Abstract
Objectives: Social isolation is recognised as a risk factor in the inflammatory process. This study explored the association between social isolation and the Dietary Inflammatory Index (DII) in community-dwelling older persons. Methods: This cross-sectional pilot study recruited 107 community-dwelling people aged over 55 years living in the Australian Capital Territory. Participants completed an extensive food frequency questionnaire and provided anthropometric and sociodemographic data. Social isolation was evaluated using the Lubben Social Network Scale (LSNS). Diet quality was assessed using DII. Results: Average age was 70.1 (±8.61) years and 62.8% were female. The average DII score was −1.10 (±1.21), indicating an anti-inflammatory diet. Higher LSNS was associated with lower DII (b (95% CI) = −0.041 (−0.066, −0.17); p < 0.01) and was positively influenced by the number of people in household (b (95% CI) = 5.731 (2.336, 9.127); p = 0.001). Conclusion: Increased risk of social isolation was associated with an increased tendency towards a more inflammatory diet. Reducing social isolation may decrease the inflammatory component of dietary intake for older persons living independently in the community.
Keywords: older adults, social isolation, dietary inflammatory index
1. Introduction
The role of nutrition as both a determinant of healthy ageing and a modifiable factor in maintaining a healthy phenotype is well established [1,2,3,4,5,6]. Equally well established is the role of non-dietary factors such as age-related physiological changes in the gut including early satiety [7,8], the diminution of senses of smell and taste [1,7,8], poor oral health [8,9], and several psychosocial factors, including social contact [7,8]. Additionally, the determinants of healthy eating for older persons are more than solely nutrition and involve complex interactions at both the individual and community levels [5,10,11,12] and a range of non-dietary factors [5,10,11,13,14,15] with a number of studies noting the association between increased risk of social isolation (and/or lack of social supports) with lower quality nutrition, including decreased intake of fruits and vegetables, reduced variety of foods, and lower energy intake [10,12,16,17,18,19,20].
Social isolation is increasingly becoming identified as a public health issue for older persons living in the community [13,21,22,23]. Factors contributing to social isolation include changed economic circumstances [22,24], declining physical health (including mobility challenges [22], loss of hearing and vision [13,25]), cognitive decline [26], death of a spouse [24], depression [13,22,27], and decreasing friendship circles [13,22,24]. Social isolation can also be associated with increased inflammatory response [28,29,30,31]. A study by Eisenberger (2016) summarises specific mechanisms demonstrating the role of social factors, such as social isolation, in immune system regulation including the impact of negative social factors that may result in pro-inflammatory responses [28,29,31]. There is a tendency for older persons to move physiologically to a pro-inflammatory state (inflammaging), [32,33,34,35,36] commonly associated with a number of ageing-related conditions such as dementia, sarcopenia, cardiovascular disease, Type 2 diabetes, and several cancers [36,37,38,39]. While not all studies are in agreement with the inflammatory markers involved, increased pro-inflammatory responses associated with negative social factors are reflected in increased levels of cytokines, C-reactive protein (CRP), and the upregulation of CD16 [28,29,30,31,40].
Compounding the negative effects of social isolation on inflammatory markers, the risk of social isolation has also been associated with poor nutritional health [16,17,19,41,42]. The impact on nutritional health due to social isolation includes increased risk of malnutrition [10,42], decreased fruit and vegetable intake [43], and decreased energy intake [10]. Poor dietary intake can result in inadequate nutrient intake and increased risk of malnutrition, with possible negative health consequences such as higher mortality risk [44,45], increased risk of sarcopenia [45] and falls [46], and poor wound healing [45,46]. Additionally, there is an established relationship between dietary intake and inflammatory response [40,47,48,49]. Diets high in whole grains, fruit and vegetables, nuts, and fish (such as the Mediterranean diet) have a positive association with lower concentrations of inflammatory markers such as CRP and tumour necrosis factor (TNF). This suggests a potential role of diet as a moderator of inflammatory response and as an important factor for healthy ageing [34,38,40,50]. The Dietary Inflammatory Index (DII) [49] is a validated dietary index assessing dietary intake with respect to the pro- and anti-inflammatory potential of food components.
There is an increasing desire of older Australians to age in place, that is, independently in their own home and community [51,52]. Ageing in place, as a concept, has the capacity to provide care appropriate to the needs of older persons at a lower cost than residential facilities and enables older persons to maintain both quality of life and independence in familiar surroundings [53,54]. However, several studies identify several known risks associated with ageing in place, including the linked risks of malnutrition and social isolation [41,42,55]. Given the link between social isolation and inflammaging and social isolation and poor diet quality, using DII as a measure of diet quality, this pilot study aims to explore if an increased risk of social isolation is associated with the inflammatory nature of dietary intake for older community-dwelling persons.
2. Methods
2.1. Sample
This was a cross-sectional pilot study of community-dwelling people aged 55 years and over living independently in the Australian Capital Territory (ACT). Participants were responders to advertisements on social media platforms, newsletters targeting older persons, and word of mouth (snowballing). Participants were eligible for inclusion if they were aged 55 years or older and living independently in the community in the ACT. No other exclusion factors were applied.
2.2. Ethics
The [University of Canberra] Human Ethics Committee approved this study prior to commencement (HREC #2079). Informed written consent was obtained from participants and all procedures were in accordance with the Declaration of Helsinki [56].
2.3. Participant Interviews
Participants attended a face-to-face interview (60–120 min) during which the following data were collected:
-
a.
Anthropometric and sociodemographic characteristics
Participants provided self-reported anthropometric data (height, weight, and waist circumference) and sociodemographic and lifestyle information (date of birth, education level, marital status, and number of people living in household). Body mass index (BMI) was calculated using self-reported data.
-
b.
