Abstract
膀胱平滑肌肉瘤(leiomyosarcoma of urinary bladder,LMS-UB)是一种高度恶性间叶来源性肿瘤,占所有膀胱恶性肿瘤的比例不足0.5%,临床表现以血尿为主。现报告低级别LMS-UB1例,患者为44岁男性,因“尿痛2周”入院。患者盆腔CT提示膀胱右侧壁肿物,初步诊断为膀胱肿瘤,予机器人辅助腹腔镜下膀胱肿瘤剜除术。术后病理检查提示低级别LMS-UB,予5个周期辅助化学治疗。随访19个月,患者无不适症状,无复发及远处转移。此前国内外暂无微创行剜除术治疗LMS-UB的相关报道,本病例为早期低级别LMS-UB提供了一种新的外科手术联合辅助化学治疗的综合治疗方案,有望减少并发症及提高患者术后生活质量。
Keywords: 膀胱肿瘤, 平滑肌肉瘤, 机器人手术, 化学治疗
Abstract
Leiomyosarcoma of urinary bladder (LMS-UB) is a highly malignant mesenchymal tumor, accounting for less than 0.5% of all bladder malignancies, with a predominant clinical presentation of hematuria. Here we report a case of low-grade LMS-UB. A 44-year-old male patient was admitted to the hospital with urodynia for 2 weeks. The patient’s pelvis CT showed a mass on the right part of the bladder. For this reason, he was initially diagnosed with bladder cancer. We performed a robot-assisted laparoscopic enucleation of the bladder tumor and low-grade LMS-UB was diagnosed with the histopathological examination. He underwent 5 cycles of adjuvant chemotherapy after surgery. At 19months postoperative follow-up, the patient had no symptoms, recurrence, or distant metastasis. There is no report on the treatment of LMS-UB with minimally invasive enucleation worldwide. This case provides a new comprehensive treatment method of enucleation combined with adjuvant chemotherapy for early low-grade LMS-UB to reduce complications and improve patients’ quality of life after surgery.
Keywords: bladder cancer, leiomyosarcoma, robotic-assisted surgery, chemotherapy
膀胱恶性肿瘤是泌尿系统常见恶性肿瘤之一,通常为尿路上皮癌,非尿路上皮肿瘤占膀胱恶性肿瘤的比例不足5%,其中膀胱平滑肌肉瘤(leiomyosarcoma of urinary bladder,LMS-UB)约占非尿路上皮肿瘤的0.1%[1-2]。目前国内外相关文献报道LMS-UB不足220例。大多数LMS-UB发现时已处于晚期,且LMS-UB肿瘤细胞多呈高级别改变,总体预后较差[2]。LMS-UB在治疗上现虽无标准治疗方案,但目前大多数学者[2-5]认为应选择以手术为主联合辅助化学治疗(以下简称“化疗”)的治疗方案。LMS-UB其主要预后因素为手术切缘是否为阴性、肿瘤大小、肿瘤浸润深度、病理分级以及是否存在远处转移等,其中最重要的预后因素为手术切缘是否为阴性[2-6]。故通常首选行根治性膀胱切除术(radical cystectomy,RC),但RC并发症多、术后患者的生活质量显著下降[7-8],对于早期低级别LMS-UB可选择行保留膀胱手术及联合辅助化疗,该治疗方案与RC相比可得到相似的长期生存率,且使患者有更高的生活质量[1, 9]。LMS-UB作为一种罕见且高度恶性的肿瘤,治疗上需精准化和多学科协作诊疗以改善患者的预后和提高患者的生活质量。现将中南大学湘雅二医院(以下简称“我院”)收治的1例低级别LMS-UB患者的临床资料和诊治情况报告如下。
1. 病例资料
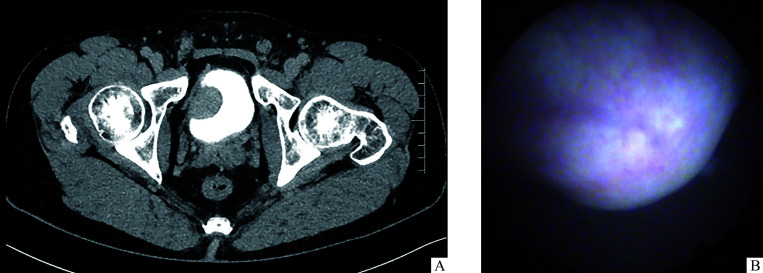
患者,男,44岁,因“尿痛2周”于2021年3月19日入住我院泌尿外科。患者于2021年3月无明显诱因开始出现尿痛症状,无血尿。曾在当地医院就诊,CT示膀胱右侧壁肿物,后于中南大学湘雅医院就诊,CT示膀胱右侧壁32 mm×24 mm×21 mm囊实性肿块,考虑膀胱癌可能(图1A)。来我院就诊,膀胱镜示膀胱右侧壁圆形隆起,表面光滑平整,与周围正常黏膜连续(图1B)。患者既往体健,吸烟20余年,平均20支/d,无疫区接触史、毒物及药物滥用史、恶性肿瘤病史、放射性物质接触史及手术史,家族中无特殊病史,体格检查无特殊。
图1.
