Abstract
BACKGROUND
Limited empirical evidence is available regarding the effect of technology-assisted cardiac rehabilitation (TACR) among coronary heart disease (CHD) patients with central obesity.
AIM
To determine the effects of 12-week TACR on health outcomes of patients with CHD.
DESIGN
Two-arm randomized controlled trial.
SETTING
Cardiovascular department of a regional hospital.
POPULATION
Coronary heart disease patients with central obesity.
METHODS
The study randomized 78 hospitalized CHD patients to receive either the 12-week TACR intervention or usual care. Guided by social cognitive theory, the intervention began with an in-person assessment and orientation session to assess and identify individual risks and familiarize with the e-platform/device before discharge. After discharge, patients were encouraged to visit the interactive CR website for knowledge and skills acquisition, data uploading, use the pedometer for daily step tracking, and interact with peers and professionals via social media for problem-solving and mutual support. Data were collected at baseline (T0), six-week (T1), and 12-week (T2).
RESULTS
Participants in the intervention group showed significant improvement in daily steps at six weeks but not 12 weeks (T1: β=2713.48, P=0.03; T2:β=2450.70, P=0.08), weekly sitting minutes (T1: β=-665.17, P=0.002; T2: β=-722.29, P=0.02), and total (vigorous, moderate, and walking) exercise at 12-week (β=-2445.99, P=0.008). Improvement in health-promoting lifestyle profile (T1: β=24.9, P<0.001; T2: β=15.50, P<0.001), smoking cessation (T2: β=-2.28, P<0.04), self-efficacy (T2: β=0.63, P=0.02), body mass index (T1:β =-0.97, P=0.03; T2: β=-0.73, P=0.04) and waist circumferences (T1: β =-1.97, P=0.003; T2: β =-3.14, P=0.002) were identified.
CONCLUSIONS
Results indicated the effectiveness of the TACR intervention in improving healthy behaviors and anthropometric parameters for CHD patients with central obesity. Individual assessment, collaborative action planning, and ongoing obesity management support should be highlighted in TACR programs for CHD patients.
CLINICAL REHABILITATION IMPACT
Central obesity should be assessed and highlighted in TACR intervention as an independent risk factor that requires corresponding behavior change and body fat management.
Key words: Cardiac rehabilitation; Coronary disease; Obesity, Technology; Randomized controlled trial
Obesity is increasingly identified as an epidemic and independent risk factor for coronary heart disease (CHD).1 It is estimated that over 80% of patients with CHD are overweight or obese.2 A recent scientific statement from the American Heart Association highlighted that obesity contributes directly to cardiovascular risk factors, including dyslipidemia, hypertension, and type 2 diabetes, leading to cardiac event onset and mortality.1 Empirical data showed that central obesity is a CHD risk marker that is independent of body mass index.3, 4 Moreover, in a given BMI category, subgroups of excessive waist circumference were associated with increased cardiovascular mortality risk. Central obesity is predictive of mortality and can capture CHD patients with normal body weight but excess fat, which unmasks higher cardiovascular risk.3, 4 Using the Asia cut-off score, a waist circumference of ≥90 cm for male and 80cm for female reflect central obesity.5
Cardiac rehabilitation (CR) is a multicomponent intervention that contains patient assessment, exercise training and physical activity promotion, health education, psychological support and cardiovascular risk management, tailored to the needs of CHD patients.6 Strong evidence shows that CR can effectively improve exercise, promote healthy behavior, improve lipid profile and obesity indices, restore psychosocial wellbeing, improve quality of life, and reduce cardiac events and mortality for patients with coronary heart disease (CHD).7, 8 Despite the effectiveness, conventional CR has low accessibility and uptake,9 urging the development of alternative CR models.10 Additionally, individuals with central obesity who undergo cardiac rehabilitation need to manage two comorbid chronic conditions and might require more individualized treatment to optimize recovery.11
Technology-assisted cardiac rehabilitation (TACR), which comprises telemonitoring and remote guidance/supervision, is a safe and cost-effective alternative to conventional CR.12, 13 It grants readily CR access with minimal time and geographical barriers by utilizing technologies such as computers, mobile phones, and monitoring sensors.14 The TACR not only allows healthcare professionals to provide online, individualized health information, collect real-time data and give immediate feedback, and offer ongoing professional support to the patients,15 it can also empower self-management of patients by using a self-directed approach, particularly allowing personal settings (e.g., individualized goals) and progress visualization on the home page.13
Emerging studies suggested the cost-effectiveness of technology-assisted cardiac rehabilitation (TACR) in improving physical activity, modifying lifestyle, alleviating stress, promoting quality of life, and reducing cardiac events/hospitalization. However, the effects of TACR in CHD patients with central obesity have not been well studied. Several randomized controlled trials provided TACR intervention to CHD patients. Results showed significant improvement in behavior modification but not in weight and/or waist circumference reduction when compared with control group receiving usual care,16-18 waitlist control,19 or conventional CR.20, 21 This may be explained by mixing CHD patients with and without central obesity and/or a lack of emphasis on identifying obesity and linking its management with behavior change, such as exercise and eating, in previous TACR interventions. The favorable behavior change and ineffective body fat management urge investigation of the effects of technology-assisted cardiac rehabilitation (phase II) in CHD patients with central obesity. The aim of this study was to investigate the effect of technology-assisted cardiac rehabilitation (TACR) among coronary heart disease (CHD) patients with central obesity.
