Abstract
Objective: This review summarizes evidence pertaining to the impact of the COVID-19 pandemic on the psychological health of children and adolescents with autism spectrum disorder (ASD).
Materials and Methods: An electronic search was conducted using four major databases: PubMed, ScienceDirect, Web of Science, and Google Scholar. Using an umbrella methodology, the reference lists of relevant papers were reviewed, and citation searches were conducted. The study included articles written in English between January 2020 and March 2021 that focused on the psychological health of autistic children and adolescents.
Results: All eight studies included in the final review were cross-sectional. Three of the eight studies were conducted in Italy, two in Turkey, and one study each in Portugal, Spain, and the United Kingdom, with a total of 1,407 participants. All studies used a mixture of standardized and non-standardized questionnaires to collect data. The total number of patients were 1407 at a mean age of 9.53 (SD = 2.96) years. Seven studies report gender; male 74.7% (657/880) and female 25.3% (223/880). The finding showed that behavioral issues in children and adolescents with ASD have significantly increased; 521 (51.9 percent) of the 1004 individuals with ASD presented with behavioral changes, including conduct problems, emotional problems, aggression, and hyperactivity. Some studies also found increased anxiety and difficulties managing emotions. Only one study reported clinical stabilization in children with ASD during COVID-19. Finally, 82.7% of families and caregivers of children with ASD (544 out of 658) faced challenges during COVID-19.
Conclusion: Although the studies in this review suggest a general worsening of ASD children's clinical status, it remains difficult to draw definitive conclusions at this moment, with newer COVID-19 variants on the rise worldwide. During this difficult pandemic period, caregivers, families, and healthcare professionals are recommended to pay more attention to the ASD patients’ health and care needs.
Keywords: COVID-19, pandemic, autism spectrum disorder, anxiety, depression, behavioral impact, psychological impact, mental health
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disability that is characterized by impairments in social communication and restricted, repetitive behavioral patterns. According to the fifth edition of the American Psychiatric Association’s Diagnostic and Statistical Manual, ASD may or may not be accompanied by intellectual impairment and linguistic difficulties (APA 2013). In the US, 1 in 59 children has ASD, and the prevalence is four times higher in boys than in girls. American children are diagnosed with ASD with an average of 4.3 years of age (Baio et al. 2018).
The Center for Disease Control and Prevention (CDC) reports that the diagnosis of ASD occurs by identifying behavioral, social, and cognitive symptoms, with varying degrees of impairment (CDC 2020). Red flags (inability to recognize one's name, difficulty talking, and avoidance of eye contact in the first year of life) can be identified by the end of the first year of life, but the majority (80-90%) of tutors/parents observe these signs by the end of the second year of life (CDC 2020, Lazenby et al. 2016, Miller et al. 2017, Moriuchi et al. 2017). Behaviors, activities and interests that are restrictive and repetitive behaviors (RRBs) are also an important domain required for the diagnosis of Autism disorder. RRBs manifest in autism in a variety of ways, including repetitive use of speech or objects, motor mannerism, intense interests, and atypical sensory responses, all of which are of immense importance for children with autism (Jacques et al. 2018). Social skills are imperative factors in children with ASD, who can have difficulty expressing their feelings and understanding those of others (Chaidi and Drigas 2020). Some behavioral characteristics, such as obsession with a certain object or the need to maintain an organized and unchanged routine, are often observed (Turner-Brown 2020).
On March 11, 2020, the World Health Organization (WHO) declared COVID-19 as a worldwide pandemic (WHO 2020b). Social distancing, hygiene care, handwashing, and masks in public environments have since been highly recommended for prevention of disease (Cucinotta and Vanelli 2020). Therefore, lockdowns have been implemented globally to slow down viral transmission through physical distancing and movement restriction. These measures may have a negative impact on individuals and communities as they lead to economic and social shocks (WHO 2020a). COVID-19 containment measures have particularly disrupted the daily routines of children, mainly due to closures of schools, because children spend the majority of their day at home, with restricted outdoor movement and decreased social interactions (Francisco et al. 2020). The changes that occurred due to the COVID-19 pandemic, such as social detachment and economic issues, have affected society psychologically, mainly with reports of cases of anxiety and depression (Özdin and Bayrak Özdin 2020). The COVID-19 pandemic and lockdown impacts have revealed increased irritability, clinginess, and lack of attention in children across all ages. As reported by parents, children also experienced uncertainty, fear, and isolation, as well as sleep disturbances and decreased appetite. It is also expected that the pandemic may have long-term implications in children (Singh et al. 2020). There have been some unique challenges in children with ASD during the Covid-19 pandemic and overall worsening of symptoms like irritability, anxiety, and emotional dysregulation (Colizzi et al. 2020, Türkoğlu et al. 2020). The disrupted normal daily activities of living of many families that prevent them from converging and gathering are relevant to children with ASD who adhere to rigid schedules. Not only the children but their families are largely impacted, who are required to meet the special needs of their children and also protect them from contacting COVID-19, thereby deteriorating their psychological health. In a study conducted by Kuloğlu-Aksaz, 2001, it was found that mothers who have children with autism and Down syndrome had higher levels of depression, state anxiety, and trait anxiety than mothers of normal children (Ersoy et al. 2020, Mutluer et al. 2020). The suspension of in-person education, extracurricular, social activities, and routine healthcare has threatened children’s mental well-being. The COVID-19 has disproportionally affected children with ASD. The disruption in their usual medical care is likely to result in increase in missed autism diagnoses as ASD screenings have been postponed or cancelled. Children with ASD have difficulties with social communication and therefore social isolation makes this impossible. COVID-19 has made their routine unpredictable. Speech therapy and applied behavior analysis (ABA), like many other services, have been impacted by logistical challenges (Bellomo et al. 2020).
