Abstract
目的
目前国内已有超声、肌电或CT引导下环咽肌A型肉毒毒素(botulinum toxin Type A,BTX-A)注射治疗环咽肌失迟缓的研究,但鲜见内镜引导下环咽肌BTX-A注射的研究报道。本研究拟探讨消化内镜引导下BTX-A注射联合球囊扩张治疗脑干梗死后环咽肌失弛缓的疗效,为脑干梗死后吞咽障碍治疗提供一种更好的治疗方法。
方法
选择2022年6月至12月长沙市第一医院康复医学科收治的脑干梗死环咽肌失迟缓患者30例,随机分为对照组与联合组,每组15例。2组患者均进行常规康复治疗,对照组行球囊扩张治疗,联合组行球囊扩张治疗和环咽肌BTX-A注射治疗。于治疗前和治疗2周后行吞咽造影检查,采用渗漏/误吸量表(Penetration-aspiration Scale,PAS)、吞咽障碍结局与严重度量表(Dysphagia Outcome Severity Scale,DOSS)、功能性经口摄食量表(Functional Oral Intake Scale,FOIS)评估患者的吞咽功能。
结果
联合组有1例患者因个人原因自行退出。治疗2周后,2组DOSS评分、PAS评分、FOIS分级均优于治疗前(均P<0.01),且联合组均优于对照组(均P<0.001)。联合组的治疗有效率为85.7%,对照组有效率为66.7%,2组比较差异无统计学意义(P>0.05)。
结论
环咽肌BTX-A注射联合球囊扩张较单独使用球囊扩张对改善吞咽功能效果更好,值得临床推广应用。
Keywords: 环咽肌失弛缓, 吞咽障碍, 脑干梗死, 肉毒毒素, 内镜
Abstract
Objective
At present, there are many reports about the treatment of cricopharyngeal achalasia by injecting botulinum toxin type A (BTX-A) into cricopharyngeal muscle guided by ultrasound, electromyography or CT in China, but there is no report about injecting BTX-A into cricopharyngeal muscle guided by endoscope. This study aims to evaluate the efficacy of endoscopic BTX-A injection combined with balloon dilatation in the treatment of cricopharyngeal achalasia after brainstem stroke, and to provide a better method for the treatment of dysphagia after brainstem stroke.
Methods
From June to December 2022, 30 patients with cricopharyngeal achalasia due to brainstem stroke were selected from the Department of Rehabilitation Medicine, the First Hospital of Changsha. They were randomly assigned into a control group and a combined group, 15 patients in each group. Patients in both groups were treated with routine rehabilitation therapy, while patients in the control group were treated with balloon dilatation, and patients in the combined group were treated with balloon dilatation and BTX-A injection. Before treatment and after 2 weeks of treatment, the patients were examined by video fluoroscopic swallowing study, Penetration-aspiration Scale (PAS), Dysphagia Outcome Severity Scale (DOSS), and Functional Oral Intake Scale (FOIS) were used to assess the swallowing function.
Results
In the combined group, 1 patient withdrew from the treatment because of personal reasons. Two weeks after treatment, the scores of DOSS, PAS, and FOIS in both groups were better than those before treatment (all P<0.01), and the combined group was better than the control group (all P<0.001). The effective rate was 85.7% in the combined group and 66.7% in the control group, with no significant difference between the 2 groups (P>0.05).
Conclusion
BTX-A injection combined with balloon dilatation is more effective than balloon dilatation alone in improving swallowing function and is worthy of clinical application.
