Abstract
Background
Cardiopulmonary resuscitation is essential for cardiopulmonary arrest, but complications from chest compressions warrant monitoring. Although rib and sternal fractures are common, abdominal injuries are rare, and splenic injuries are much rarer.
Case Presentation
A 74‐year‐old man was admitted to the emergency room with a hemorrhagic duodenal ulcer. During hospitalization, the patient went into cardiopulmonary arrest due to hemorrhagic shock. Spontaneous circulation returned after 7 min of cardiopulmonary resuscitation. He underwent transcatheter arterial embolization to stop the bleeding from the duodenal ulcer. The next day, a close examination of the patient's progressive anemia revealed splenic injury; transcatheter arterial embolization was performed to save his life.
Conclusion
It is important to consider the complication of splenic injury in patients with cardiopulmonary arrest who have undergone appropriate cardiopulmonary resuscitation. A possible mechanism—especially in patients with a full stomach—is the squeezing of the spleen by the diaphragm, abdominal wall, and stomach.
Keywords: chest compression, full stomach, gastrosplenic ligament, splenic artery, splenic injury
Following cardiopulmonary resuscitation for in‐hospital cardiac arrest due to duodenal ulcer bleeding, transcatheter arterial embolization was performed to halt bleeding. Subsequently, splenic hemorrhage was identified, and splenic artery embolization followed.
BACKGROUND
Cardiopulmonary resuscitation (CPR) is vital for cardiopulmonary arrest (CPA), but chest compression has complications. Abdominal injuries, especially splenic, are rare. 1 , 2 Reports of splenic injury from chest compression exist, yet splenic injury during in‐hospital cardiac arrest is rarer.
CASE PRESENTATION
A 74‐year‐old man was transferred from his local doctor to our emergency center because of bloody stools and difficulty moving his body. He had a history of hypertension, type 2 diabetes mellitus, and atrial fibrillation and was taking rivaroxaban 15 mg.
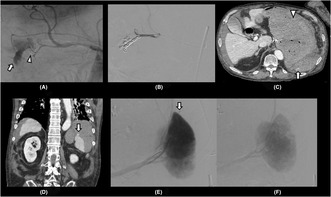
On arrival, vital signs were as follows: blood pressure, 123/62 mmHg; pulse, 96/min; respiratory rate, 20/min; SpO2, 96% (room air); body temperature, 36.2°C; and Glasgow Coma Scale score, 15. Physical examination revealed epigastric pain and rectal examination revealed black stools. His height and weight were 158 cm and 60 kg, respectively. Venous blood gas analysis showed lactic acidosis (pH, 7.42; pCO2, 34.4 mmHg; HCO3 −, 22 mmol/L; lactate, 4.2 mmol/L). Hematological examination revealed severe anemia (hemoglobin level, 4.7 g/dL), mild thrombocytopenia (platelet count, 130,000/μL), and kidney injury (serum creatinine level, 1.76 mg/dL), but no coagulation abnormalities (international normalized ratio of prothrombin time, 1.11; activated partial thromboplastin time, 26.2 s; and fibrinogen level, 363 mg/dL). Abdominal computed tomography (CT) was unremarkable, except for wall thickening of the duodenal bulb to the descending leg and inflammation of the surrounding retroperitoneum, no splenomegaly was observed (Figure 1). After administering intravenous omeprazole 20 mg and transfusing red blood cells, an emergency upper gastrointestinal endoscopy was performed. The esophagus and stomach were clear, and in the duodenum, multiple ulcers were observed in the bulbous region, but there was no active bleeding and some of the ulcers were scarred (Figure 1). The observation was uneventful, and strong gastric wall traction was not performed. The patient was admitted to the intensive care unit ward for observation after confirming spontaneous hemostasis.
FIGURE 1.
(A, B) On admission, plain computed tomography of the abdomen shows wall thickening and fat stranding in the duodenal bulb and descending leg (arrow). (C) No fluid collection is observed around the liver and spleen. (D) The first upper gastrointestinal endoscopy shows ulcers in the duodenal bulb, but no active bleeding and scarring. (E, F) The second gastrointestinal endoscopy shows a large blood clot in the stomach and active bleeding from the duodenal bulb ulcer. Hemostasis by clipping was not achieved.