The aim of this article is to review and examine the psychological impact of the COVID-19 pandemic on autistic children and adolescents in order for clinicians to gain a better understanding of and preparedness for dealing with these children and families during COVID-19 pandemic or any other natural disaster. This study not only describes the various challenges faced by ASD children and adolescents, but it also emphasizes the importance of continuing skill development for the ASD population in preparation for future emergencies.
Materials and methods
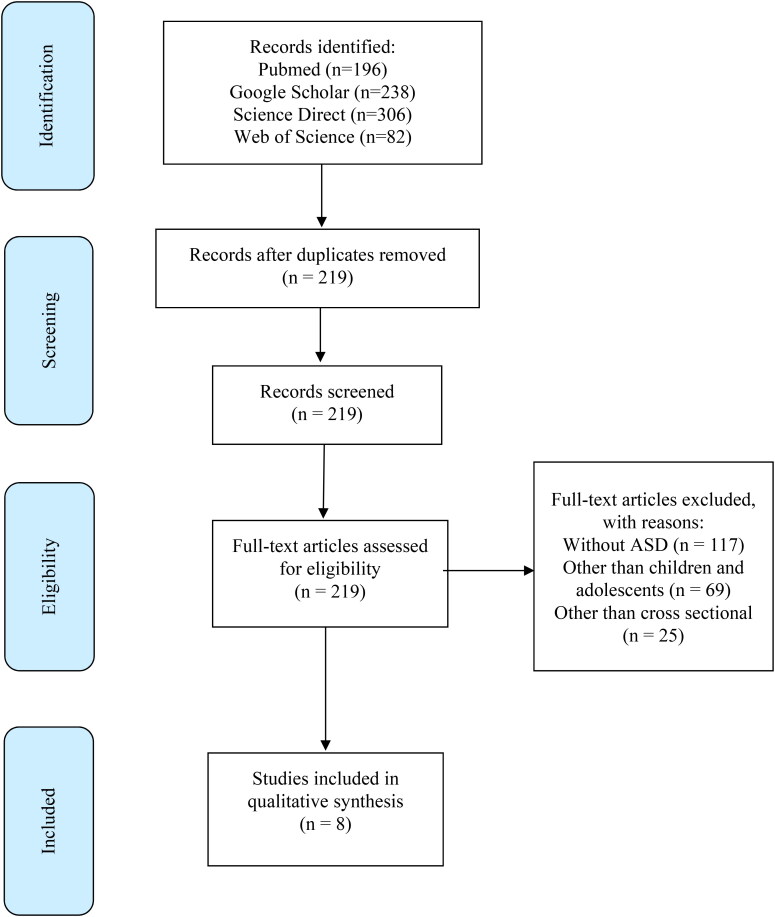
Two authors (S.S. and I.K.) appraised all the studies and extracted data onto a shared spreadsheet to shortlist studies for screening; the authors subsequently identified biases and limitations for quality appraisal. The eligibility criteria are appended in Table 1. A total of 822 records were found in the initial literature search: (i) 196 from PubMed, (ii) 306 from Science Direct, (iii) 82 from Web of Science, and (iv) 238 from Google Scholar. The search strategy (i.e. keywords combination) was first tested in PubMed before being adapted for application in the other three databases (Science Direct, Web of Science, and Google Scholar). After removing duplicated results and applying inclusion and exclusion criteria, a total of 8 studies were included in this review.
Table 1.
Demographic characteristics and important findings of selected studies.
| Author, Year | Country | Sample | Male | Female | Mean age (yrs) | Important Findings |
|---|---|---|---|---|---|---|
| Amorim et al. 2020 | Portugal | 43 children with ASD and 56 controls | 68 | 31 | 10.75 ± 3.13 | Autistic children had higher levels of anxiety in comparison to non-autistic controls. Autistic children faced difficulties in emotion management. |
| Colizzi et al. 2020 | Italy | 527 children with ASD | NR | NR | 13 ± 8.1 | Autistic children presented with intense, disruptive behavioral problems during the lockdown. Children with pre-existing behavior problems had worsening of behavior. |
| Mumbardo-Adam et al. 2021 | Spain | 47 children and adolescents with ASD | 36 | 11 | 7.3 ± 3.4 | More than half of the autistic children became much happier and calmer during the pandemic. |
| Mutluer et al. 2020 | Turkey | 87 children and adolescents with ASD | 72 | 15 | 13.96 ± 6.1 | Autistic children had sleep and appetite disturbances, worsened aggression, hypersensitivity and increased stereotypies. |
| Nonweiler et al. 2020 | United Kingdom | 453 children with neurodevelopmental disorders (106 with ASD) | 320 | 133 | 10.4 ± 3.1 | Autistic children experienced worsening in emotional symptoms as well as behavioral difficulties during the pandemic, especially girls. |
| Türkoğlu et al. 2020 | Turkey | 46 children with ASD | 38 | 08 | 7.89 (range = 4-17) | Autism Behavioral Checklist (AuBC) scores worsened from 56.41 before the start of the pandemic to 68.36 during the COVID-19 home confinement period. |
| Di Renzo et al. 2020 | Italy | 63 children with ASD | 55 | 08 | 5.9 ± 1.7 | Children with ASD experienced an increase in restricted and repetitive behaviors, mannerisms, and stereotypies, as well as motor restlessness, irritability, sleep disturbances, and mood dysregulation. |
| Siracusano et al. 2021 | Italy | 85 children with ASD | 68 | 17 | 7 (range = 2-18) | Repetitive behaviors and adaptive functioning of autistic children were not affected by the pandemic however, there was clinical stability in adaptive functioning in autistic schoolers while improved adaptive capacity in autistic preschoolers. |
ASD: Autism Spectrum Disorder.
