Abstract
This article aims to bridge existing knowledge gaps that impact clinical cardiovascular care and outcomes for women in Canada. The authors discuss various aspects of women’s heart health, emphasizing the efficacy of multidisciplinary care in promoting women’s well-being. The article also identifies the impact of national women’s heart health campaigns and the value of peer support in improving outcomes. The article addresses the particular risks that women face, such as pregnancy-related complications and hormone replacement therapy, all of which are associated with cardiovascular events, and highlights the differences in ischemic symptoms between men and women. Despite improvements in acute event outcomes, challenges persist in accessing timely ambulatory care, particularly for women. Canada has responded to these challenges by introducing Women Heart Programs, which offer tailored programs, support groups, and specialized testing. However, these programs remain few in number and are found only in urban settings. Overall, this review identifies sex and gender factors related to women’s heart health, underscoring the importance of specialized programs and multidisciplinary care in improving women’s cardiovascular health.
Graphical abstract
RÉsumÉ
Cet article vise à répondre aux incertitudes actuelles qui se répercutent sur les soins cardiovasculaires et les issues cliniques chez les femmes au Canada. Les auteurs abordent différents aspects de la santé cardiaque des femmes, mettant l’accent sur l’efficacité des soins multidisciplinaires pour améliorer le bien-être des femmes. L’article présente également l’effet des campagnes nationales sur la santé cardiaque des femmes et l’importance de l’entraide entre collègues pour améliorer les résultats. L’article traite des risques particuliers touchant les femmes, comme les complications liées à la grossesse et l’hormonothérapie substitutive, qui sont toutes associées à des événements cardiovasculaires, et il souligne les différences entre les hommes et les femmes pour ce qui est des symptômes ischémiques. Bien que des améliorations aient été observées quant à l’issue des événements aigus, des difficultés persistent sur le plan de l’accès rapide à des soins ambulatoires, surtout pour les femmes. Le Canada a répondu à ces difficultés en créant des programmes pour la santé cardiaque des femmes, qui offrent des services adaptés, des groupes de soutien et des analyses spécialisées. Cependant, ils sont encore peu nombreux et accessibles seulement en milieu urbain. Dans l’ensemble, cette analyse définit les facteurs liés au sexe et au genre qui interviennent dans la santé cardiaque des femmes, soulignant l’importance de mettre en place des programmes spécialisés et des soins multidisciplinaires pour améliorer la santé cardiovasculaire des femmes.
Lay Summary
This article highlights the importance of women’s heart programs and specialized care, along with national campaigns across Canada. The article also notes differences in symptoms between men and women during heart events. Although progress has been made, access to timely care, especially for women, remains a challenge.
Heart disease remains one of the leading causes of death in Canadian women.1 Each year, approximately 25,000 women lose their lives to heart disease, according to the most recent annual data from Statistics Canada.2,3 Despite this statistic, the prevalence of heart disease among women remains underappreciated, leading to underdiagnosis, undertreatment, and lack of awareness. In 2016, Garcia et al. highlighted the need for focused heart programs for women, to deliver comprehensive care.4 This article aims to identify a variety of factors related to women's heart health and the significance of specialized programs in addressing existing gaps in clinical cardiovascular care for women. The article highlights the crucial role and efficacy of multidisciplinary centres, including Women Heart Programs (WHPs), an inclusive term for Women Heart Centres (WHCs) and Women Heart Health Clinics (WHHCs); explains the current landscape of Canadian WHPs and the role of multidisciplinary care in women’s heart heath; examines the impact of national women's heart health campaigns that have stemmed from these programs; underscores the value of peer support; and explains the benefits of women-focused cardiac rehabilitation programs. This review identifies aspects of sex and gender that impact women’s heart health. Sex encompasses biological characteristics in humans, including chromosomes, gene expression, hormones, and reproductive anatomy.5 Gender, on the other hand, relates to socially constructed roles, behaviors, expressions, and identities attributed to individuals based on their assigned gender.5 Additionally, the article incorporates insights derived from the lived experiences of women, providing a comprehensive overview of the multifaceted dimensions of women's heart health. By investigating these critical elements, this review aims to examine how programs specializing in women’s heart health are helping to fill identified gaps in cardiovascular care for women.
Efficacy of Multidisciplinary WHPs
Multidisciplinary specialized cardiology clinics have demonstrated considerable efficacy in improving patient outcomes through the implementation of an integrated approach that encompasses effective education, counseling, and access to timely follow-up. Among these clinics, atrial fibrillation and heart function clinics have emerged as being particularly effective and extensively studied entities.6, 7, 8 A recent systematic review and meta-analysis by Gandhi et al. demonstrated that attendance at heart function clinics leads to significant reductions in heart failure hospitalization and all-cause mortality.9 Similarly, Gallagher et al. emphasized the benefits of an integrated approach in atrial fibrillation clinics, including a similar decrease in all-cause mortality and cardiovascular hospitalizations.10 Likewise, multidisciplinary cardiology clinics are beginning to show promise in improving outcomes for women. Our group recently reported the 1-year prospective data from The Women’s Heart Centre in Vancouver, British Columbia, indicating higher diagnostic accuracy, improved risk-factor management, and reduced angina hospitalization in women presenting with ischemia or myocardial infarction (MI) and no obstructive coronary artery disease (CAD; INOCA or MINOCA).11
