Abstract
目的
下咽颈段食管癌因其解剖位置较为隐秘,大多数患者就诊时即为晚期。目前,治疗该疾病多采用外科手术切除加放射治疗(以下简称放疗)为主的综合治疗方案,但由于手术切除范围较为广泛,常会导致患者下咽及颈段食管切除后大范围的环形缺损,因此肿瘤切除后的上消化道重建至关重要。本研究分别采用游离股前外侧皮瓣(free anterolateral thigh flap,ALT)和游离空肠(free jejunum,FJ)重建下咽颈段食管,探讨2种方法重建下咽颈段食管癌术后上消化道缺损的疗效及优缺点。
方法
回顾性分析2004年1月至2016年1月中南大学湘雅二医院耳鼻咽喉头颈外科42例临床IV期下咽颈段食管癌患者的临床资料。所有患者行全喉全下咽及颈段食管的切除,肿瘤切除术后所致的环周缺损分别以ALT(22例)及FJ(20例)进行一期修复。4例术前已接受放疗和化学药物治疗(以下简称化疗)的ALT组患者术后未再行放疗和化疗,其余38例患者均在术后4~8周开始行辅助放、化疗。对所有患者采取电话或门诊复查的方式进行随访,随访截止时间为2021年1月。比较2组患者术后及放疗后并发症的发生率与术后的生存率之间的差异。采用Fisher检验分析组间个体特征的差异,采用χ²检验分析组间各种并发症发生的差异,采用Kaplan-Meier生存曲线方法计算3年及5年总生存率。
结果
ALT组术后的并发症主要为吻合口瘘、乳糜漏及供区皮下血肿,放疗后的并发症主要是吻合口狭窄;而FJ组术后的并发症主要为乳糜漏、肠梗阻及肠瘘,放疗后的并发症主要为吻合口瘘及组织瓣坏死。ALT组和FJ组术后分别发生7例和5例并发症(P=0.625);放疗后分别有3例和4例发生并发症(P=0.563)。ALT组和FJ组的3年总生存率分别为52.9%和46.7%,5年总生存率分别为35.1%和31.9%,2组生存率之间的差异无统计学意义(P=0.53)。ALT组放疗后发生吻合口狭窄的病例稍多于FJ组(P=0.097);FJ组放疗后发生空肠坏死及吻合口瘘的例数稍多于ALT组(P=0.066)。
结论
采用ALT和FJ重建下咽颈段食道在术后及放疗后并发症发生情况、3年及5年生存率方面无明显差别。但ALT重建可能更易发生吻合口狭窄,而FJ重建可能不能耐受较大剂量的放疗。ALT和FJ均为下咽颈段食管重建的有效方法,临床上应根据其相应的优缺点慎重选择重建方式。
Keywords: 下咽肿瘤, 食管肿瘤, 修复方法, 游离股前外侧皮瓣, 游离空肠
Abstract
Objective
Because of its peculiar anatomical location, most patients with hypopharyngeal and cervical esophageal cancer are at advanced stage when they visit the hospital. At present, the treatment for hypopharyngeal and cervical esophageal cancer is primarily surgical resection and radiotherapy. However, due to the wide range of surgical resection, it can often lead to a large range of annular defects. Therefore, the upper digestive tract reconstruction after tumor resection is very important. We use the free anterolateral thigh flap (ALT) and free jejunum (FJ) transfer to reconstruct the hypopharyngeal and cervical esophagus, and to investigate the effect of both reconstruction methods on upper gastrointestinal tract defects.
Methods
A retrospective analysis was conducted to investigate the clinical data of 42 patients with hypopharyngeal and cervical esophageal cancer (Clinical Stage IV) from Jan. 2004 to Jan. 2016 in the Second Xiangya Hospital of Central South University. All patients underwent total laryngopharyngectomy and cervical esophageal resection. The hypopharyngeal circumferential and cervical esophageal defects were reconstructed with free ALT (n=22) or FJ (n=20). Four patients who underwent radiotherapy and chemotherapy before surgery did not receive radiotherapy or chemotherapy after surgery. The remaining 38 patients underwent postoperative radiotherapy and chemotherapy. All patients were followed up by telephone or outpatient review, with a follow-up deadline in Jan. 2021. We compared the differences between the 2 groups in postoperative complications, radiotherapy complications, and survival rate. The differences in individual characteristics between 2 groups were analyzed using Fisher test. The differences in postoperative and radiotherapy complications between two groups were analyzed using χ² test. The 3- and 5-year overall survival rates were calculated using Kaplan-Meier survival curve method.