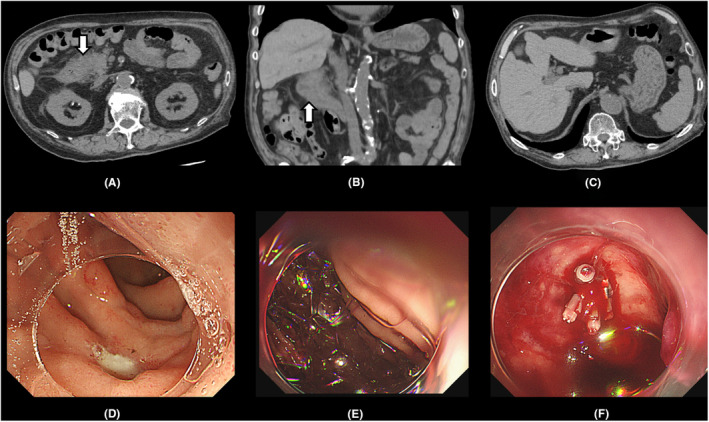
At 1 h after admission, the patient complained of epigastric pain and nausea. He vomited fresh blood, his level of consciousness decreased, and he went into CPA with a pulseless electrical activity rhythm. Appropriate CPR was performed by experienced emergency center staff; the patient was intubated and return of spontaneous circulation (ROSC) was achieved after 7 min. Emergency upper gastrointestinal endoscopy was performed again, revealing a large blood clot in the stomach and active bleeding from a duodenal bulb ulcer, which seemed to be the one found during the first endoscopy. Endoscopic hemostasis was unsuccessful (Figure 1), and emergency transcatheter arterial embolization (TAE) was performed. Extravasation into the duodenal lumen was observed from the right gastroepiploic and anterior superior pancreaticoduodenal arteries. Metal coil embolization procedures were performed, and hemostasis was achieved (Figure 2). After TAE and massive transfusion (38, 30, and 10 units of red blood cells, fresh‐frozen plasma, and platelets, respectively), the patient was resuscitated from severe hemorrhagic shock and his general condition stabilized.
FIGURE 2.
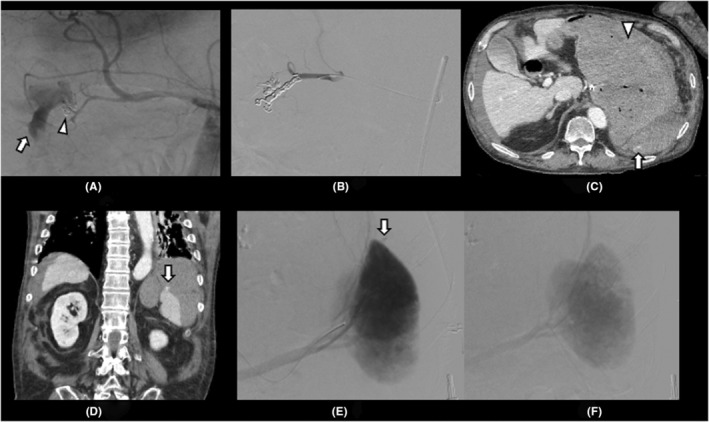
(A) Angiography shows extravasation from the right gastroepiploic artery and anterior superior pancreaticoduodenal artery into the duodenal lumen (arrow). Clips used for trying to stop bleeding are shown (arrowhead). (B) Metal coils are placed from the gastroduodenal artery to these two branches for embolization, and no extravasation is observed. (C, D) Contrast‐enhanced abdominal computed tomography on the second day shows seudoaneurysm from the spleen (arrow) and a large volume of contents but no extravasation in the stomach (arrowhead). (E) Angiography shows evidence of pseudoaneurysm from the upper pole of the spleen (arrow). (F) After embolization of the splenic artery with a gelatin sponge, no pseudoaneurysm is observed.
