Abstract
Objectives
To describe long-acting reversible contraceptive (LARC) users’ knowledge, patient-provider interactions, and condom use associated with LARC use. Methods: Data are from the 2018 National Survey of Sexual Health and Behavior, a probability survey of Americans aged 14–49. Results: Of 1,451 sexually active women, 11.2% used intrauterine devices, and 3.1% used implants. Approximately 19-26% of LARC users reported inaccurately on LARC longevity, and 30% reported relying on their provider to indicate the timing of intrauterine device removal. Consistent condom use among LARC users was rare (6.1%). Conclusions: Our findings have implications for how clinicians educate patients on LARC and condom use.
Keywords: Contraception, reproductive health—women, internet-based studies
Introduction
The right to choose if and when to become pregnant has been identified by the World Association for Sexual Health as a sexual right (World Association for Sexual Health, 2014); it is also a key tenet of reproductive justice, which has been described as the “human right to maintain personal bodily autonomy, have children, not have children, and parent the children we have in safe and sustainable communities” (Sister Song, n.d.). Long-acting reversible contraceptive (LARC) methods, which include intrauterine devices (IUDs) and subdermal hormonal implants, are highly efficacious means for pregnancy prevention and are thus valuable tools for sexual health promotion (Harper et al., 2015; Winner et al., 2012). LARC methods do not depend on user compliance in contrast, for example, to individuals having to remember to take daily hormonal contraceptive pills or to those whose partner attempts to sabotage their contraceptive use (Grimes, 2009; Sherin & Waters, 2019). Consequently, LARC effectiveness in preventing pregnancy is greater than 99% for both perfect and typical use (Winner et al., 2012), making them important tools for supporting sexual health and sexual rights, as well as reducing costs associated with unintended pregnancies and abortions (Blumenthal et al., 2011; Foster et al., 2009; Trussell et al., 1995, 2013).
In the past decade, LARC use in the United States (U.S.) has increased among cisgender women aged 15–44, from 6.0% in 2008 to 14.3% in 2014 according to the National Survey of Family Growth (NSFG) (Kavanaugh & Jerman, 2018). Despite this increase in LARC use, unintended pregnancies in the U.S. remain high, particularly for younger women, racial/ethnic minority women, and sexual minority women (Hartnett et al., 2017; Ihongbe & Masho, 2018). A national Canadian study of 113 public health units found that IUDs were the least common sexual health clinical services provided (O’Sullivan et al., 2019). Current LARC use has been found to be associated with age, education, future birth intention, sexual activity, and dissatisfaction with or discontinuation of non-LARC contraceptive methods (Branum & Jones, 2015; Ihongbe & Masho, 2018; Kavanaugh et al., 2015; Mosher et al., 2016; Whitaker et al., 2010). College students are often particularly interested in LARC methods, given a common desire to delay pregnancy and complete education (Hopkins et al., 2018). Several LARCs are also well suited for lactating individuals who wish to avoid pregnancy but need to avoid contraceptive methods that contain estrogens, in order to maintain their milk supply (Goldstuck & Steyn, 2013).
Healthcare provider interactions related to LARCs
Empirical data examining the role of healthcare provider interactions to the uptake of LARC methods are scarce, though a few qualitative studies have suggested that the provider’s confidence, counseling, instrumental supports, and even bias regarding LARC methods may affect the patient’s choice to use LARC methods (Higgins et al., 2016; Murphy et al., 2016). One study in Nigeria using a self-reported GATHER (greet, ask, tell, help, explain, return) index to measure patient–provider interactions found that greater patient–provider interactions were associated with a higher likelihood of adopting LARC methods (Kalra et al., 2019); however, no such similar study has been conducted in the U.S. To our knowledge, there has been no prior study looking at how patient–provider interactions may be associated with patients’ knowledge of LARC methods. This is important because, although patient compliance with contraceptive use is important to pregnancy prevention, patient knowledge and understanding of LARC use are supportive of patients’ reproductive autonomy, including their choices related to using LARCs and discontinuing LARCs for any reason (e.g., to become pregnant, due to side effects, due to personal preference).
Dual LARC and condom use
Though LARC methods are effective at pregnancy prevention, they offer no protection against sexually transmitted infections (STIs); thus, condom use while using LARC methods is important for STI prevention (Higgins & Cooper, 2012). However, there is concern that individuals may be less likely to use condoms after beginning LARC methods as they may potentially be less worried about unintended pregnancies (Potter & Soren, 2016; Williams & Fortenberry, 2013). Numerous studies on condom use with LARC methods have been conducted among adolescents and young women (Bastow et al., 2018; Steiner et al., 2016; Thompson et al., 2017; Tyler et al., 2014; Walsh-Buhi & Helmy, 2018) who are disproportionately burdened with STIs and unintended pregnancies, but far fewer studies have been conducted among a broader age range of adults (Bernard et al., 2018; McNicholas et al., 2017), especially at the population level. Although women in their late twenties, thirties, and forties have a lower rate of STIs compared to women under 25, their risk is not negligible particularly given the recent annual increases in STIs that affect individuals as well as newborns (i.e., congenital syphilis) (Centers for Disease Control & Prevention, 2019).
Condom use associated with LARC methods varies significantly depending on the population, year assessed, and the definition of condom use with LARC methods (e.g., consistent use vs. any use; different timeframes for measurement) (Higgins & Cooper, 2012). Prior research has consistently found condom use to be less frequent among LARC users compared to users of other contraceptive methods (Bastow et al., 2018; Bernard et al., 2018; Steiner et al., 2016; Walsh-Buhi & Helmy, 2018); thus LARC methods could serve a different purpose for women who cannot use other contraceptive methods (e.g., breastfeeding mothers, women unable to adapt to a method that emphasizes user adherence, those who face partner sabotage). A study utilizing data from the Contraceptive CHOICE Project found that LARC initiators reported lower rates of consistent condom use compared to users of other methods, however, there was no evidence supporting changes in condom use compared to pre-initiation behaviors (McNicholas et al., 2017). Importantly, LARC users were more likely to acquire an STI in the year following LARC initiation compared to users of other contraceptive methods, thereby highlighting the importance of dual-method contraception education (McNicholas et al., 2017). Prior studies have also suggested that body image appreciation may be associated with dual use of condoms and hormonal contraceptive methods among young women (Ramseyer Winter & Ruhr, 2017).
