Abstract
Neurological diseases and neurotrauma manifest significant sex differences in prevalence, progression, outcome, and therapeutic responses. Genetic predisposition, sex hormones, inflammation, and environmental exposures are among many physiological and pathological factors that impact the sex disparity in neurological diseases. MicroRNAs (miRNAs) are a powerful class of gene expression regulator that are extensively involved in mediating biological pathways. Emerging evidence demonstrates that miRNAs play a crucial role in the sex dimorphism observed in various human diseases, including neurological diseases. Understanding the sex differences in miRNA expression and response is believed to have important implications for assessing the risk of neurological disease, defining therapeutic intervention strategies, and advancing both basic research and clinical investigations. However, there is limited research exploring the extent to which miRNAs contribute to the sex disparities observed in various neurological diseases. Here, we review the current state of knowledge related to the sexual dimorphism in miRNAs in neurological diseases and neurotrauma research. We also discuss how sex chromosomes may contribute to the miRNA sexual dimorphism phenomenon. We attempt to emphasize the significance of sexual dimorphism in miRNA biology in human diseases and to advocate a gender/sex-balanced science.
Keywords: sex biased, microRNA, neurodegenerative diseases, traumatic brain injury, X chromosome, miR-223-3p
1. Introduction
There are substantial neurobiological differences between males and females during development, adulthood, and senescence [1,2,3,4,5,6,7,8,9,10]. As such, it is predictable that numerous neurological and age-related diseases have distinct prevalence, progression, and therapeutic responses between genders. For instance, women have a significantly increased risk of developing Alzheimer’s disease (AD) relative to men [11,12,13,14]. According to Alzheimer’s Disease Facts and Figures from the Alzheimer’s Association (https://www.alz.org/media/Documents/alzheimers-facts-and-figures.pdf (accessed on 20 February 2024)), almost two-thirds of Americans living with AD are women. Additionally, the prevalence of multiple sclerosis (MS) is four times higher in women compared to men [15,16]. By contrast, there is a significantly (~1.5×) higher incidence among men for Parkinson’s disease (PD) [17]. Amyotrophic lateral sclerosis (ALS) represents another sexual dimorphic neurodegenerative disease, with the incidence among men being three times higher than among women, and men typically experience an earlier onset of the disease [18,19]. Neuropsychiatric disorders also exhibit substantial sex bias in prevalence, symptoms, and age of onset [20]. For example, men have a higher prevalence of schizophrenia, hyperactivity disorder, and autistic spectrum, and women have a higher prevalence of anxiety disorders and depression [21].
The pathogenesis of neurological diseases is associated with multifactorial contributing factors, including genetic predisposition, inflammation, and environmental exposures. Sex differences in neurological diseases may be associated with any or all of these influences. Research indicates that while the increased risk of developing AD associated with the APOE E4 allele is generally assumed to be equal in men and women, this risk is actually stronger in women [22,23]. In a Korean genome-wide study on PD, the risk variants SNCA and PARK16 exhibited sex-specific patterns: SNCA locus single nucleotide polymorphisms (SNPs) predominated in females, whereas PARK16 locus SNPs were greater in males [24].
Sex is not only associated with different disease epidemiology but also impacts outcomes and responses to treatment. For example, following a stroke, women experience worse outcomes and undergo more functional decline than men [25,26]. Huntington’s disease (HD), which is highly genetically determined with limited therapeutic options [27], has a higher incidence and faster progression in women compared to men [28,29,30]. Moreover, sexually dimorphic responses to environmental modulators are also noted in HD [27,29]. Traumatic brain injury (TBI) represents another neurological condition where sex differences impact the outcomes, responses to treatment, and recovery. According to the Centers for Disease Control and Prevention (CDC), men are two-times more likely to be hospitalized and three-times more to die due to TBI, yet women were more vulnerable than men to show persisting TBI-related cognitive and somatic symptoms [31,32,33,34]. Moreover, a longer time to symptom resolution was reported in high school and collegiate female athletes [35,36,37,38].
Although a myriad of sex-specific genes and pathways have been identified, the mechanisms underlying the sexual dimorphism in diseases and pathological conditions are quite incompletely understood. As a class of powerful biological regulators in all known metazoan and plant species, microRNAs (miRNAs) have emerged as an important regulator of sexually dimorphic responses. However, few studies have examined the extent to which miRNAs contribute to the sex-biased differences observed in various neurological diseases. Here, we review the current state of knowledge related to miRNA sexual dimorphism in neurological diseases and neurotrauma research. We also discuss how sex chromosomes may contribute to the miRNA sexual dimorphism phenomenon. With this review, our goal is to emphasize the significance of sexual dimorphism in miRNA biology in human diseases and to enrich the framework for upcoming studies.
2. Overview of microRNAs
MiRNAs are short non-coding RNAs (19–25 nt) that regulate protein translation, usually by inhibiting translation or destabilizing the messenger RNA (mRNA) of a targeted gene. Since the discovery of first miRNA in Caenorhabditis elegans [39,40], phylogenetically conserved miRNAs have been characterized across many animals and plants, and the key roles of miRNAs in gene regulation are well recognized. It is estimated that at least 60% of human coding genes are regulated by miRNAs [41]. MiRNAs regulate diverse biological processes such as development, cell differentiation, proliferation, apoptosis, neurodevelopment, senescence, and immunity, and are an integral regulatory component of biological and pathological systems [42,43,44,45,46,47,48,49,50,51].
The biogenesis of miRNA involves complex processes with a stereotypical pathway that flows through multiple protein complexes [44,52]. MiRNAs are typically transcribed as primary miRNA transcripts (Pri-miRNAs) from either the introns of their host genes or standalone miRNA genes by RNA polymerase II. Pri-miRNA is further processed in the nucleus by the Drosha/DGCR8 protein complex to a 70 bp stem-loop precursor-miRNA (pre-miRNA) [44,53,54]. Pre-miRNAs are then exported to the cytoplasm by the cotransporter Exportin 5 and then further cleaved by Dicer into small double-stranded RNA in the cytoplasm [44,55,56,57]. One of the two double strands determined to be the “guide strand” is then loaded into the Argonaute (AGO)-containing RNA-induced silencing complex (RISC) [58,59], while the other strand (passenger strand) is degraded. The AGO-containing miRNA RISC complex is the effector unit of miRNA regulation, in which different members of the AGO paralogs execute overlapping and distinct actions during gene suppression [60]. For example, AGO1 mediates alternative splicing via interaction with cell-type-specific transcriptional enhancers [61]. AGO2- and AGO3-RISC complexes possess a ‘slicer’ function that may directly lead to mRNA degradation [60,62,63].
The complex processes of miRNA biogenesis and function, and the genes/proteins involved are also subject to a spectrum of regulatory mechanisms, which include transcription regulation, developmental staging, pathological stimuli, and sex hormones [64,65,66]. In terms of the widespread regulation of miRNAs by sex hormones, which is not the main focus of the current review, we recommend several excellent early review articles [67,68,69,70].
Some miRNA-related processing mechanisms are sexually dimorphic. For example, AGO4 localized in mammalian germ cells plays a key role in regulating meiotic sex chromosome inactivation [71]. Deficiency of AGO4 in germ cells caused a significant reduction in miRNAs, in which over a 20% loss of miRNAs were X chromosome-linked miRNAs (X-linked miRNAs) [71]. Additionally, miRNAs are differentially expressed in males and females across cells, tissues, organs, and extracellular circulation, and are associated with sex-biased biological and pathological processes [72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98]. However, the mechanisms for the sexually dimorphic expression of miRNAs and their biological impact in both normal and pathological events are largely unexplored [67].
3. Sex-Biased miRNAs in Neurodegenerative Diseases and Neuropsychiatric Disorders
Differential expressions and regulation of protein-coding genes by miRNAs between males and females may represent the key mechanisms underlying the sex-biased prevalence, pathogenesis, response to therapy, and outcomes of human diseases. As an important class of gene expression regulators, miRNAs play critical roles in neuronal development, differentiation, and brain morphogenesis [49,99,100]. This implies that their sexually dimorphic expression might influence the risk of neurological diseases from early development stages. A study revealed that the expression of the miR-200 family of miRNAs (miR-141-3p, miR200a-3P, miR200b-3P, and miR-429) as well as miR-875 showed a sex-specific switch in the developing rat brain [85]. At postnatal day 0 (P0), these miRNAs were elevated in females; at P7 and the adult stage, all these miRNAs were elevated in male brains (Table 1). Additionally, miRNA may influence response to early life events, such as environmental stresses, which may impact the development of neurological disease later in life.
Table 1.
Sex-biased miRNAs in neurological diseases.
| miRNAs | Species/Tissue | Disease/Condition | X-Linked Yes/No | Observation | Reference | |
|---|---|---|---|---|---|---|
| Pre-clinical studies | miR-200 family (miR-141-3p, miR200a-3P, miR200b-3P, and miR-429), miR-875 | Rat/cortex | P0/development | No | Upregulated in females | [85] |
| miR-200 family (miR-141-3p, miR200a-3P, miR200b-3P, and miR-429), miR-875 | Rat/cortex | P7, adult/development | No | Upregulated in males | [85] | |
| miR-935 | Rat/cortex | P0, P7, adult | Upregulated in males | [85] | ||
| miR-322, miR-574, and miR-873 | Mouse/brain | Prenatal stress | No | Downregulated in males | [80] | |
| Let-7g, miR-1944 | Mouse/cerebral vessels | 3xTg-AD, young to CI | No | Downregulated in males | [86] | |
| miR-133a, miR-2140 | Mouse/cerebral vessels | 3xTg-AD, young to CI | No | Downregulated in females | [86] | |
| miR-99a | Mouse/cerebral vessels | 3xTg-AD, CI to Aβ | No | Downregulated in males | [86] | |
| let-7d, let-7i, miR-23a, miR-34b-3p, miR-99a, miR-126-3p, miR-132, miR-150, miR-151-5p, miR-181a | Mouse/cerebral vessels | 3xTg-AD, pre-AD to AD | No | Changed in males | [86] | |
| miR-150, miR-539 | Mouse/cerebral vessels | 3xTg-AD, pre-AD to AD | No | Changed in females | [86] | |
| miR-137, miR-181c, miR-29a, miR29b-1 | Mouse/brain | C57/BL | No | Downregulated in females | [88] | |
| miR-137, miR-181c, miR29b-1 | Mouse/serum | High-fat diet/C57/BL | No | Downregulated in females | [87] | |
| miR-320 | Mouse/hippocampus | Sepsis/old mice | No | Changed in females not males | [89] | |
| miR-223-3p, miR-98-3p, and miR-662-5p | Mouse/hippocampus | Sepsis/old mice | Yes | Upregulated in males | [89] | |
| miR-23a | Mouse/brain | Cerebral ischemia | No | Upregulated in females | [75] | |
| miR-509-3p | Mouse/cortices | Cerebral ischemia | No | Upregulated in males downregulated in females | [90] | |
| miR-883b-3p | Mouse/cortices | Cerebral ischemia | No | Upregulated in females downregulated in males | [90] | |
| miR-142a-5p and 25 others | Mouse/microglia | B6C3F1/J/naive | Yes to some | Enriched in females | [91] | |
| miR-1298-5p and 60 others | Mouse/microglia | B6C3F1/J/naive | Yes to some | Enriched in males | [91] | |
| miR-150-5p, miR-155-5p | Mouse/CD11b+ | C57BL/6J/naïve | No | Upregulated in males | [98] | |
| miR-150-5p, miR-155-5p, miR-146a-5p, miR-223-3p | Mouse/CD11b+ | C57BL/6J/TBI | No, except miR-223-3p | Sex-specific response at different time points following TBI | [98] | |
| miR-29a, miR-29c | Mouse/brain | Radiation-induced brain injury | No | Upregulated in female | [72] | |
| Clinical studies | miR-206, miR-133a, miR-133b, miR-27a, miR-155, miR-146a, miR-221 | Human/muscle | ALS | No, except miR-222 | Upregulated in males | [92] |
| miR-146a, miR-34a-5p | Human/serum | PD | No | Upregulated in men | [93] | |
| miR-29a, miR-29b, miR-29c | Human/serum | PD | No | Downregulated in men | [94] | |
| miR-206 | Human/plasma | FTD | No | Downregulated in men | [95] | |
| miR-30b | Human/cortices | Schizophrenia | No | Downregulated in females | [96] | |
| miR-548am-5p | Human/primary dermal fibroblasts | XCI escape | Yes | Upregulated in females | [97] |
Sex-biased miRNA expression at different stages of development may lead to gender-specific changes in the onset, progression, and outcome of a neurological disease, especially neuropsychiatric disorders [101]. Prenatal environmental stresses (e.g., maternal stress, diet, and endocrine disruption) can have a major impact on brain development and contribute to the development of neuropsychiatric disorders, such as depression, schizophrenia, and autistic spectrum disorders [102,103,104,105]. These adverse effects are often sex-biased and can persist into subsequent generations [106,107,108,109]. Epigenetic mechanisms [110,111,112,113] and miRNA dysregulation [79,80], among others, were suggested to be associated with these phenomena. It was shown that early gestation is a perinatal period when organizational gonadal hormones establish the sexually dimorphic brain and are most susceptible to maternal stress [80,114]. In a mouse model of demasculinization, a study showed the paternal transmission and programming of the prenatal stress-induced demasculinized phenotype in second-generation (F2) male offspring [80]. The miRNA analysis using the brains of these male offspring 1 day after birth revealed a significant reduction in miR-322, miR-574, and miR-873, with levels similar to those of control female brains. The reduction in these miRNAs was correlated with the significant increase in β-glycan, a common target of all three miRNAs. β-glycan is a member of the TGFβ superfamily and it may be involved in regulating the release of gonadal hormones [80]. Another study showed that estrogen-sensitive miR-30b was found to be significantly reduced in the cerebral cortex of female but not male subjects with schizophrenia [96]. This sex-biased miRNA expression appeared to be regulated by estrogen and estrogen receptor signaling.