Lubben Social Network Scale Score (LSNS)
The Lubben Social Network Scale Score (LSNS) is a validated survey tool specifically designed to assess the risk of social isolation in older populations [57,58]. This tool provides a composite measure of social connections amongst older persons with respect to contact with, and support provided by, family and friends. Interviewers administered the LSNS (12 questions) to measure social isolation risk. A minimum score of 0 (indicating high risk of social isolation) was possible, with maximum score of 60 (indicating low risk of social isolation).
-
c.
Dietary assessment
A validated and comprehensive 280-item Food Frequency Questionnaire (FFQ) [59,60,61,62] was completed where the frequency of consumption of a wide range of foods usually consumed over the previous 12 months was characterised. The FFQ additionally allowed free entry of foods/beverages not specifically covered. Data from the FFQ were analysed using Foodworks (v9; Xyris Software QLD, Brisbane, Australia).
2.4. Measure of Diet Quality—Dietary Inflammatory Index (DII) Score
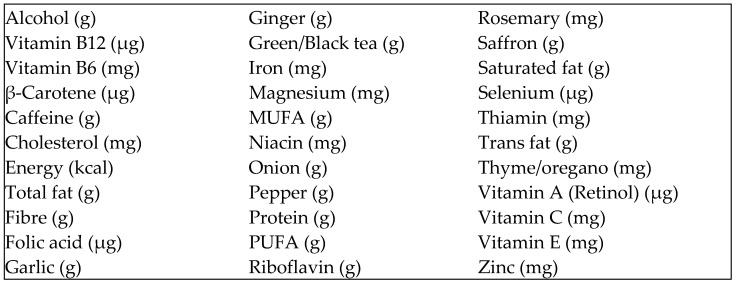
From Foodworks data, the DII scores were calculated in Microsoft Excel 2022 (Microsoft Corporation, Redmond, WA, USA) using the prescribed food parameters and algorithm [49]. Using this algorithm, DII scores tend to lie within the range from −6 (anti-inflammatory) to +6 (pro-inflammatory) with a theoretical possible range being −9.0 to +8.0 [49]. This study used 39 of the possible 45 food parameters (Figure 1). The food parameters were determined through a literature-based review of foods and food constituents and how they affect specific inflammatory markers [48]. Calculation of DII requires energy intake in kilocalories; therefore, energy intake was converted from kilojoules to kilocalories.
Figure 1.
Food parameters used to calculate DII score.
2.5. Statistical Analysis
Statistical analyses were completed using IBM® SPSS® Statistics for Windows, Version 27 (IBM Corp., Armonk, NY, USA, 2021). Continuous variables are presented as mean and standard deviation and categorical variables are presented as frequencies and relative frequencies. All variables were evaluated to determine normality and suitability for parametric or non-parametric methods using histograms, Q-Q plots, and the Kolmogorov–Smirnov test of normality. Means were compared using the Student’s Test (or Mann–Whitney U-test) to determine if differences between groups were significant. Associations between categorical variables were explored using Pearson’s Chi-squared test (or Fisher’s exact test when appropriate). Pearson’s (or Spearman’s rho) correlation coefficient was used to explore linear relationships between continuous variables. Multivariable linear regression analysis was used to explore independent associations between variables, after adjusting for potential confounding factors. Results are presented as unstandardised beta coefficients, 95% confidence interval, and p-value (p < 0.05, p < 0.001). Linearity of models was tested through scatter plots of standardised residuals against standardised predicted values. Statistical significance was set at alpha = 5%.
3. Results
3.1. Participant Characteristics
Participants (n = 107) were 70.2 ± 8.6 years (p = 0.030) of age. Most participants (n = 73) were female (68.2%); 62 participants (57.9%) were married; 65 participants (60.07%) were living in a household with one or more other person/s. With respect to education levels, 104 participants (97.2%) had completed post-secondary education with 80 participants (74.8%) having completed tertiary education. Most participants were retired (n = 80, 74.8%), and 27 participants (25.2%) were working either on a full-time or part-time/casual basis. Participant characteristics are summarised in Table 1 and Table 2.
Table 1.
Participant statistics summary by sex (n = 107).
| All | Male (M) | Female (F) | p-Value | |
|---|---|---|---|---|
| Number of Participants (n) | 107 | 34 (31.8%) | 73 (68.2%) | |
| Age (years) 1: | ||||
| Mean | 70.2 ± 8.6 | 72.8 ± 8.2 | 68.9 ± 8.5 | |
| Range | 56–94 | 60–94 | 56–88 | 0.030 |
| Marital Status: | 0.067 | |||
| Married | 62 (57.9%) | 25 (73.5%) | 37 (50.7%) | |
| Not Married—All | 45 (42.1%) | 9 (25.5%) | 36 (49.3%) | |
| Never Married | 9 | 1 | 8 | |
| Divorced | 15 | 1 | 14 | |
| Widowed | 16 | 6 | 10 | |
| Other | 5 | 1 | 4 | |
| Employment Status | 0.494 | |||
| Retired | 80 (74.8%) | 25 (73.5%) | 55 (75.3%) | |
| Employed—All | 27 (25.2%) | 9 (26.5%) | 18 (24.7%) | |
| Full-time | 12 | 3 | 9 | |
| Casual | 9 | 4 | 5 | |
| Part-time | 5 | 1 | 4 | |
| Unemployed | 1 | 1 | 0 | |
| Education | 0.102 | |||
| Year 10 only | 3 (2.8%) | 3 (8.8%) | 0 | |
| Post-secondary—All | 104 (97.2%) | 31 (91.2%) | 73 (100%) | |
| Year 12 | 7 | 1 | 6 | |
| Certificate/Diploma | 17 | 6 | 11 | |
| Undergraduate | 52 | 15 | 37 | |
| Post-graduate | 28 | 9 | 19 | |
| BMI (kg/m2) 1 | 25.19 ± 3.96 | 26.03 ± 3.73 | 24.79 ± 4.03 | |
| Range | 16.87–39.66 | 20.90–38.01 | 16.87–39.66 | 0.133 |
| Energy—Daily (kJ) 1 | 9297 ± 2249 | 9748 ± 2259 | 9087 ± 2228 | 0.158 |
| Range | 5254–16,091 | 5327–14,643 | 5254–16,091 | |
| DII Score 1 | −1.10 ± 1.21 | −0.70 ± 1.43 | −1.28 ± 1.04 | |
| Range | −3.46–+3.66 | −2.70–+3.66 | −3.46–0.85 | 0.018 |
| LSNS Score 1 | 38.7 ± 9.06 | 37.8 ± 7.58 | 39.0 ± 9.68 | |
| Range | 7–58 | 20–53 | 7–58 | 0.434 |
1 Values shown as mean ± SD. Note: DII—Dietary Inflammatory Index; LSNS—Lubben Social Network Scale.
Table 2.
