Abstract
Background:
Researchers have attempted to understand the underlying mechanism of the Latarjet procedure; however, its effects on shoulder kinematics have not been well studied.
Purpose/Hypothesis:
The purpose was to analyze shoulder kinematics after the Latarjet procedure. It was hypothesized that the nonanatomic transfer of the coracoid process during the procedure would affect normal shoulder kinematics.
Study Design:
Controlled laboratory study.
Methods:
The study included 10 patients (age range, 20-52 years) who underwent the modified Latarjet procedure between June 2016 and November 2021. Computed tomography and fluoroscopy were conducted on both shoulder joints of all patients, and 3-dimensional models were reconstructed. The 3-dimensional coordinates were encoded on the reconstructed models, and shoulder kinematics were analyzed through a 3-dimensional–2-dimensional model-image registration technique. Scapular rotation parameters (scapular upward rotation, posterior tilt, external rotation, and scapulohumeral rhythm) were compared between the Latarjet and the nonsurgical contralateral sides during humeral abduction, as was anteroposterior (AP) translation relative to the glenoid center during active humeral external rotation.
Results:
The Latarjet side displayed significantly higher values of scapular upward rotation at higher degrees of humeral elevation (130°, 140°, and 150°) compared with the nonsurgical side (P = .027). Posterior tilt, external rotation, and scapulohumeral rhythm were not significantly different between sides. AP translation at maximal humeral rotation was not significantly different between sides (Latarjet, −0.06 ± 5.73 mm vs nonsurgical, 5.33 ± 1.60 mm; P = .28). Interestingly, on the Latarjet side, AP translation increased until 40° of humeral rotation (4.27 ± 4.64 mm) but began to decrease from 50° of humeral rotation.
Conclusion:
The Latarjet side demonstrated significant changes in scapular upward rotation during higher degrees of humeral elevation compared with the contralateral shoulder. Posterior movement of the humeral head at >50° of humeral rotation could be the desired effect of anterior stabilization; however, researchers should evaluate long-term complications such as osteoarthritis.
Clinical Relevance:
Analysis of shoulder kinematics after the Latarjet procedure could provide information regarding long-term outcomes and whether the procedure would affect the daily activities of patients.
Keywords: Latarjet, shoulder kinematics, scapulohumeral rhythm, 3D-2D model-image registration technique
The Latarjet procedure is performed for patients with >25% of glenoid bone loss or off-track glenohumeral instability; its indication is widening.7,22 Its primary mechanism is understood as a dynamic sling effect of the conjoint tendon on the inferior two-thirds of the subscapularis, which plays an important role in anterior glenohumeral stability. 21
The Latarjet procedure replaces glenoid bone loss, but it has a nonanatomic sling effect on the conjoint tendon by transferring the coracoid process to glenoid anteroinferior portion. Researchers have attempted to understand the process by which the mechanism would affect the 3-dimensional (3D) shoulder kinematics in actual patients under 3D dynamic settings.11,21,23 Previous studies have demonstrated the dynamic sling effect of the conjoint tendon through cadaveric models by reporting on stability improvement in vitro.5,11 Patel et al 19 evaluated the effects of the Latarjet procedure on glenohumeral kinematics in the setting of both glenoid and humeral Hill-Sachs lesion with cadaveric models.
Cadaveric models have limitations in reproducing in vivo kinematic tension and load sharing of the shoulder joint. Di Giacomo et al 8 performed an in vivo static magnetic resonance imaging (MRI) study evaluating glenohumeral translation in the abduction and external rotation (ABER) position in patients treated with the Latarjet procedure. Bey et al2-4 measured 3D dynamics of the shoulder joint during active motion with their model-based tracking technique in order to compare the rotator cuff repair and control groups. Nonetheless, researchers have not performed an in vivo 3D dynamics evaluation of glenohumeral joint translation during active shoulder motion in patients undergoing the Latarjet procedure.
Our study was designed to assess the combined effects of the pathologic condition (traumatic instability) and the Latarjet procedure on shoulder kinematics during active shoulder abduction and external rotation. We hypothesized that the Latarjet procedure would affect normal shoulder kinematics because it involves a nonanatomic transfer of the bone block attached to various conjoint tendons to compress the subscapularis, which would result in alterations of dynamic muscular tension. 2 Thus, we aimed to compare the changes in scapular rotation during humeral abduction and humeral head anteroposterior (AP) translation in humeral external rotation.