Results
In the ALT group, the postoperative complications mainly included anastomotic fistula, chylous fistula and subcutaneous hematoma of the donor site. The radiotherapy complication was anastomotic stenosis. However, in the FJ group, the postoperative complications mainly included chylous fistula, intestinal obstruction, and intestinal fistula. The radiotherapy complications mainly contained anastomotic fistula and tissue flap necrosis. The cases of postoperative complications in the ALT group and the FJ group were 7 and 5, respectively (P=0.625), and the cases of radiotherapy complications were 3 and 4, respectively (P=0.563). The 3-year overall survival rates in the ALT group and the FJ group were 52.9% and 46.7%, respectively, and the 5-year total survival rates were 35.1% and 31.9%, respectively (P=0.53). The cases of anastomotic stenosis after radiotherapy in the ALT group were more than those in the FJ group (P=0.097). However, the cases of jejunal necrosis and anastomotic fistula after radiotherapy in the FJ group were more than those in the ALT group (P=0.066).
Conclusion
There are no significant differences in postoperative and radiotherapy complications and 3-and 5-year survival rates between the ALT group and the FJ group. The reconstruction with ALT is prone to develop anastomotic stricture. The reconstruction with FJ cannot withstand high-dose radiotherapy. The ALT and FJ are effective methods in the reconstruction of hypopharynx and cervical esophagus. The treatment protocol should be carefully chosen based on its advantages and disadvantages of these 2 methods.
Keywords: hypopharyngeal carcinoma, esophageal carcinoma, reconstructive methods, free anterolateral thigh flap, free jejunum
下咽颈段食管癌因其解剖位置较为隐秘,早期临床症状不明显,以致于大多数患者就诊时即为晚期[1]。下咽颈段食管癌具有较强的侵袭性,易发生局部侵犯、淋巴结转移和远处转移等,病情进展较为迅速。尽管现代医学技术水平已显著提高,但是下咽颈段食管癌的处理在临床中仍较为棘手。目前,治疗该疾病多采用外科手术切除加放射治疗(以下简称放疗)为主的综合治疗方案,但由于手术切除范围较为广泛,常会导致患者下咽及颈段食管切除后大范围的环形缺损,因此肿瘤切除后的上消化道重建至关重要[2]。本研究回顾性分析中南大学湘雅二医院(以下简称我院)采取游离股前外侧皮瓣(free anterolateral thigh flap,ALT)及游离空肠(free jejunum,FJ)重建下咽颈段食管42例患者的临床资料,旨在探讨ALT及FJ重建下咽颈段食管癌术后上消化道缺损的疗效及优缺点。
1. 资料与方法
1.1. 一般临床资料
2004年1月至2016年1月我院共收治下咽颈段食管癌患者42例。患者均经组织病理学诊断为鳞状细胞癌,且在我院完成综合治疗的全过程。排除标准:1)治疗前接受过下咽癌手术治疗者;2)既往或治疗时患有其他肿瘤者。42例患者均为男性,年龄为48~72(平均59.1)岁。根据重建方法,将患者分为ALT组和FJ组。根据美国癌症联合委员会(American Joint Committee on Cancer,AJCC)下咽癌TNM分期标准(第八版),在42例下咽颈段食管癌患者中,T4N0M0 6例,T4N1M0 9例,T4N2M0 18例,T4N3M0 9例,均为临床IV期。2组间TNM分期及临床分期的差异均无统计学意义(均P>0.05,表1)。患者术前均行电子鼻咽喉镜、胃镜、CT和/或MRI、B超或PET-CT等检查以明确病变部位及范围。
表1.
