Abstract
Tuberculous meningitis is an infectious disease with high mortality. Literature describing intrathecal therapy for tuberculous meningitis is scarce. We herein report a case of refractory tuberculous meningitis in a 52-year-old woman with underlying neuropsychiatric systemic lupus erythematosus. Despite systemic treatment with anti-tuberculosis drugs and dexamethasone, her meningeal irritation deteriorated. Intrathecal isoniazid and prednisolone administration was therefore initiated, and the symptoms of severe meningeal irritation improved along with head magnetic resonance imaging and cerebrospinal fluid findings. This case report highlights the efficacy of intrathecal isoniazid and steroid injections for refractory tuberculous meningitis, particularly in patients with severe meningeal irritation.
Keywords: tuberculous meningitis, intrathecal injection, neuropsychiatric systemic lupus erythematosus (NPSLE)
Introduction
Tuberculous meningitis is a severe extrapulmonary tuberculosis lesion wherein the tubercle bacillus is disseminated into the central nervous system (CNS). Mortality rates are reported to be as high as 22.8% (1) to 42.1% (2), and many patients have a refractory subclinical course.
We herein report a case of refractory tuberculous meningitis in a patient suffering from severe meningeal irritation that improved after intrathecal administration of isoniazid and steroids.
Case Report
A 52-year-old Japanese woman had been visiting the hospital for neuropsychiatric systemic lupus erythematosus (NPSLE) since she was 29 years old and had been taking prednisolone (1.5 mg) and azathioprine (100 mg). She presented with unintentional weight loss (from 50 kg to 45 kg in 3 months), an intermittent fever of approximately 38°C for 2 months, muscle weakness of the right upper extremity, numbness of the right face, and slurred speech.
Magnetic resonance imaging (MRI) of the head showed an abnormal signal in the left parietal lobe, but stroke was ruled out due to the gradual progression of symptoms and no obvious stenosis in the major vessels. However, anorexia and vomiting further occurred, and the patient was transferred to our hospital by ambulance.
At the time of admission, the patient's vitals were as follows: body temperature, 37.8°C; blood pressure, 113/75 mmHg; heart rate, 101 bpm; respiratory rate, 16 breaths per minute; and oxygen saturation, 96% on room air. The patient had right facial paralysis and right upper extremity muscle weakness. The laboratory findings were as follows: white blood cells, 4,100 /μL with 87.5% neutrophils; erythrocytes, 277×104/μL; Hb, 8.6 g/dL; platelets, 51.9×104/μL; C-reactive protein, 2.19 mg/dL; serum total protein, 8.0 g/dL; albumin, 3.0 g/dL; lactate dehydrogenase, 266 IU/L; aspartate aminotransferase, 34 IU/L; alanine aminotransferase, 13 IU/L; blood urea nitrogen, 12 mg/dL; creatinine, 0.61 mg/dL; sodium, 127 mmol/L; potassium, 4.2 mmol/L, and positive findings on T-SPOT.TB [an interferon (IFN)-γ release assay].
Chest computed tomography (CT) showed randomly distributed miliary nodules in the bilateral lung fields. A cerebrospinal fluid (CSF) examination revealed elevated cell counts (93 /μL), decreased glucose (39 mg/dL) and an elevated adenosine deaminase value (12.7 U/L), with no findings suggestive of other bacterial or fungal infections.
Based on these findings with the presence of an immunosuppressive background, miliary tuberculosis with meningitis was suspected, and oral isoniazid (300 mg), rifampicin (450 mg), ethambutol (500 mg), and pyrazinamide (1.5 g) were promptly administered in combination with intravenous dexamethasone 0.4 mg/kg/day. Soon thereafter, acid-fast bacterial staining and polymerase chain reaction (PCR) for Mycobacterium tuberculosis were both positive in the sputum specimen but both negative in the CSF specimen. Mycobacterium tuberculosis was subsequently isolated in the sputum specimen and showed no drug resistance against anti-tuberculosis drugs. Therefore, a diagnosis of miliary tuberculosis with possible tuberculous meningitis was achieved.
The dose of intravenous dexamethasone was reduced by 0.1 mg/kg every other week; however, a fever and headache became apparent. Despite improvement in chest CT findings of the lung, muscle weakness in the right upper extremity relapsed. Exacerbation of meningitis was considered, and oral levofloxacin (500 mg) was added. However, her symptoms did not improve, and the CSF cell count increased.
