Abstract
An antigenic double mutant of rabies virus (challenge virus standard [CVS] strain) was selected by successive use of two neutralizing antiglycoprotein monoclonal antibodies, both specific for antigenic site III. This mutant differed from the original virus strain by two amino acid substitutions in the ectodomain of the glycoprotein. The lysine in position 330 and the arginine in position 333 were replaced by asparagine and methionine, respectively. This double mutant was not pathogenic for adult mice. When injected intramuscularly into the forelimbs of adult mice, this virus could not penetrate the nervous system, either by the motor or by the sensory route, while respective single mutants infected motoneurons in the spinal cord and sensory neurons in the dorsal root ganglia. In vitro experiments showed that the double mutant was able to infect BHK cells, neuroblastoma cells, and freshly prepared embryonic motoneurons, albeit with a lower efficiency than the CVS strain. Upon further incubation at 37°C, the motoneurons became resistant to infection by the mutant while remaining permissive to CVS infection. These results suggest that rabies virus uses different types of receptors: a molecule which is ubiquitously expressed at the surface of continuous cell lines and which is recognized by both CVS and the double mutant and a neuron-specific molecule which is not recognized by the double mutant.
Tissue tropism of a virus is first determined by the interaction of viral surface protein(s) with molecules expressed at the surface of target cells. Expression of such molecules in a limited group of differentiated tissues restricts the tropism of a virus. Rabies virus is a clear example of such a situation. This enveloped virus, whose genome is a nonsegmented negative-strand RNA, belongs to the rhabdovirus family. The genome codes for five proteins, one of which, glycoprotein (G), is exposed at the surface of the virion (29). In vitro, the virus is able to infect various types of cells (19). In vivo its tropism is mostly restricted to neurons. However, after intramuscular inoculation, rabies virus can simultaneously infect neurons and muscle cells (15). Replication in muscle cells, which is observed particularly with street rabies viruses, is not required for infection of the nervous system (NS) (6). During the course of the NS invasion, only neurons contain viral antigens. This specificity of neuronal infection led us to postulate the existence of specific receptors for rabies virus at the surface of neurons.
Indirect evidence of specific interactions between G and neuronal molecules has been found by the use of antigenic mutants. Selection of viruses mutated in the G gene is possible by the isolation of mutants resistant to neutralization by monoclonal antibodies (MAbs) from among a sensitive population. On the basis of their reactivity toward a collection of MAbs, MAb-resistant (MAR) mutants have been classified into different groups which define antigenic sites (4). Systematic inoculation of mice with MAR mutants showed that few of them exhibited a drastic modification of pathogenicity. All of these mutants had a substitution of their arginine at position 333 of G (21). This mutation affected antigenic site III and generated viruses avirulent for all immunocompetent adult animals tested. The only exception concerned skunks, which have been reported to be susceptible to infection by this type of mutant (25), but these results have not been confirmed. To understand the reasons for this lack of pathogenicity, one of these avirulent mutants (AvO1), selected from the challenge virus standard (CVS) strain, has been studied in detail. All results obtained from mice support the idea that AvO1 is able to penetrate the NS but can infect only a subset of neurons (7). Following intramuscular injection, AvO1 as CVS infects motor and sensory neurons with the same efficiency. However, unlike CVS, the mutant does not infect other neurons at later times of infection, either in the spinal cord or in the brain (6). After intranasal inoculation, AvO1 and CVS infect first neurons of the olfactory epithelium. From there, AvO1 is transmitted to a few categories of neurons connected to olfactory receptor cells (i.e., periglomerular neurons in the olfactory bulb and neurons of the horizontal diagonal band in the brain), while CVS invades most categories of neurons of the olfactory system (mitral cells, neurons of the internal plexiform layer in the olfactory bulb and anterior olfactory nucleus, and periglomerular cells and neurons of the horizontal diagonal band) (12). In the case of AvO1, restriction of viral propagation leaves time for the immune system to develop a specific response which leads to elimination of the virus from the central NS (CNS). These results indicate that AvO1 matures from olfactory receptor cells and suggest that the mutation prevents penetration in a subset of connected neurons (12).
Antigenic site III has been described as covering amino acids 330 to 338 (21). Assuming that other amino acids located close to position 333 are also implicated in the ability of the virus to infect neurons, we selected MAR mutants with two mutations in site III and studied their residual neuroinvasiveness. This paper describes the selection and molecular characterization of an antigenic double mutant selected from the CVS strain of rabies virus. It demonstrates the reduced capacity of this mutant to infect primary cultures of rat embryonic motoneurons and its inability to invade the mouse NS after intramuscular inoculation.
MATERIALS AND METHODS
Cells and virus.
BSR cells, derived from baby hamster kidney (BHK) cells, were grown in Glasgow’s modified minimal essential medium supplemented with 10% calf serum at 37°C in a 5% CO2 incubator. NG108-15 (mouse neuroblastoma N18 × rat glioma C6) cells were cultivated in Dulbecco’s modified Eagle’s medium (DMEM; GIBCO-BRL) plus 10% fetal bovine serum (17).