游离股前外侧皮瓣组与游离空肠组的TNM分期及临床分期情况
Table 1 TNM staging and clinical stage of free anterolateral thigh flap group and free jejunum group
| 分期 | 游离皮瓣组(n=22) | 游离空肠组(n=20) |
|---|---|---|
| T分期 | ||
| T4 | 22 | 20 |
| N分期 | ||
| N0 | 3 | 3 |
| N1 | 5 | 4 |
| N2 | 10 | 8 |
| N3 | 4 | 5 |
| 临床分期 | ||
| IV期 | 22 | 20 |
1.2. 方法
1.2.1. 原发肿瘤及颈部淋巴结的处理
42例患者的肿瘤原发病灶均侵犯喉部,患者均行全喉、全下咽及颈段食管切除。4例患者因术前已行放疗、化学药物治疗(以下简称化疗),颈部无肿大淋巴结,故未行颈部淋巴结清扫术,其余38例患者均行双侧颈部淋巴结清扫术。
1.2.2. ALT移植
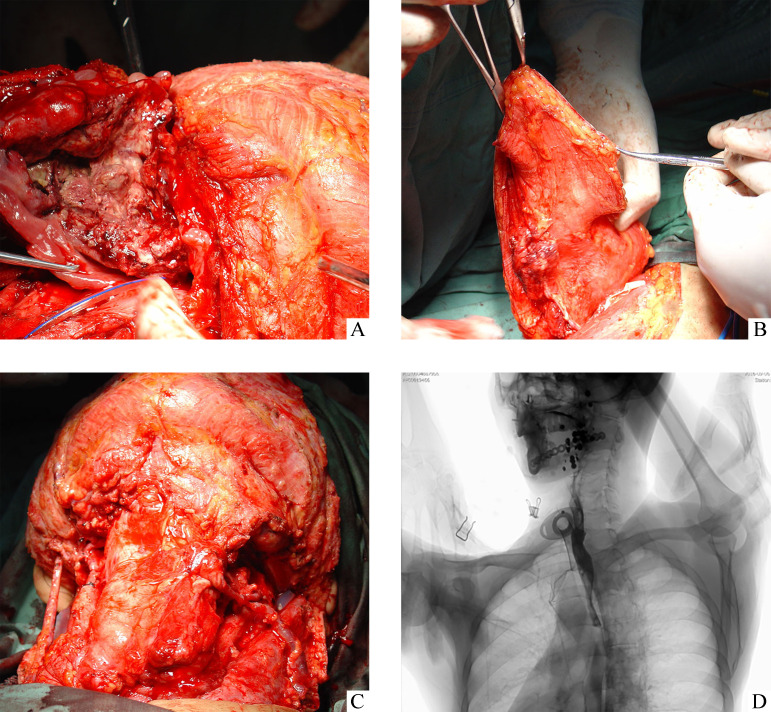
ALT组采用ALT重建上消化道,制备皮瓣后,为防止术后吻合口狭窄,将食管断端与游离皮瓣端修剪成斜面进行相互吻合(图1)。
图1.
游离股前外侧皮瓣修复下咽颈段食管缺损
Figure 1 Reconstruction with free anterolateral thigh flaps for hypopharyngeal circumferential and cervical esophageal defects
A: Exposure and dissection of tumor; B: Preparation of free anterolateral thigh flaps; C: Reconstruction with free anterolateral thigh flaps; D: Unobstructed upper gastrointestinal tract showed by postoperative barium meal.
1.2.3. FJ移植
FJ组采用FJ重建上消化道,选择并切取Treitz韧带下方血管弓发育良好且长度适宜的一段空肠,并将腹腔的空肠端端吻合。再在显微镜下将FJ的1支动脉、2支静脉分别与颈部的动静脉血管进行吻合。血管吻合完成后,调整肠系膜并修剪两端肠管,将游离的空肠肠管与口咽端及食管残端分2层进行端端吻合(图2)。
图2.
游离空肠修复下咽颈段食管缺损
Figure 2 Reconstruction with free jejunum for hypopharyngeal circumferential and cervical esophageal defects
A: Exposure and dissection of tumor; B: Preparation of free jejunum; C: Reconstruction with free jejunum; D: Unobstructed upper gastrointestinal tract showed by postoperative barium meal.