1例膀胱平滑肌肉瘤患者术前盆腔CT和膀胱镜影像(2021年3月)
Figure 1 Preoperative pelvic CT and cystoscopy image of a patient with leiomyosarcoma of urinary bladder (March 2021)
A: Pelvic CT with delayed phase shows the mass on the right anterior part of the bladder. B: Cystoscopy shows a round bulge in the right anterior part of the bladder, and the spherical bulge’s surface is smooth and flat.
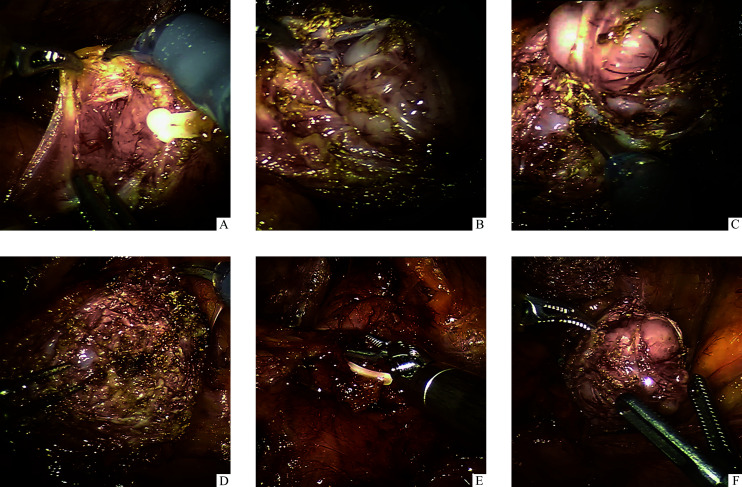
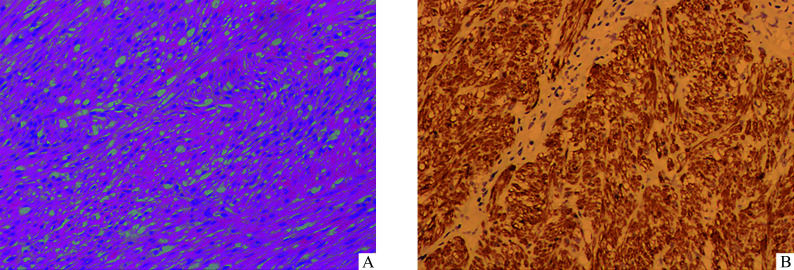
入院完善血常规、肝肾功能、电解质、凝血功能、肿瘤标志物、尿常规、大便常规、心电图等检查未见明显异常,B超提示膀胱右侧壁低回声团。根据患者的临床表现及检查结果考虑肿瘤可能来自间叶组织,且肿瘤为肌层浸润性。因患者年轻,对生活质量要求高,保留膀胱意愿强烈,肿瘤较小且无转移,故行机器人辅助腹腔镜下膀胱肿瘤剜除术。因术中可能存在损伤输尿管开口,术前行双侧D-J管植入。手术情况(图2):术中患者取头低脚高位,于其脐上4 cm置入镜头孔,左右器械臂孔位于脐水平各10 cm处,辅助孔位于右器械臂孔外侧,牵拉臂孔位于左器械臂孔外侧平脐水平及腋前线。于右侧髂总动脉水平打开后腹膜,见腹膜后靠膀胱右侧壁一直径约3 cm质硬肿块,向外突出,使用电剪打开膀胱浆膜层,发现肿瘤位于肌层,肿瘤包膜完整与正常组织分界明显,遂使用马里兰双极钳及电剪沿肿瘤包膜将肿瘤完整剥离,未损伤膀胱黏膜,使用3-0可吸收倒刺线缝合膀胱壁创面,充盈膀胱检查,无漏尿。手术时间共计85 min,术中出血量小于 20 mL。术后2 d拔除导尿管并出院,术后1个月拔除双侧D-J管。患者术后恢复良好,无并发症。术后病理检查:肿物有包膜,切面灰白编织状;镜下见肿瘤细胞呈梭形,轻-中度异型,灶性坏死,核分裂象每10个高倍视野(high power field,HPF)约3个。免疫组织化学:肌动蛋白肌肉特异性单克隆抗体(HHF35)(+),平滑肌肌动蛋白(smooth muscle actin,SMA)(+),结蛋白(Desmin)(+),高分子量钙调结合蛋白(H-caldesmon)(+)。基因检测:C-KIT和PDGFR-α基因野生型。结合免疫组织化学诊断为低级别平滑肌肉瘤(图3)。
图2.
