Abstract
Objectives:
This study aimed to evaluate the effectiveness of prophylactic laparoscopic surgery for avoiding adnexal torsion in pregnant women with benign adnexal masses.
Materials and Methods:
This report contains two analyses, each for a different group of patients. Analysis 1: Surgical and pregnancy outcomes were examined among the 126 cases who underwent laparoscopic assisted cystectomy for adnexal masses during pregnancy in our hospital between January 2001 and December 2020. Analysis 2: The incidence of adnexal torsion during pregnancy was evaluated among the cases with adnexal masses ≥5 cm who opted for conservative follow-up in our hospital between January 2011 and December 2020.
Results:
In analysis 1, the most common pathological diagnosis was a mature cystic teratoma (76.2%). The mean gestational age at surgery was 13.1 ± 1.3 weeks. No cases were converted to laparotomy and oophorectomy. Regarding delivery outcomes, 97.4% of cases went on to have full-term deliveries. In Analysis 2, the incidence of adnexal mass ≥5 cm that did not resolve spontaneously during pregnancy was 89 cases (0.8%). The frequency of malignancy was 3 cases (0.03%). In 28 cases who opted for conservative treatment, 5 (17.9%) underwent emergency surgery for adnexal torsion.
Conclusion:
Prophylactic surgery for benign adnexal masses during pregnancy can be performed laparoscopically and preserved ovarian functions. In pregnant women with adnexal masses that do not resolve spontaneously, planning laparoscopic surgery is considered beneficial for complications, such as adnexal torsion.
Keywords: Adnexal mass during pregnancy, adnexal torsion, laparoscopic-assisted surgery
INTRODUCTION
Definitive management strategies for adnexal masses in pregnancy have not been developed.[1] Several studies recommend conservative follow-up for patients with no pathological findings suggestive of malignancy.[2,3,4] However, the rate of torsion is higher in pregnant women with adnexal masses than in nonpregnant women.[5,6] Adnexal torsion during pregnancy presents several difficulties in patient management, such as increased misdiagnosis or laparotomy rates.[7]
Since 2001, our institution has used laparoscopic assisted surgery for patients with benign adnexal masses during their early stages of pregnancy to prevent complications, particularly adnexal torsion. This study investigated the surgical and pregnancy outcomes of laparoscopic-assisted surgery during pregnancy to assess the usefulness of this procedure. In addition, the frequency and characteristics of adnexal torsion in pregnant women were evaluated.
MATERIALS AND METHODS
This study included two analyses, Analysis 1 and 2. In Analysis 1, we assessed 126 cases who underwent pneumoperitoneum laparoscopic cystectomy for benign adnexal masses during pregnancy in our hospital over a 20-year period between January 2001 and December 2020. Using the patients’ medical records, age, pregnancy week at surgery, tumor size, surgical outcomes (surgery time, blood loss, and maternal end-tidal carbon dioxide levels), pathological diagnosis, and intraoperative complications were investigated. As short-term outcomes, perinatal outcomes (mode of delivery and birth weight/Apgar scores of the child) were further examined among the 116 cases whose delivery outcomes could be confirmed.
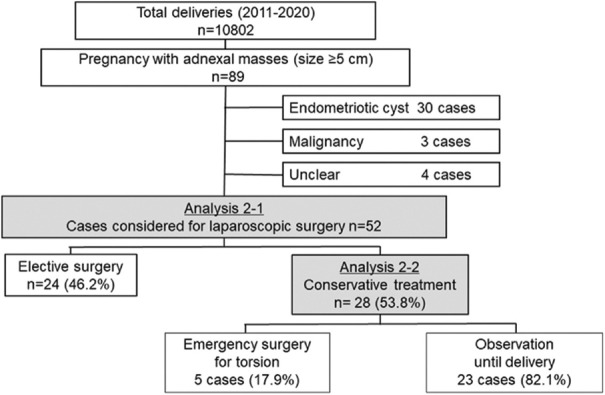
In Analysis 2, we evaluated the rate of developing concomitant adnexal masses ≥5 cm as well as their pathological details in 10,802 women who gave birth in our hospital during a 10-year period between January 2011 and December 2020 [Figure 1]. The medical records of all cases with adnexal tumors from their initial visits to our institution were reviewed. As analysis 2-1, tumor size, pathological diagnosis, and outcomes were compared with the elective surgery group and the conservative group among the 52 cases that met the criteria for prophylactic laparoscopic surgery at our institution. As analysis 2-2, the same factors were compared with the torsion group and the no adverse event group among the conservative group.