1.2.4. 血管的选择及血管吻合方法
ALT的血供选择旋股外侧动脉降支,FJ的血管选用空肠动脉,颈部的动脉血管选择甲状腺上动脉、颈横动脉或面动脉,静脉血管选择颈外静脉、甲状腺上静脉或面静脉。ALT组4例术前已接受放、化疗的患者均采取颈横动脉进行吻合。
1.2.5. 术后辅助治疗
除术前已行放疗和化疗的4例患者,其余38例患者均接受了术后辅助放疗和化疗。ALT组的放疗剂量为50~60 Gy,FJ组的放疗剂量为50~55 Gy。化疗药物为顺铂、紫杉醇和5-氟尿嘧啶。
1.3. 随访
对所有患者采取电话或门诊复查的方式进行随访,随访截止时间为2021年1月。记录患者的术后恢复、并发症以及生存情况。
1.4. 统计学处理
采用SPSS 21.0统计软件进行数据分析。采用Fisher检验分析组间个体特征的差异,采用χ²检验分析组间各种并发症发生情况的差异,采用Kaplan-Meier生存曲线方法计算3年及5年总生存率。以P<0.05为差异具有统计学意义。
2. 结 果
2.1. 手术后并发症
ALT组共22例,其中4例患者术后发生吻合口瘘;2例患者皮瓣供区术后发生皮下血肿;1例患者术后发生乳糜漏。FJ组共20例,其中2例患者术后发生乳糜漏;2例患者腹部术后发生肠梗阻;1例患者术后发生肠瘘(表2)。
表2.
游离股前外侧皮瓣组与游离空肠组修复术后并发症 发生情况的比较
Table 2 Comparison of postoperative complications for the free anterolateral thigh flap group and the free jejunum group
| 并发症 | 游离皮瓣组(n=22) | 游离空肠组(n=20) |
|---|---|---|
| 合计 | 7 | 5 |
| 受区 | ||
| 吻合口瘘 | 4 | 0 |
| 组织瓣坏死 | 0 | 0 |
| 乳糜漏 | 1 | 2 |
| 供区 | ||
| 肠梗阻 | 0 | 2 |
| 肠瘘 | 0 | 1 |
| 皮下血肿 | 2 | 0 |
术后发生吻合口瘘的4例患者均在手术前接受了放、化疗,经换药3周,待感染期过后用生物胶置入瘘道加压后吻合口瘘闭合;2例皮瓣供区发生皮下血肿的患者经再次手术清除血肿后供区伤口愈合良好;术后出现乳糜漏的3例患者,经强负压吸引、禁食及静脉营养约7 d后均治愈;术后发生肠梗阻的2例患者经胃肠减压等保守治疗后好转;1例术后发生肠瘘的患者经腹部充分引流2周后瘘口愈合。2组术后总并发症的发生例数差异无统计学意义(P=0.625)。
2.2. 术后恢复情况
42例患者中,除4例发生吻合口瘘的患者恢复时间较长外,其余38例患者均在术后2~3周开始进食并逐渐恢复正常饮食。
2.3. 放疗后并发症
4例术前已行放疗的患者术后未再行放疗,其余38例(ALT组18例,FJ组20例)患者均在术后4~8周接受放疗。ALT组放疗后,15例患者恢复良好,3例患者放疗结束后逐渐出现吻合口狭窄致使进食困难,经多次球囊扩张后逐渐恢复进食。FJ组放疗后,16例患者恢复良好;2例患者在放疗将要结束时出现吻合口瘘,经反复多次换药后瘘口愈合;2例患者放疗后出现空肠坏死,其中1例患者再次行皮瓣修复后伤口逐渐愈合,另1例患者经过换药5周后放弃进一步治疗,经颈部插管进食。2组放疗后总并发症的发生例数差异无统计学意义(P=0.563)。ALT组放疗后发生吻合口狭窄的病例稍多于FJ组(P=0.097);FJ组放疗后发生空肠坏死及吻合口瘘的例数稍多于ALT组(P=0.066)。
2.4. 生存率及死亡原因
本研究共失访3例,随访时间7~102(中位数42)个月。ALT组和FJ组的3年生存率分别为52.9%和46.7%,5年生存率分别为35.1%和31.9%。截至2021年1月已死亡28例,死亡原因包括:远处转移12例,原发灶复发6例,其他部位的原发癌4例,非原发疾病3例,原因不明3例。ALT组3年及5年的生存率均比FJ组高,但差异无统计学意义(P=0.53,图3)。
图3.
