Abstract
We used a live attenuated murine cytomegalovirus (MCMV) mutant to analyze mechanisms of vaccination against acute and latent CMV infection. We selected MCMV mutant RV7 as a vaccine candidate since this virus grows well in tissue culture but is profoundly attenuated for growth in normal and severe combined immunodeficient (SCID) mice (V. J. Cavanaugh et al., J. Virol. 70:1365–1374, 1996). BALB/c mice were immunized twice (0 and 14 days) subcutaneously (s.c.) with tissue culture-passaged RV7 and then challenged with salivary gland-passaged wild-type MCMV (sgMCMV) intraperitoneally (i.p.) on day 28. RV7 vaccination protected mice against challenge with 105 PFU of sgMCMV, a dose that killed 100% of mock-vaccinated mice. RV7 vaccination reduced MCMV replication 100- to 500-fold in the spleen between 1 and 8 days after challenge. We used the capacity to control replication of MCMV in the spleen 4 days after challenge as a surrogate for protection. Protection was antigen specific and required both live RV7 and antigen-specific lymphocytes. Interestingly, RV7 was effective when administered s.c., i.p., perorally, intranasally, and intragastrically, demonstrating that attenuated CMV applied to mucosal surfaces can elicit protection against parenteral virus challenge. B cells and immunoglobulin G were not essential for RV7-induced immunity since B-cell-deficient mice were effectively vaccinated by RV7. CD8 T cells, but not CD4 T cells, were critical for RV7-induced protection. Depletion of CD8 T cells by passive transfer of monoclonal anti-CD8 (but not anti-CD4) antibody abrogated RV7-mediated protection, and RV7 vaccination was less efficient in CD8 T-cell-deficient mice with a targeted mutation in the β2-microglobulin gene. Although gamma interferon is important for innate resistance to MCMV, it was not essential for RV7 vaccination since gamma interferon receptor-deficient mice were protected by RV7 vaccination. Establishment of and/or reactivation from latency by sgMCMV was decreased by RV7 vaccination, as measured by diminished reactivation of MCMV from splenic explants. We found no evidence for establishment of splenic latency by RV7 after s.c. vaccination. We conclude that RV7 administered through both systemic and mucosal routes is an effective vaccine against MCMV infection. It may be possible to design human CMV vaccines with similar properties.
Cytomegalovirus (CMV) infection is a significant problem in AIDS patients, newborns, and immunocompromised hosts (9), and a significant source of CMV disease is reactivation of CMV from latency (27, 28). Trials of attenuated human CMV (HCMV) isolates in humans have shown protection from acute infection (see Discussion), and a cost-benefit analysis has suggested that an effective HCMV vaccine would be valuable in preventing HCMV-related illness. Thus, an effective vaccine would lessen the burden of CMV infection and disease, particularly in congenital CMV infection, which is a significant cause of birth defects (1, 5, 31, 52, 53, 57, 66). While human trials have shown protection against HCMV disease by vaccination with an attenuated virus, the mechanisms by which exposure to an attenuated virus protects against CMV virus have not been defined. In addition, the effects of exposure to a live attenuated virus on CMV latency have not been assessed, and the question of whether oral exposure to CMV elicits immunity has not been addressed.
Questions as to mechanisms of immune protection against betaherpesviruses can be addressed in the murine CMV (MCMV) system since HCMV and MCMV are related viruses and immunologic analysis in the mouse is facilitated by genetic models and availability of reagents for analysis of T cells and latent MCMV. To date, mechanisms of immunity to MCMV and HCMV have been found to be similar (see Discussion). During MCMV infection, the products of major immediate-early (MIE) locus genes can elicit immune responses, as do additional MCMV proteins (13, 16, 61, 62). Since even immunity afforded by natural primary HCMV infection may be relatively inefficient at preventing reinfection (see Discussion), development of a vaccine will likely require maximal induction of host immunity against multiple CMV antigens. While subunit, peptide, or DNA vaccines may meet these criteria (3, 63), we have begun to analyze vaccination against CMV by using a stably attenuated live vaccine, on the theory that effective immunity may be most easily and effectively induced by live attenuated vaccination. We were encouraged to pursue this approach by (i) the precedent provided by the varicella virus vaccine now in use in humans, (ii) previous studies showing that wild-type (wt) MCMV can elicit protective immunity (26, 33, 45, 46, 60, 62), (iii) previous studies showing that a temperature-sensitive (ts) mutant of MCMV can be used as a vaccine (69), (iv) the fact that vaccinia viruses expressing MCMV proteins can effectively vaccinate against MCMV infection (16, 33), (v) the fact that vaccination with guinea pig CMV can protect against transplacental spread of guinea pig CMV (5), and (vi) the fact that vaccination with replication-defective HSV mutants protects against HSV disease and inhibits establishment of HSV latency (47, 48).
We recently demonstrated a profound attenuation in MCMV virulence associated with deletion of open reading frames m137, m138, M139, M140, and M141 of the MCMV genome (MCMV mutant RV7 [11]). While less than 5 PFU of wt tissue culture-passaged MCMV kills 100% of severe combined immunodeficient (SCID) mice, 7.8 × 105 PFU of tissue culture-passaged RV7 fails to kill SCID mice for at least 100 days (reference 11 and unpublished data). Interestingly, RV7 grows normally in fibroblasts but grows poorly in the peritoneal macrophage cell line IC-21 (11) and in primary peritoneal macrophages (unpublished data). This allows easy production of sufficient amounts of RV7 for vaccine trials despite its attenuation in vivo. However, the fact that RV7 fails to efficiently grow in macrophages, professional antigen-presenting cells, raises questions as to the nature of the immune response that might be generated by infection with RV7.
The availability of RV7 presented us with a novel opportunity to address the efficacy of a defined stably attenuated MCMV mutant as a vaccine. This is because RV7 carries a deletion which cannot revert in vivo and does not replicate to a detectable level in normal mice (11). Previous studies of vaccination with attenuated MCMV have used either (i) an attenuated ts MCMV (ts21) which is about 26-fold less virulent than wt MCMV in suckling mice but whose attenuation and mechanisms of protection have not been defined (41, 69) or (ii) tissue culture-passaged “attenuated” wt MCMV which, while less virulent than salivary gland-passaged MCMV (sgMCMV), is not stably attenuated and reverts to virulence in vivo (20, 26, 30, 45, 46, 50).
We used RV7 vaccination to determine the immune mechanisms responsible for protection by vaccination with a stably attenuated MCMV mutant. In addition, we wished to address questions that have not previously been dealt with, including whether vaccination with an attenuated MCMV mutant (i) is effective via mucosal routes, (ii) inhibits establishment of latency by wt MCMV, and (iii) results in establishment of systemic latency by the attenuated virus under conditions which result in protective immunity.
MATERIALS AND METHODS
Cells and tissue culture media.
All media contained 100 U of penicillin and 100 μg of streptomycin (Biofluids, Rockville, Md.) per ml, 1% glutamine (Biofluids), and 10 mM HEPES (Biofluids). Murine embryonic fibroblasts (MEFs) were generated by cultivation of minced BALB/c mouse embryos (days 14 to 16) in lots of Dulbecco’s modification of Eagle’s medium tested to be endotoxin free (EMEM; Mediatech, Washington, D.C.) containing 10% fetal calf serum (FCS; HyClone, Logan, Utah) (56). MEFs were used during initial passaging or thawed from frozen stocks. All MEFs were used before the 5th passage. NIH 3T12 fibroblasts (ATCC CCL 164) were used to grow virus stocks and for plaque assays as previously described (24). Dulbecco’s modified Eagle medium used in plaque assays was from GibcoBRL (Life Technologies, Grand Island, N.Y.).
Viruses, virus stocks, and plaque assay.
MCMV Smith strain was obtained from the American Type Culture Collection (VR-194, lot 10). The MCMV mutant RV7 was grown from stocks, and its identity was confirmed by Southern blotting using the HindIII-J region of the genome as a probe (11). Tissue culture-passaged wt MCMV and RV7 stocks were generated from infected 3T12 cell supernatant as previously described (24). Briefly, virus was grown in 3T12 cells until the development of cytopathic effect (CPE) was complete. Cells and media were harvested, clarified by a low-speed centrifugation, and centrifuged at 13,600 × g for 2 h, and the virus-containing pellet was resuspended in EMEM containing 5% FCS. Mock vaccinations were performed with EMEM containing 5% FCS. sgMCMV stocks were made as 10% suspensions of salivary glands of 8-week-old BALB mice infected intraperitoneally (i.p.) with 105 PFU tissue culture-passed MCMV 17 days prior to harvest (56). Virus stocks were stored at −80°C. MCMV was titered by plating serial dilutions of sample on duplicate 3T12 fibroblast monolayers and staining with neutral red as previously described (24). MCMV was inactivated by using UV light as previously described (24). Herpes simplex virus type 1 strain KOS (HSV) was obtained from Paul Olivo and grown in Vero cells as previously described (24). Reovirus serotype 3 strain Dearing (T3D) was obtained from Bernard Fields and was grown and titered as previously described (4).
Mouse strains.