Eligibility criteria
Studies were considered for review if they met the following requirements:
Studies that have assessed the psychological and emotional health of children with ASD during the Covid-19 pandemic
Studies reporting and analysing detailed reports of surveys directed towards the mental health of children with ASD across various geographical groups
Studies published in the English language
Studies between January 2020 to March 2021
Studies with the following conditions were excluded:
Studies on individuals of all ages without ASD
Studies on adults with ASD
Conference posters, workshops, case reports, case series, reviews, opinions, and commentaries
Non-English language literature
Sources of information
The authors searched the literature from January 2020 to March 2021 to retrieve peer-reviewed english-language research concerning the impact of the COVID-19 pandemic on children with autism spectrum disorder (ASD). The search for the studies was conducted using the subject medical headings applying the BOOLEAN logic (and/or): ‘Coronavirus’ or ‘COVID19’ or ‘SARS-CoV-2′, ‘Autism spectrum disorder’ or ‘ASD’ or ‘Autism’, ‘psychological challenges’ or ‘psychological impact’ or ‘mental health’ or ‘Depression’ or ‘Anxiety’ or ‘PTSD’ or ‘Trauma’, and ‘Pandemic’ or ‘Lockdown’. 'Cohen's coefficient of the agreement was computed to quantify the inter-reviewer agreement. The preferred reporting items are given in the PRISMA flow diagram as depicted in Figure 1.
Figure 1.
PRISMA flow diagram showing the identification of records from various databases, the screening and eligibility of articles and the number of articles included in the qualitative synthesis.
Results
The overall Kappa score calculated for the inter-reviewer agreement was 0.93.
Demographic characteristics of included participants
All the 8 studies that were included for final review were cross sectional (100%). From the 8 studies, three (37.5%) were carried out in Italy, two (25%) in Turkey, and one (12.5%) study each was done in Portugal, Spain, and the United Kingdom. The total number of patients were 1407 at a mean age of 9.53 (SD = 2.96) years. Seven studies report gender; male 74.7% (657/880) and female 25.3% (223/880). A total of 1004 subjects had ASD (Table 1)
Behavior
The majority of studies found significant behavioral dysregulation (Amorim et al. 2020, Colizzi et al. 2020, Di Renzo et al. 2020, Mutluer et al. 2020, Nonweiler et al. 2020, Türkoğlu et al. 2020). Children with ASD who had pre-existing behavioral problems or comorbidities (i.e. Neuromotor conditions, Gastrointestinal conditions, Allergies and food sensitivity etc.) were 2.16 times more likely to have more severe behavior problems than those who did not (Colizzi et al. 2020). Siracusano et al. 2021 also observed similar findings, reporting worsening behavioral symptoms during quarantine.
In total, 521 (51.9%) of the 1004 children with ASD who were analyzed experienced behavioral changes, which included: Anxiety, irritability, restlessness, anger, lethargy, social withdrawal, stereotyped behavior, inappropriate speech, and hyperactivity were the most common symptoms (Amorim et al. 2020, Colizzi et al. 2020, Di Renzo et al. 2020, Mutluer et al. 2020, Nonweiler et al. 2020, Türkoğlu et al. 2020). 33.6% of parents reported intensification of autistic typical symptoms in the last month, 14% reported an increase in restricted and repetitive behavior, 1.6% increase in mannerism, 14% motor stereotypies and 3.2% vocal stereotypes (Di Renzo et al. 2020). Anxiety was more prevalent in children who did not follow routines than in those who did (8.75 ± 0.96 vs. 5.36 ± 2.71, p < 0.001) (Amorim et al. 2020). Overall, behavior changes were reported by caregivers in 51.9% of the 6 included studies (N = 1004), with 85 children reporting non-significant changes in RBS-R and CBCL questionnaire analyses. In contrast to the majority of studies, parents in one study reported that their children were happier and calmer than before quarantine (40.4%) (Mumbardó-Adam et al. 2021).
The majority of parents of children with ASD (55.8%) reported negative effects on their children's emotion regulation, including social isolation (41.4%), inability to play outside (13.1%), routine changes (11.1%), boredom (9.1%), and remote school classes (7.1%) (Amorim et al. 2020). Children with neurodevelopmental abnormalities exhibited a significantly greater prevalence of emotional symptoms (42%), conduct problems (28%), and prosocial behaviors (22%) (Nonweiler et al. 2020). Obsession (11.1%) was also observed in ASD children during COVID-19 quarantine (Amorim et al. 2020).
Learning
Amorim et al. reported that during quarantine, when ASD children were supported, they maintained their routines (83.8%) and the experience of learning something new (52.5%) However, when there was little to no support, and the negative impact of quarantine exceeded the positive impact (46.5% vs. 19.6%) (Amorim et al. 2020). Similarly, children with ASD had challenges in having structured activities (75.5%) which caused disturbance in learning (Colizzi et al. 2020). One study reported that fewer children were learning new negative stereotypes, such as pulling their own ears or speaking with a louder tone of voice. The survey also showed that many children (14.9%) began to take care of themselves (personal hygiene, dressing, and eating) (Mumbardó-Adam et al. 2021). When parents were interviewed, they reported that they organized their daily schedules with their children and used new reinforcements (Mumbardó-Adam et al. 2021). Because of the quarantine, families had time to teach their children new talents (Mumbardó-Adam et al. 2021). During the quarantine, parents reported no changes in self-care skills, such as toilet use, washing, or dressing (Di Renzo et al. 2020, Siracusano et al. 2021).