游离股前外侧皮瓣组和游离空肠组患者修复术后Kaplan-Meier生存曲线
Figure 3 Kaplan-Meier survival curve for the patients with reconstruction with free anterolateral thigh flaps and free jejunum for hypopharyngeal circumferential and cervical esophageal defects
3. 讨 论
在下咽颈段食管癌的手术治疗中,切除下咽、全喉及颈段食管后常会导致患者下咽及颈段食管大范围的缺损,因此重建上消化道以恢复患者的吞咽功能是治疗此疾病需主要考虑的问题。下咽颈段食管癌患者的修复方式应根据患者的意愿、健康状况、肿瘤侵犯部位及范围、术者经验等选择合适的重建方式。目前,皮瓣修复及脏器替代修复仍是上消化道重建常见的修复方式[3-8]。而我院采取ALT及FJ重建下咽颈段食管缺损均获得了较高的成功率。
ALT属于穿支皮瓣,位于大腿的前外侧,旋股外侧动脉及其肌皮动脉穿支是其主要的供血动脉。采取ALT可以取到的皮瓣面积较大,同时可以取到较多的肌肉组织,对于减少修复术后的死腔也很有帮助[9]。由于皮瓣组织中皮肤及筋膜组织的代谢率低,细胞分裂慢,对放射线的损伤耐受力强,放疗后不易产生皮瓣坏死等并发症,因此皮瓣修复尤其适用于术后需接受较大剂量放疗的患者[10]。本研究所有ALT修复并接受术后放疗的患者中均未发生因放疗导致皮瓣坏死的情况,因此我们认为ALT修复上消化道可以接受术后常规辅助放疗的剂量。但ALT修复上消化道缺损也有一定的缺点,如术后易产生吻合口瘘,尤其是放疗后易发生吻合口狭窄等并发症[11-12]。这主要是由于皮瓣无类似食管平滑肌样的收缩功能,没有弹性,因此放疗后皮瓣组织易发生纤维化从而导致狭窄。本研究采用ALT修复的患者中有4例术后发生吻合口瘘,3例放疗后发生吻合口狭窄。发生吻合口瘘的患者均在术前接受了放疗,发生吻合口瘘的主要原因可能是术前放疗引起局部血管炎症,从而导致吻合口处愈合能力降低。而在减少吻合口狭窄的发生率方面,我们认为将皮瓣与食管断端修剪成斜面进行端端吻合,可以减少吻合口的张力。
FJ移植术早在上世纪50年代便开始应用,随着显微外科技术的发展,FJ成功率显著提高,可达94%~97%[13-14]。空肠平滑肌和食管平滑肌具有相似的组织结构,口径也非常接近,因此用空肠进行修复后患者的吞咽会更为顺畅,且无食管反流情况发生[15-16],术后相对不易发生吻合口狭窄和吻合口瘘。本研究采用FJ修复的患者均未发生术后吻合口狭窄和吻合口瘘的情况。但其中1例患者空肠吻合后出现肠管水肿,颈部伤口无法关闭,我们用无菌塑料薄膜覆盖伤口,经抗凝及扩血管治疗后,肠管水肿逐渐减轻,术后第5天再次行胸三角皮瓣修复颈部皮肤缺损,术后吻合口愈合良好。究其原因我们认为可能是血管吻合后静脉血栓形成所致。FJ移植术也有其缺点,如术后难以耐受剂量较大的放疗,一旦放疗剂量过大,则可能导致血管闭塞、空肠坏死,因此在一定程度上影响治疗效果。本研究采用FJ修复的患者中有2例放疗后发生空肠坏死,2例发生吻合口瘘,我们认为主要由于空肠肠壁黏膜腺上皮代谢率高,细胞分裂快,易受放射线损伤,难以耐受较大剂量的放疗所致。
下咽及颈段食管癌患者往往就诊时局部分期较晚,无论采取何种方式治疗该疾病,此类患者的5年生存率仍不到31%[17]。本研究中42例患者均为临床Ⅳ期,ALT组及FJ组5年生存率分别为35.1%和31.9%;2组间的术后及放疗后并发症发生例数、3年及5年生存率的比较均无明显差别。但ALT组放疗后发生吻合口狭窄的病例稍多于FJ组;FJ组放疗后发生空肠坏死及吻合口瘘的例数稍多于ALT组。因此,我们认为ALT重建可能更易发生吻合口狭窄,而FJ重建可能不能耐受较大剂量的放疗。下咽颈段食管癌患者临床中较为少见,所以本研究整体病例数较少,可能会影响最终的统计学结果。今后将积累更多相关病例,以得出更加明确的结论。
综上,本研究显示ALT及FJ均为下咽颈段食管重建的有效方法,临床上应根据其相应的优缺点慎重选择重建方式。
基金资助
国家自然科学基金(81502662);湖南省卫生健康委员会课题(202107010061);湘雅医学大数据项目(2014001)。
This work was supported by the National Natural Science Foundation (81502662), the Project of Hunan Health Committee (202107010061), and Xiangya Clinical Medicine Database (2014001), China.
