Abstract
Purpose
Venous thromboembolism (VTE) is a major complication for hip fracture patients, and may exist preoperatively. This study aimed to examine the prevalence of VTE after immediate screening in hip fracture patients.
Materials and Methods
Hip fracture patients with an elevated level of D-dimer underwent screening for VTE using computed tomography (CT) angiography. Anticoagulation treatments were administered preoperatively to patients diagnosed with VTE, followed by administration of additional anticoagulation postoperatively. Medical records were reviewed to identify risk factors for preoperative VTE and determine the prognosis of the patients.
Results
Among 524 hip fracture patients, 66 patients (12.6%) were diagnosed with VTE, including 42 patients with deep vein thrombosis (DVT), 17 patients with pulmonary thromboembolism (PTE), and 7 patients with both DVT and PTE. Of the patients with VTE, 68.2% were diagnosed within 24 hours of injury, and 33.3% of these patients had PTE. VTE patients showed a tendency toward being overweight (P<0.01) and not on anticoagulant medication (P=0.02) compared to patients without VTE. The risk of VTE was higher for femur shaft fractures (odds ratio [OR] 4.83, 95% confidence interval [CI] 2.18-10.69) and overweight patients (OR 2.12, 95% CI 1.17-3.85), and lower for patients who were previously on anticoagulants (OR 0.36, 95% CI 0.18-0.74). Patients with preoperatively diagnosed VTE were asymptomatic before and after surgery.
Conclusion
Clinicians should be aware that VTE may be present within 24 hours of injury, and screening for VTE or prophylactic measures should be considered for high-risk patients.
Keywords: Fracture, Venous thromboembolism, Screening, Overweight, Anticoagulant
INTRODUCTION
Hip fracture is a major risk factor for venous thromboembolism (VTE), and its correlation has been emphasized for more than half a century1-3). The risk of VTE is high for patients who sustain hip fractures with a prevalence of over 30% reported in the literature4,5). Most cases of VTE begin as deep vein thrombosis (DVT) in the calf veins, with progression to proximal veins, and advancement to pulmonary thromboembolism (PTE)6-8). Although distal DVT may appear to be asymptomatic, with its proximal extension to proximal veins and pulmonary arteries, it can become fatal with development of severe symptoms or even death6,9). With the increasing global population and longer life expectancy, the numbers of hip fractures and patients with VTE are expected to increase10,11).
According to one estimate, approximately one half of DVT cases associated with surgery begin intraoperatively, and among surgeries, the highest risk has been reported for major orthopedic surgery6,12,13). Therefore, current guidelines on VTE prophylaxis for patients with hip fracture focus primarily on the prophylaxis of postoperative VTE14). However, as reported by Song et al., the majority of patients with femur neck fracture in their study who were diagnosed with DVT postoperatively already had thrombus before surgery15). Prevalence of preoperative VTE as high as 29.8% has been reported for patients with hip fracture, and preoperative assessment for VTE is recommended for patients with surgical delay over 24 hours15-17).
The primary objective of this study was to assess the prevalence of VTE after immediate screening in patients with hip fracture. The second objective was to identify risk factors for preoperative VTE. The third objective was to examine the prognosis of patients diagnosed with VTE preoperatively after administration of perioperative anticoagulation. We hypothesized that VTE may be present within 24 hours of injury.
