ocular (3.8%) routes (Table 4).
Table 4.
Route of plant remedy application
| Route of Application | Frequency of Citation | Percentage |
|---|---|---|
| Oral | 65 | 61.3 |
| Dermal | 27 | 25.4 |
| Nasal | 5 | 4.7 |
| Ocular | 4 | 3.8 |
| Skin cut | 2 | 1.9 |
| Ears | 2 | 1.9 |
Dosage of Medicinal Plants and Use of Antidotes
Most frequently, traditional medicine practitioners’ prescriptions were based on patient age, gender, presence or absence of pregnancy and body condition. Different measuring materials, such as waterglass, teacup, coffee cup, teaspoon, bottle cap, handful, and between two fingertips were used to determine the dosage. Traditional medical practitioners employ different antidotes to neutralize possible adverse effects such as vomiting, nausea, diarrhea, headache, and loss of consciousness. Antidotes used mainly included fermented milk, fresh milk, honey, and coffee.
Commonly Reported Human and Livestock Diseases in the District
Of 43 human health problems occurring in Kofale District, dermatophilosis, gastrointestinal disorders, cancer, and hemorrhoids were the most prevalent reported by 35%, 31%, 18%, and 12% of the informants, respectively. Of the total 18 livestock health problems occurring in Kofale District, wound, tick infestation, leech infestation, dermatophilosis, equine glanders, anthrax, blackleg and pasteurellosis were the most reported ones with frequency of citation 26%, 22.4%, 19%, 16%, 11.3%, 7.2% and 3.3%, respectively.
Preference Ranking of Selected Medicinal Plants Used Against Human Gastrointestinal and Skin Diseases in the District
According to preference ranking exercise conducted on seven medicinal plants of the highest informant citations for their uses to treat human gastrointestinal complaints, a health problem of the second highest prevalence in the study district, Olinia rochetiana was the most preferred medicinal plant, followed by Bersama abyssinica and Vernonia amygdalina (Table 5).
Table 5.
Preference ranking of selected medicinal plants used to treat human gastrointestinal complaints in Kofale District
| Medicinal Plants Ranked | Informants Labeled A to J | Total Score | Rank | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |||
| Olinia rochetiana | 5 | 4 | 7 | 6 | 7 | 5 | 4 | 6 | 7 | 6 | 57 | 1 |
| Bersama abyssinica | 4 | 7 | 6 | 5 | 5 | 6 | 6 | 5 | 5 | 6 | 55 | 2 |
| Vernonia amygdalina | 6 | 5 | 6 | 4 | 6 | 5 | 5 | 5 | 6 | 6 | 54 | 3 |
| Euclea schimperi | 5 | 6 | 5 | 5 | 3 | 4 | 5 | 3 | 7 | 4 | 47 | 4 |
| Rumex nepalensis | 4 | 4 | 6 | 7 | 3 | 2 | 6 | 7 | 5 | 2 | 46 | 5 |
| Prunus africana | 5 | 3 | 2 | 5 | 4 | 3 | 5 | 4 | 2 | 6 | 39 | 6 |
| Myrsine melanophloeos | 4 | 3 | 3 | 3 | 6 | 4 | 3 | 2 | 6 | 2 | 36 | 7 |
A preference ranking exercise conducted on seven medicinal plants with the highest informant citations for their use in managing skin disorders, a health problem with the highest prevalence in the study district revealed that Euclea schimperi was the most preferred medicinal plant, followed by Maesa lanceolata and Vernonia amygdalina (Table 6).
Table 6.
Preference ranking of selected medicinal plants used to manage skin diseases in Kofale District
| Medicinal Plants Ranked | Informants Labeled A to J | Total Score | Rank | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |||
| Euclea schimperi | 7 | 7 | 4 | 4 | 6 | 7 | 5 | 5 | 6 | 7 | 61 | 1 |
| Maesa Lanceolata | 7 | 4 | 7 | 5 | 7 | 6 | 6 | 4 | 6 | 6 | 58 | 2 |
| Vernonia amygdalina | 7 | 7 | 4 | 4 | 5 | 5 | 6 | 7 | 5 | 4 | 57 | 3 |
| Aloe sp. | 7 | 6 | 6 | 5 | 5 | 6 | 5 | 5 | 5 | 4 | 55 | 4 |
| Prunus africana | 7 | 6 | 5 | 5 | 6 | 7 | 4 | 4 | 4 | 4 | 52 | 5 |
| Bersama abyssinica | 4 | 4 | 3 | 5 | 5 | 5 | 5 | 6 | 6 | 6 | 50 | 6 |
| Phytolacca dodecandra | 5 | 5 | 3 | 6 | 4 | 5 | 4 | 3 | 6 | 6 | 47 | 7 |
Medicinal Plants Scoring the Highest Fidelity Level and Rank Order Priority Values
Of the medicinal plants used to manage human ailments in the district, Justicia schimperiana, Embelia schimperi, Olinia rochetiana and Euclea schimperi which have been used to treat liver disorders, tapeworm infections, general gastrointestinal complaints, and dermatological disorders, respectively, scored the highest fidelity level (FL) (100%) and rank order priority (ROP) (>81%) values (Table 7).
Table 7.
Rank order priority values of medicinal plants used to treat human ailments in the Kofale District with fidelity level values of above 80%
| Medicinal Plant Spp. | Therapeutic Category | Np | N | FL (%) | RPL | ROP |
|---|---|---|---|---|---|---|
| Justicia schimperiana | Liver disorders | 235 | 235 | 100.0 | 1.00 | 100.0 |
| Embelia schimperi | Tapeworm worm infection | 197 | 197 | 100.0 | 1.00 | 100.0 |
| Olinia rochetiana | General gastrointestinal complaints | 133 | 133 | 100.0 | 0.83 | 83.1 |
| Euclea schimperi | Dermatological diseases | 131 | 131 | 100.0 | 0.82 | 81.9 |
| Aloe sp. | Hemorrhoids | 260 | 320 | 81.0 | 1.00 | 81.0 |
| Phytolacca dodecandra | Rabies | 92 | 98 | 94.0 | 0.61 | 57.6 |
| Withania somnifera | Evil spirit | 65 | 75 | 87.0 | 0.47 | 40.8 |
| Podocarpus falcatus | Epilepsy | 50 | 62 | 80.6 | 0.39 | 31.2 |
| Asparagus africanus | Cancer | 44 | 52 | 84.6 | 0.33 | 27.5 |
Among the medicinal plants claimed to manage livestock health problems in the study district, Ekebergia capensis (for treatment of babesiosis), Datura stramonium (for treatment of rabies), and Millettia ferruginea (for treatment of leech infestation) had the highest fidelity level (FL) (>97%) and rank order priority (ROP) (97%) values (Table 8).
Table 8.
Rank order priority values of medicinal plants for livestock diseases in the Kofale District
| Medicinal Plant Spp. | Therapeutic Category | Np | N | FL (%) | RPL | ROP |
|---|---|---|---|---|---|---|
| Ekebergia capensis | Babesiosis | 73 | 73 | 100 | 1.00 | 100.0 |
| Datura stramonium | Rabies | 76 | 76 | 100 | 1.00 | 100.0 |
| Millettia ferruginea | Leech infestation | 72 | 74 | 97.2 | 1.00 | 97.2 |
| Prunus africana | Wound | 102 | 121 | 82.6 | 1.00 | 82.6 |
| Maesa lanceolata | Dermatophilosis | 62 | 76 | 82 | 1.00 | 82.0 |
| Calpurnia aurea | Tick infestation | 87 | 107 | 81.3 | 1.00 | 81.3 |
| Bersama abyssinica | Equine glanders | 44 | 46 | 95.6 | 0.75 | 72.1 |
| Schefflera volkensii | Anthrax | 28 | 33 | 85 | 0.54 | 46.0 |
| Kalanchoe petitiana | Pasteurellosis | 11 | 13 | 85 | 0.21 | 18.1 |
Informant Consensus Factor Values
Human and livestock ailments in the study district reported by informants were grouped into 12 major disease categories, and informant consensus factor (ICF) values were calculated. Accordingly, skin-related diseases scored the highest ICF value (0.97), followed by gastrointestinal tract infections (0.95), cancer (0.93), animal bites (0.92), hemorrhoids, and body swelling (0.91). Respiratory tract disorder category had the lowest ICF value (0. 62) (Table 9).
Table 9.
Informant consensus factor values of disease categories in study area
| Diseases Category | Specific Ailment Reported | Use Citation (Nur) | Number of Species Used (Nt) | Informant Consensus Factor (ICF) |
|---|---|---|---|---|
| Skin-related diseases | Eczema, dandruff, lump rashes, skin lesion, ringworm, wound, wart, scabies, tick infestation, epizootic lymphangitis of horse | 288 | 10 | 0.97 |
| Gastro-intestinal tract infections and parasitic diseases | Abdominal pains, diarrhea, dysentery, typhoid fever, indigestion, stomachache, ulcers, vomiting, nausea, constipation, ascariasis, taeniasis | 286 | 16 | 0.95 |
| Cancer diseases | Breast cancer, throat cancer, skin cancers, tumor, other cancers | 124 | 9 | 0.93 |
| Animal bites | Poisoning, rabies, insect bites | 76 | 7 | 0.92 |
| Hemorrhoid, and body swellings | 100 | 9 | 0.91 | |
| Liver diseases | Hepatitis, diseases of gallbladder, bile duct diseases, jaundice | 75 | 9 | 0.87 |
| Animal bacterial diseases | Anthrax, blackleg, glanders, Pasteurellosis | 92 | 12 | 0.87 |
| Endocrine & metabolic diseases | Diabetes, blood pressure, anemia heart diseases, hypertension | 31 | 5 | 0.86 |
| Musculoskeletal diseases & nervous disorders Arthritis | Bone fracture, rheumatism, epilepsy | 28 | 5 | 0.85 |
| Spiritual complications | 29 | 7 | 0.78 | |
| Urogenital and reproductive disorders | Erectile dysfunction, syphilis, uterine infections, retained placenta, gonorrhea, abnormal menstrual cycle, infertility, breech position in pregnancy, dystocia labor | 34 | 9 | 0.75 |
| Respiratory tract-related problem | Asthma, chest pain, cough, pneumonia, tonsillitis. | 9 | 4 | 0.62 |
Ways of Acquisition of Traditional Medical Knowledge
Traditional medicinal knowledge in the district was reported to have been acquired in different ways. Among the informants interviewed, 79.8% reported that they acquired knowledge through family lines, while the remaining (20.2%) confirmed that they acquired knowledge through observation (10.8%), mentorship with other traditional medicine practitioners (3.5%), experimentation (3.5%), and friends (2.4%).