Figure 1.
Flow chart of Analysis 2 of women who delivered at our hospital from 2011 to 2020
For statistical analysis, the Student’s t-test, the Mann–Whitney U-test, and Fisher’s exact test were used in Analysis 2. The level of significance was set at P < 0.05. The statistical software ESR (Jichi Medical University Saitama Medical Center, Saitama, Japan) was used for the analysis.
In our institution, laparoscopic surgery during pregnancy is indicated for adnexal masses that (1) are ≥5 cm in size, (2) are not suspected to be functional cysts that will resolve spontaneously, (3) are not suspected to be malignant, and (4) are not tumor-like, such as endometriotic or theca lutein cysts. Endometriotic cysts are not recommended for prophylactic laparoscopic surgery during pregnancy in our institution because of the high risk of adhesions in pelvic cavity and the low risk of adnexal torsion. When an ovarian mass is detected by transvaginal ultrasonography during the early stage of pregnancy, changes in the mass appearance, such as enlargement or disappearance, are repeatedly checked. At gestational weeks 12–13, plain magnetic resonance imaging (MRI) was performed to evaluate the characteristics of the mass, except in some cases in whom MRI was contraindicated or had already been performed prior to the pregnancy. Adnexal masses larger than 5 cm are an indication for surgery at our institution, as such tumors increase the risk of adnexal torsion. Surgery is scheduled sometime after gestational weeks 12–13, when the pregnancy is past the period of organogenesis and the likelihood of spontaneous resolution of the adnexal mass decreases, and before gestational week 16 because thereafter, securing an adequate surgical field of view becomes increasingly difficult due to the growing uterus.
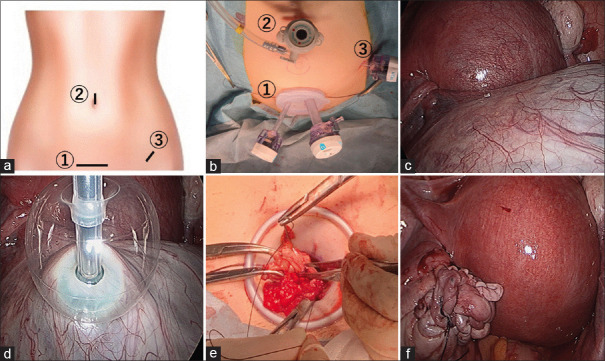
The laparoscopic cystectomy procedure for an adnexal mass during pregnancy is shown in Figure 2. All cases were administered general anesthesia and some received a combination with epidural anesthesia for intraoperative and postoperative pain management. Approximately, 5 mL of 0.375% ropivacaine was injected locally at each wound site before incision. A 3–4-cm transverse incision was made 4–5 cm above the pubic bone, and a Lap Protector Mini® and EZ Access® (both by Hakko Co., Ltd. Medical Device Division; Chikuma-shi, Nagano, Japan) were placed. EZ Access® was placed with 12 and 5-mm ports inserted into it. The insufflation pressure was set to 10 mmHg, and end-tidal carbon dioxide levels were maintained at 30–40 mmHg. The camera was inserted through the 12-mm port, and an 11-mm trocar was inserted through the umbilicus under endoscopic guidance to avoid damaging the enlarged uterus. Then, using the umbilical port as a camera port, a 5-mm auxiliary port was inserted into the left lower quadrant [Figure 2a and b]. After observing the intraabdominal cavity and confirming the absence of adhesions in the pelvis, a SAND balloon catheter® (Hakko Medical, Tokyo, Japan) was inserted through the port on the pubic bone to drain fluid from the ovarian mass [Figure 2c and d]. After confirming shrinkage of the mass, the ovary was pulled out of the body cavity. In cases where puncturing with a SAND balloon catheter® was not feasible because of a mass located in the pouch of Douglas, a rectal probe was inserted into the vagina to push the mass up from the posterior vaginal fornix, while gently elevating the uterus with a forceps to guide the mass to the ventral side of the uterus before puncture. After the ovary was pulled out of the body cavity, the pneumoperitoneum was temporarily interrupted. Cystectomy was performed outside the body cavity, and a 2-0 absorbable suture was used for closure and hemostasis [Figure 2e]. The ovary was returned to the intraabdominal cavity, and pneumoperitoneum was resumed [Figure 2f]. The pelvis was irrigated with warm saline to confirm hemostasis, and adhesion barriers were applied to the area surrounding the ovary before wound closure to complete surgery. If necessary, the drainage catheter was dwelled into the left lower quadrant to drain the fluid. The total operating time was defined as the duration from the start of the suprapubic incision to the closure of all wound sites. Prophylactic tocolytic drugs were not required preoperatively nor postoperatively. The presence or absence of a fetal heartbeat was checked immediately before and after surgery, on the day after surgery, and before discharge. In all patients, a definitive diagnosis was established based on postoperative pathological diagnosis.