MiRNAs directly regulate key molecules in the pathogenesis of various neurological diseases, and numerous dysregulated miRNAs have been characterized [115,116,117,118,119,120]. Unfortunately, few studies have considered sex as a biological factor, leaving the role of sex-biased miRNAs in neurological diseases and neurotrauma largely undefined.
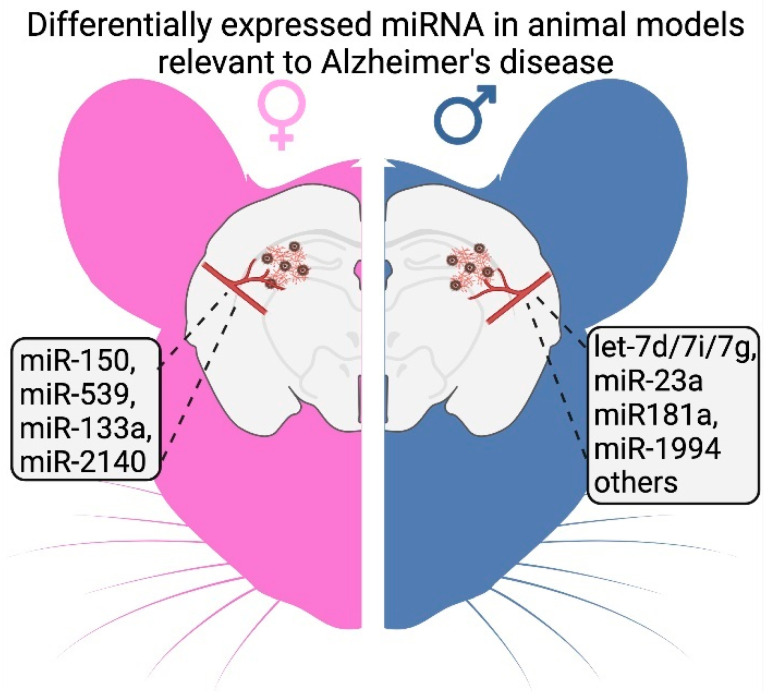
Certain trends have been identified among the limited studies report sex-specific miRNA expression in injured and diseased brains (Table 1). For instance, in a tau pathology mouse model (PS19), miRNAs were considerably more altered in males compared to females [91]. Another study completed by Chum et al. investigated 599 miRNAs in brain vessels extracted from male and female 3xTg-AD mice [86]. The study revealed extensive alterations in miRNA profiles associated with age and AD pathology. Notably, several miRNAs were significantly differentially expressed between male and female mice at various stages of AD-type pathology progression in this mouse model (Figure 1).
Figure 1.
Example of sex-dependent miRNA expression in the 3xTg-AD mouse model. Chum et al. [86] analysis of 599 miRNAs in 3xTg-AD mice brain and cerebral vessels, showing sex-specific expression changes with age and degree of pathological progression.
Several miRNAs (miR-137, miR-181c, miR-9, miR-29a, and miR-29b-1) have been found to participate in the ceramide biosynthesis pathway, regulating rate-limiting enzyme serine palmitoyltransferase (SPT) in the brain [88]. Increased levels of ceramide have been associated with AD and other neurodegenerative diseases [121,122]. It was revealed that expressions of miR-137, miR-181c, miR-29a, and miR-29b-1 (but not miR-9) were downregulated, while SPTLC1/2 (SPT long chain 1/2) protein expression levels increased in female mice [88]. Furthermore, miR-137, miR-181c, and miR-29b-1 were downregulated in the serum of female mice relative to male mice [87]. Nevertheless, whether these miRNAs show sexually dimorphic expression in the human brain is currently unknown.
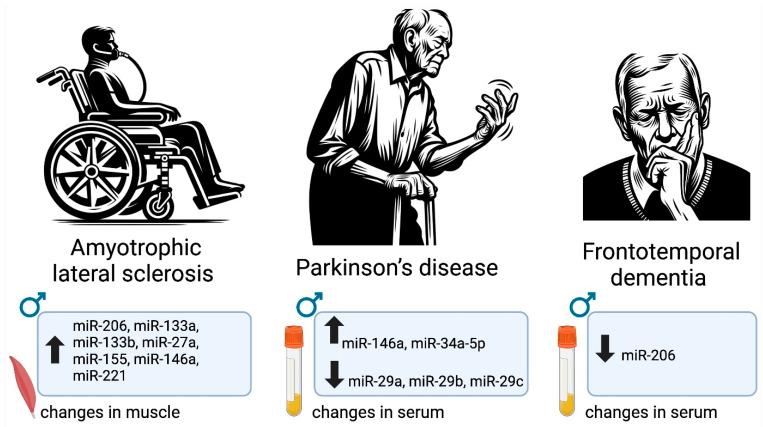
There are multiple relevant human studies defining sexually dimorphic changes in miRNAs in people with ALS, PD, and frontotemporal dementia (FTD) (Figure 2). In ALS, a set of miRNAs (miR 206, miR-133a, miR133b, miR27a, miR-155, miR-146a, and miR-221) were significantly more upregulated in males compared to females [92]. The levels of several miRNAs also exhibited gender biases in PD [93]. Specifically, miRNA-34a-5p and miR-146a-5p were significantly upregulated in men compared to women. Interestingly, these expression patterns were observed in PD patients who were never treated with levodopa [93]. Another study conducted in PD patients indicated downregulation of the miR-29 family (miR-29a, miR-29b, miR-29c) in the serum of PD patients compared to controls, and these levels were significantly more downregulated in males compared to females [94]. In a separate study involving circulating miRNAs in humans, it was observed that plasma miR-663a, miR-502-3p, and miR-206 were significantly reduced in FTD patients compared to healthy controls [95]. However, when analyzed by sex, miR-206 was only found to be significantly downregulated in male patients, while its levels in females remained comparable to healthy controls. The same study revealed that there was a significant difference in Let-7e-5p levels when comparing female FTD patients with healthy controls, and no difference was found in males or in the overall population. In an attempt to discriminate FTD from other neurodegenerative diseases, an additional plasma miRNA biomarker, miR-127-3p, was proposed [123]. Plasma miR-127-3p was able to help distinguish FTD from healthy controls and AD patients; however, no difference between males and females was detected.
Figure 2.
Sex-specific miRNA changes reported in men with ALS, PD, and FTD. In ALS, a specific set of miRNAs including miR-206 and miR-146a exhibited higher upregulation in males [92], while in PD, miRNAs like miR-34a-5p showed a similar male bias [93]. Conversely, in FTD, certain miRNAs such as miR-206 were significantly downregulated only in males [95].
Neurodegenerative disease and cognitive impairment are hypothesized to have cross-talk with neuroinflammation. For example, sepsis can induce severe and long-term cognitive deficits affecting memory, attention, verbal fluency, and executive function [124,125], and results in worse outcomes in older AD and AD-related dementia (AD/ADRD) patients [126]. Sex-biased miRNA expression patterns were reported in the hippocampus of a sepsis mouse model [89]. While miR-320 was downregulated in female old mice (24 months) on day 1 and increased on day 4 following treatment, no change was reported in males. Interestingly, X-linked miRNAs responded differentially in male and female brains. Particularly, miR-222-3p, miR-221-3p, and miR-652-3p were downregulated in both young and aged females 1 day following treatment. By contrast, three different X-linked miRNAs, miR-223-3p, miR-98-3p, and miR-662-5p, were upregulated in older males.
4. Sex-Biased miRNAs in Cerebral Vascular Diseases
The prevalence, symptoms, treatment responses, and outcomes of strokes are known to have strong sex-bias [127,128]. MiRNA regulation has been demonstrated to make contribution to the sex differences in response to stroke. In a study of sex-biased vulnerability to cerebral ischemia [75], it was found that miR-23a targets an X-linked inhibitor of apoptosis (XIAP). XIAP, encoded on the X chromosome, is a member of the potent endogenous human inhibitor of apoptosis (IAP) family [129]. XIAP was shown to contribute to the sex difference following cerebral ischemia, where it was reduced significantly in females post-ischemia [75]. Concomitantly, miR-23a was significantly increased in the female brain in response to cerebral ischemia. Thus, it was suggested that enhanced miR-23a expression is likely to be responsible for the decreased XIAP in females [75]. Sex-biased miRNA expression was reported in another cerebral ischemia study [90]. The study found that many miRNAs were induced following ischemia in the cortices of both male and female mice. However, several miRNAs exhibited sex differences in the degree of changes as well as the direction of changes. For example, miR-509-3p levels were increased in males and decreased in females, and miR-883b-3p levels were decreased in males and elevated in females [90]. Florijn et al. have shown that several X-linked and estrogen-regulated miRNAs were expressed in the neurovascular unit and may play a role in sex-specific responses to ischemic stroke [130]. However, it remains speculative as to whether these miRNAs exhibit a sexually dimorphic response to ischemic stroke, and these issues will need to be further examined.
5. Sex-Biased miRNAs in Traumatic Brain Injury (TBI)
TBI is defined as any external impact that results in brain function alteration [131]. TBI is a major cause of death and disability [132]. According to the CDC, about 190 Americans died from TBI-related injury each day in 2021. For those who survive the immediate primary injury, there may be a secondary injury (which may take days or months) consisting of complex molecular and biochemical responses [133,134,135,136,137]. Moreover, there is a clear association between a history of TBI and an increased risk of developing neurodegenerative diseases, including AD, later in life [138,139,140,141,142,143,144], suggesting there may have overlapping pathophysiological pathways between TBI and neurodegenerative diseases [145,146,147].
Numerous studies suggest a sexual dimorphism in TBI responses (see details in review by Gupte et al., 2019). Men are three-times more likely than women to die from TBI, and women often have worse symptom burdens and take longer time to recovery [31,32,33,34,35,36,37]. Multiple factors impact the outcome measurement of a TBI. For example, when studying gender difference, the injury severities and the circumstances of brain injury—whether civilians injured in a motor vehicle accident, military personnel experienced blast-induced TBI, or athletes developed chronic traumatic encephalopathy following repeated head injury—are the primary factors in the outcome of TBI. Other biological factors (age, sex hormones, injury characteristics, etc.) and extrinsic factors (size of a study cohort, clinical or physiological markers used in the study, social and behavioral elements) can all contribute to the sex-biased outcomes following TBI. Although it remains debated [32,148,149,150,151], human studies often report worse experiences (recovery, cognitive function, overall quality of life) in women following TBI [31,32,33,34,150,152]. Nevertheless, recent reports in sport-related concussion (SRC) found no differences overall in return-to-play time between male and female collegiate athletes [149], although females in contact and males in limited-contact sports experienced longer times in recovery [149]. In contrast, animal studies often present a different narrative in that better outcomes were reported more in female animals [153,154,155,156]. These mixed observations further underscore the importance of identifying sex/gender interacting cofounders in a given study, and translating animal data to human clinical studies should be performed with caution.