MATERIALS AND METHODS
1. Patients and Study Design
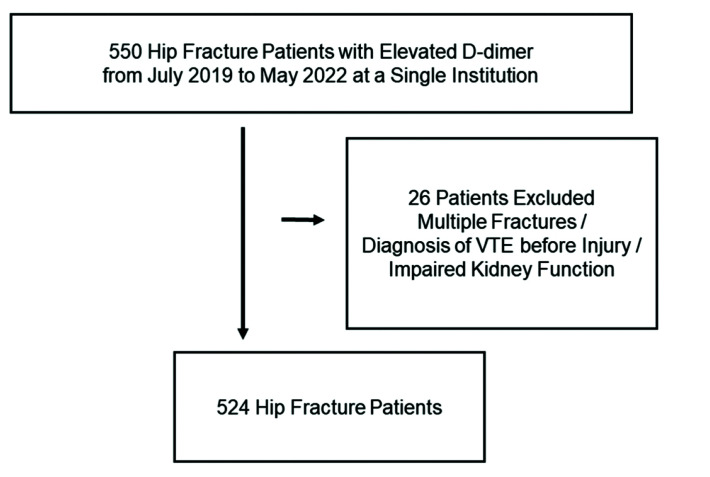
A retrospective review of patients with fractures located around the hip from July 2019 to May 2022 at a single institution was conducted. Types of fractures included femur neck fractures, intertrochanteric fractures, subtrochanteric fractures, femur shaft fractures, and pelvic bone fractures. Patients with an elevated level of D-dimer were included. Patients who had multiple fractures, a diagnosis of VTE prior to injury, or were ineligible for injection of contrast media due to impaired kidney function, were excluded (Fig. 1). This study was conducted in accordance with the Declaration of Helsinki (2013) and was approved by the Institutional Review Board (IRB) of College of Medicine, The Catholic University of Korea (approval No. HC22RISI0058). The written informed consent was waived by the IRB due to the retrospective nature of the study.
Fig. 1.
Patient flowchart. VTE: venous thromboembolism.
2. Diagnosis of VTE and Perioperative Anticoagulation
Patients with an elevated level of D-dimer underwent immediate screening for VTE using computed tomography (CT) angiography. During CT scans, scanning of patients from the thorax to the lower extremities at the arterial phase and the portal phase was performed. CT scans were performed using CT scanners (SOMATOM Force; Siemens Healthineers) with 384 detector rows. Ionic contrast material (2 mL/kg; up to 150 mL) was injected at 3 to 4 mL/sec. Bolus tracking within the descending aorta began 18 seconds after the contrast injection, and as the Hounsfield unit at the bolus tracked region reached 100, the arterial phase scan was initiated after 25 seconds. The portal phase scan began after a delay of 270 seconds. The arterial phase was scanned with a slice thickness of 3 mm and the portal phase was scanned with a slice thickness of 5 mm. Examination and interpretation of CT angiography images were performed by a board-certified radiologist who specialized in angiography, who was not informed of the purpose of the study.
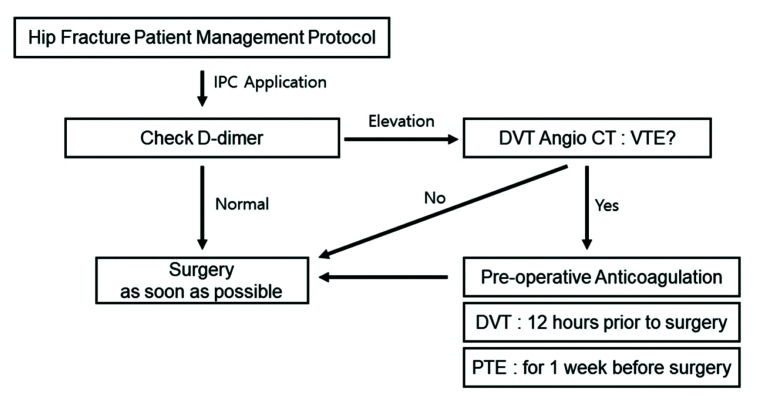
Intermittent pneumatic compression (IPC) was applied on both lower extremities on admission for all patients. In cases of preoperative DVT, a subcutaneous injection of 40 mg enoxaparin was administered 12 hours prior to surgery, followed by reapplication of IPC postoperatively, encouraging ambulation, and administration of additional anticoagulation. In cases of preoperative PTE, surgery was delayed and subcutaneous injection of 1 mg/kg enoxaparin was administered at 12-hour intervals for one week prior to surgery (Fig. 2). Unless other types of thromboprophylaxis were required due to medical conditions, IPC was reapplied postoperatively with administration of additional anticoagulation by subcutaneous injections of enoxaparin, initiated 12 hours after surgery, which was exchanged for rivaroxaban and maintained for at least three months.