The CVS strain of rabies and antigenic mutants were multiplied by infecting BSR cells at a multiplicity of infection (MOI) of 0.1 PFU per cell. Infection proceeded for 72 h at 37°C in minimal essential medium supplemented with 2% calf serum. Supernatants were collected, centrifuged at a low speed to discard cell debris, and frozen in aliquots at −70°C. The titers were determined as already described (18). Viruses were concentrated according to Gaudin et al. (9).
Antibodies and antigenic mutants.
Antiglycoprotein MAbs 50AC1 and 50AD1 were isolated after fusion of myeloma cells with spleen cells of a BALB/c mouse immunized with β-propiolactone-inactivated CVS. Their characteristics were described previously (28).
Antigenic mutants were selected for their resistance to neutralization by MAbs according to a previously described procedure (21). They were isolated from revertant clones of the AvO10 mutant or from RK4 (21, 28).
Sequencing.
Nucleotide sequences of the selected mutants were established according to the procedure described by Raux et al. (18).
Animal experiments.
All experiments were performed with 6-week-old female Swiss mice (Centre d’Elevage et de Recherche. Janvier, Legenest St.-Isle, France).
For the pathogenicity tests, five mice were intracerebrally injected with 30-μl aliquots containing 103 PFU of each virus. Animals were kept under observation for 21 days. The surviving animals were challenged at day 28 by the intramasseter route with 50 μl of CVS containing 103 50% lethal doses (LD50).
The penetration experiments were conducted according to procedures already described (6). Briefly, 10 μl (108 PFU) of virus was injected into the forelimb. Animals were sacrificed 30 h later. The thoracic portion of the spinal cord and the corresponding dorsal root ganglia ipsilateral to the inoculated member were dissected as one piece and directly frozen in dry ice. Serial sections of tissues were made with a cryostat microtome (Instrument Company Ltd., Huntingdon, England) and recovered on gelatin-treated slides. They were fixed with acetone and treated with fluorescein isothiocyanate-conjugated antinucleocapsid antibodies (Diagnostic Pasteur, Paris, France).
Primary cultures of embryonic rat motoneurons.
Spinal cord motoneurons were prepared according to the technique described by Ternaux and Portalier (24), with slight modifications. Briefly, they were isolated from 15- to 17-day-old Wistar rat embryos (Centre d’Elevage et de Recherche Janvier). A pregnant female was sacrificed, and its fetuses were removed under sterile conditions. The spinal cord was dissected and kept in calcium- and magnesium-free phosphate-buffered saline (PBS−; GIBCO-BRL). The meninges were carefully removed, and the tissue was transferred into fresh PBS−. After being sectioned into small pieces, the tissue was incubated in PBS− containing trypsin (0.025%; Sigma) and DNase I (0.005%; Boehringer) for 30 min at 37°C. After centrifugation at 300 × g for 7 min, the cells were roughly dissociated in a siliconized Pasteur pipette and incubated in PBS− containing DNase I (0.005%) for 15 min at 37°C. After centrifugation, the pellet was resuspended in Hanks’ balanced salt solution (HBSS; GIBCO-BRL), and the cells were mechanically dissociated with fire-polished siliconized Pasteur pipettes of successively decreasing internal diameters. The cell suspension was placed at the top of two cushions of Nycoprep 1.15 (Nycomed, Oslo, Norway) in HBSS (20% above 60%) and then centrifuged at 2,000 × g for 20 min at 4°C. Cells concentrated at the HBSS–Nycoprep 20% interface were collected and, after dilution in HBSS and centrifugation, resuspended in DMEM-F12 medium (GIBCO-BRL) supplemented with insulin (5 μg/ml), human transferrin (100 μg/ml), putrescine (0.1 mM), progesterone (40 nM), and estradiol (1 pM) (all furnished by Sigma), d-glucose (33 mM) and sodium bicarbonate (24 mM) (obtained from Prolabo), and l-glutamine (2 mM) and gentamicin (100 μg/ml) (purchased from GIBCO-BRL); the pH was adjusted to 7.4. This medium is referred to as defined medium. Cell density was adjusted from 3 × 105 cells/ml for short-term cultures to 3 × 106 cells/ml for long-term cultures. Then, 100 μl of this suspension was plated onto glass coverslips treated successively with poly-l-lysine (Sigma; 5 μg/ml) and laminin (Sigma; 2 μg/ml). Coverslips were placed individually into petri dishes and incubated at 37°C in a 5% CO2 incubator. Defined medium was added 1 h later and replaced daily. Morphometric, immunological, and chemical analyses performed on these preparations indicated that 90 to 95% of the cells had properties of motoneurons (2a).
Infection of motoneurons.
After various times of culturing, the motoneurons were infected with cell culture supernatants of CVS and antigenic mutants. The viral inoculum was adjusted to 2 × 106 PFU/coverslip after dilution in defined medium. After a 30-min adsorption period at room temperature, the inoculum was removed and the motoneurons were covered with defined medium and incubated for 24 h at 37°C.