BALB/c mice (5 to 7 weeks of age; National Cancer Institute, Frederick, Md.) were used for most experiments. C57BL/6J-Igh-6tm1Cgn mice (referred to as B6.Ig−/− mice) lacking B cells and immunoglobulin due to a null mutation in the immunoglobulin M (IgM) heavy chain (38) were purchased from Jackson Laboratory and bred in our facility. C57BL/6J-B2mtm1Unc mice (referred to as B6.β2−/− mice) carrying a null mutation in the gene for β2-microglobulin (39) were obtained from Jackson Laboratory and bred in our facility. Gamma interferon (IFN-γ) receptor-deficient (IFNγR−/−) mice and their congenic control 129 Ev/Sv mice (referred to as 129 mice) were obtained from Michel Aguet and bred in our facility (29). SCID mice on the CB17 background were bred in our facilities (7). Sentinel mice were assayed every 3 months and were negative for adventitious mouse pathogens by serology.
Mouse vaccination and challenge.
Mice were anesthetized with metofane prior to vaccination. Virus for vaccination was diluted in EMEM containing 5% FCS. In most experiments, mice were vaccinated subcutaneously (s.c.) in the left hind limb/base of the tail with 2 × 105 PFU of RV7 in 100 μl, using a 22-gauge needle. In other experiments, mice were vaccinated with 2 × 105 PFU of RV7 diluted into 50 μl for peroral vaccination, 10 μl for intranasal vaccination, or 100 μl for intragastric vaccination (administered via soft tubing [70]). Peroral vaccination was performed by placing 50 μl of inoculum in the mouth of a lightly anesthetized mouse and waiting until the mouse swallowed the inoculum on emerging from anesthesia. Mice were challenged intraperitoneally (i.p.) with 1.0 ml of sgMCMV, using doses specified in figure legends. Approximately 0.2 g of liver and the spleen were harvested, minced, suspended in 1.0 ml of EMEM containing 10% FCS, and frozen at −80°C prior to plaque assay.
In vivo depletion of CD4 and CD8 T cells.
Mock- or RV7-vaccinated mice were injected i.p. with rat monoclonal antibodies specific for either CD4 or CD8 to deplete T cells in vivo. Monoclonal antibodies were purified from tissue culture supernatant on protein G-Sepharose as previously described (71) and frozen at −80°C in phosphate-buffered saline. CD4 T cells were depleted with monoclonal antibody GK1.5 (ATCC TIB 207), and CD8 T cells were depleted with monoclonal antibody H35 (65). Mice treated by i.p. injection with either diluent alone or rat IgG (reagent grade; Sigma, St. Louis, Mo.) were used as controls. Mice were immunized on days 0 and 14 and challenged on day 28 with 104 PFU of sgMCMV, and spleens were harvested on day 32. One half of the spleen was used to determine viral titer, and one half was used to prepare spleen cells for fluorescence-activated cell sorting (FACS) analysis. Spleens from three to four mice per group were pooled for FACS analysis, while MCMV titers were determined in individual spleens. FACS staining was performed as described previously (4, 24) and the data were analyzed by using WinMDI (developed by Joseph Trotter). In one experiment, mice were treated on days 27 and 29 with 0.5 mg of either monoclonal or control antibodies. In this experiment, CD8 depletion was >99% in mock-vaccinated mice and 96% in RV7-vaccinated mice, while CD4 depletion was >99% in mock-vaccinated mice but only 57% in RV7-vaccinated mice. In a second experiment, mice were treated with 1.0 mg of antibody on day 27 and with 0.5 mg of antibody on days 28 and 29. Using this higher-dose protocol, CD4 and CD8 depletion was >99% in both mock-vaccinated and RV7-vaccinated mice.
Reactivation of latent MCMV from spleen explants.
Spleens were harvested from experimental mice and explanted for reactivation as follows. Individual spleens were screened for persistent infection by taking one-fourth of the spleen and freeze-thawing, sonicating, and culturing it in a T75 flask containing confluent MEFs. T75 flasks were held for 14 days and scored for CPE. This protocol reproducibly detects 1 to 5 PFU of MCMV in an organ sonicate (56). As positive controls, 5 PFU of MCMV was added to T75 flasks and scored for CPE, which in all cases was positive. For reactivation assays, one half of the spleen was minced in 10 ml of EMEM containing 10% FCS, homogenized in a 7-ml Ten Broeck tissue homogenizer (Bellco Glass, Vineland, N.J.), and then cultured in two wells of a six-well tissue culture plate. Medium from the explant wells was sampled for virus, and cultures were fed with 5 ml of EMEM containing 10% FCS every 3 to 4 days. Virus produced after reactivation was detected by freeze-thawing 100 μl of medium from explant wells and then culturing it with 100 μl of EMEM containing 10% FCS and 5 × 103 to 8 × 103 MEFs in a 96-well plate for 14 days, at which time MCMV was detected by CPE in the MEF monolayer. This assay reproducibly detects 1 to 10 PFU of MCMV (56). When two samples from an individual explant well were positive for infectious virus, reactivation was considered confirmed. To determine whether reactivating virus was wt MCMV or RV7, virus from individual explant wells was harvested after reactivation and used to infect confluent 3T12 fibroblasts. After 100% CPE was obtained, the entire contents of the dish were harvested and DNA was prepared by proteinase K-sodium dodecyl sulfate digestion followed by phenol-chloroform extraction and ethanol precipitation. Samples of DNA were digested with HindIII and BglII and analyzed by Southern blotting as previously described (56), using labeled HindIII-J genomic probe (kindly provided by D. Spector). This digestion and blotting procedure distinguishes between wt MCMV and RV7 via generation of characteristic bands on Southern blot analysis (11).
MCMV genome detection.
MCMV DNA was detected by nested PCR as previously described (55, 56). Organ DNA was prepared by using a QIAamp tissue kit (Qiagen, Chatsworth, Calif.) followed by two phenol-chloroform extractions, ethanol precipitation, and resuspension in 10 mM Tris with 1 mM EDTA. MCMV DNA was detected via nested PCR of samples containing 0.5 to 1.0 μg of total organ DNA (56). This PCR assay reproducibly detects 1 to 10 copies of the MCMV ie1 gene (55, 56). Reaction products were electrophoresed and stained with ethidium bromide to detect ie1-specific product. Previous studies showed that use of ethidium bromide to detect reaction products from this nested PCR assay is as sensitive as Southern blot analysis and that the DNA recovery methods used quantitatively recover MCMV genome sequences (56).
RESULTS
Vaccination with RV7 protects against lethal infection.
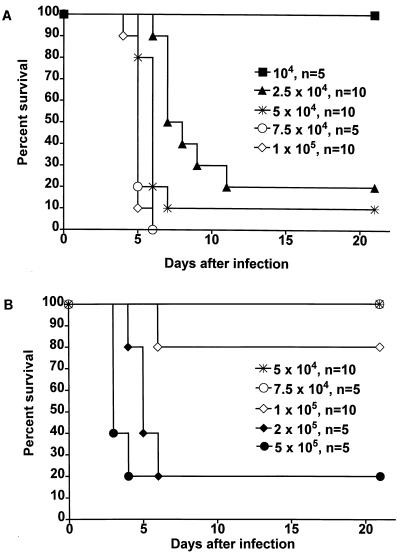
To test whether RV7 vaccination elicits a protective immune response, we inoculated BALB/c mice s.c. in the hind limb with mock vaccination medium or 2 × 105 PFU of RV7 on days 0 and 14 of experiments. On day 28, mice were challenged with increasing doses of sgMCMV and then monitored for mortality (Fig. 1). While 5 × 104 PFU of sgMCMV killed 9 of 10 mock-vaccinated mice (Fig. 1A), 10 of 10 RV7-vaccinated mice survived challenge with this dose of sgMCMV (Fig. 1B). Significant protection was seen against challenge with 105 PFU of sgMCMV (8 of 10 RV7-vaccinated and 0 of 10 mock-vaccinated mice surviving). Increasing the challenge dose above 105 PFU of sgMCMV overcame RV7-induced protection. We noted that there is a very sharp break between doses that are lethal and doses that are nonlethal in both normal and immune mice (Fig. 1). This phenomenon has been previously reported (3) and is thus a characteristic of MCMV infection in BALB/c (as well as 129 [unpublished data]) background mice. We concluded that RV7 vaccination can protect against lethal MCMV infection, confirming previous reports of protection after inoculation with a live attenuated ts MCMV mutant (69). The vaccination schedule and protocol used for these experiments were adopted for subsequent experiments.
FIG. 1.
Protection against lethal MCMV infection by RV7 vaccination. Mice were mock vaccinated (A) or vaccinated with 2 × 105 PFU of RV7 s.c. (B) on days 0 and 14 of the experiment and then challenged with sgMCMV i.p. at the indicated doses on day 28 of the experiment. The indicated number of mice were observed for mortality over the next 21 days. Data were pooled from two experiments, and the percent survival for each challenge dose is graphed versus time. Symbols that match between panel A and panel B correspond to matching challenge doses. Additional data from the experiments are not plotted. RV7-vaccinated mice challenged with 104 PFU of sgMCMV (n = 5) and 2.5 × 104 PFU of sgMCMV (n = 5) all survived.