Fig. 2.
Preoperative VTE prophylaxis protocol for hip fracture patients. IPC: Intermittent pneumatic compression, DVT: deep vein thrombosis, CT: computed tomography, VTE: venous thromboembolism, PTE: pulmonary thromboembolism.
3. Method of Assessment
A review of electronic medical records and picture archiving and communication system records was performed for collection of patient data and radiologic findings. Time from injury to diagnosis of VTE was recorded. For patients with hip fracture, age, sex, type of fracture, comorbidities, previous anticoagulation, malignancy, pre-injury ambulatory level, body mass index (BMI), smoking history, D-dimer level, and international normalized ratio (INR) were compared between patients with VTE and those without VTE. A review of medical records was performed to evaluate the prognosis of patients who were diagnosed preoperatively with VTE and the prevalence of VTE that was newly diagnosed postoperatively during the admission period.
4. Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows (ver. 20.0; IBM Corp.). Analysis of continuous data was performed using a t-test, and analysis of categorical data was performed using a chi-squared test. Logistic regression was used for multivariate analysis for identification of risk factors for VTE. A P-value of <0.05 was considered statistically significant.
RESULTS
A total of 524 patients with fractures located around the hip who had an elevated level of D-dimer underwent screening for VTE using CT angiography between July 2019 and May 2022. The mean age of the patients was 78.54±10.71 years (range, 19-101 years). The study included 140 male patients (26.7%) and 384 female patients (73.3%). There were 171 patients (32.6%) with femur neck fracture, 272 patients (51.9%) with intertrochanteric fracture, 17 patients (3.2%) with subtrochanteric fracture, 49 patients (9.4%) with femur shaft fracture, and 15 patients (2.9%) with pelvic bone fracture. A summary of patient demographics is shown in Table 1.
Table 1.
Patient Demographics
| Total | No VTE | VTE | P-value | |
|---|---|---|---|---|
| No. of patients | 524 | 458 (87.4) | 66 (12.6) | |
| Sex | 0.43 | |||
| Male | 140 (26.7) | 125 (27.3) | 15 (22.7) | |
| Female | 384 (73.3) | 333 (72.7) | 51 (77.3) | |
| Fracture type | <0.01 | |||
| Femur neck | 171 (32.6) | 150 (32.8) | 21 (31.8) | |
| Intertrochanter | 272 (51.9) | 250 (54.6) | 22 (33.3) | |
| Subtrochanter | 17 (3.2) | 14 (3.1) | 3 (4.5) | |
| Femur shaft | 49 (9.4) | 31 (6.8) | 18 (27.3) | |
| Pelvis | 15 (2.9) | 13 (2.8) | 2 (3.0) | |
| Comorbidities | ||||
| HTN | 369 (70.4) | 322 (70.3) | 47 (71.2) | 0.88 |
| DM | 176 (33.6) | 159 (34.7) | 17 (25.8) | 0.15 |
| Dyslipidemia | 68 (13.0) | 60 (13.1) | 8 (12.1) | 0.83 |
| CKD | 63 (12.0) | 56 (12.2) | 7 (10.6) | 0.71 |
| CVA | 75 (14.3) | 67 (14.6) | 8 (12.1) | 0.59 |
| CAD | 57 (10.9) | 52 (11.4) | 5 (7.6) | 0.36 |
| Arrhythmia | 34 (6.5) | 31 (6.8) | 3 (4.5) | 0.49 |
| Pulmonary disease | 82 (15.6) | 73 (15.9) | 9 (13.6) | 0.63 |
| Pre-injury Koval score (mean) | 2.58±1.93 | 2.56±1.91 | 2.71±2.06 | 0.55 |