Materials and methods
Study design
The study was a two-arm randomized controlled trial (registration number: ChiCTR1800020411). The study inclines to CONSORT guidelines of reporting trials.
Setting and participants
The study was conducted in a tertiary hospital in Wuhan in 2019, China. Participants were recruited consecutively from the hospitalized patients of four cardiology units before discharge when their medical conditions became stable as confirmed by physicians.
The inclusion criteria were: 1) adults aged ≥18; 2) diagnosed with CHD; 3) have central obesity using Asian-specific cut-off point (waist circumference ≥90 cm for male, ≥80 cm for female);5 4) able to read Chinese with a primary or above educational level; 5) own a device with Internet connection; and 6) having no prescribed physical activity restriction.
Patients who had a life-limiting condition (e.g., cancer), acute psychiatric illness, absolute and relative contradictions to exercise testing and training according to the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) guideline (Supplementary Digital Material 1: Supplementary Table I),22 or have visual, auditory, and fine motor disorders were excluded.
Sample size estimation
Referring to an RCT study comparing TACR with usual care on improving physical activity, the study required a sample of 68 participants for two groups to achieve an effect size of 0.719 with 80% power and 0.05 significance level. To account for an expected attrition rate of 12%, a sample size of 78 was adopted, based on previous CR studies of similar duration.23
Technology-assisted cardiac rehabilitation intervention
The TACR followed the international guidelines and culturally appropriate national recommendations for CR,8, 24-27 and was underpinned by the Social Cognitive Theory (SCT).28 The SCT highlights that in order to empower behavioural change in individuals, the cognitive (i.e., awareness), behavioral (e.g., self-efficacy) and environmental factors (e.g. professional support) must be optimized and addressed.28 The intervention commenced with an in-person assessment conducted by a registered nurse with training background and practice experiences in CR prior to hospital discharge. During the session, the nurse assessed participants’ exercise capacity using six-minute walk test (assisted by another cardiac nurse watching patients’ Holter monitored ECG at the nurse station) and habits, diet habits, smoking status, stress management practices, and social aspects related to CHD and central obesity management. Based on the assessments, the nurse introduced guideline-based CR recommendations. The discrepancy between the patients’ described behaviors and the CR guideline recommendation will be highlighted, and the impact of unhealthy behaviors and uncontrolled central obesity on CHD health outcomes will be elaborated. Ideal body weight was computed – men: 50 + [0.91 × (height in cm ‒ 152.4)] and women: 45.5 + [0.91 × (height in cm ‒ 152.4)]29 and normal waist circumference following Asia cut-off score were introduced to increase patients’ awareness. Then, the nurse partnered with the patient to support them in setting goals and action plans in concordance with their central obesity condition, personal risks, metabolic equivalent (MET) level from the submaximal test, and preferences and upload the goals to their personal websites. The goal setting for exercise is successive, gradually increasing the frequency, duration, and intensity of exercise to achieve at least 150 min of moderate weekly exercise. The nurse taught participants the use of Borg’s ratings of perceived exertion to gradually achieve moderate intensity (from “fairly light” to “somewhat hard” on a scale of 6 to 20). The MET level for different physical activities in daily life, such as slow walking, brisk walking, square dancing, and Tai Chi, were discussed in goal setting process with reference to the American College of Sports Medicine guideline.30 The physical activity plan was reviewed and approved by patients’ physician. In addition, the nurse organized a group orientation session to teach patients about using the CR website and pedometer (Mi band), telemonitoring for patients’ daily steps, after which the participants were invited to join the social media chatroom for group interaction and professional consultation. A user manual of the website and pedometer was provided.
The TACR components were delivered through an account and password-protected CR website (accessible via computer/mobile phone). The design of the website was guided by Health Literacy Online31 to optimize user-friendliness and readability. Since CR uses a multidisciplinary approach, cardiologists, cardiac nurses, physiotherapists and dietitians with experiences in providing CR services were involved in designing/commenting on the content of the eHealth CR program to ensure its accuracy and appropriateness for CHD patients.32 The website enables two main features: self-monitoring with motivational feedback and experiential learning for knowledge and skills acquisition. Patients were encouraged to upload weekly/daily goal-attainment data (i.e., physical activity, diet checklist). The website could analyze their data and generate graphical visualization and motivational messages for progress tracking. The website learning content includes the pathophysiology and manifestation of CHD, physical activity, healthy diet, smoking cessation, stress coping, cardiovascular risk factors management (central obesity, hypertension, cholesterol, and diabetes), symptom management and post-PCI management. The linkage between each behavior aspect and central obesity was explained (e.g., exercise and central obesity, smoking cessation and weight change).8, 24-27 Each learning content is presented sequentially: 1) introducing the role and underlying mechanism; 2) lifestyle changes; 3) actions; 4) self-monitoring and resolutions to barriers.