MiRNAs are widely altered following TBI and are involved in various pathophysiological processes, such as neuroinflammation in the injured brains [157,158,159,160]. Clinical studies using extracellular biofluids have suggested that miRNAs are abundantly present in biofluids and may serve as biomarkers for diagnosis, prognosis, and distinguishing TBI subtypes (e.g., mild vs. severe) [161,162,163,164,165,166,167]. For example, extracellular vesicle miRNAs are differentially associated with TBI history in military personnel [161]. Interestingly, the altered miRNAs in biofluids were found to be commonly implicated in neuroinflammation, apoptosis, vascular remodeling, BBB integrity, and cellular repair pathways [161,162,163,164,165,166,167]. Despite the sex-biased nature of TBI response, past studies, especially experimental TBI and TBI-related clinical trials, have been largely focused on male animals and men [32,168,169,170,171], whereas only limited prior studies have reported on miRNA sex-related differences in TBI. Some studies have reported no difference in miRNA expression profiles between males and females [158]. Nevertheless, it is encouraging that gender/sex has now been integrated as a biological variable in many recent TBI-related miRNA clinical studies [31,32,33,34,35,36,37,38,148,149,150,151,152].
Studies by Kodama et al. have shown that miRNAs were expressed differently by sex, which influences function in mouse microglia, the major immune cells in the brain; furthermore, these differences were more pronounced in aging brains [91]. Sex-specific alterations were recently reported in several inflammatory miRNAs in brain CD11b+ cells isolated from naïve and TBI mice [98]. Among the tested inflammatory miRNAs (miR-146-5p, miR-150-5p, miR-155-5p, and miR-223-3p), higher levels of miR-150-5p and miR-155-5p were observed in male brain CD11b+ cells isolated from naïve animals. Interestingly, the response of these inflammatory miRNAs to TBI was distinct. For example, miR-155-5p was elevated in the brain CD11b+ cells of both female and male mice, but female mice showed a greater induction at an early time point (3 h) compared to male mice following TBI. On the other hand, miR-150-5p levels only increased in female mice and at more chronic time points of 7 and 14 days following TBI. Despite no significant sex-biased expression having been demonstrated with miR-146a-5p and miR-223-3p in CD11b+ cells isolated from naïve mice, these miRNAs also exhibited sex-biased responses following TBI. Late increased levels of miR-146a-5p were demonstrated in females relative to male CD11b+ cells following TBI. The levels of X-linked, anti-inflammatory miR-223-3p were markedly elevated in the brain CD11b+ cells of both sexes at 3 and 24 h following TBI, with the levels in females being significantly higher than those males at 24 hr. Further analysis has demonstrated a corresponding greater reduction in miR-223-3p-validated targets TRAF6 and FBXW7 in female relative to male CD11b+ cells. These data suggest that miR-223-3p and other inflammatory-responsive miRNAs may play key roles in sex-specific neuroinflammatory response following TBI.
In an ionizing-radiation-induced brain injury mouse model, a study showed that miRNA changes were sex-biased, with larger changes observed in females than males [72]. Specifically, the miR-29 family members miR-29a and miR-29c were shown to be exclusively downregulated in female mice’s frontal cortices at 6 and 96 h post-exposure in response to ionizing radiation. The study further confirmed that the protein levels of a miR-29 target, DNA methyltransferase 3a (DNMT3a), were correspondingly upregulated. This suggests that in response to environmental cues and insults, sex-specific changes in miRNAs and their target proteins may undergo sex-dependent changes, influencing the degree of injury and outcome in males and females.
6. Impacts of X Chromosome-Linked miRNAs
Genetic background and hormonal profiles are markedly different in males and females, which significantly impacts the expression and function of miRNAs and their machinery [50,172,173,174]. The human X chromosome contains roughly 10-times more protein genes compared to the Y chromosome. Accordingly, the human X chromosome contains higher numbers of miRNAs compared to the Y chromosome and autosomes [175,176,177]. There are currently 118 annotated miRNA genes on the human X chromosome and 62 mature miRNAs have been confirmed with high confidence (source: miRBase version 22.1) [176,178]. It is predicted that the human Y chromosome contains only four miRNA genes. No miRNA is identified on mouse or rat Y chromosomes. For the readers convenience, we have compiled a full list of the currently annotated human, mouse, and rat X-linked miRNAs in Supplemental File S1 (source: miRbase version 22.1).
The difference in X chromosome gene dosage between females (two X chromosomes) and males (one X chromosome) is balanced by a mechanism known as X-chromosome inactivation (XCI) [179,180,181]: one copy of the two X chromosomes in females is randomly and permanently inactivated during early embryogenesis. Nevertheless, about 15–25% of human X-linked genes escape inactivation to some degree, which is linked to some diseases [182,183,184,185,186]. A number of miRNAs reside in the intronic regions of their host coding genes that are known to escape XCI. This suggests that the intronic miRNAs residing in XCI-escaped genes can potentially be reactivated [97,187]. However, very few examples of X-linked miRNA escape have been experimentally verified. Data analysis has revealed that miR-548am-5p might potentially escape XCI, and it was experimentally verified to express significantly higher levels in human primary dermal fibroblasts of females relative to males [97]. Remarkably, it has been shown that the immunity-related genes in the inactive X chromosome in female lymphocytes are susceptible to being partially reactivated, resulting in a higher level of immunity-related gene expression [188]. This raises the possibility that immune-related miRNAs (such as miR-223-3p) could escape XCI, especially upon altered physiological (e.g., development, aging) or pathological (e.g., cell injury, inflammation, infection) conditions [85,101,176,189,190,191].
The expression of male-biased miRNAs appears to preferentially enrich for X-linked miRNAs [83,192]. Ro et al. have reported that ~39% of testis-specific or testis-preferential miRNAs are X-linked miRNAs [193], suggesting a potential role of X-linked miRNAs in spermatogenesis [193,194,195]. Several studies have shown that many X-linked miRNAs escape meiotic sex chromosome inactivation (MSCI) and suggest that these escaped miRNAs may be specifically required during the meiotic stages of spermatogenesis in males [195,196,197,198]. However, recent work by Royo et al. has argued that X-linked miRNA expressions are highly stage-dependent during MSCI and that the observed ‘MSCI escaped’ X-linked miRNAs may be a result of long half-life of the miRNAs [194].
Dysregulation of X-linked miRNAs is also associated with a number of diseases and pathological conditions [77,199]. The X-linked miRNA, miR-223-3p, has been demonstrated to play critical roles in immunity, inflammation, and lipid metabolism in various disease conditions [200,201,202,203,204,205]. Although no sex-biased expression is reported under physiological conditions, it has been shown that miR-223-3p exhibits sex-specific alterations in mouse brain CD11b+ cells in response to TBI [98]. Many other X-chromosome-located miRNAs (including miR-18b, miR-19b, miR-20b, miR-106a, miR-221, miR-222, miR-424, and miR-503) have not been investigated in the context of sexual dimorphism but potentially could provide additional understanding in the mechanism of sex differences in disease phenotypes. It is noteworthy that two X-linked miRNAs, miR-424 and miR-503, are members of the miR-15/107 group [206], which has been implicated in regulating key proteins (BACE1, GRN) in neurodegenerative diseases [119,207,208]. However, these miRNAs have yet to be investigated for their roles in sex-biased diseases.
7. Conclusions and Perspectives
MiRNAs are critical gene mediators in development and post-development processes as no known multi-cellular organisms can sustain viability and functionality when missing essential miRNAs or miRNA machinery [49,209,210,211]. Moreover, mutations in miRNA genes or the miRNA target site of a gene often cause diseases [212,213,214,215,216,217,218,219]. However, the functional role of sex-biased miRNAs in neurological diseases and neurotrauma is underappreciated and understudied. Many questions remain unanswered. For example, in an aged brain where sex hormones have declined, what drives sex-biased miRNA expression? Which X-linked miRNAs escape XCI, and under what circumstances? Do human and experimental animal models express the same sex-biased miRNAs in the brain? If not, how can we better implement knowledge of animal sex-biased miRNAs in human studies?
Other important issues include considering sex-biased miRNA trafficking between peripheral tissues and the CNS. Neurological diseases are a diverse group of disorders associated with a variety of pathological and dysregulated physiological processes. Peripheral events, physiological or pathological, such as inflammation, diabetes, hypertension, microbiome, and endocrine disorders, can have significant impacts on the CNS. In this review, we mainly focused on the brain’s sex-biased miRNAs relevant to neurological disease. However, sex-biased expression and response miRNAs in peripheral tissues may also play an important role in the physiology and pathology of the brain, including immune response and inflammation. Although the brain possesses ‘immune privilege’ to prevent damage mediated by inflammation [220], it is now clear that there is a dynamic immune and inflammatory interaction between peripheral tissues and the brain, especially when the brain undergoes pathological changes or is under abnormal conditions [221]. Considering that neuroinflammation is a common component of neurological diseases, peripheral sex-biased inflammatory miRNA trafficking may be an important element dictating brain responses to inflammation. Accumulated evidence has demonstrated that miRNAs can be transported between brain and peripheral tissues via extracellular vesicles as well as other protein complexes that readily cross the blood–brain barrier and exert functional roles [222,223,224]. This evidence has also led to the novel development of using miRNAs as a biomarker and therapeutic strategy for neurological diseases [225,226].
Given the broad impacts of miRNAs in normal neuronal physiology and pathology, sex differences in miRNA functions have important implications for assessing the risk of neurological disease, defining therapeutic intervention strategies, as well as in basic research and clinical investigations. The relative paucity of extant sex-related miRNA studies and reports in biomedical research is a limitation of the field and should be addressed.
Acknowledgments
The figures in this article were created with BioRender.com (accessed on 26 January 2024).
Supplementary Materials
The supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms25052648/s1.
