Abstract
Objectives
The aim of this study was to examine the cumulative head acceleration event (HAE) exposure in male rugby players from the Under-13 (U13) to senior club level over 4 weeks of matches and training during the 2021 community rugby season.
Methods
This prospective, observational cohort study involved 328 male rugby players. Players were representative of four playing grades: U13 (N = 60, age 12.5 ± 0.6 years), U15 (N = 100, age 14.8 ± 0.9 years), U19 (N = 78, age 16.9 ± 0.7 years) and Premier senior men (N = 97, age 22.5 ± 3.1 years). HAE exposure was tracked across 48 matches and 113 training sessions. HAEs were recorded using boil-and-bite instrumented mouthguards (iMGs). The study assessed the incidence and prevalence of HAEs by ages, playing positions, and session types (match or training).
Results
For all age grades, weekly match HAE incidence was highest at lower magnitudes (10–29 g). Proportionally, younger players experienced higher weekly incidence rates during training. The U19 players had 1.36 times the risk of high-magnitude (> 30 g) events during matches, while the U13 players had the lowest risk compared with all other grades. Tackles and rucks accounted for the largest HAE burden during matches, with forwards having 1.67 times the risk of > 30 g HAEs in rucks compared with backs.
Conclusions
This study provides novel data on head accelerations during rugby matches and training. The findings have important implications for identifying populations at greatest risk of high cumulative and acute head acceleration. Findings may guide training load management and teaching of skill execution in high-risk activities, particularly for younger players who may be exposed to proportionally more contact during training and for older players during matches.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40279-023-01923-z.
Key Points
| Weekly exposure: For the highest age grade, matches accounted for 65% of the total weekly head acceleration events (HAEs); however, match contribution decreases steadily with age such that it was 56% in U19, 44% in U15 and just 41% in U13, likely reflecting the difference in match intensity with playing age and maturity. |
| HAE incidence: For all ages, HAEs of 10–29 g had the highest incidence rates (5–12 per player hour), whereas high magnitude (> 30 g) HAEs were rare (1–2 per week). For Premier and U19 players, > 30-g events were three times more likely to occur during matches rather than trainings. |
| Playing age: Compared with other grades, U19 players had the highest prevalence (> 60%) of high-magnitude (> 30 g) HAEs. This was attributed to the intensity of matches in the U19 ‘1st XV’ squads. Conversely, < 30% of U13 players experienced high-magnitude HAEs during match play. |
| HAEs by position: The weekly HAE incidence rate was higher for forwards compared with backs. The positional difference was largest at low magnitudes in older players for match exposure, with younger players (U13) showing no significant difference between positions. |
| Tackles and rucks: These accounted for over 80% of HAEs during matches. Forwards had a higher prevalence of > 30-g events in rucks but there were no positional differences in the tackle-related > 30-g events. |
Introduction
With over 9 million registered players in more than 120 countries, rugby is a popular and growing contact sport [1]. Growth has been attributed to the sport's increased media coverage, improved safety regulations, and development of community youth programmes [2]. In New Zealand, a country with a population of five million, the significant participation of 155,863 players in 2022 highlights the sport's popularity at the community level (NZR 2022 Player Database). While the growth of rugby at the youth and community levels presents an exciting opportunity for participation and engagement, addressing the potential safety concerns associated with the sport is crucial, and currently literature on the youth and community game is lacking.
The frequency of contact phases in rugby, such as tackles, rucks, scrums, mauls and lineouts, raises player safety concerns [3–5]. These phases often involve intense competition for ball possession, which can lead to a higher likelihood of unintentional head impact events and subsequently increase the risk of concussions for rugby players [3, 6]. In order to enhance player safety, it is essential to gain a comprehensive understanding of the contextual factors contributing to acute head injuries during contact phases [3]. On the other hand, recent insights have highlighted the potential influence of contact frequency on the brain injury threshold for contact sport athletes [7]. As a result, there is a growing emphasis on monitoring the severity of head impact events, especially those that do not immediately result in clinical outcomes, as a crucial aspect of player welfare strategies [8–11].
Head impact severity can be objectively described using linear and angular head kinematics to derive kinematic-based injury criteria or can serve as an input to finite element models that estimate the strain-based response of the brain tissue as a result of the impact event [12–14]. However, until recent advances in instrumented mouthguards (iMG), there have been limitations in the accuracy of on-field monitoring of head kinematics [15–17]. iMG technology provides a significant opportunity to monitor head kinematics because, in many countries, community rugby players are required or at least highly encouraged to wear mouthguards [18, 19]. In addition, iMG head kinematics can be obtained with greater accuracy compared with skin or helmet-mounted sensors, owing to improvements in the coupling of instrumentation to the athlete's skull via the dentition [15, 20]. This advancement allows practitioners and researchers to build longitudinal datasets of cumulative head acceleration event (HAE) exposures, providing critical insights into the potential relationships between day-to-day rugby head kinematic load and injury aetiology.
There has been little investigation into the frequency, magnitude, and distribution of HAEs sustained by junior and amateur male rugby players [8, 21]. Furthermore, no studies have investigated exposure to HAEs during training and no published studies have reported head kinematics in Under-13 (U13) to senior male community rugby grades. Therefore, this study was conducted to document the frequency and magnitude of HAEs in male rugby players from the U13 to Senior Premier club levels over 4 weeks of matches and training during the 2021 community rugby season. This study aimed to describe the HAE burden at different age levels and playing positions during match play and training.
In this manuscript, the authors focus on presenting data from the male participants in the ORCHID study, which is a larger research project investigating head acceleration events in over 700 community rugby players. The decision to subset the total project by sex was made due to substantial differences in exposure between male and female rugby players. By focusing solely on the male participants, the authors aim to provide a more detailed examination of head acceleration events within this particular subgroup of community rugby players. This approach allows analyses of the data in the appropriate exposure context, considering the unique characteristics and experiences of male rugby players, with a focus on playing grade/age.
Methods
Participants
This prospective observational cohort study examined HAE exposure by using iMGs in 328 male rugby players across 48 matches and 113 training sessions during the 2021 community rugby season. Participants were recruited from local clubs and schools, and represented the spectrum of community rugby where contact was permitted. Consenting players ranged in age from 10 to 30 years across the four playing grades (U13, U15, U19, and Senior Premier men). Parental/guardian assent was obtained for players younger than 16 years. The U13 and Premier grades comprised community-based club teams while the U15 and U19 grades comprised school-based teams. All the U19 teams, except one, were first-fifteens for their respective schools, which is the top-tier competition for secondary schools. The Premier (Prem) teams are considered the highest level of senior men’s (i.e., adult) amateur community rugby in NZ. All teams were recruited from the Dunedin metropolitan area of New Zealand and were members of the Otago Rugby Union. The population was representative of the cultural diversity within New Zealand, 58% (n = 186) identified as NZ European, 17% (n = 55) as Māori, 22% (n = 68) as Pasifika and 3% (n = 11) as other. Pasifika is a broad and diverse term that encompasses individuals from, or whose ethnic heritage links them to various Island nations and communities (e.g., Samoa, Tonga) in the South Pacific [22]. A detailed demographic breakdown is provided in Table 1. The study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki, and ethical approval was granted by the university human ethics committee (approval number H21/056).
Table 1.