| Pre-injury Koval score <4 | 364 (69.5) | 320 (69.9) | 44 (66.7) | 0.58 |
| Time from injury to admission | 0.67 | |||
| <24 hr | 388 (74.0) | 343 (74.9) | 45 (68.2) | |
| ≥24, <72 hr | 69 (13.2) | 59 (12.9) | 10 (15.2) | |
| ≥72 hr | 67 (12.8) | 56 (12.2) | 11 (16.7) | |
| Anticoagulant | 161 (30.7) | 149 (32.5) | 12 (18.2) | 0.02 |
| Cancer history | 57 (10.9) | 48 (10.5) | 9 (13.6) | 0.44 |
| Smoking | 37 (7.1) | 35 (7.6) | 2 (3.0) | 0.17 |
| Elevated INR | 29 (5.5) | 26 (5.7) | 3 (4.5) | 0.71 |
| Age (yr) | 78.54±10.71 | 78.52±10.76 | 78.67±10.42 | 0.92 |
| Height (m) | 1.58±0.07 | 1.58±0.71 | 1.57±0.09 | 0.49 |
| Weight (kg) | 56.87±9.61 | 56.71±9.54 | 57.92±10.11 | 0.34 |
| BMI (kg/m2) | 22.86±3.33 | 22.79±3.33 | 24.38±2.94 | 0.03 |
| ≥25 | 112 (21.4) | 89 (19.4) | 23 (34.8) | <0.01 |
| D-dimer (mg/L) | 16.10±12.83 | 16.70±12.95 | 12.25±11.12 | <0.01 |
Values are presented as number (%) or mean±standard deviation.
VTE: venous thromboembolism, HTN: hypertension, DM: diabetes mellitus, CKD: chronic kidney disease, CVA: cerebrovascular accident, CAD: coronary artery disease, INR: international normalized ratio, BMI: body mass index.
The overall prevalence of preoperative VTE was 12.6% (66 of 524 patients). Forty-two patients had DVT alone, 17 patients had PTE alone, and seven patients had both DVT and PTE. None of the 66 patients showed symptoms of VTE or fatal conditions prior to diagnosis of VTE. Of patients with VTE, 68.2% (45 of 66 patients) were diagnosed within 24 hours of injury, and 33.3% (15 of 45) of these patients had PTE. Patients with preoperatively diagnosed VTE were asymptomatic before and after surgery. There were no cases of VTE that were newly diagnosed postoperatively.
The prevalence of VTE was lower for patients who were previously on anticoagulants prior to injury compared with patients not on anticoagulants (18.2% vs. 32.5%, P=0.02). A higher proportion of overweight patients, with BMI of 25 kg/m2 or higher (19.4% vs. 34.8%, P<0.01) was observed in the VTE group. Time from injury to screening for VTE was not a significant factor for the prevalence of VTE (P=0.67). After adjustment for other risk factors using multivariate logistic regression, the risk of VTE was higher for patients with femur shaft fractures compared to patients with femur neck fracture (odds ratio [OR] 4.83, P<0.01). Patients who were on anticoagulants prior to diagnosis of VTE were less likely to have VTE compared with patients who were not on medication (OR 0.36, P<0.01). Being overweight with BMI 25 kg/m2 or higher was a significant risk factor for VTE (OR 2.12, P=0.01) (Table 2).
Table 2.
Multivariate Analysis for VTE Risk Factors
| OR | P-value | 95% CI | |
|---|---|---|---|
| Age | 1.03 | 0.06 | 1.00-1.06 |
| Fracture type | |||
| Femur neck | - | <0.01 | - |
| Intertrochanter | 0.91 | 0.91 | 0.19-4.39 |
| Subtrochanter | 1.29 | 0.99 | 0.34-4.97 |
| Femur shaft | 4.83 | <0.01 | 2.18-10.69 |
| Pelvis | 1.24 | 0.80 | 0.25-6.23 |
| Anticoagulant | 0.36 | <0.01 | 0.18-0.74 |
| BMI ≥25 kg/m2 | 2.12 | 0.01 | 1.17-3.85 |
VTE: venous thromboembolism, OR: odds ratio, CI: confidence interval, BMI: body mass index.