Author Contributions
Conceptualization, writing, review, and editing: W.-X.W. and U.G.; Critical review and editing: P.P., A.B. and P.T.N. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This work is funded by National Institute on Aging (R01AG082142, P01AG078116), and a grant from the Kentucky Spinal Cord and Head Injury Research Trust (KSCHIRT 23-15).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Shirokova O., Zaborskaya O., Pchelin P., Kozliaeva E., Pershin V., Mukhina I. Genetic and Epigenetic Sexual Dimorphism of Brain Cells during Aging. Brain Sci. 2023;13:195. doi: 10.3390/brainsci13020195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qureshi I.A., Mehler M.F. Genetic and epigenetic underpinnings of sex differences in the brain and in neurological and psychiatric disease susceptibility. Prog. Brain Res. 2010;186:77–95. doi: 10.1016/B978-0-444-53630-3.00006-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferri S.L., Abel T., Brodkin E.S. Sex Differences in Autism Spectrum Disorder: A Review. Curr. Psychiatry Rep. 2018;20:9. doi: 10.1007/s11920-018-0874-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.May T., Adesina I., McGillivray J., Rinehart N.J. Sex differences in neurodevelopmental disorders. Curr. Opin. Neurol. 2019;32:622–626. doi: 10.1097/WCO.0000000000000714. [DOI] [PubMed] [Google Scholar]
- 5.Cahill L. Why sex matters for neuroscience. Nat. Rev. Neurosci. 2006;7:477–484. doi: 10.1038/nrn1909. [DOI] [PubMed] [Google Scholar]
- 6.Ruigrok A.N., Salimi-Khorshidi G., Lai M.-C., Baron-Cohen S., Lombardo M.V., Tait R.J., Suckling J. A meta-analysis of sex differences in human brain structure. Neurosci. Biobehav. Rev. 2014;39:34–50. doi: 10.1016/j.neubiorev.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCarthy M.M. Sex differences in the developing brain as a source of inherent risk. Dialog. Clin. Neurosci. 2016;18:361–372. doi: 10.31887/DCNS.2016.18.4/mmccarthy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Vries G.J. Minireview: Sex Differences in Adult and Developing Brains: Compensation, Compensation, Compensation. Endocrinology. 2004;145:1063–1068. doi: 10.1210/en.2003-1504. [DOI] [PubMed] [Google Scholar]
- 9.Cosgrove K.P., Mazure C.M., Staley J.K. Evolving Knowledge of Sex Differences in Brain Structure, Function, and Chemistry. Biol. Psychiatry. 2007;62:847–855. doi: 10.1016/j.biopsych.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCarthy M.M., Arnold A.P., Ball G.F., Blaustein J.D., De Vries G.J. Sex differences in the brain: The not so inconvenient truth. J. Neurosci. 2012;32:2241–2247. doi: 10.1523/JNEUROSCI.5372-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niu H., Álvarez-Álvarez I., Guillén-Grima F., Aguinaga-Ontoso I. Prevalence and incidence of Alzheimer’s disease in Europe: A meta-analysis. Neurologia. 2017;32:523–532. doi: 10.1016/j.nrl.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 12.Chan K.Y., Wang W., Wu J.J., Liu L., Theodoratou E., Car J., Middleton L., Russ T.C., Deary I.J., Campbell H., et al. Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990–2010: A systematic review and analysis. Lancet. 2013;381:2016–2023. doi: 10.1016/S0140-6736(13)60221-4. [DOI] [PubMed] [Google Scholar]
- 13.Rajan K.B., Weuve J., Barnes L.L., McAninch E.A., Wilson R.S., Evans D.A. Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060) Alzheimer’s Dement. 2021;17:1966–1975. doi: 10.1002/alz.12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fisher D.W., Bennett D.A., Dong H. Sexual dimorphism in predisposition to Alzheimer’s disease. Neurobiol. Aging. 2018;70:308–324. doi: 10.1016/j.neurobiolaging.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahlgren C., Odén A., Lycke J. High nationwide prevalence of multiple sclerosis in Sweden. Mult. Scler. 2011;17:901–908. doi: 10.1177/1352458511403794. [DOI] [PubMed] [Google Scholar]
- 16.Compston A., Coles A. Multiple sclerosis. Lancet. 2002;359:1221–1231. doi: 10.1016/S0140-6736(02)08220-X. [DOI] [PubMed] [Google Scholar]
- 17.Wooten G.F., Currie L.J., Bovbjerg V.E., Lee J.K., Patrie J. Are men at greater risk for Parkinson’s disease than women? J. Neurol. Neurosurg. Psychiatry. 2004;75:637–639. doi: 10.1136/jnnp.2003.020982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCombe P.A., Henderson R.D. Effects of gender in amyotrophic lateral sclerosis. Gend. Med. 2010;7:557–570. doi: 10.1016/j.genm.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Kurtzke J.F. Epidemiology of amyotrophic lateral sclerosis. Adv. Neurol. 1982;36:281–302. doi: 10.1212/WNL.30.5.453. [DOI] [PubMed] [Google Scholar]
- 20.McLean C.P., Asnaani A., Litz B.T., Hofmann S.G. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 2011;45:1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ziemka-Nalecz M., Pawelec P., Ziabska K., Zalewska T. Sex Differences in Brain Disorders. Int. J. Mol. Sci. 2023;24:14571. doi: 10.3390/ijms241914571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Payami H., Montee K.R., Kaye J.A., Bird T.D., Yu C.E., Wijsman E.M., Schellenberg G.D. Alzheimer’s disease, apolipoprotein E4, and gender. JAMA. 1994;271:1316–1317. doi: 10.1001/jama.1994.03510410028015. [DOI] [PubMed] [Google Scholar]
- 23.Farrer L.A., Cupples L.A., Haines J.L., Hyman B., Kukull W.A., Mayeux R., Myers R.H., Pericak-Vance M.A., Risch N., Van Duijn C.M. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA. 1997;278:1349–1356. doi: 10.1001/jama.1997.03550160069041. [DOI] [PubMed] [Google Scholar]
- 24.Park K.W., Ryu H.-S., Shin E., Park Y., Jeon S.R., Kim S.Y., Kim J.S., Koh S.-B., Chung S.J. Ethnicity- and sex-specific genome wide association study on Parkinson’s disease. npj Park. Dis. 2023;9:141. doi: 10.1038/s41531-023-00580-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy-O’Reilly M., McCullough L.D. Sex differences in stroke: The contribution of coagulation. Exp. Neurol. 2014;259:16–27. doi: 10.1016/j.expneurol.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martínez-Sánchez P., Fuentes B., Fernández-Domínguez J., Ortega-Casarrubios M.d.l.Á., Aguilar-Amar M.J., Abenza-Abildúa M.J., Idrovo-Freire L., Díez-Tejedor E. Young Women Have Poorer Outcomes than Men after Stroke. Cerebrovasc. Dis. 2011;31:455–463. doi: 10.1159/000323851. [DOI] [PubMed] [Google Scholar]
- 27.Mo C., Hannan A.J., Renoir T. Environmental factors as modulators of neurodegeneration: Insights from gene-environment interactions in Huntington’s disease. Neurosci. Biobehav. Rev. 2015;52:178–192. doi: 10.1016/j.neubiorev.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Meoni S., Macerollo A., Moro E. Sex differences in movement disorders. Nat. Rev. Neurol. 2020;16:84–96. doi: 10.1038/s41582-019-0294-x. [DOI] [PubMed] [Google Scholar]
- 29.Zielonka D., Marinus J., Roos R.A., De Michele G. The influence of gender on phenotype and disease progression in patients with Huntington’s disease. Parkinsonism Relat. Disord. 2013;19:192–197. doi: 10.1016/j.parkreldis.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 30.Zielonka D., Stawinska-Witoszynska B. Gender Differences in Non-sex Linked Disorders: Insights From Huntington’s Disease. Front. Neurol. 2020;11:571. doi: 10.3389/fneur.2020.00571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levin H.S., Temkin N.R., Barber J., Nelson L.D., Robertson C., Brennan J., Stein M.B., Yue J.K., Giacino J.T., McCrea M.A., et al. Association of Sex and Age With Mild Traumatic Brain Injury–Related Symptoms: A TRACK-TBI Study. JAMA Netw. Open. 2021;4:e213046. doi: 10.1001/jamanetworkopen.2021.3046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gupte R.P., Brooks W.M., Vukas R.R., Pierce J.D., Harris J.L. Sex Differences in Traumatic Brain Injury: What We Know and What We Should Know. J. Neurotrauma. 2019;36:3063–3091. doi: 10.1089/neu.2018.6171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kirkness C.J., Burr R.L., Mitchell P.H., Newell D.W. Is there a sex difference in the course following traumatic brain injury? Biol. Res. Nurs. 2004;5:299–310. doi: 10.1177/1099800404263050. [DOI] [PubMed] [Google Scholar]
- 34.Mikolic A., van Klaveren D., Groeniger J.O., Wiegers E., Lingsma H.F., Zeldovich M., von Steinbuechel N., Maas A., van Lennep J.E.R., Polinder S. Differences between Men and Women in Treatment and Outcome after Traumatic Brain Injury. J. Neurotrauma. 2021;38:235–251. doi: 10.1089/neu.2021.0116. [DOI] [PubMed] [Google Scholar]
- 35.Bretzin A.C., Esopenko C., D’Alonzo B.A., Wiebe D.J. Clinical Recovery Timelines After Sport-Related Concussion in Men’s and Women’s Collegiate Sports. J. Athl. Train. 2022;57:678–687. doi: 10.4085/601-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Musko P.A., Demetriades A.K. Are Sex Differences in Collegiate and High School Sports-Related Concussion Reflected in the Guidelines? A Scoping Review. Brain Sci. 2023;13:1310. doi: 10.3390/brainsci13091310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bretzin A.C., Covassin T., Fox M.E., Petit K.M., Savage J.L., Walker L.F., Gould D. Sex Differences in the Clinical Incidence of Concussions, Missed School Days, and Time Loss in High School Student-Athletes: Part 1. Am. J. Sports Med. 2018;46:2263–2269. doi: 10.1177/0363546518778251. [DOI] [PubMed] [Google Scholar]
- 38.Covassin T., Moran R., Elbin R.J. Sex Differences in Reported Concussion Injury Rates and Time Loss From Participation: An Update of the National Collegiate Athletic Association Injury Surveillance Program From 2004–2005 Through 2008–2009. J. Athl. Train. 2016;51:189–194. doi: 10.4085/1062-6050-51.3.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee R.C., Feinbaum R.L., Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–854. doi: 10.1016/0092-8674(93)90529-Y. [DOI] [PubMed] [Google Scholar]
- 40.Wightman B., Ha I., Ruvkun G. Posttranscriptional regulation of the heterochronic gene lin-14 by lin-4 mediates temporal pattern formation in C. elegans. Cell. 1993;75:855–862. doi: 10.1016/0092-8674(93)90530-4. [DOI] [PubMed] [Google Scholar]
- 41.Friedman R.C., Farh K.K.-H., Burge C.B., Bartel D.P. Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 2009;19:92–105. doi: 10.1101/gr.082701.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petri R., Malmevik J., Fasching L., Åkerblom M., Jakobsson J. miRNAs in brain development. Exp. Cell Res. 2014;321:84–89. doi: 10.1016/j.yexcr.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 43.Ambros V. The functions of animal microRNAs. Nature. 2004;431:350–355. doi: 10.1038/nature02871. [DOI] [PubMed] [Google Scholar]
- 44.Bartel D.P. MicroRNAs: Genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–297. doi: 10.1016/S0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- 45.Chen C.-Z., Lodish H.F. MicroRNAs as regulators of mammalian hematopoiesis. Semin. Immunol. 2005;17:155–165. doi: 10.1016/j.smim.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 46.Coolen M., Bally-Cuif L. MicroRNAs in brain development and physiology. Curr. Opin. Neurobiol. 2009;19:461–470. doi: 10.1016/j.conb.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 47.Schratt G. Fine-tuning neural gene expression with microRNAs. Curr. Opin. Neurobiol. 2009;19:213–219. doi: 10.1016/j.conb.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 48.Xu P., Vernooy S.Y., Guo M., Hay B.A. The Drosophila MicroRNA Mir-14 Suppresses Cell Death and Is Required for Normal Fat Metabolism. Curr. Biol. 2003;13:790–795. doi: 10.1016/S0960-9822(03)00250-1. [DOI] [PubMed] [Google Scholar]
- 49.Giraldez A.J., Cinalli R.M., Glasner M.E., Enright A.J., Thomson J.M., Baskerville S., Hammond S.M., Bartel D.P., Schier A.F. MicroRNAs regulate brain morphogenesis in zebrafish. Science. 2005;308:833–838. doi: 10.1126/science.1109020. [DOI] [PubMed] [Google Scholar]