On day 2, his hemoglobin level dropped from 9.2 (at 7:00; 10 h after ROSC) to 7.4 (at 11:00) g/dL (Table 1), although physical examination did not reveal purpura or swelling in the abdomen suggestive of trauma. The third upper gastrointestinal endoscopy showed no active bleeding. Abdominal ultrasound showed fluid accumulation around the spleen, suggesting intra‐abdominal bleeding; therefore, urgent CT was performed. Intra‐abdominal hemorrhage around the spleen and pseudoaneurysm from the suprasplenic pole into the abdominal cavity were observed. Consequently, we diagnosed grade‐II spleen injury per the American Association for the Surgery of Trauma classification and grade‐II splenic injury per the Japanese Association for the Surgery of Trauma classification. We found a large volume of contents (CT value: 42–58 HU) in the stomach but no extravasation in the stomach or duodenum. Emergency TAE was performed, and pseudoaneurysm from the superior pole branch of the splenic artery into the abdominal cavity was observed, similar to the CT findings, and stopped by embolization with a gelatin sponge (Figure 2). Thereafter, the anemia did not progress.
TABLE 1.
The trend of hemoglobin and coagulation system from arrival at our hospital to TAE.
| First day | Second day | |||||
|---|---|---|---|---|---|---|
| 15:00 | 21:00 | 01:30 | 07:00 | 13:00 | 20:00 | |
| on ER | Immediately after ROSC | After TAE of duodenal ulcer | After TAE of splenic injury | |||
| Hb (g/dL) | 4.7 | 8.1 | 9.8 | 9.2 | 6.9 | 8.1 |
| Platelet count (/μL) | 130,000 | 106,000 | 64,000 | 43,000 | 105,000 | |
| PT‐INR | 1.11 | 1.26 | 1.27 | 1.33 | 1.29 | |
| APTT (sec) | 26 | >120 | 68 | 44 | 41 | |
| Fibrinogen (mg/dL) | 363 | 218 | 155 | 215 | 245 | |
Abbreviations: APTT, Activated Partial Thromboplastin Time; ER, emergency room; Hb, hemoglobin; PT‐INR, Prothrombin Time‐International Normalized Ratio; ROSC, return of spontaneous circulation; TAE, transcatheter arterial embolization.
Multidisciplinary treatment was continued, and on day 10, the patient gained consciousness and was extubated. The patient continued to do well and was transferred to the general ward on day 15.
DISCUSSION
We experienced a rare splenic injury during CPR for in‐hospital cardiac arrest due to hemorrhagic shock from a duodenal ulcer. Autopsy analyses reveal common chest complications, including rib and sternal fractures, and anterior mediastinal hematomas, with abdominal issues being rarer. The most frequent abdominal complication is liver injury, while splenic injuries are extremely uncommon. 1 , 2
Splenic injuries are often tied to abdominal trauma, yet this case lacked such trauma and physical signs of abdominal force. Other external forces may be associated with splenic injury. The thin splenic capsule, lacking muscle, is vulnerable to external force 3 ; thus, splenic injury may occur when the spleen is squeezed between the diaphragm and abdominal wall following a sudden increase in intra‐abdominal pressure. 4 The spleen lies amid diaphragm, stomach, and abdominal wall, and its surface meets the stomach's body. Thus, a full stomach applies pressure, causing potential splenic bleeding. 3 , 5
This patient had CPA because of hemorrhagic shock due to a hemorrhagic duodenal ulcer. Additionally, as CT conducted 20 h after ROSC still showed a large volume of blood clots in the stomach, gastric dilation may have occurred during CPR. Chest compression might have pushed the diaphragm down through the pericardium, while the dilated stomach, diaphragm, and abdominal wall could have caused splenic injury by squeezing the spleen. In a CPR‐related splenic injury case series, chest compression leading to gastrosplenic ligament traction causing vascular injury was reported. 6
The patient was taking rivaroxaban, and no antagonist was administered. Rivaroxaban has been reported to cause atraumatic splenic rupture. 7 However, in this case, the absence of splenic hemorrhage on the first CT (Figure 1) and its presence on the second CT (Figure 2), after CPR, suggest that the splenic hemorrhage was likely induced by CPR rather than spontaneous bleeding. In addition, the patient developed secondary coagulopathy following massive duodenal ulcer bleeding, which could potentially contribute to the splenic hemorrhage. Furthermore, splenomegaly is known as a potential risk for splenic injury, 8 there was no splenomegaly in this case.
Manual and mechanical chest compressions have similar complications 1 Splenic injury as a complication of CPR, is reported with manual chest compressions by paramedics 9 or bystanders 10 and with mechanical chest compressions. 9 , 11 Incorrect hand position during chest compressions may be a risk factor 12 ; therefore, appropriate position and strength are crucial to prevent complications. Our patient had in‐hospital cardiac arrest, and CPR by BLS/ACLS providers, ensuring suitable technique. Complications of splenic injury in patients with in‐hospital cardiac arrest who receive appropriate CPR are rare, and prior reports have not described the quality of CPR. 13 Splenomegaly and postoperative anatomical abnormalities are also considered risk factors but were not present in this case. Therefore, in our case, the splenic injury might have been caused by chest compression.