Figure 2.
Surgical technique of pneumoperitoneum laparoscopic surgery for benign adnexal masses during pregnancy. (a and b) Surgical incisions were made at the umbilicus, left lower quadrant, and above the pubic bone, (c and d) A SAND balloon catheter® (Hakko Medical) was inserted to drain fluid from the ovarian mass, (e) Cystectomy and sutures were performed outside the body cavity, (f) After the ovary was returned to the pelvic cavity, the pelvis was irrigated with warm saline to confirm the cessation of bleeding
Ethics
As this study was conducted as a retrospective study, informed consent was not obtained from individual patients. This study was conducted in accordance with the Declaration of Helsinki and has been approved by the hospital’s independent ethics committee (approval number 20-380; April 9, 2021).
RESULTS
Patient characteristics and surgical outcomes of Analysis 1 are presented in Table 1. No cases have been converted to laparotomy and oophorectomy. One case (0.8%) experienced an injury to the sigmoid colon serosa caused a by puncture with the SAND balloon catheter®. The injury was repaired laparoscopically with sutures, and no postsurgical complications were noted, such as ileus or intestinal perforation. The patient had a favorable subsequent course of pregnancy and gave birth vaginally at 40 weeks and 2 days.
Table 1.
Surgical and pregnancy outcomes
| Mean±SD or number of patients (%) | |
|---|---|
| Patient characteristics and surgical outcomes (n=126) | |
| Age (years) | 30.5±4.3 |
| Gestational age at surgery (weeks) | 13.1±1.3 |
| Size of ovarian tumor (mm) | 80.6±23.3 |
| Surgery duration (min) | 87.1±27.6 |
| Total blood loss during surgery (mL) | 31.4±33.5 |
| Mean of EtCO2 during surgery (mmHg) | 33.7±4.6 |
| Number of port punctures | 2.8±0.6 |
| Surgical complications (%) | 1 (0.8) |
| Pregnancy outcomes (n=116) | |
| Gestational age at delivery (weeks) | 38.7±2.8 |
| Pregnancy loss | 1 (0.9) |
| Preterm birth | 2 (1.7) |
| Neonate weight (g)† | 2999.7±379.1 |
| Apgar scores† | |
| 1 min (points) | 8.8±0.7 |
| 5 min (points) | 9.7±0.5 |
| Mode of delivery† | |
| Normal vaginal delivery | 81 (70.4) |
| Vacuum or forceps delivery | 10 (8.7) |
| Cesarean section | 24 (20.9) |
†n=115 excluding pregnancy loss. Data are expressed as mean±SD or n (%) of patients. EtCO2: End-tidal carbon dioxide concentration, SD: Standard deviation
The most common pathological diagnosis was a mature cystic teratoma, occurring in 96 cases (76.2%). Endometriotic and luteal cysts, which could not be identified by preoperative MRI, were diagnosed postoperatively in four cases (3.2%) each.
The average tumor size was 80.6 ± 23.3 mm. Thirty-seven cases (29.3%) had tumors larger than 10 cm. Notably, two instances of tumors larger than 15 cm included one luteal cyst and one serous adenoma.
The delivery outcomes are shown in Table 2. Ninety-seven percent of cases had full-term deliveries. Although the causal relationship with the surgery is unknown, one (0.9%) had an inevitable miscarriage on the day of surgery. Elective surgery was performed at gestational week 12 for a mature cystic teratoma measuring 6 cm. During the surgery, no compression or stimulation was applied to the uterus, and the surgery was completed without complications. The last preoperative confirmation of fetal heartbeat was not noted in the medical record, and it is unknown when the heartbeat stopped. Genital bleeding was observed approximately 5 h after the surgery, and ultrasound showed no heartbeat in the fetus, resulting in the diagnosis of inevitable miscarriage. There were two cases of premature birth (1.7%) (at gestational weeks 35 and 36); their causal relationships with the surgery are unknown.