Background Supporting the Need for Dedicated WHPs: Sex and Gender Differences in Cardiovascular Disease
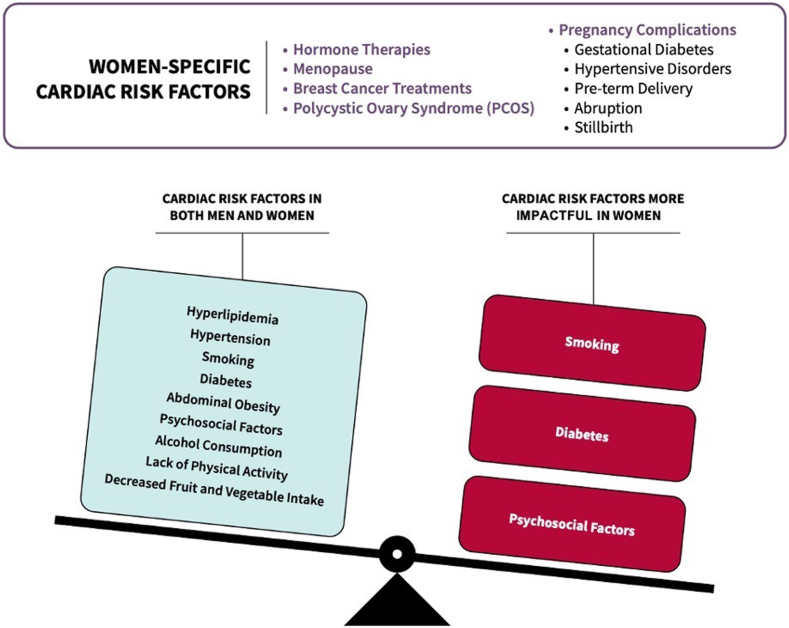
Sex- and gender-specific risk factors
Although traditional risk factors for CAD are common in both sexes, certain factors, such as diabetes, smoking, and psychosocial issues are stronger risk factors in women than in men.12 The INTERHEART study, encompassing 52 countries, identified 9 modifiable risk factors that accounted for over 90% of acute MI cases in both men and women, including abnormal lipids, hypertension, smoking, diabetes, abdominal obesity, psychosocial factors, minimal fruit and vegetable consumption, alcohol consumption, and lack of regular physical activity (Fig. 1).13 This study further described gender differences in MI risk factors. Former smoking posed a higher risk for men, whereas hypertension, diabetes, psychosocial factors, physical inactivity, and alcohol abstinence were more significant risk factors for women.13 Current evidence suggests that smoking and diabetes have more pronounced adverse effects in women, correlating strongly with coronary heart disease events and the occurrence of ST-elevation MI (STEMI).14,15 Depression and stress also detrimentally impact cardiovascular health, with women experiencing higher rates of depression, anxiety, and early life adversities, compared to those in men (Fig. 1).16,17 Psychosocial factors, including depression and work stress, increase the odds of MI by 3.5-fold in women, compared to a 2.6-fold increase in men, according to the INTERHEART study.13 Additionally, women face unique risk factors related to the effects of hormone therapy, pregnancy-related complications, including gestational diabetes and hypertensive disorders, as well as menopause (Fig. 1).18 Newer-generation oral contraceptives have been associated with an increased risk of adverse cardiovascular events, particularly in relation to blood pressure elevation, MI, and stroke.19 Pregnancy-related complications, such as gestational diabetes and hypertensive disorders, can double the risk of cardiovascular disease in women.20 Moreover, the risk of heart disease increases after a woman experiences menopause.21 Awareness of nontraditional sex-specific and sex-more-common risk factors has emerged over the past decade. In women, these include autoimmune disorders, preterm delivery, hypertensive pregnancy disorders, gestational diabetes mellitus, breast cancer treatments, migraines, and depression.18,22 Additionally, the prevalence and impact of traditional atherosclerotic cardiovascular disease (CVD) risk factors, such as diabetes mellitus, hypertension, dyslipidemia, smoking, obesity, and physical inactivity, are increasing among women.18 Ferry et al. also found that common symptoms hold more significant predictive value in women, compared to men, for MI, whether diagnosed using sex-specific or uniform criteria.23
Figure 1.
Cardiovascular risk factors among men vs women.
Presentation, including signs and symptoms
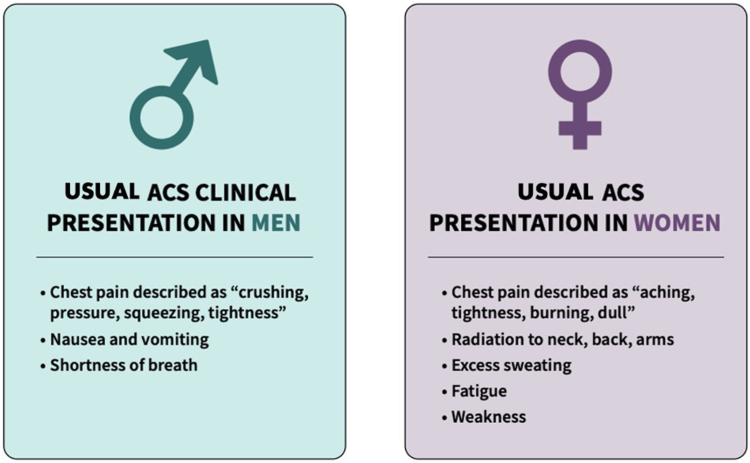
Atlhough symptoms of acute coronary syndrome (ACS) overlap for men vs women, specific differences do occur (Fig. 2).12 In a 2020 systemic review and meta-analysis, women were found to have higher odds of experiencing pain between the shoulder blades, nausea or vomiting, and shortness of breath, but lower odds of experiencing chest pain or diaphoresis, compared to men (Fig. 2).24 Similarly, in the Gender and Sex Determinants of Cardiovascular Disease: From Bench to Beyond Premature Acute Coronary Syndrome (GENESIS-PRAXY) study, which examined patients aged 18-55 years admitted to the hospital with ACS, a high proportion of both men and women experienced chest pain.25 However, women reported a higher occurrence of non-chest pain symptoms, such as nausea and neck pain.25 Similarly, the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) found that women were more likely to present with back, neck, and jaw pain, as well as palpitations, whereas men were more likely to report fatigue and weakness.26
Figure 2.
Acute coronary syndrome (ACS) clinical presentation in men vs women.
Chest pain remains the most prominent presentation for both men and women with CAD. However, women tend to describe their pain as “aching and tightness,” whereas men tend to describe it as “crushing and squeezing” (Fig. 2).27 Age also plays a significant role in the manifestation of symptoms at the time of ACS presentation. Another study conducted by Canto et al. observed that, among patients in the National Registry of Myocardial Infarction (NRMI), the proportion of chest pain reported by women was significantly lower compared to that reported by men, but this interaction was influenced by age.27 In the younger age group (≤ 45 years), a high percentage (85.8%) of women presented with chest pain, whereas in the older age group (≥ 75 years), only 51.3% of women experienced chest pain.27
WHPs hold significant potential to enhance cardiovascular healthcare for women by providing a multidisciplinary, holistic approach tailored to women's unique heart health needs. Focused on accurate screening and diagnosis, WHPs promote early detection of heart diseases through recognition of women-specific presentations and risk factors by trained heart health professionals.
Impact of CVD on women’s mental health
Robust evidence indicates an intimate connection between one’s mental health and one’s cardiovascular health through the “brain-heart axis,” as supported by a recent Scientific Statement by the American Heart Association.28 Negative mental health factors encompass depression, anxiety disorders, anger, and pessimism, which encompasses expressions of chronic stress and/or dissatisfaction with one’s life.28 An important point to note is that the diagnoses defined by the Diagnostic and Statistical Manual of Mental Disorders are reflective of chronic and debilitating effects of negative mental health on regular day-to-day functioning beyond what are considered “normal” fluctuations of mood within time- and culture-specific contexts. A summary of relative risk ratios of incident CVD by psychological status is provided in Table 1. Overall, women are twice as likely as men to be diagnosed with depression.29 Moreover, numerous studies suggest that women experiencing depression often exhibit greater symptom severity compared to that of their male counterparts.29,30
Table 1.