- 50.Rao Y.S., Pak T.R. microRNAs and the adolescent brain: Filling the knowledge gap. Neurosci. Biobehav. Rev. 2016;70:313–322. doi: 10.1016/j.neubiorev.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rao Y.S., Mott N.N., Wang Y., Chung W.C., Pak T.R. MicroRNAs in the Aging Female Brain: A Putative Mechanism for Age-Specific Estrogen Effects. Endocrinology. 2013;154:2795–2806. doi: 10.1210/en.2013-1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ha M., Kim V.N. Regulation of microRNA biogenesis. Nat. Rev. Mol. Cell Biol. 2014;15:509–524. doi: 10.1038/nrm3838. [DOI] [PubMed] [Google Scholar]
- 53.Lagos-Quintana M., Rauhut R., Lendeckel W., Tuschl T. Identification of Novel Genes Coding for Small Expressed RNAs. Science. 2001;294:853–858. doi: 10.1126/science.1064921. [DOI] [PubMed] [Google Scholar]
- 54.Gregory R.I., Yan K.-P., Amuthan G., Chendrimada T., Doratotaj B., Cooch N., Shiekhattar R. The Microprocessor complex mediates the genesis of microRNAs. Nature. 2004;432:235–240. doi: 10.1038/nature03120. [DOI] [PubMed] [Google Scholar]
- 55.Yi R., Qin Y., Macara I.G., Cullen B.R. Exportin-5 mediates the nuclear export of pre-microRNAs and short hairpin RNAs. Genes Dev. 2003;17:3011–3016. doi: 10.1101/gad.1158803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lund E., Güttinger S., Calado A., Dahlberg J.E., Kutay U. Nuclear Export of MicroRNA Precursors. Science. 2004;303:95–98. doi: 10.1126/science.1090599. [DOI] [PubMed] [Google Scholar]
- 57.Kim V.N. MicroRNA precursors in motion: Exportin-5 mediates their nuclear export. Trends Cell Biol. 2004;14:156–159. doi: 10.1016/j.tcb.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 58.Joshua-Tor L. The Argonautes. Cold Spring Harb. Symp. Quant. Biol. 2006;71:67–72. doi: 10.1101/sqb.2006.71.048. [DOI] [PubMed] [Google Scholar]
- 59.Nakanishi K. Anatomy of RISC: How do small RNAs and chaperones activate Argonaute proteins? Wiley Interdiscip. Rev. RNA. 2016;7:637–660. doi: 10.1002/wrna.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Park M.S., Araya-Secchi R., Brackbill J.A., Phan H.-D., Kehling A.C., El-Wahab E.W.A., Dayeh D.M., Sotomayor M., Nakanishi K. Multidomain Convergence of Argonaute during RISC Assembly Correlates with the Formation of Internal Water Clusters. Mol. Cell. 2019;75:725–740.e6. doi: 10.1016/j.molcel.2019.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alló M., Agirre E., Bessonov S., Bertucci P., Acuña L.G., Buggiano V., Bellora N., Singh B., Petrillo E., Blaustein M., et al. Argonaute-1 binds transcriptional enhancers and controls constitutive and alternative splicing in human cells. Proc. Natl. Acad. Sci. USA. 2014;111:15622–15629. doi: 10.1073/pnas.1416858111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Meister G., Landthaler M., Patkaniowska A., Dorsett Y., Teng G., Tuschl T. Human Argonaute2 Mediates RNA Cleavage Targeted by miRNAs and siRNAs. Mol. Cell. 2004;15:185–197. doi: 10.1016/j.molcel.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 63.Liu J., Carmell M.A., Rivas F.V., Marsden C.G., Thomson J.M., Song J.-J., Hammond S.M., Joshua-Tor L., Hannon G.J. Argonaute2 Is the Catalytic Engine of Mammalian RNAi. Science. 2004;305:1437–1441. doi: 10.1126/science.1102513. [DOI] [PubMed] [Google Scholar]
- 64.Sen A., Prizant H., Light A., Biswas A., Hayes E., Lee H.-J., Barad D., Gleicher N., Hammes S.R. Androgens regulate ovarian follicular development by increasing follicle stimulating hormone receptor and microRNA-125b expression. Proc. Natl. Acad. Sci. USA. 2014;111:3008–3013. doi: 10.1073/pnas.1318978111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.McFall T., McKnight B., Rosati R., Kim S., Huang Y., Viola-Villegas N., Ratnam M. Progesterone receptor A promotes invasiveness and metastasis of luminal breast cancer by suppressing regulation of critical microRNAs by estrogen. J. Biol. Chem. 2018;293:1163–1177. doi: 10.1074/jbc.M117.812438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Maillot G., Lacroix-Triki M., Pierredon S., Gratadou L., Schmidt S., Bénès V., Roché H., Dalenc F., Auboeuf D., Millevoi S., et al. Widespread estrogen-dependent repression of micrornas involved in breast tumor cell growth. Cancer Res. 2009;69:8332–8340. doi: 10.1158/0008-5472.CAN-09-2206. [DOI] [PubMed] [Google Scholar]
- 67.Sharma S., Eghbali M. Influence of sex differences on microRNA gene regulation in disease. Biol. Sex Differ. 2014;5:3. doi: 10.1186/2042-6410-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dai R., Ahmed S.A. Sexual dimorphism of miRNA expression: A new perspective in understanding the sex bias of autoimmune diseases. Ther. Clin. Risk Manag. 2014;10:151–163. doi: 10.2147/TCRM.S33517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Morgan C.P., Bale T.L. Sex differences in microRNA regulation of gene expression: No smoke, just miRs. Biol. Sex Differ. 2012;3:22. doi: 10.1186/2042-6410-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pak T.R., Rao Y.S., Prins S.A., Mott N.N. An emerging role for microRNAs in sexually dimorphic neurobiological systems. Pflüg. Arch. 2013;465:655–667. doi: 10.1007/s00424-013-1227-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Modzelewski A.J., Holmes R.J., Hilz S., Grimson A., Cohen P.E. AGO4 Regulates Entry into Meiosis and Influences Silencing of Sex Chromosomes in the Male Mouse Germline. Dev. Cell. 2012;23:251–264. doi: 10.1016/j.devcel.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Koturbash I., Zemp F., Kolb B., Kovalchuk O. Sex-specific radiation-induced microRNAome responses in the hippocampus, cerebellum and frontal cortex in a mouse model. Mutat. Res. 2011;722:114–118. doi: 10.1016/j.mrgentox.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 73.Ciaudo C., Servant N., Cognat V., Sarazin A., Kieffer E., Viville S., Colot V., Barillot E., Heard E., Voinnet O. Highly Dynamic and Sex-Specific Expression of microRNAs During Early ES Cell Differentiation. PLoS Genet. 2009;5:e1000620. doi: 10.1371/journal.pgen.1000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Langevin S.M., Stone R.A., Bunker C.H., Grandis J.R., Sobol R.W., Taioli E. MicroRNA-137 promoter methylation in oral rinses from patients with squamous cell carcinoma of the head and neck is associated with gender and body mass index. Carcinog. 2010;31:864–870. doi: 10.1093/carcin/bgq051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Siegel C., Li J., Liu F., Benashski S.E., McCullough L.D. miR-23a regulation of X-linked inhibitor of apoptosis (XIAP) contributes to sex differences in the response to cerebral ischemia. Proc. Natl. Acad. Sci. USA. 2011;108:11662–11667. doi: 10.1073/pnas.1102635108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gumerov V., Hegyi H. MicroRNA-derived network analysis of differentially methylated genes in schizophrenia, implicating GABA receptor B1 [GABBR1] and protein kinase B [AKT1] Biol. Direct. 2015;10:59. doi: 10.1186/s13062-015-0089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Feng J., Sun G., Yan J., Noltner K., Li W., Buzin C.H., Longmate J., Heston L.L., Rossi J., Sommer S.S. Evidence for X-Chromosomal Schizophrenia Associated with microRNA Alterations. PLoS ONE. 2009;4:e6121. doi: 10.1371/journal.pone.0006121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mujahid S., Logvinenko T., Volpe M.V., Nielsen H.C. miRNA regulated pathways in late stage murine lung development. BMC Dev. Biol. 2013;13:13. doi: 10.1186/1471-213X-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Morgan C.P., Bale T.L. Sex differences in microRNA-mRNA networks: Examination of novel epigenetic programming mechanisms in the sexually dimorphic neonatal hypothalamus. Biol. Sex Differ. 2017;8:27. doi: 10.1186/s13293-017-0149-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Morgan C.P., Bale T.L. Early Prenatal Stress Epigenetically Programs Dysmasculinization in Second-Generation Offspring via the Paternal Lineage. J. Neurosci. 2011;31:11748–11755. doi: 10.1523/JNEUROSCI.1887-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Szakats S., McAtamney A., Cross H., Wilson M.J. Sex-biased gene and microRNA expression in the developing mouse brain is associated with neurodevelopmental functions and neurological phenotypes. Biol. Sex Differ. 2023;14:57. doi: 10.1186/s13293-023-00538-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ameling S., Kacprowski T., Chilukoti R.K., Malsch C., Liebscher V., Suhre K., Pietzner M., Friedrich N., Homuth G., Hammer E., et al. Associations of circulating plasma microRNAs with age, body mass index and sex in a population-based study. BMC Med. Genom. 2015;8:61. doi: 10.1186/s12920-015-0136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cui C., Yang W., Shi J., Zhou Y., Yang J., Cui Q., Zhou Y. Identification and Analysis of Human Sex-biased MicroRNAs. Genom. Proteom. Bioinform. 2018;16:200–211. doi: 10.1016/j.gpb.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhong B., Cui C., Cui Q. Identification and Analysis of Sex-Biased MicroRNAs in Human Diseases. Genes. 2023;14:1688. doi: 10.3390/genes14091688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Murphy S.J., Lusardi T.A., Phillips J.I., Saugstad J.A. Sex differences in microRNA expression during development in rat cortex. Neurochem. Int. 2014;77:24–32. doi: 10.1016/j.neuint.2014.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chum P.P., Hakim A., Behringer E.J. Cerebrovascular microRNA Expression Profile During Early Development of Alzheimer’s Disease in a Mouse Model. J. Alzheimer’s Dis. 2022;85:91–113. doi: 10.3233/JAD-215223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Geekiyanage H., Jicha G.A., Nelson P.T., Chan C. Blood serum miRNA: Non-invasive biomarkers for Alzheimer’s disease. Exp. Neurol. 2012;235:491–496. doi: 10.1016/j.expneurol.2011.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Geekiyanage H., Chan C. MicroRNA-137/181c regulates serine palmitoyltransferase and in turn amyloid β, novel targets in sporadic Alzheimer’s disease. J. Neurosci. 2011;31:14820–14830. doi: 10.1523/JNEUROSCI.3883-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rani A., Barter J., Kumar A., Stortz J.A., Hollen M., Nacionales D., Moldawer L.L., Efron P.A., Foster T.C. Influence of age and sex on microRNA response and recovery in the hippocampus following sepsis. Aging. 2022;14:728–746. doi: 10.18632/aging.203868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lusardi T.A., Murphy S.J., Phillips J.I., Chen Y., Davis C.M., Young J.M., Thompson S.J., Saugstad J.A. MicroRNA responses to focal cerebral ischemia in male and female mouse brain. Front. Mol. Neurosci. 2014;7:11. doi: 10.3389/fnmol.2014.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kodama L., Guzman E., Etchegaray J.I., Li Y., Sayed F.A., Zhou L., Zhou Y., Zhan L., Le D., Udeochu J.C., et al. Microglial microRNAs mediate sex-specific responses to tau pathology. Nat. Neurosci. 2020;23:167–171. doi: 10.1038/s41593-019-0560-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pegoraro V., Merico A., Angelini C. Micro-RNAs in ALS muscle: Differences in gender, age at onset and disease duration. J. Neurol. Sci. 2017;380:58–63. doi: 10.1016/j.jns.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vallelunga A., Iannitti T., Somma G., Russillo M.C., Picillo M., De Micco R., Vacca L., Cilia R., Cicero C.E., Zangaglia R., et al. Gender differences in microRNA expression in levodopa-naive PD patients. J. Neurol. 2023;270:3574–3582. doi: 10.1007/s00415-023-11707-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bai X., Tang Y., Yu M., Wu L., Liu F., Ni J., Wang Z., Wang J., Fei J., Wang W., et al. Downregulation of blood serum microRNA 29 family in patients with Parkinson’s disease. Sci. Rep. 2017;7:5411. doi: 10.1038/s41598-017-03887-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Grasso M., Piscopo P., Talarico G., Ricci L., Crestini A., Tosto G., Gasparini M., Bruno G., Denti M.A., Confaloni A. Plasma microRNA profiling distinguishes patients with frontotemporal dementia from healthy subjects. Neurobiol. Aging. 