Participant demographic details for all players (n = 328)
| Grade | Matches/trainings | Mean player mins/match Mean (SD) |
Mean player mins/training Mean (SD) |
Position | N | Age (y) |
Height (cm) |
Weight (kgs) |
Rugby experience (y) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||||
| U13 | 10/32 | 54.1 (8.6) | 64.3 (19.3) | Forwards | 28 | 12.4 | 0.3 | 161.8 | 7.9 | 63.0 | 15.9 | 6.0 | 2.6 |
| Backs | 32 | 12.4 | 0.6 | 159.0 | 8.3 | 48.4 | 7.7 | 6.6 | 2.4 | ||||
| U15 | 14/23 | 61.9 (16.2) | 70.8 (19.6) | Forwards | 56 | 14.8 | 0.6 | 178.7 | 7.0 | 85.1 | 18.1 | 8.1 | 3.2 |
| Backs | 44 | 14.9 | 0.7 | 175.8 | 5.8 | 69.8 | 10.4 | 9.0 | 2.9 | ||||
| U19 | 13/29 | 59.3 (20.3) | 63.6 (17.3) | Forwards | 43 | 16.7 | 1.1 | 182.4 | 6.0 | 98.7 | 16.0 | 9.9 | 2.7 |
| Backs | 35 | 17.0 | 0.6 | 178.6 | 6.2 | 79.3 | 9.4 | 10.0 | 3.7 | ||||
| Premier | 11/29 | 68.5 (24.6) | 70.6 (11.6) | Forwards | 52 | 23.1 | 3.4 | 185.4 | 6.0 | 107.5 | 11.6 | 15.2 | 4.8 |
| Backs | 45 | 22.1 | 2.7 | 181.8 | 5.3 | 89.0 | 8.1 | 14.7 | 3.5 | ||||
The total sample population was n = 328. Fifteen players played across both the U15 and U19 grades, their demographic data is included in each cohort. One player in the U15 grade played in two teams; his demographic details are only included once in the U15 cohort. Seven players did not report their playing position (U13 n = 5; U15 n = 2); their data is not reported in the table
Study Equipment
A qualified dentist fitted each athlete with a boil-and-bite iMG (Prevent Biometrics®, MN, USA) to maximise coupling to the dentition of the player. The iMG has an embedded proximity sensor that detects the coupling quality with the dentition and tracks the 'on-tooth' time. It is further equipped with a 3.2 kHz triaxial accelerometer and gyroscope to capture linear and angular kinematics and has been validated in the laboratory and field [16, 17, 23]. The precision of the mouthguard in detecting true on-field impact events in male professional rugby league players was reported at 89% (CI 87–92) [16].
All rugby sessions were video recorded with two high-definition cameras from the side-on and end-on field angles. For matches, the referees wore a head-mounted GoPro (Hero8, GoPro Inc., USA) at a third angle. The camera video footage was synced and imported into Hudl Sportscode (v 11, Agile Sports Technologies Inc., NB, USA), along with an XML file containing all iMG event data for the respective match or training. The iMG trigger threshold was set at 5 g on a single axis, with a 50-ms sampling window [24]. The iMG data were then time synchronised to the Sportscode timeline using the time flashes captured in the video. The unique serial number for each iMG was then matched to the corresponding player’s jersey number.
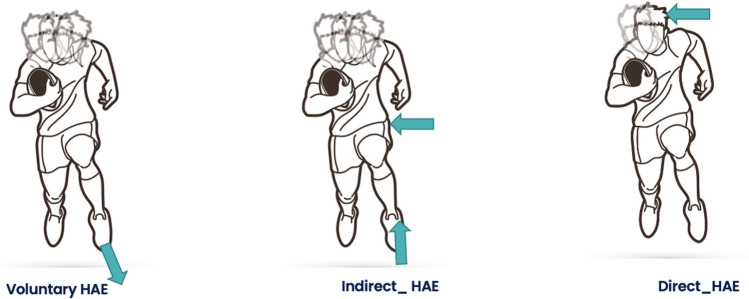
HAEs were video verified as direct, indirect, or voluntary events (Fig. 1) by a trained analyst and confirmed by a second reviewer [25]. Events were labelled as ‘unclear’ when the reviewer could not confirm the HAE mechanism because the event occurred off-camera or was obscured from camera view. As per CHAMP recommendations, all raw acceleration waveforms associated with verified and unclear events were inspected for signal quality prior to inclusion in the final dataset [26].
Fig. 1.
Schematic of the three types of head acceleration events (HAEs): voluntary, indirect and direct (L–R). A voluntary HAE (left) is generated through an individual’s self-acceleration or deceleration events such a running, changing direction or jumping. An indirect HAE (middle) is generated when contact is made with the player’s body resulting in an inertial loading of the head. Lastly, a direct HAE (right) is caused by direct contact with the head
While all match data were video verified, it was impossible to video verify all training data. This was due to a range of logistical issues around training sessions such as poor pitch lighting at night, fewer camera angles and player adherence to bib/jersey numbers. Therefore, temporospatial data windowing was performed to identify HAEs. Temporospatial windowing involves the temporal alignment of proximity data from the iMG, with temporal timestamps of HAEs and the temporal window of block-coded training events (Supplementary Fig. 1, see electronic supplementary material [ESM]) [27].
Data Reduction and Processing
All post-processing and data reduction were performed using purpose-written MATLAB routines (R2021b, MathWorks Inc., California, USA). The raw linear acceleration and angular velocity data from the iMG accelerometer and gyroscope were imported into MATLAB and filtered using a 200 Hz low-pass fourth-order Butterworth filter [28]. The filtered data were then transformed into the head centre of mass (COM). The location and coordinate system for the head COM were defined as either the 50th or 5th centile male based on the Hybrid III crash test anatomical model [29, 30]. The 5th centile was used for athletes who fit within the 5th centile of the population by height and weight. All other athletes were treated as 50th centiles.
Statistical Analysis
Incidence was calculated for each player based on the exposure type and time normalised to 60 min (E1). Player exposure time (in minutes) was extracted from the video footage for each instrumented player. Weekly incidence was calculated as HAE exposure over three units (two trainings and one match) of player exposure (E2). The relative risk that a player would experience a high-magnitude HAE was calculated and compared between grades and playing positions (RR, E3) [31]. The threshold for high-magnitude HAE was taken as the cohort median peak linear acceleration (PLA) plus interquartile range (IQR) (i.e., 75th centile) for direct HAEs (Supplementary Table 1, see ESM), based on the rationale that direct contact mechanisms carry a higher risk of injury.
| 1 |
| 2 |
| 3 |
Demographic details, including age, height, weight, and years of rugby experience, are reported using the mean and standard deviation (SD). Statistical analyses were conducted using R (v 4.0.3; R_Core_Team 2015) and MATLAB (alpha p ≤ 0.05). Inter-rater agreement was evaluated for verifying HAE events as either Yes/No or event type Direct/Indirect with Cohen's kappa. Owing to evidence of overdispersion from residual analyses, negative binomial regression was used to model the counts of impacts at or above each threshold from 5 to 40 g for linear acceleration (in 1-g increments), with log-time (match or training) included as an offset. Position (forward or back), grade (U13, U15, U19, or Prem), and session type (match or training) were included, along with three- and two-way interactions. Crossed random effects accommodated repeated measures for the players, teams, and matches.