Participant statistics summary by household type.
| All | Single Person Household | 2 or More Person Household | p-Value | |
|---|---|---|---|---|
| Number of Participants (n=) | 107 | 42 (39.3%) | 65 (60.07%) | |
| Age (years) 1: | ||||
| Mean | 70.2 ± 8.6 | 73.2 ± 8.9 | 68.2 ± 7.8 | |
| Range | 56–94 | 58–94 | 56-84 | 0.003 |
| Sex: | 0.065 | |||
| Male | 34 (32%) | 9 (26%) | 25 (74%) | |
| Female | 73 (68%) | 33 (45%) | 40 (55%) | |
| Marital Status: | <0.001 | |||
| Married (incl de facto) | 62 (57.9%) | 3 (7.2%) | 59 (90.8%) | |
| Not Married | 45 (42.1%) | 39 (92.8%) | 6 (9.2%) | |
| Never Married | 9 | 9 | 0 | |
| Divorced | 15 | 12 | 3 | |
| Widowed | 16 | 15 | 1 | |
| Other | 5 | 3 | 2 | |
| Employment Status: | 0.050 | |||
| Retired | 80 (74.8%) | 36 (85.7%) | 44 (67.1%) | |
| Employed | 27 (25.2%) | 6 (14.3%) | 21 (32.3%) | |
| Full-time | 12 | 3 | 9 | |
| Casual | 5 | 3 | 2 | |
| Part-time | 9 | 0 | 9 | |
| Unemployed | 1 | 0 | 1 | |
| Education: | 0.656 | |||
| Year 10 only | 3 (3%) | 1 (2.4%) | 2 (3.1%) | |
| Post-secondary | 104 (97%) | 41 (97.6%) | 63 (96.9%) | |
| Year 12 | 7 | 4 | 3 | |
| Certificate/Diploma | 17 | 5 | 12 | |
| Undergraduate | 52 | 19 | 33 | |
| Post-graduate | 28 | 13 | 15 | |
| BMI (kg/m2) 1 | 25.19 ± 3.96 | 25.26 ± 4.19 | 25.14 ± 3.84 | |
| Range | 16.87–39.66 | 16.87–39.66 | 18.27–38.01 | 0.879 |
| Energy—daily (kJ) 1 | 9297 ± 2249 | 8827 ± 2441 | 9600 ± 2078 | |
| Range | 5254–16,091 | 5254–16,091 | 5327–14,065 | 0.083 |
| DII Score 1 | −1.10 ± 1.21 | −0.79 ± 1.20 | −1.30 ±1.17 | |
| Range | −3.46–+3.66 | −3.46–+3.66 | −3.23–+2.38 | 0.030 |
| LSNS Score 1 | 38.7 ±9.06 | 35.2 ± 9.18 | 40.9 ± 8.23 | |
| Range | 7–58 | 7–48 | 20–58 | 0.001 |
1 Values shown as mean ± SD. Note: DII—Dietary Inflammatory Index; LSNS—Lubben Social Network Scale.
3.2. Dietary Intake
The average energy intake for all participants was 9297 ± 2249 kJ/day with intake ranging from 5254–16,091 kJ/day. Average energy intake varied between male and females and across household types. Average intake in one-person households was lower than in two-or-more-person households. However, the comparison of differences in means, based on sex and household type, found no statistical significance (p = 0.158 and 0.083, respectively). Average BMI was 25.19 ± 3.96 kg/m2 which is within an acceptable range for older persons.
3.3. Diet Quality
With respect to DII score, a more negative score indicates a less inflammatory diet. The mean DII score for all participants (−1.10 ± 1.2, p = 0.018) showed a tendency towards an anti-inflammatory diet; however, the overall range of scores is wide (−3.46 to +3.66, p = 0.030) with the widest range (−3.46 to +3.66) occurring in single-person households (Table 2). The comparison of DII means by household type and by sex found that these were associated with a less inflammatory score (p = 0.030 and p = 0.018, respectively). Univariable regression modelling found that LSNS negatively influenced DII score for all participants (b (95% CI) = −0.041 (−0.066, −0.17); p < 0.01) and explained 9.6% score variation amongst participants. Multiple regression modelling (Model 3, Table 3) adjusting for household type, sex, and age found that for every one unit increase in LSNS, DII will decrease (become less inflammatory) (b (95% CI) = −0.032 (−0.057, −0.006), p < 0.001), explaining 17.7% of score variation amongst participants. Further, Model 3 suggests that being female also influenced predicted DII score (b (95% CI) = −0.545 (−1.037, −0.053); p < 0.001) (Models 5 and 6). The univariate modelling of sex and DII shows that (b (95% CI) = −0.588 (−1.073, −0.102); p = 0.018), and R2 = 0.052.
Table 3.