Even though healthcare providers for both adolescent and adult patients have been urged to discuss condom use with their patients, existing research indicates that such patient–provider conversations are uncommon (Grubb, 2020; Centers for Disease Control and Prevention, n.d.). Moreover, there is a dearth of research regarding how conversations with healthcare providers combined with demographic and relationship characteristics are associated with condom use among LARC users. This information is key to understanding the role that healthcare providers may play in the uptake and/or management of LARC methods and condom use, and thereby help reduce STIs and unintended pregnancies. Such data may be particularly relevant for clinicians who work in publicly funded clinics and/or college health clinics as they may be less likely to have a consistent, ongoing relationship with their patient, and thus may lack opportunities to follow-up with ongoing counseling or education about LARC methods, condoms, or contraceptive use. Using a nationally representative probability sample of U.S. cisgender women ages 14–49, the purpose of our study was to describe IUD and implant users’ knowledge about these methods, patient/provider interactions regarding LARC methods, and condom use while using LARC methods.
Materials and methods
Study design and participants
The Institutional Review Board at the authors’ university reviewed and approved all protocols associated with the research (#1412111668). Data for this study are from the 2018 National Survey of Sexual Health and Behavior (NSSHB), a nationally representative probability survey of U.S. individuals aged 14–49 (Fu et al., 2019). This survey was confidential, cross-sectional in design, and administered online in February and March 2018. Participants were from the Ipsos (formerly known as GfK) KnowledgePanel (Sunnyvale, CA). Ipsos is a corporate entity that facilitates data collection through various means, including their KnowledgePanel which is a nationally representative probability sample of Americans. KnowledgePanel is constructed using address-based sampling from the U.S. Postal Service’s Delivery Sequence File; individuals are randomly selected from the U.S. population and invited, through letters and phone calls, to join the panel. People cannot join of their own accord; that is, it is not an “opt in” panel. Individuals who are contacted by Ipsos and interested in joining the panel but who lack the software or hardware to do so are provided with the necessary connections.
Ipsos KnowledgePanel members ages 18 through 49 were recruited into the 2018 NSSHB based on an equal probability selection method for general population surveys. Because KnowledgePanel members are adults ages 18 and older, to access adolescents ages 14–17, Ipsos first sent an IRB-approved recruitment email to the adult parent that described the study and sought parental consent to invite their adolescent to complete the survey. To account for differential nonresponse that may have resulted during data collection, Ipsos calculated post-stratification weights to adjust in relation to benchmarks from the March 2017 U.S. Census Bureau’s Current Population Survey.
For the 2018 NSSHB, 8,950 individuals ages 14–49 were recruited into the study, of which 5,448 (60.9%) completed the screener. A total of 4,547 respondents completed the survey (cooperation rate = 50.8%). Of these, 2,423 (53.3%) respondents were women. Our analyses were restricted to the 1,451 cisgender women ages 14–49 who reported penile-vaginal intercourse in the past 6 months.
Measures
Demographic characteristics
Demographic information, such as age, gender, race/ethnicity, education, and annual household income, were collected during recruitment into the research panel and are regularly updated by Ipsos. In addition, participants were asked “Which best describes your current relationship status?” (single and not dating; single and dating/hanging out with someone; in a relationship but not living together; living together but not married; married and living together; married but not living together). We assessed sexual identity by asking “Do you consider yourself to be:” with the following response options: heterosexual or straight; gay or lesbian; bisexual; asexual; something else.
Birth control use
We asked, “During the past six months, when you were having penile–vaginal intercourse, which birth control methods did you or your partner use?” (birth control pill; Nuva ring (vaginal ring); birth control patch; birth control shot; implant; IUD; cervical cap or diaphragm; spermicidal gel, jelly, or foam; rhythm or natural family planning method; withdrawal; unsure; other; none of these). Women who reported using any type of birth control were then asked about simultaneous condom use, “When you were using birth control, which of the following applies:” (I never/sometimes/always used a condom at the same time I (or my partner) was using another form of birth control).
Healthcare visit in the past year
Participants were asked, “In the past year, did you see a healthcare provider (doctor or nurse) for 1) a well exam or yearly checkup; or 2) other reasons (e.g., feeling sick, injured, allergies, etc.) (yes/no for each type of visit).” A condensed binary variable was created to indicate if a participant saw a healthcare provider in the past year.
Patient/provider interactions regarding LARC use
Women who reported using IUD or implant in the past 6 months were asked a series of follow-up questions about the information they had received from their healthcare provider(s). We asked, “When you had your IUD inserted, how long did your healthcare provider say it would work to prevent pregnancy?” Response options ranged numerically from 1 to 9 years, 10 or more years, don’t remember, or they didn’t say. We also asked, “Has a healthcare provider told you that IUDs do not provide any protection from STDs/STIs?” Response options were: yes, they told me; no, they didn’t tell me; don’t remember. Further, we asked “Has a healthcare provider talked with you about using condoms in addition to your IUD?” (yes; no; don’t remember) and whether their provider recommended condoms for STD prevention; for additional pregnancy prevention; for both STD and pregnancy prevention; they just recommended using condoms but didn’t say why; don’t remember; other. IUD users were also asked which type of IUD they have (Mirena; Paragard; Skyla; Liletta; Kyleena; don’t remember; N/A – I no longer have an IUD). Finally, we asked how they will know when their IUD stops working and it’s time to have it removed. Response options were: my healthcare provider will tell me; I will remember to ask my healthcare provider based on how long I have had the IUD; I’ll probably get a reminder call or postcard from my healthcare provider; I’ll probably get a reminder call or postcard from the IUD manufacturer; I don’t know; other.
