Abstract
Background
Data on the effectiveness of BA.4/5 bivalent vaccine stratified by age and prior infection are lacking.
Methods
This test-negative study used data from individuals ≥5 years of age testing for SARS-CoV-2 with symptoms (15 September 2022 to 31 January 2023) at a large national retail pharmacy chain. The exposure was receipt of 2–4 wild-type doses and a BNT162b2 BA.4/5 bivalent vaccine (>2 months since last wild-type dose). The outcome was a positive SARS-CoV-2 test. Absolute (vs unvaccinated) and relative (vs 2–4 wild-type doses) vaccine effectiveness (VE) were calculated as (1 − adjusted odds ratio from logistic regression) × 100. VE was stratified by age and self-reported prior infection.
Results
Overall, 307 885 SARS-CoV-2 tests were included (7916 aged 5–11, 16 329 aged 12–17, and 283 640 aged ≥18 years). SARS-CoV-2 positivity was 39%; 21% were unvaccinated, 70% received 2–4 wild-type doses with no bivalent vaccine, and 9% received a BNT162b2 BA.4/5 bivalent dose. At a median of 1–2 months after BNT162b2 BA.4/5 bivalent vaccination, depending on age group, absolute VE was 22%–60% and was significantly higher among those reporting prior infection (range, 55%–79%) than not (range, no protection to 50%). Relative VE was 31%–64%.
Conclusions
BNT162b2 BA.4/5 bivalent showed early additional protection against Omicron-related symptomatic COVID-19, with hybrid immunity offering greater protection.
Keywords: bivalent, BA.4/5, Omicron, VE, effectiveness, BNT162b2, SARS-CoV-2, COVID-19, United States, test negative
The BNT162b2 BA.4/5 bivalent vaccine provided early additional protection against Omicron-related symptomatic COVID-19 among immunocompetent individuals aged ≥5 years when BA.4/5 and XBB-related sublineages were circulating. In general, effectiveness was highest among those self-reporting prior SARS-CoV-2 infection.
Omicron and its sublineages have comprised the majority of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) genomes sequenced by the Centers for Disease Control and Prevention (CDC) since December 2021 [1]. Omicron has key mutations that enhance immune escape and have resulted in reduced effectiveness of original Wuhan-Hu-1–encoding mRNA coronavirus disease 2019 (COVID-19) vaccines (hereafter referred to as “original wild-type” vaccines) [2–8]. Updated COVID-19 vaccines were developed to target both wild-type and Omicron BA.4/5 strains. The US Food and Drug Administration authorized a single dose of mRNA BA.4/5 bivalent vaccines as a booster for those who completed the primary vaccination series ≥2 months ago for individuals aged ≥12 years on 31 August 2022 and children aged 5–11 years on 11 October 2022. To date, real-world studies have suggested that a BA.4/5 bivalent vaccine improves protection against BA.4/5-related severe outcomes, including COVID-19–related hospitalization and death among adolescents [9] and adults [6, 9–14]. Only a few studies have reported effectiveness of a bivalent vaccine against Omicron-related symptomatic COVID-19 [13, 15–18], and these studies have not stratified effectiveness estimates by history of prior SARS-CoV-2 infection. Given >90% of US individuals have likely been infected with SARS-CoV-2 at least once [19], these data are needed to understand performance of Omicron-adapted vaccines. Furthermore, bivalent vaccine effectiveness estimates among 5–11 year olds are scarce [9]. To address these gaps, we estimated effectiveness of a Pfizer-BioNTech BNT162b2 BA.4/5 bivalent vaccine against Omicron-related symptomatic COVID-19 among those aged ≥5 years testing for SARS-CoV-2 at a large US pharmacy chain by age group and history of prior infection.
METHODS
We followed Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. The Advarra institutional review board approved the study (Pro00058582) and granted a waiver for informed consent under US Department of Health and Human Services regulation 45 CFR 46.104(d)(4) for research using deidentified data and a complete waiver of Health Insurance Portability and Accountability Act authorization.
Study Design and Participants
This test-negative case-control study was conducted at Walgreens, a US retail pharmacy chain where >35 million SARS-CoV-2 tests have been administered at >7100 locations. This analysis included (1) children aged 5–11 years who tested for SARS-CoV-2 at a Walgreens pharmacy between 26 October 2022 and 31 January 2023, and (2) individuals aged ≥12 years who were tested between 15 September 2022 and 31 January 2023. The beginning of each study period corresponds to 14 days after the authorization of BA.4/5 bivalent vaccines for each age group (ie, the earliest each age group could be considered vaccinated with a bivalent vaccine). Patients (or parents or guardians for children aged <18 years) completed an online appointment scheduler to select a Walgreens location and SARS-CoV-2 test type (real-time polymerase chain reaction [RT-PCR], rapid nucleic acid amplification test [NAAT], or rapid antigen) [20]. Records with only a rapid antigen test were not included. Availability of RT-PCR and rapid NAAT tests varied by location.
At the time of scheduling, demographic characteristics, symptoms, clinical history including comorbidities, prior SARS-CoV-2 infection, and COVID-19 vaccination history (including number received, dates for each [month and year], and manufacturer) were collected via a self-reported questionnaire (available in English or Spanish). Patients experiencing severe symptoms were directed to contact emergency services. Race and ethnicity were self-reported using categories defined by CDC [21]; the categories American Indian or Alaska Native and Native Hawaiian or Other Pacific Islander were combined into one group (Native) due to limited sample size. At the appointment, individuals self-collected swab specimens of the anterior nares under supervision of trained Walgreens staff. All specimens were placed into a collection tube. RT-PCR specimens were transferred to an accredited laboratory and rapid NAAT specimens were processed onsite using the Abbott ID Now test (sensitivity and specificity of each test are reported in Supplementary Table 4).
Records were excluded if the individual (1) received any non-mRNA vaccine, (2) received an Omicron-adapted vaccine other than the BNT162b2 BA.4/5 bivalent, (3) received >1 dose of BNT162b2 bivalent, (4) received only 1 original wild-type dose or their last original wild-type dose ≤2 months ago (ie, not eligible for a bivalent vaccine), (5) received a BNT162b2 bivalent dose ≤2 months after their last original wild-type dose (ie, not according to current guidelines), (6) received a BNT162b2 bivalent dose <14 days ago (ie, individuals were not considered vaccinated until ≥14 days), (7) declined to report vaccination status or self-reported fewer vaccines in the current questionnaire than in a prior questionnaire (completed between 1 January 2022 and 31 January 2023), (8) were immunocompromised or received >4 original wild-type doses, (9) had invalid SARS-CoV-2 test results, (10) self-reported a prior SARS-CoV-2 infection ≤3 months ago, or (11) did not report symptoms on the testing survey. Finally, to ensure that cases and controls included in the analysis had similar healthcare seeking behaviors, we also excluded those reporting testing related to future travel or employment screening and those who tested multiple times during the study window.
Exposure
COVID-19 vaccine history was determined using patient-reported data from the online questionnaire. To determine timing of vaccination, we ascertained whether the last dose was received in the past 14 days, or if received ≥14 days ago, the month and year of receipt. The exposure of interest was receipt of 2–4 original wild-type doses plus a BNT162b2 BA.4/5 bivalent vaccine ≥14 days before testing for SARS-CoV-2, with the most recent original wild-type dose received >2 months before the bivalent dose. For estimates of absolute vaccine effectiveness (VE), the unvaccinated were the reference group. Those who received 2–4 original wild-type doses >2 months ago but not a bivalent vaccine were the reference for relative VE estimates.
Outcomes
VE was evaluated by comparing the odds of vaccination among individuals testing positive for SARS-CoV-2 (cases) versus negative (controls) via RT-PCR or rapid NAAT.
Statistical Analysis
Patient characteristics were summarized using descriptive statistics stratified by SARS-CoV-2 test result and vaccination status. Differences between groups according to case status and bivalent vaccination status were evaluated using means and standard deviations for continuous variables, and frequencies and percentages for categorical variables.