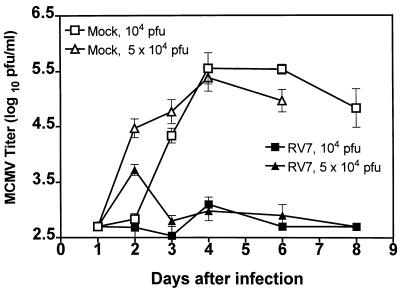
Vaccination with RV7 decreases MCMV titer in the spleen after challenge with sgMCMV.
To determine the effect of RV7 vaccination on MCMV growth in vivo, mice were challenged with sgMCMV (either 104 or 5 × 104 PFU) after RV7 or mock vaccination. Spleen titers were monitored for 8 days after infection. Mock-vaccinated mice showed increasing splenic titers of MCMV between 1 and 4 days of infection, and titers remained relatively constant thereafter (Fig. 2). In contrast, RV7-vaccinated mice showed low levels of MCMV present in the spleen between 2 and 8 days postinfection. RV7-vaccinated mice had 100- to 500-fold less splenic MCMV than mock-vaccinated mice between 4 and 8 days after infection (Fig. 2). This compared favorably with the 18- to >63-fold decreases in spleen titer previously reported after DNA vaccination against MCMV infection (3), the approximately 50-fold reduction in spleen titer induced by CD8 T cells after vaccination with vaccinia virus expressing the pp89 MCMV protein (16), and the approximately 10-fold reduction in spleen titer observed after vaccination with pp89 peptides (63). RV7 vaccination also decreased MCMV titers in the liver (not shown). Note that 10 of 10 RV7 vaccinated mice challenged with 5 × 104 PFU of sgMCMV survived (Fig. 1B); this dose of sgMCMV was lethal for 90% (9 of 10) of mock-vaccinated mice (Fig. 1A). Replication of MCMV in the spleens of RV7-vaccinated mice challenged with 5 × 104 PFU of sgMCMV was minimal, while the same challenge dose resulted in robust splenic titers in mock-vaccinated mice (Fig. 2). This finding demonstrates that RV7 vaccination can control acute infection with a lethal dose of challenge sgMCMV.
FIG. 2.
Effect of RV7 vaccination on MCMV titers in the spleen after challenge with sgMCMV. BALB/c mice were vaccinated with 2 × 105 PFU of RV7 s.c., or were mock vaccinated, on days 0 and 14 of the experiment and then challenged with sgMCMV i.p. at the indicated doses on day 28 of the experiment. At different times after challenge, spleens were harvested and the MCMV titer was determined. When spleen titer was not detected by plaque assay, the titer was arbitrarily fixed at 100 or 500, depending on the limit of plaque assay sensitivity for the given experiment. Mock-vaccinated mice challenged with 5 × 104 PFU of sgMCMV did not survive to day 8. Data were pooled from three independent experiments and represent two to six mice per time point per condition. Data are shown as mean log titer ± SEM.
Because there is an extensive literature that supports the use of spleen titer as a readout for the nature of immune responses to MCMV, we used spleen titer 4 days after infection in further experiments designed to analyze mechanisms of immunity active in RV7-vaccinated mice. The validity of spleen titer as a correlate of protective immunity has been demonstrated in adoptive transfer studies, cytokine depletion studies, T-cell depletion studies, and vaccination studies (3, 16, 21, 33–35, 42, 60, 62, 67). We selected challenge with 104 PFU of sgMCMV for further experiments in BALB/c and 129 strain mice, as this dose is below the lethal dose for mock-vaccinated mice (Fig. 1A) but establishes robust splenic infection (Fig. 2) in this group of animals, allowing for assessment of RV7 vaccine efficacy.
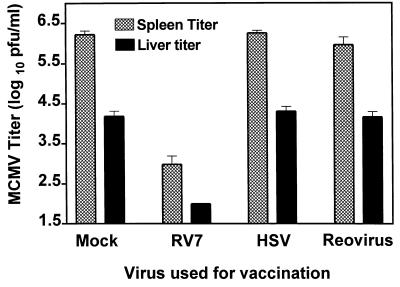
Vaccination with RV7 is antigen specific, requires infectious RV7, and requires lymphocytes.
To address whether the protection seen with RV7 is antigen specific, we vaccinated BALB/c mice with RV7 and two control viruses (HSV and reovirus T3D). All viruses were used at 2 × 105 PFU/dose with the same vaccination schedule. Mice were challenged with 104 PFU of sgMCMV on day 28 of the experiment, and 4 days later spleens and livers were harvested for titration of MCMV (Fig. 3). Mock-vaccinated mice and mice vaccinated with HSV or T3D had approximately 104 PFU of MCMV in the liver and approximately 106 PFU of MCMV in the spleen. In contrast, RV7-vaccinated mice had no detectable virus in liver (detection limit, 500 PFU) and about 500-fold less MCMV in the spleen than mock-, HSV-, or reovirus-vaccinated mice. The failure of vaccination with HSV or T3D to decrease MCMV titers in the spleen or liver demonstrated that RV7 vaccination was antigen specific.
FIG. 3.
RV7 vaccination yields antigen-specific protection. BALB/c mice were vaccinated s.c. with 2 × 105 PFU of RV7, HSV, or reovirus T3D, or were mock vaccinated, on days 0 and 14 of the experiment and then challenged with 104 PFU of sgMCMV i.p. on day 28 of the experiment. Four days later, spleens were harvested and the MCMV titer was determined. When spleen titer was not detected by plaque assay, the titer was arbitrarily fixed at 100, the limit of plaque assay sensitivity for these experiments. Spleen titer data were pooled from two independent experiments and represent 10 mice per condition. Liver titer data were obtained from a single experiment and represent five mice per condition. Data are shown as mean log titer ± SEM.
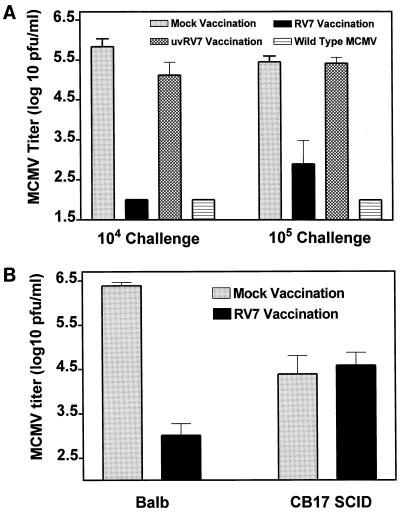
Since tissue culture-passaged RV7 stocks contained both virion antigens and nonstructural antigens from infected cells, we considered the possibility that vaccination with RV7 was due to the presence of viral antigen in RV7 preparations. RV7 was therefore inactivated by UV light and used as a vaccine (Fig. 4A). While both RV7 and MCMV vaccination conferred protection against challenge with sgMCMV, UV-inactivated RV7 was no more effective than mock vaccination at decreasing MCMV titers in the spleen 4 days after challenge infection (Fig. 4A), demonstrating that infectious RV7 is required for effective vaccination.
FIG. 4.
Protection against MCMV infection by RV7 vaccination requires viral replication and lymphocytes. (A) BALB/c mice were inoculated with 2 × 105 PFU of RV7, UV-inactivated RV7, or wt tissue culture-passaged MCMV, or were mock vaccinated, on days 0 and 14 of experiments. On day 28, mice were challenged i.p. with either 104 or 105 PFU of sgMCMV. Four days later, spleens were harvested and the MCMV titer was determined. When spleen titer was not detected by plaque assay, the titer was arbitrarily fixed at 100, the limit of plaque assay sensitivity. Data were pooled from two separate experiments (a total of six mice per condition) and are shown as mean log titer ± SEM. (B) Mice of the indicated strains were vaccinated with 2 × 105 PFU of RV7 s.c., or were mock vaccinated, on days 0 and 14 of the experiment and then challenged with 104 PFU of sgMCMV i.p. on day 28 of the experiment. Four days later, spleens were harvested and the MCMV titer was determined. Data were pooled from two experiments, with six to seven mice per condition.
It was possible that RV7 inoculation protected mice by eliciting innate responses that persisted for the 14 days between the second vaccination with RV7 and the challenge with sgMCMV. To determine if innate immune activation versus lymphocyte-based immunity was important for protection induced by RV7, we vaccinated SCID mice and challenged them with sgMCMV. SCID mice mount potent innate responses to MCMV infection (24, 49, 74). In contrast to control BALB/c mice, SCID mice were not protected by RV7 vaccination as measured by spleen titers 4 days after infection with sgMCMV (Fig. 4B), demonstrating that RV7 vaccination requires functional B and/or T cells and is not mediated by innate responses.
RV7 vaccination is dose dependent and is an effective vaccine by mucosal as well as parenteral routes.
Initial experiments used 2 × 105 PFU of RV7 per vaccination, since infection with a similar dose (1.5 × 105 PFU) of RV7 results in no detectable RV7 replication in organs of BALB mice (11). To determine if even lower doses of RV7 would be effective, we examined the effects of s.c. vaccination with 2 × 103 PFU of RV7 on days 0 and 14. Four days after day 28 challenge with 5 × 104 PFU of sgMCMV, mock-vaccinated mice (n = 4 mice) had spleen titers of 6.6 ± 0.05 (log 10 PFU/spleen ± standard error of the mean [SEM]). Spleen titers after challenge with sgMCMV in mice vaccinated with 2 × 103 PFU of RV7 were 4.0 ± 0.12 (n = 4 mice). Thus, vaccination with 100-fold less RV7 still elicited a significant level of protection.