Regression results for Lubben Social Network Scale Score: unstandardised B (95% Confidence Interval).
| Parameter | Unadjusted | Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | |
| Number of people in household (2 or more persons vs. 1 person) | 5.731 * | 2.336–9.127 | 6.159 * | 2.722–9.595 | 6.956 ** | 3.320–10.592 | 7.204 ** | 3.583–10.825 | 7.200 ** | 3.558–10.842 |
| Sex (Female vs. Male) | 2.510 | −1.094–6.114 | 3.188 | −0.552–6.927 | 3.177 | −0.533–6.888 | 3.161 | −0.609–6.931 | ||
| Age (per 1 year increase) | 0.137 | 0.072–0.346 | 0.172 | −0.040–0.384 | 0.172 | −0.041–0.3 | ||||
| Education level (Tertiary vs. Non-tertiary) | 3.155 | −0.717–7.026 | 3.155 | 0.381–20.792 | ||||||
| BMI (per 1 kg/m2 increase) | −0.012 | −0.434–0.400 | ||||||||
* Significant at p < 0.05 level. ** Significant at p < 0.001 level. Note: BMI—Body Mass Index.
3.4. Lubben Social Network Scale Scores
The average participant LSNS score was 38.7 ± 9.06 with a range of 7–58 (Table 2) suggesting that participants were generally not at high risk of social isolation. The average LSNS score for participants living in two-or-more-person households was higher than for participants in a single-person household (p = 0.001). No statistical significance for differences in means based on sex (p = 0.434) was observed. Multiple regression modelling adjusting for household type, sex, age, and BMI was undertaken (Table 4). Only household type was associated with an increased LSNS score (p < 0.001).
Table 4.
Regression Results for Dietary Inflammatory Index: Unstandardised B (95% Confidence Interval).
| Parameter | Unadjusted | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | |
| LSNS Score (per 1 unit increase) | 0.041 * | −0.066–−0.017 | −0.036 ** | −0.062–−0.010 | −0.032 * | −0.057–−0.006 | −0.033 * | −0.059–−0.008 | −0.030 * | −0.055–−0.004 | −0.030 * | −0.055–−0.004 |
| No. People in household (2 or more persons vs. 1 person) | −0.309 | −0.782–0.165 | −0.441 | −0.913–0.030 | −0.338 | −0.842–0.166 | −0.397 | −0.901–0.106 | −0.395 | −0.901–0.112 | ||
| Sex (Female vs. Male) | −0.627 * | −01.099–−0.156 | −0.545 * | −1.037–−0.053 | −0.555 * | −1.042–−0.067 | −0.543 | −1.038–−0.048 | ||||
| Age (per 1 year increase) | 0.016 | −0.012–0.43 | 0.010 | −0.017–0.038 | 0.010 | −0.018–0.038 | ||||||
| Education (Tertiary vs. Non-tertiary) | −0.440 | −0.945–0.065 | −0.444 | −0.952–0.064 | ||||||||
| BMI (per 1 kg/m2 increase) | 0.009 | −0.046–0.064 | ||||||||||
* Significant at <0.05 level. ** Significant at p < 0.001 level. Note: LSNS—Lubben Social Network Scale; BMI—Body Mass Index.
4. Discussion
There are a number of studies that support the association between inflammation, the ageing process, and the quality of ageing (inflammaging) and supporting the association between social isolation and the presence of inflammation. Additionally, older persons, particularly those ageing in the community, are at increased risk of social isolation, which is associated with both an increased risk of inflammation and reduced nutrition. The aim of this pilot project was to evaluate whether the risk of social isolation influenced the inflammatory quality of dietary intake for older independent community-living persons. The results suggest that the predicted DII score will be reduced by −0.041 units (indicative of a less inflammatory diet) for every unit increase in LSNS score (higher LSNS scores indicating lower risk of social isolation). The interactions between the risk of social isolation, inflammaging, and diet quality are multi-faceted and complex (refs [16,34,42]). However, the results of this pilot study suggest that lower risk of social isolation (as measured by LSNS) may be a contributory factor for persons following a less inflammatory diet.
While not specific to DII, these results are supported by several studies showing the negative impact of social isolation on dietary intake in older independent community living persons [10,11,15,63], predominantly through the impact on fruit and vegetable intake [10,64]. Additionally, studies have reported an association between dietary intake, sex, and social isolation, finding that men who are living alone, poorly supported socially, or experiencing social isolation are more nutritionally vulnerable [9,10,15] and consuming fewer servings of fruits and vegetables [10,15].
This pilot study additionally found that sex influenced the predicted DII score (−0.228, (CI = −1.073, −0.102), p = 0.018) for women. However, the influence was small, explaining only 5.2% of the sample variation. One possible explanation for the small effect relates to the self-selection of participants for the study, potentially reflecting an existing interest in nutrition coupled with the high level of education for most participants, suggesting that male participants may have a level of health literacy that may not be reflected in a larger population of older men [14,65]. Further, most male participants (73.5%) were married, with several studies noting the positive effects on nutritional intake experienced by married/partnered men [10,11,12,66].
One of the limitations of this study is that only risk of social isolation was measured. Several studies suggest that social isolation is more than a lack of social networks and poor social participation but includes an individual’s perception of isolation (expressed through feelings of loneliness) [27,28,67,68]. For example, an individual may have few social interactions and a limited social network but may not consider themselves lonely or experience feelings of social isolation. It is possible that some participants with low LSNS scores may not perceive themselves as at risk of social isolation, and some participants with higher LSNS scores may perceive the opposite. A study undertaken by Boulos [42] identified loneliness and social isolation as independent risk factors with respect to malnutrition among older persons. Future studies need to consider participants’ perception of social isolation to determine if the perception of social isolation, rather than risk, impacts DII scores, for example, by using the DeJong Giervald Loneliness Scale [69,70].
Additional limitations of this pilot include sex balance, self-reported data, and the single focus on food components relating to calculation of DII scores. Given that sex is known to influence nutritional behaviours and status amongst older persons, the greater number of female participants may have positively influenced DII results [9,10,15]. Further, most male participants were married, with marital status having a beneficial impact on nutritional status for males [9,10,15]. The self-reporting of anthropometric and food intake data for dietary assessment is a known limitation [71,72,73]. Weight and BMI are often under-reported [71], as are energy and fat intake [72,73]. To some extent, this limitation was mitigated through the design of the food frequency questionnaire to accommodate the free entry of food items not listed [73]. However, this remains a limitation of the study. While this pilot study focused on exploring the association between diet quality (as measured by DII) and the risk of social isolation, future studies should consider the impact of other modifiable lifestyle factors such as physical activity, smoking, and supplement intake.