Head MRI on day 30 showed increased meningitis lesions. Considering that meningitis was poorly controlled, she was then treated with methylprednisolone 500 mg for 3 days followed by intravenous dexamethasone 0.4 mg/kg, oral levofloxacin was increased to 750 mg, and oral linezolid (600 mg) was added. However, as she continued to have severe headaches and nausea, a lumbar spinal drain tube was placed on day 34 to reinforce meningitis treatment by initiating daily intrathecal administration of isoniazid 100 mg and prednisolone 20 mg. After the administration of the intrathecal injection, the fever resolved quickly, and the headaches and nausea ameliorated. Systemic steroids were subsequently decreased and switched to oral dexamethasone 0.1 mg/kg on day 55. Intrathecal injection ended with drain removal on day 63 after improvement in the head MRI findings was confirmed.
However, two days later, she developed a fever of 40°C, and severe meningeal irritation required the intervention of a palliative care team. Therefore, a lumbar spinal drain was placed again, and the intrathecal injection was initially resumed with 100 mg isoniazid and 15 mg prednisolone, followed by a gradual decrease in prednisolone. Due to leakage of spinal fluid from the puncture site, the drain was removed on day 76, and drugs were administered via puncture every few days. Throughout hospitalization, spinal fluid tests were negative for secondary hospital-acquired meningitis. Oral systemic steroids were also gradually decreased. After the final intrathecal injection on day 108, meningeal irritation was within the control range, and the patient was discharged on day 140 after completing linezolid medication on day 133. After discharge from the hospital, her symptoms remained stable, and levofloxacin was discontinued at the time of the outpatient visit, followed by ethambutol and pyrazinamide. The patient continued to receive isoniazid and rifampicin without relapse.
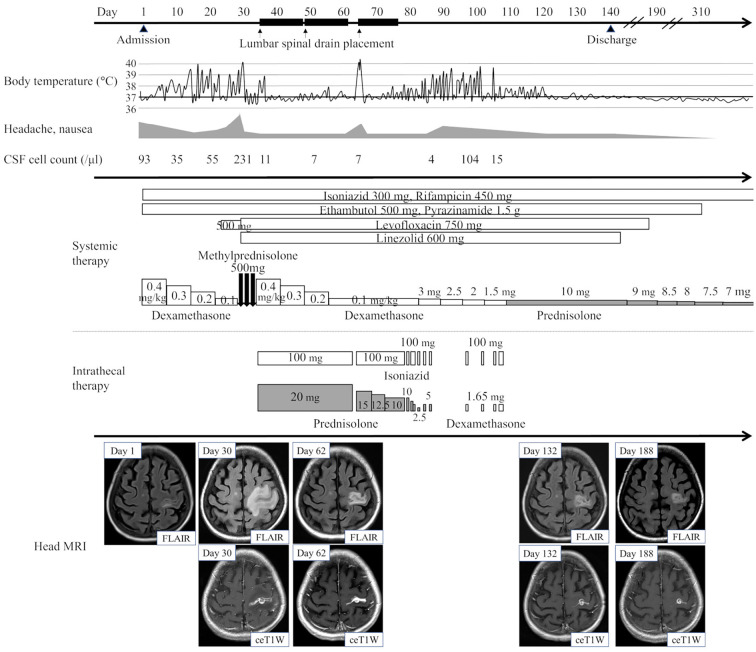
The clinical course is shown in Figure.
Figure.
Clinical course of the present case. CSF: cerebrospinal fluid, FLAIR: fluid-attenuated inversion recovery, ceT1W: contrast-enhanced T1-weighted imaging
Discussion
The present report describes a case of refractory tuberculous meningitis with severe meningeal irritation successfully treated with intrathecal isoniazid and steroid administration. CNS symptoms, a high fever, a high dose of corticosteroids, and abnormal CSF findings can be clues for coexisting infectious meningitis in patients with underlying SLE and can help distinguish NPSLE manifestations (3). The presence of blood-brain barrier (BBB) dysfunction associated with antibody-induced immune responses has been suggested in NPSLE. Neuropathy due to the infiltration of inflammatory molecules and cells into the brain associated with BBB destruction and the pathogenic role of inflammatory cytokines as well as chemokines have also been implicated (4). These background factors may have contributed to the excessive immune response in the present case, which was accompanied by CNS infection with tuberculosis and subsequent severe symptoms, resulting in a refractory and treatment-resistant course of the disease.