Keywords: cricopharyngeal achalasia, dysphagia, brainstem stroke, botulinum toxin, endoscope
脑干梗死后吞咽障碍发生率高达81%,需要留置鼻饲管,严重影响患者的生活质量,常导致吸入性肺炎加重病情[1]。环咽肌失迟缓是脑干梗死后吞咽障碍的主要原因,目前国内外针对环咽肌失弛缓症的治疗方法主要有导尿管球囊扩张术、环咽肌肉毒毒素注射及环咽肌切开术[2]。导尿管球囊扩张术由于经济、简便在临床应用较广泛,但其扩张幅度有限,疗效有待于进一步提高。1994年英国学者Schneider等[3]率先应用A型肉毒毒素(botulinum toxin Type A,BTX-A)注射治疗环咽肌失弛缓。环咽肌BTX-A 注射技术包括超声引导[4]、内镜引导[5]、CT引导[6]和肌电引导[7]。目前国内已有超声、肌电或CT引导下环咽肌BTX-A注射的研究[8-12],但鲜见内镜引导下环咽肌BTX-A注射的研究报道。本研究拟探讨消化内镜引导下BTX-A注射联合球囊扩张治疗脑干梗死后环咽肌失弛缓的效果,旨在为脑干梗死后吞咽障碍治疗提供一种更好的治疗方法。
1. 资料与方法
1.1. 一般资料
选取2022年6月至12月长沙市第一医院康复科收治的30例发病时间超过2个月的脑干梗死后环咽肌失迟缓患者,随机将患者分为对照组和联合组,各15例。将符合入组标准的患者,按照就诊或入院先后顺序进行编号(1~30),然后采用Minitab软件实现随机化分配,前15号作为对照组,后15号作为联合组。本研究经医院伦理委员会批准[审批号:(2022)伦快审〔临研〕第(12)号],并获得所有入选患者的知情同意。纳入标准:1)符合1995年中华医学会全国第四次脑血管病会议的诊断标准,并经CT或MRI检查确诊为脑干梗死的患者;不合并脑干外其他部位的脑梗死或损伤;2)年龄18~80岁;3)吞咽障碍持续2个月未好转;4)脑卒中前无吞咽障碍病史;5)生命体征稳定,意识清楚;6)经吞咽造影检查确认为环咽肌不开放或部分开放患者。排除标准:1)肉毒毒素过敏患者;2)不配合检查和治疗的严重认知障碍患者;3)凝血功能障碍患者;4)既往有其他原因导致吞咽障碍的患者。脱落标准:1)治疗期间出现其他病症而影响本研究的患者;2)因主观因素自行退出患者。
1.2. 治疗方法
2组患者均给予常规吞咽康复训练,且由同一康复治疗团队实施。在此基础上,对照组给予球囊扩张治疗,联合组给予环咽肌BTX-A注射和球囊扩张治疗。
常规吞咽康复训练:进行口颜面感觉运动功能训练,包括口周、舌部肌肉运动、冰棒刺激、门德尔松训练、坐位进食姿势指导训练等,每次30 min,每日1次,每周5次,连续治疗2周。吞咽神经肌肉电刺激采用常州雅思YS1001J吞咽障碍治疗仪进行,操作方法为电极片分别放置于颏下及甲状软骨切迹上方。刺激强度2~10 mA,以患者的耐受度为主,刺激时间20 min,每日1次,每周5次,连续治疗2周。
球囊扩张:经鼻孔将导管插入食道中,确定导管进入食道并完全穿过环咽肌后,向导管内注入2.5 mL的水作为起始量。将导尿管缓慢向外拉出,直到有卡住感觉或拉不动时,此处相当于环咽肌下缘。嘱患者右转头做主动用力吞咽动作,同时轻轻地缓慢向上牵拉导管,至球囊通过环咽肌狭窄处阻力锐减时,迅速将球囊中的水抽出。每天1次,每次5~8个轮回。在治疗过程中根据患者环咽肌阻力情况,适当调整球囊注水量。患者能主动经口进食时停止球囊扩张治疗,每周治疗5 d,连续治疗2周。
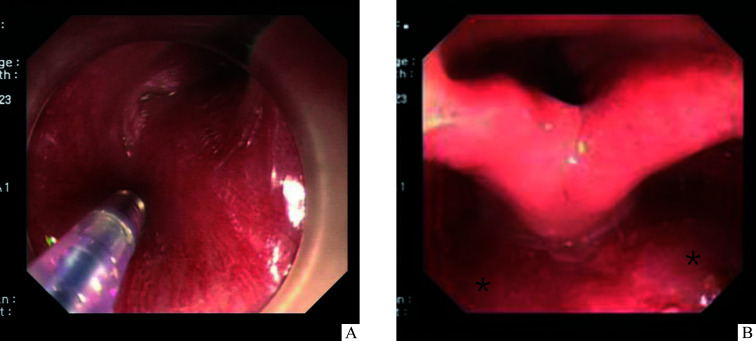
消化内镜引导下BTX-A注射:在消化内镜室由同一消化科医师操作,在内镜下选择环咽肌双侧腹侧各1个注射位点,每个位点注射BTX-A 30 U(兰州衡力生物技术开发有限公司,用生理盐水稀释至 100 U/mL),共注射60 U,观察局部无出血后退出内镜(图1)。术后第2天由吞咽康复治疗师遵循上述方法进行常规吞咽康复训练。
图1.