Results
Over the 2021 season, 328 male players across the four grades wore iMGs during a combined total of 48 matches and 113 training sessions. Thirteen players played in both U15 and U19 grades, leading to a total sample of 341 player matches (U13, n = 60; U15, n = 100; U19, n = 78; Prem, n = 97). A total of 17,865 HAEs were captured throughout the study. Of the total events, 1820 were removed, 95 contained errors indicative of sensor malfunction (Supplementary Fig. 3, see ESM), and 1725 were < 5 g, leaving the remaining 16,450 events for the analysis. The inter-rater agreement for verification of HAEs as 'yes/no' was κ = 0.873 (95% CI 0.824–0.923) and as 'direct/indirect' was κ = 0.826 (95% CI 0.781–0.870). The cohort median PLA for direct events was 26.3 g (SD 0.5), which was rounded to 30 g for RR analysis.
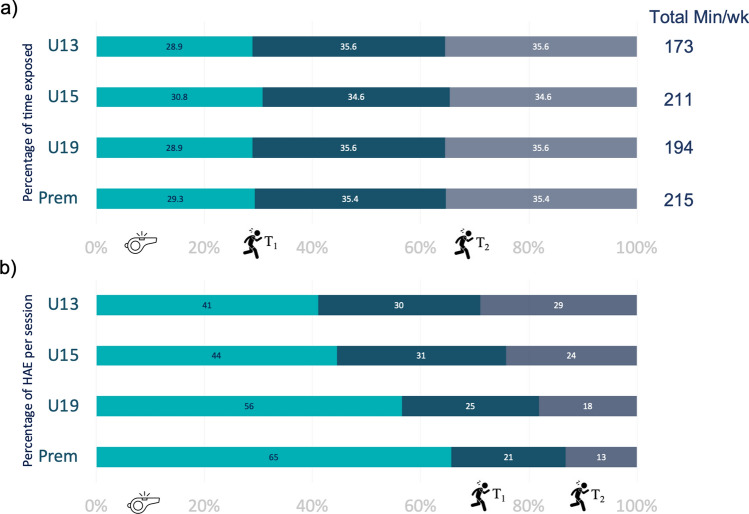
Weekly Exposure
A typical week for the included community rugby players consisted of two training sessions and a weekend match. As shown in Fig. 2a, the training-time to match-time ratio was similar across all playing grades, with approximately 30% of the total exposure occurring during the match and 70% during the two training sessions. The proportion of HAE counts between training and matches differed between the grades (Fig. 2b). Matches accounted for 65% of the HAEs in Prem, with significantly smaller proportions of HAEs occurring during matches as the age/grade decreased (Fig. 2b).
Fig. 2.
Snapshot of weekly rugby exposure per playing grade by a time exposure and b head acceleration event (HAE) exposure. A typical week was defined by one match (turquoise) and two trainings—T1 (teal) and T2 (grey). Prem Premier, U13 Under-13, U15 Under-15, U19 Under-19
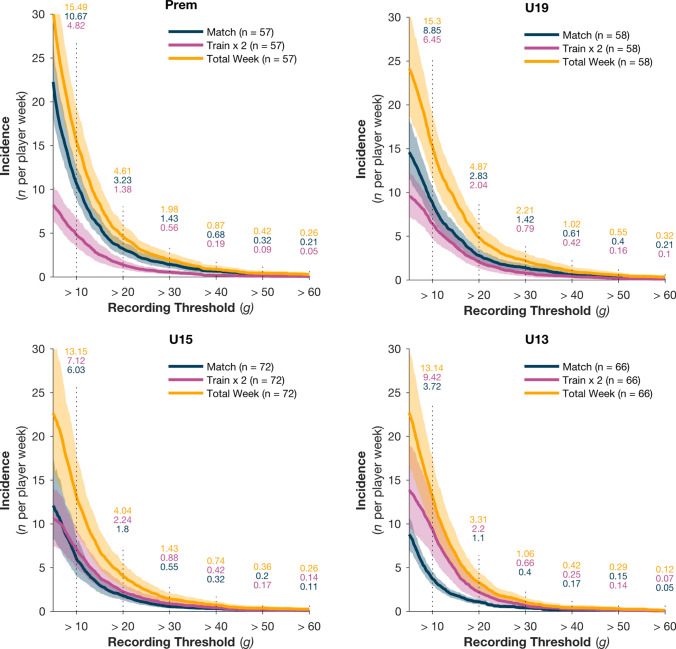
The cumulative weekly incidence rates (IR) by session type are presented in Fig. 3a–d. The general incidence pattern of HAE exposure was similar for all grades. HAE incidence was significantly higher at lower magnitudes. For example, IR 10–29 g was 6–8 times higher than IR 30–60 g (Table 2). Additionally, a significant interaction (χ2 = 14.24, p = 0.003) between grade and session type was observed at lower HAE magnitudes, and became less evident at higher magnitudes (> 30 g) (Fig. 3a–d). The Prem group had a higher incidence of HAE exposure during matches than during training (z = 3.796, p = 0.003), with the opposite pattern observed in the U13s, who had a higher incidence of HAEs during training sessions (z = 3.404, p = 0.019).
Fig. 3.
Cumulative head acceleration event (HAE) incidence rate per player week for one match (blue), two training sessions (purple) and combined (yellow) across four playing grades: Premier (Prem), Under-19 (U19), U15 and U13 (a–d, respectively). The solid line represents the mean incidence rate and shading represents the 95% confidence interval. HAE incident rates per peak linear acceleration magnitude band (10–60 g) are indicated by the numbers above each vertical line
Table 2.
Incident rates, player prevalence and relative risk ratios for HAEs in matches and trainings across the four player grades
| Player grade | Match events | Training events | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Weekly incidence rate | Prevalence | Relative risk (RR) 30–60 g | Weekly incidence rate | Prevalence | Relative risk (RR) 30–60 g | |||||||
| 10–29 g | 30–60 g | 30–60 g (%) | RR | 95% CI | p-Value | 10–29 g | 30–60 g | 30–60 g (%) | RR | 95% CI | p-Value | |
| U13 | 3.32 | 0.40 | 28 | 0.56 | 0.38–0.83 | 0.003 | 8.76 | 0.66 | 36 | 0.86 | 0.33–1.38 | 0.547 |
| U15 | 5.48 | 0.55 | 47 | 0.99 | 0.77–1.28 | 0.971 | 6.24 | 0.88 | 42 | 1.39 | 0.89–2.06 | 0.155 |
| U19 | 7.43 | 1.42 | 63 | 1.36 | 1.08–1.70 | 0.008 | 5.66 | 0.79 | 35 | 0.83 | 0.49–1.36 | 0.447 |
| Premier | 9.24 | 1.43 | 58 | 1.19 | 0.92–1.53 | 0.178 | 4.26 | 0.56 | 41 | 1.02 | 0.64–1.63 | 0.917 |
Significant values are indicated in bold
It is noteworthy that in the older grades, the 30–60 g IR for two training exposures was 0.4–0.5 times that of the single match exposure (Table 2). An adult player may experience approximately two 30–60 g events per week, but the likelihood of having such an event during training is low (Fig. 3). We also note that the youngest grades had the lowest 30–60 g IR, while U19 and Prem were similar. The prevalence of 30–60 g was highest in U19 during the match sessions, and the RR indicates their 30–60 g exposure was 1.36 times that of the rest of the population (Table 2). U13 players were least likely to experience high magnitude HAEs during matches (RR 0.56, 95% CI 0.58–0.83).