Estimated VE was calculated as 1 minus the odds ratio from multivariable adjusted generalize estimating equations logistic regression models (clustered on US Census region of pharmacy), multiplied by 100. All VE estimates were stratified by age (5–11, 12–17, 18–49, 50–64, and ≥65 years). We tested for statistical interaction between bivalent vaccination status and self-reported prior infection >3 months ago (yes/no) in both the absolute and relative VE models. For relative VE we additionally tested for statistical interaction between bivalent vaccine status and time since last original wild-type dose (2–6 or ≥7 months). The following variables were considered for inclusion in adjusted models but excluded if they did not retain statistical significance (P < .05) after adjusting for other covariates or change the odds ratio estimate by ≥10% [22]: [1] demographic characteristics [ie, age [continuous], gender [male, female, or other], and race and ethnicity), self-reported number of chronic medical conditions (0, 1, 2, or ≥3), recent close contact with someone with COVID-19 (yes/no), and test type (RT-PCR or rapid NAAT); (2) calendar week using a categorical term in 2-week increments; and (3) pharmacy-level characteristics (ie, rural, suburban, or urban Walgreens trade area designation, US Census region [Midwest, Northeast, South, or West], federal information processing system tract-level area deprivation index [ADI; continuous] [23], SARS-CoV-2 testing volume [number of tests conducted relative to the estimated catchment population of the pharmacy, continuous], and store-specific percent positivity [continuous] and COVID-19 incidence [county level] per 100 000 persons [24] [continuous], both measured in the week before the participant’s SARS-CoV-2 test).
We additionally conducted 3 sensitivity analyses to assess the impact of removing those with symptomatic COVID-19 who tested multiple times during the study window and reported testing related to future travel or employment screening on age-stratified absolute and relative VE estimates. All analyses were performed using SAS, version 7.1 (SAS Institute, Inc).
RESULTS
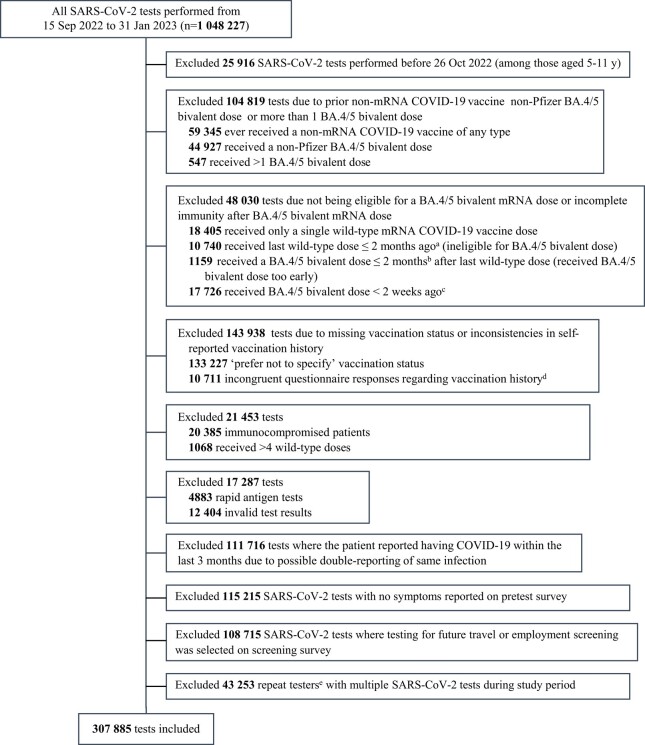
After excluding 740 342 SARS-CoV-2 tests, our analysis included 307 885 test results (with corresponding questionnaire data; Figure 1) including 7916 (3%) 5–11 year olds, 16 329 (5%) 12–17 year olds, and 283 640 (92%) adults aged ≥18 years. Overall, 39% of SARS-CoV-2 tests were positive. A greater proportion of those testing were women (60%), but positivity was slightly higher for men (41%) than women (37%). Adults aged 50–64 years had the highest positivity (46%) and 5–11 year olds had the lowest (20%). The highest positivity by race/ethnicity was observed among those identifying as Asian/non-Hispanic (42%) and the lowest among those identifying as non-Hispanic Black/African Americans (36%). Over one-third reported ≥1 chronic condition, with hypertension (18%) and overweight/obesity (15%) most frequently reported. Those reporting ≥1 condition were more likely to test positive (P < .0001), and the likelihood of testing positive increased with the number of conditions reported (Table 1). The most frequently reported symptom was new or worsening cough (71%), followed by congestion or runny nose (61%), sore throat (60%), headache (58%), and fatigue (52%). Positivity was higher among those who reported chills (49%), low-grade fever (49%), muscle pain (46%), new or worsening cough (43%), and new loss of taste or smell (43%) (Table 1).
Figure 1.
Selection criteria. aThe number of months between the last original wild-type COVID-19 mRNA dose and the testing date was calculated as the whole number representing the difference between the month and year of the last original wild-type COVID-19 mRNA dose and the month and year of the SARS-CoV-2 test date. Due to not having days, removing those with a difference of 0–2 months may remove some patients who have a difference of 3 months between the last original wild-type COVID-19 mRNA dose and the SARS-CoV-2 test date (ie, last original wild-type COVID-19 mRNA dose on the first day of July and SARS-CoV-2 test on the last day of September). Using this decision rule ensured that individuals who received their BA.4/5 bivalent dose too early or those who had received 2–4 original wild-type doses but were not yet eligible to receive a BA.4/5 bivalent dose were removed from the analysis, but may have also excluded some individuals who received their dose 2 months ago. Furthermore, the dichotomization of time since last original wild-type dose (2–6 months ago vs ≥7 months ago) could result in some misclassification of individuals classified as having received their last original wild-type dose 6 or 7 months ago. For example, the 2–6 month category could include some individuals who were vaccinated closer to 7 months ago and those in the ≥7 month category could include some individuals who received their last original wild-type dose closer to 6 months ago. bThe number of months between vaccine doses is calculated as the whole number representing the difference between the month and year of the last original wild-type COVID-19 mRNA dose and the month and year of the BA.4/5 bivalent dose. Due to not having days, removing those with a difference of 0–2 months may remove some patients who had a difference of 3 months between the last original wild-type COVID-19 mRNA dose and the BA.4/5 bivalent dose (ie, last original wild-type COVID-19 mRNA dose on the first day of July and BA.4/5 bivalent dose on the last day of September). cThe number of months between the last BA.4/5 bivalent mRNA vaccine dose and the testing date is a whole number calculated as the difference between the month and year of the testing date and the month and year of the last BA.4/5 bivalent vaccine dose. For doses received in the same month or the month before completing the SARS-CoV-2 test scheduling questionnaire, an additional question was asked to specify whether the dose was received ≥2 weeks before testing, and only doses received ≥2 weeks before testing were included. Doses received ≥2 weeks before testing but in the same month of testing were coded as having their last bivalent dose 0 months ago. dIndividuals testing multiple times at a Walgreens pharmacy between 1 January 2022 and 31 January 2023 were identified by merging testing questionnaire data based on the patient’s first name, last name, phone number, address state, date of birth, and gender. We removed records where the patient reported having received fewer vaccine doses than they had in an earlier questionnaire (from 1 January 2022 to 31 January 2023). eRepeat testers were identified by merging questionnaire data based on the patient’s first name, last name, phone number, address state, date of birth, and gender. We removed records where the patient reported having received fewer vaccines than they had in an earlier survey.
Table 1.