消化内镜引导下环咽肌BTX-A注射
Figure 1 Endoscopic guided injection of BTX-A into the cricopharyngeal muscle
A: BTX-A is injected using an endoscope via a needle catheter into cricopharyngeal muscle. B: Asterisks indicate the 2 injection sites of cricopharyngeal muscle under the endoscope. BTX-A: Botulinum toxin Type A.
1.3. 吞咽功能评价方法
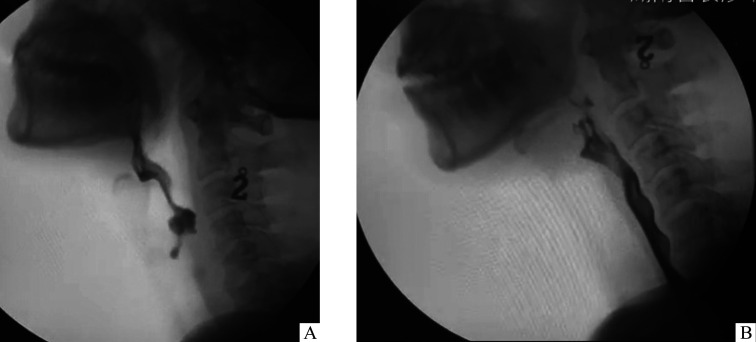
采用荷兰飞利浦医疗系统研发和制造中心有限公司Proxidiagnost N90遥控双床胃肠透视X线机进行吞咽造影检测,通过正位及侧位影像评估患者在进食过程中的吞咽情况(图2)。主要观察头部及口腔控制、吞咽启动、环咽肌开放、会厌谷及梨状窦残留程度、残留食物的清除能力、渗漏及误吸、咳嗽能力等情况,采用渗漏/误吸量表(Penetration-aspiration Scale,PAS)和吞咽障碍结局与严重度量表(Dysphagia Outcome Severity Scale,DOSS)进行定量评估,PAS量表和DOSS量表分别参照文献[13]和[14]。同时,采用功能性经口摄食量表(Functional Oral Intake Scale,FOIS)[15]评估患者的吞咽功能,FOIS根据吞咽障碍严重程度分为1~7级,1级为严重吞咽障碍,7级为吞咽功能正常,提高1级即为治疗有效。
图2.
吞咽造影
Figure 2 Swallowing imaging
A: Cricopharyngeal muscle is basically not open, and the concentrated barium contrast agent stagnated in the lower pharynx, mistakenly inhaling into the airway before botulinum toxin injection. B: Cricopharyngeal muscle opens and a concentrated barium contrast agent passes through the upper esophagus after 2 weeks of botulinum toxin injection.
1.4. 统计学处理
采用SPSS 22.0统计软件进行数据分析。符合正态分布的计量资料以均数±标准差( ±s)表示,治疗前后比较采用配对t检验,组间比较采用独立样本t检验;计数资料以例(%)表示,采用Fisher确切概率法检验;病程不符合正态分布,比较采用Mann-Whitney U检验。P<0.05为差异具有统计学意义。
2. 结 果
2.1. 2组患者一般资料比较
2组患者一般资料比较差异无统计学意义(均P>0.05,表1),具有可比性。联合组有1例患者因个人原因自行退出。
表1.