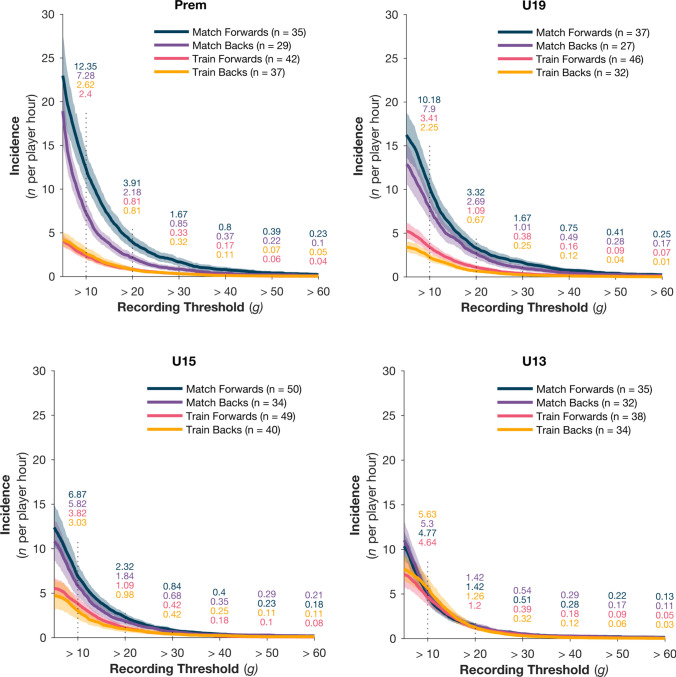
Exposure by Playing Position
Figure 4a–d show the per-hour IR comparisons for forwards and backs during the training and match sessions. There was evidence of significant three-way interactions (X2 = 729.1, p < 0.001) at lower magnitudes, the evidence and magnitude of this effect diminished when higher magnitudes (> 30 g) were used. This interaction indicates that the relationship between positions and sessions changes with playing age. For higher grades, forwards experienced higher IR in match sessions. The difference between positions and sessions diminished as age decreased. For the youngest grade and at lower magnitudes, the relationship between position and sessions is opposite to the Prem men, with backs having the highest IR (> 10 g) in training sessions. The IR became more similar for all combinations of position, grade, and session type as HAE magnitude increased. The risk ratio further indicated no significant difference in risk associated with playing position in either match (RR 1.139, CI 0.979–1.326; p = 0.0916) or training (RR 0.928, CI 0.786–1.095; p = 0.3775). Data pertaining to the angular acceleration can be found in the ESM (Supplementary Fig. 2).
Fig. 4.
Head acceleration event (HAE) incidence rate per player hour for match forwards (blue), match backs (purple), training forwards (pink) and training backs (yellow) across the four playing grades: Premier (Prem), Under-19 (U19), U15 and U13 (a–d, respectively). The solid line represents the mean incidence rate and shading represents the 95% confidence interval. HAE incident rates per peak linear acceleration magnitude band (10–60 g) are indicated by the numbers above each vertical line
Exposure by Contact Type
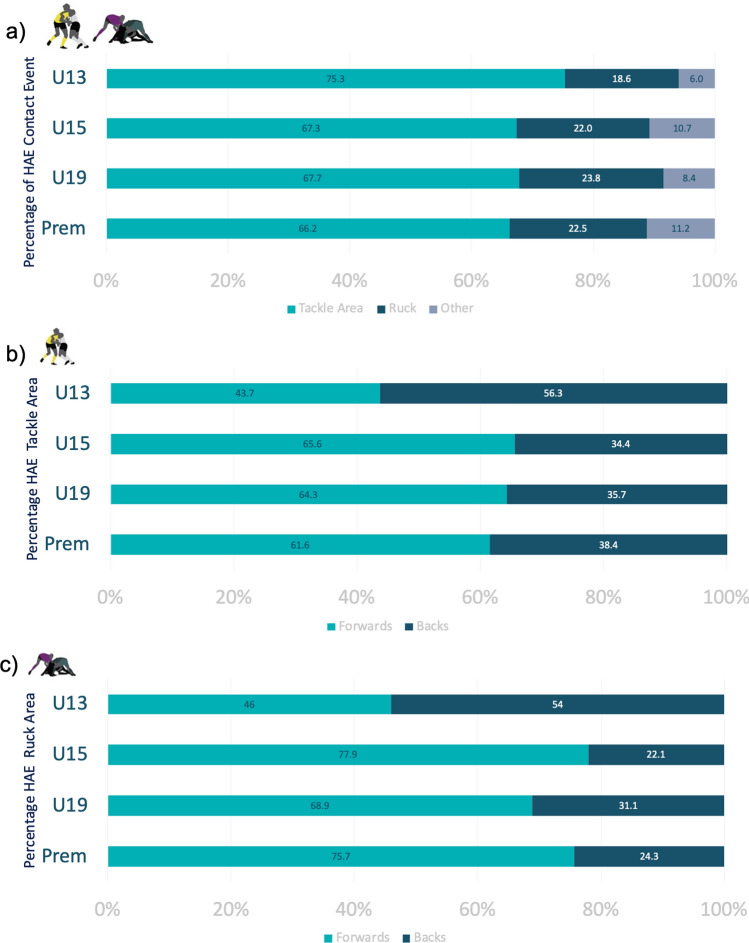
During matches, most HAEs occurred during tackles and rucks, with tackles accounting for more than 60% of HAEs per grade (Fig. 5a). The rotational acceleration of the head was similar across impact events for a given magnitude band (Table 3), except for Prem players, who had lower peak angular accelerations (PAAs) for high HAE magnitudes (> 50 g). Forwards accounted for a higher percentage of HAE exposures in tackles and rucks in all grades except U13 (Fig. 5b, c). Most significantly, compared with backs, forwards had 1.67 times the risk (RR 1.669, CI 1.148–2.425; p = 0.007) for > 30 g events in rucks but did not carry a higher risk for > 30 g events in tackles (RR 0.996, CI 0.90–1.102; p = 0.935).
Fig. 5.
Percentage of total head acceleration events (HAEs) by playing grade for a all match events, b tackle area and c rucks. The tackle area includes both the tackler and the ball carrier. Rucks were defined as a phase of play with one player on the ground and at least two opposing players engaged over them. Other events include scrum, lineouts, mauls and general play. Figs b and c compare forwards and backs. Prem Premier, U13 Under-13, U15 Under-15, U19 Under-19
Table 3.