Methods
Participants
In this retrospective cohort study, we recruited patients who underwent the modified Latarjet procedure for unilateral traumatic recurrent instability at our institution between June 2016 and November 2021.14,24 Patients with a history of shoulder surgery or injury other than dislocation and those with multidirectional instability, postoperative nerve injury, or hardware loosening were excluded.
We included 10 men (age range, 20-52 years) who underwent the modified Latarjet procedure by a single surgeon (D.S.K.) using 2 bicortical 4.0-mm cannulated screws (DePuy Synthes), with minimum follow-up period of 1 year after the operation. All of the included patients achieved bony union on the surgical site and had no complications or limitations in range of motion, with good Constant-Murley scores (>85/100). Two patients were affected on the right side, and 8 were affected on the left side. Four patients were affected on the dominant side (2 right, 2 left shoulders), and 6 patients were affected on the nondominant side (all left shoulders). All of the included patients provided written informed consent after receiving a comprehensive explanation of the purpose of our study. The protocol of this study was approved by the institutional review board of our institution.
Surgical Technique
The patients were placed in the modified beach-chair position. Incisions were made using the deltopectoral approach. The anterior coracoacromial ligament and pectoralis minor were released from the coracoid process. The surgeon attempted to harvest the largest coracoid block, up to 20 mm; however, at least 17-mm bone blocks were harvested because of the smaller size of bone blocks in Asians, allowing the fixation using 2 screws. The harvested coracoid bone blocks were fixed onto the 3- to 6-o’clock position of the glenoid rim after splitting the subscapularis and performing capsulotomy. After firm fixation with 2 bicortical 4.0-mm cannulated screws (DePuy Synthes), the capsule was repaired.
Image Acquisition and 3D Reconstruction
Preoperative MRI and computed tomography (CT) (SOMATOM Sensation 16; Siemens Medical Solutions) scans were conducted, and postoperative CT scans were conducted at 3 months after surgery as a routine outpatient clinic evaluation. At 1 year postoperatively, fluoroscopic radiographs (Infinix Active; Toshiba) of the shoulder in humeral abduction and in external rotation were captured sequentially in 2 planes on each side of the shoulder for motion-related 3D dynamics evaluation of shoulder kinematics.
For the fluoroscopic radiographs, patients were in a sitting position with their torso 30° to the plane to align the scapula perpendicular to the x-ray beam; images were obtained at 10 frames per second. First, the patients were instructed to perform scapular plane abduction to the maximal tolerable angle with the palm facing forward, the thumb pointing up, and the elbow joint extended completely. We rehearsed the rate of arm movements in every patient and calculated the total number of collected shots after each movement. The x-ray beam was transmitted perpendicular to the coronal plane. One cycle was defined as arm abduction from 0° to the maximal tolerable angle and took approximately 2 to 3 seconds. Second, we instructed the patients to externally rotate the arm in the frontal plane with the elbow at 90° of flexion and the shoulder abducted to 90° (the 90-90 position). The x-ray beam was shot perpendicular to the axial plane. All patients rotated their arm from the initial position to the maximal angle for approximately 2 to 3 seconds per cycle. Each patient performed a single cycle of the fluoroscopic procedure for both shoulders. They abducted and rotated their arm to the maximal tolerated angle, and no patient displayed a limited range of motion on gross examination. Because real-time angle measurement is impossible during fluoroscopy, numerous values obtained from various angles were again fit to the polynomial curve; interpolation was performed to obtain the exact value at the desired angles.
The CT scans of the bilateral shoulders were performed with a 1-mm slice pitch (image matrix, 512 × 512; pixel size, 0.9765625 × 0.9765625 mm). The CT images were segmented, and 3D models of the humerus, scapula, and clavicle were constructed using ITK-SNAP (Penn Image Computing and Science Laboratory) (Figure 1). X-, Y-, and Z-axes were applied to the 3D-reconstructed model using the anatomic coordinate system (Geomagic Studio).13,18 The humeral origin was at the centroid of the humeral head. The Y-axis was the longitudinal shaft axis, the Z-axis was the line penetrating the bicipital groove, and the X-axis was a line perpendicular to the plane formed by the Y- and Z-axes. The scapular origin was set at the midpoint between the most superior and inferior bony edges of the glenoid; the Y-axis pointed superiorly and the Z-axis pointed anteriorly from the origin (Figure 2).