Effect estimates of psychological status on incident cardiovascular disease (CVD) in men
Across gendered factors, bidirectional relationships are well established between depression and CVD, through dysregulated inflammation and neuroendocrine signaling as a response to chronic stress,31,32 which can further manifest as metabolic disease over time (eg, hypertension, diabetes, and dyslipidemia).32,33 Negative behavioural coping mechanisms in response to stress, such as smoking, excess alcohol consumption, disordered eating patterns, and lack of exercise, further exacerbate associated cardiometabolic risk factors,32 although these behaviours and trait manifestations have been shown to differ by sex. This difference is exemplified by a recent study of over 26,000 Canadians demonstrating that women aged over 45 years with depression had significantly higher odds of ischemic heart disease, diabetes, hypothyroidism, and a higher waist-to-hip ratio than did nondepressed women, but these associations were not significantly different in depressed vs nondepressed men; in men, the only cardiometabolic trait significantly associated with depression was hypertension.34
In 2007, a report by the World Health Organization’s Women and Gender Equity Knowledge Network termed the “gendered structural determinants of health” that describe social determinants of health that affect outcomes of women at risk of or living with CVD.35 Under this paradigm, stressors that may instigate depressive and/or anxiety symptoms may be largely described as structural or situational, reflecting societal and cultural norms toward women at a given time. In a situational, individual context, examples of workplace stressors include high-level job strain (high level of work demands with low level of job control)36 and high-effort–low-reward dynamics, which are associated with a higher risk of depression and anxiety, and consequent higher risk for CVD; this pattern has been observed across income levels.
Recognizing the increased prevalence of depression and anxiety among women with heart disease, WHPs aim to address psychological stress by facilitating appropriate referrals to social support, psychological support, and/or other medical interdisciplinary expertise.
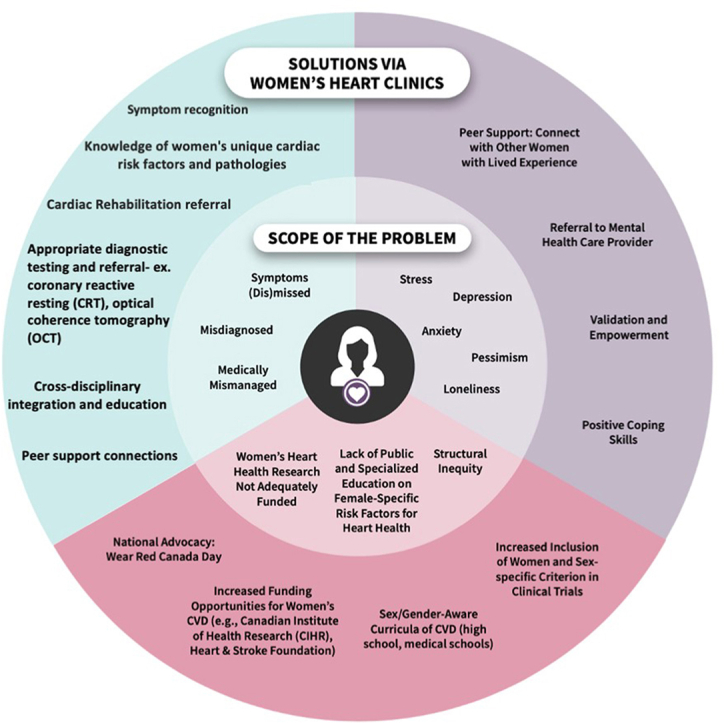
The Importance of a Dedicated WHP
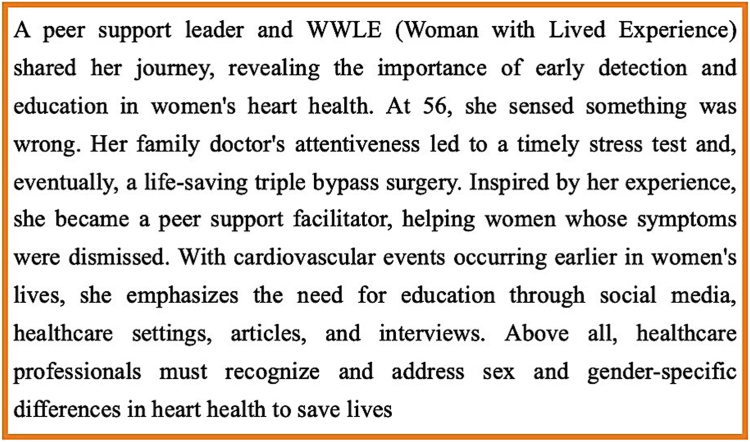
The role of a WHP in addressing cardiovascular health encompasses a focus on sex-specific cardiac risk factors, identification of unique clinical signs, symptoms, etiologies, and presentations in women, and access to specialized diagnostic procedures for entities such as INOCA and MINOCA. A WHP facilitates the provision of diverse and culturally appropriate expert care for CVDs commonly observed in women throughout their lifespan, extends this provision to encompass care for all genders, including transgender individuals, and supports the establishment of longitudinal research databases. Many women with lived experiences have shared the positive impact that a WHP has had in their lives (Fig. 3). This section further details the specifics of these specialized programs in the context of women's heart health.
Figure 3.
Insights from a woman with lived experience (WWLE).
WHP referral indications
WHPs offer comprehensive assessment and management tailored to the unique needs of women who are at risk of or living with heart disease. Referral indications to a WHP are diverse and encompass a spectrum of conditions. These indications include chest pain or MI with a normal traditional workup, palpitations, syncope, and cardiovascular risk factors such diabetes, hypertension, dyslipidemia, and obesity. WHPs serve as specialized centres where patients receive an initial consultation and follow-up, skillfully facilitated by either a nurse practitioner (NP) or a cardiologist, ensuring that women with various cardiac concerns or risk factors receive appropriate and personalized care.
How to assemble a WHP team
Assembling a proficient WHP team involves a careful approach to address the diverse and complex healthcare needs of women in relation to heart health. A well-rounded team typically includes the following: physicians with an interest in women’s heart health (i.e, cardiologists, internists); mental health practitioners (ie, psychiatrists, counselors, and/or psychologists); experts in cardio-oncology and cardio-rheumatology; professionals experienced in managing pregnancy-related disorders; and culturally and linguistically competent nursing and allied health professionals. The latter may include a dietician, a social worker, and an exercise physiologist. This multidisciplinary team composition is important in not only detecting women at risk but also effectively mitigating the onset of ischemic heart disease. Later in this article, we delve into the role of allied health in more detail.
Assessments performed
A comprehensive range of assessments is conducted to ensure a thorough evaluation of women's cardiovascular health. These assessments encompass a detailed symptom review, focused on recognizing any specific cardiac symptoms or concerns. Additionally, the team investigates sex-specific risk factors and risk factors that affect women more than men. The cardio-obstetric history assessment is a crucial component, delving into the cardiovascular aspects of pregnancy-related health, and psychological screening addresses mental health considerations. Furthermore, a gendered social determinants of health assessment considers the broader societal factors that influence women’s well-being. These comprehensive evaluations ensure that a WHP provides a holistic and tailored approach to caring for women's cardiovascular health, considering both physiological and psychosocial factors.