Table 2.
Comparison between the elective surgery group and the conservative group (n=52)
| Elective surgery group† (n=24) | Conservative group‡ (n=28) | P | |
|---|---|---|---|
| Age (years) | 30.3±4.5 | 33.1±4.9 | 0.04 |
| BMI (kg/m2) | 20.4±3.9 | 20.9±3.1 | 0.73 |
| Size of ovarian tumor (mm) | 79.2±19.1 | 65.8±20.4 | 0.02 |
| Pathological findings | |||
| Mature cystic teratoma | 20 (83.3) | 14 (50.0) | 0.01 |
| Mucinous cystadenoma | 1 (4.2) | 2 (7.1) | |
| Serous cystadenoma | 2 (8.3) | 12 (42.8) | |
| Leydig cell tumor | 1 (4.2) | 0 | |
| Pregnancy outcomes | |||
| Gestational age at delivery (weeks) | 38.8±1.6 | 38.7±1.2 | 0.84 |
| Miscarriage | 0 | 0 | - |
| Preterm birth | 1 (4.2) | 0 | 0.46 |
| Neonate weight (g) | 2924.0±487.2 | 2921.2±259.4 | 0.98 |
| Apgar scores | |||
| 1 min (points) | 8.1±1.9 | 8.7±0.8 | 0.14 |
| 5 min (points) | 9.1±2.0 | 9.6±0.6 | 0.17 |
†Elective surgery group included patients for whom prophylactic laparoscopic surgery for adnexal masses were performed during pregnancy, ‡Conservative group included patients who met the criteria for prophylactic laparoscopic surgery but opted for conservative treatment. Data are expressed as mean±SD or n (%) of patients. BMI: Body mass index, SD: Standard deviation
The rate of developing concomitant adnexal masses ≥5 cm in 10,802 women is shown in Figure 1. Adnexal masses that regressed during pregnancy were excluded from the study. Adnexal masses of ≥5 cm were present in 89 cases, accounting for 0.8% of all pregnancies. Endometriotic cysts were diagnosed in 30 cases (0.3% of all pregnancies) by image evaluation using ultrasound or MRI. Three cases with malignancy (0.03%) underwent laparotomy for pathological diagnosis; two cases (0.02%) were diagnosed with mucinous borderline tumor, and the remaining one case (0.01%) was diagnosed with squamous cell carcinoma.
Fifty-two cases (0.5%) met the criteria for laparoscopic surgery during the early stage of pregnancy at our institution. Of these, 24 cases (46.2%) underwent elective surgery (elective surgery group) and 28 cases (53.8%) opted for observation (conservative group). Table 2 shows the findings of the comparison between the two groups. The size of the adnexal mass was significantly larger in the elective surgery group than in the conservative group. Solid tumors such as mature cystic teratoma and Leydig cell tumors were significantly high in the elective surgery group than in the conservative group. No significant difference was observed between the two groups in pregnancy outcomes.
Five of the 28 cases who opted for observation underwent emergency surgery following a diagnosis of adnexal torsion. The rate of torsion in pregnant women with a concurrent adnexal mass ≥5 cm was 17.9%. In the other 23 cases, no symptoms requiring hospitalization were observed. Table 3 shows the findings of the comparison between cases who underwent emergency surgery due to torsion (torsion group) and those who remained on conservative therapy until delivery (no adverse event group). No significant difference was observed between the two groups in any of the factors, including tumor size and pregnancy outcomes. The pathological diagnoses of the five cases who underwent emergency surgery were mature cystic teratoma in two cases and serous cystadenoma in three cases. Notably, the torsion group included two cases of 5 cm dermoid cysts. One and three patients had adnexal torsion in the first and second trimesters, respectively. Laparoscopic detorsion and cystectomy were performed for four patients. Another patient underwent a cesarean section with adnexal detorsion and cystectomy in the third trimester.
Table 3.