2019;84:240.e1–240.e12. doi: 10.1016/j.neurobiolaging.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 96.Mellios N., Galdzicka M., Ginns E., Baker S.P., Rogaev E., Xu J., Akbarian S. Gender-Specific Reduction of Estrogen-Sensitive Small RNA, miR-30b, in Subjects With Schizophrenia. Schizophr. Bull. 2012;38:433–443. doi: 10.1093/schbul/sbq091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Matarrese P., Tieri P., Anticoli S., Ascione B., Conte M., Franceschi C., Malorni W., Salvioli S., Ruggieri A. X-chromosome-linked miR548am-5p is a key regulator of sex disparity in the susceptibility to mitochondria-mediated apoptosis. Cell Death Dis. 2019;10:673. doi: 10.1038/s41419-019-1888-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Prajapati P., Wang W.-X., Pesina S.A., Geleta U., Springer J.E. Sex-Specific Alterations in Inflammatory MicroRNAs in Mouse Brain and Bone Marrow CD11b+ Cells Following Traumatic Brain Injury. Cell. Mol. Neurobiol. 2021;43:423–429. doi: 10.1007/s10571-021-01164-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Delaloy C., Liu L., Lee J.-A., Su H., Shen F., Yang G.-Y., Young W.L., Ivey K.N., Gao F.-B. MicroRNA-9 Coordinates Proliferation and Migration of Human Embryonic Stem Cell-Derived Neural Progenitors. Cell Stem Cell. 2010;6:323–335. doi: 10.1016/j.stem.2010.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Krichevsky A.M., King K.S., Donahue C.P., Khrapko K., Kosik K.S. A microRNA array reveals extensive regulation of microRNAs during brain development. RNA. 2003;9:1274–1281. doi: 10.1261/rna.5980303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ziats M.N., Rennert O.M. Identification of differentially expressed microRNAs across the developing human brain. Mol. Psychiatry. 2014;19:848–852. doi: 10.1038/mp.2013.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Markham J.A., Koenig J.I. Prenatal stress: Role in psychotic and depressive diseases. Psychopharmacology. 2011;214:89–106. doi: 10.1007/s00213-010-2035-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kinney D.K., Miller A.M., Crowley D.J., Huang E., Gerber E. Autism Prevalence Following Prenatal Exposure to Hurricanes and Tropical Storms in Louisiana. J. Autism Dev. Disord. 2008;38:481–488. doi: 10.1007/s10803-007-0414-0. [DOI] [PubMed] [Google Scholar]
- 104.Khashan A.S., Abel K.M., McNamee R., Pedersen M.G., Webb R.T., Baker P.N., Kenny L.C., Mortensen P.B. Higher Risk of Offspring Schizophrenia Following Antenatal Maternal Exposure to Severe Adverse Life Events. Arch. Gen. Psychiatry. 2008;65:146–152. doi: 10.1001/archgenpsychiatry.2007.20. [DOI] [PubMed] [Google Scholar]
- 105.van Os J., Selten J.P. Prenatal exposure to maternal stress and subsequent schizophrenia. The May 1940 invasion of The Netherlands. Br. J. Psychiatry. 1998;172:324–326. doi: 10.1192/bjp.172.4.324. [DOI] [PubMed] [Google Scholar]
- 106.Franklin T.B., Russig H., Weiss I.C., Gräff J., Linder N., Michalon A., Vizi S., Mansuy I.M. Epigenetic transmission of the impact of early stress across generations. Biol. Psychiatry. 2010;68:408–415. doi: 10.1016/j.biopsych.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 107.Weinstock M. Gender Differences in the Effects of Prenatal Stress on Brain Development and Behaviour. Neurochem. Res. 2007;32:1730–1740. doi: 10.1007/s11064-007-9339-4. [DOI] [PubMed] [Google Scholar]
- 108.Grundwald N.J., Brunton P.J. Prenatal stress programs neuroendocrine stress responses and affective behaviors in second generation rats in a sex-dependent manner. Psychoneuroendocrinology. 2015;62:204–216. doi: 10.1016/j.psyneuen.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Weinstock M. Sex-dependent changes induced by prenatal stress in cortical and hippocampal morphology and behaviour in rats: An update. Stress. 2011;14:604–613. doi: 10.3109/10253890.2011.588294. [DOI] [PubMed] [Google Scholar]
- 110.Guerrero-Bosagna C., Settles M., Lucker B., Skinner M.K. Epigenetic Transgenerational Actions of Vinclozolin on Promoter Regions of the Sperm Epigenome. PLoS ONE. 2010;5:e13100. doi: 10.1371/journal.pone.0013100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Maher B. Personal genomes: The case of the missing heritability. Nature. 2008;456:18–21. doi: 10.1038/456018a. [DOI] [PubMed] [Google Scholar]
- 112.Slatkin M. Epigenetic Inheritance and the Missing Heritability Problem. Genetics. 2009;182:845–850. doi: 10.1534/genetics.109.102798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Matsuda K.I., Mori H., Kawata M. Epigenetic mechanisms are involved in sexual differentiation of the brain. Rev. Endocr. Metab. Disord. 2012;13:163–171. doi: 10.1007/s11154-012-9202-z. [DOI] [PubMed] [Google Scholar]
- 114.Mueller B.R., Bale T.L. Sex-Specific Programming of Offspring Emotionality after Stress Early in Pregnancy. J. Neurosci. 2008;28:9055–9065. doi: 10.1523/JNEUROSCI.1424-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nelson P.T., Wang W.X., Rajeev B.W. MicroRNAs (miRNAs) in neurodegenerative diseases. Brain Pathol. 2008;18:130–138. doi: 10.1111/j.1750-3639.2007.00120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Liu N.-K., Xu X.-M. MicroRNA in central nervous system trauma and degenerative disorders. Physiol. Genom. 2011;43:571–580. doi: 10.1152/physiolgenomics.00168.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Barbato C., Giorgi C., Catalanotto C., Cogoni C. Thinking about RNA? MicroRNAs in the brain. Mamm. Genome. 2008;19:541–551. doi: 10.1007/s00335-008-9129-6. [DOI] [PubMed] [Google Scholar]
- 118.Kuss A.W., Chen W. MicroRNAs in brain function and disease. Curr. Neurol. Neurosci. Rep. 2008;8:190–197. doi: 10.1007/s11910-008-0031-0. [DOI] [PubMed] [Google Scholar]
- 119.Wang W.X., Rajeev B.W., Stromberg A.J., Ren N., Tang G., Huang Q., Rigoutsos I., Nelson P.T. The expression of microRNA miR-107 decreases early in Alzheimer’s disease and may accelerate disease progression through regulation of beta-site amyloid precursor protein-cleaving enzyme 1. J. Neurosci. 2008;28:1213–1223. doi: 10.1523/JNEUROSCI.5065-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hébert S.S., Horré K., Nicolaï L., Papadopoulou A.S., Mandemakers W., Silahtaroglu A.N., Kauppinen S., Delacourte A., De Strooper B. Loss of microRNA cluster miR-29a/b-1 in sporadic Alzheimer’s disease correlates with increased BACE1/beta-secretase expression. Proc. Natl. Acad. Sci. USA. 2008;105:6415–6420. doi: 10.1073/pnas.0710263105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cutler R.G., Kelly J., Storie K., Pedersen W.A., Tammara A., Hatanpaa K., Troncoso J.C., Mattson M.P. Involvement of oxidative stress-induced abnormalities in ceramide and cholesterol metabolism in brain aging and Alzheimer’s disease. Proc. Natl. Acad. Sci. USA. 2004;101:2070–2075. doi: 10.1073/pnas.0305799101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Filippov V., Song M.A., Zhang K., Vinters H.V., Tung S., Kirsch W.M., Yang J., Duerksen-Hughes P.J. Increased ceramide in brains with Alzheimer’s and other neurodegenerative diseases. J. Alzheimers Dis. 2012;29:537–547. doi: 10.3233/JAD-2011-111202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Piscopo P., Grasso M., Puopolo M., D’acunto E., Talarico G., Crestini A., Gasparini M., Campopiano R., Gambardella S., Castellano A.E., et al. Circulating miR-127-3p as a Potential Biomarker for Differential Diagnosis in Frontotemporal Dementia. J. Alzheimer’s Dis. 2018;65:455–464. doi: 10.3233/JAD-180364. [DOI] [PubMed] [Google Scholar]
- 124.Iwashyna T.J., Ely E.W., Smith D.M., Langa K.M. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chung H.Y., Wickel J., Brunkhorst F.M., Geis C. Sepsis-Associated Encephalopathy: From Delirium to Dementia? J. Clin. Med. 2020;9:703. doi: 10.3390/jcm9030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gracner T., Agarwal M., Murali K.P., Stone P.W., Larson E.L., Furuya E.Y., Harrison J.M., Dick A.W. Association of Infection-Related Hospitalization With Cognitive Impairment Among Nursing Home Residents. JAMA Netw. Open. 2021;4:e217528. doi: 10.1001/jamanetworkopen.2021.7528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kaidonis G., Rao A.N., Ouyang Y.-B., Stary C.M. Elucidating sex differences in response to cerebral ischemia: Immunoregulatory mechanisms and the role of microRNAs. Prog. Neurobiol. 2019;176:73–85. doi: 10.1016/j.pneurobio.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 128.Golomb M.R., Fullerton H.J., Nowak-Gottl U., Deveber G. Male predominance in childhood ischemic stroke: Findings from the international pediatric stroke study. Stroke. 2009;40:52–57. doi: 10.1161/STROKEAHA.108.521203. [DOI] [PubMed] [Google Scholar]
- 129.Deveraux Q.L., Reed J.C. IAP family proteins—Suppressors of apoptosis. Genes Dev. 1999;13:239–252. doi: 10.1101/gad.13.3.239. [DOI] [PubMed] [Google Scholar]
- 130.Florijn B.W., Bijkerk R., Kruyt N.D., van Zonneveld A.J., Wermer M.J.H. Sex-Specific MicroRNAs in Neurovascular Units in Ischemic Stroke. Int. J. Mol. Sci. 2021;22:11888. doi: 10.3390/ijms222111888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Menon D.K., Schwab K., Wright D.W., Maas A.I. Position statement: Definition of traumatic brain injury. Arch. Phys. Med. Rehabil. 2010;91:1637–1640. doi: 10.1016/j.apmr.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 132.Faul M., Coronado V. Epidemiology of traumatic brain injury. Handb. Clin. Neurol. 2015;127:3–13. doi: 10.1016/B978-0-444-52892-6.00001-5. [DOI] [PubMed] [Google Scholar]
- 133.Felderhoff-Mueser U., Ikonomidou C. Mechanisms of neurodegeneration after paediatric brain injury. Curr. Opin. Neurol. 2000;13:141–145. doi: 10.1097/00019052-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 134.Ray S.K., Dixon C.E., Banik N.L. Molecular mechanisms in the pathogenesis of traumatic brain injury. Histol. Histopathol. 2002;17:1137–1152. doi: 10.14670/HH-17.1137. [DOI] [PubMed] [Google Scholar]
- 135.Patt S., Brodhun M. Neuropathological sequelae of traumatic injury in the brain. An overview. Exp. Toxicol. Pathol. 1999;51:119–123. doi: 10.1016/S0940-2993(99)80084-0. [DOI] [PubMed] [Google Scholar]
- 136.Intosh M., Saatman K., Raghupathi R., Graham D., Smith D.H., Lee V.M., Trojanowski J.Q. gThe Dorothy Russell Memorial Lecture* The molecular and cellular sequelae of experimental traumatic brain injury: Pathogenetic mechanisms. Neuropathol. Appl. Neurobiol. 1998;24:251–267. doi: 10.1046/j.1365-2990.1998.00121.x. [DOI] [PubMed] [Google Scholar]
- 137.Rosenfeld J.V., Maas A.I., Bragge P., Morganti-Kossmann M.C., Manley G.T., Gruen R.L. Early management of severe traumatic brain injury. Lancet. 2012;380:1088–1098. doi: 10.1016/S0140-6736(12)60864-2. [DOI] [PubMed] [Google Scholar]
- 138.Plassman B., Havlik R., Steffens D., Helms M., Newman T., Drosdick D., Phillips C., Gau B., Welsh–Bohmer K., Burke J., et al. Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology. 2000;55:1158–1166. doi: 10.1212/WNL.55.8.1158. [DOI] [PubMed] [Google Scholar]
- 139.Wang H.-K., Lin S.-H., Sung P.-S., Wu M.-H., Hung K.-W., Wang L.-C., Huang C.-Y., Lu K., Chen H.-J., Tsai K.-J. Population based study on patients with traumatic brain injury suggests increased risk of dementia. J. Neurol. Neurosurg. Psychiatry. 2012;83:1080–1085. doi: 10.1136/jnnp-2012-302633. [DOI] [PubMed] [Google Scholar]