DISCUSSION
VTE may be present in patients with fractures located around the hip within 24 hours of injury. Of patients with VTE, 68.2% (45 of 66) were diagnosed within 24 hours of injury, including 15 patients with PTE. There was no correlation with time from injury to the prevalence of VTE (P=0.67). The results of our study indicate that VTE that includes PTE can occur in fracture patients at any time after injury within 24 hours. As all patients in our study who were diagnosed with VTE preoperatively were asymptomatic, if they had not undergone preoperative screening for VTE, they would have undergone surgery with the presence of emboli in their pulmonary arteries. The acute inflammatory reaction caused by tissue trauma and activation of the clotting cascade can be regarded as unique risk factors for PTE under the perioperative circumstances of surgical patients18). Incidence of symptomatic intraoperative PTE between 0.6% to 10% has been reported, and diagnosis and management in the intraoperative setting can be difficult, due to ongoing performance of surgical procedures19).
VTE occurs for the first time in approximately 100 persons per 100,000 annually in the United States20). The prevalence of preoperative VTE for the patients in our study was 12.6% (66 of 524). The relatively higher prevalence may be due to the high-risk characteristics of our study cohort including old age and fracture. The preemptive screening performed prior to development of symptoms could be another explanation.
General risk factors for VTE include advanced age, cancer, prior VTE, venous insufficiency, pregnancy, trauma, frailty, and immobility21). Shin et al.17), who studied risk factors for VTE in hip fracture patients with a delay of more than 24 hours from injury to surgery, concluded that female gender, subtrochanteric fracture, pulmonary disease, cancer, previous hospitalization for VTE, and varicose veins can be regarded as risk factors for VTE. In our study, patients with femur shaft fractures, patients who were not on anticoagulants, and overweight patients (BMI ≥25 kg/m2) were at risk of VTE. The results may differ from those reported in previous studies, as other studies were based on patients with postoperative VTE or patients with preoperative VTE with surgical delay17,21). In our study, the risk of preoperative VTE was 0.36 times lower for patients who were previously on anticoagulants due to underlying diseases, compared to patients who did not receive anticoagulant administration (OR 0.36, P<0.01).
All VTE patients in our study were asymptomatic preoperatively, and after receiving perioperative anticoagulation, remained asymptomatic postoperatively. In addition, there were no patients with VTE that was newly diagnosed postoperatively. Development of symptoms of VTE is dependent on the extent of thrombosis, perfusion by collateral vessels, severity of occlusion of the associated vessel, and the patient’s capacity to tolerate the thrombosis1). Although VTE may present without symptoms, in cases of symptomatic DVT, patients may experience leg pain, swelling, and erythema, and dyspnea, intrathoracic distress, or shock may be observed in patients with PTE6,21). Early diagnosis and treatment of VTE using mechanical and pharmacological measures may provide an explanation for our results.
Preoperative measures to reduce the incidence or for management of preoperative VTE is required for patients who sustain fractures around the hip. According to current guidelines for use in clinical practice, both mechanical and pharmacological VTE prophylaxis is recommended after individualized risk assessment14,22,23). If there are no contraindications, application of compression stockings or IPC is recommended on admission and postoperatively until mobilization close to the patient’s pre-admission status can be achieved24,25). Preoperative pharmacological prophylaxis is recommended in cases where surgical delay is expected, commencing as early as within 14 hours of admission, following assessment of risk for bleeding and thrombosis24). Injection of low-molecular-weight heparin (LMWH), no less than 12 hours preoperatively, or unfractionated heparin, under close serological monitoring, is recommended as appropriate preoperative agents26,27). Postoperative pharmacological thromboprophylaxis commencing 12 hours after wound closure, and continuing for at least 28 days is recommended24). Although no definitive leading pharmacological agent has been identified, LMWH has become the standard agent according to many guidelines based on increased bioavailability, low bleeding complications, and long plasma half-life14,24,25,27). Promising results in reduction of VTE have been achieved with aspirin and direct oral anticoagulant such as rivaroxaban, however, there are concerns with regard to hemorrhagic events in the immediate postoperative period26,28,29). Regarding treatment of preoperative VTE, there is no definite protocol for treatment of patients with preoperative VTE who require surgery, and inferior vena cava filtering is reserved for patients who cannot receive any form of prophylaxis preoperatively30).