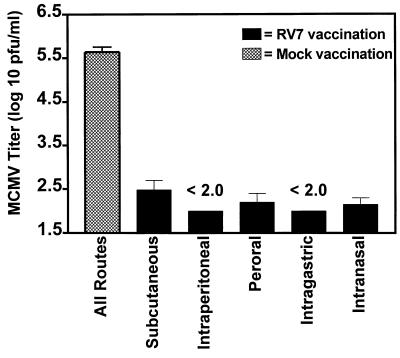
We next examined the effect of route of vaccination on RV7-mediated protection. RV7 was administered, at 2 × 105 PFU/dose, s.c., i.p., intragastrically, perorally, and intranasally. Protection was evident by all of these routes, as shown by decreased MCMV titers 4 days after day 28 challenge with 104 PFU of sgMCMV (Fig. 5). Because of possible microtrauma caused during intragastric intubation which would result in parenteral immunization, the peroral route was used to confirm effective vaccination via the mucosal route. Peroral vaccination was performed by gently placing a drop of RV7-containing medium in the mouth, eliminating the possibility of trauma during vaccination resulting in inadvertent parenteral immunization. The efficacy of RV7 vaccination after intragastric, peroral, and intranasal immunization demonstrates that when a live attenuated MCMV strain is used, mucosal immunization can be effective and that parenteral vaccination is not required for protection against parenteral challenge with MCMV.
FIG. 5.
RV7 vaccination is effective by multiple routes. BALB/c mice were vaccinated with 2 × 105 PFU of RV7, or were mock vaccinated, using the different routes noted on days 0 and 14 of the experiment and then challenged with 104 PFU of sgMCMV i.p. on day 28 of the experiment. For details of vaccination procedures, see Materials and Methods. Four days later, spleens were harvested and the MCMV titer was determined. When spleen titer was not detected by plaque assay, the titer was arbitrarily fixed at 100, the limit of plaque assay sensitivity. Data for mock vaccinations were pooled from four different experiments using s.c., intragastric, and i.p. routes (15 mice in total). Data for RV7 vaccination were pooled from two to three independent experiments and represents 6 to 10 mice per condition. Data are shown as mean log titer ± SEM.
RV7 vaccination is mediated by CD8 T cells.
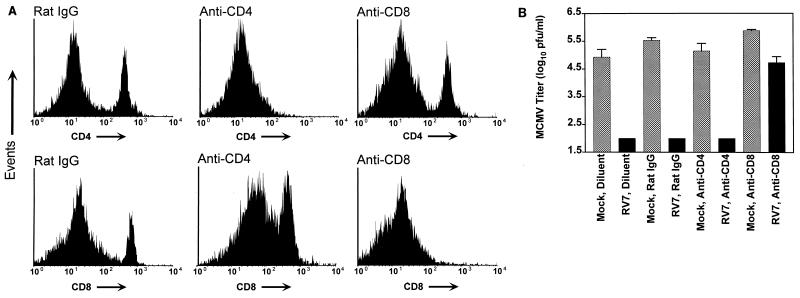
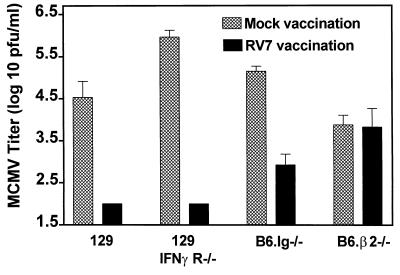
Previous studies have shown that CD8 T cells are primary mediators of protection elicited by infection with wt MCMV (and HCMV [see Discussion]) and that T cells are important for protection elicited by inoculation with a ts mutant of MCMV (69). However, the specific cellular mechanisms responsible for protection by attenuated MCMV vaccination have not previously been defined, and the fact that RV7 fails to grow normally in macrophages, which are professional antigen-presenting cells, raised questions as to the nature of protective immunity elicited by RV7 vaccination. We therefore evaluated whether RV7 vaccination is dependent on CD8 T cells. Mice were vaccinated with RV7 or mock vaccinated and then depleted of either CD4 or CD8 T cells by the administration of monoclonal anti-CD4 or anti-CD8 antibodies both before and after i.p. challenge infection on day 28 with 104 PFU of sgMCMV (see Materials and Methods). Diluent and rat IgG served as control treatments. We evaluated both viral titer and the efficacy of T-cell depletion in spleens 4 days after challenge. The efficacy of antibody depletion of T-cell subsets was demonstrated by FACS analysis (Fig. 6A). In mock-vaccinated mice, depletion of CD4 and CD8 T cells was >99%. As expected, since T-cell immunity is not expected within 4 days of primary infection, CD4 or CD8 depletion in mock-vaccinated mice had no effect on MCMV titers 4 days after challenge. While depletion of CD4 T cells from RV7-vaccinated mice had no effect on MCMV titer in the spleen, depletion of CD8 T cells essentially abrogated the protective effect of vaccination (Fig. 6B). We conclude that CD8 T cells are critical for the protection against acute MCMV infection conferred by RV7 vaccination. This result was confirmed by the demonstration that RV7 vaccination fails to efficiently protect CD8-deficient B6.β2−/− mice (Fig. 7). The failure to effectively vaccinate B6.β2−/− mice with RV7 was not due to an inability of mice on the B6 background to respond to RV7 vaccination, since B6.Ig−/− mice are effectively vaccinated by RV7 (see below).
FIG. 6.
Effect of depletion of CD4 and CD8 T cells on RV7 vaccination. BALB/c mice were vaccinated with 2 × 105 PFU of RV7 s.c., or were mock vaccinated, on days 0 and 14 of the experiment and then challenged with 104 PFU of sgMCMV i.p. on day 28 of two independent experiments. To deplete CD4 and CD8 T cells, rat monoclonal antibodies were passively administered to mice before and after challenge on day 28, using the doses and schedules specified in Materials and Methods. Purified rat IgG and the diluent used for preparing antibodies for injection were used as controls. Four days after challenge, spleens were harvested; one half was taken for determination of MCMV titer, and one half was used to determine the efficacy of CD4 and CD8 T-cell depletion by FACS analysis. (A) Single-color FACS histograms showing the proportions of CD4 and CD8 T cells in spleens from MCMV-infected mice after treatment with the indicated antibodies. Spleen cells from diluent-treated mice and rat IgG-treated mice were similar, and thus only FACS profiles from rat IgG-treated mice are shown. Two experiments were performed with different depletion regimens, and the FACS data shown are from the regimen using higher doses of anti-CD4 and anti-CD8 antibodies (see Materials and Methods). (B) MCMV titer in spleens of mice from the indicated groups. For CD8 depletion, and CD4 depletion in mock-vaccinated animals, data from two experiments using the different depletion regimens were pooled (n = 7 mice per condition). CD4 depletion in RV7-vaccinated mice using the lower-dose protocol resulted in only 57% depletion, so data are presented only from the experimental protocol using higher doses of anti-CD4 antibodies, which resulted in >99% depletion (n = 3 mice). Using the lower-dose protocol, where CD4 depletion was only 57%, we also failed to detect infectious MCMV in four of four RV7-vaccinated mice (not shown). When spleen titer was not detected by plaque assay, the titer was arbitrarily fixed at 100, the limit of plaque assay sensitivity. Data are shown as mean log titer ± SEM.
FIG. 7.
Efficiency of RV7 vaccination in mice with various immunodeficiencies. Mice of the indicated strains were vaccinated with 2 × 105 PFU of RV7 s.c., or were mock vaccinated, on days 0 and 14 of the experiment and then challenged with sgMCMV i.p. on day 28 of the experiment. Four days later, spleens were harvested and the MCMV titer was determined. Data were pooled from the following numbers of experiments and numbers of experimental animals: (i) 129, three experiments, 9 to 10 mice per condition, 104 PFU of sgMCMV challenge; (ii) 129 IFNγR−/−, three experiments, 8 to 9 mice per condition, 104 PFU of sgMCMV challenge; (iii) B6.Ig−/−, one experiment, 4 mice per condition, 106 PFU of sgMCMV challenge (similar results were obtained in two additional experiments using a challenge dose of either 5 × 104 PFU [n = 4 mice) or 2 × 105 PFU [n = 4 mice] of sgMCMV); (iv) B6.β2−/−, two experiments, 8 to 9 mice per condition, 106 PFU of sgMCMV challenge (similar results were obtained in a third experiment with a challenge dose of 2 × 105 PFU of sgMCMV). When spleen titer was not detected by plaque assay, the titer was arbitrarily fixed at 100, the limit of plaque assay sensitivity. Data are shown as mean log titer ± SEM.
Neither B cells nor signaling through the IFN-γ receptor is required for effective RV7 vaccination.