Sample Characteristics for Those Testing for SARS-CoV-2 at Walgreens Pharmacies Between 15 September 2022 and 31 January 2023, Overall and by SARS-CoV-2 Testing Status (n = 307 855)
| Characteristic | Total | SARS-CoV-2 Positive | SARS-CoV-2 Negative | Positivity | |
|---|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | % | P Valuea | |
| Total | 307 885 (8.76) | 118 706 (21.06) | 189 024 (70.18) | 38.56 | |
| Age, y | |||||
| 5–11 | 7916 (2.57) | 1611 (1.36) | 6305 (3.33) | 20.35 | <.0001b |
| 12–17 | 16 329 (5.30) | 4132 (3.48) | 12 197 (6.45) | 25.30 | <.0001b |
| ≥18 | 283 640 (92.13) | 112 963 (95.16) | 170 677 (90.22) | 39.83 | <.0001c |
| 18–49 | 190 921 (62.01) | 70 456 (59.35) | 120 465 (63.68) | 36.90 | Ref |
| 50–64 | 57 448 (18.66) | 26 593 (22.40) | 30 855 (16.31) | 46.29 | <.0001b |
| ≥65 | 35 271 (11.46) | 15 914 (13.41) | 19 357 (10.23) | 45.12 | <.0001b |
| Mean (SD) | 40.26 (18.00) | 43.10 (17.77) | 38.48 (17.92) | <.0001 | |
| Gender | |||||
| Female | 184 892 (60.05) | 67 980 (57.27) | 116 912 (61.80) | 36.77 | <.0001 |
| Male | 122 031 (39.64) | 50 436 (42.49) | 71 595 (37.85) | 41.33 | Ref |
| Other | 962 (0.31) | 290 (0.24) | 672 (0.36) | 30.15 | <.0001 |
| Race/ethnicity | |||||
| Hispanic/any race | 63 091 (20.49) | 24 553 (20.68) | 38 538 (20.37) | 38.92 | .6793 |
| Asian/non-Hispanic or Latino | 22 535 (7.32) | 9386 (7.91) | 13 149 (6.95) | 41.65 | .0006 |
| Black or African American/non-Hispanic or Latino | 46 710 (15.17) | 16 637 (14.02) | 30 073 (15.90) | 35.62 | .0204 |
| Native/non-Hispanic or Latinod | 2932 (0.95) | 1073 (0.90) | 1859 (0.98) | 36.60 | .2609 |
| White/non-Hispanic or Latino | 152 388 (49.50) | 59 229 (49.90) | 93 159 (49.24) | 38.87 | Ref |
| Decline to answer | 20 229 (6.57) | 7828 (6.59) | 12 401 (6.56) | 38.70 | .7967 |
| Currently pregnant? | |||||
| No | 224 984 (73.07) | 85 340 (71.89) | 139 644 (73.82) | 37.93 | Ref |
| Yes | 4287 (1.39) | 1543 (1.30) | 2744 (1.45) | 35.99 | .0026 |
| Does not apply | 78 614 (25.53) | 31 823 (26.81) | 46 791 (24.73) | 40.48 | <.0001 |
| Recent close contact with someone diagnosed with or presumed to have COVID-19 | |||||
| No | 176 854 (57.44) | 63 607 (53.58) | 113 247 (59.86) | 35.97 | Ref |
| Yes | 131 031 (42.56) | 55 099 (46.42) | 75 932 (40.14) | 42.05 | <.0001 |
| Chronic conditions reported | |||||
| At least 1 | 112 905 (36.67) | 46 771 (39.40) | 66 134 (34.96) | 41.43 | <.0001e |
| Chronic lung disease, eg, COPD, moderate to severe asthma, cystic fibrosis, or pulmonary embolism | 14 365 (4.67) | 4971 (4.19) | 9394 (4.97) | 34.60 | <.0001 |
| Cirrhosis of the liver | 574 (0.19) | 226 (0.19) | 348 (0.18) | 39.37 | .7132 |
| Current or former smoker | 27 522 (8.94) | 11 484 (9.67) | 16 038 (8.48) | 41.73 | <.0001 |
| Diabetes | 23 095 (7.50) | 9956 (8.39) | 13 139 (6.95) | 43.11 | <.0001 |
| Heart condition | 15 410 (5.01) | 6365 (5.36) | 9045 (4.78) | 41.30 | <.0001 |
| High blood pressure | 56 970 (18.50) | 25 061 (21.11) | 31 909 (16.87) | 43.99 | <.0001 |
| Overweight or obesity | 47 410 (15.40) | 18 992 (16.00) | 28 418 (15.02) | 40.06 | <.0001 |
| Kidney failure or end-stage renal disease | 1409 (0.46) | 605 (0.51) | 804 (0.42) | 42.94 | <.0001 |
| None | 194 980 (63.33) | 71 935 (60.60) | 123 045 (65.04) | 36.89 | |
| Number of condition(s) reported | |||||
| 0 | 194 980 (63.33) | 71 935 (60.60) | 123 045 (64.04) | 36.89 | Ref |
| 1 | 64 287 (20.88) | 26 399 (22.24) | 37 888 (20.03) | 41.06 | <.0001 |
| 2 | 30 349 (9.86) | 12 697 (10.70) | 17 652 (9.33) | 41.84 | <.0001 |
| ≥ 3 | 18 269 (5.93) | 7675 (6.47) | 10 594 (5.60) | 42.01 | <.0001 |
| Symptoms reported | |||||
| Low-grade fever, <102°F | 107 854 (35.03) | 52 651 (44.35) | 55 203 (29.18) | 48.82 | <.0001 |
| Chills | 109 231 (35.48) | 53 936 (45.44) | 55 295 (29.23) | 49.38 | <.0001 |
| Fatigue | 159 834 (51.91) | 65 711 (55.36) | 94 123 (49.75) | 41.11 | <.0001 |
| Headache | 178 744 (58.06) | 73 383 (61.82) | 105 361 (55.69) | 41.05 | <.0001 |
| Muscle pain | 113 489 (36.86) | 52 037 (43.84) | 61 452 (32.48) | 45.85 | <.0001 |
| Congestion/runny nose | 188 160 (61.11) | 78 515 (66.14) | 109 645 (57.96) | 41.73 | <.0001 |
| New loss of taste or smell | 29 915 (9.72) | 12 816 (10.80) | 17 099 (9.04) | 42.84 | <.0001 |
| Sore throat | 185 864 (60.37) | 76 239 (64.23) | 109 625 (57.95) | 41.02 | <.0001 |
| New or worsening cough | 218 845 (71.08) | 95 164 (80.17) | 123 681 (65.38) | 43.48 | <.0001 |
| Shortness of breath/difficulty breathing, not severe | 61 023 (19.82) | 22 797 (19.20) | 38 226 (20.21) | 37.36 | <.0001 |
| Diarrhea | 38 683 (12.56) | 13 807 (11.63) | 24 876 (13.15) | 35.69 | <.0001 |
| Vomiting | 18 988 (6.17) | 6322 (5.33) | 12 666 (6.70) | 33.29 | <.0001 |
| SARS-CoV-2 test type | |||||
| PCR | 99 490 (32.31) | 40 430 (34.06) | 59 060 (31.22) | 40.64 | Ref |
| Rapid NAAT | 208 395 (67.69) | 78 276 (65.94) | 130 119 (68.78) | 37.56 | .0008 |
| Original wild-type vaccination history | |||||
| Unvaccinated | 64 846 (21.06) | 21 417 (18.04) | 43 429 (22.96) | 33.03 | Ref |
| 2 doses only | 110 560 (35.91) | 42 321 (35.65) | 68 239 (36.07) | 38.28 | <.0001f,g |
| ≥ 3 doses | 132 479 (43.03) | 54 968 (46.31) | 77 511 (40.97) | 41.49 | <.0001f |
| 3 doses only | 109 141 (35.45) | 44 992 (37.90) | 64 149 (33.91) | 41.22 | <.0001g |
| 4 doses only | 23 338 (7.58) | 9976 (8.40) | 13 362 (7.06) | 42.75 | <.0001g |
| Months since last original wild-type doseh | |||||
| 2–6 | 29 224 (12.02) | 11 048 (11.36) | 18 176 (12.47) | 37.80 | <.0001 |
| ≥ 7 | 213 815 (87.98) | 86 241 (88.64) | 127 574 (87.53) | 40.33 | Ref |
| BA.4/5 bivalent vaccination status | |||||
| Did not receive bivalent vaccine | 280 924 (91.24) | 109 798 (92.50) | 171 126 (90.46) | 39.08 | <.0001i |
| ≥ 2 original wild-type doses but no bivalent vaccine | 216 078 (70.18) | 88 381 (74.45) | 127 697 (67.50) | 40.90 | <.0001j |
| Unvaccinated | 64 846 (21.06) | 21 417 (18.04) | 43 429 (22.96) | 33.03 | .8149j |
| Prior SARS-CoV-2 infection | <.0001 | ||||
| No | 174 591 (56.71) | 83 362 (70.23) | 91 229 (48.22) | 47.75 | Ref |
| Yes, > 3 mo agok | 133 294 (43.29) | 35 344 (29.77) | 97 950 (51.78) | 26.52 | <.0001 |
| Average weekly incidence rate (per 100 000) in participating counties over study period, mean (SD) | 109.77 (60.55) | 114.00 (60.75) | 107.10 (60.28) | NA | <.0001 |
| Average store-specific percent positivity (No. of tests in a store, divided by the store trade area’s population size) in participating stores over study period, mean (SD) | 38.56 (29.43) | 61.02 (25.05) | 24.46 (22.37) | NA | <.0001 |
| US census region | <.0001 | ||||
| Midwest | 80 982 (26.30) | 31 397 (26.45) | 49 585 (26.21) | 38.77 | |
| Northeast | 36 187 (11.75) | 15 098 (12.72) | 21 089 (11.15) | 41.72 | |
| South | 130 215 (42.29) | 47 870 (40.33) | 82 345 (43.53) | 36.76 | |
| West | 60 501 (19.65) | 24 341 (20.51) | 36 160 (19.11) | 40.23 | |
| Rural/urban area of pharmacy trade region | |||||
| Rural | 76 298 (24.78) | 29 675 (25.00) | 46 623 (24.64) | 38.89 | .9519 |
| Suburban | 206 825 (67.18) | 79 208 (66.73) | 127 617 (67.46) | 38.30 | .5471 |
| Urban | 24 762 (8.04) | 9823 (8.28) | 14 939 (7.90) | 39.67 | Ref |
| Area deprivation index of pharmacy, mean (SD) | 58.51 (28.49) | 58.24 (28.37) | 58.67 (28.56) | NA | .9851 |
| Average store-specific testing volume per 100 persons in pharmacy trade area over study period, mean (SD) | 0.26 (0.16) | 0.27 (0.16) | 0.26 (0.16) | NA | <.0001 |
Abbreviations: COPD, chronic obstructive pulmonary disease; COVID-19, coronavirus disease 2019; NAAT, nucleic acid amplification test; PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; NA, Not Applicable; ICC, intraclass correlation coefficient.