This study is the first to examine the incidence of preoperative VTE in hip fracture patients immediately after sustaining an injury using CT angiography. However, this study has limitations. First, the study was of a retrospective design, and the results may have been influenced by confounding factors or bias. Second, this was a single center study, and the results may differ in other provinces with different social backgrounds and ethnicity around the world. Third, patients with impaired kidney function who were not eligible to receive an injection of contrast media were excluded from the study. Fourth, although patients underwent examination using CT angiography after providing informed consent, they were exposed to radiation and received injections of contrast media, which could cause side effects. However, unlike ultrasound used in other studies, CT angiography offers the advantage of detecting DVT and PTE during one examination. To lower the radiation dose, CT angiography was performed using tube voltage at a setting of 100 kV in the arterial phase and 80 kV in the delay phase, which is comparatively lower than CT scans of the abdomen or chest with tube voltage settings of 120 kV at our institution. To prevent side effects from contrast media, all patients received adequate hydration and renal protection prior to administration of contrast media. None of the patients in our study developed side effects. Fifth, the indication for CT angiography was an elevated level of D-dimer. Many confounding factors are associated with D-dimer elevation, including trauma, female gender, increasing age, immobility, and drug use31). Therefore, there may be uncertainty with regard to the necessity of CT angiography for these patients. However, only a negative D-dimer result combined with a three-level Wells rule can safely rule out VTE14,26,32). If D-dimer elevation is not acceptable as an indication for CT angiography in patients with hip fracture, conduct of additional study to determine indications for VTE screening, such as the risk factors for preoperative VTE, is warranted.
CONCLUSION
The risk of VTE is high for patients with fractures located around the hip at any time after sustaining an injury, particularly patients with femur shaft fracture, overweight patients, and patients who are not on anticoagulants. Clinicians should be aware that VTE may be present within 24 hours of injury, and screening for VTE or prophylactic measures should be considered for high-risk patients.
Funding Statement
FUNDING No funding to declare.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
References
- 1.Anderson FA, Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I9–16. doi: 10.1161/01.CIR.0000078469.07362.E6. [DOI] [PubMed] [Google Scholar]
- 2.Sevitt S, Gallagher NG. Prevention of venous thrombosis and pulmonary embolism in injured patients. A trial of anticoagulant prophylaxis with phenindione in middle-aged and elderly patients with fractured necks of femur. Lancet. 1959;2:981–9. doi: 10.1016/S0140-6736(59)91464-3. https://doi.org/10.1016/s0140-6736(59)91464-3. [DOI] [PubMed] [Google Scholar]
- 3.Shin WC, Lee SM, Suh KT. Recent updates of the diagnosis and prevention of venous thromboembolism in patients with a hip fracture. Hip Pelvis. 2017;29:159–67. doi: 10.5371/hp.2017.29.3.159. https://doi.org/10.5371/hp.2017.29.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakase J, Toribatake Y, Mouri Y, Seki H, Kitaoka K, Tomita K. Heparin versus danaproid for prevention of venous thromboembolism after hip surgery. J Orthop Surg (Hong Kong) 2009;17:6–9. doi: 10.1177/230949900901700102. https://doi.org/10.1177/230949900901700102. [DOI] [PubMed] [Google Scholar]