Medicinal Plant Knowledge Comparison Between Different Social Groups
Interview data analyses showed that a significantly (p < 0.05) higher mean number of medicinal plants (6.52944 ± 0.1041) was reported by older informants (age > 60 years) compared to youngsters (20–40 years of age) (1.833 ± 0.1931) and those between the ages of 41–60 years (2.69603± 0.18031). Similarly, significantly (p < 0.05) higher mean numbers of medicinal plants were reported by illiterate (5.296 ± 3.0703) and traditional medicine practitioners (8.9058 ± 3.620) as compared with that of literate (3.6234 ± 3.122) and general informants (3.389 ± 1.661) (Table 10), respectively. But, there was no significant difference (p = 0.8789) between the mean numbers of medicinal plants reported by male (4.638 ± 3.252) and female (4.0714 ± 2.355) respondents.
Table 10.
Comparison of medicinal plant knowledge among different groups of informants
| Demographic Features | Categories | No. | No. of Plants Reported (Mean ± SD) | P-value |
|---|---|---|---|---|
| Gender | male | 360 | 4.638 ± 3.252 | 0.8789 |
| female | 28 | 4.0714 ± 2.355 | ||
| Age | 20–40 | 86 | 1.833 ± 0.1931 | |
| 41–60 | 210 | 2.69603± 0.18031 | ||
| 61–86 | 92 | 6.52944±0.1041 | 0.0001 | |
| Education | Illiterate | 226 | 5.296 ± 3.0703 | 0.0001 |
| Literate | 162 | 3.6234 ± 3.122 | ||
| Experience | Traditional medicine practitioners | 84 | 8.9058 ± 3.620 | 0.0001 |
| General informants | 304 | 3.389 ± 1.661 |
Threats to Medicinal Plants and Conservation Practices
Agricultural expansion and deforestation are commonly cited threats to medicinal plants as reported by 91% and 80% of the informants, respectively. Other stated threats included drought (8%), timber and firewood production (11%), overexploitation (4%), and exotic species plantations (3%). The preference ranking exercise conducted by the informants also ranked agricultural expansion and deforestation as the major and leading threats (Table 11).
Table 11.
Ranking of commonly reported threats against medicinal plants in the study area
| Major Treats | Informants Labelled K1 to K10 | Total Score | Rank | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| K1 | K2 | K3 | K4 | K5 | K6 | K7 | K8 | K9 | K10 | |||
| Deforestation | 4 | 5 | 4 | 4 | 4 | 5 | 5 | 3 | 5 | 4 | 43 | 2 |
| Agricultural expansion | 5 | 5 | 4 | 5 | 5 | 4 | 5 | 5 | 4 | 5 | 47 | 1 |
| Timber & firewood making | 4 | 3 | 3 | 4 | 5 | 4 | 5 | 3 | 4 | 5 | 40 | 3 |
| Plantation of exotic species | 1 | 2 | 2 | 3 | 4 | 2 | 1 | 2 | 3 | 1 | 20 | 5 |
| Over exploitation | 2 | 4 | 3 | 3 | 3 | 2 | 2 | 1 | 2 | 2 | 24 | 4 |
Medicinal plant conservation practices in the study area were poor. Only a few informants (13%) reported the cultivation of medicinal plants, including Achyranthes aspera, Asparagus africanus, Ocimum lamiifolium, Rumex nepalensis, Ruta chalepensis, Withania somnifera and Aloe sp. in homestead gardens.
Ranking of Threatened Medicinal Plants
Preference ranking exercise, carried out on six threatened medicinal plants based on the interview results, revealed Hagenia abyssinica as the most threatened medicinal plant, followed by Juniperus procera and Podocarpus falcatus (Table 12).
Table 12.
Ranking of medicinal plants reported as threatened in the study district
| Medicinal Plants List | Informants Coded A-J | Total Score | Rank | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | |||
| Hagenia abyssinica | 5 | 4 | 5 | 5 | 4 | 5 | 4 | 5 | 5 | 5 | 47 | 1 |
| Juniperus procera | 5 | 5 | 4 | 4 | 5 | 4 | 3 | 5 | 5 | 5 | 45 | 2 |
| Podocarpus falcatus | 5 | 4 | 5 | 4 | 4 | 5 | 3 | 4 | 4 | 5 | 44 | 3 |
| Asparagus africanus | 4 | 5 | 5 | 5 | 3 | 4 | 3 | 3 | 5 | 2 | 43 | 4 |
| Withania somnifera | 5 | 5 | 2 | 4 | 4 | 5 | 5 | 3 | 3 | 4 | 40 | 5 |
| Cordia africana | 4 | 2 | 4 | 5 | 3 | 4 | 2 | 5 | 4 | 4 | 37 | 6 |
| Croton macrostachyus | 3 | 2 | 2 | 1 | 3 | 2 | 1 | 3 | 1 | 1 | 19 | 7 |
Discussion
The findings of this study showed the high dependence of the people in the Kofale District of West-Arsi Zone on traditional herbal medicine in their day-to-day primary healthcare needs, as demonstrated by the high number of medicinal plant species reported by informants. In Kofale District, 106 medicinal plant species have been claimed to be used to manage both human and livestock ailments, which is a higher number than that reported for other districts in the country. Studies by Tolossa et al,20 Ashagre and Molla,158 Yineger et al,71 and Gijan and Dalle28 reported the use of 91, 98, 101, and 102 medicinal plants, respectively. The utilization of a relatively high number of medicinal plants in the study district may be linked to people’s restricted access to modern healthcare facilities, cultural acceptability of medicinal plant-based treatments, and better vegetation cover in the area. All medicinal plants reported in the current study were found to have similar or different medicinal uses elsewhere in the country, as shown in Table 3. Of the total claimed medicinal plants, some were claimed to have been used elsewhere in the world for same or similar purpose, which include Asparagus africanus for treatment of tumor and cancer in Cote d’Ivoire,159 Calpurnia aurea as antidermatophytic in Kenya,160 Carissa spinarum against wound in India,161 Croton macrostachyus against cancer in India,162 Euclea schimperi against skin sores and rashes in Namibia,163 Ocimum gratissimum as analgesic in Nigeria,164 Physalis peruviana to treat gastro-intestinal tract disorders in Uganda,165 Podocarpus falcatus to treat cancer in China,166 Rumex abyssinicus to relieve stomachache in Africa,167 Syzygium guineense to treat stomachache in Mali168 and Verbascum sinaiticum against hepatitis in Egypt.169
The dominance of the families Asteraceae, Fabaceae, and Solanaceae in contributing high number of medicinal plants in the study district could be due linked to their diversity in species and/or richness in medically active constituents. Fabaceae and Asteraceae are among the dominant families in the Flora of Ethiopia and Eritrea in terms of species richness contributing 48650 and 440170 species, respectively. Studies conducted in other areas of country have also reported a high contribution of Asteraceae,74,125,171 Fabaceae14,161–163 and Solanaceae14 to the medicinal flora.
The majority of claimed medicinal plants was collected from the wild and semi-wild habitats is in accordance with the results of other studies conducted elsewhere in different parts of the country.23,38,67,74,81,135 The poor cultivation practice of medicinal plants in the district might be related to their easy accessibility in the wild.
This study also shown that shrubs were the most dominant medicinal flora in the study district, which might be because of their year-round availability, in contrast to trees that were exposed to selective cutting and herbs that blossom seasonally after the rainy season. The dominance of shrubby medicinal plants has been observed in other parts of the country.20,135,172
Leaves were the dominant plant parts employed in remedy preparations for the treatment of human and livestock ailments in the study district, which could be attributed to their perceived efficacy, accessibility, ease of harvesting, and simplicity of preparation. The common use of leaves in the preparation of remedies has also been reported in studies conducted elsewhere in the country.14,20,23,28,125 Harvesting leaves has been reported to have much less damaging effects on the mother plant as compared to other parts such as roots and barks, the gathering of which could seriously affect the existence of individual plants.24,135
Different techniques were employed in the preparation of remedies in the district, with the crushing method taking the lead, which is in agreement with the results of previous studies conducted elsewhere in the country.21,27 Moreover, the finding related to the condition of the plants used for preparation indicated that the majority of remedies were made from fresh plant parts, which is in agreement with the results of studies carried out elsewhere in the country.173,174 Fresh materials retain volatile bioactive compounds, such as essential oils, which may be lost upon drying.