aStatistical significance was assessed using bivariate generalized estimating equations logistic regression models that clustered on US Census region of pharmacy to account for Intraclass Correlation Coefficient (ICC) by Walgreens pharmacy region.
bComparing categories: 5–11, 12–17, 18–49, 50–64, and ≥65 years.
cComparing categories: ≥ 18 vs <18 years.
dIncludes American Indian, Alaska Native, Native Hawaiian, or Other Pacific Islander.
eComparing categories: any chronic conditions vs no chronic conditions.
fComparing categories: unvaccinated, 2 doses only, ≥3 doses.
gComparing unvaccinated, 2 doses, 3 doses, and 4 doses.
hBecause only month and year are available for vaccine doses, 2–6 months may include some patients who were vaccinated 7 months ago; 7–11 months may include some patients who were vaccinated 6 or 12 months ago.
iComparing categories: did vs did not receive bivalent vaccine.
jCompared with receipt of the bivalent vaccine.
kHistory of prior COVID-19 infection included the following response options: No; Yes, within the last week; Yes, 1 week to 3 months ago; and Yes, >3 months ago. Those indicating a prior COVID-19 infection within the last week or 1 week to 3 months ago were excluded from the analysis. This variable represents self-reported prior COVID-19 infection >3 months ago (yes vs no).
Overall, 21% were unvaccinated, 70% received 2–4 original wild-type doses and no bivalent vaccine, and 9% received 2–4 original wild-type doses plus a BA.4/5 bivalent vaccine (Table 2). Median time since receipt of a bivalent vaccine was 1 month for 5–11 year olds and 2 months for those aged ≥12 years (Supplementary Table 1). Of those with 2–4 original wild-type doses (11% of whom also received a bivalent vaccine), 88% received their last original wild-type dose ≥7 months ago.
Table 2.
Sample Characteristics for Those Testing for SARS-CoV-2 at Walgreens Pharmacies Between 15 September 2022 and 31 January 2023, Overall and by Vaccination Status (n = 307 885)
| Characteristic | Received BA.4/5 Bivalent Vaccine (n = 26 961) |
Unvaccinateda (n = 64 846) | 2–4 Original Wild-Type Doses but no Bivalent Vaccineb (n = 216 078) | ||
|---|---|---|---|---|---|
| No. (%) | No. (%) | P Valuec,d | No. (%) | P Valued,e | |
| Age, y | |||||
| 5–11 | 370 (1.37) | 4702 (7.25) | <.0001f | 2844 (1.32) | <.0001f |
| 12–17 | 762 (2.83) | 6107 (9.42) | <.0001f | 9460 (4.38) | <.0001f |
| ≥ 18 | 25 829 (95.80) | 54 037 (83.33) | <.0001f,g | 203 774 (94.31) | <.0001g |
| 18–49 | 12 404 (46.01) | 44 070 (67.96) | Ref | 134 447 (62.22) | Ref |
| 50–64 | 6270 (23.26) | 7359 (11.35) | <.0001f | 43 819 (20.28) | <.0001f |
| ≥65 | 7155 (26.54) | 2608 (4.02) | <.0001f | 25 508 (11.80) | <.0001f |
| Mean (SD) | 49.47 (19.06) | 32.60 (15.98) | <.0001 | 41.41 (17.62) | <.0001 |
| Gender | |||||
| Female | 16 627 (61.67) | 36 734 (56.65) | <.0001 | 131 531 (60.87) | .1579 |
| Male | 10 202 (37.84) | 28 019 (43.21) | Ref | 83 810 (38.79) | Ref |
| Other | 132 (0.49) | 93 (0.14) | <.0001 | 737 (0.34) | <.0001 |
| Race/ethnicity | |||||
| Hispanic/any race | 3001 (11.13) | 14 436 (22.26) | <.0001 | 45 654 (21.13) | <.0001 |
| Asian/non-Hispanic or Latino | 2551 (9.46) | 1396 (2.15) | <.0001 | 18 588 (8.60) | <.0001 |
| Black or African American/non-Hispanic or Latino | 2177 (8.07) | 13 890 (21.42) | <.0001 | 30 643 (14.18) | <.0001 |
| Native/non-Hispanic or Latinoh | 148 (0.55) | 792 (1.22) | <.0001 | 1992 (0.92) | <.0001 |
| White/non-Hispanic or Latino | 17 818 (66.09) | 29 176 (44.99) | Ref | 105 394 (48.78) | Ref |
| Decline to answer | 1266 (4.70) | 5156 (7.95) | <.0001 | 13 807 (6.39) | <.0001 |
| Currently pregnant? | |||||
| No | 19 710 (73.11) | 46 635 (71.92) | Ref | 158 639 (73.42) | Ref |
| Yes | 238 (0.88) | 1148 (1.77) | <.0001 | 2901 (1.34) | <.0001 |
| Does not apply | 7013 (26.01) | 17 063 (26.31) | .3877 | 54 538 (25.24) | .1805 |
| Recent close contact with someone diagnosed with or presumed to have COVID-19 | <.0001 | ||||
| No | 15 220 (56.45) | 37 617 (58.01) | Ref | 124 017 (57.39) | Ref |
| Yes | 11 741 (43.55) | 27 229 (41.99) | <.0001 | 92 061 (42.61) | <.0001 |
| Chronic conditions reported | |||||
| At least 1 | 13 066 (48.46) | 17 444 (26.90) | <.0001 | 82 395 (38.13) | <.0001i |
| Chronic lung disease, eg, COPD, moderate to severe asthma, cystic fibrosis, or pulmonary embolism | 1769 (6.56) | 2459 (3.79) | <.0001 | 10 137 (4.69) | <.0001 |
| Cirrhosis of the liver | 71 (0.26) | 114 (0.18) | .0012 | 389 (0.18) | .0007 |
| Current or former smoker | 2705 (10.03) | 5888 (9.08) | .3628 | 18 929 (8.76) | .0404 |
| Diabetes | 2774 (10.29) | 2885 (4.45) | <.0001 | 17 436 (8.07) | <.0001 |
| Heart condition | 2166 (8.03) | 2164 (3.34) | <.0001 | 11 080 (5.13) | <.0001 |
| High blood pressure | 7243 (26.86) | 7297 (11.25) | <.0001 | 42 430 (19.64) | <.0001 |
| Overweight or obesity | 5891 (21.85) | 6220 (9.59) | <.0001 | 35 299 (16.34) | <.0001 |
| Kidney failure or end-stage renal disease | 167 (0.62) | 204 (0.31) | <.0001 | 1038 (0.48) | .0061 |
| None | 13 895 (51.54) | 47 402 (73.10) | Ref | 133 683 (61.87) | Ref |
| Number of condition(s) reported | |||||
| 0 | 13 895 (51.54) | 47 402 (73.10) | Ref | 133 683 (61.87) | Ref |
| 1 | 6878 (25.51) | 10 919 (16.84) | <.0001 | 46 490 (21.52) | <.0001 |
| 2 | 3670 (13.61) | 4209 (6.49) | <.0001 | 22 470 (10.40) | <.0001 |