Common differential diagnoses
Within the scope of a WHP, healthcare professionals encounter a diverse range of differential diagnoses that demand specialized assessment and tailored care. Notably, INOCA emerges as a prominent concern, affecting primarily midlife women aged 45-65 years.37 INOCA's pathophysiology encompasses factors such as coronary microvascular dysfunction, coronary endothelial dysfunction, and epicardial vasospasm. Another notable diagnostic challenge seen commonly in WHPs is MINOCA. The etiology of MINOCA can be multifaceted, involving factors such as underlying plaque disruption, epicardial coronary vasospasm, occult microthrombi, spontaneous coronary artery dissection, and Takotsubo cardiomyopathy. Other entities commonly seen in WHPs are cardio-oncology diagnoses, assessment of cardiac disorders during or prior to pregnancy, and hormone-related issues in the context of CVD and/or cardiovascular risk. Within the specialized framework of a WHP, these gender-specific diagnoses receive evaluation and individualized management.
Specialized testing and interpretation of results
Nonobstructive syndromes, such as MINOCA and INOCA, are particularly common in women; MINOCA accounts for 6% of MI (10% in women), and INOCA accounts for up to two-thirds of invasive coronary angiograms in women with chest pain, more than half of whom will have abnormalities on invasive vasomotor testing.38, 39, 40
MINOCA and INOCA are underdiagnosed, and standard diagnostic tests for ischemic heart disease, including exercise stress testing, stress imaging, coronary computed tomography angiography (CCTA), and coronary angiography, have low sensitivity and specificity in these nonobstructive syndromes.41,42 WHPs with an interest in MINOCA and INOCA in women often offer specialized testing that is not available at general cardiology clinics. This testing includes invasive coronary reactivity testing, optical coherence tomography (OCT), positron emission tomography, and cardiac magnetic resonance imaging (CMR).43,44 In an international study of 170 women with MINOCA, 84.5% had a specific etiology diagnosed when OCT and CMR were reliably performed.45 In women with INOCA, up to two-thirds had evidence of coronary microvascular dysfunction during coronary reactivity testing using adenosine and acetylcholine.46
Treatments offered and follow-up
WHPs offer a comprehensive range of treatments and services tailored to address the unique cardiovascular needs of women. These services encompass risk-factor evaluation, counseling on family history, women-only exercise classes, and smoking-cessation treatment. Educational sessions are offered to enhance awareness and empower women with knowledge about heart health. Consultations with specialized healthcare professionals, such as dietitians, psychiatrists, and counselors, are available to address specific needs.
Moreover, WHPs offer primary and secondary prevention of CVD and serves as a resource for patients seeking second opinions, particularly those with persistent chest pain, prior MI with normal coronary arteries (indicating potential microvascular angina or coronary vasospasm), and undiagnosed or nonobstructive CAD. Patients are offered follow-ups and are connected to appropriate resources to optimize their hearth health.
Current Canadian WHPs
WHPs have gained recognition as crucial initiatives to address sex- and gender-based disparities in CVD outcomes.11,47 Initially regarded as mere trends, the intensifying evidence of increasing CVD morbidity and mortality among women necessitates specialized programs tailored to their unique cardiovascular needs.47 Approximately 50 WHPs exist globally, 6 of which are in Canada. These programs are often supported by charitable foundations, philanthropic entities, and industry sponsors, and they often go beyond routine heart disease prevention, diagnosis, treatment, and education.11
A recent prospective study conducted in Vancouver, British Columbia, demonstrated the positive impact of specialized WHP care for women with nonobstructive CAD.11 Significant improvements were observed in diagnosis, risk-factor management, angina control, quality of life, and mental health, along with a reduced number of emergency department visits and angina-related hospitalizations.11 Moreover, WHPs address heart conditions and risk factors that disproportionately impact women, such as adverse pregnancy outcomes, peripartum cardiomyopathy, polycystic ovary syndrome, menopause, and hormonal therapy.47,48 However, despite these promising outcomes, the availability of WHPs in Canada remains limited (Fig. 4). Expansion of WHPs across Canada is crucial to address the existing disparities in CVD outcomes among women.
Figure 4.
Distribution of the 6 Women’s Heart Centres across Canada.
Role of Multidisciplinary Care Providers in WHPs
Equipped with a diverse team of clinicians specializing in primary care, mental health practitioners, specialists in cardio-oncology, cardio-rheumatology, pregnancy-related disorders, cardio-oncology, and neurocognition, as well as culturally and linguistically competent nursing and allied health professionals, these centres are strongly positioned to detect women at risk and mitigate the onset of ischemic heart disease.49 In this section, we cover the roles of NPs and psychologists and psychiatrists in detail.
Role of NPs
NPs are common healthcare providers in Canadian WHPs who, in coordination with other team members, contribute to these goals. NPs are highly educated, often with doctorate-level preparation, and specialize in diagnosing, creating treatment plans, and prescribing for specific patient populations.50 They play a key role in enhancing outcomes for women at risk of CVD by focusing on primary prevention. By recognizing and addressing modifiable risk factors such as hypertension, dyslipidemia, diabetes, obesity, unhealthy dietary habits, lack of physical activity, and tobacco usage, NPs contribute to the prevention of heart disease in women. They can address these risk factors by considering both medical and social issues that may be barriers to patients.
Role of psychiatrists and psychologists
A chronic disease diagnosis can have varying effects on one’s mental health, for various reasons, such as perceived control over one’s clinical trajectory, knowledge and education about the disease, and perceived social support. Mental health trained professionals, such as specialized therapists, psychologists, and psychiatrists, form an integral component of the WHP care team for women living with CVD. Through varying degrees of training, these professionals enable a confidential space for patients to discuss strategies to address any stressors in their life—related to the diagnosis or not—that would impact their clinical trajectory and their long-term well-being. As each person brings unique life experiences to the table, these professionals counsel with personalized advice and support strategies tailored to address the patient’s living circumstances (eg, whether the patient is living alone or with any family members or friends, patients' working status, patients' degree of caregiving role, etc.) and complement any prior experiences and/or medications with mental health professionals (eg, considerations of previous trauma, cultural sensitivity, etc.). Considerations in choosing which mental health professional is best suited to help depend on factors such as cost (eg, out of pocket vs covered by provincial healthcare plans), type of support needed (eg, 1-1 support, group therapy, and/or medication), and type of specialized training, if warranted.
Research, Education, and Awareness Campaigns
Role of research
Historically, cardiovascular research has been focused predominantly on male participants, with women being significantly underrepresented. Even when women were included in clinical trials, their representation remained limited, accounting for only about one-third of participants, at most.51 Despite some improvements driven by federal mandates in the US since the 1990s, research on women’s heart health continues to lag and requires additional support. Notably, the sex-specific pathophysiology of heart disease, including cardiac remodelling and the presence of sex-specific thresholds for cardiac biomarkers such as troponin and natriuretic peptides, remains inadequately explained.52,53 Furthermore, medical therapies have been studied predominantly in men, leading to limited understanding of the variations in outcomes experienced by women after cardiovascular surgeries and interventions.54 Addressing these gaps is crucial to advancing our understanding of women’s heart health and improving their outcomes. Women’s heart health clinics afford the opportunity to combine research with clinical care and offer an opportunity for recruitment of study participants.
