ABSTRACT
Background:
Depression associated with diabetes is one of major obstacles in diabetic patient management. This study aims to determine the prevalence of depression and its associated risk factors among diabetic patients of both types (I and II).
Materials and Methods:
A cross-sectional analytical study was conducted at Armed Forces Hospital, Southern Region, Kingdom of Saudi Arabia, among adult diabetic patients attending the diabetic center. An interview-validated questionnaire was utilized to collect data. It consists of three main parts: demographic data, diabetic assessment tool, and patient health questionnaire-9.
Results:
A total of 386 diabetic patients were included. The age of them ranged between 17 and 95 years with an arithmetic mean of 53.4 years and a standard deviation of ± 18.2 years. Almost two-thirds (62.2%) were males. The prevalence of depression among diabetic patients was 48.2%, mostly of mild (31.4%) or moderate severity (12.7%). Multivariate logistic regression analysis revealed that female diabetic patients were at almost double-fold risk of developing depression compared to males [adjusted odds ratio (AOR) =2.73, 95% confidence interval (CI): 1.70–4.38], P < 0.001. Also, type II diabetic patients were at almost double-fold risk of developing depression compared to type I diabetic patients (AOR = 2.07, 95% CI: 1.16–3.67), P = 0.013. Patients with history of any social issue with the family, relatives, or friends were at about three-fold risk of developing depression compared to those without such history (AOR = 3.45, 95% CI: 2.11–5.66), P < 0.001. Patients who reported compliance to diet were at higher risk for developing depression compared to their peers (AOR = 2.57, 95% CI: 1.25–5.28), P = 0.010, while those compliant to physical activity about 150 min/week or more were at significant lower risk to develop depression (AOR = 0.56, 95% CI: 0.35–0.89), P = 0.015. Patients with nephropathy or neuropathy were more likely to have depression compared to their counterparts (AOR = 2.52. 95% CI: 1.33–4.80, P = 0.005 and AOR = 1.80, 95% CI: 1.11–2.90, P = 0.016, respectively).
Conclusion:
Depression is a very prevalent problem affecting diabetic patients, particularly those of type II, female patients, and those with nephropathy or neuropathy. Therefore, regular screening of diabetic patients for depression and referral of severe cases to psychiatric care are highly warranted.
Keywords: Depression, diabetes, prevalence, risk factors, Saudi Arabia
Introduction
Depression associated with diabetes is one of major obstacles in diabetic patient management. In Saudi Arabia, the prevalence of depression and anxiety disorders in 2017 was nearly 4.5% and 4.3%, respectively (World Health Organization, 2017).[1] According to the Center of Disease Control and Prevention, people with diabetes are 2–3 times more likely to have depression than people without diabetes. Only 25% to 50% of people with diabetes who have depression get diagnosed and treated.[2]
The term diabetes mellitus describes diseases of abnormal carbohydrate metabolism that are characterized by hyperglycemia. It is associated with a relative or absolute impairment in insulin secretion, along with varying degrees of peripheral resistance to the action of insulin.[3]
In Saudi Arabia, the prevalence of diabetes in adults is 18.3% and the total cases of diabetes in adults are 4,275,200, as reported by International Diabetes Federation.[4]
Most of studies were conducted in Jazan region, Saudi Arabia, and there are limitations in studies conducted in Asir region. Despite Jazan and Asir from the same zone (southern region), the precise prevalence of depression among diabetic patients in Asir region is unknown; in addition to our aim in getting estimation of depression among our patients, we need to provide evidence for decision-makers to implement effective interventions, such as screening and educational programs and add psychiatric care to improve outcome in our diabetic center.
This study aims to determine the prevalence of depression and its associated risk factors among diabetic patients attending King Fahad Armed Forces Hospital (KFAFH), Southern Region, Saudi Arabia.
Materials and Methods
Cross-sectional analytical study design was conducted at KFAFH, Southern Region, Kingdom of Saudi Arabia (KSA). It is considered as one of the greatest medical organizations, provides medical and health services (curative, preventive, diagnostic) in all medical specialties for employees of the Ministry of Defense in Southern Region, in addition to being a reference hospital, receives critical cases transferred by the military hospitals from Sharurah, Najran, Jizan, as well as reception cases transferred from civilian hospitals in the region, and provides open-heart surgery services, kidney transplant, and all other medical specialties similar to other available hospitals in the southern region.[5]
Adult diabetic patients attending the diabetic center, KFAFH, Southern Region, throughout the study period provided that they had the eligibility criteria were invited to participate in the study. Inclusion criteria were adult patients (males or females and from all nationalities) with type 1 or 2 diabetes diagnosed more than 1 year ago, aged between 14 and 95 years, and capable of independent communication and giving informed verbal consent. Patients with gestational diabetes and history of psychiatric disease or on psychiatric medication diagnosed before diabetes were excluded.