2组患者一般资料比较
Table 1 Comparison of general data between 2 groups
| 组别 | n | 年龄/岁 | 性别(男/女)/例 |
梗死部位 (延髓/脑桥)/例 |
病程/d | 留置胃管/例 |
环咽肌(完全不开放/ 部分不开放)/例 |
|---|---|---|---|---|---|---|---|
| 联合组 | 14 | 65.8±5.7 | 11/3 | 10/4 | 87.2±15.7 | 14 | 9/5 |
| 对照组 | 15 | 67.6±6.1 | 10/5 | 12/3 | 90.7±14.2 | 15 | 10/5 |
| t/χ 2 | 0.759 | 0.717 | 0.539 | 0.631 | 0.000 | 0.135 | |
| P | 0.455 | 0.474 | 0.589 | 0.534 | 1.000 | 0.893 |
2.2. 2组患者治疗前后吞咽功能比较
治疗前,2组DOSS评分、PAS评分、FOIS分级比较,差异均无统计学意义(均P>0.05)。治疗2周后,2组DOSS评分、PAS评分、FOIS分级均优于治疗前,且联合组DOSS评分、PAS评分、FOIS分级均优于对照组,差异均有统计学意义(均P<0.001,表2~4)。联合组治疗前FOIS分级1级3例,2级11例;治疗后FOIS分级2级2例,5级8例,6级4例,有效率85.7%(12/14);对照组治疗前FOIS分级1级4例,2级11例;治疗后FOIS分级2级5例,3级4例,4级6例,有效率66.7%(10/15);2组有效率比较差异无统计学意义(χ2=9.323,P=0.389)。联合组和对照组均无不良反应发生。
表2.
2组患者治疗前后DOSS评分比较
Table 2 Comparison of DOSS between 2 groups before and after treatment
| 组别 | n | 治疗前 | 治疗2周后 | t | p |
|---|---|---|---|---|---|
| 联合组 | 14 | 1.77±0.44 | 5.23±0.73 | 14.23 | <0.001 |
| 对照组 | 15 | 1.79±0.43 | 3.93±0.62 | 15.00 | <0.001 |
| t | 0.099 | 5.043 | |||
| P | 0.922 | <0.001 |
DOSS:吞咽障碍结局与严重度量表。
表4.
2组患者治疗前后FOIS分级比较
Table 4 Comparison of FOIS between 2 groups before and after treatment
| 组别 | n | 治疗前 | 治疗2周后 | t | P |
|---|---|---|---|---|---|
| 联合组 | 14 | 1.79±0.43 | 4.86±1.29 | 8.299 | <0.001 |
| 对照组 | 15 | 1.73±0.46 | 3.07±0.88 | 4.934 | <0.001 |
| t | 0.3184 | 4.382 | |||
| P | 0.7526 | <0.001 |
FOIS:功能性经口摄食量表。
表3.
2组患者治疗前后PAS评分比较
Table 3 Comparison of PAS between 2 groups before and after treatment
| 组别 | n | 治疗前 | 治疗2周后 | t | P |
|---|---|---|---|---|---|
| 联合组 | 14 | 5.50±0.94 | 3.43±0.64 | 6.109 | <0.001 |
| 对照组 | 15 | 5.67±0.62 | 4.53±0.52 | 6.859 | <0.001 |