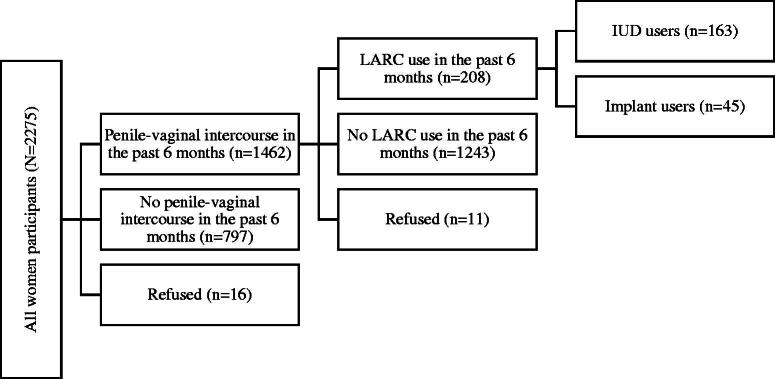
Statistical analysis
All analyses were conducted using Stata version 15 with svy commands to account for survey weights. Demographic characteristics are presented separately for sexually active women in the past 6 months reporting IUD use, implant use, or any other non-LARC contraceptive use during that time period (Figure 1). For further analysis focused on LARC use, the sample was limited only to women who reported using an IUD or implant. IUD- or implant-specific survey items were presented stratified by LARC type. How long their healthcare provider said an IUD would work to prevent pregnancy was further stratified by type of IUD because different types correspond to different lengths in their period of effectiveness. Condom use among LARC users was dichotomized to never used condoms at the same time versus sometimes/always used condoms at the same time. Combining IUD and implant users, we used weighted logistic regression to identify correlates of condom use while using LARC methods compared to those only using LARC methods without condoms (dependent variable), with the main independent variable of interest being whether provider counseling about condom use was associated with actual use. Other demographic covariates (i.e., age, race, education, income), as well as current relationship status and whether or not they had seen a provider in the past year, were entered into the final adjusted model. p-Values less than .05 were considered statistically significant.
Figure 1.
Flow chart of the study sample.
Results
Of women who reported penile–vaginal intercourse in the past 6 months, 11.2% (n = 163) reported IUD use and 3.1% (n = 45) reported implant use in the past 6 months, translating to a LARC use prevalence of 14.3% (Figure 1). Among contraceptive users, those using LARCs were significantly more likely to be 14–24 years old, though more than one-quarter of contraceptive users from ages 25–49 reported LARC use (and usually IUD use) (Table 1). LARC use was also significantly associated with annual income, with those in the lowest and highest household income brackets more often reporting LARC use.
Table 1.
Weighted Demographic Characteristics of IUD, Implant, and Non-LARC Contraceptive Users.
| IUD users (n = 163) |
Implant users (n = 45) |
Non-LARC contraceptive users (n = 566) |
||
|---|---|---|---|---|
| Row % (n) | Row % (n) | Row % (n) | p-Value | |
| Age | .026 | |||
| 14–24 | 19.2 (28) | 11.3 (16) | 69.5 (100) | |
| 25–39 | 20.4 (102) | 5.7 (28) | 73.8 (368) | |
| 40+ | 25.3 (33) | 0.4 (1) | 74.3 (98) | |
| Race/ethnicity | .320 | |||
| White, non-Hispanic | 23.4 (109) | 4.3 (20) | 72.3 (337) | |
| Black, non-Hispanic | 17.2 (18) | 10.7 (12) | 72.1 (78) | |
| Other, non-Hispanic | 23.4 (8) | 3.9 (1) | 73.8 (28) | |
| Hispanic | 17.4 (25) | 8.1 (12) | 74.5 (109) | |
| 2+ Races | 7.5 (1) | 2.9 (0) | 89.6 (14) | |
| Education | .144 | |||
| Less than high school | 13.1 (8) | 5.0 (3) | 81.9 (48) | |
| High school | 21.2 (29) | 4.8 (7) | 74.0 (103) | |
| Some college | 24.2 (62) | 9.8 (25) | 66.1 (170) | |
| Bachelor’s degree or higher | 19.9 (64) | 3.3 (11) | 76.8 (246) | |
| Annual household income | .035 | |||
| ≤$25,000 | 23.0 (19) | 5.3 (4) | 71.7 (59) | |
| $25,000–$49,999 | 15.6 (25) | 10.5 (17) | 73.9 (118) | |
| $50,000–$74,999 | 15.2 (20) | 3.9 (5) | 81.0 (108) | |
| ≥$75,000 | 24.8 (99) | 4.8 (19) | 70.5 (281) | |
| Current relationship status | .074 | |||
| Single, not dating | 7.9 (6) | 11.2 (8) | 80.9 (56) | |
| Single and dating | 17.7 (13) | 8.2 (6) | 74.2 (54) | |
| In a relationship | 18.9 (50) | 69 (18) | 74.2 (197) | |
| Married | 25.6 (93) | 3.6 (13) | 70.8 (258) | |
| Sexual identity | .719 | |||
| Heterosexual | 20.4 (143) | 5.6 (39) | 74.0 (516) | |
| Lesbian | 6.2 (16) | 0.0 (0) | 93.8 (2) | |
| Bisexual | 29.0 (19) | 7.5 (5) | 63.5 (42) | |
| Asexual | 0.0 (0) | 0.0 (0) | 100.0 (2) | |
| Something elsea | 18.7 (1) | 16.3 (1) | 65.0 (4) | |
| Seen healthcare provider in the past year | .702 | |||
| Yes | 21.2 (146) | 5.8 (40) | 73.0 (504) | |
| No | 16.4 (13) | 5.1 (4) | 78.5 (61) |
aResponses for something else included demisexual and trisexual.