Parents and caregivers
Majority of parents evaluated the current period of change as challenging (93.9%) (Colizzi et al. 2020). Caregivers reported higher mean scores of anxiety levels in themselves than in their children (Amorim et al. 2020). The challenges faced by caregivers during quarantine include child teaching (26.3%), dealing with children's behavior (26.3%), maintaining routines (16.2%), keeping children occupied (13.1%), and social isolation (5.1%) (Amorim et al. 2020). Parents also reported difficulty in managing their children’s meals (23%), autonomies (31%), and free time (78.1%) (Colizzi et al. 2020). Most of the parent anxiety corresponds with an increase in child behavior traits of irritability, lethargy, hyperactivity, inappropriate speech, and self-injury (Mutluer et al. 2020). Significant improvement in general ability of children with ASD emerged in parental work continuation during lockdown compared to ASD with no continuation of their usual job (Siracusano et al. 2021). Parents who continued working did not report significant improvement in their child’s functioning (Siracusano et al. 2021). However, some parents of ASD children reported high scores for their general management of quarantine as a family (Mumbardó-Adam et al. 2021). They developed new strategies to better manage quarantine with their ASD children such as involving children in more family routines and activities, creating activities, and visual support (Mumbardó-Adam et al. 2021). Useful supports for such parents were family cohesion and online contact with relatives, online psychological support, being allowed to go out for walk, more free time and job flexibility. Setting new routines (Mumbardó-Adam et al. 2021).
The studies showed that most of the parents had difficulty managing the situation due to anxiety and stress, which ultimately affected the symptoms of ASD in their children.
Psychosocial support
Support from the local health services, both direct and indirect school support, as well as private therapists, was helpful during the quarantine period (Colizzi et al. 2020). The study by Colizzi emphasized that there is a need for in-home health care support, center-based healthcare support, loosening quarantine restrictions, and in hospital healthcare support, ending lockdown (Colizzi et al. 2020). Few families were supported through online sessions with children, families, phone calls, or emails (Mumbardó-Adam et al. 2021). Due to psychosocial support, there was improvement in the quality of relationships and play between siblings as well as progress in verbal communication and non-verbal communication (Di Renzo et al. 2020). Psychosocial support helped with greater attention to and engagement in activities such as homework, drawing, or playing (Di Renzo et al. 2020). Parents who underwent online parental support during the lockdown found their children had significant improvement in their ASD symptoms as compared to parents who did not (Siracusano et al. 2021). However, none of the children benefited from any online special education (Türkoğlu et al. 2020). The majority of studies indicate that psychosocial support via the Internet and online sessions improved the behavior and emotional disturbances of both children with ASD and their parents.
Sleep
Sleep disturbances were identified in some studies included in this review (Mutluer et al. 2020, Türkoğlu et al. 2020). Children with ASD who were confined at home experienced more disruption in their circadian rhythm than children who were not confined. In the majority of cases, there was a substantial escalation in ASD symptoms as a result of the children's sleep and circadian rhythm disruption (Türkoğlu et al. 2020). Sleep regulation issues, difficulty falling asleep, nocturnal awakenings, and difficulty waking up were also observed by Di Renzo et al. 2020.
Critical appraisal
First, the response rates of the participants were rather low or not reported in the majority of the studies. The exceptions were Siracusano et al. 2021, where 8 participants declined out of 119 eligible participants, and Di Renzo et al. 2020, where all individuals who met the eligibility criteria participated. The low response rates of the remaining studies might have introduced underestimation of the observed effects if the participants who experienced more negative outcomes were less likely to participate in the studies. Second, although the questionnaires used were validated and established instruments, they are prone to social desirability bias. Thus, it may reasonably assume that the severity and frequency of negative events were under-reported by the participants. Third, in the context of quarantine, only Mumbardó-Adam et al. (2021) and Colizzi et al. (2020) detailed the support received by participants, which were not adequately described in the other studies. Thus, the reported results might be confounded by the level and type of support received by participants. Providing this information is also useful to generalize the findings to other settings as shown in Table 2. Although, the severity of ASD in the sample can vary and can itself have an impact on the findings of mental health impact, but unfortunately most of the included studies in this review article have not mentioned the severity of ASD in participants.
Table 2.