The strengths of this study include its novelty in this population, its use of a validated measure of diet quality, and its contribution to the limited pool of nutrition studies investigating the link between diet quality and healthy ageing with respect to older persons ageing in place. Further analysis should also be undertaken to determine if specific dietary patterns/food choices were more prominent in those with a higher risk of social isolation, contributing to a more inflammatory nature of dietary intake.
5. Conclusions
The results of this pilot study suggest that a decreased risk of social isolation is associated with a less inflammatory diet in community-dwelling people aged 55 years or over, as measured by DII, with female participants having a lower DII score (less inflammatory). While the effects are small, our findings provide some evidence identifying the association between diet quality and the risk of social isolation in this population. These findings support that diet should be considered as an important pillar for healthy ageing and promoting the role of anti-inflammatory diets is an important component to modulate inflammaging in older persons who may be at risk of social isolation.
Author Contributions
Conceptualisation, N.M.D. and J.K. Methodology, N.M.D., J.K., N.N. and E.L. Validation, N.M.D. and E.G. Formal analysis, E.L. Investigation, E.L., N.M.D., D.R., M.B. and M.R. Data curation, E.L. Visualisation, E.L. and E.G. Writing—original draft preparation, E.L. Writing—review and editing, N.M.D., E.G., N.N., R.B., S.I., E.L., D.R., M.B., M.R. and J.K. Supervision, J.K., R.B., N.N., S.I., E.G. and N.M.D. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was approved by the Institutional Review Board (IRB) at The University of Canberra Human Ethics Committee (approval no. HREC #2079, approval date: 28 August 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Fluitman K.S., Hesp A.C., Kaihatu R.F., Nieuwdorp M., Keijser B.J., IJzerman R.G., Visser M. Poor Taste and Smell Are Associated with Poor Appetite, Macronutrient Intake, and Dietary Quality but Not with Undernutrition in Older Adults. J. Nutr. 2021;151:605–614. doi: 10.1093/jn/nxaa400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morley J.E. Undernutrition in Older Adults. Fam. Pract. 2012;29((Suppl. 1)):i89–i93. doi: 10.1093/fampra/cmr054. [DOI] [PubMed] [Google Scholar]
- 3.Locher J.L., Ritchie C.S., Robinson C.O., Roth D.L., Smith West D., Burgio K.L. A Multidimensional Approach to Understanding under-Eating in Homebound Older Adults: The Importance of Social Factors. Gerontologist. 2008;48:223–234. doi: 10.1093/geront/48.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wickramasinghe K., Mathers J.C., Wopereis S., Marsman D.S., Griffiths J.C. From Lifespan to Healthspan: The Role of Nutrition in Healthy Ageing. J. Nutr. Sci. 2020;9:e33. doi: 10.1017/jns.2020.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shlisky J., Bloom D.E., Beaudreault A.R., Tucker K.L., Keller H.H., Freund-Levi Y., Fielding R.A., Cheng F.W., Jensen G.L., Wu D., et al. Nutritional Considerations for Healthy Aging and Reduction in Age-Related Chronic Disease. Adv. Nutr. 2017;8:17–26. doi: 10.3945/an.116.013474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiefte-de Jong J.C., Mathers J.C., Franco O.H. Nutrition and Healthy Ageing: The Key Ingredients. Proc. Nutr. Soc. 2014;73:249–259. doi: 10.1017/S0029665113003881. [DOI] [PubMed] [Google Scholar]
- 7.Rémond D., Shahar D.R., Gille D., Pinto P., Kachal J., Peyron M.A., Dos Santos C.N., Walther B., Bordoni A., Dupont D., et al. Understanding the Gastrointestinal Tract of the Elderly to Develop Dietary Solutions That Prevent Malnutrition. Oncotarget. 2015;6:13858. doi: 10.18632/oncotarget.4030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitelock E., Ensaff H. On Your Own: Older Adults’ Food Choice and Dietary Habits. Nutrients. 2018;10:413. doi: 10.3390/nu10040413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Host A., McMahon A.-T., Walton K., Charlton K. Factors Influencing Food Choice for Independently Living Older People—A Systematic Literature Review. J. Nutr. Gerontol. Geriatr. 2016;35:67–94. doi: 10.1080/21551197.2016.1168760. [DOI] [PubMed] [Google Scholar]
- 10.Conklin A.I., Forouhi N.G., Surtees P., Khaw K.-T., Wareham N.J., Monsivais P. Social Relationships and Healthful Dietary Behaviour: Evidence from over-50s in the Epic Cohort, UK. Soc. Sci. Med. 2014;100:167–175. doi: 10.1016/j.socscimed.2013.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bloom I., Edwards M., Jameson K.A., Syddall H.E., Dennison E., Gale C.R., Baird J., Cooper C., Aihie Sayer A., Robinson S. Influences on Diet Quality in Older Age: The Importance of Social Factors. Age Ageing. 2017;46:277–283. doi: 10.1093/ageing/afw180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vesnaver E., Keller H.H. Social Influences and Eating Behavior in Later Life: A Review. J. Nutr. Gerontol. Geriatr. 2011;30:2–23. doi: 10.1080/01639366.2011.545038. [DOI] [PubMed] [Google Scholar]