Immunofluorescence.
At 24 h after infection, the motoneurons were fixed for 10 min in 3.7% formaldehyde in phosphate-buffered saline (PBS) and then for 5 min in 3.7% formaldehyde–0.1% Triton X-100 in PBS. After three washes in PBS, cells were incubated with a monoclonal mouse anti-MAP2 antibody (Sigma; 1/100 in PBS) overnight at 4°C. To eliminate unbound primary antibody, cells were washed three times with PBS and then incubated in a mixture of rabbit anti-rabies nucleocapsid conjugated to fluorescein isothiocyanate (Diagnostic Pasteur; 1/20 in PBS) and donkey anti-mouse immunoglobulin G conjugated to tetramethyl rhodamine isothiocyanate (Jackson Immunoresearch; 1/100 in PBS) for 3 h at 37°C. The coverslips were washed three times in PBS and mounted upside down onto glass slides with Immu-mount (Shandon). About 103 living motoneurons were counted with the rhodamine filter at a ×40 magnification. Infected cells were identified with the fluorescein filter.
RESULTS
Selection of an antigenic avirulent double mutant.
All avirulent mutants isolated from different rabies virus strains carry a single substitution in the glycoprotein, where arginine 333 is replaced by cysteine, glutamine, glycine, leucine, methionine, or serine in CVS (21, 28), by isoleucine in Evelyn-Rokitnicki-Abelseth (ERA) (8), and by glutamate or serine in street Alabama Dufferin (SAD) (11). An antigenic mutant carrying a lysine at position 333 was selected from the SADBern strain. This mutant was avirulent in mice after intramuscular inoculation but retained residual pathogenicity by the intracerebral route (11), like a mutant isolated from the CVS strain (28). These results suggest that a positive charge at position 333 might be important in the pathogenic process. A further basic amino acid, the lysine at position 330, is present in antigenic site III (Fig. 1). Two MAR mutants with a substitution at that position were selected with appropriate MAbs: F69, which has a threonine (28), and RK4, which has an asparagine (Table 1). These two mutants were fully pathogenic for adult mice. They were partially neutralized by MAbs 28AD2 and 50AD1, whereas MAR mutants with a substitution at position 333 could not be neutralized by these antibodies.
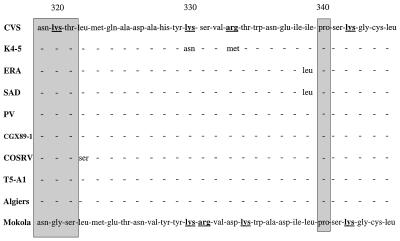
FIG. 1.
Conservation of antigenic site III in laboratory and wild-type strains of rabies virus as well as Mokola virus (26), a rabies-related virus. Sequences are shown for fixed strains CVS (32), ERA (1), SAD (5), and Pasteur virus (PV) (27) and for wild-type strains CGX89-1 (2), COSRV (14), T5-A1 (16), and Algiers (4). The K4-5 sequence was determined in this study. Positively charged amino acids are in bold and are underlined. The glycosylation site and the proline are boxed.
TABLE 1.
Characteristics of CVS and mutants having one or two substitutions in antigenic site III
| Virus | Selecting MAb | Amino acid at position:
|
LD50 i.c.a (PFU/ml) | |
|---|---|---|---|---|
| 330 | 333 | |||
| CVS | Lysine | Arginine | 10 | |
| RK4 | 50AC1 | Asparagine | Arginine | 10 |
| RL1 | 248-8 | Lysine | Methionine | >106 |
| K4-5 | 50AD1 | Asparagine | Methionine | >106 |
LD50 i.c., 50% lethal dose administered intracerebrally.
We selected an additional mutation at position 333 from mutant RK4 by using MAb 50AD1. The resulting mutant, K4-5, carried two amino acid substitutions: lysine to asparagine and arginine to methionine at positions 330 and 333, respectively (Table 1). Intracerebral inoculation of K4-5 indicated that this mutant was nonpathogenic for adult mice. Control experiments with mutants having one or the other substitution, RK4 and RL1, showed that RK4 (K330N) was pathogenic and that RL1 was avirulent (R333M) (28) (Table 1).
Infection of the mouse NS after peripheral inoculation.
In order to test if the presence of these two mutations in the glycoprotein gene had an effect on the early events of the infection in animals, the double and respective single mutants were intramuscularly injected into the forelimbs of adult mice. By this route of inoculation, it has been shown that AvO1 (the prototype of avirulent mutants) was able to infect motoneurons in the spinal cord and sensory neurons in the dorsal root ganglia as efficiently as CVS (6). Both viruses directly penetrated nerve endings without prior multiplication in the muscle at the site of inoculation. At 30 h after inoculation of a high virus dose (Table 2), the thoracic portion of the spinal cord and the corresponding dorsal root ganglia were dissected from infected animals. At this time, only primary infected neurons can be detected (6). Serial sections of both tissues were processed for detection of rabies virus antigens. Like the pathogenic viruses CVS and RK4, the avirulent mutant RL1 infected both motoneurons and sensory neurons during the first cycle of infection in the mouse NS (Table 2). All infected neurons were located ipsilateral to the inoculation site (data not shown). The double mutant, on the other hand, did not infect any neurons in four injected mice, either in the spinal cord or in the ganglia. A fifth mouse exhibited infection of only three neurons in one dorsal root ganglion (Table 2). It should be noted that these mice received a 10-fold-higher virus inoculum than did those injected with the CVS strain.