The nurse moderated peer interaction in the WeChat chatroom to encourage progress and experience sharing and to moderate peer interaction/support. Patients were encouraged to raise cardiac-related questions in the chatroom using pseudonym names. During the eHealth CR program implementation, the nurse coordinated the care and consulted with the relevant CR staff if necessary to fully address participants’ questions and evaluate their health status. Nurses are effective in coordinating care with other CR staff and process the professional knowledge in empowering lifestyle change in patients’ home settings.
Control group
Participants in the control group received usual care, a 10-minute didactic coaching on medication usage and lifestyle modification (physical activity, diet, and smoking cessation) delivered by physicians when delivering discharge summary. They were taught how to use a pedometer for data-collection purposes.
Measurements
Sociodemographic data, including age, sex, education, marital status, employment condition, and co-residency, were collected. Clinical data were retrieved from the digital medical record, including diagnosis, treatment, diseased coronary vessels, and cardiovascular comorbidities.
Primary outcome: physical activity
Physical activity was measured objectively and subjectively using a pedometer (Mi Band, China) and International Physical Activity Questionnaire (IPAQ), respectively. Participants were asked to wear the pedometer for three days at each data collection time point to calculate average steps as an outcome.33 The IPAQ has a good reliability with intra-class correlation coefficients of 0.74 to 0.97 for each sub-domain for Chinese adults.34
Other outcomes
The Health-Promoting Lifestyle Profile II (HPLP-II) was used to measure the healthy behaviors of the participants.35 The HPLP-II has been translated and validated with Cronbach’s α coefficient of 0.63 to 0.81 among Chinese adults.36 The smoking status was assessed by asking about participants’ current smoking status, including non-smoker, current smoker, and ex-smoker.37 Cardiac self-efficacy was measured by the Cardiac Self-efficacy Scale (CSES), a 5-point Likert Scale, evaluating participants’ confidence in maintaining function and controlling symptoms.38 A higher score indicates greater self-efficacy. The CSES has an excellent internal consistency with Cronbach’s alpha 0.90 (English version) and 0.926 (Chinese version)39 Health-related quality of life was measured by the MacNew Heart Disease (MacNew HRQoL), assessing the influence of CHD on participants’ physical, emotional, and social wellbeing.40 The MacNew questionnaire was translated and validated among the Chinese CHD population, with intraclass correlation coefficients ranging from 0.88 to 0.93.41 Psychological wellbeing was measured by the 21-item Depression Anxiety Stress Scale 21 (DASS-21).42, 43 The translated and validated Chinese DASS-21 had Cronbach’s alpha ≥0.80.44 The cardiac physiological risk parameters were assessed using standardized approaches, containing body mass index (BMI) (Xiheng, RGZ-120-RT, China), blood pressure (Omron HEM-7124, Japan), and waist circumference.
Data collection and ethics considerations
The Joint Chinese University of Hong Kong – New Territories East Cluster Clinical Research Ethics Committee granted ethical approval for this study (No.2018.469). Eligibility was assessed by the nurse by reviewing medical records, interviewing patients, and seeking advice from a senior CR nurse wherever there was uncertainty. The nurse introduced the study to potential participants with an information sheet and verbal explanation. They were ensured of their right to withdraw at any time without adverse effects. The nurse obtained final confirmation on eligibility from on-site physicians for eligible patients who agreed to participate. Two trained research assistants collected baseline data after obtaining written informed consent in the hospital. Block randomization, with a random block size of four, six and eight generated by ‘Random Allocation Software’, was used to allocate the participants. The group assignments were written and enclosed in an opaque and sealed envelope in the sequence accordingly. Another research assistant opened the envelope to the participants after the baseline data collection. Post-test data were collected 6-week and 12-week post-intervention by the two research assistants who had no information about group assignment.
Statistical analysis
Data analysis was conducted using SPSS 28. Descriptive statistics were calculated to summarize participants’ characteristics. Normality assessment of continuous variables was assessed by estimating skewness that a skewness value within -2 to 2 was considered as normally distributed. The t-test, Chi-square, and Mann-Whitney Test were selected to determine between-group comparability in demographic, clinical, and outcome variables at baseline. The generalized estimating equation (GEE) model was used to calculate changes in the outcome variables between the two groups across the study endpoints. The GEE model follows the intention to treat principle, can handle the missing data mathematically, and accommodate group*time interaction effect for better estimation of intervention effect. Any sociodemographic and clinical variables with between-group differences P<0.20 at baseline were regarded as a covariate and adjusted in the GEE model. Effect sizes were calculated for all mean differences at T2 (12 weeks) using Hedges’ g. All tests are two-sided with a significance level of 0.05.
Data availability
The data associated with the paper are not publicly available but are available from the corresponding author on reasonable request.
Results
Recruitment, attrition, intervention engagement
A total of 78 participants were recruited, with 39 per study group. The CONSORT flow diagram is presented in Figure 1.
Figure 1.