- 13.Nicholson N.R. A Review of Social Isolation: An Important but Underassessed Condition in Older Adults. J. Prim. Prev. 2012;33:137–152. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 14.IrIrz X., Fratiglioni L., Kuosmanen N., Mazzocchi M., Modugno L., Nocella G., Shakersain B., Traill W.B., Xu W., Zanello G. Sociodemographic Determinants of Diet Quality of the Eu Elderly: A Comparative Analysis in Four Countries. Public Health Nutr. 2014;17:1177–1189. doi: 10.1017/S1368980013001146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shatenstein B., Gauvin L., Keller H., Richard L., Gaudreau P., Giroux F., Jabbour M., Morais J.A., Payette H. Individual and Collective Factors Predicting Change in Diet Quality over 3 Years in a Subset of Older Men and Women from the Nuage Cohort. Eur. J. Nutr. 2016;55:1671–1681. doi: 10.1007/s00394-015-0986-y. [DOI] [PubMed] [Google Scholar]
- 16.Bloom I., Lawrence W., Barker M., Baird J., Dennison E., Sayer A.A., Cooper C., Robinson S. What Influences Diet Quality in Older People? A Qualitative Study among Community-Dwelling Older Adults from the Hertfordshire Cohort Study, UK. Public Health Nutr. 2017;20:2685–2693. doi: 10.1017/S1368980017001203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Del Brutto O.H., Rumbea D.A., Mera R.M., Recalde B.Y., Sedler M.J. Social Determinants of Health (Social Risk) and Nutritional Status among Community-Dwelling Older Adults Living in a Rural Setting: The Atahualpa Project. J. Prim. Care Community Health. 2022;13:1–5. doi: 10.1177/21501319221087866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Locher J.L., Robinson C.O., Roth D.L., Ritchie C.S., Burgio K.L. The Effect of the Presence of Others on Caloric Intake in Homebound Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2005;60:1475–1478. doi: 10.1093/gerona/60.11.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pieroth R., Radler D.R., Guenther P.M., Brewster P.J., Marcus A. The Relationship between Social Support and Diet Quality in Middle-Aged and Older Adults in the United States. J. Acad. Nutr. Diet. 2017;117:1272–1278. doi: 10.1016/j.jand.2017.03.018. [DOI] [PubMed] [Google Scholar]
- 20.Sahyoun N.R., Zhang X.L. Dietary Quality and Social Contact among a Nationally Representative Sample of the Older Adult Population in the United States. J. Nutr. Health Aging. 2005;9:177–183. [PubMed] [Google Scholar]
- 21.Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An Overview of Systematic Reviews on the Public Health Consequences of Social Isolation and Loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 22.Moormann K.I., Pabst A., Bleck F., Löbner M., Kaduszkiewicz H., van der Leeden C., Hajek A., Brettschneider C., Heser K., Kleineidam L., et al. Social Isolation in the Oldest-Old: Determinants and the Differential Role of Family and Friends. Soc. Psychiatry Psychiatr. Epidemiol. 2023:1–10. doi: 10.1007/s00127-023-02524-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang J., Moorman S.M. Beyond the Individual: Evidence Linking Neighborhood Trust and Social Isolation among Community-Dwelling Older Adults. Int. J. Aging Hum. Dev. 2021;92:22–39. doi: 10.1177/0091415019871201. [DOI] [PubMed] [Google Scholar]
- 24.Courtin E., Knapp M. Social Isolation, Loneliness and Health in Old Age: A Scoping Review. Health Soc. Care Community. 2017;25:799–812. doi: 10.1111/hsc.12311. [DOI] [PubMed] [Google Scholar]
- 25.Moorman S.M., Greenfield E.A., Lee C.S.H. Perceived Hearing Loss, Social Disengagement, and Declines in Memory. J. Appl. Gerontol. 2021;40:679–683. doi: 10.1177/0733464820909244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Griffin S.C., Mezuk B., Williams A.B., Perrin P.B., Rybarczyk B.D. Isolation, Not Loneliness or Cynical Hostility, Predicts Cognitive Decline in Older Americans. J. Aging Health. 2020;32:52–60. doi: 10.1177/0898264318800587. [DOI] [PubMed] [Google Scholar]
- 27.Cornwell E.Y., Waite L.J. Social Disconnectedness, Perceived Isolation, and Health among Older Adults. J. Health Soc. Behav. 2009;50:31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith K.J., Gavey S., RIddell N.E., Kontari P., Victor C. The Association between Loneliness, Social Isolation and Inflammation: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2020;112:519–541. doi: 10.1016/j.neubiorev.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Leschak C.J., Eisenberger N.I. Two Distinct Immune Pathways Linking Social Relationships with Health: Inflammatory and Antiviral Processes. Psychosom. Med. 2019;81:711. doi: 10.1097/psy.0000000000000685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Powell N.D., Sloan E.K., Bailey M.T., Arevalo J.M., Miller G.E., Chen E., Kobor M.S., Reader B.F., Sheridan J.F., Cole S.W. Social Stress up-Regulates Inflammatory Gene Expression in the Leukocyte Transcriptome Via Β-Adrenergic Induction of Myelopoiesis. Proc. Natl. Acad. Sci. USA. 2013;110:16574–16579. doi: 10.1073/pnas.1310655110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eisenberger N.I., Moieni M., Inagaki T.K., Muscatell K.A., Irwin M.R. In Sickness and in Health: The Co-Regulation of Inflammation and Social Behavior. Neuropsychopharmacology. 2017;42:242–253. doi: 10.1038/npp.2016.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morrisette-Thomas V., Cohen A.A., Fülöp T., Riesco É., Legault V., Li Q., Milot E. Inflamm-Aging Does Not Simply Reflect Increases in Pro-Inflammatory Markers. Mech. Ageing Dev. 2014;139:49–57. doi: 10.1016/j.mad.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Franceschi C., Campisi J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2014;69((Suppl. S1)):S4–S9. doi: 10.1093/gerona/glu057. [DOI] [PubMed] [Google Scholar]