Antibodies can play a role in protection against acute and reactivated MCMV infection (21, 33, 36). To determine if B cells and antibody are essential for vaccination we vaccinated B6.Ig−/− mice, which are deficient in surface IgG-bearing B cells and circulating immunoglobulin due to a null mutation in the transmembrane exon of IgM (38). We found that B6.Ig−/− mice responded well to RV7 vaccination (Fig. 7), indicating that B cells are not required for effective vaccination. IFN-γ plays an important role in innate resistance to MCMV and may enhance CD8 T cell killing of MCMV infected targets (see Discussion). In addition, administration of anti-IFN-γ increases MCMV titer in recipients of immune CD8 T cells (25). To test the requirement for IFN-γ signaling in RV7 vaccination, we used IFN-γ receptor-deficient (IFNγR−/−) mice (29) and found that RV7 vaccination is effective (Fig. 7), thus demonstrating that the IFN-γ receptor is not required for effective vaccination.
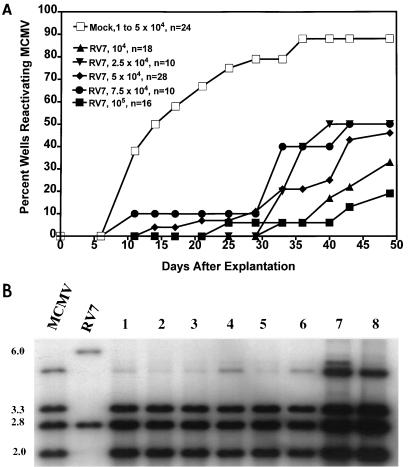
RV7 vaccination reduces reactivation of latent MCMV from splenic explants.
MCMV establishes latent infection in multiple organs and reactivates efficiently from splenic explants (37, 44, 56). To assess the effect of RV7 vaccination on the establishment of MCMV latency, we determined the efficiency and kinetics of reactivation from splenic explants from vaccinated and control animals (Fig. 8A). Mice were vaccinated with RV7 or mock vaccinated on days 0 and 14 of experiments and challenged with between 104 and 105 PFU of sgMCMV on day 28. Sixty days later, spleens were removed and assessed for persistent virus by coculturing one-fourth of the spleen with MEFs after freeze-thawing and sonicating. This assay destroys latent virus and sensitively detects persistent MCMV in the spleen (56). No persistent infection was found in spleens taken 60 days after challenge. To assess the kinetics of reactivation of latent MCMV, spleen explants were prepared and monitored for 47 to 49 days. Across multiple experiments, spleen explants from mock-vaccinated mice reactivated MCMV between 10 and 35 days postexplantation, with the majority of reactivation events occurring by day 20 (Fig. 8A). In contrast, spleens from RV7-vaccinated mice challenged with 104 PFU of sgMCMV showed significant delay in reactivation and also a decrease in the total number of spleen explant wells showing reactivation. We considered the possibility that increasing the dose of sgMCMV used to infect RV7-vaccinated mice might overcome the effect of RV7 vaccination on reactivation of latent MCMV from spleen explants. This was important since it was possible that effects on reactivation from latency would be seen only when immune animals were challenged with sublethal doses of MCMV. We therefore infected RV7-vaccinated mice with up to 105 PFU of sgMCMV (Fig. 8A). Even at these higher challenge doses, reactivation from spleen explants was delayed and fewer wells reactivated MCMV.
FIG. 8.
Effect of RV7 vaccination on reactivation of MCMV from spleen explants. BALB/c mice were vaccinated s.c. with 2 × 105 PFU of RV7, or were mock vaccinated, on days 0 and 14 of the experiment and then challenged i.p. with the indicated doses of sgMCMV on day 28. On day 88 of the experiment, one-fourth of the spleen was sonicated and cocultured with MEFs to detect persistent infection. No cultures scored positive for persistent infection in these experiments, demonstrating that spleens were latently infected. (A) One half of the spleen was homogenized and explanted into two tissue culture wells. Every 3 to 4 days, samples of the supernatant from spleen explant wells were harvested and cultured with MEFs to detect infectious virus. Data were pooled from three experiments and are presented as the percentage of wells reactivating versus the days of explant culture. The number of wells per condition (two wells per mouse evaluated) are noted. (B) To identify the virus reactivating in the spleen explants shown in panel A, MCMV was grown from individual reactivated explant wells. Viral DNA was prepared, digested with HindIII and BglII, and analyzed by Southern blotting with 32P-labeled HindIII J fragment of the MCMV genome. The patterns expected from wild-type MCMV and mutant RV7 are demonstrated by the controls on the left side; sizes in kilobases are indicated. No band at 6.0 kb (specific to RV7) was detected in MCMV from reactivating wells even on prolonged exposures. We show here data from eight isolates. An additional seven isolates were analyzed, with comparable results.
We further assessed whether RV7 vaccination leads to systemic latency with RV7. When RV7 was administered s.c., as in our usual vaccination protocol, we detected no reactivation from splenic explants (0 of 10 mice) and no RV7 DNA in the spleen (0 of 10 mice), using a nested PCR assay that detects 1 to 10 copies in 172,000 cell equivalents of DNA (data not shown and reference 56). However, when we administered RV7 at a dose of 106 PFU i.p., RV7 genome was detected by nested PCR in the spleens of seven of eight mice harvested 88 days after RV7 administration (data not shown). Although unlikely, given the s.c. route of RV7 administration in the vaccination protocol, we considered the possibility that reactivation that we observed in vaccinated mice (Fig. 8A) was reactivation of RV7. Multiple isolates of MCMV that reactivated from splenic explants (Fig. 8A) were therefore examined by Southern blot analysis for the presence of RV7 genome (Fig. 8B). None of 15 independent isolates (8 are represented in Fig. 8B) of MCMV that reactivated from splenic explants showed evidence (even on prolonged exposures) of bands characteristic of RV7.
DISCUSSION
HCMV infection can have devastating consequences for newborns and AIDS patients. However, an effective vaccine is not yet available. Cost-benefit analysis suggests that a vaccine could have a significant positive effect on reducing human disease (19, 31, 57). An important step in understanding vaccination against CMV is defining mechanisms by which different vaccine approaches elicit protection. MCMV is particularly well suited to this type of analysis due to the availability of an extensive literature on the natural history of the infection, the fact that several different vaccine strategies have been studied, and the availability of genetic approaches to defining mechanisms of protection. This led us to analyze the effect of vaccination with a stably attenuated MCMV mutant on MCMV infection in normal and genetically altered mice with specific immunodeficiencies. Analyzing the effectiveness of live attenuated vaccination is important since other approaches (DNA vaccination, CMV proteins expressed in other virus vectors, subunit vaccination, and peptide vaccination) are being analyzed as approaches to vaccination against MCMV (3, 8, 16, 63), but the only approach shown to date to have value in humans is infection with live or live attenuated HCMV (1, 22, 51–54, 64).
Most previously published work with “attenuated” MCMV vaccination used tissue culture-passaged virus that, while less virulent than salivary gland-derived virus, grows in the salivary gland and reverts to virulence and can thus not be properly considered an attenuated mutant (20, 26, 45, 46, 50). RV7 cannot revert to virulence due to the presence of a large deletion encompassing at least four open reading frames and is more than 100,000-fold less virulent than even tissue culture-passaged wt MCMV in SCID mice (reference 11 and unpublished observations).
In this report, we make the following important points. First, vaccination with a stable avirulent MCMV mutant (RV7) effectively immunizes against challenge with virulent wt MCMV. Effective vaccination requires live RV7, is antigen specific, and requires lymphocytes. Second, vaccination is effective by several mucosal routes. This is true even though our challenge was direct i.p. infection with virulent MCMV. This result demonstrates that mucosal vaccination can lead to effective systemic resistance to parenteral MCMV infection. Third, vaccination required CD8 T cells, not CD4 T cells or antibody. Fourth, vaccination did not require signaling through the IFN-γ receptor. Last, vaccination decreased, but did not eliminate, establishment of and/or reactivation from MCMV latency as measured in a spleen explant reactivation assay. Although this assay system does not distinguish between decreased levels of latent genome and decreased ability to reactivate, either of these results would be a beneficial result of vaccination with a live attenuated MCMV strain.
Live attenuated vaccination against CMV.
More than one strain of HCMV can be isolated from apparently immunocompetent individuals (12, 27, 28, 43), and multiple MCMV isolates can be isolated from an individual wild mouse (6). These data suggest that prior infection fails to prevent reinfection with HCMV and MCMV, suggesting that even immunity established by natural HCMV infection is incompletely protective. This argues that a CMV vaccine must approach or exceed the efficacy of natural CMV challenge in order to be effective at preventing infection. However, multiple studies show that immunity can protect against disease caused by HCMV. Seropositive mothers are less likely than nonimmune mothers to be infected with HCMV from their children (1), and seropositive persons are resistant to HCMV-induced disease when challenged with a low-passage isolate of HCMV (54). In patients undergoing renal transplantation, preexisting immunity protects against HCMV disease and primary infections in seronegative recipients are more severe than infections in seropositive recipients (64). These studies argue that an effective immune response at least limits disease due to reinfection. This is confirmed by the demonstration that vaccination with live HCMV can lessen disease severity in renal transplant recipients and healthy volunteers (51–53), although the level of protection afforded by attenuated HCMV vaccination is likely less than the protection afforded by wt infection (1). These data suggested that analysis of the immune response to a live attenuated MCMV mutant would provide a viable model for understanding how to optimize vaccination against CMV. Use of specific mutants of MCMV may allow definition of approaches that optimize vaccine efficacy while maintaining attenuation.