TABLE 2.
Infection of mouse dorsal root ganglia (DRG) and spinal cord (SC) after peripheral inoculation of CVS and antigenic mutantsa
| Mouse | No. of infected neurons 30 h after inoculation of (PFU):
|
|||||||
|---|---|---|---|---|---|---|---|---|
| CVS (4 × 108)
|
RK4 (4 × 108)
|
RL1 (4 × 108)
|
K4-5 (4 × 109)
|
|||||
| DRG | SC | DRG | SC | DRG | SC | DRG | SC | |
| 1 | 48 | 80 | 18 | 19 | 50 | 37 | 0 | 0 |
| 2 | 41 | 87 | 16 | 58 | 36 | 39 | 0 | 0 |
| 3 | 18 | 9 | 19 | 66 | 30 | 35 | 0 | 0 |
| 4 | 15 | 13 | 44 | 44 | 0 | 0 | ||
| 5 | 25 | 53 | 3 | 0 | ||||
Ten microliters of concentrated virus was inoculated into the right forelimbs of adult mice. Each group of two values was obtained from the same animal.
Infection of neuroblastoma cells by avirulent mutants.
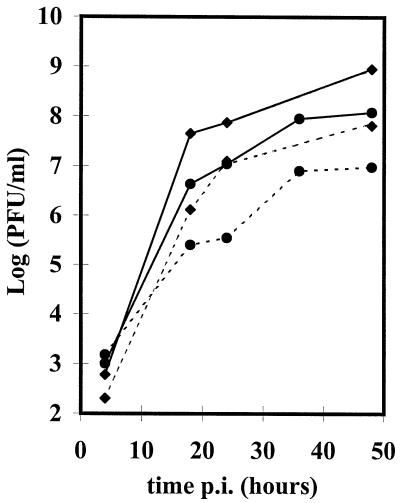
To test the capacity of the double mutant to multiply in continuous cell lines, BSR and NG108-15 cells were infected with CVS or antigenic mutant at an MOI of 5 or 6 PFU/cell. Virus supernatants were titrated on BSR cells (Fig. 2). Rabies virus-infected cells were detected by immunofluorescence 18 h after adsorption. At this MOI, 100% of BSR cells were infected with both viruses. K4-5 infected only 50% of NG108-15 cells, while CVS infected 100% of these cells, suggesting that the penetration of the mutant was slightly affected. In all cases, the intensities of the fluorescence 18 h after infection were comparable, an indication that protein synthesis proceeded at the same rate once penetration had occurred. With both viruses, production of virus was lower in neuroblastoma cells than in BSR cells. Production of mutant virus was also lower than that of CVS on both types of cells. For instance, at 48 h after infection, production of virus with K4-5 and CVS was equal, respectively, to 10 and 65 PFU/cell on NG108-15 cells and to 120 and 900 PFU/cell on BSR cells.
FIG. 2.
One-step growth curves for CVS (⧫) and K4-5 (•) on BSR (——) and NG108-15 (–––) cells. The MOIs were 5 (CVS) and 6 (K4-5). After 1 h of adsorption at room temperature, the inoculum was removed and cell layers were washed before the addition of the medium. Supernatants were changed after 4 h in order to remove desorbed virus. Incubation was done at 37°C. p.i., postinfection.
Progressive resistance of spinal motoneurons to infection by the double mutant.