| t | 0.568 | 5.104 | |||
| P | 0.575 | <0.001 |
PAS:渗漏/误吸量表。
3. 讨 论
环咽肌位于第6颈椎水平的咽和食管的交界处,是食管上括约肌的主要组成部分。环咽肌失迟缓是指环咽肌的紧张性收缩或不协调,在正常的吞咽过程中,环咽肌放松并张开以允许液体或食物通过,而其紧闭则由上食管括约肌静息压力维持[16]。环咽肌失迟缓病因和病理生理机制仍不十分清楚,神经源损伤(中枢神经系统和周围神经系统)、头颈部肿瘤或外伤、胃食管反流等疾病是其常见病因,脑干梗死是最常见的病因[17]。BTX-A是一种神经毒素,通过抑制突触前胆碱能神经末梢的乙酰胆碱释放来阻断神经肌肉传递,BTX-A注射已被证明可以治疗多种肌肉痉挛性疾病,如痉挛性斜颈、眼睑痉挛、面肌痉挛等[18]。本研究选取脑干梗死后环咽肌失迟缓患者,发病时间均>2个月,均留置胃管。研究结果显示:治疗2周后,2组DOSS评分、PAS评分、FOIS分级均优于治疗前,且联合组均优于对照组。由此表明环咽肌BTX-A注射联合球囊扩张较单独使用球囊扩张对改善吞咽功能效果更好,消化内镜引导相对B超或CT引导更直观,无放射性,创伤更小,具有一定的优势。
内镜注射的方法主要有纤维喉镜和消化内镜,在环咽肌背内侧和双侧腹侧选择2~4位点进行注射[5, 19]。最近关于环咽肌解剖的研究[20]显示环咽肌后外侧是BTX-A的最佳注射部位。由于BTX-A在每个注射位点渗透范围约2 cm,所以本研究在环咽肌双侧腹侧各选取1个位点进行注射。研究[21]报道BTX-A的注射剂量为10~100 U,浓度50~100 U/mL,较高的剂量可能会有更高的成功率及较长的持续时间,但也有增加咽喉肌无力的风险。注射BTX-A的不良反应主要有短暂性吞咽困难恶化、暂时性声带麻痹、颈部蜂窝织炎、注射部位疼痛和吸入性肺炎等[22]。本研究选取BTX-A的注射剂量为60 U,浓度为100 U/mL,未见不良反应发生,考虑与注射位点精准,同时采用100 U/mL相对高稀释度的溶液有关。研究[2]显示环咽肌BTX-A注射的平均有效率为76%(43%~100%),与患者选择、注射部位、注射剂量、注射技术等有关。Jeong等[19]采用消化内镜引导下注射14例吞咽障碍患者,有效率为78.6%。Kim等[20]采用喉镜引导下注射12例患者患者,有效率为80%。本研究有效率为85.7%,较文献报道有所提高,可能与联合球囊扩张治疗有关。研究[2]显示球囊扩张的平均有效率为81%(58%~100%),本研究有效率为66.7%,与对照组比较无明显差异,但治疗后联合组FIOS分级提高更多,提示联合组治疗效果更好。咽腔压力测试研究显示[12, 23]:环咽肌BTX-A注射可降低食管上括约肌静息压力,延长食管上括约肌松弛时间,有利于吞咽功能恢复。BTX-A注射的疗效一般可持续3~6个月,也可持续1年或更久[21]。本研究的疗效尚需要进一步随访观察。
本研究在国内首次报道消化内镜引导下环咽肌BTX-A注射治疗脑卒中后环咽肌失迟缓的对照研究,结果提示:消化内镜引导下BTX-A注射联合球囊扩张是治疗脑干梗死后环咽肌失弛缓所致吞咽困难的有效措施之一,值得临床推广应用。
基金资助
湖南省自然科学基金(2021JJ70057);湖南省临床医疗技术创新引导项目(2020SK53005)。
This work was supported by the Natural Science Foundation of Hunan Province (2021JJ70057) and the Clinical Medical Technology Innovation Guidance Project of Hunan Province (2020SK53005), China.