| ≥ 3 | 2518 (9.34) | 2316 (3.57) | <.0001 | 13 435 (6.22) | <.0001 |
| Symptoms reported | |||||
| Low-grade fever, <102°F | 6223 (23.08) | 27 402 (42.26) | <.0001 | 74 229 (34.35) | <.0001 |
| Chills | 7064 (26.20) | 25 440 (39.23) | <.0001 | 76 727 (35.51) | <.0001 |
| Fatigue | 12 905 (47.87) | 33 163 (51.14) | .0091 | 113 766 (52.65) | <.0001 |
| Headache | 12 834 (47.60) | 40 895 (63.06) | <.0001 | 125 015 (57.86) | <.0001 |
| Muscle pain | 6962 (25.82) | 27 261 (42.04) | <.0001 | 79 266 (36.68) | <.0001 |
| Congestion/runny nose | 17 207 (63.82) | 37 134 (57.26) | <.0001 | 133 819 (61.93) | .0011 |
| New loss of taste or smell | 1560 (5.79) | 8238 (12.70) | <.0001 | 20 117 (9.31) | <.0001 |
| Sore throat | 16 127 (59.82) | 36 465 (56.23) | <.0001 | 133 272 (61.68) | <.0001 |
| New or worsening cough | 17 558 (65.12) | 47 005 (72.49) | <.0001 | 154 282 (71.40) | <.0001 |
| Shortness of breath/difficulty breathing, not severe | 3612 (13.40) | 15 873 (24.48) | <.0001 | 41 538 (19.22) | <.0001 |
| Diarrhea | 2363 (8.76) | 10 475 (16.15) | <.0001 | 25 845 (11.96) | <.0001 |
| Vomiting | 802 (2.97) | 6532 (10.07) | <.0001 | 11 654 (5.39) | <.0001 |
| SARS-CoV-2 test type | |||||
| PCR | 11 728 (43.50) | 15 583 (24.03) | Ref | 72 179 (33.40) | Ref |
| Rapid NAAT | 15 233 (56.50) | 49 263 (75.97) | <.0001 | 143 899 (66.60) | <.0001 |
| Wild-type vaccination history | |||||
| Unvaccinated | NA | 64 846 (100.00) | NA | NA | NA |
| 2 doses only | 3501 (12.99) | NA | NA | 107 059 (49.55) | Ref |
| ≥ 3 doses | 23 460 (87.01) | NA | NA | 109 019 (50.45) | <.0001j |
| 3 doses only | 16 229 (60.19) | NA | NA | 92 912 (43.00) | <.0001k |
| 4 doses only | 7231 (26.82) | NA | NA | 16 107 (7.45) | <.0001k |
| Months since last wild-type dosel | |||||
| 2–6 | 3199 (11.87) | NA | NA | 26 025 (12.04) | .2513 |
| ≥7 | 23 762 (88.13) | NA | NA | 190 053 (87.96) | Ref |
| SARS-CoV-2 test status | |||||
| Negative | 18 053 (66.96) | 43 429 (66.97) | Ref | 127 697 (59.10) | Ref |
| Positive | 8908 (33.04) | 21 417 (33.03) | .7554 | 88 381 (40.90) | <.0001 |
| Prior SARS-CoV-2 infection | |||||
| No | 18 279 (67.80) | 29 821 (45.99) | Ref | 126 491 (58.54) | Ref |
| Yes, > 3 mo agom | 8682 (32.20) | 35 025 (54.01) | <.0001 | 89 587 (41.46) | <.0001 |
| Average weekly incidence rate (per 100 000) in participating counties over study period, mean (SD) | 110.40 (57.95) | 108.30 (62.56) | .9698 | 110.10 (60.25) | .8095 |
| Average store-specific percent positivity (No. of positive tests in a store, divided by the number of total tests) in participating stores over study period, mean (SD) | 36.74 (29.06) | 36.12 (29.42) | .9780 | 39.51 (29.43) | .0023 |
| US census region | |||||
| Midwest | 7882 (29.23) | 18 074 (27.87) | <.0001 | 55 026 (25.47) | <.0001 |
| Northeast | 3779 (14.02) | 5388 (8.31) | <.0001 | 27 020 (12.50) | <.0001 |
| South | 9224 (34.21) | 30 576 (47.15) | Ref | 90 415 (41.84) | Ref |
| West | 6076 (22.54) | 10 808 (16.67) | <.0001 | 43 617 (20.19) | <.0001 |
| Rural/urban area of pharmacy trade region | |||||
| Rural | 5593 (20.74) | 20 650 (31.84) | .0113 | 50 055 (23.17) | .4568 |
| Suburban | 18 981 (70.40) | 40 398 (62.30) | .4372 | 147 446 (68.24) | .6422 |
| Urban | 2387 (8.85) | 3798 (5.86) | Ref | 18 577 (8.60) | Ref |
| Area deprivation index of pharmacy, mean (SD) | 50.52 (28.91) | 65.91 (26.57) | <.0001 | 57.28 (28.54) | <.0001 |
| Average store-specific testing volume per 100 persons in pharmacy trade area over study period, mean (SD) | 0.13 (0.15) | 0.27 (0.15) | <.0001 | 0.27 (0.15) | <.0001 |
Abbreviations: COPD, chronic obstructive pulmonary disease; COVID-19, coronavirus disease 2019; NAAT, nucleic acid amplification test; PCR, polymerase chain reaction; Ref, reference; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; VE, vaccine effectiveness; NA, Not Applicable; ICC, intraclass correlation coefficient.
aUnexposed group for absolute VE.
bUnexposed group for relative VE.
c P value for received BA.4/5 bivalent vaccine vs unvaccinated.
d P value for received BA.4/5 bivalent vaccine vs received 2–4 original wild-type doses but no bivalent vaccine.
eStatistical significance was assessed using bivariate generalized estimating equations logistic regression models that clustered on US Census region of pharmacy to account for intraclass correlation coefficient (ICC) by Walgreens pharmacy region.
fComparing categories: 5–11, 12–17, 18–49, 50–64, and ≥65 years.
gComparing categories: ≥ 18 vs <18 years.
hIncludes American Indian, Alaska Native, Native Hawaiian, or Other Pacific Islander.
iComparing categories: any chronic conditions vs no chronic conditions.
jComparing categories: unvaccinated, 2 doses only, ≥3 doses.
kComparing unvaccinated, 2 doses, 3 doses, and 4 doses.
lBecause only month and year are available for vaccine doses, 2–6 months may include some patients who were vaccinated 7 months ago; 7–11 months may include some patients who were vaccinated 6 or 12 months ago.
mHistory of prior COVID-19 infection included the following response options: No; Yes, within the last week; Yes, 1 week to 3 months ago; and Yes, >3 months ago. Those indicating a prior COVID-19 infection within the last week or 1 week to 3 months ago were excluded from the analysis. This variable represents self-reported prior COVID-19 infection >3 months ago (yes vs no).