1例膀胱平滑肌肉瘤行机器人辅助腹腔镜下剜除术的术中情况
Figure 2 Intraoperative conditions of robot-assisted laparoscopic enucleation in a patient with leiomyosarcoma of urinary bladder
A: Tumor located in the muscular layer; B and C: Tumor enucleated following the contour of the capsule; D: After the enucleation, no damage to the mucosal layer; E: After the enucleation, the bladder repaired with absorbable barbed sutures; F: Operative specimen.
图3.
1例膀胱平滑肌肉瘤行机器人辅助腹腔镜下剜除术的术后病理检查
Figure 3 Postoperative histopathological examination for a patient with leiomyosarcoma of urinary bladder
A: Tumor is composed of irregular intersecting bundles of spindle cells with nuclear pleomorphism (Hematoxylin and eosin staining, ×100). B: Tumor cells are positive forDesmin (Immunohistochemical staining, ×100).
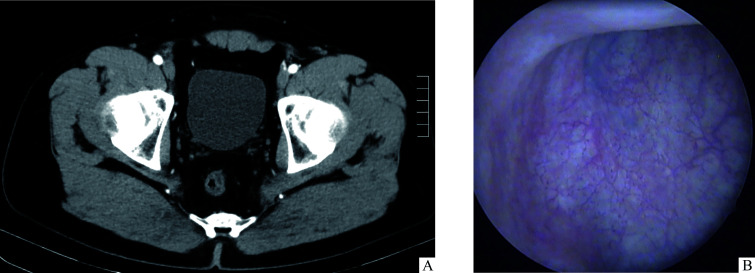
患者术后于2021年5月19日至9月1日在我院肿瘤科行5个周期辅助化疗,具体方案:异环磷酰胺(2 000 mg)第1~4天,静脉滴注每日1次;盐酸多柔比星脂质体(40 mg)第1天,静脉滴注1次。5个周期辅助化疗后患者无明显不适。术后每3个月定期随访患者1次,随访内容包括患者临床表现及辅助检查。患者术后未出现尿路刺激征、血尿、腹痛等症状,无手术并发症,术后生活质量高,复查全腹部、肺部增强CT和膀胱镜均未见LMS-UB复发及远处转移(图4)。
图4.