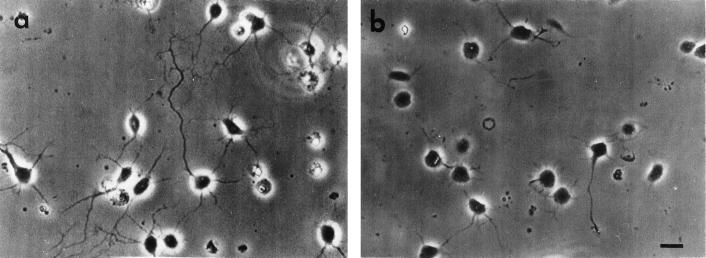
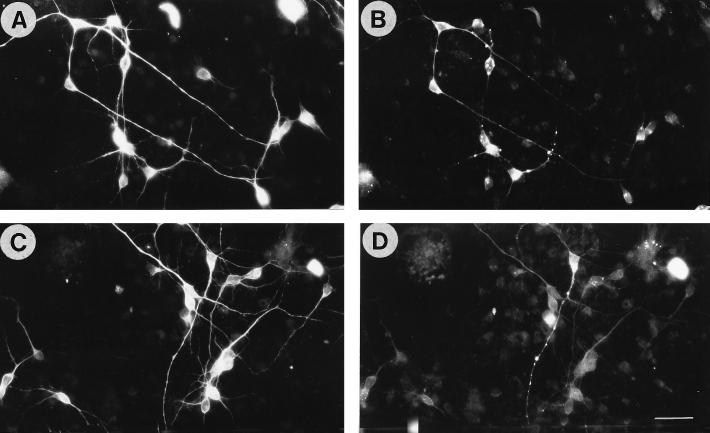
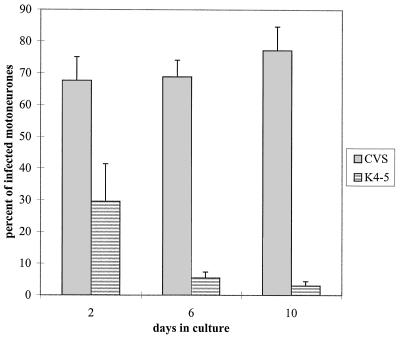
We decided to monitor the infectious process in primary cultures of spinal motoneurons. These motoneurons were isolated from the spinal cord of 15- to 17-day-old rat fetuses and purified by differential centrifugation as described in Materials and Methods. Under our conditions, where defined medium was changed daily, motoneurons could be maintained in cultures for up to 2 weeks (Fig. 3a). Immunocytochemistry analysis performed on these cells with an antiacetylcholine antibody indicated that this cell population synthesized acetylcholine (Fig. 3b). Coverslips were seeded with 3 × 104 to 3 × 105 motoneurons on a poly-l-lysine- and laminin-treated surface. These motoneurons were infected with CVS or the double mutant at 2, 6, and 10 days after plating. At that stage, about 10% of the motoneurons were still alive. The inoculum size was standardized to 4 × 106 PFU/coverslip, but the real MOI could not be calculated because the virus also attached to the laminin substrate. Infection was stopped 24 h later, and infected neurons were counted by double-labeling immunofluorescence. These cells were identified as neurons by immunocytochemistry (Fig. 4A and C). At any stage of infection, between 68 and 77% of cells were infected with CVS (Fig. 4B and 5). On the contrary, the double mutant could infect only 30% of motoneurons after 2 days in cultures (Fig. 5). Then, the resistance to infection increased with time, and after 10 days in cultures, less than 3% of motoneurons were infected with the double mutant (Fig. 4D and 5). A similar experiment was performed on mouse spinal motoneurons purified from 13-day-old embryos. Following 6 days in cultures, the mouse motoneurons were infected for 24 h with CVS or the double mutant as described for rat motoneuron infection. After immunocytochemical processing, in the CVS-infected culture, 444 of 502 (88.4%) MAP2+ motoneurons contained rabies virus antigens, while in the double mutant-infected culture, only 7 of 505 (1.4%) MAP2+ motoneurons were positive for rabies virus antigens.
FIG. 3.
Purified rat embryonic spinal motoneurons in cultures. (a) Cultures of dissociated motoneurons were grown on glass coverslips coated with poly-l-lysine (0.005%) and laminin (0.001%) in the presence of DMEM-F12 medium with additives. Living cells were observed by phase-contrast microscopy 6 days after plating. (b) Immunoperoxidase detection of acetylcholine in the same culture of motoneurons after fixation with paraformaldehyde. Bar, 15 μm.
FIG. 4.
Infection of spinal motoneurons from rat embryos after 10 days in cultures with CVS or antigenic double mutant K4-5. Cells were plated on glass coverslips treated with poly-l-lysine and laminin, kept for 10 days, and then infected for 24 h with CVS (A and B) or K4-5 (C and D). Cultures were fixed and permeabilized before simultaneous detection of neurons (A and C) and viral antigens (B and D) by double-labeling immunofluorescence. Bar, 30 μm.
FIG. 5.
Rat embryonic spinal motoneurons acquire progressive resistance to infection with mutant K4-5 in vitro. Motoneurons were seeded on poly-l-lysine- and laminin-treated glass coverslips at a density of 3 × 104 to 3 × 105 cells per coverslip, depending on the culture time. They were infected at day 2, 6, or 10 with CVS or K4-5 for 24 h at 37°C. After fixation and permeabilization, neurons were identified with an anti-MAP2 mouse MAb, and infected cells were detected with a rabbit anti-rabies virus nucleocapsid antibody. The percentage of infected motoneurons was estimated as the ratio of the number of doubly-labeled cells to the number of MAP2-labeled cells (value estimated from 103 MAP2+ cells counted). The experiment was performed in quadruplicate.
DISCUSSION
It has been well documented that rabies virus infects most continous cell lines in vitro, while its tropism is restricted mostly to neurons in animals. In addition, pathogenic strains infect most neuronal populations in the CNS. Previous studies suggested the existence of two kinds of receptors used by rabies virus to attach to a target cell: ubiquitously distributed cell surface molecules and specific molecules present on a few cell lines and on some differentiated tissues (31). Ubiquitous receptors could be lipids and gangliosides (22, 23, 31), and a specific receptor could be the nicotinic acetylcholine receptor (13). However, since this complex is not present on many categories of neurons permissible for rabies virus, it cannot be the only receptor which mediates viral entry into neurons.