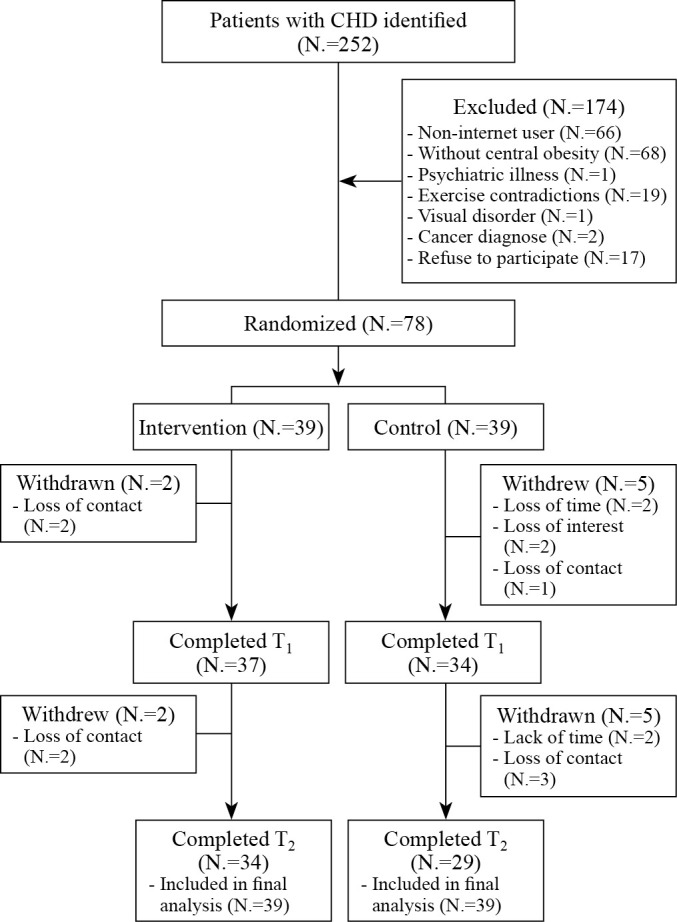
—CONSORT patient flow diagram.
Participants had an average age of 55.73±7.17, and the majority were male (80.8%, N.=63), married (97.4%, N.=76) and co-reside with their family (97.4%, N.=76). The baseline characteristics and outcome variables of participants are presented in Supplementary Digital Material 2 (Supplementary Table II). No significant between-group differences were detected at baseline. Two sociodemographic and clinical variables with baseline difference P<0.2 were adjusted in the GEE model, including PCI treatment (or medication only) and dyslipidemia.
Effects on physical activity
The changes from baseline to each post-test endpoint across outcome variables of both groups are presented in Supplementary Digital Material 3 (Supplementary Table III). Based on the GEE analysis, participants in the intervention group showed a significant group*time interaction effect in physical activity as measured by daily steps (β=2713.48, P=0.03), weekly sitting minutes (β=-665.17, P=0.002), compared to the control group at 6-week post-intervention. Participants in the intervention group maintained their improvement over the control group in physical activity as measured by weekly sitting minutes (β=-722.29, P=0.02), total (vigorous, moderate, and walking) exercise (β=-2445.99, P=0.008). A favorable improvement in daily steps in the intervention group was observed, although not statistically significant (β=2450.70, P=0.08). The effect size falls in the range of small to medium (Hedge’s g 0.30-0.78).
Effects on other outcomes
Participants in the TACR group also showed a significant group × time interaction effect in health-promoting lifestyle profile from baseline to 6 weeks (β=24.9, P<0.001) and to 12 weeks (β=15.50, P<0.001) compared with the control group. The improvement in smoking cessation (β=-2.28, P<0.04) and self-efficacy (β=0.63, P=0.02) were observed from baseline to 12 wks when compared with the control group. The effect size falls in the range of small to large (Hedge’s g 0.21-1.44).
For HRQoL, no significant intervention effect was observed on global quality of life across study endpoints (T1: β =-0.03, P=0.89; T2: β=0.38, P=0.20) between the two groups. There were no significant effect on physical domain (T1: β=-0.11, P=0.61; T2: β=-0.39, P=0.22), emotional domain (T1: β=0.03, P=0.90; T2: β = 0.32, p=0.27), and social domain (T1: β=-0.15, P=0.50; T2: β=0.51, P=0.12) of HRQoL.
Pertaining psychological wellbeing, compared to the control group, the intervention group showed no significant improvement in DASS total score (T1: β=0.13, P=0.94; T2: β=-0.53, P =0.80) and depression (T1: β=-0.04, P=0.92; T2: β=-0.59, P=0.43), anxiety (T1: β=-0.1, P=0.83; T2: β=0.03, P=0.83), stress (T1: β=0.26, P=0.77; T2: β=0.08, P=0.94) subscale.
Participants in the intervention group showed significant improvement in body mass index (T1: β =-0.97, P=0.03; T2: β=-0.73, P=0.04) and waist circumferences (T1: β=-1.97, P=0.003; T2: β=-3.14, P=0.002). The effect size falls in the range of medium to large (Hedge’s g 0.64-2.42).