1例膀胱平滑肌肉瘤行机器人辅助腹腔镜下剜除术的术后腹部CT(A)和膀胱镜(B)影像未见复发或远处转移(2022年9月)
Figure 4 Postoperative abdominal CT (A) and cystoscopy (B) image showing no distant metastasis or recurrence in a patient with leiomyosarcoma of urinary bladder (September 2022)
2. 讨 论
平滑肌肉瘤是最常见的肉瘤之一,占所有软组织肉瘤的10%~20%,可以在身体的任何部位发生,通常发生在子宫、腹膜后等位置,累及膀胱极为罕见[10]。目前对LMS-UB的发病机制知之甚少,可能与视网膜母细胞瘤的pRb和p16基因突变、使用环磷酰胺化疗、盆腔放射治疗及反复尿路感染有关[2, 11-14]。大多数LMS-UB在诊断时已处于晚期,只有不到15%的患者在早期被发现,且肿瘤细胞多呈高级别改变,总体预后差[2],LMS-UB的中位生存率约为46个月,术后局部复发率约为16%,远处转移的复发率约为53%,最常见的转移部位为骨、肺、脑和肝[5]。
LMS-UB的主要临床表现为血尿、尿路刺激症和排尿困难,肿瘤好发于膀胱顶部、侧壁,很少发生在三角区[15]。笔者认为LMS-UB出现血尿,与肿瘤侵犯膀胱黏膜及黏膜下层密切相关,本例患者以尿痛为主要临床表现,无血尿,考虑肿瘤可能未侵犯膀胱黏膜及黏膜下层。膀胱镜常用于膀胱肿瘤筛查,在膀胱镜下尿路上皮癌通常呈菜花样改变,然而LMS-UB通常呈局限性隆起或者不规则溃疡性肿块[16]。在影像学检查中,CT平扫肿块多呈椭圆形或不规则形软组织密度影,肿块内密度均匀或不均匀,可见片状坏死区;CT增强扫描呈不均匀中度或明显强化,可见增粗迂曲血管影[17];MR的T1加权像上呈中等信号,T2加权像上呈不均匀低信号[18]。LMS-UB镜下特点:肿瘤细胞通常排列成束状,肿瘤细胞呈短梭形或卵圆形,胞质呈嗜酸性,可呈“雪茄形”核和核周空泡;免疫组织化学可见肌炎特异性抗体(myositis specific antibody,MSA)、SMA、Desmin等呈强阳性[19-22]。根据核异型性、有丝分裂活性和肿瘤坏死程度可将肿瘤分为高级别和低级别[20-22]。本例患者术后病理检查提示轻-中度异型,核分裂相约3个/10 HPF,<25%坏死,SMA(+),Desmin(+),考虑为低级别LMS-UB,故术后继续联合辅助化疗行保留膀胱的综合治疗。
LMS-UB在治疗上虽无明确共识,但目前大多数学者[2-5]认为应采用手术为主联合辅助化疗的综合治疗手段。在高级别晚期LMS-UB治疗上,考虑其侵袭性和预后不良,首选RC联合辅助化疗的综合治疗方案,但RC术后有性功能障碍、肠道功能障碍、吻合口狭窄和输尿管反流等并发症,患者生活质量严重下降[8]。因此在早期低级别LMS-UB治疗上,考虑患者术后生活质量和预后,可行保留膀胱手术及联合辅助化疗。化疗在LMS-UB治疗中的作用十分重要,既可以抑制肿瘤的生长和扩散,还可以降低术后病灶复发的风险。新辅助和术后化疗可以有效地缓解LMS-UB患者的临床症状和延长其生存期 [2, 5, 23],因此化疗已被广泛应用于LMS-UB的治疗中。目前一线化疗方案以蒽环类药物为基础,常用为多柔比星联合异环磷酰胺方案(AI方案)[15, 23-24]。在无法手术或术后复发的晚期及转移性LMS-UB患者中常进行姑息性化疗及靶向治疗。肿瘤血管生成是LMS-UB发生和转移的重要因素,故LMS-UB的靶向治疗常使用抗血管生成的酪氨酸激酶抑制剂[25]。
本例患者年轻,保留膀胱意愿强烈,肿瘤较小(直径<5 cm),术前检查未提示转移,故考虑行保留膀胱手术。达芬奇机器人与传统腹腔镜相比术中操作更加精细[26]、术中可细致观察肿瘤形态,进一步判断肿瘤性质,从而对治疗方式做出最佳选择[27],对于膀胱重建及相关的尿路重建有较大帮助[28-30],术中发现肿瘤与正常膀胱组织分界明显,行机器人辅助腹腔镜下膀胱肿瘤剜除术,术后予5个周期辅助化疗,术后定期复查膀胱镜、全腹部及肺部增强CT,未见明显复发及远处转移,患者术后生活质量高。目前,国内外暂无微创下行剜除术治疗LMS-UB的相关报道,膀胱肿瘤剜除术与经尿道膀胱肿瘤切除术和膀胱部分切除术相比,未损伤膀胱黏膜,创伤小,出血少,患者恢复快,漏尿及尿外渗等并发症少[31]。本病例为早期低级别未侵犯黏膜的LMS-UB提供了一种新的外科手术联合辅助化疗的治疗方案,可以减少并发症的发生和提高患者生活质量,但对于早期低级别LMS-UB行保留膀胱手术联合辅助化疗的可靠性,还需长期的随访及收集更多病例进行分析和论证。
综上所述,LMS-UB是一种极为罕见的高度侵袭性的恶性肿瘤,现无标准治疗方案,其治疗效果欠佳,预后不良,故应采用个性化及精准化治疗,需泌尿外科联合肿瘤科等多学科医师共同协作治疗该疾病。
基金资助
湖南省自然科学基金(2021JJ30977)。
This work was supported by the Natural Science Foundation of Hunan Province, China (2021JJ30977).