Previous work on the fixed strain CVS showed that point mutations in the glycoprotein gene leading to the replacement of arginine at position 333 generated avirulent viruses with a restricted capacity to propagate in the CNS (10, 12). These viruses were able to penetrate motoneurons and sensory neurons as efficiently as the original CVS strain after intramuscular injection, yet transneuronal transfer of the mutant viruses did not occur (6). On the contrary, the double mutant K4-5 (K330N-R333M) described here infected neither sensory neurons nor motoneurons by this route of inoculation. Since a mutation in the viral glycoprotein likely influences virus entry or eggress but not viral replication, these data suggest that the block occurs at an early step of the viral life cycle, such as binding, endocytosis, or fusion, reflecting a lack of interaction between the mutated glycoprotein and a neuronal component.
Using primary cultures of motoneurons, we were able to extend data obtained in the animal experiments. These neurons were isolated from rat embryonic spinal cord and were considered to be motoneurons on the basis of several criteria (see Results). In these cultures, we found that motoneuron susceptibility to K4-5 decreased to less than 3% after 10 days. Thus, the more the motoneurons survive in cultures, the more they are resistant to K4-5. This situation is reminiscent of what was observed for mice with mutants having a substitution at position 333 of the glycoprotein. Such mutants are still pathogenic for baby mice and multiply in their brains like the wild type (28). They lose the capability to invade the NS within the first 3 weeks after birth (unpublished data).
Experiments with established cell lines, BSR or neuroblastoma, did not reveal dramatic differences between CVS and K4-5, although the mutant was slightly affected in its capability to penetrate NG108-15 cells (at an MOI of 6, only 50% of the cells were infected). Although the fluorescence of infected cells was of a similar intensity, viral production was lower with the mutant than with CVS, probably because maturation and/or virus stability was affected by the mutations. With both viruses, viral production was lower in neuroblastoma cells. However, the multiplication of K4-5 and CVS in in vitro cell cultures was not dramatically different. Once again, this observation illustrates the difficulty in the use of any kind of established cell line to identify specific neuronal rabies virus receptors, because such cells express ubiquitous receptors. Recently, this problem was partly circumvented by the use of a binding assay with Sf21 insect cells, expressing the rabies virus glycoprotein at their surface, and several established cell lines. We demonstrated that only neuronal cell lines (including the one used in these studies) expressed specific binding sites for the rabies virus glycoprotein and that the two mutations present in K4-5 abolished this binding (28a). These binding sites might be “high-affinity” neuron-specific receptors for rabies to which the mutated glycoprotein could not bind (or to which it bound with a lower affinity insufficient to mediate the attachment of lepidoptera cells to neuroblastoma cells).
K4-5 differs from CVS by two amino acid substitutions in the ectodomain of the glycoprotein. These changes are located at positions 330 and 333, previously identified as belonging to antigenic site III (21). A partial amino acid sequence comparison of several laboratory and wild-type strains showed an almost complete conservation of antigenic site III (Fig. 1). Antigenic site III has been defined as a continuous and conformational site (4). This domain could be delineated by (i) a potential glycosylation site at position 319 (Fig. 1), which is present in all strains (1–3, 5, 27, 32) and which has been demonstrated to be used in CVS (30), and (ii) a proline at position 340 (this amino acid is known to cause bending in the secondary structure of proteins). Another argument in favor of the structural importance of this proline is the presence of the minor site a. Antigenic mutations at this site have been located at positions 342 and 343, and no change in the sensitivity of MAR mutants from minor site a and MAbs from site III, and vice versa, has been observed (4). Moreover, the structural organization of site III is also conserved in the glycoproteins of Mokola virus (26). This finding may be an indication of the importance of this region for the viability of the lyssaviruses.
The region from positions 320 to 340 contains two positively charged amino acids, with the exception of lysine at position 320, which is located in the Asn-X-Ser/Thr motif and which is probably masked by the sugar chain (Fig. 1). Substitution of these two residues with uncharged ones renders the virus unable to penetrate sensory neurons and motoneurons. Replacement of only one positively charged amino acid (in RK4 and AvO1 mutants) does not reduce the capacity of these mutants to infect these types of neurons, but in AvO1 it blocks transmission to interneurons (6).
The selection of antigenic mutants with a restricted capacity to infect neurons by use of neutralizing MAbs allowed the identification of two key amino acids for the penetration of rabies virus in neurons. It is likely that further key amino acids will also be implicated in the interaction of the viral glycoprotein with the cell receptor. The development of reverse genetics for the negative-strand RNA viruses and especially for rabies virus (20) has provided new tools for the study of amino acids implicated in interactions with the neuronal receptor(s). On the other hand, K4-5, by its inability to infect motoneurons and sensory neurons, will be useful for the identification of neuronal receptors for rabies virus.
ACKNOWLEDGMENTS
This work was supported by the CNRS through UPR 9053 (to P.C., A.F., and C.T.) and 9041 (to J.-P.T.).