Approximately 99% of IUD users reported the type of IUD they were using: Mirena (77.4%, n = 126), Paragard (12.8%, n = 21), Skyla (6.5%, n = 11), Kyleena (2.6%, n = 4), and Liletta (0). However, up to 19% of IUD users and 26% of implant users reported inaccurate information about their method’s longevity (Table 2). Regarding how they will know when to have their IUD removed, 53% reported that they will ask their provider, 30% believed their provider would inform them (17% expected to be told during a clinic visit and 13% expected a reminder call or postcard), and 10% reported not knowing (Table 3). None were relying on manufacturer information for a reminder.
Table 2.
Participants’ Perception of How Long IUDs and Implants Last.
| How long IUDs and implants last | Mirena users (n = 126) |
Paragard users (n = 21) |
Skyla users (n = 11) |
Kyleena users (n = 4) |
Implant users (n = 45) |
|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | % (n) | |
| 1 year | 0.7 (1) | 0.0 (0) | 7.3 (1) | 0.0 (0) | 3.9 (2) |
| 2 years | 2.5 (3) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 6.7 (3) |
| 3 years | 6.6 (8) | 0.0 (0) | 85.3 (9) | 18.9 (1) | 74.1 (34) |
| 4 years | 1.7 (2) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 6.0 (3) |
| 5 years | 81.3 (103) | 17.8 (4) | 0.0 (0) | 81.1 (3) | 2.2 (1) |
| 6 years | 2.3 (3) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| 7 years | 2.2 (3) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| 10 or more years | 1.7 (2) | 82.2 (17) | 7.5 (1) | 0.0 (0) | 6.0 (3) |
| Don’t remember | 1.0 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 1.0 (0) |
Note. Boldened statistics indicate the period of effectiveness recommended by the manufacturer.
Table 3.
Provider Conversations Regarding IUD and Implant Use and Simultaneous Condom Use While Using LARC Methods.
| IUD users (n = 163) |
Implant users (n = 45) |
|
|---|---|---|
| % (n) | % (n) | |
| How to know when to have IUD removed | ||
| My healthcare provider will tell me | 17.2 (28) | |
| I will remember to ask my healthcare provider based on how long I have had the IUD | 53.0 (86) | |
| I’ll probably get a reminder call or postcard from my healthcare provider | 12.9 (21) | |
| I’ll probably get a reminder call or postcard from the manufacturer. | 0.0 (0) | |
| I don’t know | 10.3 (17) | |
| Othera | 6.5 (11) | |
| Healthcare provider told you that IUDs/implants do not protect against STIs | ||
| Yes | 94.9 (155) | 90.8 (41) |
| No | 0.8 (1) | 3.5 (2) |
| Don’t remember | 4.3 (7) | 5.7 (3) |
| Healthcare provider talked about using condoms in addition to IUD/implant | ||
| Yes | 34.7 (56) | 59.8 (27) |
| No | 48.1 (78) | 34.6 (16) |
| Don’t remember | 16.3 (27) | 5.7 (3) |
| Reason for recommending condom use | ||
| For STI prevention | 47.8 (27) | 19.7 (5) |
| For additional pregnancy prevention | 5.8 (3) | 5.5 (1) |
| For both STI and pregnancy prevention | 43.1 (24) | 74.4 (20) |
| They recommended using condoms but didn’t say why | 0.6 (0) | 0.4 (0) |
| Don’t remember | 2.6 (1) | 0.0 (0) |
| Condom use while using LARC methods | ||
| Never | 75.5 (123) | 56.8 (25) |
| Sometimes | 19.3 (31) | 33.9 (15) |
| Always | 5.2 (8) | 9.4 (4) |
aRespondents who chose “other” were able to further describe in a text box; these responses include: had the IUD removed in the past month, know the removal date myself, or received a card with the removal date written down.
Nearly all LARC users (94%) reported that their healthcare provider noted that LARCs do not protect against STIs. However, only 35% of IUD users and 60% of implant users reported that their provider talked with them about also using condoms. Condom use was recommended for STI prevention purposes (48% of IUD users; 20% of implant users) as well as for combined STI and pregnancy prevention (43% of IUD users; 74% of implant users). Consistent condom use, or always using condoms at the same time, was uncommon for both IUD and implant users (5.2% and 9.4%, respectively), though 19% of IUD users and 33% of implant users reported sometimes using condoms during the past 6 months.
The likelihood of condom use among LARC users was significantly lower if their healthcare provider had not talked with them about condom use (OR = 0.34, 95% CI: 0.14–0.82) in the unadjusted model (Table 4). After adjusting for age, race/ethnicity, education, household income, current relationship status, and whether the individuals has seen a healthcare provider in the past year, the association between the healthcare provider talking about condom use and actual condom use was no longer statistically significant (aOR = 0.66, 95% CI: 0.26–1.71). Correlates of reporting condom use among LARC users included younger age, being non-White, not married, though only relationship status remained statistically significant in the adjusted model (not married vs. married aOR = 0.20, 95% CI: 0.02–1.86). Women who are older and married were more likely to have talked with their provider about condom use; Black women (as compared to White women) were less likely to have talked with their provider about condom use (data not shown).
Table 4.
Factors Associated with Condom Use While Using LARC Methods vs. Using Only LARC Methods.