- 140.Gardner R.C., Burke J.F., Nettiksimmons J., Kaup A., Barnes D.E., Yaffe K. Dementia risk after traumatic brain injury vs nonbrain trauma: The role of age and severity. JAMA Neurol. 2014;71:1490–1497. doi: 10.1001/jamaneurol.2014.2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lee Y.-K., Hou S.-W., Lee C.-C., Hsu C.-Y., Huang Y.-S., Su Y.-C. Increased Risk of Dementia in Patients with Mild Traumatic Brain Injury: A Nationwide Cohort Study. PLoS ONE. 2013;8:e62422. doi: 10.1371/journal.pone.0062422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Nordström P., Michaëlsson K., Gustafson Y., Nordström A. Traumatic brain injury and young onset dementia: A nationwide cohort study. Ann. Neurol. 2014;75:374–381. doi: 10.1002/ana.24101. [DOI] [PubMed] [Google Scholar]
- 143.Gardner R.C., Langa K.M., Yaffe K. Subjective and objective cognitive function among older adults with a history of traumatic brain injury: A population-based cohort study. PLoS Med. 2017;14:e1002246. doi: 10.1371/journal.pmed.1002246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cole J.H., Leech R., Sharp D.J. Alzheimer’s Disease Neuroimaging Initiative. Prediction of brain age suggests accelerated atrophy after traumatic brain injury. Ann. Neurol. 2015;77:571–581. doi: 10.1002/ana.24367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Graham N.S., Sharp D.J. Understanding neurodegeneration after traumatic brain injury: From mechanisms to clinical trials in dementia. J. Neurol. Neurosurg. Psychiatry. 2019;90:1221–1233. doi: 10.1136/jnnp-2017-317557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Johnson V.E., Stewart W., Arena J.D., Smith D.H. Traumatic Brain Injury as a Trigger of Neurodegeneration. Adv. Neurobiol. 2017;15:383–400. doi: 10.1007/978-3-319-57193-5_15. [DOI] [PubMed] [Google Scholar]
- 147.Zaloshnja E., Miller T., Langlois J.A., Selassie A.W. Prevalence of Long-Term Disability From Traumatic Brain Injury in the Civilian Population of the United States, 2005. J. Head Trauma Rehabil. 2008;23:394–400. doi: 10.1097/01.HTR.0000341435.52004.ac. [DOI] [PubMed] [Google Scholar]
- 148.Farace E., Alves W.M. Do women fare worse: A metaanalysis of gender differences in traumatic brain injury outcome. J. Neurosurg. 2000;93:539–545. doi: 10.3171/jns.2000.93.4.0539. [DOI] [PubMed] [Google Scholar]
- 149.Master C.L., Katz B.P., Arbogast K.B., McCrea M.A., McAllister T.W., Pasquina P.F., Lapradd M., Zhou W., Broglio S.P. Differences in sport-related concussion for female and male athletes in comparable collegiate sports: A study from the NCAA-DoD Concussion Assessment, Research and Education (CARE) Consortium. Br. J. Sports Med. 2021;55:1387–1394. doi: 10.1136/bjsports-2020-103316. [DOI] [PubMed] [Google Scholar]
- 150.Berry C., Ley E.J., Tillou A., Gil Cryer G., Margulies D.R., Salim A. The Effect of Gender on Patients With Moderate to Severe Head Injuries. J. Trauma Inj. Infect. Crit. Care. 2009;67:950–953. doi: 10.1097/TA.0b013e3181ba3354. [DOI] [PubMed] [Google Scholar]
- 151.Beijer E., van Wonderen S.F., Zuidema W.P., Visser M.C., Edwards M.J.R., Verhofstad M.H.J., Tromp T.N., Brom C.E.v.D., van Lieshout E.M.M., Bloemers F.W., et al. Sex Differences in Outcome of Trauma Patients Presented with Severe Traumatic Brain Injury: A Multicenter Cohort Study. J. Clin. Med. 2023;12:6892. doi: 10.3390/jcm12216892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Maas A.I.R., Menon D.K., Manley G.T., Abrams M., Åkerlund C., Andelic N., Aries M., Bashford T., Bell M.J., Bodien Y.G., et al. Traumatic brain injury: Progress and challenges in prevention, clinical care, and research. Lancet Neurol. 2022;21:1004–1060. doi: 10.1016/S1474-4422(22)00309-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Roof R.L., Hall E.D. Estrogen-Related Gender Difference in Survival Rate and Cortical Blood Flow after Impact-Acceleration Head Injury in Rats. J. Neurotrauma. 2000;17:1155–1169. doi: 10.1089/neu.2000.17.1155. [DOI] [PubMed] [Google Scholar]
- 154.Bramlett H.M., Dietrich W.D. Neuropathological Protection after Traumatic Brain Injury in Intact Female Rats Versus Males or Ovariectomized Females. J. Neurotrauma. 2001;18:891–900. doi: 10.1089/089771501750451811. [DOI] [PubMed] [Google Scholar]
- 155.Tucker L.B., Burke J.F., Fu A.H., McCabe J.T. Neuropsychiatric Symptom Modeling in Male and Female C57BL/6J Mice after Experimental Traumatic Brain Injury. J. Neurotrauma. 2017;34:890–905. doi: 10.1089/neu.2016.4508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Clevenger A.C., Kim H., Salcedo E., Yonchek J.C., Rodgers K.M., Orfila J.E., Dietz R.M., Quillinan N., Traystman R.J., Herson P.S. Endogenous Sex Steroids Dampen Neuroinflammation and Improve Outcome of Traumatic Brain Injury in Mice. J. Mol. Neurosci. 2018;64:410–420. doi: 10.1007/s12031-018-1038-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Redell J.B., Liu Y., Dash P.K. Traumatic brain injury alters expression of hippocampal microRNAs: Potential regulators of multiple pathophysiological processes. J. Neurosci. Res. 2009;87:1435–1448. doi: 10.1002/jnr.21945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Liu L., Sun T., Liu Z., Chen X., Zhao L., Qu G., Li Q. Traumatic Brain Injury Dysregulates MicroRNAs to Modulate Cell Signaling in Rat Hippocampus. PLoS ONE. 2014;9:e103948. doi: 10.1371/journal.pone.0103948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wang W.-X., Visavadiya N.P., Pandya J.D., Nelson P.T., Sullivan P.G., Springer J.E. Mitochondria-associated microRNAs in rat hippocampus following traumatic brain injury. Exp. Neurol. 2015;265:84–93. doi: 10.1016/j.expneurol.2014.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wang W.-X., Springer J., Prajapati P., Vekaria H.J., Spry M., Cloud A.L., Sullivan P.G. Temporal changes in inflammatory mitochondria-enriched microRNAs following traumatic brain injury and effects of miR-146a nanoparticle delivery. Neural Regen. Res. 2021;16:514–522. doi: 10.4103/1673-5374.293149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Devoto C., Lai C., Qu B.-X., Guedes V.A., Leete J., Wilde E.A., Walker W.C., Diaz-Arrastia R., Kenney K., Gill J. Exosomal MicroRNAs in Military Personnel with Mild Traumatic Brain Injury: Preliminary Results from the Chronic Effects of Neurotrauma Consortium Biomarker Discovery Project. J. Neurotrauma. 2020;37:2482–2492. doi: 10.1089/neu.2019.6933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ghai V., Fallen S., Baxter D., Scherler K., Kim T.-K., Zhou Y., Meabon J.S., Logsdon A.F., Banks W.A., Schindler A.G., et al. Alterations in Plasma microRNA and Protein Levels in War Veterans with Chronic Mild Traumatic Brain Injury. J. Neurotrauma. 2020;37:1418–1430. doi: 10.1089/neu.2019.6826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Atif H., Hicks S.D. A Review of MicroRNA Biomarkers in Traumatic Brain Injury. J. Exp. Neurosci. 2019;13:117906951983228. doi: 10.1177/1179069519832286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Di Pietro V., Porto E., Ragusa M., Barbagallo C., Davies D., Forcione M., Logan A., Di Pietro C., Purrello M., Grey M., et al. Salivary MicroRNAs: Diagnostic Markers of Mild Traumatic Brain Injury in Contact-Sport. Front. Mol. Neurosci. 2018;11:290. doi: 10.3389/fnmol.2018.00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Di Pietro V., Ragusa M., Davies D., Su Z., Hazeldine J., Lazzarino G., Hill L.J., Crombie N., Foster M., Purrello M., et al. MicroRNAs as Novel Biomarkers for the Diagnosis and Prognosis of Mild and Severe Traumatic Brain Injury. J. Neurotrauma. 2017;34:1948–1956. doi: 10.1089/neu.2016.4857. [DOI] [PubMed] [Google Scholar]
- 166.Papa L., Slobounov S.M., Breiter H.C., Walter A., Bream T., Seidenberg P., Bailes J.E., Bravo S., Johnson B., Kaufman D., et al. Elevations in MicroRNA Biomarkers in Serum Are Associated with Measures of Concussion, Neurocognitive Function, and Subconcussive Trauma over a Single National Collegiate Athletic Association Division I Season in Collegiate Football Players. J. Neurotrauma. 2019;36:1343–1351. doi: 10.1089/neu.2018.6072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hicks S.D., Johnson J., Carney M.C., Bramley H., Olympia R.P., Loeffert A.C., Thomas N.J. Overlapping MicroRNA Expression in Saliva and Cerebrospinal Fluid Accurately Identifies Pediatric Traumatic Brain Injury. J. Neurotrauma. 2018;35:64–72. doi: 10.1089/neu.2017.5111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Beery A.K., Zucker I. Sex bias in neuroscience and biomedical research. Neurosci. Biobehav. Rev. 2011;35:565–572. doi: 10.1016/j.neubiorev.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Zucker I., Beery A.K. Males still dominate animal studies. Nature. 2010;465:690. doi: 10.1038/465690a. [DOI] [PubMed] [Google Scholar]
- 170.Späni C.B., Braun D.J., Van Eldik L.J. Sex-related responses after traumatic brain injury: Considerations for preclinical modeling. Front. Neuroendocr. 2018;50:52–66. doi: 10.1016/j.yfrne.2018.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Biegon A. Considering Biological Sex in Traumatic Brain Injury. Front. Neurol. 2021;12:576366. doi: 10.3389/fneur.2021.576366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Tarallo R., Giurato G., Bruno G., Ravo M., Rizzo F., Salvati A., Ricciardi L., Marchese G., Cordella A., Rocco T., et al. The nuclear receptor ERβ engages AGO2 in regulation of gene transcription, RNA splicing and RISC loading. Genome Biol. 2017;18:189. doi: 10.1186/s13059-017-1321-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Linscott M.L., Yildiz Y., Flury S., Newby M.L., Pak T.R. Age and 17β-Estradiol (E2) Facilitate Nuclear Export and Argonaute Loading of microRNAs in the Female Brain. Non-Coding RNA. 2023;9:74. doi: 10.3390/ncrna9060074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Rao Y.S., Shults C.L., Pinceti E., Pak T.R. Prolonged ovarian hormone deprivation alters the effects of 17β-estradiol on microRNA expression in the aged female rat hypothalamus. Oncotarget. 2015;6:36965–36983. doi: 10.18632/oncotarget.5433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Guo X., Su B., Zhou Z., Sha J. Rapid evolution of mammalian X-linked testis microRNAs. BMC Genom. 2009;10:97. doi: 10.1186/1471-2164-10-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Pinheiro I., Dejager L., Libert C. X-chromosome-located microRNAs in immunity: Might they explain male/female differences? The X chromosome-genomic context may affect X-located miRNAs and downstream signaling, thereby contributing to the enhanced immune response of females. Bioessays. 2011;33:791–802. doi: 10.1002/bies.201100047. [DOI] [PubMed] [Google Scholar]
- 177.Carè A., Bellenghi M., Matarrese P., Gabriele L., Salvioli S., Malorni W. Sex disparity in cancer: Roles of microRNAs and related functional players. Cell Death Differ. 2018;25:477–485. doi: 10.1038/s41418-017-0051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Di Palo A., Siniscalchi C., Salerno M., Russo A., Gravholt C.H., Potenza N. What microRNAs could tell us about the human X chromosome. Cell. Mol. Life Sci. 2020;77:4069–4080. doi: 10.1007/s00018-020-03526-7. Erratum in Cell. Mol. Life Sci. 2021, 78, 4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Lyon M.F. Gene Action in the X-chromosome of the Mouse (Mus musculus L.) Nature. 1961;190:372–373. doi: 10.1038/190372a0. [DOI] [PubMed] [Google Scholar]
- 180.Lyon M.F. X-chromosome inactivation: A repeat hypothesis. Cytogenet. Cell Genet. 1998;80:133–137. doi: 10.1159/000014969. [DOI] [PubMed] [Google Scholar]
- 181.Payer B., Lee J.T. X Chromosome Dosage Compensation: How Mammals Keep the Balance. Annu. Rev. Genet. 2008;42:733–772. doi: 10.1146/annurev.genet.42.110807.091711. [DOI] [PubMed] [Google Scholar]
- 182.Carrel L., Willard H.F. X-inactivation profile reveals extensive variability in X-linked gene expression in females. Nature. 2005;434:400–404. doi: 10.1038/nature03479. [DOI] [PubMed] [Google Scholar]
- 183.Lyon M.F. X-chromosome inactivation and human genetic disease. Acta Paediatr. Suppl. 2002;91:107–112. doi: 10.1111/j.1651-2227.2002.tb03120.x. [DOI] [PubMed] [Google Scholar]