For blood pressure, participants in the intervention group showed no significant differences in systolic blood pressure (T1: β=1.24, P=0.81; T2: β=-3.3, P=0.53) and diastolic blood pressure (T1: β=-0.94, P=0.80; T2: β=-1.90, P=0.64) when compared to the control group.
Adverse events
There was no report of adverse events related to study participation. Four participants in the intervention group and two in the control group reported receiving planned PCI treatment during the study period. Two participants in the intervention group and two in the control group reported cardiovascular-related re-hospitalization.
Intervention usage
During the 12-week, the study has a website visit rate of 66.7% (26 participants logged in to the website). The average number of website visits among participants who visited the website was 8.7±10.14. The study observed active interaction in an online chatroom by 30 participants with an average of 3.33±4.55 peer interaction and 2.2±2.38 professional consultation (messages on the same topic were counted once). Only 17 participants uploaded data on their personal website regarding goal attainment, among which all achieved predetermined behavior change goals. Seven participants never visited the website nor engaged in the online chatroom dialogue, among which four participated in the post-test data collection.
Discussion
Limited empirical evidence is available regarding the effect of TACR in CHD patients with central obesity. Given the adverse effects of central obesity on CHD progression, this study provided technology-assisted CR, including a website, a pedometer, and an online chatroom, for CHD patients with central obesity condition after hospital discharge. Guided by social cognitive theory, a cardiovascular nurse engaged patients in identifying central obesity problem and personal risk factors, engaging goal setting, together with telemonitoring data and a motivational website to reflect/encourage goal attainment. Patient-professional interaction was facilitated in a peer-supported chatroom to optimize real-time professional advice, promote health conversation, and mobilize peer influence/support for problem-solving. The positive effects on physical activity, health-promoting lifestyle profile, smoking cessation, body mass index, and waist circumference of patients with CHD were encouraging. Managing these risk factors is crucial in slowing disease progression and preventing subsequent cardiac events. The improvement in self-efficacy further supported the use of social cognitive theory in TACR.
The study’s findings are consistent with a meta-analysis that demonstrated positive effects of TACR programs in improving the physical activity of patients with CHD.13, 45 More time spent in moderate-to-vigorous physical activity has been associated with a lower incidence of cardiovascular disease.46 The finding of increased levels of daily steps and moderate-vigorous physical exercise from the study results in patients with central obesity is encouraging, given that at least 20 minutes of moderate-vigorous physical exercise per week is associated with the lowest risks of all-cause and cardiovascular mortality.47
Furthermore, this study observed comprehensive heart-healthy behavior modifications, whereas previous studies more frequently reported the effects of program on physical activity and put less emphasis on dietary or smoking cessation. Smoking cessation and a healthy diet are strongly recommended in the context of secondary prevention and rehabilitation by cardiology specialists in at-risk populations who have experienced a cardiac event.29 Progress in a broader range of behavioral changes may be reflective of the comprehensiveness of the CR program with an extensive embodiment of behavior change techniques.48
More importantly, the TACR intervention showed significant improvement in anthropometric parameters (i.e., body weightand waist circumference). Such results added evidence regarding the effectiveness of TACR in optimizing behaviour risk factors and anthropometric outcomes for patients with central obesity conditions. Previous studies that suggested no significant improvement in body weight reduction and/or waist circumference when compared with the control group16-21 may be attributed to the recruitment of general CHD patients with/without obesity condition and a focus on exercise. Assessing and elaborating on central obesity condition and linking obesity reduction regarding exercise and other healthy lifestyle behaviors should be highlighted in TACR intervention for CHD patients with central obesity.
Patients’ engagement was captured by tracking website visits, data uploading activities, and chatroom interactions. Considering the combined number of website visits, pedometer, and online chatrooms by the patients, this study reached a high intervention usage rate based on the definition of a previous review.49 Engagement in each platform may not appear high, which implies that participants have different preferences and compatibility conditions in using their smartphones/laptops to access the CR. To improve intervention usage, some models/frameworks that focus on reducing the barriers to technology-based self-learning at home should considered, such as the effort-optimize Intervention Model.50 Using artificial intelligence or gamification that includes rewards or the opportunity to compare goal attainment with peers may attract the participants to improve engagement for the future TACR.51 Future studies may also evaluate their perceived website usability and qualitative experiences to improve eHealth design.
Limitations of the study
Several limitations should be mentioned. First, the generalizability is limited by recruiting participants from one regional hospital with a good literacy level with smartphone/computer usage background. The low representation of women is also worth noticing. The TACR interventions for women should be further investigated, as they tend to be older and have more medical and psychological comorbidities.52 Second, the non-use attrition may challenge the cause-effect relationship as four participants had no/minimal intervention use. Lastly, the study only evaluated the effects of TACR for 12 weeks to mimic the duration of conventional CR. Future studies should incorporate a longer-term evaluation to determine the sustained intervention effects.