Sample size was estimated using the Online Raosoft sample size calculator with the assumptions that the number of booking visits for both type 1 and type 2 of diabetes in diabetic center clinics per years is 6612 patients, the margin of error is 5%, the confidence level is 95%, and the response distribution is 50%. Accordingly, the estimated minimum required sample size was 364 patients.
At diabetic clinics in the KFAFH southern region diabetic center, the researcher chose the patients to answer the questionnaire depending on a convenience non-probability sampling technique.
An interview-validated questionnaire was utilized to collect data. It consists of three main parts: demographic data, diabetes assessment tool, and depression assessment tool (patient health questionnaire: tilized to collect data. chose the patients to answer the questionnaire dependber ofa few minutes and rapidly scored by the researcher.[6] Liu et al.[7] reported that PHQ-9 had a good internal consistency (α = 0.80) and test–retest reliability (intra-class correlation coefficient = 0.87). PHQ-9 has nine questions with a score ranging from 0 to 3 for each setting. The validated Arabic version was utilized in this study.[8] Patients who scored between 0 and 4 were considered having no depression, 5–9 having mild, 10–14 having moderate, 15–16 having moderately severe, and 20–27 having severe depression.[9]
The researcher sent the study proposal to the KFAFH-Southern Region ethical committee; then after getting the approval, the researcher got permission from the Diabetic Center director and participated patients through verbal consents, and the researcher explained the purpose of the study to all participants.
Statistical analysis
The data were collected and verified by hand and then coded before computerized data entry. The Statistical Package for Social Sciences (SPSS) software version 28.0 was used for data entry and analysis. Descriptive statistics [e.g. number, percentage, mean, range, standard deviation (SD)] and analytic statistics using Chi-square test and independent samples t-test were applied. Multivariate logistic regression analysis expressed as adjusted odds ratio (AOR) and its 95% confidence interval (CI) were adopted to control for confounders. P values <0.05 were considered as statistically significant throughout the study.
Results
A total of 386 Saudi diabetic patients were included in the study. Their demographic characteristics are summarized in Table 1. Their age ranged between 17 and 95 years with an arithmetic mean of 53.4 years and an SD of ±18.2 years. Almost two-thirds (62.2%) were males. The majority of them (80.9%) were currently married and having children (81.1%). Only 14% were employed, whereas 45.8% were unemployed. Regarding their educational level, only 15.5% were college/higher educated. Most of them (45.4%) reported a monthly income of 5000 SR or less.
Table 1.
Demographic characteristics of the participants
| Frequency | Percentage | |
|---|---|---|
| Gender | ||
| Male | 240 | 62.2 |
| Female | 146 | 37.8 |
| Age in years | ||
| Range | 17-95 | |
| Mean±standard deviation | 53.4±18.2 | |
| Marital status | ||
| Single | 60 | 15.5 |
| Married | 312 | 80.9 |
| Divorced/separated | 4 | 1.0 |
| Widowed | 10 | 2.6 |
| Having children | ||
| Yes | 313 | 81.1 |
| ≤5 | 113 | 36.1 |
| >5 | 200 | 63.9 |
| No | 73 | 18.9 |
| Occupation | ||
| Employed | 54 | 14.0 |
| Unemployed | 177 | 45.8 |
| Retired | 155 | 40.2 |
| Educational level | ||
| No Formal education | 87 | 22.5 |
| Primary school | 71 | 18.4 |
| Intermediate school | 59 | 15.3 |
| Secondary school | 109 | 28.3 |
| College/higher | 160 | 15.5 |
| Income (Saudi Riyals/month) | ||
| ≤5000 | 175 | 45.4 |
| 5000-10000 | 134 | 34.7 |
| >10000 | 77 | 19.9 |
Previous history of visiting a psychiatrist or psychologist was mentioned by 10.9% of the participants. Almost one-third of them (36.8%) had someone at home to take care of them. Histories of having any social issue with family, relatives, or friends and family history of depression, anxiety, or stress were reported by 31.6% and 17.9% of them, respectively. Current or ex-smoking states were reported by 6.5% and 3.9% of the participants, respectively. More than one-third of them (38.1%) were obese [body mass index (BMI) ≥30 kg/m2] and 31.7% had a high blood pressure (≥140/90 mm/Hg) [Table 2].