A greater proportion of those aged ≥65 years (20%) or who had received ≥3 original wild-type doses (18%) had received a bivalent vaccine. Bivalent vaccine uptake increased with the number of comorbidities reported. Those testing at pharmacies in more disadvantaged areas (higher ADI scores) were less likely to have received a bivalent vaccine (mean ADI, 51 for those with a bivalent vaccine, 57 for only 2–4 original wild-type doses, and 66 for unvaccinated). Those least likely to have received a bivalent vaccine were 5–17 year olds (5%), those identifying as non-Hispanic Black/African American (5%), Hispanic (5%), or non-Hispanic Native (5%), and pregnant women (6%). Those testing at pharmacies in rural areas (7%) or the South (7%) were also less likely to have received a bivalent vaccine (Table 2).
Overall, 43% reported prior infection. Those reporting prior infection were less likely to test positive (27%) than those without prior infection (48%; P < .0001). Unvaccinated individuals were most likely to report prior infection (54% vs 41% of those with only 2–4 original wild-type doses and 32% of those with a bivalent vaccine; P < .0001; Table 2).
Absolute VE
Depending on age group, adjusted absolute VE (vs the unvaccinated) point estimates against symptomatic COVID-19 ranged from 22% to 60% overall (Table 3). For each age group, there was a statistically significant interaction between BA.4/5 bivalent vaccination status and prior infection. Across all age groups, absolute VE point estimates were significantly higher for those reporting prior SARS-CoV-2 infection (range, 55%–79%) than among those not reporting prior infection (range, 22%–50%) (Table 3). Absolute VE was highest among 5–11 year olds and tended to decrease as age increased (Table 3). Supplementary Table 2 presents unadjusted absolute VE estimates and strata-specific sample sizes.
Table 3.
Adjusted Absolute VE and Corresponding 95% CIs Against Symptomatic COVID-19, Stratified by Age Group and by Age Group and History of Prior SARS-CoV-2 Infection
| Age, y | Overall | No Prior Infection | Prior Infection, >3 mo Ago |
|---|---|---|---|
| VE (95% CI) | VE (95% CI) | VE (95% CI) | |
| 5–11 | 60.17 (32.42–99.48) | 49.77 (9.77–72.04)a | 79.43 (64.48–88.09)a |
| 12–17 | 38.98 (17.49–98.80) | 27.60 (−2.61 to 48.92) | 61.77 (48.59–71.57) |
| 18–49 | 41.99 (35.67–95.09) | 29.71 (22.04–36.61) | 57.72 (53.73–61.36) |
| 50–64 | 36.15 (15.96–95.22) | 23.94 (10.74–35.20) | 55.03 (49.58–59.88) |
| ≥65 | 22.48 (16.75–39.75) | 21.51 (10.47–31.20) | 56.09 (48.89–62.29) |
Absolute VE compares those who received 2–4 original wild-type doses plus a BNT162b2 BA.4/5 bivalent vaccine ≥14 days before testing for SARS-CoV-2 and the unvaccinated. All models used generalized estimating equations (clustered on US Census region of pharmacy) and adjusted for age (continuous), gender, race/ethnicity, prior SARS-CoV-2 infection, calendar week of SARS-CoV-2 test (categorical; 2-week intervals), recent contact with someone with confirmed or presumed to have COVID-19, US Census region of pharmacy, and store-specific percent positivity in the week prior to the SARS-CoV-2 testing date.
Abbreviations: CI, confidence interval; COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; VE, vaccine effectiveness.
aTwo individuals with gender Other removed from the absolute model due to zero cell errors when stratified by prior infection and inability to compute estimates.
Relative VE
Relative VE (vs receipt of 2–4 wild-type doses) decreased with increasing age (adjusted VE point estimates, 64% among 5–11 year olds, 53% among 12–17 year olds, 47% among 18–49 year olds, 38% among 50–64 year olds, and 31% among those aged ≥65 years; Table 4). No statistically significant interaction was observed by time since last original wild-type dose (Supplementary Table 5). Interaction between BA.4/5 bivalent vaccination status and prior infection was statistically significant only for 5–11 year olds (VE for those with and without prior infection was 76% and 59%, respectively; Table 4). Supplementary Table 3 presents unadjusted relative VE estimates and strata-specific sample sizes.
Table 4.
Adjusted Relative VE and Corresponding 95% CIs for Symptomatic COVID-19, Stratified by Age Group and by Age Group and History of Prior SARS-CoV-2 Infection
| Age, y | Overall | No Prior Infection | Prior Infection >3 mo Ago |
|---|---|---|---|
| VE (95% CI) | VE (95% CI) | VE (95% CI) | |
| 5–11a | 63.64 (45.42–75.79) | 58.89 (33.87–74.45)b | 75.74 (64.98–83.20)b |
| 12–17 | 52.82 (40.58–62.53) | 50.35 (36.14–61.40) | 59.64 (40.84–72.46) |
| 18–49 | 47.08 (43.52–50.41) | 46.94 (42.18–51.35) | 47.31 (45.59–49.90) |
| 50–64 | 37.91 (34.77–40.90) | 37.54 (33.56–41.28) | 39.06 (38.90–42.07) |
| ≥65 | 31.44 (27.74–34.95) | 30.81 (27.10–34.32) | 34.64 (17.81–48.01) |
Relative vaccine effectiveness compares those who received 2–4 original wild-type doses plus a BNT162b2 BA.4/5 bivalent vaccine ≥14 days before testing for SARS-CoV-2 and those who received 2–4 original wild-type mRNA doses >2 months ago but not a BA.4/5 bivalent vaccine.
Models clustered on US Census region of pharmacy and adjusted for age (continuous), gender, race/ethnicity, recent contact with someone with confirmed or presumed to have COVID-19, prior SARS-CoV-2 infection, time since last wild-type dose, calendar week of SARS-CoV-2 test (categorical; 2-week intervals), US Census region of pharmacy, area deprivation index for pharmacy location (continuous), store-specific percent positivity in the week prior to the SARS-CoV-2 testing date, and local county-level case incidence per 100 000 persons during the week prior to the SARS-CoV-2 testing date.
Abbreviations: CI, confidence interval; COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; VE, vaccine effectiveness.
aTwo individuals with gender Other removed from the stratified estimates due to zero cell counts and failure of model to run as a result.
bOn the multiplicative scale, effect modification by prior infection was statistically significant for the 5–11-year-old age group.
Sensitivity Analyses
Sensitivity analyses showed that excluding those who tested related to future travel or employment screening or who tested more than once during the study period did not meaningfully impact results (Supplementary Tables 6–8). Those excluded due to testing related to future travel or employment screening were less likely to have received the BA.4/5 bivalent vaccine and more likely to test positive (P value < .0001). Individuals excluded because they tested more than once during the study period were more likely to have received the BA.4/5 bivalent vaccine and less likely to test positive (P value < .0001).
DISCUSSION
In this test-negative case-control study among immunocompetent individuals aged ≥5 years testing for SARS-CoV-2 at Walgreens retail pharmacies, the Pfizer-BioNTech BNT162b2 BA.4/5 bivalent vaccine improved protection against symptomatic COVID-19 during a period when BA.4/5 and XBB-related Omicron sublineages were circulating. Consistent with other reports highlighting the benefit of hybrid immunity in both clinical studies of neutralization activity [25–27] and real-world studies [7, 28–31], effectiveness was highest among those with prior infection, with absolute VE point estimates ranging from 55% to 79% against symptomatic COVID-19 across all age groups. Relative VE estimates, which estimated improvement in protection provided by a BNT162b2 bivalent vaccine among individuals who previously received 2–4 original wild-type doses, showed a statistically significant additional benefit of receiving a bivalent vaccine regardless of age, history of prior infection, or time since receipt of the most recent original wild-type dose. Point estimates of relative VE ranged from 59% to 76% for 5–11 year olds (depending on history of prior infection), and from 31% to 53% among those aged ≥12 years. Median time since receiving a bivalent vaccine was only 1–2 months, thus our results should be interpreted as early evidence of increased protection following a bivalent vaccine. Longer-term studies of durability are needed.