Conclusions
This study identified the significant effects of a 12-week TACR program in improving physical activity, health-promoting lifestyle profile, smoking cessation, body mass index, and waist circumference of patients with CHD with central obesity following a cardiac event. The effectiveness of this intervention provided insights into the development of a comprehensive CR program with an intensive embodiment of theory-guided initiatives/techniques to promote health outcomes of CHD patients with central obesity. Long-term follow-up is needed to determine long-term effectiveness.
Acknowledgements
The authors acknowledge clinicians for their support in this work.
Footnotes
Conflicts of interest: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Funding: This research was funded by the Ministry of Health, Czech Republic; conceptual development of research organization (FNBr, 65269705).
References
- 1.Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, et al. American Heart Association Council on Lifestyle and Cardiometabolic Health ; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2021;143:e984–1010. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33882682&dopt=Abstract 10.1161/CIR.0000000000000973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ades PA, Savage PD. The Treatment of Obesity in Cardiac Rehabilitation: A REVIEW AND PRACTICAL RECOMMENDATIONS. J Cardiopulm Rehabil Prev 2021;41:295–301. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34461619&dopt=Abstract 10.1097/HCR.0000000000000637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piché ME, Poirier P, Lemieux I, Després JP. Overview of Epidemiology and Contribution of Obesity and Body Fat Distribution to Cardiovascular Disease: an Update. Prog Cardiovasc Dis 2018;61:103–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29964067&dopt=Abstract 10.1016/j.pcad.2018.06.004 [DOI] [PubMed] [Google Scholar]
- 4.Mu L, Liu JM, Zhou GH, Wu CQ, Chen BW, Lu Y, et al. Obesity Prevalence and Risks Among Chinese Adults Findings From the China PEACE Million Persons Project, 2014-2018. Circ-Cardiovasc Qual. 2021;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Obesity: preventing and managing the global epidemic. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 6.Taylor RS, Dalal HM, McDonagh ST. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat Rev Cardiol 2022;19:180–94. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34531576&dopt=Abstract 10.1038/s41569-021-00611-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamm LF, Sanderson BK, Ades PA, Berra K, Kaminsky LA, Roitman JL, et al. Core competencies for cardiac rehabilitation/secondary prevention professionals: 2010 update: position statement of the American Association of Cardiovascular and Pulmonary Rehabilitation. J Cardiopulm Rehabil Prev 2011;31:2–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21217254&dopt=Abstract 10.1097/HCR.0b013e318203999d [DOI] [PubMed] [Google Scholar]
- 8.American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. Sixth edition. Champaign, IL: Human Kinetics; 2020. [Google Scholar]
- 9.Ritchey MD, Maresh S, McNeely J, Shaffer T, Jackson SL, Keteyian SJ, et al. Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative. Circ Cardiovasc Qual Outcomes 2020;13:e005902. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31931615&dopt=Abstract 10.1161/CIRCOUTCOMES.119.005902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas RJ, Petersen CE, Olson TP, Beatty AL, Ding R, Supervia M. Asynchronous and Synchronous Delivery Models for Home-Based Cardiac Rehabilitation: A SCIENTIFIC REVIEW. J Cardiopulm Rehabil Prev 2021;41:407–12. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34727559&dopt=Abstract 10.1097/HCR.0000000000000656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell T, Rash JA, Vallis M. Appreciating the Importance of Unmet Needs Associated With Obesity in Cardiac Rehabilitation: A Call for Critical Improvement in Program Availability. Can J Cardiol 2019;35:684–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31151697&dopt=Abstract 10.1016/j.cjca.2019.04.005 [DOI] [PubMed] [Google Scholar]
- 12.Batalik L, Filakova K, Sladeckova M, Dosbaba F, Su J, Pepera G. The cost-effectiveness of exercise-based cardiac telerehabilitation intervention: a systematic review. Eur J Phys Rehabil Med 2023;59:248–58. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36692413&dopt=Abstract 10.23736/S1973-9087.23.07773-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Su JJ, Yu DS, Paguio JT. Effect of eHealth cardiac rehabilitation on health outcomes of coronary heart disease patients: A systematic review and meta-analysis. J Adv Nurs 2020;76:754–72. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31769527&dopt=Abstract 10.1111/jan.14272 [DOI] [PubMed] [Google Scholar]