Table 2.
Social, psychiatric, and medical characteristics of the participants
| Frequency | Percentage | |
|---|---|---|
| Previous history of visiting a psychiatrist or psychologist | ||
| No | 344 | 89.1 |
| Yes | 42 | 10.9 |
| Before one month | 7 | 16.6 |
| Before 6 months | 1 | 2.4 |
| More than 6 months | 34 | 81.0 |
| Have someone at home to take care of you | ||
| No | 244 | 63.2 |
| Yes | 142 | 36.8 |
| Have any social issue with your family, relatives, or friends | ||
| No | 264 | 68.4 |
| Yes | 122 | 31.6 |
| Family history of depression, anxiety, or stress | ||
| No | 317 | 82.1 |
| Yes | 69 | 17.9 |
| Smoking status | ||
| Non-smoker | 246 | 89.6 |
| Current smoker | 25 | 6.5 |
| Ex-smoker | 15 | 3.9 |
| Body mass index (kg/m2) (n=378) | ||
| <18.5 | 10 | 2.6 |
| 18.5–24.9 | 94 | 24.9 |
| 25–29.9 | 130 | 34.4 |
| 30–34.9 | 103 | 27.2 |
| 35–39.9 | 32 | 8.5 |
| ≥40 | 9 | 2.4 |
| Blood pressure (mm/Hg) (n=378) | ||
| Normal <120/80 | 84 | 22.2 |
| Borderline 121/81-139/89 | 174 | 46.1 |
| High ≥140/90 | 120 | 31.7 |
Type 2 diabetes represented 78% of patients. The duration of diabetes exceeded 10 years among 62.8% of patients. The HBA1c level exceeded 9% among 30.1% of them. A combination of oral hypoglycemia drugs and insulin was used in the current management of diabetes among 43.8% of patients. Compliance to medication, diet, and physical activity about 150 min/week or more were reported by 19.4%, 12.7%, and 63.5% of the participants, respectively, Table 3.
Table 3.
Diabetes-related characteristics of the participants
| Frequency | Percentage | |
|---|---|---|
| Type of diabetes | ||
| Type 1 | 85 | 22.0 |
| Type 2 | 301 | 78.0 |
| Duration of DM (years) (n=384) | ||
| <1 | 7 | 1.8 |
| 1-10 | 136 | 35.4 |
| >10 | 241 | 62.8 |
| HBA1c level (n=375) | ||
| <7 | 59 | 15.7 |
| 7-9 | 203 | 54.2 |
| >9 | 113 | 30.1 |
| Current diabetes management | ||
| Oral hypoglycemic drugs. | 116 | 30.1 |
| Multiple daily insulin injections | 101 | 26.2 |
| Oral hypoglycemia drugs + insulin. | 169 | 43.8 |
| Compliance to medication | ||
| No | 311 | 80.6 |
| Yes | 75 | 19.4 |
| Compliance to diet | ||
| No | 337 | 87.3 |
| Yes | 49 | 12.7 |
| Compliance to physical activity about 150 min/week or more | ||
| No | 141 | 36.5 |
| Yes | 245 | 63.5 |
The commonest reported diabetic complications were erectile dysfunction among males (45.7%), peripheral neuropathy (34.7%), and diabetic retinopathy (28.5%) [Figure 1].
Figure 1.
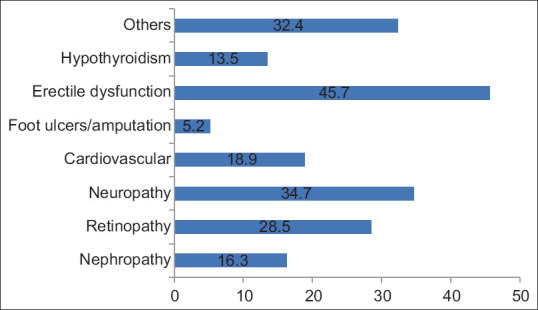
Diabetes complications among the participants
As demonstrated from Figure 2, the prevalence of depression among diabetic patients was 48.2%, mostly of mild (31.4%) or moderate severity (12.7%).