Critical appraisal of autistic studies.
| Author Names | Sample Selection |
Measurements and Analysis |
Overall Grading |
|||
|---|---|---|---|---|---|---|
| Selection of Participants | Retaining Participants | Measurements | Statistical Analysis | Interpretation | Discussion | |
| Amorim et al. 2020 |
|
Not Applicable. |
|
Acceptable. | Unproven Chi-square interpretations on the three levels of responses. | Balanced |
| Colizzi et al. 2020 | Time duration of ASD diagnosis was not provided | Not Applicable. | The survey was specifically designed by physicians, psychologists and ASD parents raising a major concern if parents were actively involved in the survey and participation in survey. | The adjusted odds ratio (OR) should be computed. | Parenting and comorbid medical conditions seem to be confounders in the reported findings. | The design and methods are not sufficiently detailed. Thus, the "qualitative" responses need to be interpreted with caution. |
| Mumbardo- Adam et al. 2010 |
|
Not Applicable. |
|
Acceptable. | Proportional with the reported frequencies. | Balanced |
| Mutluer et al. 2020 | Low response rate (46%) of the participants is highly concerning since the study was conducted on the patient database of a university hospital. | Not Applicable. | Suitable as based on validated questionnaires. | Satisfactory, however the pairing of ANOVA and Spearman is questionable. | - The Anxiety Score Table (Table 5) is controversial. The correlation of two assessment tools (ABC and BAI) is highly misleading. Categorizing BAI to tertile and analyzing OR based on ABC sub-scores (Predictive modelling) might be more appropriate. | BAI total score analysis was not sufficiently supported in the discussion. |
| Nonweiler et al. 2020 | Convenience sampling techniques may introduce selection bias. | Not Applicable. | The use of SDQ is appropriate | Acceptable. | Appropriate as supported by the Pair-wise comparison of study groups | - The diagnosis of ASD and ADHD were a limitation and hence were not mentioned in the discussion. -Increased chance of misclassification as data is self-reported. |
| Di Renzo et al. 2020 | All eligible participants were included in the analysis. | Not explicitly discussed. | The assessment instruments (ABAS II; ASDBI) were acceptable. However, the rationale of not using the remaining SSP was not presented. | Acceptable. | The Multivariate ANOVA (MANOVA) assessment tool was correctly interpreted. | The limitations of measurement techniques used in the studies (Altena et al. 2020, Becker and Gregory 2020, Golberstein et al. 2020) were not clearly discussed. |
| Türkoğlu et al. 2020 | The justifications for the unmet inclusion criteria were not presented. Likewise, the exclusion of ASD participants with any chronic physical disease and neurodevelopmental disorders is questionable. | Not Applicable. | The assessment instruments were acceptable. | The CSHQ questionnaire does not provide interval-type variables. Thus, Table 3 is doubtful. | The assessment of mediation effects requires a large sample size. Therefore, the non-significance reported is misleading. | The results are supported by the discussion; however, the results were derived from indeterminate methods. |
| Siracusano et al. 2021 | The selection and eligibility of study participants from the database pool was not detailed. | Efforts to lower the re-opening phase (T1) drop-outs is not provided. By rescheduling appointments, or through personalized invitations the dropouts could have been avoided. | Suitable assessments used. | Acceptable. | In line with the reported results | The authors acknowledged the non-uniformity of the time difference between baseline clinical evaluation (T0) and re-opening phase (T1) participants in Table 1. However, the proposed solution of inserting time difference as an independent variable was ambiguous. |
ASD: Autism Spectrum Disorder; ABC: Aberrant Behaviour Checklist; BAI: Beck Anxiety Inventory; SDQ: Strengths and Difficulties Questionnaire; ADHD: Attention Deficit Hyperactivity Disorder; ABAS II: Adaptive Behaviour Assessment System-II; ASDBI: Autism Spectrum Disorder Behaviour Inventory; SSP: Short Sensory Profile; CSHQ: Children’s Sleep Habit Questionnaire;.
Discussion
Pandemics and mental health have a well-established link, including the emergence of new psychological conditions and the worsening of pre-existing psychiatric conditions such as anxiety, depression, and post-traumatic stress disorder. Previously, pandemics, such as the Ebola virus, caused serious mental health implications owing to the loss of life, grief and despair experienced not only by patients and family members, but also by health-care workers (Tucci et al. 2017). This review identified a large number of families challenged in the context of quarantine-induced outcomes (82.7%). There is a link between social isolation and poor mental health in a similar context, and isolation is frequently seen in pandemics such as COVID-19. There is a high cost associated with COVID-19 quarantine and social distancing interventions, as well as a severe sense of social isolation and loneliness, which can have serious physical and mental health consequences (Hwang et al. 2020). The impact might be disproportionately amplified with pre-existing mental illness. Such isolation becomes incredibly difficult for vulnerable populations, such as those who have autism. These individuals are likely to experience social isolation in general, and prolonged isolation and quarantine can have a negative impact on their mental health.
When compared to children without autism spectrum disorder, children with autism spectrum disorder are disproportionately affected by stressful environments. The factors that may induce stress in children include separation anxiety, trauma, which may be physical and/or emotional, unfamiliar situations, bullying, as well as punishments (Theoharides and Kavalioti 2019). An unexpected sudden change in environment may manifest as increased anxiety, social and learning issues (Theoharides and Kavalioti 2019). It is difficult for ASD children to verbalize how they feel under stress due to social and language development issues, resulting in more suppressed behavioral maladaptation compared to children who do not have social and language issues. Autistic children have difficulties with working memory, a component of executive functions that is an important component of cognition and critical to meeting educational goals. Stress invariably affects this domain (Tager-Flusberg 1999, Wang et al. 2017), with stress caused by pandemic leading to more educational issues in this clinical population.