Oral was the most popular route of remedy administration which could be due to the reason that it creates favorable environmental condition for quick physiological reaction of the preparation against the pathogens and by so doing boosts its healing power.20 Oral administration has an additional advantage in that it allows the traditional medicine practitioners to reverse complication that might happen on the clients during treatment using antidotes. Other ethnobotanical studies conducted elsewhere in Ethiopia also reported oral administration as a common route of remedy application.12,14,16,20,27,175
Skin-related and gastrointestinal tract diseases had the highest ICF values, which might imply better consensus among informants in the study district regarding the selection of plants used to manage such diseases.176,177
Of the medicinal plants employed to treat human health problems, Justicia schimperiana, Embelia schimperi, Olinia rochetiana and Euclea schimperi which were used to treat liver disorders, tapeworm infection, general gastrointestinal complaints, and skin diseases, respectively, scored the highest FL and ROP values, which are measures of therapeutic potential.35 Justicia schimperiana was reported to have shown antioxidant,178 lousicidal and acaricidal,179 anticancer180 and antimalarial181 activities. Crude extracts of Embelia schimperi exhibited anthelmintic182 and antioxidant properties.183 Investigation reported the antibacterial,184 antidiarrheal185 and anti-inflammatory186 activities of Olinia rochetiana. Leaf extracts of Euclea schimperi demonstrated antioxidant and antibacterial activities.187 Generally, there is a higher consensus among informants in the study district regarding the selection of medicinal plants for the treatment of skin infections and gastrointestinal complaints, as revealed by the highest informant consensus factor (ICF) values scored by the two disease categories, which again is a sign of their better healing potential. Similar medicinal uses of these plants have been widely reported in different parts of the country.14,17,25,54,71,86,88,98,188 Among the medicinal plants claimed to manage livestock health problems, Ekebergia capensis and Datura stramonium which are used against babesiosis and rabies, respectively, scored the highest FL and ROP values. Previous studies have also reported the anti-infectious properties.28,81
Data analysis revealed that older, illiterate, and key informants in the study district reported significantly higher mean numbers of medicinal plants than that reported by the young, literate, and general informants, respectively. The fact that the younger generation had less medicinal plant knowledge compared to the older generation could be due to the reason that the former are more prone to acculturation and modernization and thus are more reluctant to learn and practice traditional medicine. Studies conducted in other areas of the country also reported that older people have better knowledge of medicinal plants than younger people.21,74,175 The reason that key informants had better knowledge of medicinal plants in the study district compared to general informants is also in agreement with the findings of previous studies conducted elsewhere in the country.26,189 The fact that literate informants in the district had less knowledge of medicinal plants than illiterate ones could be attributed to the influence of modern education. A study conducted in other areas of the country reported similar results.118
Agricultural expansion and deforestation were identified as major threats to the survival of medicinal plants in the district. Research carried out elsewhere in the country also revealed that agricultural expansion and deforestation are main threats to medicinal plants.28,60,94,190
Conclusion
The diversity of reported medicinal plants (106 species) employed to manage human and livestock disorders is indicative of plant-related rich knowledge of traditional medicine practices in the Kofale district. Leaves have been reported to be the most commonly utilized plant part in the preparation of remedies for the treatment of various ailments. Skin and gastrointestinal disorders were the major disease categories, with the highest ICF values. Medicinal plants, including Euclea schimperi, Olinia rochetiana, Embelia schimperi, and Justicia schimperiana, were the ones having the highest FL and ROP values for their use in the treatment of skin diseases, general gastrointestinal complaints, tapeworm infections, and liver disorders. Different scientific investigations also revealed the bioactivity of these plants against a number of aetiological agents. Comparative studies conducted on sociodemographic factors in the district revealed that older, illiterate, and key informants had better knowledge of the use of medicinal plants for the treatment of various human and livestock diseases than younger, literate, and general informants, respectively. In future phytochemical and pharmacological investigations, priority needs to be given to medicinal plants that scored the highest FL and ROP values and those plants that were used to treat disease categories with the highest ICF values.
Acknowledgments
We are thank the residents of Kofale District, particularly the informants, for sharing their accumulated indigenous knowledge and use of medicinal plants. Our gratitude also goes to the Healthcare, Agricultural, and Biodiversity Conservation offices of Kofale District for their cooperation in facilitating this study. We are grateful to Addis Ababa University for its financial support to conduct this investigation.
Funding Statement
This study was sponsored by the School of Graduate Studies of Addis Ababa University and the Office of the Vice President for Research and Technology Transfer of Addis Ababa University (grant number TR/003/2021). We confirm that the information is accurate and the grant number is correct.
Data Sharing Statement
Data concerning this study were kept on a desktop computer at the Aklilu Lemma Institute of Pathobiology (ALIPB), Addis Ababa University (AAU). Readers may get access to the data through requests made to ALIPB. Plant voucher specimens were stored at the mini-herbarium of the Endod and Other Medicinal Plants Research Unit (ALIPB, AAU).
Ethical Consideration
The study proposal was evaluated and approved by the Ethical Review Committee of the Aklilu Lemma Institute of Pathobiology at the Addis Ababa University. Permissions were granted by the zone, district, and kebele administrations to conduct the fieldwork. Verbal consent was obtained from the study participants, which was also approved by the Review Committee. We confirm that our study complies with the Declaration of Helsinki.191
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization. The World Health Report 2000: Health Systems: Improving Performance. World Health Organization; 2000. [Google Scholar]
- 2.Muzammil S, Neves Cruz J, Mumtaz R, et al. Effects of drying temperature and solvents on in vitro diabetic wound healing potential of Moringa oleifera leaf extracts. Molecules. 2023;28(2):710. doi: 10.3390/molecules28020710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah NA, Khan MR, Nadhman A. Antileishmanial, toxicity, and phytochemical evaluation of medicinal plants collected from Pakistan. Biomed Res Int. 2014;2014:1–7. doi: 10.1155/2014/384204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balunas MJ, Kinghorn AD. Drug discovery from medicinal plants. Life Sci. 2005;78(5):431–441. doi: 10.1016/j.lfs.2005.09.012 [DOI] [PubMed] [Google Scholar]
- 5.Alves FS, Cruz JN, de Farias Ramos IN, Do Nascimento Brandão DL, Queiroz RN. Evaluation of antimicrobial activity and cytotoxicity effects of extracts of piper nigrum L. and piperine. Separations. 2022;10(1):21. doi: 10.3390/separations10010021 [DOI] [Google Scholar]
- 6.da Silva DF, de Souza JL, da Costa DM, et al. Antiplasmodial activity of coumarins isolated from Polygala boliviensis: in vitro and in silico studies. J Biomol Struct Dyn. 2023;27:1–21. [DOI] [PubMed] [Google Scholar]
- 7.Shahane K, Kshirsagar M, Tambe S, et al. An Updated Review on the Multifaceted Therapeutic Potential of Calendula officinalis L. Pharmaceuticals. 2023;16(4):611. doi: 10.3390/ph16040611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abebe D, Ayehu A. Medicinal Plants and Enigmatic Health Practices of Northern Ethiopia. Addis Ababa: B.S.P.E; 1993. [Google Scholar]
- 9.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, International Agency for Research on Cancer, World Health Organization. Some Traditional Herbal Medicines, Some Mycotoxins, Naphthalene and Styrene. Vol. 82. Lyon: World Health Organization; 2002. [PMC free article] [PubMed] [Google Scholar]
- 10.Tesfahuneygn G, Gebreegziabher G. Medicinal plants used in traditional medicine by Ethiopians: a review article. J Respir Med Lung Dis. 2019;4:1–3. [Google Scholar]