Figure 1.

(A) Representative computed tomography axial image from which the 3D model of the scapula (shaded in gray) and humerus (shaded in blue) was constructed. (B) Reconstructed 3D model showing gray-shaded scapula, blue-shaded humerus, and gold-shaded screw.
Figure 2.
Three-dimensional models of the (A) shoulder joint, (B) glenoid, and (C) humerus. Upon reconstruction, the anatomic coordinates were applied with Geomagic Studio. The red line is the X-axis; green line, Y-axis; and purple line, Z-axis.
3D Model/2-Dimensional Image Registration
The 3D models with anatomic coordinates were registered to the 2-dimensional (2D) fluoroscopic images using JointTrack, an open-source software program (www.sourceforge.net/projects/jointtrack).15-17,20 Similar 3D model/2D image registration techniques have been discussed previously. 1 The size and orientation of the 3D-reconstructed models were fit to the 2D fluoroscopic images by the first author (J.P.), an operator who is aware of the relevant anatomic features. The first author also constructed the 3D model for registration of the fluoroscopic image series (Figure 3). A similar concept of single-plane 3D shape registration was described previously in uninjured shoulder joints, and the precision of this technique was confirmed as being 0.53 mm for in-plane translation, 1.6 mm for out-of-plane translation, and 0.54° for rotation.6,16
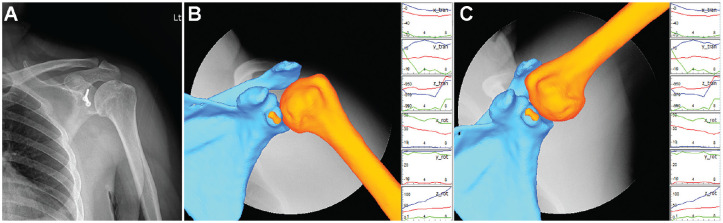
Figure 3.
Three-dimensional (3D) models with coordinates are encoded on 2-dimensional (2D) fluoroscopic images with the 3D-2D model-image registration technique. (A) Clinical radiograph of a left shoulder after undergoing the Latarjet procedure, and the corresponding 3D model with applied fluoroscopic image at (B) the resting position (palm facing forward, thumb pointing up, and elbow joint extended completely) and (C) maximal abduction. The graphs in parts B and C indicate rotation (rot) and translation (tran) of each axis of the specific model using JointTrack software.
The humeral and scapular kinematic parameters in the radiographic coordinate system were analyzed using Euler and Cardan angles. 12 Humeral abduction was defined as the degree of rotation around the Z-axis, and humeral external rotation was defined as the degree of rotation around the Y-axis. Regarding scapular motion, anterior-posterior tilt was defined as the rotation around the X-axis, internal-external rotation was defined as the rotation around the Y-axis, and upward-downward rotation was defined as the rotation around the Z-axis. The AP translation of the humeral head center was defined relative to the Z-axis of the center of the scapula (Figure 2).
Data Extraction
We calculated humeral abduction as the independent variable for scapular rotation parameters (including upward rotation, posterior tilt, external rotation, and scapulohumeral rhythm [SHR]) and humeral external rotation as the independent variable for relative AP translation of the humeral head with the scapula. MATLAB code (MathWorks) was used to extract the shoulder kinematic values for every 10° increment of humeral ABER, and polynomial curve fitting and interpolation were performed to analyze the expected data at specific 10° increments of the independent variables.
SHR was calculated as (ΔH−ΔS)/ΔS = 1/(ΔS/ΔH) – 1, 16 where ΔH indicates changes in the humeral abduction angle and ΔS represents changes in the scapular upward rotation angle. Polynomial curve fitting was previously performed for humeral abduction and scapular upward rotation in the data interpolation stage. Subsequently, ΔS/ΔH was calculated with differentials of the function expression. The humeral abduction angle was the independent value for SHR. Thus, we calculated the SHR for both shoulders with 10° increments of humeral abduction.