Six of the eight studies included in this review reported behavioral problems in children with ASD that increased during the pandemic. Amorim et al and Colizzi et al studies were for one month (April 2020) in Portugal and Italy respectively, Di Renzo et al study was from February to April 2020 in Italy, Nonweiler et al study was from April to June 2020 in the United Kingdom, Mutluer et al study was during the lockdown (time period unspecified) in Turkey. Mumbardo-Adam et al conducted their study in April 2020 in Spain; Siracussano et al study was from March to April 2020 in Italy, and lastly, Turkoglu et al study was from April to May 2020 in Turkey. The prevalence was documented to be 51.9% out of the 1004 individuals analyzed. Studies have shown that children with ASD are at an increased risk of anxiety, which can lead to an exacerbation of ASD symptoms and behavioral problems (Hallett et al. 2013, Pugliese et al. 2013, White et al. 2012). Sprang and Silman reported that based on parental reports in the United States, the most common diagnoses among developmentally normal youth who received mental health services during or after the H1N1 pandemic were generalized anxiety disorder (20%) and adjustment disorder (20%) (Sprang and Silman 2013). Similarly, many other studies (Amorim et al. 2020, Nonweiler et al. 2020) found an increase in anxiety and emotional instability since the beginning of the COVID-19 pandemic. According to their parents, anxiety and irritability were important causes for the shift in the behavior of children during the pandemic, according to their parents (Amorim et al. 2020).
On the other hand, the clinical stability reported by Siracusano et al. (Siracusano et al. 2021) may be explained by a baseline difference in the study populations, such as mean age, amount of available support, geographical location, pandemic burden, and the extent of COVID-19 associated restrictions in the region. Another reason for the non-concordant results might be using non-standardized data collection techniques by some other studies, such as Colizzi et al. (Colizzi et al. 2020).
Individuals with autism are more likely to experience problems regulating their emotions than people with typical development (Cai et al. 2018). This problem further worsened during the COVID-19 pandemic, where multiple studies reported that a negative impact on emotion management was observed in children with ASD during the pandemic compared to their baseline status before the pandemic began (Amorim et al. 2020, Nonweiler et al. 2020). This increase in emotional problems, such as heightened levels of irritability, verbal outbursts, oppositional behavior, and more frequent episodes of crying, can be attributed to the pandemic's uncertainty, as well as COVID-19 related restrictions that have limited access to important school-based support programs, including speech therapy, occupational therapy, and social skills groups (Kalvin et al. 2021).
Unlike most of the studies in our review, Mumbardó-Adam et al. (2021) noticed that a substantial percentage of autistic children in their sample population appeared happier and calmer. This clinical stability during pandemic may be explained by removing well-known stressors like school and social interactions due to quarantine restrictions. This is supported by Clark et al. who previously identified "overstimulation, unpredictability, and demands (at school/in the community)" as major barriers to anxiety management in autistic children (Clark and Adams 2020).
Though all groups of people seem to be struggling as a result of the pandemic, children with Special Educational Needs and Disabilities (SEND) and their parents appear to be the most affected in terms of loss of routine, support network, anxiety of unpredictability and mood and behavior changes (Asbury et al. 2021). To help parents handle these challenges, professional advice should focus on how they can meet their child's educational and mental health needs. Additional resources should be provided for home learning, and opportunities should be created for the children to see familiar faces such as their teachers and other people from their support network (Asbury et al. 2021).
Some recommendations in literature were made, and we concur that simple steps should be taken to better care for ASD children during this pandemic:
It is critical to share pandemic information with these children in a safe environment, focusing on their questions and concerns. Parents can use social stories or other visuals to help their children understand the basic preventive techniques during the pandemic, such as washing hands and wearing masks (KidsHealth 2021, Lim et al. 2020).
It is critical to establish a healthy routine for these children at home, including timely study, meals, and play. Parents can create visual schedules or to-do lists for their children and set timers to help them with transitions and build clear expectations in their routines (KidsHealth 2021).
Children must maintain social connections with trusted friends and family members via video calls (Lim et al. 2020).
Parents must also take care of themselves and not be afraid to seek help when dealing with their ASD children. It is essential to talk to the child’s healthcare provider, teacher or behavior specialist for further guidance (KidsHealth 2021, Lim et al. 2020).
Such measures should be implemented on a larger scale immediately, and their efficacy should be investigated both during the pandemic and in the future. Overall, this will facilitate finding effective approaches to solve the needs and challenges faced by autistic children and their families.
Conclusion
It is difficult to assess the full ramifications of the ongoing psychological impact of the COVID-19 pandemic on children with ASD and to make definitive conclusions. The preliminary findings from the cross-sectional studies in this review suggest an overall worsening in various domains of ASD symptoms (irritability, anxiety, and emotional dysregulation). Home-based supportive interventions, such as maintaining routines and active participation from parents and schools, have yielded better results in alleviating stress, anxiety, and behavioral problems in autistic patients.
Authors' contributions
Saeed Ahmed, MD, Ikram Khaliq, MBBS, Shahana Ayub, MD, Aunsa Hanif, MBBS, Sundas Saboor, MD, Sheikh Shoib, MD, Muhammad Youshay Jawad, MBBS, Fauzia Arain, MD, Amna Anwar, MBBS, Irfan Ullah, MBBS, Sadiq Naveed, MDhave contributed in the conception, study design, execution, and interpretation of the article. All authors have drafted, substantially revised and critically reviewed the article. All authors have agreed that the article shall be submitted to the International Journal of Developmental Disabilities.
All authors have reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. All authors have agreed to take responsibility, be accountable for the contents of the article and share responsibility to resolve any questions raised about the accuracy or integrity of the published work.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding details
This research received no external funding or grants.