利益冲突声明
所有作者均声明不存在利益冲突。
作者贡献
王爽 数据分析,论文设计、撰写与修改;杨新明、唐青来 论文设计、指导及修改;彭霞 论文指导及修改;郭璐、唐小珺 数据采集和分析。所有作者阅读并同意最终的文本。
原文网址
http://xbyxb.csu.edu.cn/xbwk/fileup/PDF/202207888.pdf
参考文献
- 1. Schizas, Theochari NA, Ziogas IA, et al. Carcinomas of the hypopharynx and cervical esophagus: a systematic review and quality of evidence assessment[J]. J BUON, 2021, 26(1): 39-50. [PubMed] [Google Scholar]
- 2. Khalid FA, Saleem M, Yousaf MA, et al. Oropharyngeal, hypopharyngeal and cervical esophageal reconstruction: an experience of pedicle flaps[J]. J Coll Physicians Surg Pak, 2019, 29(2): 168-172. 10.29271/jcpsp.2019.02.168. [DOI] [PubMed] [Google Scholar]
- 3. Jiang M, He XT, Wu DG, et al. Reconstruction techniques for hypopharyngeal and cervical esophageal carcinoma[J]. J Thorac Dis, 2015, 7(3): 449-454. 10.3978/j.issn.2072-1439.2015.02.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Elfeky AE, Nasr WF, Khazbak A, et al. Hypopharyngeal reconstruction: a comparison of three alternatives[J]. Eur Arch Otorhinolaryngol, 2015, 272(10): 3045-3050. 10.1007/s00405-014-3306-x. [DOI] [PubMed] [Google Scholar]
- 5. 徐伟, 吕正华, 邹纪东, 等. 下咽颈段食管癌行游离空肠移植重建103例临床分析[J]. 中华耳鼻咽喉头颈外科杂志, 2016, 51(12): 914-917. 10.3760/cma.j.issn.1673-0860.2016.12.007. [DOI] [PubMed] [Google Scholar]; XU Wei, Zhenghua LÜ, ZOU Jidong, et al. Reconstruction with free jejuna flap for the defect after removal of hypopharyngeal and cervical esophageal caneer: clinical analyses of 103 cases[J]. Chinese Journal of Otorhinolaryngology Head and Neck Surgery, 2016, 51(12): 914-917. 10.3760/cma.j.issn.1673-0860.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 6. 文译辉, 文卫平, 王章锋, 等. 锁骨上岛状皮瓣在下咽及食管上段恶性肿瘤手术修复中的应用[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(1): 16-20. 10.3760/cma.j.issn.1673-0860.2018.01.004. [DOI] [PubMed] [Google Scholar]; WEN Yihui, WEN Weiping, WANG Zhangfeng, et al. Clinical application of supraclavicular flap for oncologic reconstruction of hypopharynx and upper esophagus[J]. Chinese Journal of Otorhinolaryngology Head and Neck Surgery, 2018, 53(1): 16-20. 10.3760/cma.j.issn.1673-0860.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 7. 李树春, 李振东, 刘宏伟, 等. 应用胃上提和复合喉气管瓣重建下咽颈段食管癌切除后全周缺损163例临床分析[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(9): 661-667. 10.3760/cma.j.issn.1673-0860.2018.09.005. [DOI] [PubMed] [Google Scholar]; LI Shuchun, LI Zhendong, LIU Hongwei, et al. Application of gastric pull up and complex laryngotracheal flap to reconstruct the circumferencial defect after resection of the hypopharyngeal and cervical esophageal cancers[J]. Chinese Journal of Otorhinolaryngology Head and Neck Surgery, 2018, 53(9): 661-667. 10.3760/cma.j.issn.1673-0860.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 8. 温树信, 王斌全. 股前外侧皮瓣: 一种理想的下咽及颈段食管缺损修复组织[J]. 临床耳鼻咽喉头颈外科杂志, 2015, 29(17): 1508-1510. 10.13201/j.issn.1001-1781.2015.17.003. [DOI] [PubMed] [Google Scholar]; WEN Shuxin, WANG Binquan. Anterolateral thigh flap, a better flap for reconstruction of hypopharyngeal and cervical esophageal defects[J]. Journal of Clinical Otorhinolaryngology Head and Neck Surgery, 2015, 29(17): 1508-1510. 10.13201/j.issn.1001-1781.2015.17.003. [DOI] [PubMed] [Google Scholar]