In studies presented here, we show that vaccination with a live attenuated MCMV mutant can protect against parenteral challenge with virulent MCMV. The facts that we observed protection against lethal infection (Fig. 1) and that we controlled visceral replication even after challenge with lethal doses of virulent MCMV (Fig. 2) argue that we induced an effective immune response. These data show that live attenuated vaccination is likely more effective and less variable than vaccination with DNA encoding a single MCMV protein (3), although optimization of DNA vaccination protocols may result in increased efficacy approaching that of vaccination with a live attenuated virus.
Another striking advantage for the live attenuated approach that we have undertaken is the efficacy of vaccination via mucosal surfaces in the absence of adjuvant (Fig. 5). RV7 vaccination was effective by intranasal, peroral, and intragastric routes. This is intriguing since the efficacy of these vaccine routes was apparent even against parenteral challenge with a high dose of virulent MCMV. It is possible that mucosal challenge will elicit both a protective systemic and a protective mucosal response. In this case, the host could be protected both at the mucosal surface and systemically by the same vaccination. The efficacy of mucosal vaccination against mucosal challenge needs to be explored further. In addition, the efficacy of intragastric vaccination strongly suggests that the intestine is a natural port of entry for CMV. A similar phenomenon has recently been noted for HSV, demonstrating the need for more analysis of interactions between intestinal mucosa and herpesviruses and demonstrating that enveloped herpesviruses can infect the intestinal tract despite the harsh local conditions present in the gastrointestinal tract (23).
One interesting question not addressed in our studies is the effect of mucosal vaccination with attenuated MCMV on replication in the salivary gland. We did not assess this in our studies because we focused on events in vaccinated mice that occur before death due to MCMV infection in unvaccinated mice (generally days 4 to 10 after infection with lethal doses of MCMV [Fig. 1]). This focus prevented us from assessing replication in salivary gland which occurs 2 to 6 weeks after infection (3, 34, 35, 42, 62). This will be an interesting question for future studies since clearance of the salivary gland involves CD4 T cells and IFN-γ (34, 42), neither of which was required for control of MCMV replication in the spleen early after infection in the studies presented here.
Role of CD8 T cells in protection and vaccination against CMV disease.
The severity of HCMV disease correlates inversely with the strength of cytotoxic T-cell responses to HCMV (58), and a phase 1 trial of adoptively transferred CD8 T cells showed protection against HCMV viremia and HCMV-associated disease (73). In addition, passively transferred antibody can limit HCMV disease (75). Similarly, the preeminence of CD8 responses in protecting against acute infection has been well documented for MCMV (33, 60, 62). CD8 T cells specific for proteins encoded in the MIE locus are protective (25, 33, 40, 72). Vaccination with vaccinia virus expressing the MIE protein is protective via generation of CD8 T cells, and expression of a single epitope within the pp89 MIE protein IE1 is protective in the H-2d haplotype (16–18, 33). In addition, DNA immunization with vector expressing IE1 protein is protective (3). The importance of CD8 T cells for both HCMV and MCMV immunity is underlined by the fact that both viruses downregulate major histocompatibility complex class I molecules on the surface of infected cells, thus decreasing CD8 T-cell recognition (2, 10, 14, 15, 32, 68, 76). While CD8 T cells are protective against MCMV, CD4 T cells can play a protective role in the absence of CD8 T cells (35), and CD4 T cells are important for clearance of MCMV from the salivary gland (34, 35, 42). These background data led us to assess whether live attenuated vaccination could effectively elicit a protective CD8 T-cell response and whether CD4 T cells or antibody were required for vaccination. The issue of which T cells are responsible for vaccination after exposure to attenuated MCMV has not previously been evaluated.
We show here that RV7 vaccination requires CD8 T cells (Fig. 6 and 7). This was shown both by depleting CD8 T cells prior to challenge and by analyzing vaccine effectiveness in CD8 T-cell-deficient β2−/− mice. Both experimental approaches strongly suggest that the great majority of the protective effect of RV7 vaccination is due to CD8 T cells. Thus, depletion of CD8 T cells from RV7-vaccinated animals led to MCMV titers in the spleen nearly equivalent to spleen titers seen in unvaccinated animals (Fig. 6), and β2−/− mice (under these experimental conditions) did not show partial protection (Fig. 7). We do not believe that we have eliminated a role for CD8-independent RV7-mediated immune responses. It has been demonstrated that mechanisms for CMV clearance may depend on the organ evaluated. For example, CD4 T cells have an important role in the salivary gland, and liver and spleen differ in the mechanisms by which natural killer cells clear MCMV (34, 67). Thus, it is possible that RV7 vaccination elicits CD8-independent protective responses that might be active at sites other than the spleen, which was the primary focus of studies presented here.
Mechanism of protection elicited by RV7 vaccination.
In addition to effects of CD4 and CD8 T cells, passive transfer of anti-MCMV antibody can protect against MCMV challenge (21, 33). Although B cells and antibody are not essential for clearing acute primary infection, their role in limiting dissemination of recurrent virus argues that antibody might be important in protection against secondary infection with MCMV (36). We found that B cells and antibody are not required for protection by RV7 vaccination. Since antibody does not influence primary infection (36) or secondary infection (this study), our data support the interpretation that a key role of antibody is in limiting dissemination after reactivation from latency (36).
IFN-γ plays an important role in control of acute MCMV infection. In a B- and T-cell-independent manner, IFN-γ controls MCMV replication in SCID mice (24), an effect likely explained by the important role that IFN-γ plays in NK cell-dependent clearance of CMV infection (49). IFN-γ may also be important for CD8 T-cell function since IFN-γ can overcome MCMV-mediated inhibition of CD8 T-cell recognition of MCMV-infected targets, and anti-IFN-γ can inhibit the effectiveness of adoptively transferred CD8 T cells in vivo (25). In addition, IFN-γ and CD4 T cells are critical for clearance of MCMV from the salivary gland (34, 42). For these reasons, we hypothesized that IFN-γ might be required for either the induction or the effector phase of RV7 vaccine responses. We noted that the MCMV titers in the spleen were more than 10-fold higher in mock-vaccinated IFNγR−/− mice than mock-vaccinated congenic control 129 mice. This finding is consistent with previous data on the importance of IFN-γ during primary infection (24, 49, 67). However, IFNγR−/− mice on the 129 background were effectively vaccinated by RV7. This finding shows that IFN-γ is not required for induction of protective secondary responses to MCMV, which leaves open the question of the specific aspects of CD8 T-cell function that are required for protection. Potential mechanisms not addressed by these studies are tumor necrosis factor secretion, Fas-mediated cell killing, and perforin-mediated lysis and/or apoptosis.
RV7 vaccination and latency.
It has been shown that in the HSV system, vaccination with replication-defective HSV mutants elicits a response that inhibits establishment of latency, as measured by reactivation from trigeminal ganglia and decreases in the number of neurons expressing the latency-associated transcript (47, 48). This result encouraged us to evaluate whether reactivation from splenic explants was altered by RV7 vaccination. Spleen explant reactivation of MCMV has been used in a number of studies to evaluate the establishment of latency by MCMV (37, 44, 56). We found a consistent delay in the time to reactivation (about 20 days) and a decrease in the overall number of reactivating wells when spleens were taken from mice vaccinated with RV7 prior to challenge with MCMV (Fig. 8A). This finding demonstrates that RV7 vaccination alters the capacity of MCMV to reactivate from spleens in an in vitro assay, either by inhibition of the establishment of MCMV latency or by inhibition of reactivation. Inhibition of the establishment of latency could result in a decrease in the total number of cells carrying latent virus or in fewer copies of latent genome per cell. It was previously demonstrated that the copy number of latent viral genome in tissue is a major determinant in the risk of MCMV recurrence in vivo (59). Inhibition of reactivation in the in vitro assay could be mediated by RV7-induced immune effector cells, or possibly by changes in the cytokine secretion by cells present in the spleens of RV7-vaccinated animals. These possibilities will require further investigation.
RV7 did not reactivate from spleens taken from RV7-vaccinated mice or from spleens of RV7-vaccinated mice infected with wt MCMV after vaccination (Fig. 8B). This finding suggests that subcutaneously administered RV7 does not efficiently establish latency or reactivate from latency in the spleen. This is consistent with a failure of RV7 to spread efficiently in the host (11) but does not demonstrate that RV7 is incapable of reactivation. In fact, when we administered RV7 i.p. at a high dose, we did detect RV7 DNA in spleens 88 days after infection, suggesting that the lack of reactivation of RV7 from the spleen after s.c. vaccination is due to failure to spread to the spleen rather than to an inability to establish latency. However, the efficiency with which RV7 vaccination induced protective immunity combined with the inability of RV7 to establish systemic latency after s.c. inoculation demonstrates that efficient establishment of systemic latency can be separated from vaccine efficacy. This suggests the possibility that attenuated vaccines can be designed and administered such that establishment of systemic latency is minimized while immunogenicity is maintained. Definition of the MCMV gene program operating during latency might provide avenues for engineering viruses that cannot establish or reactivate from latency but still maintain immunogenicity.