Our findings have important public health implications, particularly for informing the debate about whether mRNA COVID-19 vaccines are currently only useful for preventing severe COVID-19. Recent estimates suggest that >90% of US residents have been previously infected with SARS-CoV-2 [19]. Thus, our findings showing early effectiveness of a BNT162b2 BA.4/5 bivalent vaccine against symptomatic COVID-19, especially among those who self-reported prior infection, suggest that there are wider public health benefits of COVID-19 vaccination beyond preventing severe illness alone. Even if durability against these milder end points is relatively short, a well-timed booster campaign that utilizes a well-matched vaccine (eg, like the 2023/2024 vaccination campaign) will likely (1) reduce SARS-CoV-2 infections, which may in turn lessen transmission; and (2) help prevent human and economic burden stemming from symptomatic illness in a broader population beyond just those at highest risk of severe disease.
It was unclear why VE was higher among 5–11 year olds compared to other age groups, especially compared to the elderly. Higher VEs among this age group may reflect more recent receipt of a bivalent vaccine (median time since a bivalent vaccine was 1 month) due to more recent approval for this age group, compared to those aged ≥12 years where median time since a bivalent vaccine was 2 months. It is also possible that lower VE among older age groups reflects increased susceptibility, reduced immune responses, or both—particularly for individuals aged ≥50 years [32, 33]. Finally, other studies have shown that VE against infection may be higher when the doses are administered with more months between them, which may also explain the lower VE observed in older age groups who have received additional doses with shorter intervals between doses [34, 35].
There is limited data describing the effectiveness of BA.4/5 bivalent vaccines against symptomatic SARS-CoV-2 infection, especially during periods of XBB circulation. Only one publication described effectiveness of a bivalent vaccine in 5–11 years olds [36]. Our relative VE estimates in this age group were consistent with this report [36], but were conducted in a broader nationwide population. Importantly, we also provided absolute VE estimates for comparability and stratified VE by history of prior infection. For individuals aged ≥12 years, only 2 published studies have reported effectiveness against infection or mild illness [13, 16]. One study conducted among North Carolina residents aged ≥12 years reported relative VE against any infection ranging from 4% to 29% [13], and point estimates that were lower than ours for this age group (31% to 53%). However, our study was conducted in a broader population and in the retail pharmacy setting, which may partially explain differences in study findings. The second published study was conducted by CDC and reported absolute and relative VE against symptomatic COVID-19 in adults aged ≥18 years [16]. Our VE estimates in this age group were consistent with this CDC report [16] but are unique in that we stratified by self-reported prior SARS-CoV-2 infection.
Despite evidence of their effectiveness, only 19% of US adults and 4% of 5–17 year olds had received a BA.4/5 bivalent vaccine by 31 January 2023 [37]. Slow uptake is likely due to a combination of factors including low awareness and confusion about eligibility for the bivalent vaccine; pandemic and vaccine fatigue; a lower perceived risk of severe outcomes associated with Omicron and high levels of preexisting immunity from prior infection, vaccination, or both; and persistent misinformation regarding the safety or performance of COVID-19 vaccines [38, 39]. Continued efforts are needed to improve uptake of current and future COVID-19 vaccines (eg, XBB-adapted vaccines for the 2023–2024 viral respiratory season) through targeted and tailored campaigns focused on simplified communication to help clarify risks and vaccine eligibility [39, 40].
Like all observational studies, our results may be biased by unmeasured confounding. Additionally, because prior infection, symptoms, comorbidities, and vaccination history were self-reported, all were subject to misclassification and recall bias. For example, individuals may not know if they were previously infected (e.g., asymptomatic, paucisymptomatic, or not tested). Although we stratified by self-reported prior infection, we were unable to account for time since infection or the variant causing prior infection, both of which may impact VE estimates [17, 18]. Moreover, if unvaccinated individuals were more likely to have unreported prior infections, especially during the first Omicron wave, a phenomenon known as “differential depletion of susceptibles” [41–43] could occur and bias absolute VE estimates against subsequent Omicron sublineages downward. To help mitigate this, we also presented relative VE estimates, which confirmed a benefit of bivalent vaccines. Another limitation was that although we had information about whether the bivalent vaccine was given ≥14 days before completing the SARS-CoV-2 test questionnaire, for COVID-19 vaccine doses given >14 days prior, only month and year of administration were recorded. This could lead to imprecision in defining time since last original wild-type or bivalent dose and time between the last original wild-type and bivalent dose. As most bivalent doses were administered in the past 3 months, this was unlikely to largely influence our results. Additionally, given slow uptake of bivalent vaccines [17], our estimates reflect VE among early adopters, who may differ from those who receive bivalent vaccines later with respect to underlying risk factors, health care-seeking behaviors, or other characteristics. Further, individuals testing at pharmacies may differ from those testing at other locations like clinics or at home. However, pharmacy-based testing captures a broad and diverse population of mild COVID-19 cases. Finally, median time since receiving a bivalent vaccine was only 1–2 months in our study. Thus, long-term durability remains unknown.
CONCLUSION
Our findings suggest that the BNT162b2 BA.4/5 bivalent vaccine provided early additional protection against Omicron-related symptomatic COVID-19 among immunocompetent individuals aged ≥5 years when BA.4/5 and XBB-related sublineages were circulating. In general, effectiveness was highest among those self-reporting prior SARS-CoV-2 infection. Longer-term studies of vaccine durability are needed.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online (http://jid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Supplementary Material
Contributor Information
Abby E Rudolph, Pfizer, Collegeville, Pennsylvania, USA.
Farid L Khan, Pfizer, Collegeville, Pennsylvania, USA.
Amy Shah, Walgreens Center for Health and Wellbeing Research, Deerfield, Illinois, USA.
Tanya G Singh, Walgreens Center for Health and Wellbeing Research, Deerfield, Illinois, USA.
Timothy L Wiemken, Pfizer, Collegeville, Pennsylvania, USA.
Laura A Puzniak, Pfizer, Collegeville, Pennsylvania, USA.
Luis Jodar, Pfizer, Collegeville, Pennsylvania, USA.
John M McLaughlin, Pfizer, Collegeville, Pennsylvania, USA.
Notes
Acknowledgments. The authors thank Dr Renae Smith-Ray, PhD, MA of Walgreens for concept review and supervision support of the Walgreens research team. The authors also thank Dr Srinivas Rao, PhD of Pfizer for statistical analysis support and Joann Zamparo, MPH of Pfizer for study support. All contributors were compensated for their contributions to this study as employees of their respective organizations.
Disclaimer. Pfizer, Inc participated in the design, analysis, and interpretation of the data; preparation, review, approval of the manuscript, and decisions to submit the manuscript for publication.
Financial support. This work was supported by Pfizer Inc, and was conducted as a collaboration between Walgreens and Pfizer.
References
- 1. World Health Organization . COVID-19 weekly epidemiological update, edition 72. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---28-december-2021. Accessed 12 July 2022.