We are indebted to Karin Kaelin for careful reading of the manuscript. We thank Jacqueline Bénéjean and Genevieve Payen for excellent technical assistance.
REFERENCES
- 1.Anilionis A, Wunner W H, Curtis P J. Structure of the glycoprotein gene in rabies virus. Nature (London) 1981;294:275–278. doi: 10.1038/294275a0. [DOI] [PubMed] [Google Scholar]
- 2.Bai X H, Warner C K, Fekadu M. Comparisons of nucleotide and deduced amino acid sequences of the glycoprotein genes of a Chinese street strain (CGX89-1) and a Chinese vaccine strain (3aG) of rabies virus. Virus Res. 1993;27:101–112. doi: 10.1016/0168-1702(93)90074-w. [DOI] [PubMed] [Google Scholar]
- 2a.Bataillé, S., P. Portalier, P. Coulon, and J. P. Ternaux. Influence of acetylcholinesterase on embryonic spinal rat motoneuron growth in culture: a quantitative morphometric study. Eur. J. Neurosci., in press. [DOI] [PubMed]
- 3.Benmansour A, Brahimi M, Tuffereau C, Coulon P, Lafay F, Flamand A. Rapid sequence evolution of street rabies glycoprotein is related to the highly heterogeneous nature of the viral population. Virology. 1992;187:33–45. doi: 10.1016/0042-6822(92)90292-w. [DOI] [PubMed] [Google Scholar]
- 4.Benmansour A, Leblois H, Coulon P, Tuffereau C, Gaudin Y, Flamand A, Lafay F. Antigenicity of rabies virus glycoprotein. J Virol. 1991;65:4198–4203. doi: 10.1128/jvi.65.8.4198-4203.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conzelmann K-K, Cox J H, Schneider L G, Thiel H-J. Molecular cloning and complete nucleotide sequence of the attenuated rabies virus SAD B19. Virology. 1990;175:485–499. doi: 10.1016/0042-6822(90)90433-r. [DOI] [PubMed] [Google Scholar]
- 6.Coulon P, Derbin C, Kucera P, Lafay F, Préhaud C, Flamand A. Invasion of the peripheral nervous systems of adult mice by the CVS strain of rabies virus and its avirulent derivative AvO1. J Virol. 1989;63:3550–3554. doi: 10.1128/jvi.63.8.3550-3554.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coulon P, Lafay F, Tuffereau C, Flamand A. The molecular basis for altered pathogenicity of lyssavirus variants. Curr Top Microbiol Immunol. 1994;187:69–84. doi: 10.1007/978-3-642-78490-3_4. [DOI] [PubMed] [Google Scholar]
- 8.Dietzschold B, Wunner W H, Wiktor T J, Lopes A D, Lafon M, Smith C L, Koprowski H. Characterization of an antigenic determinant of the glycoprotein that correlates with pathogenicity of rabies virus. Proc Natl Acad Sci USA. 1983;80:70–74. doi: 10.1073/pnas.80.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaudin Y, Ruigrok R W H, Tuffereau C, Knossow M, Flamand A. Rabies virus glycoprotein is a trimer. Virology. 1992;187:627–632. doi: 10.1016/0042-6822(92)90465-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jackson A C. Biological basis of rabies virus neurovirulence in mice: comparative pathogenesis study using the immunoperoxidase technique. J Virol. 1991;65:537–540. doi: 10.1128/jvi.65.1.537-540.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lafay F, Bénéjean J, Tuffereau C, Flamand A, Coulon P. Vaccination against rabies—construction and characterization of SAG2, a double avirulent derivative of SAD(Bern) Vaccine. 1994;12:317–320. doi: 10.1016/0264-410x(94)90095-7. [DOI] [PubMed] [Google Scholar]
- 12.Lafay F, Coulon P, Astic L, Saucier D, Riche D, Holley A, Flamand A. Spread of the CVS strain of rabies virus and of the avirulent mutant AvO1 along the olfactory pathways of the mouse after intranasal inoculation. Virology. 1991;183:320–330. doi: 10.1016/0042-6822(91)90145-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lentz T L, Benson R J J, Klimovicz D, Wilson P T, Hawrot E. Binding of rabies virus to purified Torpedo acetylcholine receptor. Mol Brain Res. 1986;1:211–219. doi: 10.1016/0169-328x(86)90027-6. [DOI] [PubMed] [Google Scholar]
- 14.Morimoto K, Patel M, Corisdeo S, Hooper D C, Fu Z F, Rupprecht C E, Koprowski H, Dietzschold B. Characterization of a unique variant of bat rabies virus responsible for newly emerging human cases in North America. Proc Natl Acad Sci USA. 1996;93:5653–5658. doi: 10.1073/pnas.93.11.5653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murphy F A, Bauer S P, Harrison A K, Winn W C., Jr Comparative pathogenesis of rabies and rabies-like viruses: viral infection and transit from inoculation site to the central nervous system. Lab Invest. 1973;28:361–376. [PubMed] [Google Scholar]