ACKNOWLEDGMENTS
H.W.V. was supported by grant AI39616 from the National Institute of Allergy and Infectious Diseases. Additional support was provided by a grant to H.W.V. from the Mallinckrodt Foundation and the Council for Tobacco Research and by American Cancer Society Junior Faculty Research Award JFRA-525. M.R.M. was supported by a Connaught Laboratories Fellowship for Pediatricians in Infectious Disease and grant K08 AI01418 from the National Institute of Allergy and Infectious Diseases. A.E.C. and R.M.S. were supported by grant CA41451 from the National Cancer Institute.
REFERENCES
- 1.Adler S P, Starr S E, Plotkin S A, Hempfling S H, Buis J, Manning M L, Best A M. Immunity induced by primary human cytomegalovirus infection protects against secondary infection among women of childbearing age. J Infect Dis. 1995;171:26–32. doi: 10.1093/infdis/171.1.26. [DOI] [PubMed] [Google Scholar]
- 2.Ahn K, Angulo A, Ghazal P, Peterson P A, Yang Y, Fruh K. Human cytomegalovirus inhibits antigen presentation by a sequential multistep process. Proc Natl Acad Sci USA. 1996;93:10990–10995. doi: 10.1073/pnas.93.20.10990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armas J C G, Morello C S, Cranmer L D, Spector D H. DNA immunization confers protection against murine cytomegalovirus infection. J Virol. 1996;70:7921–7928. doi: 10.1128/jvi.70.11.7921-7928.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barkon M L, Haller B L, Virgin H W. Circulating immunoglobulin G can play a critical role in clearance of intestinal reovirus infection. J Virol. 1996;70:1109–1116. doi: 10.1128/jvi.70.2.1109-1116.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bia F J, Miller S A, Lucia H L, Griffith B P, Tarsio M, Hsiung G D. Vaccination against transplacental cytomegalovirus transmission: vaccine reactivation and efficacy in guinea pigs. J Infect Dis. 1984;149:355–362. doi: 10.1093/infdis/149.3.355. [DOI] [PubMed] [Google Scholar]
- 6.Booth T W, Scalzo A A, Carello C, Lyons P A, Farrell H E, Singleton G R, Shellam G R. Molecular and biological characterization of new strains of murine cytomegalovirus isolated from wild mice. Arch Virol. 1993;132:209–220. doi: 10.1007/BF01309855. [DOI] [PubMed] [Google Scholar]
- 7.Bosma M J. The scid mutation: occurrence and effect. Curr Top Microbiol Immunol. 1989;152:3–9. doi: 10.1007/978-3-642-74974-2_1. [DOI] [PubMed] [Google Scholar]
- 8.Britt W, Fay J, Seals J, Kensil C. Formulation of an immunogenic human cytomegalovirus vaccine: responses in mice. J Infect Dis. 1995;171:18–25. doi: 10.1093/infdis/171.1.18. [DOI] [PubMed] [Google Scholar]
- 9.Britt W J, Alford C A. Cytomegalovirus. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. Philadelphia, Pa: Lippincott-Raven; 1996. pp. 2493–2523. [Google Scholar]
- 10.Campbell A E, Slater J S, Cavanaugh V J, Stenberg R M. An early event in murine cytomegalovirus replication inhibits presentation of cellular antigens to cytotoxic T lymphocytes. J Virol. 1992;66:3011–3017. doi: 10.1128/jvi.66.5.3011-3017.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cavanaugh V J, Stenberg R M, Staley T L, Virgin H W, MacDonald M R, Paetzold S, Farrell H E, Rawlinson W D, Campbell A E. Murine cytomegalovirus with a deletion spanning HindIII-J and -I displays altered cell and tissue tropism. J Virol. 1996;70:1365–1374. doi: 10.1128/jvi.70.3.1365-1374.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chandler S H, Handsfield H H, McDougall J K. Isolation of multiple strains of cytomegalovirus from women attending a clinic for sexually transmitted diseases. J Infect Dis. 1987;155:655–660. doi: 10.1093/infdis/155.4.655. [DOI] [PubMed] [Google Scholar]
- 13.Cranmer L D, Clark C L, Morello C S, Farrell H E, Rawlinson W D, Spector D H. Identification, analysis, and evolutionary relationships of the putative murine cytomegalovirus homologs of the human cytomegalovirus UL82 (pp71) and UL83 (pp65) matrix phosphoproteins. J Virol. 1996;70:7929–7939. doi: 10.1128/jvi.70.11.7929-7939.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Del Val M, Hengel H, Hacker H, Hartlaub U, Ruppert T, Lucin P, Koszinowski U H. Cytomegalovirus prevents antigen presentation by blocking the transport of peptide-loaded major histocompatibility complex class I molecules into the medial-Golgi compartment. J Exp Med. 1992;176:729–738. doi: 10.1084/jem.176.3.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DelVal M, Munch K, Reddehase M J, Koszinowski U H. Presentation of CMV immediate-early antigen to cytolytic T lymphocytes is selectively prevented by viral genes expressed in the early phase. Cell. 1989;58:305–315. doi: 10.1016/0092-8674(89)90845-3. [DOI] [PubMed] [Google Scholar]
- 16.DelVal M, Schlicht H-J, Volkmer H, Messerle M, Reddehase M J, Koszinowski U H. Protection against lethal cytomegalovirus infection by a recombinant vaccine containing a single nonomeric T-cell epitope. J Virol. 1991;65:3641–3646. doi: 10.1128/jvi.65.7.3641-3646.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DelVal M, Schlicht H J, Ruppert T, Reddehase M J, Koszinowski U H. Efficient processing of an antigenic sequence for presentation by MHC class I molecules depends on its neighboring residues in the protein. Cell. 1991;66:1145–1153. doi: 10.1016/0092-8674(91)90037-y. [DOI] [PubMed] [Google Scholar]
- 18.DelVal M, Volkmer H, Rothbard J B, Jonjic S, Messerle M, Schickedanz J, Reddehase M J, Koszinowski U H. Molecular basis for cytolytic T-lymphocyte recognition of the murine cytomegalovirus immediate-early protein pp89. J Virol. 1988;62:3965–3972. doi: 10.1128/jvi.62.11.3965-3972.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dobbins J G, Stewart J A, Demmler G J. Surveillance of congenital cytomegalovirus disease, 1990–1991. Morbid Mortal Weekly Rep. 1992;41:35–44. [PubMed] [Google Scholar]
- 20.Eizuru Y, Minamishima Y. Co-variation of pathogenicity and antigenicity in murine cytomegalovirus. Microbiol Immunol. 1979;23:559–564. doi: 10.1111/j.1348-0421.1979.tb00496.x. [DOI] [PubMed] [Google Scholar]
- 21.Farrell H E, Shellam G R. Protection against murine cytomegalovirus infection by passive transfer of neutralizing and non-neutralizing monoclonal antibodies. J Gen Virol. 1991;72:149–156. doi: 10.1099/0022-1317-72-1-149. [DOI] [PubMed] [Google Scholar]
- 22.Fleisher G R, Starr S E, Friedman H M, Plotkin S A. Vaccination of pediatric nurses with live attenuated cytomegalovirus. Am J Dis Child. 1982;136:294–296. doi: 10.1001/archpedi.1982.03970400012003. [DOI] [PubMed] [Google Scholar]
- 23.Gesser R M, Koo S C. Oral inoculation with herpes simplex virus type 1 infects enteric neurons and mucosal nerve fibers within the gastrointestinal tract in mice. J Virol. 1996;70:4097–4102. doi: 10.1128/jvi.70.6.4097-4102.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heise M T, Virgin H W. The T cell independent role of gamma interferon and tumor necrosis factor alpha in macrophage activation during murine cytomegalovirus and herpes simplex virus infection. J Virol. 1995;69:904–909. doi: 10.1128/jvi.69.2.904-909.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hengel H, Lucin P, Jonjic S, Ruppert T, Koszinowski U H. Restoration of cytomegalovirus antigen presentation by gamma interferon combats viral escape. J Virol. 1994;68:289–297. doi: 10.1128/jvi.68.1.289-297.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Howard R J, Balfour H H J. Prevention of morbidity and mortality of wild murine cytomegalovirus by vaccination with attenuated cytomegalovirus. Proc Soc Exp Biol Med. 1977;156:365–368. doi: 10.3181/00379727-156-39937. [DOI] [PubMed] [Google Scholar]
- 27.Huang E-S, Alford C A, Reynolds D W, Stagno S, Pass R F. Molecular epidemiology of cytomegalovirus infections in women and their infants. N Engl J Med. 1980;303:958–962. doi: 10.1056/NEJM198010233031702. [DOI] [PubMed] [Google Scholar]
- 28.Huang E-S, Huong S-M, Tegtemeier G E, Alford C. Cytomegalovirus: genetic variation of viral genomes. Ann N Y Acad Sci. 1980;354:332–346. doi: 10.1111/j.1749-6632.1980.tb27976.x. [DOI] [PubMed] [Google Scholar]