Comparison of median peak angular acceleration (PAA) by peak linear acceleration (PLA) magnitude for match events (tackles, rucks, other) presented by playing grade
| Age grade | PLA (g) | PAA (rads/s2) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tackle area | Ruck area | Other | ||||||||
| Count | Median | IQR | Count | Median | IQR | Count | Median | IQR | ||
| U13 | 5–10 | 188 | 746.44 | (487.19) | 40 | 666.14 | (380.86) | 15 | 626.17 | (664.19) |
| 10–19 | 295 | 1210.60 | (849.07) | 90 | 1053.94 | (775.67) | 35 | 1304.80 | (939.11) | |
| 20–29 | 101 | 1951.84 | (1266.26) | 30 | 2076.77 | (1443.37) | 14 | 2370.71 | (877.51) | |
| 30–49 | 28 | 2594.66 | (1547.43) | 7 | 3389.08 | (2701.02) | 1 | 3188.37 | 0.00 | |
| 50 + | 27 | 5566.28 | (2134.74) | 5 | 6675.72 | (1711.52) | 1 | 4932.04 | 0.00 | |
| U15 | 5–10 | 196 | 747.05 | (372.65) | 54 | 627.65 | (357.97) | 51 | 647.67 | (534.27) |
| 10–19 | 580 | 1047.10 | (693.21) | 205 | 995.00 | (563.14) | 110 | 1258.35 | (1276.56) | |
| 20–29 | 229 | 1888.86 | (1171.60) | 70 | 1828.00 | (1261.86) | 33 | 2317.95 | (1171.73) | |
| 30–49 | 78 | 2761.08 | (1692.96) | 22 | 2440.20 | (1653.39) | 7 | 4514.77 | (3162.63) | |
| 50 + | 50 | 4968.66 | (2763.89) | 21 | 3636.90 | (2631.24) | 6 | 3555.43 | (2888.29) | |
| U19 | 5–10 | 165 | 666.06 | (385.86) | 40 | 665.51 | (241.81) | 32 | 455.24 | (447.87) |
| 10–19 | 470 | 1024.97 | (601.82) | 174 | 862.85 | (610.86) | 75 | 965.74 | (625.55) | |
| 20–29 | 149 | 1685.92 | (933.24) | 77 | 1659.02 | (1050.56) | 14 | 1415.38 | (678.31) | |
| 30–49 | 78 | 2721.21 | (1104.66) | 28 | 2213.46 | (1256.40) | 7 | 3140.48 | (2284.46) | |
| 50 + | 61 | 4511.63 | (2756.34) | 18 | 3603.15 | (2299.41) | 5 | 4954.29 | (2833.46) | |
| Premier | 5–10 | 116 | 635.78 | (371.16) | 35 | 575.06 | (217.74) | 50 | 516.80 | (556.43) |
| 10–19 | 475 | 966.17 | (540.97) | 186 | 892.62 | (564.32) | 84 | 928.39 | (622.58) | |
| 20–29 | 157 | 1651.14 | (825.03) | 59 | 1489.24 | (893.40) | 21 | 2050.43 | (889.29) | |
| 30–49 | 60 | 2356.03 | (1172.09) | 18 | 2114.49 | (1343.99) | 6 | 3748.60 | (1914.61) | |
| 50 + | 54 | 3945.17 | (2929.91) | 18 | 2992.87 | (2341.45) | 3 | 3567.56 | (1028.08) | |
Discussion
This study examines the head acceleration burden in community rugby over a 4-week playing period in playing grades from U13 to Prem men. Our results provide novel information on exposure to HAEs in community games, particularly concerning age and playing positions, with potential implications for training and match interventions to manage head impact burden in the sport.
Weekly Exposure
The time spent exposed to rugby was proportionally similar across the grades, with the match and each training session representing approximately one-third of the total exposure time. Although the proportional exposure time was similar between the grades, HAE distribution was not. Matches accounted for 41% of the week's HAE exposure in the youngest players (U13), and this increased with each successive grade, with the most significant proportion of HAEs during matches (65% of all HAEs) in Prem men.
This finding is important in three ways. First, it shows that per hour of rugby, matches are more likely to cause HAEs than training sessions, in all age grades. Second, the increase in match contribution with age reflects the relative increase in match intensity that occurs naturally with playing experience and physical development. This is supported by findings that match injury incidence increases with playing level and age [32]. Third, it may reflect differences in training approaches as age and overall season length increases. While the in-season competition period is similar across age grades (3–4 months), the pre-season training/preparation period varies from one week in U13 players up to 10 weeks in U19 and Prem players. Because older players have longer pre-season preparation, they can dedicate more training time in-season to tactical preparation. Hence, older players dedicated one training session per week to contact and one to tactical preparation, which was reflected in the percentage difference in HAEs between T1 and T2 for U19 and Prem. In contrast, as younger players have an overall shorter pre-season, they have more of a contact focus in both weekly training sessions and spend more time developing technical proficiency for contact in both sessions [33]. This difference in the training approach would expose younger players to cumulatively more contact during training sessions; thus, HAEs are relatively more likely to occur during training than matches in these groups. This may have implications for how the sport advises coaches on training focus and contact loads.
For the following discussion point, it may be helpful to introduce some context for the range and magnitude of HAEs. To begin, our video verification revealed interquartile ranges associated with direct (5–26 g), indirect (5–18 g) and voluntary (5–12 g) HAE mechanisms (Supplemental Table 2, see ESM). From the wider literature, HAEs up to 6 g have been reported on roller coasters [34], up to 10 g have been reported for trampolining [35], 10–19 g have been reported in women’s artistic gymnastics [36] and 20–30 g have been reported in automobile testing for rear impact collisions [37]. The automobile study noted that concussion risk in rear impact collisions of this magnitude was negligible [34], while recent iMG studies of American Football players identified HAEs associated with diagnosed concussion events that ranged between 40–150 g [11, 38]. With this context in mind, we would propose that HAEs < 29 g are low risk while events > 30 g carry higher potential for injury.
In our community rugby cohort, HAEs of 10–29 g occurred at 6–8 times the rate of 30–60 g events. The IR for > 30 g events ranged from 1/week in our youngest cohort to 2.2/week in the U19s. It is important to note that IRs represent an average per-player exposure and that HAEs are not necessarily spread evenly among the population [39]. For example, U19 and Prem had similar IRs for 30–60 g match events, yet 63% of U19 players were exposed to at least one 30–60 g event, compared with 58% of Prem players (Table 2). Therefore, the relative risk of experiencing a high-magnitude HAE is 1.36 times higher for an U19 player than for the rest of the playing population. This finding might also suggest that some Prem players experience a larger proportion of 30–60 g events relative to their cohort. Examining the techniques and behaviours of these ‘higher risk’ players may be warranted to determine the HAE aetiology.
The fact that school-based U19 players are more likely to experience at least one 30–60 g event during match play is consistent with previous studies that highlighted an increase in match injury rates in this population [40]. Our U19 cohort were recruited from ‘1st XVs’, which is the top tier for schoolboy rugby. Top tier schoolboy teams also have a higher level of professionalism and physical preparation, and attract a high level of community interest in spectator attendance and fanfare, which can significantly impact playing behaviour, leading to higher contact intensity, poorer decision making, and reduced focus on technique [41–43]. Larger urban schools may have paid professional coaches, dedicated strength and conditioning programmes, links to professional teams, and televised interschool matches [44]. The level of professionalism improves skill development and readiness to play but may have a negative consequence regarding game intensity [45]. Further examination of match events and mechanisms that lead to higher HAEs in U19 school-based players is required.
Exposure by Playing Position and Contact Type
Consistent with the previous literature, the weekly HAE exposure rate was higher for forwards than for backs [8, 21, 46–49]. This is likely the result of their greater exposure to contact events, since forwards typically make more tackles and carries, and are involved in more rucks than backs, and training activities will reflect these match demands.