Comparison between the torsion group and the no adverse event group (n=28)
| Torsion group† (n=5) | No adverse event group‡ (n=23) | P | |
|---|---|---|---|
| Age (years) | 31.4±3.6 | 33.5±5.2 | 0.41 |
| BMI (kg/m2) | 18.8±2.2 | 20.9±2.6 | 0.12 |
| Size of ovarian tumor (mm) | 71.0±28.8 | 64.7±18.8 | 0.63 |
| Pathological findings | |||
| Mature cystic teratoma | 2 (40.0) | 12 (52.2) | 0.76 |
| Mucinous cystadenoma | 0 | 2 (8.7) | |
| Serous cystadenoma | 3 (60.0) | 9 (39.1) | |
| Pregnancy outcomes | |||
| Gestational age at delivery (weeks) | 38.6±0.9 | 38.7±1.3 | 0.88 |
| Miscarriage | 0 | 0 | - |
| Preterm birth | 0 | 0 | - |
| Neonate weight (g) | 2902.0±171.6 | 2925.4±277.7 | 0.86 |
| Apgar scores | |||
| 1 min (points) | 8.4±0.9 | 8.8±0.7 | 0.42 |
| 5 min (points) | 9.6±0.5 | 9.7±0.6 | 0.68 |
†Torsion group included patients who required emergency surgery for adnexal torsion during pregnancy, ‡No adverse event group included patients with no complications during pregnancy. Data are expressed as mean±SD or n (%) of patients. BMI: Body mass index, SD: Standard deviation
DISCUSSION
According to Analysis 1, none of the 126 cases who underwent prophylactic laparoscopic surgery during pregnancy in the 20-year period have been converted to laparotomy. For improved safety, at our institution, the indications for surgery have been defined, and attempts are made to further reduce the invasiveness by using the same surgical procedure. Another measure taken is the use of the SAND balloon catheter® to perform cystectomy outside the body cavity. A similar surgical procedure was reported by Kurihara et al.[8] This procedure has three advantages. First, it can shorten the duration of pneumoperitoneum; second, it enables safe operation even when the surgical field is compromised by a large uterus; third, in cases of mature cystic teratomas, the incidence of chemical peritonitis is low because of minimal leakage of fluid. Another crucial measure taken is that the first incision is made 4–5 cm above the pubic bone, not at the umbilicus. In previous case reports, uterine trauma was reported as caused by inserting the initial trocar through the umbilicus.[9] Therefore, trocar insertion should be carefully performed in pregnant women.
The rate of intraoperative complications was 0.8%, and no cases were converted to laparotomy in this study. The only complication was an injury to the sigmoid colon serosa caused by a puncture with the SAND balloon catheter®. Kurihara et al. reported no surgical complications in 14 cases of laparoscopic surgery with the SAND balloon catheter® among pregnant patients with ovarian cysts.[8] In a report of 115 cases in a 14-year series by Wan Ghazali et al., the rates of visceral injuries and conversion to laparotomy were 0% and 1.7%, respectively.[10] The type of complications could have occurred even in nonpregnancy surgery. When there is a risk of puncture by a SAND balloon catheter due to a small size of the adnexal mass, a bag-assisted laparoscopic procedure can be considered: the affected ovary is placed inside a retrieval bag and pulled out of the body cavity.[11] With reference to these reports, it may be important to present the complication rate to the patient before surgery.
One case (0.9%) had an inevitable miscarriage on the day of surgery, although the causal relationship with the surgery remains unknown. Wan Ghazali et al. reported that only two of 115 cases (1.7%) had complications of second-trimester miscarriage.[10] The percentage of spontaneous miscarriages in the second trimester was found to be approximately 0.3%–5% of pregnancies.[12] A previous study has reported that the rates of miscarriage associated with surgery for adnexal masses were 6.4% in the first trimester and 2.1% in the second trimester.[13] According to a meta-analysis, the rate of miscarriage is 0%–8.5% for laparoscopic surgery.[14] Compared to these rates, the miscarriage rate in this study was not high. This study suggests that surgery for adnexal masses in pregnant women does not affect delivery outcomes.