- 9. Oh TS, Kwon JG, Jeong WS, et al. A flag-shaped anterolateral thigh free flap for complete circumferential hypopharyngeal reconstruction with dead space obliteration and monitoring flap inset[J]. J Plast Reconstr Aesthet Surg, 2019, 72(11): 1785-1794. 10.1016/j.bjps.2019.05.038. [DOI] [PubMed] [Google Scholar]
- 10. Chan JY, Chow VL, Chan RC, et al. Oncological outcome after free jejunal flap reconstruction for carcinoma of the hypopharynx[J]. Eur Arch Otorhinolaryngol, 2012, 269(7): 1827-1832. 10.1007/s00405-011-1836-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chang TY, Hsiao JR, Lee WT, et al. Esophageal reconstruction after oncological total laryngopharyngoesophagectomy: Algorithmic approach[J]. Microsurgery, 2019, 39(1): 6-13. 10.1002/micr.30304. [DOI] [PubMed] [Google Scholar]
- 12. Fujiwara T, Shih HS, Chen CC, et al. Interdigitation of the distal anastomosis between tubed fasciocutaneous flap and cervical esophagus for stricture prevention[J]. Laryngoscope, 2011, 121(2): 289-293. 10.1002/lary.21289. [DOI] [PubMed] [Google Scholar]
- 13. Gaur P, Blackmon SH. Jejunal graft conduits after esophagectomy[J]. J Thorac Dis, 2014, 6(Suppl 3): S333-S340. 10.3978/j.issn.2072-1439.2014.05.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reece GP, Schusterman MA, Miller MJ, et al. Morbidity and functional outcome of free jejunal transfer reconstruction for circumferential defects of the pharynx and cervical esophagus[J]. Plast Reconstr Surg, 1995, 96(6): 1307-1316. 10.1097/00006534-199511000-00012. [DOI] [PubMed] [Google Scholar]
- 15. 鄢丹桂, 张彬, 李德志, 等. 游离空肠移植重建下咽及颈段食管112例临床分析[J]. 中华耳鼻咽喉头颈外科杂志, 2011, 46(5): 373-377. 10.3760/cma.j.issn.1673-0860.2011.05.006. [DOI] [PubMed] [Google Scholar]; YAN Dangui, ZHANG Bin, LI Dezhi, et al. Reconstruction of hypopharyngeal circumferential and cervical esophageal defects with free jejunal interposition in 112 cases[J]. Chinese Journal of Otorhinolaryngology Head and Neck Surgery, 2011, 46(5): 373-377. 10.3760/cma.j.issn.1673-0860.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 16. 刘穹, 王嘉陵, 刘良发, 等. 自体游离空肠重建喉咽及颈段食管[J]. 中国耳鼻咽喉头颈外科, 2008, 15(11): 605-607. [Google Scholar]; LIU Qiong, WANG Jialing, LIU Liangfa, et al. Free jejunal graft for hypopharyngeal and cervical esophageal reconstruction[J]. Chinese Archives of Otolaryngology-Head and Neck Surgery, 2008, 15(11): 605-607. [Google Scholar]
- 17. Marion Y, Lebreton G, Brévart C, et al. Gastric pull-up reconstruction after treatment for advanced hypopharyngeal and cervical esophageal cancer[J]. Eur Ann Otorhinolaryngol Head Neck Dis, 2016, 133(6): 397-400. 10.1016/j.anorl.2016.08.002. [DOI] [PubMed] [Google Scholar]