- 184.Navarro-Cobos M.J., Balaton B.P., Brown C.J. Genes that escape from X-chromosome inactivation: Potential contributors to Klinefelter syndrome. Am. J. Med. Genet. Part C Semin. Med. Genet. 2020;184:226–238. doi: 10.1002/ajmg.c.31800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Balaton B.P., Brown C.J. Escape Artists of the X Chromosome. Trends Genet. 2016;32:348–359. doi: 10.1016/j.tig.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 186.Tukiainen T., Villani A.-C., Yen A., Rivas M.A., Marshall J.L., Satija R., Aguirre M., Gauthier L., Fleharty M., Kirby A., et al. Landscape of X chromosome inactivation across human tissues. Nature. 2017;550:244–248. doi: 10.1038/nature24265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Chen K., Ma Y., Wu S., Zhuang Y., Liu X., Lv L., Zhang G. Construction and analysis of a lncRNA-miRNA-mRNA network based on competitive endogenous RNA reveals functional lncRNAs in diabetic cardiomyopathy. Mol. Med. Rep. 2019;20:1393–1403. doi: 10.3892/mmr.2019.10361. [DOI] [PubMed] [Google Scholar]
- 188.Wang J., Syrett C.M., Kramer M.C., Basu A., Atchison M.L., Anguera M.C. Unusual maintenance of X chromosome inactivation predisposes female lymphocytes for increased expression from the inactive X. Proc. Natl. Acad. Sci. USA. 2016;113:E2029–E2038. doi: 10.1073/pnas.1520113113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Liu Y., Sinke L., Jonkman T.H., Slieker R.C., van Zwet E.W., Daxinger L., Heijmans B.T. BIOS Consortium The inactive X chromosome accumulates widespread epigenetic variability with age. Clin. Epigenet. 2023;15:135. doi: 10.1186/s13148-023-01549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Peeters S.B., Posynick B.J., Brown C.J. Out of the Silence: Insights into How Genes Escape X-Chromosome Inactivation. Epigenomes. 2023;7:29. doi: 10.3390/epigenomes7040029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Grigoryan A., Pospiech J., Krämer S., Lipka D., Liehr T., Geiger H., Kimura H., Mulaw M.A., Florian M.C. Attrition of X Chromosome Inactivation in Aged Hematopoietic Stem Cells. Stem Cell Rep. 2021;16:708–716. doi: 10.1016/j.stemcr.2021.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Mishima T., Takizawa T., Luo S.-S., Ishibashi O., Kawahigashi Y., Mizuguchi Y., Ishikawa T., Mori M., Kanda T., Goto T., et al. MicroRNA (miRNA) cloning analysis reveals sex differences in miRNA expression profiles between adult mouse testis and ovary. Reproduction. 2008;136:811–822. doi: 10.1530/REP-08-0349. [DOI] [PubMed] [Google Scholar]
- 193.Ro S., Park C., Sanders K.M., McCarrey J.R., Yan W. Cloning and expression profiling of testis-expressed microRNAs. Dev. Biol. 2007;311:592–602. doi: 10.1016/j.ydbio.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Royo H., Seitz H., ElInati E., Peters A.H.F.M., Stadler M.B., Turner J.M.A. Silencing of X-Linked MicroRNAs by Meiotic Sex Chromosome Inactivation. PLoS Genet. 2015;11:e1005461. doi: 10.1371/journal.pgen.1005461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Song R., Ro S., Michaels J.D., Park C., McCarrey J.R., Yan W. Many X-linked microRNAs escape meiotic sex chromosome inactivation. Nat. Genet. 2009;41:488–493. doi: 10.1038/ng.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Sosa E., Flores L., Yan W., McCarrey J.R. Escape of X-linked miRNA genes from meiotic sex chromosome inactivation. Development. 2015;142:3791–3800. doi: 10.1242/dev.127191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Meunier J., Lemoine F., Soumillon M., Liechti A., Weier M., Guschanski K., Hu H., Khaitovich P., Kaessmann H. Birth and expression evolution of mammalian microRNA genes. Genome Res. 2013;23:34–45. doi: 10.1101/gr.140269.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Buchold G.M., Coarfa C., Kim J., Milosavljevic A., Gunaratne P.H., Matzuk M.M. Analysis of MicroRNA Expression in the Prepubertal Testis. PLoS ONE. 2010;5:e15317. doi: 10.1371/journal.pone.0015317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Gonçalves T.F., Piergiorge R.M., dos Santos J.M., Gusmão J., Pimentel M.M.G., Santos-Rebouças C.B. Network Profiling of Brain-Expressed X-Chromosomal MicroRNA Genes Implicates Shared Key MicroRNAs in Intellectual Disability. J. Mol. Neurosci. 2019;67:295–304. doi: 10.1007/s12031-018-1235-7. [DOI] [PubMed] [Google Scholar]
- 200.Johnnidis J.B., Harris M.H., Wheeler R.T., Stehling-Sun S., Lam M.H., Kirak O., Brummelkamp T.R., Fleming M.D., Camargo F.D. Regulation of progenitor cell proliferation and granulocyte function by microRNA-223. Nature. 2008;451:1125–1129. doi: 10.1038/nature06607. [DOI] [PubMed] [Google Scholar]
- 201.Neudecker V., Haneklaus M., Jensen O., Khailova L., Masterson J.C., Tye H., Biette K., Jedlicka P., Brodsky K.S., Gerich M.E., et al. Myeloid-derived miR-223 regulates intestinal inflammation via repression of the NLRP3 inflammasome. J. Exp. Med. 2017;214:1737–1752. doi: 10.1084/jem.20160462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Calvente C.J., Del Pilar H., Tameda M., Johnson C.D., Feldstein A.E. MicroRNA 223 3p Negatively Regulates the NLRP3 Inflammasome in Acute and Chronic Liver Injury. Mol. Ther. 2020;28:653–663. doi: 10.1016/j.ymthe.2019.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Bauernfeind F., Rieger A., Schildberg F.A., Knolle P.A., Schmid-Burgk J.L., Hornung V. NLRP3 Inflammasome Activity Is Negatively Controlled by miR-223. J. Immunol. 2012;189:4175–4181. doi: 10.4049/jimmunol.1201516. [DOI] [PubMed] [Google Scholar]
- 204.Haneklaus M., Gerlic M., O’Neill L.A.J., Masters S.L. miR-223: Infection, inflammation and cancer. J. Intern. Med. 2013;274:215–226. doi: 10.1111/joim.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Yuan X., Berg N., Lee J.W., Le T.-T., Neudecker V., Jing N., Eltzschig H. MicroRNA miR-223 as regulator of innate immunity. J. Leukoc. Biol. 2018;104:515–524. doi: 10.1002/JLB.3MR0218-079R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Finnerty J.R., Wang W.X., Hébert S.S., Wilfred B.R., Mao G., Nelson P.T. The miR-15/107 group of microRNA genes: Evolutionary biology, cellular functions, and roles in human diseases. J. Mol. Biol. 2010;402:491–509. doi: 10.1016/j.jmb.2010.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Wang W.X., Danaher R.J., Miller C.S., Berger J.R., Nubia V.G., Wilfred B.S., Neltner J.H., Norris C.M., Nelson P.T. Expression of miR-15/107 family microRNAs in human tissues and cultured rat brain cells. Genom. Proteom. Bioinform. 2014;12:19–30. doi: 10.1016/j.gpb.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Wang W.-X., Wilfred B.R., Madathil S.K., Tang G., Hu Y., Dimayuga J., Stromberg A.J., Huang Q., Saatman K.E., Nelson P.T. miR-107 Regulates Granulin/Progranulin with Implications for Traumatic Brain Injury and Neurodegenerative Disease. Am. J. Pathol. 2010;177:334–345. doi: 10.2353/ajpath.2010.091202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Kataoka Y., Takeichi M., Uemura T. Developmental roles and molecular characterization of a Drosophila homologue of Arabidopsis Argonaute1, the founder of a novel gene superfamily. Genes Cells. 2001;6:313–325. doi: 10.1046/j.1365-2443.2001.00427.x. [DOI] [PubMed] [Google Scholar]
- 210.Bernstein E., Kim S.Y., Carmell M.A., Murchison E.P., Alcorn H., Li M.Z., Mills A.A., Elledge S.J., Anderson K.V., Hannon G.J. Dicer is essential for mouse development. Nat. Genet. 2003;35:215–217. doi: 10.1038/ng1253. [DOI] [PubMed] [Google Scholar]
- 211.Alisch R.S., Jin P., Epstein M., Caspary T., Warren S.T. Argonaute2 Is Essential for Mammalian Gastrulation and Proper Mesoderm Formation. PLoS Genet. 2007;3:e227. doi: 10.1371/journal.pgen.0030227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Calin G.A., Dumitru C.D., Shimizu M., Bichi R., Zupo S., Noch E., Aldler H., Rattan S., Keating M., Rai K., et al. Frequent deletions and down-regulation of micro- RNA genes miR15 and miR16 at 13q14 in chronic lymphocytic leukemia. Proc. Natl. Acad. Sci. USA. 2002;99:15524–15529. doi: 10.1073/pnas.242606799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Calin G.A., Sevignani C., Dumitru C.D., Hyslop T., Noch E., Yendamuri S., Shimizu M., Rattan S., Bullrich F., Negrini M., et al. Human microRNA genes are frequently located at fragile sites and genomic regions involved in cancers. Proc. Natl. Acad. Sci. USA. 2004;101:2999–3004. doi: 10.1073/pnas.0307323101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Zhang L., Huang J., Yang N., Greshock J., Megraw M.S., Giannakakis A., Liang S., Naylor T.L., Barchetti A., Ward M.R., et al. microRNAs exhibit high frequency genomic alterations in human cancer. Proc. Natl. Acad. Sci. USA. 2006;103:9136–9141. doi: 10.1073/pnas.0508889103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Kwanhian W., Lenze D., Alles J., Motsch N., Barth S., Döll C., Imig J., Hummel M., Tinguely M., Trivedi P., et al. MicroRNA-142 is mutated in about 20% of diffuse large B-cell lymphoma. Cancer Med. 2012;1:141–155. doi: 10.1002/cam4.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sethupathy P., Borel C., Gagnebin M., Grant G.R., Deutsch S., Elton T.S., Hatzigeorgiou A.G., Antonarakis S.E. Human microRNA-155 on chromosome 21 differentially interacts with its polymorphic target in the AGTR1 3’ untranslated region: A mechanism for functional single-nucleotide polymorphisms related to phenotypes. Am. J. Hum. Genet. 2007;81:405–413. doi: 10.1086/519979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.SanGiovanni J.P., SanGiovanni P.M., Sapieha P., De Guire V. miRNAs, single nucleotide polymorphisms (SNPs) and age-related macular degeneration (AMD) Clin. Chem. Lab. Med. 2017;55:763–775. doi: 10.1515/cclm-2016-0898. [DOI] [PubMed] [Google Scholar]
- 218.Meola N., Gennarino V.A., Banfi S. microRNAs and genetic diseases. PathoGenetics. 2009;2:7. doi: 10.1186/1755-8417-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Willemsen M.H., Vallès A., Kirkels L.A.M.H., Mastebroek M., Loohuis N.O., Kos A., Wissink-Lindhout W.M., de Brouwer A.P.M., Nillesen W.M., Pfundt R., et al. Chromosome 1p21.3 microdeletions comprising DPYD and MIR137 are associated with intellectual disability. J. Med. Genet. 2011;48:810–818. doi: 10.1136/jmedgenet-2011-100294. [DOI] [PubMed] [Google Scholar]
- 220.Galea I., Bechmann I., Perry V.H. What is immune privilege (not)? Trends Immunol. 2007;28:12–18. doi: 10.1016/j.it.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 221.Rezai-Zadeh K., Gate D., Town T. CNS infiltration of peripheral immune cells: D-Day for neurodegenerative disease? J. Neuroimmune Pharmacol. 2009;4:462–475. doi: 10.1007/s11481-009-9166-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Gupta A., Pulliam L. Exosomes as mediators of neuroinflammation. J. Neuroinflamm. 2014;11:68. doi: 10.1186/1742-2094-11-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Pegtel D.M., Peferoen L., Amor S. Extracellular vesicles as modulators of cell-to-cell communication in the healthy and diseased brain. Philos. Trans. R. Soc. B Biol. Sci. 2014;369:20130516. doi: 10.1098/rstb.2013.0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Panaro M.A., Benameur T., Porro C. Extracellular Vesicles miRNA Cargo for Microglia Polarization in Traumatic Brain Injury. Biomolecules. 2020;10:901. doi: 10.3390/biom10060901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Hill A.F. Extracellular Vesicles and Neurodegenerative Diseases. J. Neurosci. 2019;39:9269–9273. doi: 10.1523/JNEUROSCI.0147-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Dutta S., Hornung S., Taha H.B., Bitan G. Biomarkers for parkinsonian disorders in CNS-originating EVs: Promise and challenges. Acta Neuropathol. 2023;145:515–540. doi: 10.1007/s00401-023-02557-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.