- 11.Teklehaymanot T, Giday M. Ethnobotanical study of wild edible plants of Kara and Kwego semi-pastoralist people in Lower Omo River Valley, Debub Omo Zone, SNNPR, Ethiopia. J Ethnobiol Ethnomed. 2010;6(1):23. doi: 10.1186/1746-4269-6-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lulekal E, Asfaw Z, Kelbessa E, Van Damme P. Ethnomedicinal study of plants used for human ailments in Ankober District, North Shewa Zone, Amhara region, Ethiopia. J Ethnobiol Ethnomed. 2013;9(1):63. doi: 10.1186/1746-4269-9-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sen T, Samanta SK. Medicinal plants, human health and biodiversity: a broad review. Adv Biochem Eng Biotechnol. 2015;147:59–110. doi: 10.1007/10_2014_273 [DOI] [PubMed] [Google Scholar]
- 14.Giday M, Ameni G. An ethnobotanical survey of plants of veterinary importance in two woredas of Southern Tigray, Northern Ethiopia. SINET: Ethiop J Sci. 2003;26:123–136. [Google Scholar]
- 15.Awas T, Demissew S Ethnobotanical study of medicinal plants in Kafficho people, southwestern Ethiopia. In Proceedings of the 16th International Conference of Ethiopian Studies; 2009. Vol. 3, pp. 711–726. Trondheim, Norway: NTNU-Trykk Press. [Google Scholar]
- 16.Mesfin F, Demissew S, Teklehaymanot T. An ethnobotanical study of medicinal plants in Wonago Woreda, SNNPR, Ethiopia. J Ethnobiol Ethnomed. 2009;5(1):28. doi: 10.1186/1746-4269-5-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teklehaymanot T. Ethnobotanical study of knowledge and medicinal plants use by the people in Dek Island in Ethiopia. J Ethnopharmacol. 2009;124(1):69–78. doi: 10.1016/j.jep.2009.04.005 [DOI] [PubMed] [Google Scholar]
- 18.Belayneh A, Asfaw Z, Demissew S, Bussa NF. Medicinal plants potential and use by pastoral and agro-pastoral communities in Erer Valley of Babile Wereda, Eastern Ethiopia. J Ethnobiol Ethnomed. 2012;8(1):42. doi: 10.1186/1746-4269-8-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agize M, Demissew S, Asfaw Z. Ethnobotany of medicinal plants in Loma and Gena bosa districts (woredas) of dawro zone, southern Ethiopia. Topclass J Herb Med. 2013;2:194–212. [Google Scholar]
- 20.Tolossa K, Debela E, Athanasiadou S, Tolera A, Ganga G, Houdijk JG. Ethno-medicinal study of plants used for treatment of human and livestock ailments by traditional healers in South Omo, Southern Ethiopia. J Ethnobiol Ethnomed. 2013;9(1):32. doi: 10.1186/1746-4269-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chekole G, Asfaw Z, Kelbessa E. Ethnobotanical study of medicinal plants in the environs of Tara-gedam and Amba remnant forests of Libo Kemkem District, northwest Ethiopia. J Ethnobiol Ethnomed. 2015;11(1):4. doi: 10.1186/1746-4269-11-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yohannis SW, Asfaw Z, Kelbessa E. Ethnobotanical study of medicinal plants used by local people in Menz Gera Midir District, North Shewa Zone, Amhara Regional State, Ethiopia. J Med Plants Research. 2018;12(21):296–314. doi: 10.5897/JMPR2018.6616 [DOI] [Google Scholar]
- 23.Kassa Z, Asfaw Z, Demissew S. An ethnobotanical study of medicinal plants in Sheka Zone of Southern Nations, Nationalities and Peoples Regional State, Ethiopia. J Ethnobiol Ethnomed. 2020;16(1):7. doi: 10.1186/s13002-020-0358-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teka A, Asfaw Z, Demissew S, Van Damme P. Traditional uses of medicinal plants practiced by the indigenous communities in Gurage Zone, south central Ethiopia. Ethnobot Res Appl. 2020;19:41. [Google Scholar]
- 25.Eshete MA, Molla EL. Cultural significance of medicinal plants in healing human ailments among Guji semi-pastoralist people, Suro Barguda District, Ethiopia. J Ethnobiol Ethnomed. 2021;17(1):61. doi: 10.1186/s13002-021-00487-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Woldemariam G, Demissew S, Asfaw Z. An ethnobotanical study of traditional medicinal plants used for human ailments in Yem ethnic group, south Ethiopia. Ethnobot Res Appl. 2021;22:08. [Google Scholar]
- 27.Bekele M, Woldeyes F, Lulekal E, Bekele T, Demissew S. Ethnobotanical investigation of medicinal plants in Buska Mountain range, Hamar district, Southwestern Ethiopia. J Ethnobiol Ethnomed. 2022;18(1):60. doi: 10.1186/s13002-022-00558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gijan M, Dalle M. Ethnobotanical study of medicinal plants in Nagelle Arsi district, West Arsi zone of Oromia, Ethiopia. J Nat Sci Res. 2019;9:13. [Google Scholar]
- 29.Girma Z, Abdela G, Awas T. Ethnobotanical study of medicinal plant species in Nensebo District, south-eastern Ethiopia. Ethnobot Res Appl. 2022;24:6. [Google Scholar]
- 30.Population Census Commission (PCC). Summary and Statistical Report of the 2007 Population and Housing Census. Population Census Commission (PCC), Federal Democratic Republic of Ethiopia: Addis Ababa. 2008. [Google Scholar]
- 31.Cochran WG. Sampling Techniques. New York: John Wiley & Sons; 1977. [Google Scholar]
- 32.Martin GJ. Ethnobotany: A Method Manual. London: Chapman and Hall; 1995. [Google Scholar]
- 33.Cotton CM. Ethnobotany: Principles and Applications. Chichester: John Wiley & Sons; 1996. [Google Scholar]
- 34.Alexiades MN. Collecting ethnobotanical data: an introduction to basic concepts and techniques. In: Alexiades MN, editor. Selected Guidelines for Ethnobotanical Research: A Field Manual. The New York Botanical Garden. 1996:53–94. [Google Scholar]
- 35.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J Ethnopharmacol. 1986;16(2–3):275–287. doi: 10.1016/0378-8741(86)90094-2 [DOI] [PubMed] [Google Scholar]
- 36.Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: healers’ consensus and cultural importance. Soc Sci Med. 1998;47(11):1859–1871. doi: 10.1016/S0277-9536(98)00181-6 [DOI] [PubMed] [Google Scholar]
- 37.Ali-Shtayeh MS, Jamous RM, Jamous RM. Traditional Arabic Palestinian ethnoveterinary practices in animal health care: a field survey in the West Bank (Palestine). J Ethnopharmacol. 2016;182:35–49. doi: 10.1016/j.jep.2016.02.005 [DOI] [PubMed] [Google Scholar]
- 38.Tadesse A, Kagnew B, Kebede F, Kebede M. Ethnobotanical study of medicinal plants used to treat human ailment in Guduru District of Oromia Regional State, Ethiopia. J Pharmacogn Phytother. 2018;10(3):64–75. doi: 10.5897/JPP2018.0496 [DOI] [Google Scholar]
- 39.Tesfaye S, Braun H, Asres K, et al. Ethiopian Medicinal Plants traditionally used for the treatment of cancer; Part 3: selective cytotoxic activity of 22 Plants against human cancer Cell Lines. Molecules. 2021;26(12):3658. doi: 10.3390/molecules26123658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seid MA, Aydagnehum SG. Medicinal plants biodiversity and local healthcare management system in Chencha district; Gamo Gofa, Ethiopia. J Pharmacogn Phytochem. 2013;2:284–293. [Google Scholar]
- 41.Megersa M, Jima TT, Goro KK. The use of medicinal plants for the treatment of toothache in Ethiopia. Evid Based Complement Altern Med. 2019;2019:1–16. doi: 10.1155/2019/2645174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bitew H, Gebregergs H, Tuem KB, Yeshak MY. Ethiopian medicinal plants traditionally used for wound treatment: a systematic review. Ethiop J Health Dev. 2019;33:102–127. [Google Scholar]
- 43.Nibret E, Wink M. Trypanocidal and cytotoxic effects of 30 Ethiopian medicinal plants. Z Naturforsch C J Biosci. 2011;66(11–12):541–546. doi: 10.1515/znc-2011-11-1202 [DOI] [PubMed] [Google Scholar]
- 44.Eguale T, Tadesse D, Giday M. In vitro anthelmintic activity of crude extracts of five medicinal plants against egg-hatching and larval development of Haemonchus contortus. J Ethnopharmacol. 2011;137(1):108–113. doi: 10.1016/j.jep.2011.04.063 [DOI] [PubMed] [Google Scholar]
- 45.Bacha K, Tariku Y, Gebreyesus F, et al. Antimicrobial and anti-Quorum Sensing activities of selected medicinal plants of Ethiopia: implication for development of potent antimicrobial agents. BMC Microbiol. 2016;16(1):139. doi: 10.1186/s12866-016-0765-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fufa MF, Deressa F, Deyou T, Abdisa N. Isolation and characterization of compounds from the leaves of Melia azedarach and stem bark of Albizia schimperiana and evaluation for antimicrobial activities. Med Chem (Los Angeles). 2018;8:154–165. [Google Scholar]
- 47.Belayneh A, Demissew S, Bussa NF, Bisrat D. Ethno-medicinal and bio-cultural importance of aloes from south and east of the Great Rift Valley floristic regions of Ethiopia. Heliyon. 2020;6(6):e04344. doi: 10.1016/j.heliyon.2020.e04344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nigussie G, Wale M. Medicinal plants used in traditional treatment of malaria in Ethiopia: a review of ethnomedicine, anti-malarial and toxicity studies. Malar J. 2022;21(1):262. doi: 10.1186/s12936-022-04264-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Addis G, Urga K, Dikasso D. Ethnobotanical study of edible wild plants in some selected districts of Ethiopia. Human Ecolo. 2005;33(1):83–118. doi: 10.1007/s10745-005-1656-0 [DOI] [Google Scholar]