Figure 2.
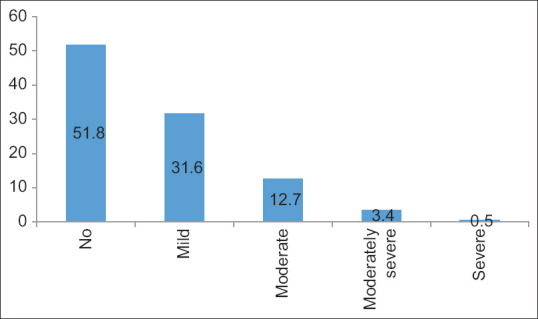
Prevalence and severity of depression among diabetic patients according to patient Health Questionnaire-9 (PHQ-9) tool
Female diabetic patients were more likely to have depression compared to male patients (61% vs 40.4%), P < 0.001. Patients who have children had a higher rate of depression compared to those without children (50.8% vs 37%), P = 0.033. Almost two-thirds (62.1%) of patients with no formal education compared to 41.7% of those with college/higher education expressed depression, P = 0.026. Other factors (age, marital status, number of children, occupation, and income) were not significantly associated with depression.
Patients with any social issue with the family, relatives, or friends were more likely to express depression compared to their peers (67.2% vs 39.4%), P < 0.001. Other studied factors (having someone at home to take care of patients, family history of depression, anxiety, or stress, smoking status, BMI, and blood pressure) were not significantly associated with depression among diabetic patients.
Type 2 diabetic patients were more likely to develop depression compared to type 1 diabetic patients (52.5% vs. 32.9%), P = 0.001. Almost two-thirds of patients who reported compliance with anti-diabetic medication or diet (62.7% and 65.3%, respectively) expressed depression compared to 44.7% and 45.7% of those who showed no compliance to medication and diet, respectively (P values were 0.005 and 0.010, respectively). Patients who did not show compliance to physical activity about 150 min/week or more were more likely to be depressed compared to their counterparts (61% vs 40.8%), P < 0.001. Diabetic patients with nephropathy (P < 0.001), neuropathy (P < 0.001), and other chronic diseases (P = 0.019) had a higher significant rate of depression compared to those without such complications. Other factors (duration of diabetes, HbA1c level, current diabetes management, retinopathy, cardiovascular diseases, diabetic foot, erectile dysfunction, and hypothyroidism) were not significantly associated with depression.
Multivariate logistic regression analysis revealed that female diabetic patients were at almost double-fold risk of developing depression compared to males (AOR = 2.73, 95% CI: 1.70–4.38), P < 0.001. Also, type 2 diabetic patients were at almost double-fold risk of developing depression compared to type I diabetic patients (AOR = 2.07, 95% CI: 1.16–3.67), P = 0.013. Patients with history of any social issue with their family, relatives, or friends were at about three-fold risk of developing depression compared to those without such history (AOR = 3.45, 95% CI: 2.11–5.66), P < 0.001. Patients who reported compliance to diet were at higher risk for developing depression compared to their peers (AOR = 2.57, 95% CI: 1.25–5.28), P = 0.010, while those compliant to physical activity about 150 min/week or more were at significant lower risk to develop depression (AOR = 0.56, 95% CI: 0.35–0.89), P = 0.015. Patients with nephropathy or neuropathy were more likely to have depression compared to their counterparts (AOR = 2.52. 95% CI: 1.33–4.80, P = 0.005 and AOR = 1.80, 95% CI: 1.11-2.90, P = 0.016), respectively. Patients’ history of having children, education, compliance to medications, and other chronic diseases were not significant associated with depression after controlling for confounding effect, Table 4.
Table 4.