利益冲突声明
作者声称无任何利益冲突。
作者贡献
刘超 研究设计,论文撰写与修改;李元、谭智、刘华 数据分析;周美云、李洁、梁俊俊 数据采集;肖乐 研究设计,论文指导及修改。所有作者阅读并同意最终的文本。
原文网址
http://xbyxb.csu.edu.cn/xbwk/fileup/PDF/2023081203.pdf
参考文献
- 1. Meng NH, Wang TG, Lien IN. Dysphagia in patients with brainstem stroke: incidence and outcome[J]. Am J Phys Med Rehabil, 2000, 79(2): 170-175. 10.1097/00002060-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 2. Kocdor P, Siegel ER, Tulunay-Ugur OE. Cricopharyngeal dysfunction: a systematic review comparing outcomes of dilatation, botulinum toxin injection, and myotomy[J]. Laryngoscope, 2016, 126(1): 135-141. 10.1002/lary.25447. [DOI] [PubMed] [Google Scholar]
- 3. Schneider I, Pototschnig C, Thumfart WF, et al. Treatment of dysfunction of the cricopharyngeal muscle with botulinum a toxin: introduction of a new, noninvasive method[J]. Ann Otol Rhinol Laryngol, 1994, 103(1): 31-35. 10.1177/000348949410300105. [DOI] [PubMed] [Google Scholar]
- 4. Wang YC, Shyu SG, Wu CH, et al. Ultrasound-guided injection of botulinum toxin for cricopharyngeal dysphagia[J/OL]. Am J Phys Med Rehabil, 2018, 97(10): e102-e103[2023-05-10]. 10.1097/phm.0000000000000959. [DOI] [PubMed] [Google Scholar]
- 5. Sharma S, Kumar G, Eweiss A, et al. Endoscopic-guided injection of botulinum toxin into the cricopharyngeus muscle: our experience[J]. J Laryngol Otol, 2015, 129: 990-995. 10.1017/S0022215115002327. [DOI] [PubMed] [Google Scholar]
- 6. Huai J, Hou Y, Guan JW, et al. Botulinum toxin A injection using esophageal balloon radiography combined with CT guidance for the treatment of cricopharyngeal dysphagia[J]. Dysphagia, 2020, 35(4): 630-635. 10.1007/s00455-019-10070-5. [DOI] [PubMed] [Google Scholar]
- 7. Wajsberg B, Hoesli RC, Wingo ML, et al. Efficacy and safety of electromyography-guided injection of botulinum toxin to treat retrograde cricopharyngeus dysfunction[J/OL]. OTO Open, 2021, 5(1): 2473974X21989587[2023-05-18]. 10.1177/2473974X21989587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. 王利春, 黄凤慧, 苗维, 等. CT引导下肉毒毒素环咽肌注射治疗真性延髓麻痹所致吞咽障碍1例报道[J]. 中国康复理论与实践, 2019, 25(4): 477-480. [Google Scholar]; WANG Lichun, HUANG Fenghui, MIAO Wei, et al. CT-guided botulinum toxin injection into cricopharyngeus for dysphagia after true bulbar palsy: a case report[J]. Chinese Journal of Rehabilitation Theory and Practice, 2019, 25(4): 477-480. [Google Scholar]
- 9. Luan S, Wu SL, Xiao LJ, et al. Comparison studies of ultrasound-guided botulinum toxin injection and balloon catheter dilatation in the treatment of neurogenic cricopharyngeal muscle dysfunction[J]. NeuroRehabilitation, 2021, 49(4): 629-639. 10.3233/nre-210113. [DOI] [PubMed] [Google Scholar]
- 10. Zhu LL, Chen JJ, Shao XZ, et al. Botulinum toxin A injection using ultrasound combined with balloon guidance for the treatment of cricopharyngeal dysphagia: analysis of 21 cases[J]. Scand J Gastroenterol, 2022, 57(7): 884-890. 10.1080/00365521.2022.2041716. [DOI] [PubMed] [Google Scholar]
- 11. 杨瑛, 许梅娜, 李相良, 等. 超声引导下肉毒毒素环咽肌注射治疗延髓背外侧综合征所致吞咽障碍1例报道[J]. 中国康复理论与实践, 2020, 26(11): 1358-1364. 10.3969/j.issn.1006-9771.2020.11.020. 32249491 [DOI] [Google Scholar]; YANG Ying, XU Meina, LI Xiangliang, et al. Cricopharyngeal botulinum toxin injection under ultrasonic guidance for dysphagia from Wallenberg’s syndrome: a case report[J]. Chinese Journal of Rehabilitation Theory and Practice, 2020, 26(11): 1358-1364. 10.3969/j.issn.1006-9771.2020.11.020. [DOI] [Google Scholar]