- 34.Di Giosia P., Stamerra C.A., Giorgini P., Jamialahamdi T., Butler A.E., Sahebkar A. The Role of Nutrition in Inflammaging. Ageing Res. Rev. 2022;77:101596. doi: 10.1016/j.arr.2022.101596. [DOI] [PubMed] [Google Scholar]
- 35.Kemoun P.H., Ader I., Planat-Benard V., Dray C., Fazilleau N., Monsarrat P., Cousin B., Paupert J., Ousset M., Lorsignol A., et al. A Gerophysiology Perspective on Healthy Ageing. Ageing Res. Rev. 2022;73:101537. doi: 10.1016/j.arr.2021.101537. [DOI] [PubMed] [Google Scholar]
- 36.Dugan B., Conway J., Duggal N.A. Inflammaging as a Target for Healthy Ageing. Age Ageing. 2023;52:afac328. doi: 10.1093/ageing/afac328. [DOI] [PubMed] [Google Scholar]
- 37.vel Szic K.S., Declerck K., Vidaković M., Vanden Berghe W. From Inflammaging to Healthy Aging by Dietary Lifestyle Choices: Is Epigenetics the Key to Personalized Nutrition? Clin. Epigenet. 2015;7:33. doi: 10.1186/s13148-015-0068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Assmann K.E., Adjibade M., Shivappa N., Hébert J.R., Wirth M.D., Touvier M., Akbaraly T., Hercberg S., Galan P., Julia C., et al. The Inflammatory Potential of the Diet at Midlife Is Associated with Later Healthy Aging in French Adults. J. Nutr. 2018;148:437–444. doi: 10.1093/jn/nxx061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shivappa N., Godos J., Hébert J.R., Wirth M.D., Piuri G., Speciani A.F., Grosso G. Dietary Inflammatory Index and Colorectal Cancer Risk—A Meta-Analysis. Nutrients. 2017;9:1043. doi: 10.3390/nu9091043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corley J., Shivappa N., Hébert J.R., Starr J., Deary I. Associations between Dietary Inflammatory Index Scores and Inflammatory Biomarkers among Older Adults in the Lothian Birth Cohort 1936 Study. J. Nutr. Health Aging. 2019;23:628–636. doi: 10.1007/s12603-019-1221-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Romero-Ortuno R., Casey A.M., Cunningham C.U., Squires S., Prendergast D., Kenny R.A., Lawlor B.A. Psychosocial and Functional Correlates of Nutrition among Community-Dwelling Older Adults in Ireland. J. Nutr. Health Aging. 2011;15:527–531. doi: 10.1007/s12603-010-0278-4. [DOI] [PubMed] [Google Scholar]
- 42.Boulos C., Salameh P., Barberger-Gateau P. Social Isolation and Risk for Malnutrition among Older People. Geriatr. Gerontol. Int. 2017;17:286–294. doi: 10.1111/ggi.12711. [DOI] [PubMed] [Google Scholar]
- 43.Kalousova L. Social Isolation as a Risk Factor for Inadequate Diet of Older Eastern Europeans. Int. J. Public Health. 2014;59:707–714. doi: 10.1007/s00038-014-0582-6. [DOI] [PubMed] [Google Scholar]
- 44.van der Pols-Vijlbrief R., Wijnhoven H.A., Molenaar H., Visser M. Factors Associated with (Risk of) Undernutrition in Community-Dwelling Older Adults Receiving Home Care: A Cross-Sectional Study in the Netherlands. Public Health Nutr. 2016;19:2278–2289. doi: 10.1017/S1368980016000288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Norman K., Haß U., Pirlich M. Malnutrition in Older Adults—Recent Advances and Remaining Challenges. Nutrients. 2021;13:2764. doi: 10.3390/nu13082764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roberts H.C., Lim S.E., Cox N.J., Ibrahim K. The Challenge of Managing Undernutrition in Older People with Frailty. Nutrients. 2019;11:808. doi: 10.3390/nu11040808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang P., Song M., Eliassen A.H., Wang M., Fung T.T., Clinton S.K., Rimm E.B., Hu F.B., Willett W.C., Tabung F.K., et al. Optimal Dietary Patterns for Prevention of Chronic Disease. Nat. Med. 2023;29:719–728. doi: 10.1038/s41591-023-02235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cavicchia P.P., Steck S.E., Hurley T.G., Hussey J.R., Ma Y., Ockene I.S., Hébert J.R. A New Dietary Inflammatory Index Predicts Interval Changes in Serum High-Sensitivity C-Reactive Protein. J. Nutr. 2009;139:2365–2372. doi: 10.3945/jn.109.114025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shivappa N., Steck S.E., Hurley T.G., Hussey J.R., Hébert J.R. Designing and Developing a Literature-Derived, Population-Based Dietary Inflammatory Index. Public Health Nutr. 2014;17:1689–1696. doi: 10.1017/S1368980013002115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Peng M., Yuan S., Lu D., Ling Y., Huang X., Lyu J., Xu A. Dietary Inflammatory Index, Genetic Susceptibility and Risk of Incident Dementia: A Prospective Cohort Study from Uk Biobank. J. Neurol. 2023:1–11. doi: 10.1007/s00415-023-12065-7. [DOI] [PubMed] [Google Scholar]
- 51.Rose K., Kozlowski D., Horstmanshof L. Experiences of Ageing in Place in Australia and New Zealand: A Scoping Review. J. Community Appl. Soc. Psychol. 2023;33:623–645. doi: 10.1002/casp.2669. [DOI] [Google Scholar]
- 52.Australian Institute of Health and Welfare . The Desire to Age in Place among Older Australians Canberra. AIHW; Canberra, Australia: 2013. Contract No.: Cat. No. AUS 169. [Google Scholar]
- 53.Sixsmith A., Sixsmith J. Ageing in Place in the United Kingdom. Ageing Int. 2008;32:219–235. doi: 10.1007/s12126-008-9019-y. [DOI] [Google Scholar]