- 50.Thulin M. Fabaceae. In: Hedberg I, Edwards S, editors. Flora of Ethiopia and Eritrea. Volume 3: Pittosporaceae to Araliaceae. The National Herbarium, Addis Ababa University, Addis Ababa; 1989:49–251. [Google Scholar]
- 51.Dikasso D, Makonnen E, Debella A, et al. In vivo anti-malarial activity of hydroalcoholic extracts from Asparagus africanus Lam. in mice infected with Plasmodium berghei. Ethiop J Health Dev. 2006;20:112–118. [Google Scholar]
- 52.Asmerom D, Kalay TH, Araya TY, Desta DM, Wondafrash DZ, Tafere GG. Medicinal plants used for the treatment of erectile dysfunction in Ethiopia: a systematic review. BioMed Res Int. 2021;2021:1–12. doi: 10.1155/2021/6656406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yared D, Mekonnen Y, Debella A. In vivo antimalarial activities of fractionated extracts of Asparagus africanus in mice infected with Plasmodium berghei. Pharmacologyonline. 2012;3:88–94. [Google Scholar]
- 54.Asres K, Bucar F, Kartnig T, Witvrouw M, Pannecouque C, De Clercq E. Antiviral activity against human immunodeficiency virus type 1 (HIV‐1) and type 2 (HIV‐2) of ethnobotanically selected Ethiopian medicinal plants. Phytother Res. 2001;15(1):62–69. doi: [DOI] [PubMed] [Google Scholar]
- 55.Kifle ZD, Abdelwuhab M, Melak AD, Meseret T, Adugna M, Adugna M. Pharmacological evaluation of medicinal plants with antidiabetic activities in Ethiopia: a review. Metabol Open. 2022;13:100174. doi: 10.1016/j.metop.2022.100174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kifle ZD, Anteneh DA, Atnafie SA. Hypoglycemic, anti-hyperglycemic and anti-hyperlipidemic affects of Bersama abyssinica fresen (melianthaceae) leaves’ solvent fractions in normoglycemic and streptozotocin-induced diabetic mice. J Exp Pharmacol. 2020;12:385–396. doi: 10.2147/JEP.S273959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ayalew M, Bekele A, Mengistie MG, Atnafie SA. Evaluation of the antidiarrheal activity of 80% methanol extract and solvent fractions of the leaf of Bersama abyssinica fresen (Melianthaceae) in mice. BMC Complement Med Ther. 2022;22(1):8. doi: 10.1186/s12906-021-03498-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zewdie KA, Bhoumik D, Wondafrash DZ, Tuem KB. Evaluation of in-vivo antidiarrhoeal and in-vitro antibacterial activities of the root extract of Brucea antidysenterica JF Mill (Simaroubaceae). BMC Complement Med Ther. 2020;20(1):201. doi: 10.1186/s12906-020-03001-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ragunathan M, Solomon M. The study of spiritual remedies in orthodox rural churches and traditional medicinal practice in Gondar Zuria district, Northwestern Ethiopia. Pharmacogn J. 2009;1. [Google Scholar]
- 60.Bogale M, Sasikumar JM, Egigu MC. An ethnomedicinal study in tulo district, west hararghe zone, Oromia region, Ethiopia. Heliyon. 2023;9(4):e15361. doi: 10.1016/j.heliyon.2023.e15361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Birhanu Z, Wuhab MA, Abula T. Antimalarial activity of Calpurnia aurea hydro alcoholic leaf extract in mice infected with Plasmodium berghei. Pharmacologyonline. 2015;2:73–79. [Google Scholar]
- 62.Feyisa M, Kassahun A, Giday M. Medicinal Plants Used in Ethno veterinary Practices in Adea Berga District, Oromia Region of Ethiopia. Evid Based Complement Altern Med. 2021;2021:1–22. doi: 10.1155/2021/5641479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Berhanu M, Tintagu T, Fentahun S, Giday M. Research Article Ethnoveterinary Survey of Medicinal Plants Used for Treatment of Animal Diseases in Ambo District of Oromia Regional State of Ethiopia. Evid Based Complement Altern Med. 2020;2020:1–12. doi: 10.1155/2020/8816227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Suleman S, Tufa TB, Kebebe D, et a. Treatment of malaria and related symptoms using traditional herbal medicine in Ethiopia. J Ethnopharmacol. 2018;213:262–279. doi: 10.1016/j.jep.2017.10.034 [DOI] [PubMed] [Google Scholar]
- 65.Giday M, Teklehaymanot T, Animut A, Mekonnen Y. Medicinal plants of the Shinasha, Agew-awi and Amhara peoples in northwest Ethiopia. J Ethnopharmacol. 2007;110(3):516–525. doi: 10.1016/j.jep.2006.10.011 [DOI] [PubMed] [Google Scholar]
- 66.Assefa B, Megersa M, Jima TT. Ethnobotanical study of medicinal plants used to treat human diseases in Gura Damole District, Bale Zone, and Southeast Ethiopia. Asian J Ethnobiol. 2021;4(1):42–52. doi: 10.13057/asianjethnobiol/y040105 [DOI] [Google Scholar]
- 67.Mesfin F, Seta T, Assefa A. An ethnobotanical study of medicinal plants in Amaro Woreda, Ethiopia. Ethnobot Res Appl. 2014;12:341–354. doi: 10.17348/era.12.0.341-354 [DOI] [Google Scholar]
- 68.Saka A, Tesfaye JL, Gudata L, et al. Synthesis, characterization, and antibacterial activity of ZnO nanoparticles from fresh leaf extracts of Apocynaceae, Carissa spinarum L.(Hagamsa). J Nanomater. 2022;2022:1–6. doi: 10.1155/2022/6230298 [DOI] [Google Scholar]
- 69.Nedi T, Mekonnen N, Urga K. Diuretic effect of the crude extracts of Carissa edulis in rats. J Ethnopharmacol. 2004;95(1):57–61. doi: 10.1016/j.jep.2004.06.017 [DOI] [PubMed] [Google Scholar]
- 70.Khalil OS, Ismail HA, Elkot WF. Physicochemical, functional and sensory properties of probiotic yoghurt flavored with white sapote fruit (Casimiroa edulis). J Food Sci Technol. 2022;59(9):3700–3710. doi: 10.1007/s13197-022-05393-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yineger H, Kelbessa E, Bekele T, Lulekal E. Plants used in traditional management of human ailments at Bale Mountains National Park, Southeastern Ethiopia. J Med Plant Res. 2008;2:132–153. [Google Scholar]
- 72.Mekonnen AG, Gebeyehu BT, Woldearegay M. Experience of patients with breast cancer with traditional treatment and healers’ understanding of causes and manifestations of breast cancer in North Shewa zone, Ethiopia: a phenomenological study. BMJ open. 2022;12(12):e063726. doi: 10.1136/bmjopen-2022-063726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yineger H, Kelbessa E, Bekele T, Lulekal E. Ethnoveterinary medicinal plants at Bale Mountains National Park, Ethiopia. J Ethnopharmacol. 2007;112(1):55–70. doi: 10.1016/j.jep.2007.02.001 [DOI] [PubMed] [Google Scholar]
- 74.Giday M, Asfaw Z, Woldu Z. Medicinal plants of the Meinit ethnic group of Ethiopia: an ethnobotanical study. J Ethnopharmacol. 2009;124(3):513–521. doi: 10.1016/j.jep.2009.05.009 [DOI] [PubMed] [Google Scholar]
- 75.Woldeab B, Regassa R, Alemu T, Megersa M. Medicinal plants used for treatment of diarrhoeal related diseases in Ethiopia. Evid Based Complement Altern Med. 2018;2018:1–20. doi: 10.1155/2018/4630371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Issa M, Chandel S, Singh HP, et al. Appraisal of phytotoxic, cytotoxic and genotoxic potential of essential oil of a medicinal plant Vitex negundo. Ind Crops Prod. 2020;145:112083. doi: 10.1016/j.indcrop.2019.112083 [DOI] [Google Scholar]
- 77.Asfaw A, Lulekal E, Bekele T, Debella A, Debebe E, Sisay B. Medicinal plants used to treat livestock ailments in Ensaro District, North Shewa Zone, Amhara Regional State, Ethiopia. BMC Vet Res. 2022;18(1):235. doi: 10.1186/s12917-022-03320-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Osman A, Sbhatu DB, Giday M. Medicinal plants used to manage human and livestock ailments in Raya Kobo District of Amhara Regional State, Ethiopia. Evid Based Complement Altern Med. 2020;2020:1–19. doi: 10.1155/2020/1329170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Getachew S, Medhin G, Asres A, Abebe G, Ameni G. Traditional medicinal plants used in the treatment of tuberculosis in Ethiopia: a systematic review. Heliyon. 2022;8(5):e09478. doi: 10.1016/j.heliyon.2022.e09478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Taye B, Giday M, Animut A, Seid J. Antibacterial activities of selected medicinal plants in traditional treatment of human wounds in Ethiopia. Asian Pac J Trop Biomed. 2011;5(5):370–375. doi: 10.1016/S2221-1691(11)60082-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yirga G. Assessment of traditional medicinal plants in Endrta district, south-eastern Tigray, northern Ethiopia. Afr J Plant Sci. 2010;4:255–260. [Google Scholar]
- 82.Yirga G, Teferi M, Kasaye M. Survey of medicinal plants used to treat human ailments in Hawzen district, Northern Ethiopia. Int J Biodivers Conserv. 2011;3:709–714. [Google Scholar]
- 83.Fentahun M, Ayele Y, Amsalu N, Alemayehu A, Amsalu G. Antibacterial evaluation and phytochemical analysis of selected medicinal plants against some pathogenic enteric bacteria in Gozamin District, Ethiopia. J Pharmacovigil. 2017;5:5. [Google Scholar]
- 84.Getaneh S, Girma Z. An ethnobotanical study of medicinal plants in Debre Libanos Wereda, Central Ethiopia. Afr J Plant Sci. 2014;8(7):366–379. doi: 10.5897/AJPS2013.1041 [DOI] [Google Scholar]