Predictors of depression among diabetic patients: Multivariate logistic regression analysis
| B | SE | AOR | 95% CI | P | |
|---|---|---|---|---|---|
| Gender | |||||
| Malea | 1.004 | 0.241 | 1.0 | - -- | <0.001 |
| Female | 2.73 | 1.70-4.38 | |||
| Type of diabetes | |||||
| Type 1a | 0.726 | 0.293 | 1.0 | - -- | 0.013 |
| Type 2 | 2.07 | 1.16-3.67 | |||
| Have any social issue with your family, relatives, or friends | |||||
| Noa | 1.239 | 0.252 | 1.0 | - -- | <0.001 |
| Yes | 3.45 | 2.11-5.66 | |||
| Compliance to diet | |||||
| Noa | 0.943 | 0.368 | 1.0 | - -- | 0.010 |
| Yes | 2.57 | 1.25-5.28 | |||
| Compliance to physical activity about 150 min/week or more | |||||
| Noa | - 0.584 | 0.241 | 1.0 | - -- | 0.015 |
| Yes | 0.56 | 0.35-0.89 | |||
| Nephropathy | |||||
| Noa | 0.925 | 0.328 | 1.0 | - -- | 0.005 |
| Yes | 2.52 | 1.33-4.80 | |||
| Neuropathy | |||||
| Noa | 0.587 | 0.244 | 1.0 | - -- | 0.016 |
| Yes | 1.80 | 1.11-2.90 |
SE=Standard error, AOR=Adjusted odds ratio, CI=Confidence interval. a: Reference category; B: Slope. Terms of having children, education, compliance to medications, and other chronic diseases were not significant and removed from the final regression model
Discussion
Researchers from different countries have explored the association between depression and diabetes.[10,11,12,13,14] However, little is known about the magnitude of such association and its determinants among diabetic patients of both types in KSA, particularly in the Southern Region.
In the present study, the prevalence of depression among diabetic patients was 48.2%, mostly of mild (31.4%) or moderate severity (12.7%). This prevalence is comparable to what has been reported previously in Eastern province, Saudi Arabia (49.6%).[15] However, it is higher than those reported previously in other Saudi studies carried out in Arar (37%),[16] Al-Jouf Region (22.4%),[17] Jazan city (37.6% and 40.6%),[18,19] and Western Region (33.8%).[20]
Overseas studies showed variable results. Some of them reported prevalence rates comparable to what has been reported in the current study as those carried out in Qatar (52.5%),[21] Mexico (48.3%),[22] and Ethiopia (47%).[23] However, it is higher than those reported in Palestine (40%),[24] Philippines (18.2% and 31%),[25,26] United Arab of Emirates (12.5%),[27] and Germany (10.2%).[28] Comparison between the aforementioned studies either conducted locally, including the present one, or internationally should be taken with caution putting in consideration variations in the demographics of patients, conduction of the study among all diabetic patients or those of specific types, using different tools in defining depression and finally different cultures, even in the same country. However, the high rate of depression among diabetic patients reported in this study is not surprising as the link between depression and diabetes has been previously confirmed, despite being unclear. Different explanations have been mentioned in the literature, including the shared parallel biological processes that include insulin resistance, hypothalamic pituitary adrenal access, and circadian rhythm.[29] Additionally, diabetic care needs long life, careful eating style, checking blood glucose, hypoglycemic and hyperglycemic adverse symptom monitoring, regular exercise, and complication monitoring, which often impact badly the quality of life of patients with diabetes. All those needs could lead to depression among those patients.[16]
In accordance with others,[24,30,31,32,33,34,35,36] female diabetic patients were at higher risk of developing depression compared to males in this study. This could be explained by some factors such as lack of social support and being more sensitive constitutionally to adverse life events.[33,34]
In the present study, type 2 diabetic patients were at higher risk for developing depression compared to type I diabetic patients. This agrees with what has been reported by Gemeay EM et al. (2015) in Riyadh.[35] However, it contradicts what has been observed by others who indicated that depression was more reported among type 1 DM than type 2 DM patients.[16,36]
In the present study, patients with history of any social issue with their family, relatives, or friends were at higher risk of developing depression compared to those without such history. The same has been observed in other studies conducted in Saudi Arabia[16,37,38] and Jordan.[39]
Patients who reported compliance to diet were at higher risk for developing depression compared to their peers, while those compliant to physical activity about 150 min/week or more were at significant lower risk to develop depression. Compliance to diet might be associated with some degree of stress that might affect the psychological status of patients and leads to development of depression, while compliance to physical exercise has been proved by others to improve the psychological status of persons. Egede et al.[40] suggested that a decreased compliance to diet, exercise, and medication was associated with depression among diabetic adults. Also, Alhunayni NM et al. (2020) documented an association between depression and poor compliance with diet and physical activity,[16] and Al-Amer RA et al. (2011)[39] reported an association between depression and having poor compliance with diet among diabetics, while Salinero-Fort MA et al. (2018)[41] observed an association between low physical activity and a higher risk of depression among diabetic patients.