Fortunately, recent directives from Canadian granting agencies now require researchers to address sex and gender as biological and social variables in their applications. For example, the Canadian Institutes of Health Research have introduced guidelines requiring consideration of sex and gender in research studies, including for their Fellowship Awards. Similarly, the Heart and Stroke Foundation mandates that funding applicants indicate whether sex or gender, or both, are being considered in their research projects. These efforts reflect a growing recognition of the importance of incorporating sex and gender considerations into research and highlight the commitment to advancing women's heart health through increased funding and support.
The Canadian Women’s Heart Health Alliance conducted a national survey entitled "National Survey: Knowledge Gaps and Status of Existing Cardiac and/or Stroke-focused Research Programs That Incorporate Sex and Gender in Canada" to assess the current state of women’s heart health research across the country. The survey results revealed geographic gaps in representation and identified areas of research that present opportunities for future directions, knowledge translation strategies, and collaborations to strengthen women’s heart health initiatives in Canada.55 Lastly, innovative strides are being made in women’s heart programs as they increasingly embrace the future of research, incorporating cutting-edge technologies, such as machine learning and artificial intelligence.
Education and specialized training for working at WHPs in Canada
Becoming a specialist in women’s heart health requires additional years of training after a physician’s cardiology residency, known as fellowship years. In Canada to date, only the University of Ottawa Heart Institute with its Canadian Women’s Heart Health Centre has graduated its first women’s heart health cardiology fellow. In the US, several fellowship programs provide focused training in clinical, basic, and translational research in heart disease in women, and sex and gender differences in cardiovascular health. For example, the Cedars Sinai Barbra Streisand Women’s Heart Center, part of the Smidt Heart Institute, offers a 1-to-2–year fellowship known as the Barbra Streisand Women’s Heart Center Fellowship. In 2017, the Canadian Women’s Heart Health Centre published results identifying the need to increase knowledge regarding women’s heart health.55 To address this need, 9 educational modules were created targeting trainees and healthcare professionals within cardiology, general internal medicine, and emergency medicine.56 Moreover, modules were developed with the aim of teaching use in secondary schools. However, more efforts need to be made in providing further educational opportunities for physicians to learn about women’s heart health.
Moreover, NPs working at WHPs receive on-site education, mentorship, and training, progressing from novice to expert with guidance from cardiologists, senior NPs, and other interprofessional team members. Some sites offer formal fellowship opportunities established by the employer.
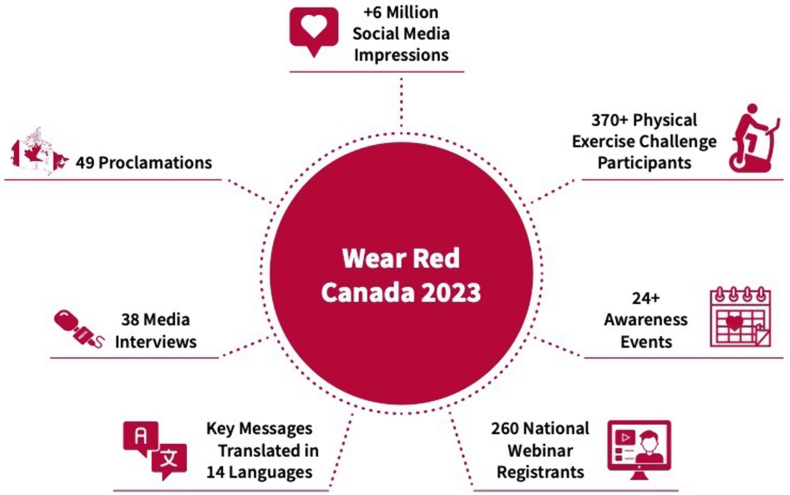
Role of advocacy, including Wear Red Canada
In both the US and Canada, organizations such as the National Institutes of Health (NIH), the American Heart Association (AHA) with its Go Red for Women campaign, and Canada’s Women’s Heart Health Alliance play crucial roles in advocating for women’s heart health. In Canada, women’s heart health campaigns, such as Wear Red Canada day (a national advocacy campaign held annually in February) emerged following a report in February 2018 entitled “Ms.Understood” by the Heart and Stroke Foundation of Canada. This report was focused on the 5 “unders” of women: under-aware, underdiagnosed, undertreated, undersupported, and underresearched. After this event, the Canada’s Women’s Heart Health Alliance Advocacy Task Force, supported by its members and WHPs across the country, translated this into an annual day of awareness nationally, initially in 2019, which has continued to grow in impact every year since (Fig. 5).
Figure 5.
Achievements and events of the annual Wear Red Canada 2023 campaign.
The Power of Peer Support
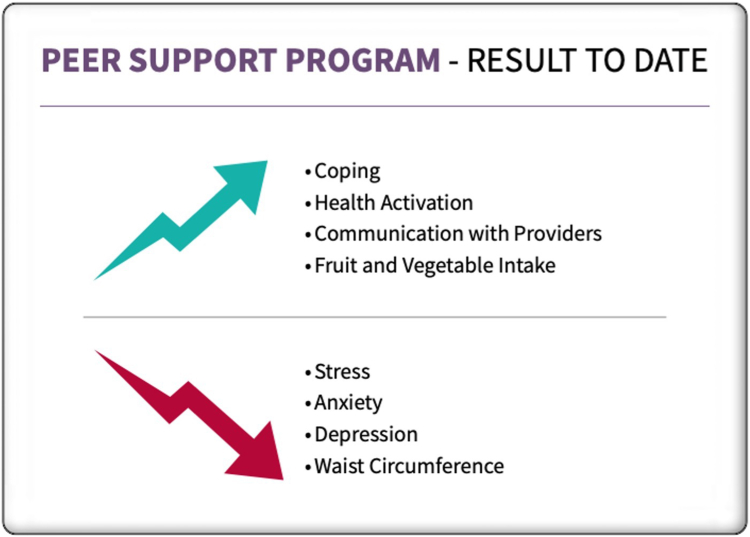
Research indicates that women often experience depression and reduced quality of life following a cardiovascular diagnosis, highlighting the importance of addressing their unique needs.57,58 They express a strong desire for social support and the opportunity to share their experiences relating to CVD.59 Peer support, involving trained individuals who have faced similar challenges, plays a crucial role in women's recovery from CVD. In Canada, several peer-support programs, such as Women@Heart, have been established in various provinces. These programs provide a structured curriculum, led by trained peer leaders, and they focus on empowering women to better understand and manage their cardiovascular health. Initial evaluations of Women@Heart have shown that those in the program have significant improvements in coping, stress management, health activation, and mental well-being (Fig. 6).60 Participants value the sense of community and the emotional support they find in these programs, as well as the opportunity to advocate for their healthcare needs. This finding highlights the importance of tailored support for women living with heart disease in Canada and underscores the value of peer-led initiatives in addressing their unique challenges.