- 12. 温红梅, 万桂芳, 唐志明, 等. 超声、球囊联合肌电引导注射肉毒毒素治疗脑卒中后环咽肌失弛缓: 1例报告[J]. 中国康复医学杂志, 2019, 34(9): 1088-1091. 10.3969/j.issn.1001-1242.2019.09.021. [DOI] [Google Scholar]; WEN Hongmei, WAN Guifang, TANG Zhiming, et al. Ultrasound, balloon and electromyography-guided injection of botulinum toxin in the treatment of post-stroke cricopharyngeal achalasia: a case report[J]. Chinese Journal of Rehabilitation Medicine, 2019, 34(9): 1088-1091. 10.3969/j.issn.1001-1242.2019.09.021. [DOI] [Google Scholar]
- 13. Borders JC, Brates D. Use of the penetration-aspiration scale in dysphagia research: a systematic review[J]. Dysphagia, 2020, 35(4): 583-597. 10.1007/s00455-019-10064-3. [DOI] [PubMed] [Google Scholar]
- 14. 楼伟伟, 窦祖林. 吞咽障碍结局与严重度量表[J]. 神经损伤与功能重建, 2007, 2(1): 63-64. 10.3870/j.issn.1001-117X.2007.01.023. [DOI] [Google Scholar]; LOU Weiwei, DOU Zulin. Scale of outcome and severity of dysphagia[J]. Neural Injury and Functional Reconstruction, 2007, 2(1): 63-64. 10.3870/j.issn.1001-117X.2007.01.023. [DOI] [Google Scholar]
- 15. Zhou H, Zhu Y, Zhang X. Validation of the Chinese version of the functional oral intake scale (fois) score in the assessment of acute stroke patients with dysphagia [J]. Stud Health Technol Inform, 2017, 245: 1195-1199. [PubMed] [Google Scholar]
- 16. Panebianco M, Marchese-Ragona R, Masiero S, et al. Dysphagia in neurological diseases: a literature review[J]. Neurol Sci, 2020, 41(11): 3067-3073. 10.1007/s10072-020-04495-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yang H, Yi YB, Han Y, et al. Characteristics of cricopharyngeal dysphagia after ischemic stroke[J]. Ann Rehabil Med, 2018, 42(2): 204-212. 10.5535/arm.2018.42.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chiu SY, Burns MR, Malaty IA. An update on botulinum toxin in neurology[J]. Neurol Clin, 2021, 39(1): 209-229. 10.1016/j.ncl.2020.09.014. [DOI] [PubMed] [Google Scholar]
- 19. Jeong SH, Kim YJ, Kim YJ, et al. Endoscopic botulinum toxin injection for treatment of pharyngeal dysphagia in patients with cricopharyngeal dysfunction[J]. Scand J Gastroenterol, 2018, 53(10/11): 1201-1205. 10.1080/00365521.2018.1506820. [DOI] [PubMed] [Google Scholar]
- 20. Kim BH, Kim DH, Lee JH, et al. Evaluating intramuscular neural distribution in the cricopharyngeus muscle for injecting botulinum toxin[J]. Auris Nasus Larynx, 2023, 50(1): 87-93. 10.1016/j.anl.2022.05.004. [DOI] [PubMed] [Google Scholar]
- 21. 张祎辰, 高正玉, 王强, 等. 环咽肌失弛缓症的A型肉毒毒素注射研究进展[J]. 中华物理医学与康复杂志, 2020, 42(2): 189-192. 10.3760/cma.j.issn.0254-1424.2020.02.024. [DOI] [Google Scholar]; ZHANG Yichen, GAO Zhengyu, WANG Qiang, et al. Research progress on injection of botulinum toxin A in cricopharyngeal achalasia[J]. Chinese Journal of Physical Medicine and Rehabilitation, 2020, 42(2): 189-192. 10.3760/cma.j.issn.0254-1424.2020.02.024. [DOI] [Google Scholar]
- 22. Alfonsi E, Merlo IM, Ponzio M, et al. An electrophysiological approach to the diagnosis of neurogenic dysphagia: implications for botulinum toxin treatment[J]. J Neurol Neurosurg Psychiatry, 2010, 81(1): 54-60. 10.1136/jnnp.2009.174698. [DOI] [PubMed] [Google Scholar]
- 23. Xie MS, Zeng PS, Wan GF, et al. The effect of combined guidance of botulinum toxin injection with ultrasound, catheter balloon, and electromyography on neurogenic cricopharyngeal dysfunction: a prospective study[J]. Dysphagia, 2022, 37(3): 601-611. 10.1007/s00455-021-10310-7. [DOI] [PubMed] [Google Scholar]