The positional difference was largest at low magnitudes in older players for match exposure, with the position and session-type gap narrowing with decreasing age. Consequently, U13s had the opposite position incidence profile, with backs experiencing more HAEs in training sessions at lower magnitudes. The U13 backs also had a higher proportion of HAEs in the tackle (56%) and rucks (54%) than the U13 forwards. This discrepancy could reflect the lack of specialisation in positional play in the U13s, where player size, development, and skill level may be more significant factors for contact events [50]. The lack of positional specialisation could also explain the greater training exposure in U13s. In higher grades, training sessions involve ‘units’ where the drills will be specifically tailored to the match requirements of that position group. The lack of specialisation and increased attention on basic skills in U13s is the likely reason for the similar HAE incidence in U13 forwards and backs.
Apart from U13s, all grades had higher weekly numbers of 10–29 g events during match play than during training. During match play, the tackle was responsible for 66–75% of HAE exposure, with forwards contributing the highest proportion of those events (44–65%). Surprisingly, we found no difference in the prevalence of high-magnitude (30–60 g) tackle-related HAEs in forwards compared with backs. This finding may be incongruent with the current literature, which suggests that while forwards perform more 'heavy and severe' impacts than backs [51], backs have higher risk for tackle concussion injury due to larger tackle entry velocities [3]. The lack of positional differences in our sample could reflect a difference in player skill or athleticism at the community level compared with elite/professional games. However, further exploration of tackle-related HAEs in community games is necessary to provide deeper insights and context for these observations.
The ruck area was the second largest contributor (18–24%) to match HAEs, with forwards accounting for 46–78% of the burden depending on age grade. Moreover, forwards were significantly more likely than backs to experience a 30–60 g event in a ruck. It is well known that tackles and rucks carry the highest risk of injury and that players with more involvement in these events would likely also carry a higher risk of injury [3, 52]. Thus, our findings may suggest that in the community game, the back-row forwards carry a higher concussion risk in ruck events because these players are 'typically' the first to arrive at the breakdown [53]. There is some evidence in the professional and community adult grades supporting this supposition [53, 54]. However, future work will provide richer insights into the ruck and positional differences, to further elucidate whether the risk is due to player technique, player behaviour, rule enforcement, or intensity control.
Limitations
This study had several limitations. First, iMG fit quality may have differed between the grades. While smaller players were offered smaller-sized iMGs with a lower overall volume of material, obtaining optimal fit may still be difficult because younger players were more likely to have a narrow dental arch, triangular bite, and missing or misaligned teeth. Poorer iMG fit may lead to a higher volume of false and voluntary triggers of the iMG. We did all we could to mitigate the fit effect by having qualified dentists perform the iMG fitting and tracking the iMG-tooth displacement from the proximity sensor, which gave us a quality-of-fit score. Secondly, we could not fully video verify all training HAEs owing to poor video quality. Therefore, we relied on our impressions from the waveform data to distinguish between voluntary versus direct/indirect events. Furthermore, we could only confirm tackle- and ruck-related HAEs from the match sessions. We are currently working on optimisation techniques to be used in the future to elucidate tackle- and ruck-related events in the training sessions. Thirdly, we did not follow teams over the entire season because of time constraints and the large cohort of athletes we tracked. Instead, we chose to observe a minimum of 4 weeks of exposure time, meaning at least four matches and eight training sessions per team. The length of the observation period was controlled, but staggered by grade over the season. This means that some grades might have been captured at the beginning of the season and others near the end. Seasonal differences could affect the intensity of play or training, although the mixed-model procedure adopted in the analysis should accommodate these variations. Finally, our current study did not include information on concussions or other types of injuries, which may have important implications in injury identification, prevention and management. This will be the focus of future research.
Conclusions/Implications
The findings of this study have important implications for community rugby, particularly with respect to age, position, and session exposure. The results suggest that playing grade/age and position significantly influence HAE exposure incidence, with forwards experiencing the highest incidence, particularly during match play in tackle and ruck areas. Consequently, it may be prudent for community rugby coaches and referees to focus attention on tackle and ruck techniques, particularly in the U19 grades. A focus on managing the intensity of match play at higher grades in the school environment may also warrant further investigation. The study also found that the contribution of training sessions to weekly HAE exposure drastically diminished with age. This has important implications for how the sport guides training load, particularly for younger players where skill acquisition is still in the associative phase and coaching of close contact skills often takes priority over the strategy coaching that is often seen in older players. Youth community coaches may need to develop alternative approaches to coaching contact skills without full contact load.
This study provides new information on the exposure to HAEs in community rugby and marks the beginning of our investigation of this cohort. Clearly, there is a need for ongoing research to understand the mechanisms that lead to HAEs and develop targeted injury prevention strategies for high-risk players.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This study would not have been possible without the support of a number of organisations and individuals from the Dunedin community rugby family and all the players and coaches who participated in this study. Specifically, we would like to thank AG, HW, JJT, WW, TH and JP who aided with data collection and impact verification, DM, BRC, JM, and DT who assisted with the mouthguard fitting, and all other research assistants who aided in the data collection and video coding of the impact data used in this study. We would like to thank Otago Rugby Football Union for all their support of the project and assistance with team recruitment. We would like to thank Otago Polytechnic, HC, Elevate Analysis and AS for their support with video capture of trainings and matches and coding. We would also like to thank Prevent Biometrics, particularly AB and DG, for their support and cooperation.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Declarations
Author Contributors
MDB, DS, EF, and RT conceptualised the research project and designed the study. DS, JR, and MDB collected data for the study. All authors were responsible for analysis and interpretation of the results. MDB, DS and JR drafted the manuscript. All authors critically reviewed and edited the manuscript prior to submission.
Funding
World Rugby funded this project grant number 21392.
Data availability statement
Data are available on reasonable request to the corresponding author.
Ethics approval
This study involved human participants and was approved by Ethics name: University of Otago Human Ethics CommitteeID:H21_056UOHEC (Health) ID H21_056. Participants gave informed consent to participate in the study before taking part.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Competing interests
MDB has received research funding from World Rugby. JR is currently employed by New Zealand Rugby. RT is a consultant for World Rugby. DS was employed by New Zealand Rugby at the time of study and received research funding from World Rugby and is currently employed by World Rugby. EF is a consultant for World Rugby. PD and BN have no competing interests.
Equity, diversity, and inclusion statement
Our study was on male community rugby players in New Zealand. Our study included men and boys playing rugby at grassroots levels, mainly from the Otago region, and represent various cultural (NZ European, Māori, Pasifika and other Asian nations) and socioeconomic backgrounds. The research team included four women and three men (first and second authors are women). The authors’ disciplines include exercise science, physiotherapy, mechanical engineering, biomedical sciences and sports medicine.