References
- Altena, E., Baglioni, C., Espie, C. A., Ellis, J., Gavriloff, D., Holzinger, B., Schlarb, A., Frase, L., Jernelöv, S. and Riemann, D. 2020. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. Journal of sleep research, 29, e13052. [DOI] [PubMed] [Google Scholar]
- Amorim, R. Catarino, Miragaia S., Ferreras P., Viana C., V. and Guardiano, M.. 2020. The impact of COVID-19 on children with autism spectrum disorder. Rev Neurol, 71, 285–291. [DOI] [PubMed] [Google Scholar]
- APA, 2013. Diagnostic and statistical manual of mental disorders (DSM-5®). Arlington, VA: American Psychiatric Publication. [Google Scholar]
- Asbury, K., Fox, L., Deniz, E., Code, A. and Toseeb, U.. 2021. How is COVID-19 affecting the mental health of children with special educational needs and disabilities and their families? Journal of Autism and Developmental Disorders, 51, 1772–1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baio, J., Wiggins, L., Christensen, D. L., Maenner, M. J., Daniels, J., Warren, Z., Kurzius-Spencer, M., Zahorodny, W., Robinson Rosenberg, C., White, T., Durkin, M. S., Imm, P., Nikolaou, L., Yeargin-Allsopp, M., Lee, L. C., Harrington, R., Lopez, M., Fitzgerald, R. T., Hewitt, A., Pettygrove, S.Constantino, J. N., Vehorn, A., Shenouda, J., Hall-Lande, J., VAN Naarden Braun, K. and Dowling, N. F.. 2018. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveillance Summaries, 67, 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker, S. P. and Gregory, A. M. 2020. Editorial Perspective: Perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. Journal of Child Psychology and Psychiatry, 61, 757–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellomo, T. R., Prasad, S., Munzer, T. and Laventhal, N.. 2020. The impact of the COVID-19 pandemic on children with autism spectrum disorders. Journal of Pediatric Rehabilitation Medicine, 13, 349–354. [DOI] [PubMed] [Google Scholar]
- Cai, R. Y., Richdale, A. L., Uljarević, M., Dissanayake, C. and Samson, A. C.. 2018. Emotion regulation in autism spectrum disorder: Where we are and where we need to go. Autism Research : official Journal of the International Society for Autism Research, 11, 962–978. [DOI] [PubMed] [Google Scholar]
- CDC, 2020. Centers for Disease Control and Prevention (CDC). Signs and Symptoms of Autism Spectrum Disorders [Online]. Available at://www.cdc.gov/ncbddd/autism/signs.html [Accessed 16 February 2021].
- Chaidi, I. and Drigas, A.. 2020. Autism, expression, and understanding of emotions: literature review. International Journal of Online and Biomedical Engineering, 16, 95. [Google Scholar]
- Clark, M. and Adams, D.. 2020. Parent perspectives of what helps and hinders their child on the autism spectrum to manage their anxiety. Clinical Psychologist, 24, 315–328. [Google Scholar]
- Colizzi, M., Sironi, E., Antonini, F., Ciceri, M. L., Bovo, C. and Zoccante, L.. 2020. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: An online parent survey. Brain Sciences, 10, 341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta, D. and Vanelli, M.. 2020. WHO declares COVID-19 a pandemic. Acta Bio Medica: Atenei Parmensis, 91, 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Renzo, M., Di Castelbianco, F. B., Vanadia, E., Petrillo, M., D’Errico, S., Racinaro, L. and Rea, M.. 2020. Parent-reported behavioural changes in children with autism spectrum disorder during the COVID-19 lockdown in Italy. Continuity in Education, 1, 117–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ersoy, K., Altin, B., Sarikaya, B. B. and Özkardaş, O. G.. 2020. The comparison of impact of health anxiety on dispositional hope and psychological well-being of mothers who have children diagnosed with autism and mothers who have normal children, in Covid-19 pandemic. Sosyal Bilimler Araştırma Dergisi, 9, 117–126. [Google Scholar]
- Francisco, R., Pedro, M., Delvecchio, E., Espada, J. P., Morales, A., Mazzeschi, C. and Orgilés, M.. 2020. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Frontiers in Psychiatry, 11, 570164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein, E., , Wen, H. and , Miller, B. F. 2020. Coronavirus Disease 2019 (COVID-19) and Mental Health for Children and Adolescents. JAMA Pediatrics, 174, 819 doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Hallett, V., Lecavalier, L., Sukhodolsky, D. G., Cipriano, N., Aman, M. G., McCracken, J. T., McDougle, C. J., Tierney, E., King, B. H., Hollander, E., Sikich, L., Bregman, J., Anagnostou, E., Donnelly, C., Katsovich, L., Dukes, K., Vitiello, B., Gadow, K. and Scahill, L.. 2013. Exploring the manifestations of anxiety in children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43, 2341–2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang, T.-J., Rabheru, K., Peisah, C., Reichman, W. and Ikeda, M.. 2020. Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics, 32, 1217–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacques, C., Courchesne, V., Meilleur, A.-A S., Mineau, S., Ferguson, S., Cousineau, D., Labbe, A., Dawson, M. and Mottron, L.. 2018. What interests young autistic children? An exploratory study of object exploration and repetitive behavior. PloS One, 13, e0209251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalvin, C. B., Jordan, R. P., Rowley, S. N., Weis, A., Wood, K. S., Wood, J. J., Ibrahim, K. and Sukhodolsky, D. G.. 2021. Conducting CBT for Anxiety in Children with Autism Spectrum Disorder During COVID-19 Pandemic. Journal of Autism and Developmental Disorders, 51, 4239–4247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KIDSHEALTH . 2021. Coronavirus (COVID-19): Helping Kids With Autism Cope [Online]. Available at://kidshealth.org/en/parents/coronavirus-autism.html [Accessed 21 May 2021].