Figure 6.
Outcomes of Canadian peer-support programs to date.
Women-Tailored Cardiac Rehabilitation
Cardiac rehabilitation plays a vital role in promoting the well-being and recovery of individuals with cardiovascular diagnoses, but obstacles hinder the participation of women, who have notably lower referral rates than men.61,62 These barriers include inadequate referrals, geographic distances to programs, comorbidities, exercise-related issues, family responsibilities, and mental health challenges, including depression and anxiety. Recognizing these challenges, Canadian cardiac rehabilitation programs have introduced women-focused models, offering tailored sessions and flexible delivery options, including home-based and centre-based formats. Research has confirmed the significant benefits of ’women’s participation in these programs, which leads to improvements in physical and mental quality of life.63 Canadian WHPs are beneficial, as they refer and connect women to appropriate cardiac rehabilitation programs.
Discussion
This review highlights the many benefits that multidisciplinary WHPs offer. First, these programs are equipped to accurately recognize the signs and symptoms of heart disease in women and offer a tailored approach to identifying and addressing cardiovascular risk factors in women. Second, they offer specialized testing not available at general cardiology clinics, including invasive coronary reactivity testing, OCT, positron emission tomography, and CMR with protocols tailored to INOCA and MINOCA. Moreover, the multidisciplinary nature of these WHPs allows for healthcare professionals, such as NPs, psychiatrists, and psychologists, to provide support in management of risk factors and mental health. Finally, WHPs connect women with heart disease to cardiac rehabilitation centres and peer-support networks that improve women’s heart health and quality of life.
Despite these benefits, accessibility to WHPs remains an issue, as they are concentrated mainly in urban centres, leaving remote communities underserved. Even in urban areas, few WHPs exist across Canada. One potential solution to this accessibility issue is the use of telemedicine or virtual care platforms, which can effectively bridge the distance between healthcare providers and patients, especially for those residing in remote communities. Therefore, integration and prioritization of telemedicine in WHPs is crucial to increasing their reach to underserved populations and promoting equity in healthcare access.
The future goals of WHPs in Canada encompass a multifaceted approach aimed at advancing women's cardiovascular health. The integration of evidence-based practice and practice-based evidence methodologies will remain a fundamental objective. This approach entails continual refinement of clinical practices through rigorous research, ultimately leading to the development of comprehensive guidelines tailored to the particular needs of women. Establishing community partnerships should be a priority, fostering collaboration with local healthcare providers, organizations, and advocacy groups. These partnerships will amplify the reach and impact of WHP initiatives. National collaborations with healthcare institutions and researchers will facilitate the sharing of expertise and resources. Patient engagement will continue to be a core value, as WHPs aim to actively involve women in their own care decisions and treatment plans.
Summary
WHPs aim to address sex-specific risk factors, improve accessibility to specialized care, and promote community and peer support for better cardiovascular health outcomes in women. WHPs also offer opportunities for training, research, and advocacy. Future research should identify barriers in non-urban areas, explore the effectiveness of virtual care, quantify the impacts of peer support and community-based programs, conduct longitudinal studies on WHPs, and investigate the need for medical education reform to enhance care for women with heart disease.
Acknowledgements
The authors thank Drs. Colleen Norris and Hellen Tulloch for their support and information sharing for this review.
Ethics Statement
Ethics considerations did not apply, as this was a review article.
Patient Consent
The authors confirm that patient consent is not applicable to this article. This is a review article and does not include patient-identifying information.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 451 for disclosure information.
References
- 1.Government of Canada Heart disease in Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/heart-disease-canada.html Available at:
- 2.Canada S. 2017. Highlights from the Canadian Chronic Disease Surveillance System.https://www.canada.ca/en/public-health/services/publications/diseases-conditions/heart-disease-canada-fact-sheet.html Available at: [Google Scholar]
- 3.Canadian Women’s Heart Health Centre . 2021. Canadian Women’s Heart Health.https://cwhhc.ottawaheart.ca/education/what-makes-women-different Available at: [Google Scholar]
- 4.Garcia M., Miller V.M., Gulati M., et al. Focused cardiovascular care for women: the need and role in clinical practice. Mayo Clin Proc. 2016;91:226–240. doi: 10.1016/j.mayocp.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Institutes of Health Research (CIHR) What is gender? What is sex? https://cihr-irsc.gc.ca/e/48642.html Available at:
- 6.Cruz J., Mariano Z., Dorian P. Atrial fibrillation clinics in Canada: a nationwide project report. Can J Cardiol. 2018;34:1219–1224. doi: 10.1016/j.cjca.2018.05.017. [DOI] [PubMed] [Google Scholar]
- 7.McAlister F.A., Bakal J.A., Kaul P., et al. Changes in heart failure outcomes after a province-wide change in health service provision: a natural experiment in Alberta, Canada. Circ Heart Fail. 2013;6:76–82. doi: 10.1161/CIRCHEARTFAILURE.112.971119. [DOI] [PubMed] [Google Scholar]
- 8.Del Sindaco D., Pulignano G., Di Lenarda A., et al. Role of a multidisciplinary program in improving outcomes in cognitively impaired heart failure older patients. Monaldi Arch Chest Dis. 2012;78:20–28. doi: 10.4081/monaldi.2012.140. [DOI] [PubMed] [Google Scholar]
- 9.Gandhi S., Mosleh W., Sharma U.C., et al. Multidisciplinary heart failure clinics are associated with lower heart failure hospitalization and mortality: systematic review and meta-analysis. Can J Cardiol. 2017;33:1237–1244. doi: 10.1016/j.cjca.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Gallagher C., Elliott A.D., Wong C.X., et al. Integrated care in atrial fibrillation: a systematic review and meta-analysis. Heart. 2017;103:1947–1953. doi: 10.1136/heartjnl-2016-310952. [DOI] [PubMed] [Google Scholar]
- 11.Parvand M., Cai L., Ghadiri S., et al. One-year prospective follow-up of women with INOCA and MINOCA at a Canadian Women’s Heart Centre. Can J Cardiol. 2022;38:1600–1610. doi: 10.1016/j.cjca.2022.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Parvand M., Rayner-Hartley E., Sedlak T. Recent developments in sex-related differences in presentation, prognosis, and management of coronary artery disease. Can J Cardiol. 2018;34:390–399. doi: 10.1016/j.cjca.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Yusuf S., Hawken S., Ounpuu S., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 14.Huxley R.R., Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378:1297–1305. doi: 10.1016/S0140-6736(11)60781-2. [DOI] [PubMed] [Google Scholar]