If unexpected shock or anemia occurs after cardiopulmonary resuscitation, clinicians should perform ultrasound and CT examinations to look for hemorrhagic complications.
CONCLUSION
We report a rare case of splenic injury as a complication of chest compression after CPR for CPA due to hemorrhagic shock owing to a bleeding duodenal ulcer. Although liver injury is the most common abdominal complication after CPR, we should consider that splenic injury may occur after chest compressions.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest for this article.
ETHICS STATEMENT
Approval of the research protocol: N/A.
Informed consent: Informed consent for the publication of this case report was obtained from the patient's family.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
ACKNOWLEDGEMENTS
We thank Editage (www.editage.com) for English language editing.
Fujimori D, Koyama T, Ooki S, Ito M, Yoshiike Y, Nakamura S, et al. Splenic injury caused by cardiopulmonary resuscitation in a full stomach with hematoma after hemorrhagic shock due to bleeding duodenal ulcer: A case report. Acute Med Surg. 2024;11:e940. 10.1002/ams2.940
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Karasek J, Blankova A, Doubková A, Pitasova T, Nahalka D, Bartes T, et al. Trauma associated with cardiopulmonary resuscitation based on autopsy reports after the 2015 ERC guidelines. Am J Emerg Med. 2022;61:81–86. [DOI] [PubMed] [Google Scholar]
- 2. Krischer JP, Fine EG, Davis JH, Nagel EL. Complications of cardiac resuscitation. Chest. 1987;92:287–291. [DOI] [PubMed] [Google Scholar]
- 3. Kodikara S, Sivasubramanium M. Mechanisms of delayed splenic rupture: a new hypothesis. Legal Med. 2009;11:S515–S517. [DOI] [PubMed] [Google Scholar]
- 4. Wehbe E, Raffi S, Osborne D. Spontaneous splenic rupture precipitated by cough: a case report and a review of the literature. Scand J Gastroenterol. 2008;43:634–637. [DOI] [PubMed] [Google Scholar]
- 5. Garg P, Chitkara N, Dass B. Stomach jolt—a possible mechanism for gastrosplenic injury in blunt abdominal trauma. Indian J Gastroenterol. 1996;15:153. [PubMed] [Google Scholar]
- 6. Subramani K, Thomas AN, Reeve RS. Occult splenic rupture with cardiovascular collapse: a report of three cases in critically ill patients. Intensive Care Med. 2002;28:1819–1821. [DOI] [PubMed] [Google Scholar]
- 7. Labaki ML, De Kock M. Atraumatic splenic rupture in a patient treated with rivaroxaban: a case report and a narrative review. Clin Case Reports. 2022;10:e6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fitchet A, Neal R, Bannister P. Lesson of the week: splenic trauma complicating cardiopulmonary resuscitation. BMJ. 2001;322:480–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yamada T, Nakao S, Fukuma H, Matsuoka T. Delayed massive bleeding from minor splenic injury due to mechanical chest compression for cardiopulmonary resuscitation. Acute Med Surg. 2023;10:e845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Salzman M, Friedman J. Bystander cardiopulmonary resuscitation‐induced splenic laceration and hepatosplenic hematoma. Am J Emerg Med. 2012;30(388):e1–e2. [DOI] [PubMed] [Google Scholar]
- 11. Miyazaki Y, Kooguchi K, Fukui M, Kato Y, Wada T, Yokomine T, et al. A case of traumatic liver and spleen injuries after cardiopulmonary resuscitation by mechanical chest compression device, AutoPulse®. Jpn Soc Intensive Care Med. 2018;25:255–258. [Google Scholar]
- 12. Olds K, Byard RW, Langlois NE. Injuries associated with resuscitation ‐ an overview. J Forensic Leg Med. 2015;33:39–43. [DOI] [PubMed] [Google Scholar]
- 13. Berlinerblau R, Marmolejos F, Bykofsky MM. Delayed rupture of the spleen after cardiac massage. JAMA. 1980;243:364–365. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