References
- 1.WORLD RUGBY. Global Participation in Rugby [Internet]. Year in Review 2018. 2018. p. 1. Available from: https://www.world.rugby/organisation/about-us/annual-reports
- 2.Whitrow NPE, Hickey JM, Satterfield JW, Godfrey MG, Whitrow NPE, Hickey JM;, et al. Association of Marketing Theory and Practice Proceedings [Internet]. 2014. Available from: https://digitalcommons.georgiasouthern.edu/amtp-proceedings_2014/44
- 3.Tucker R, Raftery M, Kemp S, Brown J, Fuller G, Hester B, et al. Risk factors for head injury events in professional rugby union: a video analysis of 464 head injury events to inform proposed injury prevention strategies. Br J Sports Med. 2017;51:1152–1157. doi: 10.1136/bjsports-2017-097895. [DOI] [PubMed] [Google Scholar]
- 4.Archbold P, Rankin AT, Webb M, Davies R, Nicholas R, Eames NWA, et al. Injury patterns in U15 rugby players in Ulster schools: a rugby injury surveillance (RISUS) study. Transl Sports Med 2021;4:524–33. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/tsm2.248
- 5.Kemp SP, Brooks JH, Cross MJ, Morrow P, Williams S, Anstiss T, et al. England professional rugby injury surveillance project. 2015.
- 6.West SW, Starling L, Kemp S, Williams S, Cross M, Taylor A, et al. Trends in match injury risk in professional male rugby union: a 16-season review of 10 851 match injuries in the English Premiership (2002–2019): the Professional Rugby Injury Surveillance Project. Br J Sports Med [Internet]. 2021 [cited 2023 Feb 24];55:676–82. Available from: https://bjsm.bmj.com/content/55/12/676 [DOI] [PubMed]
- 7.Seifert J, Shah AS, Harezlak J, Rowson S, Mihalik JP, Riggen L, et al. Time delta head impact frequency: an analysis on head impact exposure in the lead up to a concussion: findings from the NCAA-DOD care consortium. Ann Biomed Eng. 2022;50:1473–1487. doi: 10.1007/s10439-022-03032-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King D, Hume PA, Brughelli M, Gissane C. Instrumented mouthguard acceleration analyses for head impacts in amateur rugby union players over a season of matches. Am J Sports Med. 2015;43:614–624. doi: 10.1177/0363546514560876. [DOI] [PubMed] [Google Scholar]
- 9.O’Connor KL, Rowson S, Duma SM, Broglio SP. Head-impact-measurement devices: a systematic review. J Athl Train. National Athletic Trainers’ Association Inc., 2017;206–27 [DOI] [PMC free article] [PubMed]
- 10.Wu L. Sports concussions: can head impact sensors help biomedical engineers to design better headgear? Br J Sports Med [Internet]. 2020 [cited 2022 Dec 12];54:370–1. Available from: https://bjsm.bmj.com/content/54/7/370 [DOI] [PubMed]
- 11.Bartsch AJ, Hedin D, Alberts J, Benzel EC, Cruickshank J, Gray RS, et al. High energy side and rear American football head impacts cause obvious performance decrement on video. Ann Biomed Eng. 2020;48:2667–2677. doi: 10.1007/s10439-020-02640-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhan X, Li Y, Liu Y, Domel AG, Alizadeh HV, Raymond SJ, et al. The relationship between brain injury criteria and brain strain across different types of head impacts can be different. J R Soc Interface. 2021;18:2. doi: 10.1098/rsif.2021.0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elkin BS, Gabler LF, Panzer MB, Siegmund GP. Brain tissue strains vary with head impact location: a possible explanation for increased concussion risk in struck versus striking football players. Clin Biomech. 2019;64:49–57. doi: 10.1016/j.clinbiomech.2018.03.021. [DOI] [PubMed] [Google Scholar]
- 14.Cecchi NJ, Domel AG, Liu Y, Rice E, Lu R, Zhan X, et al. Identifying factors associated with head impact kinematics and brain strain in high school American football via instrumented mouthguards. Ann Biomed Eng [Internet]. 2021 [cited 2023 Feb 13];49:2814–26. Available from: https://link.springer.com/article/10.1007/s10439-021-02853-5 [DOI] [PMC free article] [PubMed]
- 15.Wu LC, Nangia V, Bui K, Hammoor B, Kurt M, Hernandez F, et al. In vivo evaluation of wearable head impact sensors. Ann Biomed Eng. 2016;44:1234–1245. doi: 10.1007/s10439-015-1423-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones B, Tooby J, Weaving D, Till K, Owen C, Begonia M, et al. Ready for impact? A validity and feasibility study of instrumented mouthguards (iMGs). Br J Sports Med [Internet]. 2022;bjsports-2022–105523. Available from: https://bjsm.bmj.com/lookup/doi/10.1136/bjsports-2022-105523 [DOI] [PubMed]
- 17.Liu Y, Domel AG, Yousefsani SA, Kondic J, Grant G, Zeineh M, et al. Validation and Comparison of Instrumented Mouthguards for Measuring Head Kinematics and Assessing Brain Deformation in Football Impacts. Ann Biomed Eng [Internet]. 2020 [cited 2022 Feb 18];48:2580–98. Available from: https://link.springer.com/article/10.1007/s10439-020-02629-3 [DOI] [PMC free article] [PubMed]
- 18.Quarrie KL, Gianotti SM, Chalmers DJ, Hopkins WG. An evaluation of mouthguard requirements and dental injuries in New Zealand rugby union. Br J Sports Med. 2005;39:650–654. doi: 10.1136/bjsm.2004.016022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rugby Canada. rugby.ca Integrity ~ Respect ~ Solidarity ~ Passion ~ Discipline Rugby Canada AGE GRADE Law VARIATIONS FOR Community RUGBY.
- 20.Wu LC, Laksari K, Kuo C, Luck JF, Kleiven S, ‘Dale’ Bass CR,, et al. Bandwidth and sample rate requirements for wearable head impact sensors. J Biomech. 2016;49:2918–2924. doi: 10.1016/j.jbiomech.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 21.King D, Hume P, Gissane C, Clark T. Head impacts in a junior rugby league team measured with a wireless head impact sensor: An exploratory analysis. J Neurosurg Pediatr. 2017;19:13–23. doi: 10.3171/2016.7.PEDS1684. [DOI] [PubMed] [Google Scholar]
- 22.Treaty Resource Centre and Multicultural New Zealand. Multicultural New Zealand. 2016.
- 23.Kieffer EE, Begonia MT, Tyson AM, Rowson S. A two-phased approach to quantifying head impact sensor accuracy: in-laboratory and on-field assessments. Ann Biomed Eng. 2020;48:2613–2625. doi: 10.1007/s10439-020-02647-1. [DOI] [PubMed] [Google Scholar]
- 24.Wang T, Kenny R, Wu LC. Head impact sensor triggering bias introduced by linear acceleration thresholding. Ann Biomed Eng. 2021;49:2. doi: 10.1007/s10439-021-02868-y. [DOI] [PubMed] [Google Scholar]
- 25.Tierney G. Concussion biomechanics, head acceleration exposure and brain injury criteria in sport: a review. Sports Biomech. 2021;2:2. doi: 10.1080/14763141.2021.2016929. [DOI] [PubMed] [Google Scholar]
- 26.Rowson S, Mihalik J, Urban J, Schmidt J, Marshall S, Harezlak J, et al. Consensus head acceleration measurement practices (CHAMP): study design and statistical analysis. Ann Biomed Eng. 2022;50:1346–1355. doi: 10.1007/s10439-022-03101-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arbogast KB, Caccese JB, Buckley TA, McIntosh AS, Henderson K, Stemper BD, et al. Consensus head acceleration measurement practices (CHAMP): origins, methods, transparency and disclosure. Ann Biomed Eng. 2022;50:1317–1345. doi: 10.1007/s10439-022-03025-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bussey MD, Davidson P, Salmon D, Romanchuk J, Tong D, Sole G. Influence of the frame of reference on head acceleration events recorded by instrumented mouthguards in community rugby players. BMJ Open Sport Exerc Med. 2022;8:2. doi: 10.1136/bmjsem-2022-001365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bendjellal F, Oudenard L, Uriot J, Brigout C, Brun-Cassan F. Computation of Hybrid III Head Dynamics in Various Impact Situations. JOURNAL OF PASSENGER CARS. 1990.