- 14.Su JJ, Liu JY, Cheung DS, Wang S, Christensen M, Kor PP, et al. Long-term effects of e-Health secondary prevention on cardiovascular health: a systematic review and meta-analysis. Eur J Cardiovasc Nurs 2023;22:562–74. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36695341&dopt=Abstract 10.1093/eurjcn/zvac116 [DOI] [PubMed] [Google Scholar]
- 15.Platz K, Kools S, Howie-Esquivel J. Benefits, Facilitators, and Barriers of Alternative Models of Cardiac Rehabilitation: A QUALITATIVE SYSTEMATIC REVIEW. J Cardiopulm Rehabil Prev 2023;43:83–92. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36346781&dopt=Abstract 10.1097/HCR.0000000000000738 [DOI] [PubMed] [Google Scholar]
- 16.Devi R, Powell J, Singh S. A web-based program improves physical activity outcomes in a primary care angina population: randomized controlled trial. J Med Internet Res 2014;16:e186. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25217464&dopt=Abstract 10.2196/jmir.3340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blioumpa C, Karanasiou E, Antoniou V, Batalik L, Kalatzis K, Lanaras L, et al. Efficacy of supervised home-based, real time, videoconferencing telerehabilitation in patients with type 2 diabetes: a single-blind randomized controlled trial. Eur J Phys Rehabil Med 2023;59:628–39. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37350165&dopt=Abstract 10.23736/S1973-9087.23.07855-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su JJ, Yu DS. Effects of a nurse-led eHealth cardiac rehabilitation programme on health outcomes of patients with coronary heart disease: A randomised controlled trial. Int J Nurs Stud 2021;122:104040. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34333211&dopt=Abstract 10.1016/j.ijnurstu.2021.104040 [DOI] [PubMed] [Google Scholar]
- 19.Zutz A, Ignaszewski A, Bates J, Lear SA. Utilization of the internet to deliver cardiac rehabilitation at a distance: a pilot study. Telemed J E Health 2007;13:323–30. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17603835&dopt=Abstract 10.1089/tmj.2006.0051 [DOI] [PubMed] [Google Scholar]
- 20.Batalik L, Dosbaba F, Hartman M, Konecny V, Batalikova K, Spinar J. Long-term exercise effects after cardiac telerehabilitation in patients with coronary artery disease: 1-year follow-up results of the randomized study. Eur J Phys Rehabil Med 2021;57:807–14. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33619944&dopt=Abstract 10.23736/S1973-9087.21.06653-3 [DOI] [PubMed] [Google Scholar]
- 21.Varnfield M, Karunanithi M, Lee CK, Honeyman E, Arnold D, Ding H, et al. Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: results from a randomised controlled trial. Heart 2014;100:1770–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24973083&dopt=Abstract 10.1136/heartjnl-2014-305783 [DOI] [PubMed] [Google Scholar]
- 22.American Association of Cardiovascular and Pulmonary Rehabilitation. AACVPR Cardiac Rehabilitation Resource Manual: promoting health and preventing disease. Champaign, IL: Human Kinetics; 2013. [Google Scholar]
- 23.Widmer RJ, Allison TG, Lennon R, Lopez-Jimenez F, Lerman LO, Lerman A. Digital health intervention during cardiac rehabilitation: A randomized controlled trial. Am Heart J 2017;188:65–72. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28577682&dopt=Abstract 10.1016/j.ahj.2017.02.016 [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association . 9. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018;41(Suppl 1):S86–104. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29222380&dopt=Abstract 10.2337/dc18-S009 [DOI] [PubMed] [Google Scholar]
- 25.American Psychological Association. Publication search for “Emotional health”; 2023 [Internet]. Available from: https://www.apa.org/pubs/search?query=&fq=ClassificationFilt:%22Emotional%20Health%22&sort=ContentDateSort [cited 2023, Nov 15].
- 26.Hu DY, Tong QG. Hypertension and Hyperlipidemia. Diet and Exercise. Beijing: China Light Industry Press; 2017. [Google Scholar]
- 27.Chinese National Center for Cardiovascular Diseases. Report on cardiovascular disease in China 2018. Beijing: Encyclopedia of China Publishing House; 2019. [Google Scholar]
- 28.Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004;31:143–64. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15090118&dopt=Abstract 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 29.Thomas RJ, Sapir O, Gomes PF, Iftikhar U, Smith JR, Squires RW. Advances, Challenges, and Progress in Cardiac Rehabilitation in Chronic CVD Management. Curr Atheroscler Rep 2023;25:247–56. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=37040008&dopt=Abstract 10.1007/s11883-023-01100-7 [DOI] [PubMed] [Google Scholar]
- 30.American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription, Eleventh edition. Lippincott Williams & Wilkins; 2020. [Google Scholar]
- 31.Office of Disease Prevention and Health Promotion. Health Literacy Online; 2016 [Internet]. Available from: https://health.gov/healthliteracyonline/ [cited 2023, November 15].