利益冲突声明
作者声称无任何利益冲突。
作者贡献
曾忠义 患者管理,临床资料收集,论文撰写及修改;吴枭、彭凯、任达 患者随访,图片整理,论文修改;朱煊、张磊 诊疗方案制订,论文设计、指导及修改。所有作者阅读并同意最终的文本。
原文网址
http://xbyxb.csu.edu.cn/xbwk/fileup/PDF/202305782.pdf
参考文献
- 1. Gupta DK, Singh V, Sinha RJ, et al. Leiomyosarcoma, a nonurothelial bladder tumor: a rare entity with therapeutic diversity[J]. Korean J Urol, 2013, 54(6): 409-411. 10.4111/kju.2013.54.6.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rodríguez D, Preston MA, Barrisford GW, et al. Clinical features of leiomyosarcoma of the urinary bladder: analysis of 183 cases[J]. Urol Oncol, 2014, 32(7): 958-965. 10.1016/j.urolonc.2014.01.025. [DOI] [PubMed] [Google Scholar]
- 3. Nazemi A, Daneshmand S. Adult genitourinary sarcoma: a population-based analysis of clinical characteristics and survival[J]. Urol Oncol, 2020, 38(5): 334-343. 10.1016/j.urolonc.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 4. Izumi K, Mizokami A, Sugimoto K, et al. Role of surgical resection in adult urological soft tissue sarcoma: 25-year experience[J]. Urol Int, 2010, 84(3): 309-314. 10.1159/000288234. [DOI] [PubMed] [Google Scholar]
- 5. Spiess PE, Kassouf W, Steinberg JR, et al. Review of the M.D. Anderson experience in the treatment of bladder sarcoma[J]. Urol Oncol, 2007, 25(1): 38-45. 10.1016/j.urolonc.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 6. Li LD, Liang JY, Song TR, et al. A nomogram model to predict prognosis of patients with genitourinary sarcoma[J]. Front Oncol, 2021, 11: 656325. 10.3389/fonc.2021.656325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Xu YF, Wang GC, Zheng JH, et al. Partial cystectomy: is it a reliable option for the treatment of bladder leiomyosarcoma?[J/OL]. Can Urol Assoc J, 2011, 5(1): E11-E13 [2022-09-28]. 10.5489/cuaj.10031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. 中华医学会泌尿外科学分会,中国膀胱癌联盟. 肌层浸润性膀胱癌保留膀胱综合治疗专家共识[J]. 中华泌尿外科杂志, 2022, 43(6): 401-406. 10.3760/cma.j.cn112330-20220629-00394. [DOI] [Google Scholar]; Chinese Urological Association, Chinese Bladder Cancer Consortium . Expert consensus on bladder-sparing treatment for muscle invasive bladder cancerin[J]. Chinese Journal of Urology, 2022, 43(6): 401-406. 10.3760/cma.j.cn112330-20220629-00394. [DOI] [Google Scholar]
- 9. Sato R, Watanabe D, Yonemasu H, et al. Total endoscopic management of a patient with urinary bladder leiomyosarcoma presenting with dysuria: a case report[J]. Urol Case Rep, 2018, 20: 45-47. 10.1016/j.eucr.2018.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. George S, Serrano C, Hensley ML, et al. Soft tissue and uterine leiomyosarcoma[J]. J Clin Oncol, 2018, 36(2): 144-150. 10.1200/JCO.2017.75.9845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ramírez Sevilla C, Admella-Salvador C, Romero-Martin JA, et al. Bladder leiomyosarcoma 25 years after treatment with cyclophosphamide in patient with history of retinoblastoma[J]. Urol Int, 2018, 100(1): 119-121. 10.1159/000437442. [DOI] [PubMed] [Google Scholar]