The current study revealed that patients with nephropathy or neuropathy were more likely to have depression compared to their counterparts. An association between development of diabetic complications in general and having depression has been documented in several studies as those patients need more care that affects their quality of life.[16,41,42] Furthermore, D’Amato C et al.[43] documented that pain of diabetic peripheral neuropathy was the most significant predictor of depression compared to other diabetes complications.
The present study is not without limitations, including its cross-sectional design, as the causal relationship between exposures and outcome cannot be established. Additionally, diagnosis of depression was not clinical as it depended on utilizing the PHQ-9 screening tool. Finally, it is a single-center study which could impact the generalizability of findings. Despite those limitations, the study is important from a public health point of view as it explored the magnitude and determinants of the association between diabetes and depression that might affect the glycemic control among affected diabetic patients.
Conclusion
Depression is a very prevalent problem affecting diabetic patients, particularly those of type 2. Additionally, female patients, those with history of any social issue with their family, relatives, or friends; those who reported compliance to diet; those not compliant to physical activity about 150 min/week or more; and patients with nephropathy or neuropathy were more likely to have depression compared to their counterparts.
Based on the study’s findings, the following are recommended:
Regular screening of diabetic patients for depression and referral of severe cases to psychiatric care.
Collaboration between diabetic team and psychiatric one as regards the management of diabetes including lifestyle modification
Particular attention should be given to high-risk groups including females and patients with diabetic complications
Further multi-centric study including diabetic patients from different disciplines is highly recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Depression and other common mental disorders. Geneva: WHO; 2017. [Google Scholar]
- 2.Center for Disease Control and Prevention (CDC) Diabetes and Mental Health. [[Last accessed on 2022 Sept 30]]. Available from: https://www.cdc.gov/diabetes/managing/mental-health.html .
- 3.American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S15–33. doi: 10.2337/dc21-S002. [DOI] [PubMed] [Google Scholar]
- 4.International Diabetes Fedaration (IDF) Diabetes Atlas. 2019. https://www.diabetesatlas.org/en/
- 5.Armed Forces hospital, Southern Region. Electronic services. Available at: https://www.afhsr.med.sa/!web/eserv_out.php .
- 6.Bartlett JE, Kotrlik JW, Higgins CC. Organizational Research: Determining Appropriate Sample Size in Survey Research. Inf Technol Learn Perform J. 2001;19:43–50. [Google Scholar]
- 7.Liu SI, Yeh ZT, Huang HC, Sun FJ, Tjung JJ, Hwang LC, et al. Validation of patient health questionnaire for depression screening among primary care patients in Taiwan. Compr Psychiatry. 2011;52:96–101. doi: 10.1016/j.comppsych.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 8.AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, et al. An Arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann Gen Psychiatry. 2017;16:32. doi: 10.1186/s12991-017-0155-1. doi: 10.1186/s12991-017-0155-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8:348–53. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mikaliūkštienė A, Žagminas K, Juozulynas A, Narkauskaitė L, Sąlyga J, Jankauskienė K, et al. Prevalence and determinants of anxiety and depression symptoms in patients with type 2 diabetes in Lithuania. Med Sci Monit. 2014;20:182–90. doi: 10.12659/MSM.890019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun N, Lou P, Shang Y, Zhang P, Wang J, Chang G, et al. Prevalence and determinants of depressive and anxiety symptoms in adults with type 2 diabetes in China: A cross-sectional study. BMJ Open. 2016;6:e012540. doi: 10.1136/bmjopen-2016-012540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tovilla-Zárate C, Juárez-Rojop I, Peralta Jimenez Y, Jiménez MA, Vázquez S, Bermúdez-Ocaña D, et al. Prevalence of anxiety and depression among outpatients with type 2 diabetes in the Mexican population. PLoS One. 2012;7:e36887. doi: 10.1371/journal.pone.0036887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Datta D. Prevalence and determinants of depression in type 2 diabetes patients: Problem in generalization. Indian J Med Res. 2011;133:555–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Bensbaa S, Agerd L, Boujraf S, Araab C, Aalouane R, Rammouz I, et al. Clinical assessment of depression and type 2 diabetes in Morocco: Economical and social components. J Neurosci Rural Pract. 