| LARC only (n = 148) |
LARC + condom (n = 59) |
Unadjusted model |
Adjusted model |
|||||
|---|---|---|---|---|---|---|---|---|
| Row % (n) | Row % (n) | OR | (95% CI) | p | aOR | (95% CI) | p | |
| Healthcare provider talked about condom use | ||||||||
| Yes | 54.3 (45) | 45.8 (38) | 1.00 | 1.00 | ||||
| No | 82.7 (102) | 17.3 (21) | 0.34 | (0.14–0.82) | .017 | 0.66 | (0.26–1.71) | .390 |
| Age | ||||||||
| 14–24 | 49.0 (22) | 51.0 (22) | 1.00 | 1.00 | ||||
| 25–39 | 75.9 (98) | 24.1 (31) | 0.31 | (0.12–0.80) | .017 | 0.39 | (0.12–1.30) | .125 |
| 40+ | 83.6 (28) | 16.4 (6) | 0.19 | (0.05–0.78) | .022 | 0.21 | (0.03–1.47) | .115 |
| Race/ethnicity | ||||||||
| White, non-Hispanic | 77.7 (101) | 22.3 (29) | 1.00 | 1.00 | ||||
| Other | 61.2 (48) | 38.8 (30) | 2.21 | (1.00–4.88) | .049 | 2.26 | (0.79–6.42) | .126 |
| Education | ||||||||
| Bachelor’s degree or higher | 78.5 (58) | 21.5 (16) | 1.00 | 1.00 | ||||
| Some college | 74.1 (64) | 25.9 (23) | 1.28 | (0.55–2.95) | .564 | 0.57 | (0.20–1.65) | .299 |
| High school or less | 55.7 (26) | 44.3 (21) | 2.91 | (1.05–8.04) | .040 | 0.55 | (0.14–2.17) | .395 |
| Annual household income | ||||||||
| ≤49,999 | 67.5 (43) | 32.6 (21) | 1.00 | 1.00 | ||||
| $50,000–$74,999 | 71.2 (18) | 28.8 (7) | 0.84 | (0.29–2.45) | .747 | 1.11 | (0.28–4.41) | .886 |
| ≥$75,000 | 73.8 (87) | 26.2 (31) | 0.74 | (0.32–1.71) | .476 | 1.14 | (0.34–3.83) | .833 |
| Current relationship status | ||||||||
| Married | 85.9 (91) | 14.1 (15) | 1.00 | 1.00 | ||||
| Other | 56.1 (57) | 43.9 (44) | 4.76 | (2.10–10.81) | <.001 | 3.37 | (1.15–9.85) | .027 |
| Seen healthcare provider in the past year | ||||||||
| Yes | 71.5 (132) | 28.6 (53) | 1.00 | 1.00 | ||||
| No | 84.2 (14) | 15.8 (3) | 0.47 | (0.11–2.08) | 0.317 | 0.20 | (0.02–1.86) | .158 |
Discussion
Among our sample of U.S. cisgender women aged 14–49, the prevalence of LARC use in the past 6 months was 14.3% (with most of the LARC use being IUD use). Our prevalence rate was comparable with 2014 NSFG data, which found that 14.3% of women ages 15–44 reported current LARC use (Kavanaugh & Jerman, 2018). In the 2018 NSSHB, although we did not observe a higher rate of LARC use compared to the 2014 NSFG, prevalence rates vary with different populations, and we recruited women of a slightly broader age range (14–49 for NSSHB compared to 15–44 for NSFG). It is also recommended for clinicians to provide education/counseling regarding LARC methods and STI prevention both at LARC initiation and follow-up to ensure patients have received adequate counseling regardless of where or when they initiated the LARC method (McNicholas & Madden, 2017; Sherin & Waters, 2019).
We were encouraged to see that nearly all the IUD users in our study could identify the type of IUD they are currently using (as an initial indicator of LARC knowledge), though because our data were self-reported we could not verify the accuracy of their self-reports. Subsequent research might clinically validate women’s knowledge of which LARC they are using, given its relevance to the duration of efficacy. Although most women reported accurate information about their stated LARC method’s period of effectiveness, about one in five women reported inaccurate information and close to one-third of IUD users indicated that they are relying on their healthcare provider to inform them when to have it removed.
This dependence on healthcare providers to signal LARC removal may pose particular challenges for women who move frequently, those who do not have a regular healthcare provider, or those who rely on other venues of care (e.g., publicly funded clinics, emergency room, urgent care, college health clinics, etc.). Our results support the need to raise healthcare providers’ awareness that a sizable proportion of patients are depending on them to communicate when their IUD or implant is approaching the end of its effectiveness. To reduce the risk of unintended pregnancy while on an outdated LARC, it may be helpful to patients if their healthcare provider reviews their contraception at each office visit, letting them know about how much longer their LARC may be effective. This area seems ripe for innovation; for example, pharmaceutical companies or healthcare providers could invite LARC users to sign up to receive email or text alerts in the months prior to when their LARC needs to be removed. Such reminders may even help to reconnect patients with providers if it has been a long time since their last gynecologic exam.
Provider education on how to counsel patients on LARC use should be implemented and may thus serve as an opportunity to train providers on engaging in a broader range of sexual health issues, such as sexual pleasure (Ford et al., 2019). Given the increasing proportion of cisgender women who use LARCs, there is also a great need to improve follow-up and transfer services for patients who have initiated LARC methods. Our findings also have implications for sexual health educators, who are well-positioned to educate LARC users that the duration of LARC effectiveness varies by type (i.e., IUD vs. implant) as well as by brand (e.g., Mirena vs. Paragard vs. Skyla). Sexual health educators can encourage LARC users to be proactive about their sexual health and to initiate a conversation with their provider at least once each year about their contraceptive use and effectiveness.
Consistent condom use in the past 6 months was rare among LARC users (6.1%), though over one-fifth reported sometimes using a condom. Given the strong association between relationship status and condom use, it may be that women in monogamous relationships, or ostensibly monogamous relationships, do not feel the need to use condoms while using LARC methods because their main purpose is to prevent pregnancy and not STIs with a regular partner. Additionally, LARC use may give male partners a sense that they can have condomless sex with a lower risk of repercussions such as unintended pregnancy; subsequent research might further examine issues of gender and power in relation to dual LARC and condom use. The prevalence of any condom use in the past 6 months was 28.5% among LARC users and 40.0% among non-LARC contraceptive users in our sample. The Contraceptive CHOICE Project, a convenience sample of women ages 14–45 in St. Louis, reported 32% of LARC users reported condom use in the past 6 months (Bernard et al., 2018). Data from the NSFG showed that rates for condom use among IUD/implant users were low in both the interview month (1.8%) and at last intercourse (1.9%) (Pazol et al., 2010). Given that STI rates have been increasing annually in the U.S. (Centers for Disease Control & Prevention, 2019), our data have implications for the need for healthcare providers to talk with their patients (including LARC users) about STI risk, STI testing, and condom use.