- Lazenby, D. C., Sideridis, G. D., Huntington, N., Prante, M., Dale, P. S., Curtin, S., Henkel, L., Iverson, J. M., Carver, L., Dobkins, K., Akshoomoff, N., Tagavi, D., Nelson, C. A., 3RD. and Tager-Flusberg, H.. 2016. Language differences at 12 months in infants who develop autism spectrum disorder. Journal of Autism and Developmental Disorders, 46, 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim, T., Tan, M. Y., Aishworiya, R. and Kang, Y. Q.. 2020. Autism spectrum disorder and COVID-19: Helping caregivers navigate the pandemic. Annals of the Academy of Medicine, Singapore, 49, 384–386. [PubMed] [Google Scholar]
- Miller, M., Iosif, A.-M., Hill, M., Young, G. S., Schwichtenberg, A. and Ozonoff, S.. 2017. Response to name in infants developing autism spectrum disorder: A prospective study. The Journal of Pediatrics, 183, 141–146. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriuchi, J. M., Klin, A. and Jones, W.. 2017. Mechanisms of diminished attention to eyes in autism. American Journal of Psychiatry, 174, 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumbardó-Adam, C., Barnet-López, S. and Balboni, G.. 2021. How have youth with Autism Spectrum Disorder managed quarantine derived from COVID-19 pandemic? An approach to families perspectives. Research in Developmental Disabilities, 110, 103860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutluer, T., Doenyas, C. and Genc, H. A.. 2020. Behavioral Implications of the Covid-19 process for autism spectrum disorder, and individuals' comprehension of and reactions to the pandemic conditions. Frontiers in Psychiatry, 11, 561882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonweiler, J., Rattray, F., Baulcomb, J., Happé, F. and Absoud, M.. 2020. Prevalence and associated factors of emotional and behavioural difficulties during COVID-19 pandemic in children with neurodevelopmental disorders. Children, 7, 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özdin, S. and Bayrak Özdin, Ş.. 2020. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. International Journal of Social Psychiatry, 66, 504–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugliese, C. E., White, B. A., White, S. W. and Ollendick, T. H.. 2013. Social anxiety predicts aggression in children with ASD: Clinical comparisons with socially anxious and oppositional youth. Journal of Autism and Developmental Disorders, 43, 1205–1213. [DOI] [PubMed] [Google Scholar]
- Singh, S., Roy, M. D., Sinha, C. P. T. M. K., Parveen, C. P. T. M. S., Sharma, C. P. T. G. and Joshi, C. P. T. G.. 2020. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Research, 293, 113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siracusano, M., Segatori, E., Riccioni, A., Emberti Gialloreti, L., Curatolo, P. and Mazzone, L.. 2021. The impact of COVID-19 on the adaptive functioning, behavioral problems, and repetitive behaviors of Italian children with autism spectrum disorder: an observational study. Children, 8, 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang, G. and Silman, M.. 2013. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness, 7, 105–110. [DOI] [PubMed] [Google Scholar]
- Tager-Flusberg, H. 1999. A psychological approach to understanding the social and language impairments in autism. International Review of Psychiatry (Abingdon, England), 11, 325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theoharides, T. C. and Kavalioti, M.. 2019. Effect of stress on learning and motivation-relevance to autism spectrum disorder. International Journal of Immunopathology and Pharmacology, 33, 2058738419856760. [DOI] [PMC free article] [PubMed]
- Tucci, V., Moukaddam, N., Meadows, J., Shah, S., Galwankar, S. C. and Kapur, G. B.. 2017. The forgotten plague: Psychiatric manifestations of Ebola, Zika, and emerging infectious diseases. Journal of Global Infectious Diseases, 9, 151–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Türkoğlu, S., Uçar, H. N., Çetin, F. H., Güler, H. A. and Tezcan, M. E.. 2020. The relationship between chronotype, sleep, and autism symptom severity in children with ASD in COVID-19 home confinement period. Chronobiology International, 37, 1207–1213. [DOI] [PubMed] [Google Scholar]
- Turner-Brown, L. and Frisch, M. 2020. Understanding and Addressing Restricted and Repetitive Behaviors in Children with Autism. In: Vivanti, G., Bottema-Beutel, K. & Turner-Brown, L. (eds.) Clinical Guide to Early Interventions for Children with Autism. Cham: Springer International Publishing. p. 61–77. [Google Scholar]
- Wang, Y., Zhang, Y.-B., Liu, L.-L., Cui, J.-F., Wang, J., Shum, D. H., VAN Amelsvoort, T. and Chan, R. C.. 2017. A meta-analysis of working memory impairments in autism spectrum disorders. Neuropsychology Review, 27, 46–61. [DOI] [PubMed] [Google Scholar]
- White, S. W., Bray, B. C. and Ollendick, T. H.. 2012. Examining shared and unique aspects of social anxiety disorder and autism spectrum disorder using factor analysis. Journal of Autism and Developmental Disorders, 42, 874–884. [DOI] [PubMed] [Google Scholar]
- WHO, 2020a. Coronavirus disease (COVID-19): Herd immunity, lockdowns and COVID-19 [Online]. Available at://www.who.int/news-room/q-a-detail/herd-immunity-lockdowns-and-covid-19 [Accessed 13 April 2021].
- WHO , 2020b. WHO Director-General's opening remarks at the media briefing on COVID-19 [Online]. Available at://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–-11-march-2020 [Accessed 05 April 2021].