- 12. Chou WH, McGregor B, Schmidt A, et al. Cyclophosphamide-associated bladder cancers and considerations for survivorship care: a systematic review[J]. Urol Oncol, 2021, 39(10): 678-685. 10.1016/j.urolonc.2021.05.017. [DOI] [PubMed] [Google Scholar]
- 13. Ohan H, Minassian G, Minassian H, et al. Retinoblastoma in infancy with subsequent bladder leiomyosarcoma in adulthood: genomic considerations[J]. Urology, 2020, 140: 38-40. 10.1016/j.urology.2020.03.010. [DOI] [PubMed] [Google Scholar]
- 14. Ribeiro JG, Klojda CA, Araújo CP, et al. Giant leiomyosarcoma of the urinary bladder[J]. J Clin Diagn Res, 2016, 10(5): PD14-PD15. 10.7860/JCDR/2016/18971.7858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zieschang H, Koch R, Wirth MP, et al. Leiomyosarcoma of the urinary bladder in adult patients: a systematic review of the literature and Meta-analysis[J]. Urol Int, 2019, 102(1): 96-101. 10.1159/000494357. [DOI] [PubMed] [Google Scholar]
- 16. Fiorentino V, Pierconti F, Lenci N, et al. Urinary bladder leiomyosarcoma with osteoclast-like multinucleated giant cells: a case report[J]. BMC Cancer, 2019, 19(1): 763. 10.1186/s12885-019-5981-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. 姜喜锋, 徐红卫, 汪浒, 等. 膀胱非上皮性恶性肿瘤的CT表现[J]. 实用放射学杂志, 2018, 34(3): 389-391. 10.3969/j.issn.1002-1671.2018.03.016. [DOI] [Google Scholar]; JIANG Xifeng, XU Hongwei, WANG Hu, et al. CT manifestations of non-epithelial malignant tumors of bladder[J]. Journal of Practical Radiology, 2018, 34(3): 389-391. 10.3969/j.issn.1002-1671.2018.03.016. [DOI] [Google Scholar]
- 18. Wong-You-Cheong JJ, Woodward PJ, Manning MA, et al. From the archives of the AFIP: neoplasms of the urinary bladder: radiologic-pathologic correlation[J]. Radiographics, 2006, 26(2): 553-580. 10.1148/rg.262055172. [DOI] [PubMed] [Google Scholar]
- 19. 马平, 魏谨, 高福平. 原发膀胱平滑肌肉瘤临床病理分析及文献复习[J]. 现代肿瘤医学, 2013, 21(2): 424-426. 10.3969/j.issn.1672-4992.2013.02.69. [DOI] [Google Scholar]; MA Ping, WEI Jin, GAO Fuping. Leiomyosarcoma in urinary bladder clinicopathological feature and review of literature[J]. Journal of Modern Oncology, 2013, 21(2): 424-426. 10.3969/j.issn.1672-4992.2013.02.69. [DOI] [Google Scholar]
- 20. Martin SA, Sears DL, Sebo TJ, et al. Smooth muscle neoplasms of the urinary bladder: a clinicopathologic comparison of leiomyoma and leiomyosarcoma[J]. Am J Surg Pathol, 2002, 26(3): 292-300. 10.1097/00000478-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 21. Lee TK, Miyamoto H, Osunkoya AO, et al. Smooth muscle neoplasms of the urinary bladder: a clinicopathologic study of 51 cases[J]. Am J Surg Pathol, 2010, 34(4): 502-509. 10.1097/PAS.0b013e3181cf326d. [DOI] [PubMed] [Google Scholar]
- 22. Lindberg MR, Fisher C, Thway K, et al. Leiomyosarcoma of the urinary bladder: a clinicopathological study of 34 cases[J]. J Clin Pathol, 2010, 63(8): 708-713. 10.1136/jcp.2010.077883. [DOI] [PubMed] [Google Scholar]
- 23. Rosser CJ, Slaton JW, Izawa JI, et al. Clinical presentation and outcome of high-grade urinary bladder leiomyosarcoma in adults[J]. Urology, 2003, 61(6): 1151-1155. 10.1016/s0090-4295(03)00021-9. [DOI] [PubMed] [Google Scholar]