- 15.Puymirat E., Simon T., Steg P.G., et al. Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. JAMA. 2012;308:998–1006. doi: 10.1001/2012.jama.11348. [DOI] [PubMed] [Google Scholar]
- 16.Shah A.J., Ghasemzadeh N., Zaragoza-Macias E., et al. Sex and age differences in the association of depression with obstructive coronary artery disease and adverse cardiovascular events. J Am Heart Assoc. 2014;3 doi: 10.1161/JAHA.113.000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smolderen K.G., Strait K.M., Dreyer R.P., et al. Depressive symptoms in younger women and men with acute myocardial infarction: insights from the VIRGO study. J Am Heart Assoc. 2015;4 doi: 10.1161/JAHA.114.001424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia M., Mulvagh S.L., Merz C.N.B., Buring J.E., Manson J.E. Cardiovascular disease in women: clinical perspectives. Circ Res. 2016;118:1273–1293. doi: 10.1161/CIRCRESAHA.116.307547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Le-Ha C., Beilin L.J., Burrows S., et al. Oral contraceptive use in girls and alcohol consumption in boys are associated with increased blood pressure in late adolescence. Eur J Prev Cardiol. 2013;20:947–955. doi: 10.1177/2047487312452966. [DOI] [PubMed] [Google Scholar]
- 20.Ahmed R., Dunford J., Mehran R., Robson S., Kunadian V. Pre-eclampsia and future cardiovascular risk among women: a review. J Am Coll Cardiol. 2014;63:1815–1822. doi: 10.1016/j.jacc.2014.02.529. [DOI] [PubMed] [Google Scholar]
- 21.El Khoudary S.R., Aggarwal B., Beckie T.M., et al. Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American Heart Association. Circulation. 2020;142:e506–e532. doi: 10.1161/CIR.0000000000000912. [DOI] [PubMed] [Google Scholar]
- 22.Young L., Cho L. Unique cardiovascular risk factors in women. Heart. 2019;105:1656–1660. doi: 10.1136/heartjnl-2018-314268. [DOI] [PubMed] [Google Scholar]
- 23.Ferry A.V., Anand A., Strachan F.E., et al. Presenting symptoms in men and women diagnosed with myocardial infarction using sex-specific criteria. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.119.012307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Oosterhout R.E.M., de Boer A.R., Maas A.H.E.M., et al. Sex differences in symptom presentation in acute coronary syndromes: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.119.014733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pelletier R., Humphries K.H., Shimony A., et al. Sex-related differences in access to care among patients with premature acute coronary syndrome. CMAJ. 2014;186:497–504. doi: 10.1503/cmaj.131450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hemal K., Pagidipati N.J., Coles A., et al. Sex differences in demographics, risk factors, presentation, and noninvasive testing in stable outpatients with suspected coronary artery disease: insights from the PROMISE trial. JACC Cardiovasc Imaging. 2016;9:337–346. doi: 10.1016/j.jcmg.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Canto J.G., Rogers W.J., Goldberg R.J., et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA. 2012;307:813–822. doi: 10.1001/jama.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levine G.N., Cohen B.E., Commodore-Mensah Y., et al. Psychological health, well-being, and the mind-heart-body connection: a scientific statement from the American Heart Association. Circulation. 2021;143:e763–e783. doi: 10.1161/CIR.0000000000000947. [DOI] [PubMed] [Google Scholar]
- 29.Eid R.S., Gobinath A.R., Galea L.A.M. Sex differences in depression: insights from clinical and preclinical studies. Prog Neurobiol. 2019;176:86–102. doi: 10.1016/j.pneurobio.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 30.Marcus S.M., Kerber K.B., Rush A.J., et al. Sex differences in depression symptoms in treatment-seeking adults: confirmatory analyses from the Sequenced Treatment Alternatives to Relieve Depression study. Compr Psychiatry. 2008;49:238–246. doi: 10.1016/j.comppsych.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harshfield E.L., Pennells L., Schwartz J.E., et al. Association between depressive symptoms and incident cardiovascular diseases. JAMA. 2020;324:2396–2405. doi: 10.1001/jama.2020.23068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tobaldini E., Carandina A., Toschi-Dias E., et al. Depression and cardiovascular autonomic control: a matter of vagus and sex paradox. Neurosci Biobehav Rev. 2020;116:154–161. doi: 10.1016/j.neubiorev.2020.06.029. [DOI] [PubMed] [Google Scholar]
- 33.Milaneschi Y., Lamers F., Berk M., Penninx B.W.J.H. Depression heterogeneity and its biological underpinnings: toward immunometabolic depression. Biol Psychiatry. 2020;88:369–380. doi: 10.1016/j.biopsych.2020.01.014. [DOI] [PubMed] [Google Scholar]
- 34.Théberge E., Dennis J. Sex differences in the associations of genetic, sociodemographic and cardiovascular risk factors with depression in the Canadian Longitudinal Study on Aging (CLSA) [e-pub ahead of print] medRxiv. [DOI]
- 35.World Health Organization Unequal, unfair, ineffective and inefficient gender inequity in health: why it exists and how we can change it. https://cdn.who.int/media/docs/default-source/documents/social-determinants-of-health/women-and-gender-equity-knowledge-network-final-report-2007.pdf?sfvrsn=41d416c1_3 Available at:
- 36.Slopen N., Glynn R.J., Buring J.E., et al. Job strain, job insecurity, and incident cardiovascular disease in the Women’s Health Study: results from a 10-year prospective study. PLoS One. 2012;7 doi: 10.1371/journal.pone.0040512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pacheco C., Luu J., Mehta P.K., et al. INOCA and MINOCA: Are women’s heart centres the answer to understanding and management of these increasing populations of women (and men)? Can J Cardiol. 2022;38:1611–1614. doi: 10.1016/j.cjca.2022.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahajan A.M., Gandhi H., Smilowitz N.R., et al. Seasonal and circadian patterns of myocardial infarction by coronary artery disease status and sex in the ACTION Registry-GWTG. Int J Cardiol. 2019;274:16–20. doi: 10.1016/j.ijcard.2018.08.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jespersen L., Hvelplund A., Abildstrøm S.Z., et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33:734–744. doi: 10.1093/eurheartj/ehr331. [DOI] [PubMed] [Google Scholar]
- 40.Reis S.E., Holubkov R., Conrad Smith A.J., et al. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am Heart J. 2001;141:735–741. doi: 10.1067/mhj.2001.114198. [DOI] [PubMed] [Google Scholar]
- 41.Tamis-Holland J.E., Jneid H., Reynolds H.R., et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Association. Circulation. 2019;139:891–908. doi: 10.1161/CIR.0000000000000670. [DOI] [PubMed] [Google Scholar]