Statistical Analysis
The changes in scapular rotation during humeral abduction and in humeral head AP translation during humeral external rotation were compared between the Latarjet and nonsurgical shoulders using 2-way repeated-measures analysis of variance. The initial values for scapular rotation (measured in degrees) and humeral head AP translation (measured in millimeters) were reset to zero when the humeral abduction or external rotation values were zero. This approach helped to minimize errors derived from varying scapular orientations and locations among the patients. A post hoc Bonferroni-corrected t test was performed upon detecting a significant difference. P values <.05 were considered statistically significant.
Results
Figure 4 depicts comparisons between the Latarjet and nonsurgical sides for scapular upward rotation, posterior tilt, and external rotation and SHR for every 10° of humeral elevation during humeral abduction. Figure 5 depicts the comparison between the Latarjet and nonsurgical sides for humeral head AP translation for every 10° of external rotation of the humerus.
Figure 4.
Comparison between the Latarjet and nonsurgical sides for scapular rotation parameters according to humeral abduction. (A) Scapular upward rotation, (B) scapular posterior tilt, (C) scapular external rotation, and (D) scapulohumeral rhythm. Error bars indicate standard deviation. *Statistically significant difference between sides (P < .05).
Figure 5.

Comparison between the Latarjet and nonsurgical sides for humeral anteroposterior (AP) translation relative to the glenoid center according to humeral external rotation. Error bars indicate standard deviation.
Scapular Upward Rotation
In both the Latarjet and nonsurgical sides, scapular upward rotation increased with humeral elevation. Interestingly, the overall changes of scapular upward rotation were greater on the Latarjet side, but only those at the higher degrees of humeral elevation (130°, 140°, and 150°) were significantly different from the nonsurgical side. The scapular upward rotation at 150° of humeral elevation was 51.74°± 10.54° and 30.51°± 6.46° for the Latarjet and nonsurgical sides, respectively (P = .027) (Figure 4A).
Scapular Posterior Tilt
In both groups, the scapular posterior tilt values increased with the degree of humeral elevation. The Latarjet side displayed lower values of scapular posterior tilt than the nonsurgical side; however, the difference was nonsignificant. The scapular posterior tilt at 150° of humeral elevation was 33.54°± 3.93° and 39.1°± 5.64° for the Latarjet and nonsurgical sides, respectively (P = .291) (Figure 4B).
Scapular External Rotation
The degree of scapular external rotation increased in both groups in proportion to the humeral elevation angles. The Latarjet side displayed overall limitation of scapular external rotation compared with the nonsurgical side; however, the difference was not significant. The values of scapular external rotation at 150° of humeral elevation were 16.15°± 8.76° and 22.0°± 4.2° for the Latarjet and nonsurgical sides, respectively (P = .48) (Figure 4C).
Scapulohumeral Rhythm
The slope of the upward rotation of the scapula (ΔS/ΔH) increased more on the Latarjet side with humeral elevation; simultaneously, SHR [1/(ΔS/ΔH) – 1] displayed decreasing values for the Latarjet side. The difference of values in SHR between the Latarjet and nonsurgical sides increased with humeral elevation; however, this difference was nonsignificant. The values of SHR at 150° of humeral elevation were 1.71 ± 0.36 and 6.93 ± 3.39 for the Latarjet and nonsurgical sides, respectively (P = .14) (Figure 4D).
AP Translation of the Humeral Head
With the forearm facing straight forward in the 90-90 position (defined as 0° of Y-axis rotation of the humerus), we calculated AP translation beginning from 30° of internal rotation (–30°) to the maximal external rotation (90°) of the humerus, which ended at the maximal external rotation ABER position. The humeral head translated anteriorly with an increase in humeral rotation on the nonsurgical side. Interestingly, on the Latarjet side, AP translation increased until 40° of humeral rotation (4.27 ± 4.64 mm) but began to decrease at 50° of rotation. No significant differences were found in AP translation at any angle of humeral rotation. However, at the maximal humeral rotation, the AP translation values were −0.06 ± 5.73 mm and 5.33 ± 1.60 mm in the Latarjet and nonsurgical sides, respectively (P = .28) (Figure 5).