Furthermore, altered consciousness and altered sensorium were poor prognostic factors in this patient (1). In patients with tuberculous meningitis, adjunctive systemic corticosteroid therapy with dexamethasone or prednisolone is recommended (5). In the present case, the detected M. tuberculosis was sensitive to all anti-mycobacterium drugs, and CT findings in the lung fields improved, indicating that the choice of systemic anti-tuberculosis drugs was not problematic. However, the patient suffered from tremendous meningeal irritation, and meningitis was not controlled with systemic drug treatment. Therefore, we decided to perform intrathecal injection treatment with isoniazid and steroids. Although isoniazid has been reported to have a good CSF penetration rate of 80% to 90%, the concentration of the drug in the CSF was not evaluated in this case. Isoniazid intrathecal infusion was initiated with the expectation of an enhanced bactericidal effect. To prevent the appearance of drug-induced aseptic meningitis (6), we used steroids in combination with isoniazid. In addition, intrathecal steroid infusion was performed, since the systemic administration of steroids had failed to control meningeal irritation unless high doses were used. Long-term use of high-dose systemic steroids carries a risk of many side effects and may be disadvantageous for controlling infection.
The number of tubercle bacilli in the spinal fluid of this clinically diagnosed tuberculous meningitis case was considered to be low compared to that of confirmed cases. In addition, repeated spinal fluid examinations performed during the course of treatment never detected M. tuberculosis in all of the staining, culture, and PCR tests, and anti-tuberculosis drug failure was not suspicious from an antimicrobial point of view. Therefore, the severe meningeal irritation was suggested to have been largely caused by an intense immunological response. Serum complement titers and autoantibodies were continuously evaluated for NPSLE activity, but there were no findings that suggested disease progression. Topical administration of steroids appears to be effective in controlling severe meningeal irritation by suppressing the excessive immune response.
The combination of intrathecal administration of isoniazid and prednisolone has been reported to be associated with a reduced mortality rate (7), although little is known about its efficacy. Intrathecal treatment for tuberculous meningitis is not mentioned in any of the major guidelines, and treatments are not yet standardized. Literature references to intrathecal injection are limited, and the specific dosage, as well as the method of administration, have not been established. Furthermore, there is little literature discussing the role of isoniazid and steroids in intrathecal injections.
In conclusion, the present case demonstrates the efficacy of intrathecal isoniazid and steroids for tuberculous meningitis, especially in patients with severe meningeal irritation.
Written informed consent was obtained from the patient.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Wen L, Li M, Xu T, Yu X, Wang L, Li K. Clinical features, outcomes and prognostic factors of tuberculous meningitis in adults worldwide: systematic review and meta-analysis. J Neurol 266: 3009-3021, 2019. [DOI] [PubMed] [Google Scholar]
- 2.Navarro-Flores A, Fernandez-Chinguel JE, Pacheco-Barrios N, Soriano-Moreno DR, Pacheco-Barrios K. Global morbidity and mortality of central nervous system tuberculosis: a systematic review and meta-analysis. J Neurol 269: 3482-3494, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen J, Feng X, Wang H, et al. Discriminating infectious meningitis versus neuropsychiatric involvement in patients with systemic lupus erythematosus: a single-center experience. Clin Rheumatol 34: 365-369, 2015. [DOI] [PubMed] [Google Scholar]
- 4.Deijns SJ, Broen JCA, Kruyt ND, et al. The immunologic etiology of psychiatric manifestations in systemic lupus erythematosus: a narrative review on the role of the blood brain barrier, antibodies, cytokines and chemokines. Autoimmun Rev 19: 102592, 2020. [DOI] [PubMed] [Google Scholar]
- 5.Nahid P, Dorman SE, Alipanah N, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America clinical practice guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis 63: e147-e195, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morís G, Garcia-Monco JC. The challenge of drug-induced aseptic meningitis revisited. JAMA Intern Med 174: 1511-1512, 2014. [DOI] [PubMed] [Google Scholar]
- 7.Li K, Wang L, Wen L, Wang J, Li M. Intrathecal therapy for tuberculous meningitis: propensity-matched cohort study. Neurol Sci 43: 2693-2698, 2022. [DOI] [PubMed] [Google Scholar]