- 42.Merz C.N., Beltrame J.F., S.G., et al. Insights to advance our management of myocardial ischemia: From obstructive epicardial disease to functional coronary alterations. Am Hear J Plus Cardiol Res Pract. 2021;11 doi: 10.1016/j.ahjo.2021.100060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tonet E., Pompei G., Faragasso E., et al. Coronary microvascular dysfunction: PET, CMR and CT assessment. J Clin Med. 2021;10:1848. doi: 10.3390/jcm10091848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koilpillai P., Aggarwal N.R., Mulvagh S.L. State of the art in noninvasive imaging of ischemic heart disease and coronary microvascular dysfunction in women: indications, performance, and limitations. Curr Atheroscler Rep. 2020;22:73. doi: 10.1007/s11883-020-00894-0. [DOI] [PubMed] [Google Scholar]
- 45.Reynolds H.R., Maehara A., Kwong R.Y., et al. Coronary optical coherence tomography and cardiac magnetic resonance imaging to determine underlying causes of myocardial infarction with nonobstructive coronary arteries in women. Circulation. 2021;143:624–640. doi: 10.1161/CIRCULATIONAHA.120.052008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sara J.D., Widmer R.J., Matsuzawa Y., et al. Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. JACC Cardiovasc Interv. 2015;8:1445–1453. doi: 10.1016/j.jcin.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 47.Gulati M., Hendry C., Parapid B., Mulvagh S.L. Why we need specialised centres for women’s hearts: changing the face of cardiovascular care for women. Eur Cardiol. 2021;16:e52. doi: 10.15420/ecr.2021.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mulvagh S.L., Mullen K.-A., Nerenberg K.A., et al. The Canadian Women’s Heart Health Alliance atlas on the epidemiology, diagnosis, and management of cardiovascular disease in women—Chapter 4: sex- and gender-unique disparities: CVD across the lifespan of a woman. CJC Open. 2022;4:115–132. doi: 10.1016/j.cjco.2021.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Aggarwal N.R., Mulvagh S.L. In: Sex Differences in Cardiac Disease. Aggarwal N.R., Wood M.J., editors. Elsevier; 2021. Chapter 29 – women’s heart programs; pp. 671–686.https://www.sciencedirect.com/science/article/pii/B9780128193693000022?via%3Dihub Available at: [Google Scholar]
- 50.Woo B.F.Y., Lee J.X.Y., Tam W.W.S. The impact of the advanced practice nursing role on quality of care, clinical outcomes, patient satisfaction, and cost in the emergency and critical care settings: a systematic review. Hum Resour Health. 2017;15:63. doi: 10.1186/s12960-017-0237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Whitelaw S., Sullivan K., Eliya Y., et al. Trial characteristics associated with under-enrolment of females in randomized controlled trials of heart failure with reduced ejection fraction: a systematic review. Eur J Heart Fail. 2021;23:15–24. doi: 10.1002/ejhf.2034. [DOI] [PubMed] [Google Scholar]
- 52.Piro M., Della Bona R., Abbate A., Biasucci L.M., Crea F. Sex-related differences in myocardial remodeling. J Am Coll Cardiol. 2010;55:1057–1065. doi: 10.1016/j.jacc.2009.09.065. [DOI] [PubMed] [Google Scholar]
- 53.Lee K.K., Ferry A.V., Anand A., et al. Sex-specific thresholds of high-sensitivity troponin in patients with suspected acute coronary syndrome. J Am Coll Cardiol. 2019;74:2032–2043. doi: 10.1016/j.jacc.2019.07.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Côté N., Clavel M.-A. Sex differences in the pathophysiology, diagnosis, and management of aortic stenosis. Cardiol Clin. 2020;38:129–138. doi: 10.1016/j.ccl.2019.09.008. [DOI] [PubMed] [Google Scholar]
- 55.McDonnell L.A., Turek M., Coutinho T., et al. Women’s Heart Health: knowledge, beliefs, and practices of Canadian physicians. J Womens Health (Larchmt) 2018;27:72–82. doi: 10.1089/jwh.2016.6240. [DOI] [PubMed] [Google Scholar]
- 56.Adreak N., Srivaratharajah K., Mullen K.-A., et al. Incorporating a women’s cardiovascular health curriculum into medical education. CJC Open. 2021;3(12 suppl):S187–S191. doi: 10.1016/j.cjco.2021.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Okunrintemi V., Valero-Elizondo J., Patrick B., et al. Gender differences in patient-reported outcomes among adults with atherosclerotic cardiovascular disease. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.010498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hare D.L., Toukhsati S.R., Johansson P., Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35:1365–1372. doi: 10.1093/eurheartj/eht462. [DOI] [PubMed] [Google Scholar]
- 59.McDonnell L.A., Pipe A.L., Westcott C., et al. Perceived vs actual knowledge and risk of heart disease in women: findings from a Canadian survey on heart health awareness, attitudes, and lifestyle. Can J Cardiol. 2014;30:827–834. doi: 10.1016/j.cjca.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 60.Witt D., Benson G., Campbell S., Sillah A., Berra K. Measures of patient activation and social support in a peer-led support network for women with cardiovascular disease. J Cardiopulm Rehabil Prev. 2016;36:430–437. doi: 10.1097/HCR.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 61.Colella T.J.F., Gravely S., Marzolini S., et al. Sex bias in referral of women to outpatient cardiac rehabilitation? A meta-analysis. Eur J Prev Cardiol. 2015;22:423–441. doi: 10.1177/2047487314520783. [DOI] [PubMed] [Google Scholar]
- 62.Samayoa L., Grace S.L., Gravely S., et al. Sex differences in cardiac rehabilitation enrollment: a meta-analysis. Can J Cardiol. 2014;30:793–800. doi: 10.1016/j.cjca.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 63.Mamataz T., Ghisi G.L.M., Pakosh M., Grace S.L. Nature, availability, and utilization of women-focused cardiac rehabilitation: a systematic review. BMC Cardiovasc Disord. 2021;21:459. doi: 10.1186/s12872-021-02267-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gan Y., Gong Y., Tong X., et al. Depression and the risk of coronary heart disease: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2014;14:371. doi: 10.1186/s12888-014-0371-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Emdin C.A., Odutayo A., Wong C.X., Tran J., Hsiao A.J., Hunn B.H. Meta-analysis of anxiety as a risk factor for cardiovascular disease. Am J Cardiol. 2016;118:511–519. doi: 10.1016/j.amjcard.2016.05.041. [DOI] [PubMed] [Google Scholar]
- 66.Akosile W., Colquhoun D., Young R., Lawford B., Voisey J. The association between post-traumatic stress disorder and coronary artery disease: a meta-analysis. Austr Psychiatr Bulletin Royal Australian New Zealand Coll Psychiatrist. 2018;26:524–530. doi: 10.1177/1039856218789779. [DOI] [PubMed] [Google Scholar]
- 67.Heikkilä K., Fransson E.I., Nyberg, et al. IPD-Work Consortium Job strain and health-related lifestyle: findings from an individual-participant meta-analysis of 118,000 working adults. Am J Public Health. 2013;103:2090–2097. doi: 10.2105/AJPH.2012.301090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Richardson S., Shaffer J.A., Falzon L., Krupka D., Davidson K.W., Edmondson D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol. 2012;110:1711–1716. doi: 10.1016/j.amjcard.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Steptoe A., Shankar A., Demakakos P., Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A. 2013;110(15):5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]