In Analysis 2, the incidence of adnexal torsion was 17.9% (5 cases) in cases that were placed under observation without surgery during pregnancy. No significant difference was observed between the torsion and no adverse event groups in any of the factors, including tumor size. These results indicate that there was no obvious risk of adnexal torsion during pregnancy. Previous studies have shown that the rates of adnexal torsion during pregnancy ranged widely, from 3% to 28%.[5] The rate is markedly higher than the rate among nonpregnant women (2%–6%).[15] Other studies have revealed that 12%–25% of women with adnexal torsion are during pregnancy.[6,16]
Our institution set the cutoff size for adnexal tumors requiring prophylactic surgery during pregnancy at 5 cm. Because, some reports that included nonpregnant patients found that adnexal masses >5 cm in diameter were associated with a particularly increased risk for adnexal torsion.[6,17,18]
With regard to the potential problem of developing adnexal torsion during pregnancy, the following three concerns may pose challenges. First, it may be difficult to receive appropriate care if the facility has no obstetrician, gynecologist, or anesthesiologist. Second, laparoscopic surgery may not be feasible due to an enlarged uterus depending on the stage of pregnancy, leaving no choice but to perform laparotomy. It has been reported that 8.3% of emergency surgeries for adnexal torsion are performed by laparotomy.[19] Third, it may be difficult to identify whether the acute abdomen was caused by adnexal torsion or pregnancy complications, such as miscarriage or preterm birth.[7] In the torsion group of Analysis 2 in this study, all cases preserved ovarian functions and had a favorable subsequent course of pregnancy. Four cases (80%) were laparoscopically operable with the exception of one case of cesarean section of the third trimester. It was a positive influence that our institution had a large number of laparoscopies and obstetricians. One review of literature about adnexal torsion during pregnancy has reported that preserving ovarian functions was 62% and laparoscopic surgery was 72%.[20] Based on these reasons, we believe it is useful to plan laparoscopic surgery for a pregnant woman with an adnexal mass that does not regress spontaneously.
This study had two limitations. First, the long-term prognosis of children whose mothers underwent surgery during pregnancy has not been elucidated. Although it has been suggested that this surgical procedure involving pneumoperitoneum and general anesthesia has no impact on the delivery outcomes,[10,21] whether the same can be said for the children after they grow up is unknown. A larger, long-term study is warranted. Second, this was a retrospective study. The rate of adnexal torsion revealed in Analysis 2 was the percentage in a group that excluded cases in which prophylactic surgery was chosen. It is not known whether all cases in whom prophylactic surgery was performed would have had torsion at follow-up. It is possible that bias have been involved in the selection of cases, which should be acknowledged. Therefore, randomized trials are required in the future to verify these findings.
CONCLUSION
Prophylactic surgery for benign adnexal masses during pregnancy can be performed laparoscopically and preserved ovarian functions. We believe that the results of this study demonstrate that laparoscopic-assisted cystectomy in the second trimester is beneficial for avoiding complications, such as adnexal torsion in pregnant women with adnexal masses that do not resolve spontaneously. In future, a prospective study is warranted to understand the incidence of adnexal torsion and examine the usefulness of laparoscopic surgery in the prevention of complications during pregnancy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the staff of our department for their support in this study. Further, we are particularly grateful to Professor Jun Kumakiri for his continuous support, and I would like to express my appreciation to Associate Professor Jun Takeda who provided the valuable data.