Discussion
Researchers have attempted to understand the stabilization mechanism underlying the Latarjet procedures. Wellmann et al 22 stated that belt-suspension stabilization by the conjoint tendons and subscapularis tendon is central to the ABER position and that the transferred coracoacromial ligament with capsule reconstruction is crucial in abduction and neutral rotation. Studies have proven the normalization of articular contact pressures of the glenohumeral joint and the sling effect of the coracobrachialis crossing the subscapularis. 10 Yamamoto et al 23 stated that the sling effect is the primary contributor to stability and that the percentage of effect increases with the range of motion. Patel et al 19 measured the upper limit of the Latarjet procedure with combined defects of glenoid bone loss and humeral head bone defect in cadaveric models; the investigators stated that coracoid transfer itself would not resolve the instability in cases with >31% humeral head bone loss. The stability gained after the Latarjet procedure does not depend solely on the bony structure augmentation itself but rather depends more on the musculocutaneous component (sling effect of the conjoint tendon and subscapularis).
Kinematic tension must be recreated to evaluate the actual effect of the muscular component of the Latarjet procedure. Despite several attempts to reproduce the dynamic component in elaborate settings with cadaveric models,5,11,19,23 recreating physiologic muscle tension and proprioception has been unsuccessful. Researchers have reported on the disharmony of glenohumeral translational results between in vivo and in vitro studies. 8 Thus, dynamic in vivo evaluation of shoulder kinematics is crucial; however, technical impalpability is the primary issue because of the challenging motion-related dynamic CT scan.
Di Giacomo et al 8 evaluated glenohumeral translation with in vivo MRI in the ABER position in patients who underwent the Latarjet procedure. Those authors understood the limitations of an in vitro study and performed elaborate work to recreate the in vivo dynamic contraction in the ABER position. Nonetheless, the patients’ position was static during the MRI scan; although ABER position represents the end critical position in the evaluation of glenohumeral stability, it does not reproduce dynamic shoulder kinematics while patients elevate their arm from 0° to the maximal degrees in real time. We can use a fluoroscopic view while patients abduct and rotate their arm on both sides, thus highlighting whether 2D images can be converted to 3D images for dynamic kinematic evaluation. Matsuki et al 16 performed a novel study using biplane and monoplane fluoroscopes to address scapular asymmetry by analyzing dynamic scapular rotation using a 3D-2D registration technique.
In our study, most shoulder kinematic parameters did not display a significant difference between the Latarjet and nonsurgical sides. This finding could be attributed to our small sample size. However, upward rotation of the scapula displayed significantly higher values at maximal degrees of humeral elevation. One can assume that because maximal humeral abduction is rare in daily activities, the Latarjet procedure does not significantly affect patients’ shoulder kinematics during daily activities. The exact mechanism of the Latarjet procedure is not understood; nonetheless, the dynamic sling effect of conjoint tendon on subscapularis may have played a significant role. However, the trapezius, rhomboids, and serratus anterior muscles are not expected to be directly affected by the Latarjet procedure. Consequently, alterations in scapular mechanics are more likely to result from decreased glenohumeral motion and loss of the pectoralis minor antagonist.
Study results indicated that AP translation of the humeral head decreased with a >50° increase in humeral rotation, suggesting that the head began to move posteriorly. The ABER position makes the humeral head move anteriorly and is the critical position for anterior instability of shoulder. Because of the sling effect, the Latarjet procedure may affect normal physiologic parameters and prevent anterior dislocation, which was the desired result. However, this phenomenon can cause more pressure on the posterior glenohumeral joint and may generate glenohumeral osteoarthritis in the long term. 9 Furthermore, decreased external rotation and posterior tilt of the scapula could lead to subacromial impingement. In addition, increased posterior translation will increase internal impingement and posterior labral pathology. Considering these results, we can point to the potential for increasing the sample size and extending the follow-up period to guide the direction of future studies. Longer term follow-up of patients with Latarjet is needed to determine whether these theoretical concerns actually occur clinically.