- 54.Pani-Harreman K.E., Bours G.J., Zander I., Kempen G.I., van Duren J.M. Definitions, Key Themes and Aspects of ‘Ageing in Place’: A Scoping Review. Ageing Soc. 2021;41:2026–2059. doi: 10.1017/S0144686X20000094. [DOI] [Google Scholar]
- 55.Bjørner T., Korsgaard D., Reinbach H.C., Perez-Cueto F.J. A Contextual Identification of Home-Living Older Adults’ Positive Mealtime Practices: A Honeycomb Model as a Framework for Joyful Aging and the Importance of Social Factors. Appetite. 2018;129:125–134. doi: 10.1016/j.appet.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 56.World Medical Association World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 57.Lubben J., Blozik E., Gillmann G., Iliffe S., von Renteln Kruse W., Beck J.C., Stuck A.E. Performance of an Abbreviated Version of the Lubben Social Network Scale among Three European Community-Dwelling Older Adult Populations. Gerontologist. 2006;46:503–513. doi: 10.1093/geront/46.4.503. [DOI] [PubMed] [Google Scholar]
- 58.Lubben J.E. Assessing Social Networks among Elderly Populations. Fam. Community Health. 1988;11:42–52. doi: 10.1097/00003727-198811000-00008. [DOI] [Google Scholar]
- 59.D’Cunha N.M., Georgousopoulou E.N., Boyd L., Veysey M., Sturm J., O’Brien B., Lucock M., McKune A.J., Mellor D.D., Roach P.D., et al. Relationship between B-Vitamin Biomarkers and Dietary Intake with Apolipoprotein E ε4 in Alzheimer’s Disease. J. Nutr. Gerontol. Geriatr. 2019;38:173–195. doi: 10.1080/21551197.2019.1590287. [DOI] [PubMed] [Google Scholar]
- 60.Beckett E.L., Martin C., Boyd L., Porter T., King K., Niblett S., Yates Z., Veysey M., Lucock M. Reduced Plasma Homocysteine Levels in Elderly Australians Following Mandatory Folic Acid Fortification—A Comparison of Two Cross-Sectional Cohorts. J. Nutr. Intermed. Metab. 2017;8:14–20. doi: 10.1016/j.jnim.2017.04.001. [DOI] [Google Scholar]
- 61.Dufficy L., Naumovski N., Ng X., Blades B., Yates Z., Travers C., Lewis P., Sturm J., Veysey M., Roach P.D., et al. G80a Reduced Folate Carrier Snp Influences the Absorption and Cellular Translocation of Dietary Folate and Its Association with Blood Pressure in an Elderly Population. Life Sci. 2006;79:957–966. doi: 10.1016/j.lfs.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 62.Ambrosini G., Mackerras D., De Klerk N., Musk A. Comparison of an Australian Food-Frequency Questionnaire with Diet Records: Implications for Nutrition Surveillance. Public Health Nutr. 2003;6:415–422. doi: 10.1079/PHN2002434. [DOI] [PubMed] [Google Scholar]
- 63.Locher J.L., Ritchie C.S., Roth D.L., Baker P.S., Bodner E.V., Allman R.M. Social Isolation, Support, and Capital and Nutritional Risk in an Older Sample: Ethnic and Gender Differences. Soc. Sci. Med. 2005;60:747–761. doi: 10.1016/j.socscimed.2004.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sahyoun N.R., Zhang X.L., Serdula M.K. Barriers to the Consumption of Fruits and Vegetables among Older Adults. J. Nutr. Elder. 2006;24:5–21. doi: 10.1300/J052v24n04_03. [DOI] [PubMed] [Google Scholar]
- 65.Schoufour J.D., de Jonge E.A., Kiefte-de Jong J.C., van Lenthe F.J., Hofman A., Nunn S.P., Franco O.H. Socio-Economic Indicators and Diet Quality in an Older Population. Maturitas. 2018;107:71–77. doi: 10.1016/j.maturitas.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 66.Hughes G., Bennett K.M., Hetherington M.M. Old and Alone: Barriers to Healthy Eating in Older Men Living on Their Own. Appetite. 2004;43:269–276. doi: 10.1016/j.appet.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 67.De Jong Gierveld J., Havens B. Cross-National Comparisons of Social Isolation and Loneliness: Introduction and Overview. Can. J. Aging/Rev. Can. Vieil. 2004;23:109–113. doi: 10.1353/cja.2004.0021. [DOI] [PubMed] [Google Scholar]
- 68.Petersen N., König H.-H., Hajek A. The Link between Falls, Social Isolation and Loneliness: A Systematic Review. Arch. Gerontol. Geriatr. 2020;88:104020. doi: 10.1016/j.archger.2020.104020. [DOI] [PubMed] [Google Scholar]
- 69.Penning M.J., Liu G., Chou P.H.B. Measuring Loneliness among Middle-Aged and Older Adults: The Ucla and De Jong Gierveld Loneliness Scales. Soc. Indic. Res. 2014;118:1147–1166. doi: 10.1007/s11205-013-0461-1. [DOI] [Google Scholar]
- 70.De Jong Gierveld J., Van Tilburg T. The De Jong Gierveld Short Scales for Emotional and Social Loneliness: Tested on Data from 7 Countries in the Un Generations and Gender Surveys. Eur. J. Ageing. 2010;7:121–130. doi: 10.1007/s10433-010-0144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Flegal K.M., Ogden C.L., Fryar C., Afful J., Klein R., Huang D.T. Comparisons of Self-Reported and Measured Height and Weight, Bmi, and Obesity Prevalence from National Surveys: 1999–2016. Obesity. 2019;27:1711–1719. doi: 10.1002/oby.22591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kirkpatrick S.I., Vanderlee L., Raffoul A., Stapleton J., Csizmadi I., Boucher B.A., Massarelli I., Rondeau I., Robson P.J. Self-Report Dietary Assessment Tools Used in Canadian Research: A Scoping Review. Adv. Nutr. 2017;8:276–289. doi: 10.3945/an.116.014027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ravelli M.N., Schoeller D.A. Traditional Self-Reported Dietary Instruments Are Prone to Inaccuracies and New Approaches Are Needed. Front. Nutr. 2020;7:90. doi: 10.3389/fnut.2020.00090. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are contained within the article.