- 16.Nadindavis S A, Casey G A, Wandeler A I. A molecular epidemiological study of rabies virus in central Ontario and western Quebec. J Gen Virol. 1994;75:2575–2583. doi: 10.1099/0022-1317-75-10-2575. [DOI] [PubMed] [Google Scholar]
- 17.Nelson P, Clifford C, Nirenberg M. Synapse formation between clonal neuroblastoma × glioma hybrid cells and striated muscle cells. Proc Natl Acad Sci USA. 1976;73:123–127. doi: 10.1073/pnas.73.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raux H, Coulon P, Lafay F, Flamand A. Monoclonal antibodies which recognize the acidic configuration of the rabies glycoprotein at the surface of the virion can be neutralizing. Virology. 1995;210:400–408. doi: 10.1006/viro.1995.1356. [DOI] [PubMed] [Google Scholar]
- 19.Reagan K J, Wunner W H. Rabies virus interaction with various cell lines is independent of the acetylcholine receptor. Arch Virol. 1985;84:277–282. doi: 10.1007/BF01378980. [DOI] [PubMed] [Google Scholar]
- 20.Schnell M J, Mebatsion T, Conzelmann K K. Infectious rabies viruses from cloned cDNA. EMBO J. 1994;13:4195–4203. doi: 10.1002/j.1460-2075.1994.tb06739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seif I, Coulon P, Rollin P E, Flamand A. Rabies virulence: effect on pathogenicity and sequence characterization of rabies virus mutations affecting antigenic site III of the glycoprotein. J Virol. 1985;53:926–934. doi: 10.1128/jvi.53.3.926-934.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Superti F, Hauttecoeur B, Morelec M J, Goldoni P, Bizzini B, Tsiang H. Involvement of gangliosides in rabies virus infection. J Gen Virol. 1986;67:47–56. doi: 10.1099/0022-1317-67-1-47. [DOI] [PubMed] [Google Scholar]
- 23.Superti F, Seganti L, Tsiang H, Orsi N. Role of phospholipids in rhabdovirus attachment to CER cells. Arch Virol. 1984;81:321–328. doi: 10.1007/BF01310002. [DOI] [PubMed] [Google Scholar]
- 24.Ternaux J-P, Portalier P. Culture of hypoglossal cells dissociated from foetal and new-born rats. J Neurosci Methods. 1993;49:33–47. doi: 10.1016/0165-0270(93)90107-3. [DOI] [PubMed] [Google Scholar]
- 25.Tolson N D, Charlton K M, Stewart R B, Casey G A, Webster W A, MacKenzie K, Campbell J B, Lawson K F. Mutants of rabies virus in skunks: immune response and pathogenicity. Can J Vet Res. 1990;54:178–183. [PMC free article] [PubMed] [Google Scholar]
- 26.Tordo N, Bourhy H, Sather S, Ollo R. Structure and expression in the baculovirus of the Mokola virus glycoprotein: an efficient recombinant vaccine. Virology. 1993;194:59–69. doi: 10.1006/viro.1993.1235. [DOI] [PubMed] [Google Scholar]
- 27.Tordo N, Poch O, Ermine A, Keith G, Rougeon F. Walking along the rabies genome: is the large G-L intergenic region a remnant gene? Proc Natl Acad Sci USA. 1986;83:3914–3918. doi: 10.1073/pnas.83.11.3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tuffereau C, Leblois H, Bénéjean J, Coulon P, Lafay F, Flamand A. Arginine or lysine in position 333 of ERA and CVS glycoprotein is necessary for rabies virulence in mice. Virology. 1989;172:206–212. doi: 10.1016/0042-6822(89)90122-0. [DOI] [PubMed] [Google Scholar]
- 28a.Tuffereau, C., J. Bénéjean, A.-M. Roque Alfonso, A. Flamand, and M. K. Fishman. Neuronal cell surface molecules mediate specific binding to rabies virus glycoprotein expressed by a recombinant baculovirus on the surfaces of lepidoptera cells. J. Virol., in press. [DOI] [PMC free article] [PubMed]
- 29.Wagner R R, Rose J K. Rhabdoviridae: the viruses and their replication. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. Philadelphia, Pa: Lippincott-Raven; 1996. pp. 1121–1135. [Google Scholar]
- 30.Wunner W H, Dietzschold B, Smith C L, Lafon M, Golub E. Antigenic variants of CVS rabies virus with altered glycosylation sites. Virology. 1985;140:1–12. doi: 10.1016/0042-6822(85)90440-4. [DOI] [PubMed] [Google Scholar]
- 31.Wunner W H, Reagan K J, Koprowski H. Characterization of saturable binding sites for rabies virus. J Virol. 1984;50:691–697. doi: 10.1128/jvi.50.3.691-697.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yelverton E, Norton S, Obijeski J F, Goeddel D V. Rabies virus glycoprotein analogs: biosynthesis in Escherichia coli. Science. 1983;219:614–620. doi: 10.1126/science.6297004. [DOI] [PubMed] [Google Scholar]