Limitations
This study has some limitations. We could not perform presurgical dynamic evaluation for patients with glenohumeral instability; thus, it is difficult to determine whether the kinematic differences seen were a result of the pathology itself on the surgically reconstructed side. Thus, the reported values may not have been solely derived from the effects of the surgical procedure. Moreover, the limited number of cases could affect the significance of our results. Thus, the study may be underpowered to detect some differences because of the small sample size. In our center, Latarjet procedures are less commonly performed than Bankart repairs and are usually reserved for patients with severe glenohumeral instability; patient recruitment was also affected because of the coronavirus 2019 pandemic. Multicenter studies using a similar dynamic evaluation protocol could be beneficial in the future. In addition, our findings did not reflect dynamic positioning of patients during the fluoroscopic procedure and differences in the anatomic orientation of the scapula. To minimize the error, the patients were instructed to sit with the torso 30° to the plane and maintain the position. Radiation hazard can be another issue for patients undergoing fluoroscopy for both shoulders. We could not include other sets of shoulder movements, such as horizontal extension (ie, the apprehension position), because of these problems. We conducted each cycle a single time for approximately 2 to 3 seconds in order to minimize radiation exposure. This 3D-2D matching technique has merits over other types of dynamic motion analysis, for instance, external motion capture technique involves non-rigid coupling of probes to bones and skin slippage can occur. We hypothesized that the differences in scapular rotation and relative humeral translation to the glenoid were principally attributable to anatomic differences rather than the effect of dynamic muscular tension at a humeral ABER position of 0°, which implies the neutral position. Attempts to confirm the difference at resting position as well as before surgery could reveal the effects of specific components in the future.
Conclusion
The Latarjet side of the study patients demonstrated significant changes in scapular upward rotation during maximal humeral elevation compared with the contralateral nonsurgical shoulder. Posterior tilt, external rotation, and SHR were not significantly different between the sides. Posterior movement of the humeral head at >50° of humeral rotation could be the desired effect of anterior stabilization; however, researchers should evaluate long-term complications such as osteoarthritis or subacromial impingement and determine whether these theoretical concerns occur in practice. It would be beneficial to determine the true kinematic effect of the surgery itself, excluding the pathologic presurgical condition, if possible.
Footnotes
Final revision submitted August 3, 2023; accepted August 18, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: Grant support was received from the National Research Foundation of Korea funded by the Korean government (NRF-2021R1C1C1003481 to H.H.). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Yonsei University Wonju Severance Christian Hospital (ref No. CR322005).
References
- 1. Banks SA, Hodge WA. Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng. 1996;43(6):638-649. doi: 10.1109/10.495283 [DOI] [PubMed] [Google Scholar]
- 2. Bey MJ, Kline SK, Zauel R, Lock TR, Kolowich PA. Measuring dynamic in-vivo glenohumeral joint kinematics: technique and preliminary results. J Biomech. 2008;41(3):711-714. doi: 10.1016/j.jbiomech.2007.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bey MJ, Peltz CD, Ciarelli K, et al. In vivo shoulder function after surgical repair of a torn rotator cuff: glenohumeral joint mechanics, shoulder strength, clinical outcomes, and their interaction. Am J Sports Med. 2011;39(10):2117-2129. doi: 10.1177/0363546511412164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bey MJ, Zauel R, Brock SK, Tashman S. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng. 2006;128(4):604-609. doi: 10.1115/1.2206199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boons HW, Giles JW, Elkinson I, Johnson JA, Athwal GS. Classic versus congruent coracoid positioning during the Latarjet procedure: an in vitro biomechanical comparison. Arthroscopy. 2013;29(2):309-316. doi: 10.1016/j.arthro.2012.09.007 [DOI] [PubMed] [Google Scholar]