- 5.Pedersen AB, Ehrenstein V, Szépligeti SK, Sørensen HT. Excess risk of venous thromboembolism in hip fracture patients and the prognostic impact of comorbidity. Osteoporos Int. 2017;28:3421–30. doi: 10.1007/s00198-017-4213-y. https://doi.org/10.1007/s00198-017-4213-y. [DOI] [PubMed] [Google Scholar]
- 6.Kearon C. Natural history of venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I22–30. doi: 10.1161/01.CIR.0000078464.82671.78. https://doi.org/10.1161/01.CIR.0000078464.82671.78. [DOI] [PubMed] [Google Scholar]
- 7.Moser KM, LeMoine JR. Is embolic risk conditioned by location of deep venous thrombosis? Ann Intern Med. 1981;94(4 pt 1):439–44. doi: 10.7326/0003-4819-94-4-439. https://doi.org/10.7326/0003-4819-94-4-439. [DOI] [PubMed] [Google Scholar]
- 8.Negus D, Pinto DJ. Natural history of postoperative deep-vein thrombosis. Lancet. 1969;2:645. doi: 10.1016/S0140-6736(69)90355-9. https://doi.org/10.1016/s0140-6736(69)90355-9. [DOI] [PubMed] [Google Scholar]
- 9.Geerts WH, Code KI, Jay RM, Chen E, Szalai JP. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994;331:1601–6. doi: 10.1056/NEJM199412153312401. https://doi.org/10.1056/NEJM199412153312401. [DOI] [PubMed] [Google Scholar]
- 10.Brown CA, Starr AZ, Nunley JA. Analysis of past secular trends of hip fractures and predicted number in the future 2010-2050. J Orthop Trauma. 2012;26:117–22. doi: 10.1097/BOT.0b013e318219c61a. https://doi.org/10.1097/BOT.0b013e318219c61a. [DOI] [PubMed] [Google Scholar]
- 11.Schulman S, Ageno W, Konstantinides SV. Venous thromboembolism: past, present and future. Thromb Haemost. 2017;117:1219–29. doi: 10.1160/TH16-10-0823. https://doi.org/10.1160/TH16-10-0823. [DOI] [PubMed] [Google Scholar]
- 12.Collaborative overview of randomised trials of antiplatelet therapy--III: reduction in venous thrombosis and pulmonary embolism by antiplatelet prophylaxis among surgical and medical patients. Antiplatelet Trialists' Collaboration. BMJ. 1994;308:235–46. doi: 10.1136/bmj.308.6923.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.White RH, Romano PS, Zhou H, Rodrigo J, Bargar W. Incidence and time course of thromboembolic outcomes following total hip or knee arthroplasty. Arch Intern Med. 1998;158:1525–31. doi: 10.1001/archinte.158.14.1525. https://doi.org/10.1001/archinte.158.14.1525. [DOI] [PubMed] [Google Scholar]
- 14.The ICM-VTE Trauma Delegates. Recommendations from the ICM-VTE: trauma. J Bone Joint Surg Am. 2022;104(Suppl 1):280–308. doi: 10.2106/JBJS.21.01476. https://doi.org/10.2106/JBJS.21.01476. [DOI] [PubMed] [Google Scholar]
- 15.Song K, Yao Y, Rong Z, Shen Y, Zheng M, Jiang Q. The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures. Arch Orthop Trauma Surg. 2016;136:1459–64. doi: 10.1007/s00402-016-2535-4. https://doi.org/10.1007/s00402-016-2535-4. [DOI] [PubMed] [Google Scholar]
- 16.He SY, Zhang P, Qin HJ, Jiang N, Yu B. Incidence and risk factors of preoperative deep venous thrombosis following hip fracture: a retrospective analysis of 293 consecutive patients. Eur J Trauma Emerg Surg. 2022;48:3141–7. doi: 10.1007/s00068-021-01861-3. https://doi.org/10.1007/s00068-021-01861-3. [DOI] [PubMed] [Google Scholar]
- 17.Shin WC, Woo SH, Lee SJ, Lee JS, Kim C, Suh KT. Preoperative prevalence of and risk factors for venous thromboembolism in patients with a hip fracture: an indirect multidetector CT venography study. J Bone Joint Surg Am. 2016;98:2089–95. doi: 10.2106/JBJS.15.01329. https://doi.org/10.2106/JBJS.15.01329. [DOI] [PubMed] [Google Scholar]