While most women reported that their provider indicated that IUDs do not provide STI protection, few recalled actual counseling about condom use. While it is reassuring that one of the primary reasons that the provider is recommending condom use is for STI prevention, a sizeable proportion is recommending condom use for both pregnancy and STI prevention among LARC users. With the effectiveness of LARC methods for preventing pregnancy being greater than 99% (Winner et al., 2012), messages regarding condom use among LARC users should be framed to emphasize STI prevention. Prior research has demonstrated that LARC users were less likely to report condom use and more likely to acquire STIs than non-LARC users (Bastow et al., 2018; Bernard et al., 2018; Steiner et al., 2016; Walsh-Buhi & Helmy, 2018). Under this context, it would be important for healthcare providers to thoroughly and consistently counsel patients on condom use in addition to LARC methods, as well as the need for STI testing. We did find evidence of a correlation between the provider specifically talking about condoms and actual condom use in unadjusted analyses, though this association did not remain significant after accounting for other demographic factors. Current relationship status was the strongest correlate. Consistent with prior research (Bernard et al., 2018; Pazol et al., 2010; Thompson et al., 2017; Walsh-Buhi & Helmy, 2018), we found that those in a relationship were less likely to report condom use with LARC methods. Motivations for using condoms have been associated with a lack of trust or familiarity with a sexual partner (Crosby et al., 2014). Individuals in established relationships may perceive themselves as having little to no risk for STIs and use condoms less frequently. We also observed a greater likelihood of condom use among LARC users associated with younger age and with nonwhites, consistent with prior research (Bernard et al., 2018; Pazol et al., 2010), though results were not statistically significant after adjusting for potential confounders. Due to the smaller numbers of LARC users in our study, it may be that we lacked statistical power to identify such relationships. Given that younger age and racial minority status are correlated with higher STI risk, it may be that these individuals are using condoms as an extra level of protection due to perceived high risk of STIs or as a result of greater public health prevention efforts available to youth and racial/ethnic minorities (Bernard et al., 2018).
A strength of our research is that our data are from the 2018 NSSHB, which is a nationally representative probability survey of Americans across a broad age range. We included adolescents as young as 14-years-old, in recognition of the fact that people of various ages engage in partnered sexual activities (Herbenick et al., 2010), and that there is a dearth of data on younger adolescents in connection with contraceptive use and knowledge (even the NSFG begins at age 15). Our age range also extended through age 49, which is important given that midlife women are vulnerable to unintended pregnancy but less often included in contraceptive research (Johnson-Mallard et al., 2017). Additionally, data were collected online which has been shown to enhance self-report of sensitive information, including sexual health information (Burkill et al., 2016).
There are also several limitations to our study. Although a strength of our research is that the 2018 NSSHB was a U.S. nationally representative probability survey, the number of LARC users was small and should be interpreted as exploratory; subsequent research might seek to examine similar issues in larger samples of LARC users. We were further limited in certain subgroups and stratified analyses due to smaller numbers of LARC users. More specifically, we did not have the capability to examine the association between the reason that the provider recommended condom use and actual condom use due to small sample sizes. This is an important gap for future research to fill as it would generate implications on how the type of message the provider is conveying affects actual condom use. LARC methods are often used by non-binary individuals as well (Bentsianov et al., 2018; Francis et al., 2018), but we were also unable to examine LARC use among non-cisgender women, as these sample sizes are small in nationally representative studies. In addition, we were unable to examine temporal relationships between patient/provider interactions about condom use and actual condom use due to the cross-sectional nature of the study and not restricting the patient/provider interactions to a certain timeframe. Subsequent research focused on LARC user experiences are needed to further explore more detailed associations between patient–provider interactions, LARC use, and condom use, as well as perhaps in connection with the frequency of healthcare utilization, relationship status, or even relationship structure (e.g., degrees of openness and monogamy). Finally, our data relies on self-report and may be prone to recall bias. We are, however, not expecting differential levels of bias between LARC users who report condom use versus those who do not.
In conclusion, healthcare providers play a key role in women’s sexual healthcare, including their knowledge regarding LARC methods and condom use. As LARC uptake continues to grow in the U.S. and STI rates remain high, sexual health histories and healthcare counseling about condom use are critical to support patients in STI prevention. We need to disseminate a clear message to encourage dual protection against STIs and unintended pregnancies. Our findings have implications on how healthcare providers educate their patients on potential LARC use, condom use while using LARC methods, and STI prevention.
Disclosure statement
D. Herbenick has received grant funding from Church & Dwight Co., Inc. All other authors have declared no conflicts of interest.