- 85.Kewessa G, Abebe T, Demessie A. Indigenous knowledge on the use and management of medicinal trees and shrubs in Dale District, Sidama Zone, Southern Ethiopia. Ethnobot Res Appl. 2015;14:171–182. doi: 10.17348/era.14.0.171-182 [DOI] [Google Scholar]
- 86.Debebe Y, Tefera M, Mekonnen W, et al. Evaluation of anthelmintic potential of the Ethiopian medicinal plant Embelia schimperi Vatke in vivo and in vitro against some intestinal parasites. BMC Complement Altern Med. 2015;15(1):187. doi: 10.1186/s12906-015-0711-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lulekal E, Rondevaldova J, Bernaskova E, et al. Antimicrobial activity of traditional medicinal plants from Ankober district, north Shewa Zone, Amhara region, Ethiopia. Pharm Biol. 2014;52(5):614–620. doi: 10.3109/13880209.2013.858362 [DOI] [PubMed] [Google Scholar]
- 88.Animaw Z, Asres K, Tadesse S, et al. Teratogenic evaluation of 80% ethanol extract of Embelia schimperi vatke fruits on rat embryo and fetuses. J Toxicol. 2022;2022:1–12. doi: 10.1155/2022/4310521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Usman KA, Egigu MC, Mahalingam JS. Ethnobotanical study on traditional medicinal plants used by Oromo ethnic people of Goro district, Bale zone of Oromia region, Ethiopia. Ethnobot Res Appl. 2022;24:1–21. [Google Scholar]
- 90.Fadipe LA, Yaro AH, Haruna AK, Ilyas M. Anticonvulsant activity of the methanolic extract of Entada abyssinica Steud. Ex a Rich Biol Environ Sci J Trop. 2007;5:76–80. [Google Scholar]
- 91.Aerts R, November EJ, Rayyan M. Improvised Hand Injury Treatment Using Traditional Veterinary Medicine in Ethiopia. Wilderness & Environm Med. 2017;28(4):322–326. doi: 10.1016/j.wem.2017.06.012 [DOI] [PubMed] [Google Scholar]
- 92.Seifu T, Mehari B, Atlabachew M, Chandravanshi B. Polyphenolic content and antioxidant activity of leaves of Urtica simensis grown in Ethiopia. Lat Am Appl Res. 2017;47:35–40. [Google Scholar]
- 93.Gemechu A, Giday M, Worku A, Ameni G. In vitro anti-mycobacterial activity of selected medicinal plants against Mycobacterium tuberculosis and Mycobacterium bovis strains. BMC Complement Altern Med. 2013;13(1):291. doi: 10.1186/1472-6882-13-291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tefera BN, Kim YD. Ethnobotanical study of medicinal plants in the Hawassa Zuria District, Sidama zone, Southern Ethiopia. J Ethnobiol Ethnomed. 2019;15(1):25. doi: 10.1186/s13002-019-0302-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Alemayehu G, Asfaw Z, Kelbessa E. Ethnobotanical study of medicinal plants used by local communities of Minjar-Shenkora District, North Shewa Zone of Amhara Region, Ethiopia. J Med Plants Stud. 2015;3:01–11. [Google Scholar]
- 96.Gebre T, Addis G, Lemma H, et al. In-vitro antibacterial activity of Cymbopogon citratus (DC.) Stapf. and Eucalyptus globulus Labill. Ethiop J Public Health and Nutr. 2020;2. [Google Scholar]
- 97.Teka A, Maryo M. Ethiopian Medicinal Plants Used for Respiratory Tract Disorders: ethnomedicinal Review. Evid Based Complement Altern Med. 2023;2023:1–9. doi: 10.1155/2023/7612804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gebremariam T, Abula T, Gebremariam MG. Antibacterial and phytochemical screening of root extracts of Euclea racemosa subsp. schimperi. Int J Pharmacogn. 2015;2:66–70. [Google Scholar]
- 99.Tesfaye S, Tadesse S, Engidawork E, et al. Screening of Twenty-one Ethiopian Medicinal Plants for their Antiproliferative Activity against Human Acute Myeloid Leukemia (MV4-11) Cell Line. Ethiop Pharm J. 2019;35(2):143–148. doi: 10.4314/epj.v35i2.7 [DOI] [Google Scholar]
- 100.Gadisa E, Tadesse E. Antimicrobial activity of medicinal plants used for urinary tract infections in pastoralist community in Ethiopia. BMC Complement Med Ther. 2021;21(1):74. doi: 10.1186/s12906-021-03249-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Feyisa K, Feyisa W, Girma T, Kemal T. Traditional medicinal plants used for the treatment of urological and urogenital diseases in Ethiopia: a Review. Pharmacogn J. 2022;14. [Google Scholar]
- 102.Demie G, Negash M, Awas T. Ethnobotanical study of medicinal plants used by indigenous people in and around Dirre Sheikh Hussein heritage site of South-eastern Ethiopia. J Ethnopharmacol. 2018;220:87–93. doi: 10.1016/j.jep.2018.03.033 [DOI] [PubMed] [Google Scholar]
- 103.Girma Z, Abdela G, Awas T. Ethnobotanical study of medicinal plant species in Nensebo District, south-eastern Ethiopia. Ethnobot Res Appl. 2022;24:1–25. [Google Scholar]
- 104.Megersa M, Tamrat N. Medicinal plants used to treat human and livestock ailments in Basona Werana District, North Shewa Zone, Amhara region, Ethiopia. Evid Based Complement Altern Med. 2022;2022:1–18. doi: 10.1155/2022/5242033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Desalegn A, Egigu MC, Sasikumra JM. Ethnobotanical study on medicinal plants used by ethnic people of Gechi District, South West Oromia, Ethiopia. Nus Biosci. 2022;14(1):104–116. [Google Scholar]
- 106.Andualem D, Negesse T, Tolera A. Chemical composition, in vitro organic matter digestibility and kinetics of rumen dry matter degradability of morphological fractions of stinging nettle (Urtica simensis). Adv Biol Res. 2016;10:183–190. [Google Scholar]
- 107.Mekonnen A, Sidamo T, Asres K, Engidawork E. In vivo wound healing activity and phytochemical screening of the crude extract and various fractions of Kalanchoe petitiana A. Rich (Crassulaceae) leaves in mice. J Ethnopharmacol. 2013;145(2):638–646. doi: 10.1016/j.jep.2012.12.002 [DOI] [PubMed] [Google Scholar]
- 108.Birhan YS, Kitaw SL, Alemayehu YA, Mengesha NM. Ethnoveterinary medicinal plants and practices in Enarj Enawga district, East Gojjam zone, Amhara region, Ethiopia. Int J Anim Sci. 2018;2:1014. [Google Scholar]
- 109.Ayele TT. A review on traditionally used medicinal plants/herbs for cancer therapy in Ethiopia: current status, challenge and future perspectives. Org Chem Curr Res. 2018;7(02):2. doi: 10.4172/2161-0401.1000192 [DOI] [Google Scholar]
- 110.Makonnen E, Debella A, Abebe D, Teka F. Analgesic properties of some Ethiopian medicinal plants in different models of nociception in mice. Phytother Res. 2003;17(9):1108–1112. doi: 10.1002/ptr.1306 [DOI] [PubMed] [Google Scholar]
- 111.Fikadu Y, Yaya EE, Chandravanshi BS. Chemical composition and antioxidant activities of the essential oils of Lippia adoensis Hochst ex. Walp and Ocimum sanctum Linn. Bull Chem Soc Ethiop. 2022;36(1):95–108. doi: 10.4314/bcse.v36i1.9 [DOI] [Google Scholar]
- 112.Gemeda N, Woldeamanuel Y, Asrat D, Debella A, Belete Y. Assessment of Lippia adoensis Hochst. var. koseret, Rosmarinus officinalis L. and Ruta chalepensis L. essential oils as a potential source of fungitoxic and mycosporicidal activity against toxigenic Aspergillus species. Pharmacologyonline. 2015;2:85–94. [Google Scholar]
- 113.Degu S, Berihun A, Muluye R, et al. Medicinal plants that used as repellent, insecticide and larvicide in Ethiopia. Pharm Pharmacol Int J. 2020;8(5):274–283. doi: 10.15406/ppij.2020.08.00306 [DOI] [Google Scholar]
- 114.Buli GA, Duga AG, Dessalegn E. Antimicrobial activity of Lippia adoensis var. koseret against human pathogenic bacteria and fungi. Am J Clin Exp Med. 2015;3(3):118–123. doi: 10.11648/j.ajcem.20150303.18 [DOI] [Google Scholar]
- 115.Tekalign E, Tadege G, Fisseha N, Nureye D. Suppressive, Curative, and Prophylactic Effects of Maesa lanceolata Forssk. Against Rodent Malaria Parasite Plasmodium berghei. BioMed Res Int. 2022;2022:1–18. doi: 10.1155/2022/8901555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tadesse D, Eguale T, Giday M, Mussa A. Ovicidal and larvicidal activity of crude extracts of Maesa lanceolata and Plectranthus punctatus against Haemonchus contortus. J Ethnopharmacol. 2009;122(2):240–244. doi: 10.1016/j.jep.2009.01.014 [DOI] [PubMed] [Google Scholar]
- 117.Duresa LW, Manaye D. Phytochemical screening and antioxidant activity of selected Mango (Mangifera indica L.) and avocado (Persea Americana) fruits in Illu Ababor zone, Oromia Regional sSate, Ethiopia. Indo Am J Pharm Res. 2017;7:67. [Google Scholar]
- 118.Teklehaymanot T, Giday M, Medhin G, Mekonnen Y. Knowledge and use of medicinal plants by people around Debre Libanos monastery in Ethiopia. J Ethnopharmacol. 2007;111(2):271–283. doi: 10.1016/j.jep.2006.11.019 [DOI] [PubMed] [Google Scholar]
- 119.Fenta M, Kahaliw W. Evaluation of antimalarial activity of hydromethanolic crude extracts and solvent fractions of the leaves of Nuxia congesta R. Br. Ex Fresen (Buddlejaceae) in Plasmodium berghei infected mice. J Exp Pharmacol. 2019;11:121–134. doi: 10.2147/JEP.S230636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wubetu M, Sintayehu M, Aeta MA. Ethnobotany of medicinal plants used to treat various mental illnesses in Ethiopia: a systematic review. Asian J Plant Sci Res. 2018;8:9–33. [Google Scholar]