- 30.Bartsch A, Samorezov S, Benzel E, Miele V, Brett D. Validation of an ‘intelligent Mouthguard’ Single Event Head Impact Dosimeter. SAE Technical Papers. 2014;2014-Novem. [DOI] [PubMed]
- 31.Kirkwood BR, Sterne JAC. Essential medical statistics. Medical statistics. 2003.
- 32.Viviers PL, Viljoen JT, Derman W. A review of a decade of rugby union injury epidemiology: 2007–2017. Sports Health. 2018;10:223–227. doi: 10.1177/1941738118757178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hendricks S. Trainability of junior Rugby Union players. South Afr J Sports Med. 2012;24:2. [Google Scholar]
- 34.Pfister BJ, Chickola L, Smith DH. Head motions while riding roller coasters: implications for brain injury. Am J Forensic Med Pathol [Internet]. 2009 [cited 2022 Oct 19];30:339–45. Available from: https://pubmed.ncbi.nlm.nih.gov/19901817/ [DOI] [PMC free article] [PubMed]
- 35.Sands WA, Kelly B, Bogdanis G, Barker L, Donti O, McNeal JR, et al. Comparison of bungee-aided and free-bouncing accelerations on trampoline. Science of Gymnastics Journal [Internet]. 2019;11:279–88. Available from: http://shura.shu.ac.uk/25705/
- 36.Pritchard NS, Urban JE, Miller LE, Lintner L, Stitzel JD. An analysis of head kinematics in women’s artistic gymnastics. Sci Gymn J. 2020;12:229–242. doi: 10.52165/sgj.12.3.229-242. [DOI] [Google Scholar]
- 37.Courtney A, Campbell IC, Courtney E, Pasquesi SA. Risk of concussion due to head acceleration in rear impact sled tests of passenger automobile seats. Traffic Inj Prev. 2018;19:S133–S135. doi: 10.1080/15389588.2018.1532200. [DOI] [PubMed] [Google Scholar]
- 38.Stemper BD, Shah AS, Harezlak J, Rowson S, Mihalik JP, Duma SM, et al. Comparison of head impact exposure between concussed football athletes and matched controls: evidence for a possible second mechanism of sport-related concussion. Ann Biomed Eng. 2019;47:2057–2072. doi: 10.1007/s10439-018-02136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nielsen RO, Debes-Kristensen K, Hulme A, Bertelsen ML, Møller M, Parner ET, et al. Are prevalence measures better than incidence measures in sports injury research? Br J Sports Med. 2019;2:2. doi: 10.1136/bjsports-2017-098205. [DOI] [PubMed] [Google Scholar]
- 40.Quarrie K, Gianotti S, Murphy I. Injury risk in New Zealand Rugby Union: a nationwide study of injury insurance claims from 2005 to 2017. Sports Med. 2020;50:22. doi: 10.1007/s40279-019-01176-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blascovich J, Mendes WB, Hunter SB, Salomon K. Social ‘facilitation’ as challenge and threat. J Pers Soc Psychol. 1999;77:25. doi: 10.1037/0022-3514.77.1.68. [DOI] [PubMed] [Google Scholar]
- 42.van Meurs E, Greve J, Strauss B. Moving in the presence of others–a systematic review and meta-analysis on social facilitation. Int Rev Sport Exerc Psychol. 2022;2:2. [Google Scholar]
- 43.Wallace HM, Baumeister RF, Vohs KD. Audience support and choking under pressure: a home disadvantage? J Sports Sci. 2005;23:2. doi: 10.1080/02640410400021666. [DOI] [PubMed] [Google Scholar]
- 44.Gall P, Leach M. Review of New Zealand secondary school rugby. New Zealand Rugby. 2019.
- 45.Broglio SP, Sosnoff JJ, Shin S, He X, Alcaraz C, Zimmerman J. Head Impacts During High School Football: A Biomechanical Assessment. J Athl Train [Internet]. 2009;44:342–9. Available from: http://meridian.allenpress.com/jat/article-pdf/44/4/342/1455615/1062-6050-44_4_342.pdf [DOI] [PMC free article] [PubMed]
- 46.Fuller CW, Taylor A, Raftery M. Epidemiology of concussion in men’s elite Rugby-7s (Sevens World Series) and Rugby-15s (Rugby World Cup, Junior World Championship and Rugby Trophy, Pacific Nations Cup and English Premiership) Br J Sports Med. 2015;49:478–483. doi: 10.1136/bjsports-2013-093381. [DOI] [PubMed] [Google Scholar]
- 47.King D, Hume PA, Clark T. Nature of tackles that result in injury in professional rugby league. Res Sports Med. 2012;20:86–104. doi: 10.1080/15438627.2012.660824. [DOI] [PubMed] [Google Scholar]
- 48.King D, Hume P, Gissane C, Clark T. Semi-professional rugby league players have higher concussion risk than professional or amateur participants: a pooled analysis. Sports Med. 2017;47:197–205. doi: 10.1007/s40279-016-0576-z. [DOI] [PubMed] [Google Scholar]
- 49.King DA, Hume PA, Gissane C, Clark TN. Similar head impact acceleration measured using instrumented ear patches in a junior rugby union team during matches in comparison with other sports. J Neurosurg Pediatr. 2016;18:65–72. doi: 10.3171/2015.12.PEDS15605. [DOI] [PubMed] [Google Scholar]
- 50.Durandt J, Hendricks S, Marshall M, Roux A, Hare E. Under-13 rugby: What are the issues? A panel discussion. South African Journal of Sports Medicine [Internet]. 2015 [cited 2023 Feb 20];27:63–6. Available from: http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S1015-51632015000300002&lng=en&nrm=iso&tlng=en
- 51.Paul L, Naughton M, Jones B, Davidow D, Patel A, Lambert M, et al. Quantifying collision frequency and intensity in rugby union and rugby sevens: a systematic review. Sports Med Open [Internet]. 2022 [cited 2023 Feb 13];8:12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/35050440 [DOI] [PMC free article] [PubMed]
- 52.Tierney GJ, Denvir K, Farrell G, Simms CK. The effect of tackler technique on head injury assessment risk in elite rugby union. Med Sci Sports Exerc. 2018;50:603–608. doi: 10.1249/MSS.0000000000001461. [DOI] [PubMed] [Google Scholar]
- 53.Roberts SP, Trewartha G, England M, Shaddick G, Stokes KA. Epidemiology of time-loss injuries in English community-level rugby union. BMJ Open [Internet]. 2013;3:3998. Available from: http://bmjopen.bmj.com/ [DOI] [PMC free article] [PubMed]
- 54.Roberts S, Trewartha G, England M, Goodison W, Stokes K. Epidemiology of head injuries in English community level rugby union. Br J Sports Med. 2014;48:25. doi: 10.1136/bjsports-2014-093494.252. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request to the corresponding author.