References
- Bastow, B., Sheeder, J., Guiahi, M., & Teal, S. (2018). Condom use in adolescents and young women following initiation of long- or short-acting contraceptive methods. Contraception, 97(1), 70–75. 10.1016/j.contraception.2017.10.002 [DOI] [PubMed] [Google Scholar]
- Bentsianov, S., Gordon, L., Goldman, A., Jacobs, A., & Steever, J. (2018). Use of copper intrauterine device in transgender male adolescents. Contraception, 98(1), 74–75. 10.1016/j.contraception.2018.02.010 [DOI] [PubMed] [Google Scholar]
- Bernard, C., Zhao, Q., & Peipert, J. F. (2018). Dual method use among long-acting reversible contraceptive users. The European Journal of Contraception & Reproductive Health Care, 23(2), 97–104. 10.1080/13625187.2018.1445850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal, P. D., Voedisch, A., & Gemzell-Danielsson, K. (2011). Strategies to prevent unintended pregnancy: Increasing use of long-acting reversible contraception. Human Reproduction Update, 17(1), 121–137. 10.1093/humupd/dmq026 [DOI] [PubMed] [Google Scholar]
- Branum, A. M., & Jones, J. (2015). Trends in long-acting reversible contraception use among U.S. women aged 15-44. National Center for Health Statistics. [PubMed] [Google Scholar]
- Burkill, S., Copas, A., Couper, M. P., Clifton, S., Prah, P., Datta, J., Conrad, F., Wellings, K., Johnson, A. M., & Erens, B. (2016). Using the web to collect data on sensitive behaviours: A study looking at mode effects on the British National Survey of Sexual Attitudes and Lifestyles. PLoS One, 11(2), e0147983. 10.1371/journal.pone.0147983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter, A., Ford, J. V., Luetke, M., Fu, T.-C J., Townes, A., Hensel, D. J., Dodge, B., & Herbenick, D. (2019). “Fulfilling his needs, not mine”: Reasons for not talking about painful sex and associations with lack of pleasure in a nationally representative sample of women in the United States. The Journal of Sexual Medicine, 16(12), 1953–1965. 10.1016/j.jsxm.2019.08.016 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2019). Sexually transmited disease surveillance 2018. https://www.cdc.gov/std/stats18/
- Centers for Disease Control and Prevention . (n.d.). Condoms and STDs: Fact sheet for public health personnel. https://www.cdc.gov/condomeffectiveness/latex.html
- Crosby, R. A., Milhausen, R. R., Graham, C. A., Yarber, W. L., Sanders, S. A., Charnigo, R., & Shrier, L. A. (2014). Condom use motivations and selected behaviours with new versus established sex partners. Sexual Health, 11(3), 252–257. 10.1071/SH13159 [DOI] [PubMed] [Google Scholar]
- Ford, J. V., Corona Vargas, E., Finotelli Jr, I., Fortenberry, J. D., Kismödi, E., Philpott, A., Rubio-Aurioles, E., & Coleman, E. (2019). Why pleasure matters: Its global relevance for sexual health, sexual rights and wellbeing. International Journal of Sexual Health, 31(3), 217–230. 10.1080/19317611.2019.1654587 [DOI] [Google Scholar]
- Foster, D. G., Rostovtseva, D. P., Brindis, C. D., Biggs, M. A., Hulett, D., & Darney, P. D. (2009). Cost savings from the provision of specific methods of contraception in a publicly funded program. American Journal of Public Health, 99(3), 446–451. 10.2105/AJPH.2007.129353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis, A., Jasani, S., & Bachmann, G. (2018). Contraceptive challenges and the transgender individual. Women’s Midlife Health, 4(1), 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu, T. C., Hensel, D. J., Beckmeyer, J. J., Dodge, B., & Herbenick, D. (2019). Considerations in the measurement and reporting of withdrawal: Findings from the 2018 National Survey of Sexual Health and Behavior. The Journal of Sexual Medicine, 16(8), 1170–1177. 10.1016/j.jsxm.2019.05.022 [DOI] [PubMed] [Google Scholar]
- Goldstuck, N. D., & Steyn, P. S. (2013). Intrauterine contraception after cesarean section and during lactation: A systematic review. International Journal of Women’s Health, 5, 811–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimes, D. A. (2009). Forgettable contraception. Contraception, 80(6), 497–499. 10.1016/j.contraception.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Grubb, L. K. (2020). Barrier protection use by adolescents during sexual activity. Pediatrics, 146(2), e2020007237. 10.1542/peds.2020-007237 [DOI] [PubMed] [Google Scholar]
- Harper, C. C., Rocca, C. H., Thompson, K. M., Morfesis, J., Goodman, S., Darney, P. D., Westhoff, C. L., & Speidel, J. J. (2015). Reductions in pregnancy rates in the USA with long-acting reversible contraception: A cluster randomised trial. Lancet, 386(9993), 562–568. 10.1016/S0140-6736(14)62460-0 [DOI] [PubMed] [Google Scholar]
- Hartnett, C. S., Lindley, L. L., & Walsemann, K. M. (2017). Congruence across sexual orientation dimensions and risk for unintended pregnancy among adult US women. Women’s Health Issues, 27(2), 145–151. 10.1016/j.whi.2016.10.010 [DOI] [PubMed] [Google Scholar]
- Herbenick, D., Reece, M., Schick, V., Sanders, S., Dodge, B., & Fortenberry, J. D. (2010). Sexual behavior in the United States: Results from a national probability sample of men and women ages 14-94. The Journal of Sexual Medicine, 7, 255–265. 10.1111/j.1743-6109.2010.02012.x [DOI] [PubMed] [Google Scholar]
- Higgins, J. A., & Cooper, A. D. (2012). Dual use of condoms and contraceptives in the USA. Sexual Health, 9(1), 73–80. 10.1071/SH11004 [DOI] [PubMed] [Google Scholar]
- Higgins, J. A., Kramer, R. D., & Ryder, K. M. (2016). Provider bias in long-acting reversible contraception (LARC) promotion and removal: Perceptions of young adult women. American Journal of Public Health, 106(11), 1932–1937. 10.2105/AJPH.2016.303393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins, K., Hubert, C., Coleman-Minahan, K., Jean Stevenson, A., White, K., Grossman, D., & Potter, J. (2018). Community college students want to use more effective birth control methods but can’t always get what they want. PRC Research Brief, 3(5), 1–2. [Google Scholar]
- Ihongbe, T. O., & Masho, S. W. (2018). Changes in the use of long-acting reversible contraceptive methods among U.S. nulliparous women: Results from the 2006-2010, 2011-2013, and 2013-2015. Journal of Women’s Health, 27(3), 245–252. 10.1089/jwh.2017.6609 [DOI] [PubMed] [Google Scholar]