- 6. Chung H, Kim D, Banks SA, et al. Evaluation of three-dimensional in vivo scapular kinematics and scapulohumeral rhythm between shoulders with a clavicle hook plate and contralateral healthy shoulders. Int Orthop. 2019;43(2):379-386. doi: 10.1007/s00264-018-4003-y [DOI] [PubMed] [Google Scholar]
- 7. Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy. 2014;30(1):90-98. doi: 10.1016/j.arthro.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 8. Di Giacomo G, Scarso P, De Vita A, Rojas Beccaglia MA, Pouliart N, de Gasperis N. Glenohumeral translation in ABER position during muscle activity in patients treated with Latarjet procedure: an in vivo MRI study. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):521-525. doi: 10.1007/s00167-015-3896-x [DOI] [PubMed] [Google Scholar]
- 9. Domos P, Lunini E, Walch G. Contraindications and complications of the Latarjet procedure. Shoulder Elbow. 2018;10(1):15-24. doi: 10.1177/1758573217728716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ghodadra N, Gupta A, Romeo AA, et al. Normalization of glenohumeral articular contact pressures after Latarjet or iliac crest bone-grafting. J Bone Joint Surg Am. 2010;92(6):1478-1489. doi: 10.2106/JBJS.I.00220 [DOI] [PubMed] [Google Scholar]
- 11. Giles JW, Boons HW, Elkinson I, et al. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013;22(6):821-827. doi: 10.1016/j.jse.2012.08.002 [DOI] [PubMed] [Google Scholar]
- 12. Hebert LJ, Moffet H, McFadyen BJ, Dionne CE. Scapular behavior in shoulder impingement syndrome. Arch Phys Med Rehabil. 2002;83(1):60-69. doi: 10.1053/apmr.2002.27471 [DOI] [PubMed] [Google Scholar]
- 13. Kon Y, Nishinaka N, Gamada K, Tsutsui H, Banks SA. The influence of handheld weight on the scapulohumeral rhythm. J Shoulder Elbow Surg. 2008;17(6):943-946. doi: 10.1016/j.jse.2008.05.047 [DOI] [PubMed] [Google Scholar]
- 14. Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49(8):994-997. [PubMed] [Google Scholar]
- 15. Lawrence RL, Ellingson AM, Ludewig PM. Validation of single-plane fluoroscopy and 2D/3D shape-matching for quantifying shoulder complex kinematics. Med Eng Phys. 2018;52:69-75. doi: 10.1016/j.medengphy.2017.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Matsuki K, Matsuki KO, Mu S, et al. In vivo 3-dimensional analysis of scapular kinematics: comparison of dominant and nondominant shoulders. J Shoulder Elbow Surg. 2011;20(4):659-665. doi: 10.1016/j.jse.2010.09.012 [DOI] [PubMed] [Google Scholar]
- 17. Matsuki K, Wada Y. Validation of 2D/3D registration technique for shoulder joint using single-and bi-plane fluoroscopy. Jpn J Clin Biomech. 2012;33:151-155. [Google Scholar]
- 18. Nishinaka N, Tsutsui H, Mihara K, et al. Determination of in vivo glenohumeral translation using fluoroscopy and shape-matching techniques. J Shoulder Elbow Surg. 2008;17(2):319-322. doi: 10.1016/j.jse.2007.05.018 [DOI] [PubMed] [Google Scholar]
- 19. Patel RM, Walia P, Gottschalk L, et al. The effects of Latarjet reconstruction on glenohumeral kinematics in the presence of combined bony defects: a cadaveric model. Am J Sports Med. 2016;44(7):1818-1824. doi: 10.1177/0363546516635651 [DOI] [PubMed] [Google Scholar]
- 20. Sugi A, Matsuki K, Fukushi R, et al. Comparing in vivo three-dimensional shoulder elevation kinematics between standing and supine postures. JSES Int. 2021;5(6):1001-1007. doi: 10.1016/j.jseint.2021.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Walch G, Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg. 2000;1(4):256-261. [Google Scholar]
- 22. Wellmann M, de Ferrari H, Smith T, et al. Biomechanical investigation of the stabilization principle of the Latarjet procedure. Arch Orthop Trauma Surg. 2012;132(3):377-386. doi: 10.1007/s00402-011-1425-z [DOI] [PubMed] [Google Scholar]
- 23. Yamamoto N, Muraki T, An KN, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013;95(15):1390-1397. doi: 10.2106/JBJS.L.00777 [DOI] [PubMed] [Google Scholar]
- 24. Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg. 2011;20(2)(suppl):S61-S69. doi: 10.1016/j.jse.2010.07.022 [DOI] [PubMed] [Google Scholar]