- 121.Desalegn A, Egigu M, sasikumar JM. Ethnobotanical study on medicinal plants used by ethnic people of Gechi District, South West Oromia, Ethiopia. Nus Biosci. 2022;14(1):104–116. doi: 10.13057/nusbiosci/n140113 [DOI] [Google Scholar]
- 122.Amuka O, Tarus PK, Machocho AK, Ruttoh EK. Plant Extracts as Solutions to Multi Drug Resistant, Indigofera homblei Bak. f and Martin, Fabaceae, a Plant used in Kenya against Microbial Related Conditions. Adv Tech Biol Med. 2015;3(03):2379. doi: 10.4172/2379-1764.1000140 [DOI] [Google Scholar]
- 123.Esser KB, Semagn K, Wolde-Yohannes L. Medicinal use and social status of the soap berry endod (Phytolacca dodecandra) in Ethiopia. J Ethnopharmacol. 2003;85(2–3):269–277. doi: 10.1016/S0378-8741(03)00007-2 [DOI] [PubMed] [Google Scholar]
- 124.Tuasha N, Petros B, Asfaw Z. Medicinal plants used by traditional healers to treat malignancies and other human ailments in Dalle District, Sidama Zone, Ethiopia. J Ethnobiol Ethnomed. 2018;14(1):15. doi: 10.1186/s13002-018-0213-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Agize M, Asfaw Z, Nemomissa S, Gebre T. Ethnobotany of traditional medicinal plants and associated indigenous knowledge in Dawuro Zone of Southwestern Ethiopia. J Ethnobiolo Ethnomed. 2022;18(1):48. doi: 10.1186/s13002-022-00546-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tekle Y. Medicinal plants in the ethno veterinary practices of Bensa woreda, Southern Ethiopia. Open Access Lib J. 2015;2:e1258. [Google Scholar]
- 127.Yeshiwas D, Mekonnen A. Comparative study of the antioxidant and antibacterial activities of two guava (Psidium guajava) fruit varieties cultivated in Andasa Horticulture Site, Ethiopia. Chem Int. 2018;4:154–162. [Google Scholar]
- 128.Gashe F, Belete A, Gebre-Mariam T. Evaluation of antimicrobial and anti-inflammatory activities and formulation studies on the leaf extracts of Psidium guajava L. Ethiop Pharm J. 2010;28:131–142. [Google Scholar]
- 129.Dilebo T, Feyissa T, Asfaw Z. In-vitro propagation of multi-use enset [Ensete ventricosum (Welw.) Cheesman] landraces using bulla as gelling agents. Plant Cell Tissue Organ Cult. 2023;155(3):693–708. doi: 10.1007/s11240-023-02590-8 [DOI] [Google Scholar]
- 130.Abew B, Sahile S, Moges F. In vitro antibacterial activity of leaf extracts of Zehneria scabra and Ricinus communis against Escherichia coli and methicillin resistance Staphylococcus aureus. Asian Pac J Trop Biomed. 2014;4(10):816–820. doi: 10.12980/APJTB.4.201414B16 [DOI] [Google Scholar]
- 131.Asressu KH, Tesema TK. Chemical and antimicrobial investigations on essential oil of Rosmarinus officinalis leaves grown in Ethiopia and comparison with other countries. J Appl Pharm. 2014;6(3):132–142. doi: 10.21065/19204159.6.3.112 [DOI] [Google Scholar]
- 132.Manilal A, Sabu KR, Shewangizaw M, et al. In vitro antibacterial activity of medicinal plants against biofilm-forming methicillin-resistant Staphylococcus aureus: efficacy of Moringa stenopetala and Rosmarinus officinalis extracts. Heliyon. 2020;6(1):e03303. doi: 10.1016/j.heliyon.2020.e03303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Emam JA, Yaya EE, Choudhary MI, Yousuf S, Gebremedhin TM. In Vitro Antioxidant and Anti-inflammatory Activities of Twenty-two Ethiopian Medicinal Plants. Ethiop Pharm J. 2021;37(1):89–94. doi: 10.4314/epj.v37i1.8 [DOI] [Google Scholar]
- 134.Yrga Adugna B, Mequanint Adinew G, Ayalew Getahun K, et al. Evaluation of the antidiabetic activity of hydromethanolic roots extracts of Rumex abyssinicus jacq:(Polygonaceae) in Swiss albino mice. Evidence-Based Complementary and Alternative Medicine Evid Based Complement Altern Med. 2022;2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lulekal E, Kelbessa E, Bekele T, Yineger H. An ethnobotanical study of medicinal plants in Mana Angetu District, southeastern Ethiopia. J Ethnobiol Ethnomed. 2008;4(1):10. doi: 10.1186/1746-4269-4-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Alemeye M, Gebre-marima T, Asres K. Antimicrobial activities and formulations of the extracts of chewing sticks commonly used in Ethiopia for oral cleansing. Ethiop Pharmaceutical J. 2018;34(2):95–108. doi: 10.4314/epj.v34i2.3 [DOI] [Google Scholar]
- 137.Mekuriaw E, Mengistu E, Erdedo A, Mamo H. In vitro antibacterial activity, preliminary phytochemical screening profile, and In vivo toxicity of seven traditional medicinal plants in Ethiopia. Trad Integr Med. 2021;6:398–414. [Google Scholar]
- 138.Meragiaw M, Asfaw Z. Review of antimalarial, pesticidal and repellent plants in the Ethiopian traditional herbal medicine. Research Rev. 2014;3:21–45. [Google Scholar]
- 139.Abdeta D, Abay SM, Giday M, Kebede N, Terefe G. Antitrypanosomal effect of hydromethanolic extract of Solanum anguivi Lam on field Isolates of Trypanosoma congolense Infected Mice. J Parasitol Res. 2021;2021:1–8. doi: 10.1155/2021/1239379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tegegne AA, Mulugeta A, Genetu B, Endale A, Elias A. Perception towards COVID-19 related symptoms and traditional medicine used for their management among patients and their attendants in Ethiopian comprehensive specialized hospitals: a cross-sectional study. Infect and Drug Resist. 2022;15:5023–5034. doi: 10.2147/IDR.S380211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hishe M, Asfaw Z. Review on ethnobotanical studies on traditional medicinal plants used to treat livestock and human ailments in Tigray region, Ethiopia. Adv J Biol Sci Res. 2015;3:008–0036. [Google Scholar]
- 142.Teka A, Rondevaldova J, Asfaw Z, et al. In vitro antimicrobial activity of plants used in traditional medicine in Gurage and Silti Zones, south central Ethiopia. BMC Complement Altern Med. 2015;15(1):286. doi: 10.1186/s12906-015-0822-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zemene M, Geta M, Huluka SA, Birru EM. Anti-malarial activity of the 80% methanol leaf extract and solvent fractions of Stephania abyssinica (Dill. & A. Rich.)Walp. against Plasmodium berghei infection in mice. Ethiop Pharm J. 2020;36(2):109–120. doi: 10.4314/epj.v36i2.4 [DOI] [Google Scholar]
- 144.Alemneh D. Ethnobotanical Study of Ethno-veterinary medicinal plants in Yilmana Densa and Quarit Districts, West Gojjam Zone, Amhara Region, Ethiopia. Ethnobot Res Appl. 2021;22:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ayele Y, Urga K, Engidawork E. Evaluation of in vivo antihypertensive and in vitro vasodepressor activities of the leaf extract of Syzygium guineense (willd) D.C. Phytother Res. 2010;24(10):1457–1462. doi: 10.1002/ptr.3141 [DOI] [PubMed] [Google Scholar]
- 146.Esubalew ST, Belete A, Lulekal E, Gabriel T, Engidawork E, Asres K. Review of ethnobotanical and ethnopharmacological evidences of some Ethiopian medicinal plants traditionally used for the treatment of cancer. Ethiop J Health Dev. 2017;31:161–187. [Google Scholar]
- 147.Bussa NF, Belayneh A. Traditional medicinal plants used to treat cancer, tumors and inflammatory ailments in Harari Region, Eastern Ethiopia. S Afr J Bot. 2019;122:360–368. doi: 10.1016/j.sajb.2019.03.025 [DOI] [Google Scholar]
- 148.Abeje BA, Bekele T, Getahun KA, Asrie AB. Evaluation of Wound Healing Activity of 80% Hydromethanolic Crude Extract and Solvent Fractions of the Leaves of Urtica simensis in Mice. J Exp Pharmacol. 2022;14:221–241. doi: 10.2147/JEP.S363676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Sisay W, Andargie Y, Molla M. Antimalarial Efficacy of Hydromethanolic Root Extract and Solvent Fractions of Urtica simensis Hochst. ex. A. Rich. (Urticaceae): an Experimental Study on Plasmodium berghei-Infected Mice. Evid Based Complement Altern Med. 2022;2022:1–16. doi: 10.1155/2022/6702733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Umer S, Asres K, Veeresham C. Hepatoprotective activities of two Ethiopian medicinal plants. Pharm Biol. 2010;48(4):461–468. doi: 10.3109/13880200903173593 [DOI] [PubMed] [Google Scholar]
- 151.Alemneh D. Ethnobotanical study of plants used for human ailments in Yilmana densa and Quarit districts of west Gojjam Zone, Amhara region, Ethiopia. BioMed Res Int. 2021;2021:1–18. doi: 10.1155/2021/6615666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bihonegn T, Giday M, Yimer G, Animut A, Sisay M. Antimalarial activity of hydromethanolic extract and its solvent fractions of Vernonia amygdalina leaves in mice infected with Plasmodium berghei. SAGE Open Med. 2019;7:1–10. doi: 10.1177/2050312119849766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lambebo MK, Kifle ZD, Gurji TB, Yesuf JS. Evaluation of wound healing activity of methanolic crude extract and solvent fractions of the leaves of Vernonia auriculifera Hiern (Asteraceae) in mice. J Exp Pharmacol. 2021;13:677–692. doi: 10.2147/JEP.S308303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Haile F, Kifle ZD, Dejenie TA, Berhane N, Berhane N. Synergetic antibacterial activity of Vernonia auriculifera Hiern and Buddleja polystachya Fresen on selected human pathogenic bacteria. Metabol Open. 2022;16:100210. doi: 10.1016/j.metop.2022.100210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ashenafi E, Abula T, Abay SM, Arayaselassie M, Taye S, Muluye RA. Analgesic and Anti-Inflammatory Effects of 80% Methanol Extract and Solvent Fractions of the Leaves of Vernonia auriculifera Hiern. J Exp Pharmacol. 2023;15:29–40. doi: 10.2147/JEP.S398487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Shilema A, Zerom K, Mussa A. Ethnoveterinary practices against animal trypanosomosis in Amaro district, Southern Ethiopia. Int J Med Plants Res. 2013;2:238–241. [Google Scholar]