- 18.Desciak MC, Martin DE. Perioperative pulmonary embolism: diagnosis and anesthetic management. J Clin Anesth. 2011;23:153–65. doi: 10.1016/j.jclinane.2010.06.011. https://doi.org/10.1016/j.jclinane.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 19.Koessler MJ, Fabiani R, Hamer H, Pitto RP. The clinical relevance of embolic events detected by transesophageal echocardiography during cemented total hip arthroplasty: a randomized clinical trial. Anesth Analg. 2001;92:49–55. doi: 10.1097/00000539-200101000-00010. https://doi.org/10.1097/00000539-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 20.White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I4–8. doi: 10.1161/01.CIR.0000078468.11849.66. [DOI] [PubMed] [Google Scholar]
- 21.Goldhaber SZ. Risk factors for venous thromboembolism. J Am Coll Cardiol. 2010;56:1–7. doi: 10.1016/j.jacc.2010.01.057. https://doi.org/10.1016/j.jacc.2010.01.057. [DOI] [PubMed] [Google Scholar]
- 22.Kruger PC, Eikelboom JW, Douketis JD, Hankey GJ. Deep vein thrombosis: update on diagnosis and management. Med J Aust. 2019;210:516–24. doi: 10.5694/mja2.50201. https://doi.org/10.5694/mja2.50201. [DOI] [PubMed] [Google Scholar]
- 23.Dalen JE, Alpert JS. Natural history of pulmonary embolism. Prog Cardiovasc Dis. 1975;17:259–70. doi: 10.1016/S0033-0620(75)80017-X. https://doi.org/10.1016/s0033-0620(75)80017-x. [DOI] [PubMed] [Google Scholar]
- 24.National Institute for Health and Care Excellence (NICE), author Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism [Internet] London: NICE; 2018. Mar 21, [updated 2019 Aug 13; cited 2022 Sep 8]. Available from: https://www.nice.org.uk/guidance/ng89 . [Google Scholar]
- 25.Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898–944. doi: 10.1182/bloodadvances.2019000975. https://doi.org/10.1182/bloodadvances.2019000975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e278S–325S. doi: 10.1378/chest.11-2404. https://doi.org/10.1378/chest.11-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institute for Health and Care Excellence (NICE), author Venous thromboembolism in adults [Internet] NICE; London: 2021. Aug 19, [cited 2022 Sep 8]. Available from: https://www.nice.org.uk/guidance/qs201 . [Google Scholar]
- 28.Ley EJ, Brown CVR, Moore EE, et al. Updated guidelines to reduce venous thromboembolism in trauma patients: a Western Trauma Association critical decisions algorithm. J Trauma Acute Care Surg. 2020;89:971–81. doi: 10.1097/TA.0000000000002830. https://doi.org/10.1097/TA.0000000000002830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moon KH, Kang JS, Youn YH. Is the oral chemical prophylaxis necessary for the prevention of venous thromboembolism after joint arthroplasty in a Korean population? Hip Pelvis. 2019;31:150–7. doi: 10.5371/hp.2019.31.3.150. https://doi.org/10.5371/hp.2019.31.3.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anderson DR, Dunbar M, Murnaghan J, et al. Aspirin or rivaroxaban for VTE prophylaxis after hip or knee arthroplasty. N Engl J Med. 2018;378:699–707. doi: 10.1056/NEJMoa1712746. https://doi.org/10.1056/NEJMoa1712746. [DOI] [PubMed] [Google Scholar]
- 31.Flevas DA, Megaloikonomos PD, Dimopoulos L, Mitsiokapa E, Koulouvaris P, Mavrogenis AF. Thromboembolism prophylaxis in orthopaedics: an update. EFORT Open Rev. 2018;3:136–48. doi: 10.1302/2058-5241.3.170018. https://doi.org/10.1302/2058-5241.3.170018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kabrhel C, Mark Courtney D, et al. Factors associated with positive D-dimer results in patients evaluated for pulmonary embolism. Acad Emerg Med. 2010;17:589–97. doi: 10.1111/j.1553-2712.2010.00765.x. https://doi.org/10.1111/j.1553-2712.2010.00765.x. [DOI] [PMC free article] [PubMed] [Google Scholar]