- 32.Su JJ, Yu DS. Effectiveness of eHealth cardiac rehabilitation on health outcomes of coronary heart disease patients: a randomized controlled trial protocol. BMC Cardiovasc Disord 2019;19:274. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31783800&dopt=Abstract 10.1186/s12872-019-1262-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El-Amrawy F, Nounou MI. Are Currently Available Wearable Devices for Activity Tracking and Heart Rate Monitoring Accurate, Precise, and Medically Beneficial? Healthc Inform Res 2015;21:315–20. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26618039&dopt=Abstract https://doi.org/ 10.4258/hir.2015.21.4.315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Macfarlane D, Chan A, Cerin E. Examining the validity and reliability of the Chinese version of the International Physical Activity Questionnaire, long form (IPAQ-LC). Public Health Nutr 2011;14:443–50. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20939939&dopt=Abstract 10.1017/S1368980010002806 [DOI] [PubMed] [Google Scholar]
- 35.Walker SN, Sechrist KR, Pender NJ. The Health-Promoting Lifestyle Profile: development and psychometric characteristics. Nurs Res 1987;36:76–81. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=3644262&dopt=Abstract 10.1097/00006199-198703000-00002 [DOI] [PubMed] [Google Scholar]
- 36.Cao WJ, Chen CS, Hua Y, Li YM, Xu YY, Hua QZ. Factor analysis of a health-promoting lifestyle profile (HPLP): application to older adults in Mainland China. Arch Gerontol Geriatr 2012;55:632–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22854282&dopt=Abstract 10.1016/j.archger.2012.07.003 [DOI] [PubMed] [Google Scholar]
- 37.Global Adult Tobacco Survey Collaborative Group. Tobacco questions for surverys: A subset of key questions from the global adult tobacco survey (GATS). Second edition. Center for Disease Control and Prevention; 2011. [Google Scholar]
- 38.Sullivan MD, LaCroix AZ, Russo J, Katon WJ. Self-efficacy and self-reported functional status in coronary heart disease: a six-month prospective study. Psychosom Med 1998;60:473–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=9710293&dopt=Abstract 10.1097/00006842-199807000-00014 [DOI] [PubMed] [Google Scholar]
- 39.Zhang X, Zhan Y, Liu J, Chai S, Xu L, Lei M, et al. Chinese translation and psychometric testing of the cardiac self-efficacy scale in patients with coronary heart disease in mainland China. Health Qual Life Outcomes 2018;16:43. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29530024&dopt=Abstract 10.1186/s12955-018-0872-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Höfer S, Lim L, Guyatt G, Oldridge N. The MacNew Heart Disease health-related quality of life instrument: a summary. Health Qual Life Outcomes 2004;2:3. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=14713315&dopt=Abstract 10.1186/1477-7525-2-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thompson DR, Oldridge NB, Yu DS, Yu CM. Translation and validation of two Chinese health-related quality of life instruments in patients with coronary heart disease. Hong Kong Med J 2009;15(Suppl 2):8–11. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19258626&dopt=Abstract [PubMed] [Google Scholar]
- 42.Crawford JR, Henry JD. The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. Br J Clin Psychol 2003;42:111–31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12828802&dopt=Abstract 10.1348/014466503321903544 [DOI] [PubMed] [Google Scholar]
- 43.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 1995;33:335–43. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7726811&dopt=Abstract 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- 44.Chan RC, Xu T, Huang J, Wang Y, Zhao Q, Shum DH, et al. Extending the utility of the Depression Anxiety Stress scale by examining its psychometric properties in Chinese settings. Psychiatry Res 2012;200:879–83. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22921506&dopt=Abstract 10.1016/j.psychres.2012.06.041 [DOI] [PubMed] [Google Scholar]
- 45.Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart 2016;102:1183–92. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26936337&dopt=Abstract 10.1136/heartjnl-2015-308966 [DOI] [PubMed] [Google Scholar]
- 46.Dempsey PC, Strain T, Khaw KT, Wareham NJ, Brage S, Wijndaele K. Prospective Associations of Accelerometer-Measured Physical Activity and Sedentary Time With Incident Cardiovascular Disease, Cancer, and All-Cause Mortality. Circulation 2020;141:1113–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32223676&dopt=Abstract 10.1161/CIRCULATIONAHA.119.043030 [DOI] [PubMed] [Google Scholar]
- 47.Hamer M, Stamatakis E. Physical activity and mortality in men and women with diagnosed cardiovascular disease. Eur J Cardiovasc Prev Rehabil 2009;16:156–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19276984&dopt=Abstract 10.1097/HJR.0b013e32831f1b77 [DOI] [PubMed] [Google Scholar]
- 48.Su JJ, Paguio J, Baratedi WM, Abu-Odah H, Batalik L. Experience of coronary heart disease patients with a nurse-led eHealth cardiac rehabilitation: qualitative process evaluation of a randomized controlled trial. Heart Lung 2023;57:214–21. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36265371&dopt=Abstract 10.1016/j.hrtlng.2022.10.005 [DOI] [PubMed] [Google Scholar]
- 49.Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JE. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res 2012;14:e152. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23151820&dopt=Abstract 10.2196/jmir.2104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baumel A, Muench FJ. Effort-Optimized Intervention Model: Framework for Building and Analyzing Digital Interventions That Require Minimal Effort for Health-Related Gains. J Med Internet Res 2021;23:e24905. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33709943&dopt=Abstract 10.2196/24905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sotirakos S, Fouda B, Mohamed Razif NA, Cribben N, Mulhall C, O’Byrne A, et al. Harnessing artificial intelligence in cardiac rehabilitation, a systematic review. Future Cardiol 2022;18:154–64. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33860679&dopt=Abstract https://doi.org/ 10.2217/fca-2021-0010 [DOI] [PubMed] [Google Scholar]
- 52.Khadanga S, Gaalema DE, Savage P, Ades PA. Underutilization of Cardiac Rehabilitation in Women: BARRIERS AND SOLUTIONS. J Cardiopulm Rehabil Prev 2021;41:207–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34158454&dopt=Abstract 10.1097/HCR.0000000000000629 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data associated with the paper are not publicly available but are available from the corresponding author on reasonable request.