REFERENCES
- 1.Goh W, Bohrer J, Zalud I. Management of the adnexal mass in pregnancy. Curr Opin Obstet Gynecol. 2014;26:49–53. doi: 10.1097/GCO.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 2.McMinn E, Schwartz N. Adnexal masses in pregnancy. Clin Obstet Gynecol. 2020;63:392–404. doi: 10.1097/GRF.0000000000000528. [DOI] [PubMed] [Google Scholar]
- 3.Bunyavejchevin S, Phupong V. Laparoscopic surgery for presumed benign ovarian tumor during pregnancy. Cochrane Database Syst Rev. 2013;1:CD005459. doi: 10.1002/14651858.CD005459.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Senarath S, Ades A, Nanayakkara P. Ovarian cysts in pregnancy: A narrative review. J Obstet Gynaecol. 2021;41:169–75. doi: 10.1080/01443615.2020.1734781. [DOI] [PubMed] [Google Scholar]
- 5.Aggarwal P, Kehoe S. Ovarian tumours in pregnancy: A literature review. Eur J Obstet Gynecol Reprod Biol. 2011;155:119–24. doi: 10.1016/j.ejogrb.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 6.Houry D, Abbott JT. Ovarian torsion: A fifteen-year review. Ann Emerg Med. 2001;38:156–9. doi: 10.1067/mem.2001.114303. [DOI] [PubMed] [Google Scholar]
- 7.Smorgick N, Pansky M, Feingold M, Herman A, Halperin R, Maymon R. The clinical characteristics and sonographic findings of maternal ovarian torsion in pregnancy. Fertil Steril. 2009;92:1983–7. doi: 10.1016/j.fertnstert.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 8.Kurihara K, Minagawa M, Masuda M, Fukuyama M, Tanigaki K, Yamamoto A, et al. The evaluation of laparoscopic surgery on pregnant patients with ovarian cysts and its effects on pregnancy over the past 5 years. Gynecol Minim Invasive Ther. 2018;7:1–5. doi: 10.4103/GMIT.GMIT_12_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedman JD, Ramsey PS, Ramin KD, Berry C. Pneumoamnion and pregnancy loss after second-trimester laparoscopic surgery. Obstet Gynecol. 2002;99:512–3. doi: 10.1016/s0029-7844(01)01664-7. [DOI] [PubMed] [Google Scholar]
- 10.Wan Ghazali WA, Shukri NA, Abdul Halim NH. Laparoscopic cystectomy in pregnancy, a viable solution –A 14 years series. Gynecol Minim Invasive Ther. 2017;6:157–61. doi: 10.1016/j.gmit.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Q, Fang F, Zhang C. A self-made bag-assisted laparoendoscopic single-site surgery in ovarian teratomectomy during pregnancy. Gynecol Minim Invasive Ther. 2022;11:174–5. doi: 10.4103/gmit.gmit_19_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Michels TC, Tiu AY. Second trimester pregnancy loss. Am Fam Physician. 2007;76:1341–6. [PubMed] [Google Scholar]
- 13.Zou G, Xu P, Zhu L, Ding S, Zhang X. Comparison of subsequent pregnancy outcomes after surgery for adnexal masses performed in the first and second trimester of pregnancy. Int J Gynaecol Obstet. 2020;148:305–9. doi: 10.1002/ijgo.13065. [DOI] [PubMed] [Google Scholar]
- 14.Ye P, Zhao N, Shu J, Shen H, Wang Y, Chen L, et al. Laparoscopy versus open surgery for adnexal masses in pregnancy: A meta-analytic review. Arch Gynecol Obstet. 2019;299:625–34. doi: 10.1007/s00404-018-05039-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sasaki KJ, Miller CE. Adnexal torsion: Review of the literature. J Minim Invasive Gynecol. 2014;21:196–202. doi: 10.1016/j.jmig.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 16.Rackow BW, Patrizio P. Successful pregnancy complicated by early and late adnexal torsion after in vitro fertilization. Fertil Steril. 2007;87:12.e9–12. doi: 10.1016/j.fertnstert.2006.05.091. [DOI] [PubMed] [Google Scholar]
- 17.Dawood MT, Naik M, Bharwani N, Sudderuddin SA, Rockall AG, Stewart VR. Adnexal torsion: Review of radiologic appearances. Radiographics. 2021;41:609–24. doi: 10.1148/rg.2021200118. [DOI] [PubMed] [Google Scholar]
- 18.Bridwell RE, Koyfman A, Long B. High risk and low prevalence diseases: Ovarian torsion. Am J Emerg Med. 2022;56:145–50. doi: 10.1016/j.ajem.2022.03.046. [DOI] [PubMed] [Google Scholar]
- 19.Daykan Y, Bogin R, Sharvit M, Klein Z, Josephy D, Pomeranz M, et al. Adnexal torsion during pregnancy: Outcomes after surgical intervention-a retrospective case-control study. J Minim Invasive Gynecol. 2019;26:117–21. doi: 10.1016/j.jmig.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 20.Djavadian D, Braendle W, Jaenicke F. Laparoscopic oophoropexy for the treatment of recurrent torsion of the adnexa in pregnancy: Case report and review. Fertil Steril. 2004;82:933–6. doi: 10.1016/j.fertnstert.2004.03.048. [DOI] [PubMed] [Google Scholar]
- 21.Rizzo AG. Laparoscopic surgery in pregnancy: Long-term follow-up. J Laparoendosc Adv Surg Tech A. 2003;13:11–5. doi: 10.1089/109264203321235403. [DOI] [PubMed] [Google Scholar]