- 157.Wondimu T, Asfaw Z, Kelbessa E. Ethnobotanical study of medicinal plants around ‘Dheeraa’town, Arsi Zone, Ethiopia. J Ethnopharmacol. 2007;112(1):152–161. doi: 10.1016/j.jep.2007.02.014 [DOI] [PubMed] [Google Scholar]
- 158.Ashagre ME, Molla EL. Cultural Significance of Medicinal Plants in Healing Human Ailments Among Guji Semi-Pastoralist People, Suro Barguda District, Ethiopia. J Ethnobiol Ethnomed. 2021;17(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Akissi ZL, Yao-Kouassi AP, Magid AA, Koffi JK, Voutquenne-Nazabadioko L. Chemical constituents and antioxidant capacities of Asparagus africanus Lam. Phytochem Lett. 2023;53:22–30. doi: 10.1016/j.phytol.2022.11.004 [DOI] [Google Scholar]
- 160.Wanga LA, Indieka AS, Matasyoh JC. Antidermatophytic quinolizidine alkaloids from Calpurnia aurea subsp. aurea (Aiton) Benth. Fitoterapia. 2023;171:105698. doi: 10.1016/j.fitote.2023.105698 [DOI] [PubMed] [Google Scholar]
- 161.Sanwal R, Chaudhary AK. Wound healing and antimicrobial potential of Carissa spinarum Linn. In albino mice. J Ethnopharmacol. 2011;135(3):792–796. doi: 10.1016/j.jep.2011.04.025 [DOI] [PubMed] [Google Scholar]
- 162.Maroyi A. Ethnopharmacological Uses, Phytochemistry, and Pharmacological Properties of Croton macrostachyus Hochst. Ex Delile: a Comprehensive Review. Evid Based Complement Alternat Med. 2017;2017:1–17. doi: 10.1155/2017/1694671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chinsembu KC, Hijarunguru A, Mbangu A. Ethnomedicinal plants used by traditional healers in the management of HIV/AIDS opportunistic diseases in Rundu, Kavango East Region, Namibia. S Afr J Bot. 2015;100:33–42. doi: 10.1016/j.sajb.2015.05.009 [DOI] [Google Scholar]
- 164.Ugbogu OC, Emmanuel O, Agi GO, et al. A review on the traditional uses, phytochemistry, and pharmacological activities of clove basil (Ocimum gratissimum L.). Heliyon. 2021;7(11):e08404. doi: 10.1016/j.heliyon.2021.e08404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kasali FM, Tusiimire J, Kadima JN, Tolo CU, Weisheit A, Agaba AG. Ethnotherapeutic uses and phytochemical composition of Physalis peruviana L.: an overview. Sci World J. 2021;2021:1–22. doi: 10.1155/2021/5212348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Deng Z, Sheng F, Yang SY, Liu Y, Zou L, Zhang LL. A comprehensive review on the medicinal usage of Podocarpus species: phytochemistry and pharmacology. J Ethnopharmacol. 2023;310:116401. doi: 10.1016/j.jep.2023.116401 [DOI] [PubMed] [Google Scholar]
- 167.Bussmann RW, Paniagua-Zambrana NY, Njoroge GN. Rumex abyssinicus Jacq. Rumex usambarensis (Dammer) Dammer Polygonaceae. In: Ethnobotany of the Mountain Regions of Africa 2021 Jan 23. Cham: Springer International Publishing. 919–926; 2021. [Google Scholar]
- 168.Nguyen D, Rieu I, Mariani C, van Dam NM. How plants handle multiple stresses: hormonal interactions underlying responses to abiotic stress and insect herbivory. Plant Mol Biol. 2016;91(6):727–740. doi: 10.1007/s11103-016-0481-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Mahmoud SM, Abdel-Azim NS, Shahat AA, Ismail SI, Hammouda FM. Phytochemical and biological studies on Verbascum sinaiticum growing in Egypt. Nat Prod Sci. 2007;13:186–189. [Google Scholar]
- 170.Tadesse M. Asteraceae. In: Hedberg I, Friis I, Edwards S, editors. Flora of Ethiopia and Eritrea. Volume 4 Part 2: Asteraceae. The National Herbarium, Addis Ababa University, Addis Ababa; 2004:1–408. [Google Scholar]
- 171.Tadesse M, Hunde D, Getachew Y. Survey of medicinal plants used to treat human diseases in Seka Chekorsa, Jimma Zone, Ethiopia. Ethiop J Health Sci. 2005;15:89–106. [Google Scholar]
- 172.Eshete MA, Kelbessa E, Dalle G. Ethnobotanical study of medicinal plants in Guji agro-pastoralists, Blue Hora District of Borana Zone, Oromia region, Ethiopia. J Med Plants Stud. 2016;4:170–184. [Google Scholar]
- 173.Gebrehiwot M. An Ethnobotanical Study of Medicinal Plants in Seru Wereda, Arsi Oromia Zone of Ethiopia (Msc Thesis). Addis Ababa: Addis Ababa University; 2010. [Google Scholar]
- 174.Beyene T. Ethnobotany of Medicinal Plants in Erob and Gulomahda Districts, Eastern Zone of Tigray Region, Ethiopia (Phd Thesis). Addis Ababa: Addis University; 2015. [Google Scholar]
- 175.Kidane L, Gebremedhin G, Beyene T. Ethnobotanical study of medicinal plants in Ganta Afeshum District, Eastern Zone of Tigray, northern Ethiopia. J Ethnobiol Ethnomed. 2018;14(1):64. doi: 10.1186/s13002-018-0266-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Heinrich M. Ethnobotany and its role in drug development. Phytother Res. 2000;14(7):479–488. doi: [DOI] [PubMed] [Google Scholar]
- 177.Leonti M, Vibrans H, Sticher O, Heinrich M. Ethnopharmacology of the Popoluca, Mexico: an evaluation. J Pharm Pharmacol. 2001;53(12):1653–1669. doi: 10.1211/0022357011778052 [DOI] [PubMed] [Google Scholar]
- 178.Abate L, Mengistu T. Phytochemical screening and peroxide value determination of methanolic extract of four traditional medicinal plants from Debre Tabor Town, Ethiopia. J Med Plant Res. 2018;12(16):203–208. doi: 10.5897/JMPR2018.6579 [DOI] [Google Scholar]
- 179.Gizaw A, Kena B, Babele DA, et al. Phytochemical screening and in vitrolousicidal and acaricidal activities of Justicia schimperiana (Hochst. ex Nees) T. Anderson leaf in West Showa Zone, Ethiopia. Ann Phytomedicine. 2022;11:725–731. [Google Scholar]
- 180.Tesfay D, Endale M, Getaneh E, Abdisa E, Guta L, Melaku Y. Chemical composition and antibacterial activity of essential oils from various parts of Gladiolus Candidus, Ranunculus Multifidus, Artemisia Abyssinica and Crinum Abyscinicum. Bull Chem Soc Ethiop. 2022;36(4):865–878. doi: 10.4314/bcse.v36i4.12 [DOI] [Google Scholar]
- 181.Komlaga G, Agyare C, Dickson RA, et al. Medicinal plants and finished marketed herbal products used in the treatment of malaria in the Ashanti region, Ghana. J Ethnopharmacol. 2015;172:333–346. doi: 10.1016/j.jep.2015.06.041 [DOI] [PubMed] [Google Scholar]
- 182.Muthee JK. Anthelmintic efficacy of selected medicinal plants against gastrointestinal nematodes in naturally infected sheep in Kenya. J Phytopharmacol. 2018;7(2):111–115. doi: 10.31254/phyto.2018.7202 [DOI] [Google Scholar]
- 183.Zebeaman M, Gebeyehu R. Phytochemical Screening and Antioxidant Activity of the fruit of Embelia Schimperi V. (family Myrsinaceae). Int JPhotochem. 2018;4:27–32. [Google Scholar]
- 184.Kimutai N, Ogutu PA, Mutai C. Antibacterial Activities of Selected Medicinal Plants from Nandi County, Kenya. Asian Jr Microbiol Biotech Env Sc. 2020;22:541–547. [Google Scholar]
- 185.Terefe L, Nardos A, Debella A, et al. Antidiarrheal Activities of the Methanol Leaf Extracts of Olinia rochetiana (Oliniaceae) Against Castor Oil-Induced Diarrhea in Mice. J Exp Pharmacol. 2023;2023:485–495. doi: 10.2147/JEP.S441555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Tadeg H, Mohammed E, Asres K, Gebre-Mariam T. Performance evaluation of topical formulations of the crude extracts of L. adoensis and O. rochetiana. Ethiop Pharm J. 2004;22:15–26. [Google Scholar]
- 187.Gebremariam T, Abula T, Gebremariam MG. Antibacterial and phytochemical screening of root extracts of Euclea racemosa subsp. Schimperi Int J Pharmacog. 2015;2:66–70. [Google Scholar]
- 188.Bazezew AM, Emire SA, Sisay MT. Bioactive composition, free radical scavenging and fatty acid profile of Ximenia americana grown in Ethiopia. Heliyon. 2021;7(6):e07187. doi: 10.1016/j.heliyon.2021.e07187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Regassa R. Useful plant species diversity in home gardens and its contribution to household food security in Hawassa city, Ethiopia. Afr J Plant Sci. 2016;10(10):211–233. doi: 10.5897/AJPS2016.1439 [DOI] [Google Scholar]
- 190.Gonfa N, Tulu D, Hundera K, Raga D. Ethnobotanical study of medicinal plants, its utilization, and conservation by indigenous people of Gera district, Ethiopia. Cogent Food Agric. 2020;6(1):1852716. doi: 10.1080/23311932.2020.1852716 [DOI] [Google Scholar]
- 191.World Health Organization. World Medical Association Declaration of Helsinki. Bull World Health Org. 2001;79(4):373–374. [PMC free article] [PubMed] [Google Scholar]