2014;5:250–3. doi: 10.4103/0976-3147.133576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El Mahalli AA. Prevalence and predictors of depression among type 2 diabetes mellitus outpatients in eastern province, Saudi Arabia. Int J Health Sci (Qassim) 2015;9:119–26. [PMC free article] [PubMed] [Google Scholar]
- 16.Alhunayni NM, Mohamed AE, Hammad SM. Prevalence of depression among type-II diabetic patients attending the diabetic clinic at Arar National Guard Primary Health Care Center, Saudi Arabia. Psychiatry J 2020. 2020:9174818. doi: 10.1155/2020/9174818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alduraywish A, Abdel Fattah D, Abd-Eltawab A, Al-Ruwili M, Alhassan A, Alnafe N, et al. Depression and anxiety and their correlates in patients with diabetes mellitus in Al-Jouf Region, Saudi Arabia. Clinical Medicine and Diagnostics. 2017;7:48–56. [Google Scholar]
- 18.Albasheer OB, Mahfouz MS, Solan Y, Khan DA, Muqri MA, Almutairi HA, et al. Depression and related risk factors among patients with type 2 diabetes mellitus, Jazan area, KSA: A cross-sectional study. Diabetes Metab Syndr. 2018;12:117–21. doi: 10.1016/j.dsx.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Madkhali JM, Hakami AA, Dallak AH, Hakami RM, Yatimi AA, Hamdi ME, et al. Prevalence and associated factors of depression among patients with diabetes at Jazan province, Saudi Arabia: A cross-sectional study. Psychiatry J. 2019;2019:6160927. doi: 10.1155/2019/6160927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alzahrani A, Alghamdi A, Alqarni T, Alshareef R, Alzahrani A. Prevalence and predictors of depression, anxiety, and stress symptoms among patients with type II diabetes attending primary healthcare centers in the western region of Saudi Arabia: A cross-sectional study. Int J Ment Health Syst. 2019;13:48. doi: 10.1186/s13033-019-0307-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bener A, Abdulla Al-Hamaq AOA, Dafeeah E. High prevalence of depression, anxiety and stress symptoms among diabetes mellitus patient. Open Psychiatry J. 2011;5:5–12. [Google Scholar]
- 22.Tovilla-Zárate C, Juárez-Rojop I, Peralta Jimenez Y, Jiménez MA, Vázquez S, Bermúdez-Ocaña D, et al. Prevalence of anxiety and depression among outpatients with type 2 diabetes in the Mexican population. PLoS One. 2012;7:e36887. doi: 10.1371/journal.pone.0036887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Habtewold TD, Alemu SM, Haile YG. Sociodemographic, clinical, and psychosocial factors associated with depression among type 2 diabetic outpatients in Black Lion General Specialized Hospital, Addis Ababa, Ethiopia: A cross-sectional study. BMC Psychiatry. 2016;16:103. doi: 10.1186/s12888-016-0809-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sweileh WM, Abu-Hadeed HM, Al-Jabi SW, Zyoud SH. Prevalence of depression among people with type 2 diabetes mellitus: A cross sectional study in Palestine. BMC Public Health. 2014;14:163. doi: 10.1186/1471-2458-14-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Victoria GMB, Dampil AO. Prevalence of depression among patients with type 2 diabetes mellitus and its associated clinical factors. J ASEAN Fed Endocr Soc. 2019;34:197–203. doi: 10.15605/jafes.034.02.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nieva SJD, Capellan MLD, Montano CN. Prevalence and risk factors for depression among Filipino adults with diabetes mellitus type 2 at the Makati Medical Center Outpatient Department. Philipp J Int Med. 2017;55:1–10. [Google Scholar]
- 27.Sulaiman N, Hamdan A, Tamim H, Mahmood DA, Young D. The prevalence and correlates of depression and anxiety in a sample of diabetic patients in Sharjah, United Arab Emirates. BMC Fam Pract. 2010;11:80. doi: 10.1186/1471-2296-11-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kruse J, Schmitz N, Thefeld W German national health interview and examination survey. On the association between diabetes and mental disorders in a community sample: Results from the German national health interview and examination survey. Diabetes Care. 2003;26:1841–6. doi: 10.2337/diacare.26.6.1841. [DOI] [PubMed] [Google Scholar]