- 24. von Mehren M, Randall RL, Benjamin RS, et al. Soft tissue sarcoma, version 2. 2018, NCCN clinical practice guidelines in oncology[J]. J Natl Compr Canc Netw, 2018, 16(5): 536-563. 10.6004/jnccn.2018.0025. [DOI] [PubMed] [Google Scholar]
- 25. 崔抗, 赵瑞华, 冯涵. 软组织肉瘤靶向治疗药物的研究进展[J]. 中国临床新医学, 2019, 12(4): 366-371. 10.3969/j.issn.1674-3806.2019.04.04. [DOI] [Google Scholar]; CUI Kang, ZHAO Ruihua, FENG Han. Advances in targeted therapeutic drugs of soft tissue sarcoma[J]. Chinese Journal of New Clinical Medicine, 2019, 12(4): 366-371. 10.3969/j.issn.1674-3806.2019.04.04. [DOI] [Google Scholar]
- 26. 尹慧芳, 曾飞, 薛敏, 等. 机器人辅助腹腔镜下阴道骶骨固定术治疗盆腔器官脱垂的疗效[J]. 中南大学学报(医学版), 2020, 45(6): 709-714. 10.11817/j.issn.1672-7347.2020.190517. [DOI] [PubMed] [Google Scholar]; YIN Huifang, ZENG Fei, XUE Min, et al. Therapeutic effect of robot-assisted laparoscopic sacrocolpopexy in the treatment of pelvic organ prolapse[J]. Journal of Central South University.Medical Science, 2020, 45(6): 709-714. 10.11817/j.issn.1672-7347.2020.190517. [DOI] [PubMed] [Google Scholar]
- 27. 王宇昊, 夏佳东, 薛建新, 等. 机器人辅助腹腔镜下膀胱部分切除术治疗膀胱炎性肌纤维母细胞瘤1例[J]. 临床泌尿外科杂志, 2019, 34(10): 842-844. 10.13201/j.issn.1001-1420.2019.10.021. [DOI] [Google Scholar]; WANG Yuhao, XIA Jiadong, XUE Jianxin, et al. Robot-assisted laparoscopic partial cystectomy for bladder inflammatory myofibroblastic tumor: a case report[J]. Journal of Clinical Urology, 2019, 34(10): 842-844. 10.13201/j.issn.1001-1420.2019.10.021. [DOI] [Google Scholar]
- 28. Shakir NA, Zhao LC. Robotic-assisted genitourinary reconstruction: current state and future directions[J]. Ther Adv Urol, 2021, 13: 17562872211037111. 10.1177/17562872211037111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. 李品, 周辉霞, 曹华林, 等. 机器人辅助腹腔镜儿童膀胱横纹肌肉瘤切除术的疗效分析[J]. 中华泌尿外科杂志, 2020, 41(11): 856-860. 10.3760/cma.j.cn112330-20200622-00480. [DOI] [Google Scholar]; LI Pin, ZHOU Huixia, CAO Hualin, et al. Preliminary experience of robotic-assisted laparoscopic surgery for bladder rhabdomyosarcoma in children[J]. Chinese Journal of Urology, 2020, 41(11): 856-860. 10.3760/cma.j.cn112330-20200622-00480. [DOI] [Google Scholar]
- 30. 夏丹, 来翀, 王平, 等. 机器人辅助腔镜技术处理泌尿系统疾病: 单中心600例报道[J]. 中华泌尿外科杂志, 2016, 37(6): 403-406. 10.3760/cma.j.issn.1000-6702.2016.06.002. [DOI] [Google Scholar]; XIA Dan, LAI Chong, WANG Ping, et al. The robotic-assisted laparoscopic surgery treating urological diseases: experiences of 600 cases in a single medical center[J]. Chinese Journal of Urology, 2016, 37(6): 403-406. 10.3760/cma.j.issn.1000-6702.2016.06.002. [DOI] [Google Scholar]
- 31. 董效飞, 宋震, 张少青, 等. 腹腔镜肿瘤剜除术治疗浆膜下型膀胱平滑肌瘤的临床体会[J]. 中华腔镜泌尿外科杂志(电子版), 2018, 12(4): 270-273. 10.3877/cma.j.issn.1674-3253.2018.04.014. [DOI] [Google Scholar]; DONG Xiaofei, SONG Zhen, ZHANG Shaoqing, et al. Clinical experiences of laparoscopic enucleation of subserosal bladder leiomyoma[J]. Chinese Journal of Endourology. Electronic Edition, 2018, 12(4): 270-273. 10.3877/cma.j.issn.1674-3253.2018.04.014. [DOI] [Google Scholar]