- Johnson-Mallard, V., Kostas-Polston, E. A., Woods, N. F., Simmonds, K. E., Alexander, I. M., & Taylor, D. (2017). Unintended pregnancy: A framework for prevention and options for midlife women in the US. Women’s Midlife Health, 3(1), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalra, N., Ayankola, J., & Babalola, S. (2019). Healthcare provider interaction and other predictors of long-acting reversible contraception adoption among women in Nigeria. International Journal of Gynaecology and Obstetrics, 144(2), 153–160. 10.1002/ijgo.12705 [DOI] [PubMed] [Google Scholar]
- Kavanaugh, M. L., & Jerman, J. (2018). Contraceptive method use in the United States: Trends and characteristics between 2008, 2012 and 2014. Contraception, 97(1), 14–21. 10.1016/j.contraception.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanaugh, M. L., Jerman, J., & Finer, L. B. (2015). Changes in use of long-acting reversible contraceptive methods among US women, 2009–2012. Obstetrics and Gynecology, 126(5), 917–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNicholas, C. P., Klugman, J. B., Zhao, Q., & Peipert, J. F. (2017). Condom use and incident sexually transmitted infection after initiation of long-acting reversible contraception. American Journal of Obstetrics and Gynecology, 217(6), 672.e1–672.e6. 10.1016/j.ajog.2017.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNicholas, C. P., & Madden, T. (2017). Meeting the contraceptive needs of a community: Increasing access to long-acting reversible contraception. Missouri Medicine, 114(3), 163–167. [PMC free article] [PubMed] [Google Scholar]
- Mosher, W. D., Moreau, C., & Lantos, H. (2016). Trends and determinants of IUD use in the USA, 2002–2012. Human Reproduction, 31(8), 1696–1702. 10.1093/humrep/dew117 [DOI] [PubMed] [Google Scholar]
- Murphy, M. K., Stoffel, C., Nolan, M., & Haider, S. (2016). Interdependent barriers to providing adolescents with long-acting reversible contraception: Qualitative insights from providers. Journal of Pediatric and Adolescent Gynecology, 29(5), 436–442. 10.1016/j.jpag.2016.01.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Sullivan, L. F., Majerovich, J. A., & Milliken, M. (2019). A national survey of the provision of sexual health clinical services by public health in Canada: First insights. International Journal of Sexual Health, 31(1), 17–25. [Google Scholar]
- Pazol, K., Kramer, M. R., & Hogue, C. J. (2010). Condoms for dual protection: Patterns of use with highly effective contraceptive methods. Public Health Reports, 125(2), 208–217. 10.1177/003335491012500209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter, J., & Soren, K. (2016). Long-acting reversible contraception and condom use: We need a better message. Journal of Amercian Medical Association Pediatrics, 170(5), 417–418. [DOI] [PubMed] [Google Scholar]
- Ramseyer Winter, V., & Ruhr, L. R. (2017). Body appreciation and contraceptive use among college women: A brief report. International Journal of Sexual Health, 29(2), 168–172. 10.1080/19317611.2016.1259707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherin, M., & Waters, J. (2019). Long-acting reversible contraceptives for adolescent females: A review of current best practices. Current Opinion in Pediatrics, 31(5), 675–682. 10.1097/MOP.0000000000000811 [DOI] [PubMed] [Google Scholar]
- Sister Song . (n.d.). Reproductive justice. https://www.sistersong.net/reproductive-justice
- Steiner, R. J., Liddon, N., Swartzendruber, A. L., Rasberry, C. N., & Sales, J. M. (2016). Long-acting reversible contraception and condom use among female US high school students: Implications for sexually transmitted infection prevention. Journal of American Medical Association Pediatrics, 170(5), 428–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, E. L., Vamos, C. A., Griner, S. B., Logan, R., Vazquez-Otero, C., & Daley, E. M. (2017). Sexually transmitted infection prevention with long-acting reversible contraception: Factors associated with dual use. Sexually Transmitted Diseases, 44(7), 423–427. 10.1097/OLQ.0000000000000620 [DOI] [PubMed] [Google Scholar]
- Trussell, J., Henry, N., Hassan, F., Prezioso, A., Law, A., & Filonenko, A. (2013). Burden of unintended pregnancy in the United States: Potential savings with increased use of long-acting reversible contraception. Contraception, 87(2), 154–161. 10.1016/j.contraception.2012.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trussell, J., Leveque, J. A., Koenig, J. D., London, R., Borden, S., Henneberry, J., LaGuardia, K. D., Stewart, F., Wilson, T. G., & Wysocki, S. (1995). The economic value of contraception: A comparison of 15 methods. American Journal of Public Health, 85(4), 494–503. 10.2105/ajph.85.4.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler, C. P., Whiteman, M. K., Kraft, J. M., Zapata, L. B., Hillis, S. D., Curtis, K. M., Anderson, J., Pazol, K., & Marchbanks, P. A. (2014). Dual use of condoms with other contraceptive methods among adolescents and young women in the United States. The Journal of Adolescent Health: official Publication of the Society for Adolescent Medicine, 54(2), 169–175. 10.1016/j.jadohealth.2013.07.042 [DOI] [PubMed] [Google Scholar]
- Walsh-Buhi, E. R., & Helmy, H. L. (2018). Trends in long-acting reversible contraceptive (LARC) use, LARC use predictors, and dual-method use among a national sample of college women. Journal of American College Health, 66(4), 225–236. 10.1080/07448481.2017.1399397 [DOI] [PubMed] [Google Scholar]
- Whitaker, A. K., Dude, A. M., Neustadt, A., & Gilliam, M. L. (2010). Correlates of use of long-acting reversible methods of contraception among adolescent and young adult women. Contraception, 81(4), 299–303. 10.1016/j.contraception.2009.11.008 [DOI] [PubMed] [Google Scholar]
- Williams, R. L., & Fortenberry, J. D. (2013). Dual use of long-acting reversible contraceptives and condoms among adolescents. The Journal of Adolescent Health, 52(4), S29–S34. 10.1016/j.jadohealth.2013.02.002 [DOI] [PubMed] [Google Scholar]
- Winner, B., Peipert, J. F., Zhao, Q., Buckel, C., Madden, T., Allsworth, J. E., & Secura, G. M. (2012). Effectiveness of long-acting reversible contraception. The New England Journal of Medicine, 366(21), 1998–2007. 10.1056/NEJMoa1110855 [DOI] [PubMed] [Google Scholar]
- World Association for Sexual Health . (2014). Declaration of sexual rights. https://worldsexualhealth.net/resources/declaration-of-sexual-rights/