- 2. Collie S, Nayager J, Bamford L, Bekker LG, Zylstra M, Gray G. Effectiveness and durability of the BNT162b2 vaccine against Omicron sublineages in South Africa. N Engl J Med 2022; 387:1332–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tartof SY, Slezak JM, Puzniak L, et al. BNT162b2 vaccine effectiveness against SARS-CoV-2 Omicron BA.4 and BA.5. Lancet Infect Dis 2022; 22:1663–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Link-Gelles R, Levy ME, Natarajan K, et al. Association between COVID-19 mRNA vaccination and COVID-19 illness and severity during Omicron BA. 4 and BA. 5 sublineage periods. medRxiv, doi: 2022.10.04.22280459, 5 October 2022, preprint: not peer reviewed. [Google Scholar]
- 5. Goldberg Y, Mandel M, Bar-On YM, et al. Waning immunity after the BNT162b2 vaccine in Israel. N Engl J Med 2021; 385:e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Surie D, DeCuir J, Zhu Y, et al. Early estimates of bivalent mRNA vaccine effectiveness in preventing COVID-19–associated hospitalization among immunocompetent adults aged≥ 65 years—IVY Network, 18 States, September 8–November 30, 2022. MMWR Morb Mortal Wkly Rep 2022; 71(5152):1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goldberg Y, Mandel M, Bar-On YM, et al. Protection and waning of natural and hybrid immunity to SARS-CoV-2. N Engl J Med 2022; 386:2201–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Britton A, Embi PJ, Levy ME, et al. Effectiveness of COVID-19 mRNA vaccines against COVID-19-associated hospitalizations among immunocompromised adults during SARS-CoV-2 Omicron predominance-VISION Network, 10 States, December 2021-August 2022. MMWR Morb Mortal Wkly Rep 2022; 71:1335–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin DY, Xu Y, Gu Y, et al. Effectiveness of bivalent boosters against severe Omicron infection. N Engl J Med 2023; 388:764–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tenforde MW, Weber ZA, Natarajan K, et al. Early estimates of bivalent mRNA vaccine effectiveness in preventing COVID-19-associated emergency department or urgent care encounters and hospitalizations among immunocompetent adults-VISION Network, Nine States, September-November 2022. MMWR Morb Mortal Wkly Rep 2022; 71:1616–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Poukka E, Goebeler S, Nohynek H, Leino T, Baum U. Bivalent booster effectiveness against severe COVID-19 outcomes in Finland, September 2022-January 2023. medRxiv, doi: 2023.03.02.23286561, 5 March 2023, preprint: not peer reviewed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Andersson NW, Thiesson EM, Baum U, et al. Comparative effectiveness of bivalent BA.4–5 and BA.1 mRNA booster vaccines among adults aged ≥50 years in Nordic countries: nationwide cohort study. BMJ 2023; 382:e075286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lin DY, Xu Y, Gu Y, Zeng D, Sunny SK, Moore Z. Durability of bivalent boosters against Omicron subvariants. N Engl J Med 2023; 388:1818–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Arbel R, Peretz A, Sergienko R, et al. Effectiveness of a bivalent mRNA vaccine booster dose to prevent severe COVID-19 outcomes: a retrospective cohort study. Lancet Infect Dis 2023; 23:914–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Link-Gelles R, Ciesla AA, Roper LE, et al. Early estimates of bivalent mRNA booster dose vaccine effectiveness in preventing symptomatic SARS-CoV-2 infection attributable to Omicron BA.5-and XBB/XBB.1.5-related sublineages among immunocompetent adults-increasing community access to testing program, United States, December 2022-January 2023. MMWR Morb Mortal Wkly Rep 2023; 72:119–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Link-Gelles R, Ciesla AA, Fleming-Dutra KE, et al. Effectiveness of bivalent mRNA vaccines in preventing symptomatic SARS-CoV-2 infection—increasing community access to testing program, United States, September-November 2022. MMWR Morb Mortal Wkly Rep 2022; 71:1526–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Auvigne V, Tamandjou C, Schaeffer J, Vaux S, Parent du Chatelet I. Protection against symptomatic SARS-CoV-2 BA.5 infection conferred by the Pfizer-BioNTech Original/BA.4–5 bivalent vaccine compared to the mRNA original (ancestral) monovalent vaccines—a matched cohort study in France. medRxiv, doi: 2023.03.17.23287411, 28 March 2023, preprint: not peer reviewed. [DOI] [PubMed] [Google Scholar]
- 18. Shrestha NK, Burke PC, Nowacki AS, Simon JF, Hagen A, Gordon SM. Effectiveness of the coronavirus disease 2019 bivalent vaccine. Open Forum Infectious Diseases 2023; 10(6):ofad209. doi: 10.1093/ofid/ofad2092022.12.17.22283625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Klaassen F, Chitwood MH, Cohen T, et al. Changes in population immunity against infection and severe disease from severe acute respiratory syndrome coronavirus 2 Omicron variants in the United States between December 2021 and November 2022. Clin Infect Dis 2023; 77:355–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Walgreens . COVID-19 testing for ages 3+. https://www.walgreens.com/findcare/covid19/testing. Accessed 1 October 2022.
- 21. Yoon P, Hall J, Fuld J, et al. Alternative methods for grouping race and ethnicity to monitor COVID-19 outcomes and vaccination coverage. MMWR Morb Mortal Wkly Rep 2021; 70:1075–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989; 129:125–37. [DOI] [PubMed] [Google Scholar]
- 23. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. N Engl J Med 2018; 378:2456–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Centers for Disease Control and Prevention . United States COVID-19 community levels by County. https://data.cdc.gov/Public-Health-Surveillance/United-States-COVID-19-Community-Levels-by-County/3nnm-4jni. Accessed 31 January 2023.
- 25. Chalkias S, Feng J, Chen X, et al. Neutralization of Omicron subvariant BA.2.75 after bivalent vaccination. N Engl J Med 2022; 387:2194–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chalkias S, Harper C, Vrbicky K, et al. A bivalent Omicron-containing booster vaccine against Covid-19. N Engl J Med 2022; 387:1279–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zou J, Kurhade C, Patel S, et al. Neutralization of BA.4-BA.5, BA.4.6, BA.2.75.2, BQ.1.1, and XBB.1 with bivalent vaccine. N Engl J Med 2023; 388:854–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jang EJ, Choe YJ, Kim RK, Lee S, Park SK, Park YJ. Estimated effectiveness of prior SARS-CoV-2 BA.1 or BA.2 infection and booster vaccination against Omicron BA.5 subvariant infection. JAMA Netw Open 2023; 6:e232578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pouwels KB, Pritchard E, Matthews PC, et al. Effect of Delta variant on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. Nat Med 2021; 27:2127–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hall V, Foulkes S, Insalata F, et al. Protection against SARS-CoV-2 after Covid-19 vaccination and previous infection. N Engl J Med 2022; 386:1207–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hulme WJ, Horne EMF, Parker EPK, et al. Comparative effectiveness of BNT162b2 versus mRNA-1273 covid-19 vaccine boosting in England: matched cohort study in OpenSAFELY-TPP. BMJ 2023; 380:e072808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Allen JC, Toapanta FR, Chen W, Tennant SM. Understanding immunosenescence and its impact on vaccination of older adults. Vaccine 2020; 38:8264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Crooke SN, Ovsyannikova IG, Poland GA, Kennedy RB. Immunosenescence and human vaccine immune responses. Immun Ageing 2019; 16:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Amirthalingam G, Bernal JL, Andrews NJ, et al. Serological responses and vaccine effectiveness for extended COVID-19 vaccine schedules in England. Nat Commun 2021; 12:7217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Skowronski DM, Febriani Y, Ouakki M, et al. Two-dose severe acute respiratory syndrome coronavirus 2 vaccine effectiveness with mixed schedules and extended dosing intervals: test-negative design studies from British Columbia and Quebec, Canada. Clin Infect Dis 2022; 75:1980–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lin DY, Xu Y, Gu Y, et al. Effects of COVID-19 vaccination and previous SARS-CoV-2 infection on Omicron infection and severe outcomes in children under 12 years of age in the USA: an observational cohort study [published online ahead of print 16 June 2023]. Lancet Infect Dis doi: 10.1016/S1473-3099(23)00272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Centers for Disease Control and Prevention . COVID-19 vaccination demographics in the United States, National, 2023. https://data.cdc.gov/Vaccinations/COVID-19-Vaccination-Demographics-in-the-United-St/km4m-vcsb. Accessed 31 January 2023.
- 38. Stamm TA, Partheymuller J, Mosor E, et al. Determinants of COVID-19 vaccine fatigue. Nat Med 2023; 29:1164–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sinclair AH. Reasons for receiving or not receiving bivalent COVID-19 booster vaccinations among adults—United States, November 1–December 10, 2022. MMWR Morb Mortal Wkly Rep 2023; 72:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Neely SR, Scacco JM. Receptiveness of American adults to COVID-19 vaccine boosters: a survey analysis. PEC Innov 2022; 1:100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. World Health Organization . Evaluation of COVID-19 vaccine effectiveness in a changing landscape of COVID-19 epidemiology and vaccination: interim guidance, 1 October 2022: second addendum to evaluation of COVID-19 vaccine effectiveness: interim guidance, 2022. https://www.paho.org/en/node/88928.
- 42. Lipsitch M, Goldstein E, Ray GT, Fireman B. Depletion-of-susceptibles bias in influenza vaccine waning studies: how to ensure robust results. Epidemiol Infect 2019; 147:e306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Smith PG, Rodrigues LC, Fine PE. Assessment of the protective efficacy of vaccines against common diseases using case-control and cohort studies. Int J Epidemiol 1984; 13:87–93. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.