- 29.Moulton CD, Pickup JC, Ismail K. The link between depression and diabetes: The search for shared mechanisms. Lancet Diabetes Endocrinol. 2015;3:461–71. doi: 10.1016/S2213-8587(15)00134-5. [DOI] [PubMed] [Google Scholar]
- 30.Joseph N, Unnikrishnan B, Raghavendra Babu YP, Kotian MS, Nelliyanil M. Proportion of depression and its determinants among type 2 diabetes mellitus patients in various tertiary care hospitals in Mangalore city of South India. Indian J Endocrinol Metab. 2013;17:681–8. doi: 10.4103/2230-8210.113761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Amer RM, Sobeh MM, Zayed AA, Al-Domi HA. Depression among adults with diabetes in Jordan: Risk factors and relationship to blood sugar control. J Diabetes Complications. 2011;25:247–52. doi: 10.1016/j.jdiacomp.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 32.Kariri TA, Agili AO, Al-Hagawy AJ, Majrashi MA, Kariri SA, Kariri FA, et al. Depression among Saudi type 2 diabetic patients attending Samtah primary healthcare centers, Jazan Region, Saudi Arabia. World Journal of Pharmacy and Pharmaceutical Sciences. 2018;7(7):141–151. [Google Scholar]
- 33.Cols-Sagarra C, López-Simarro F, Alonso-Fernández M, Mancera-Romero J, Pérez-Unanua MP, Mediavilla-Bravo JJ, et al. Prevalence of depression in patients with type 2 diabetes attended in primary care in Spain. Prim Care Diabetes. 2016;10:369–75. doi: 10.1016/j.pcd.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 34.Krag MØ, Hasselbalch L, Siersma V, Nielsen AB, Reventlow S, Malterud K, et al. The impact of gender on the long-term morbidity and mortality of patients with type 2 diabetes receiving structured personal care: A 13 year follow-up study. Diabetologia. 2016;59:275–85. doi: 10.1007/s00125-015-3804-4. [DOI] [PubMed] [Google Scholar]
- 35.Gemeay EM, Moawed SA, Mansour EA, Ebrahiem NE, Moussa IM, Nadrah WO. The association between diabetes and depression. Saudi Med J. 2015;36:1210–5. doi: 10.15537/smj.2015.10.11944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hawamdeh S, Almakhzoomy I, Hayajneh Y. Screening and correlates of depression and HbA1 C in United Arab Emirates (UAE) women with diabetes. Perspect Psychiatr Care. 2013;49:262–8. doi: 10.1111/ppc.12013. [DOI] [PubMed] [Google Scholar]
- 37.Al-Mohaimeed AA. Prevalence and factors associated with anxiety and depression among type 2 diabetes in Qassim: A descriptive cross-sectional study. J Taibah Univ Med Sci. 2017;12:430–6. doi: 10.1016/j.jtumed.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Madkhali JM, Hakami AA, Dallak AH, Hakami RM, Yatimi AA, Hamdi ME, et al. Prevalence and associated factors of depression among patients with diabetes at Jazan province, Saudi Arabia: A cross-sectional study. Psychiatry J 2019. 2019:6160927. doi: 10.1155/2019/6160927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-Amer RM, Sobeh MM, Zayed AA, Al-Domi HA. Depression among adults with diabetes in Jordan: Risk factors and relationship to blood sugar control. J Diabetes Complications. 2011;25:247–52. doi: 10.1016/j.jdiacomp.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 40.Egede LE, Ellis C, Grubaugh AL. The effect of depression on self-care behaviors and quality of care in a national sample of adults with diabetes. Gen Hosp Psychiatry. 2009;31:422–7. doi: 10.1016/j.genhosppsych.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 41.Salinero-Fort MA, Gómez-Campelo P, San Andrés-Rebollo FJ, Cárdenas-Valladolid J, Abánades-Herranz JC, Carrillo de Santa Pau E, et al. Prevalence of depression in patients with type 2 diabetes mellitus in Spain (the DIADEMA Study): Results from the MADIABETES cohort. BMJ Open. 2018;8:e020768. doi: 10.1136/bmjopen-2017-020768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sachdeva S, Garg R, Kaur SP, Kathuria H, Gupta JK, Jindal A. To study the association of depression with complications of type 2 diabetes and to find qut any correlati on between type of complication and depression. Annals of International medical and Dental Research. 2016;2(6):55–58. [Google Scholar]
- 43.D'Amato C, Morganti R, Greco C, Di Gennaro F, Cacciotti L, Longo S, et al. Diabetic peripheral neuropathic pain is a stronger predictor of depression than other diabetic complications and comorbidities. Diab Vasc Dis Res. 2016;13:418–28. doi: 10.1177/1479164116653240. [DOI] [PubMed] [Google Scholar]