- 29.Huang S, Hendriks W, Althage A, Hemmi S, Bluethmann H, Kamijo R, Vilcek J, Zinkernagel R M, Aguet M. Immune response in mice that lack the interferon-gamma receptor. Science. 1993;259:1742–1745. doi: 10.1126/science.8456301. [DOI] [PubMed] [Google Scholar]
- 30.Ibusuki K, Kumura K, Minamishima Y. Pathogenicity of murine cytomegalovirus for newborn mice: analysis with the attenuated mutants. Arch Virol. 1993;131:127–139. doi: 10.1007/BF01379085. [DOI] [PubMed] [Google Scholar]
- 31.Istas A S, Demmler G J, Dobbins J G, Stewart J A National Congenital Cytomegalovirus Disease Registry Collaborating Group. Surveillance for congenital cytomegalovirus disease: a report from the national congenital cytomegalovirus disease registry. Clin Infect Dis. 1995;20:665–670. doi: 10.1093/clinids/20.3.665. [DOI] [PubMed] [Google Scholar]
- 32.Jones T R, Hanson L K, Sun L, Slater J S, Stenberg R M, Campbell A E. Multiple independent loci within the human cytomegalovirus unique short region down-regulate expression of major histocompatibility complex class I heavy chains. J Virol. 1995;69:4830–4841. doi: 10.1128/jvi.69.8.4830-4841.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jonjic S, DelVal M, Keil G M, Reddehase M J, Koszinowski U H. A nonstructural viral protein expressed by a recombinant vaccinia virus protects against lethal cytomegalovirus infection. J Virol. 1988;62:1653–1658. doi: 10.1128/jvi.62.5.1653-1658.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jonjic S, Mutter W, Weiland F, Reddehase M J, Koszinowski U H. Site-restricted persistent cytomegalovirus infection after selective long-term depletion of CD4+ T lymphocytes. J Exp Med. 1989;169:1199–1212. doi: 10.1084/jem.169.4.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jonjic S, Pavic I, Lucin P, Rukavina D, Koszinowski U H. Efficacious control of cytomegalovirus infection after long-term depletion of CD8+ T lymphocytes. J Virol. 1990;64:5457–5464. doi: 10.1128/jvi.64.11.5457-5464.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jonjic S, Pavic I, Polic B, Crnkovic I, Lucin P, Koszinowski U H. Antibodies are not essential for the resolution of primary cytomegalovirus infection but limit dissemination of recurrent virus. J Exp Med. 1994;179:1713–1717. doi: 10.1084/jem.179.5.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jordan M C, Mar V L. Spontaneous activation of latent cytomegalovirus from murine spleen explants: role of lymphocytes and macrophages in release and replication of virus. J Clin Invest. 1982;70:762–768. doi: 10.1172/JCI110672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kitamura D, Roes J, Kuhn R, Rajewsky K. A B cell-deficient mouse by targeted disruption of the membrane exon of the immunoglobulin mu chain gene. Nature. 1991;350:423–426. doi: 10.1038/350423a0. [DOI] [PubMed] [Google Scholar]
- 39.Koller B H, Marrack P, Kappler J W, Smithies O. Normal development of mice deficient in beta 2M, MHC class I proteins, and CD8+ T cells. Science. 1990;248:1227–1230. doi: 10.1126/science.2112266. [DOI] [PubMed] [Google Scholar]
- 40.Koszinowski U H, Keil G M, Schwarz H, Schickedanz J, Reddehase M J. A nonstructural polypeptide encoded by immediate-early transcription unit 1 of murine cytomegalovirus is recognized by cytolytic T lymphocytes. J Exp Med. 1987;166:289–294. doi: 10.1084/jem.166.1.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kumura K, Ibusuki K, Minamishima Y. Independent existence of mutations responsible for temperature sensitivity and attenuation in a mutant of murine cytomegalovirus. Virology. 1990;175:572–574. doi: 10.1016/0042-6822(90)90443-u. [DOI] [PubMed] [Google Scholar]
- 42.Lucin P, Pavic I, Polic B, Jonjic S, Koszinowski U H. Gamma interferon-dependent clearance of cytomegalovirus infection in salivary glands. J Virol. 1992;66:1977–1984. doi: 10.1128/jvi.66.4.1977-1984.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McFarlane E S, Koment R W. Use of restriction endonuclease digestion to analyze strains of human cytomegalovirus isolated concurrently from an immunocompetent heterosexual man. J Infect Dis. 1986;154:167–168. doi: 10.1093/infdis/154.1.167. [DOI] [PubMed] [Google Scholar]
- 44.Mercer J A, Wiley C A, Spector D H. Pathogenesis of murine cytomegalovirus infection: identification of infected cells in the spleen during acute and latent infections. J Virol. 1988;62:987–997. doi: 10.1128/jvi.62.3.987-997.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Minamishima Y. Immunoprophylaxis of experimental cytomegalovirus infection. Ann Microbiol (Paris) 1977;128:399–407. [PubMed] [Google Scholar]
- 46.Minamishima Y, Eizuru Y, Yoshida A, Fukunishi R. Murine model for immunoprophylaxis of cytomegalovirus infection. I. Efficacy of immunization. Microbiol Immunol. 1978;22:693–700. doi: 10.1111/j.1348-0421.1978.tb00422.x. [DOI] [PubMed] [Google Scholar]
- 47.Morrison L A, Knipe D M. Immunization with replication-defective mutants of herpes simplex virus type 1: sites of immune intervention in pathogenesis of challenge virus infection. J Virol. 1994;68:689–696. doi: 10.1128/jvi.68.2.689-696.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Morrison L A, Knipe D M. Mechanisms of immunization with a replication-defective mutant of herpes simplex virus 1. Virol. 1996;220:402–413. doi: 10.1006/viro.1996.0328. [DOI] [PubMed] [Google Scholar]
- 49.Orange J S, Wang B, Terhorst C, Biron C A. Requirement for natural killer cell-produced interferon-gamma in defense against murine cytomegalovirus infection and enhancement of this defense pathway by interleukin 12 administration. J Exp Med. 1995;182:1045–1056. doi: 10.1084/jem.182.4.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Osborn J E, Walker D L. Virulence and attenuation of murine cytomegalovirus. Infect Immun. 1970;3:228–236. doi: 10.1128/iai.3.2.228-236.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Plotkin S A, Friedman H M, Fleisher G R, Dafoe D C, Grossman R A, Smiley M L, Starr S E, Wlodaver C, Friedman A D, Barker C F. Towne-vaccine-induced prevention of cytomegalovirus disease after renal transplants. Lancet. 1984;ii:528–530. doi: 10.1016/s0140-6736(84)90930-9. [DOI] [PubMed] [Google Scholar]
- 52.Plotkin S A, Higgins R, Kurtz J B, Morris P J, Campbell D A, Shope T C, Spector S A, Dankner W M. Multicenter trial of Towne strain attenuated virus vaccine in seronegative renal transplant recipients. Transplantation. 1994;58:1176–1178. [PubMed] [Google Scholar]
- 53.Plotkin S A, Starr S E, Friedman H M, Gonczol E, Weibel R E. Protective effects of towne cytomegalovirus vaccine against low-passage cytomegalovirus administered as a challenge. J Infect Dis. 1989;159:860–865. doi: 10.1093/infdis/159.5.860. [DOI] [PubMed] [Google Scholar]
- 54.Plotkin S A, Weibel R E, Alpert G, Starr S E, Friedman H M, Preblud S R, Hoxie J. Resistance of seropositive volunteers to subcutaneous challenge with low-passage human cytomegalovirus. J Infect Dis. 1985;151:737–739. doi: 10.1093/infdis/151.4.737. [DOI] [PubMed] [Google Scholar]
- 55.Pollock J L, Presti R M, Paetzold S, Virgin H W. Latent murine cytomegalovirus infection in macrophages. Virology. 1997;227:168–179. doi: 10.1006/viro.1996.8303. [DOI] [PubMed] [Google Scholar]
- 56.Pollock J L, Virgin H W. Latency, without persistence, of murine cytomegalovirus in spleen and kidney. J Virol. 1995;69:1762–1768. doi: 10.1128/jvi.69.3.1762-1768.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Porath A, Mcnutt R A, Smiey L M, Weigle K A. Effectiveness and cost benefit of a proposed live cytomegalovirus vaccine in the prevention of congenital disease. Rev Infect Dis. 1990;12:31–40. doi: 10.1093/clinids/12.1.31. [DOI] [PubMed] [Google Scholar]
- 58.Quinnan G V, Kirmani N, Rook A H, Manischewitz J F, Jackson L, Moreschi G, Santos G W, Saral R, Burns W H. Cytotoxic T cells in cytomegalovirus infection: HLA-restricted T-lymphocyte and non-T-lymphocyte cytotoxic responses correlate with recovery from cytomegalovirus infection in bone-marrow-transplant recipients. N Engl J Med. 1982;307:7–13. doi: 10.1056/NEJM198207013070102. [DOI] [PubMed] [Google Scholar]
- 59.Reddehase M J, Baltheson M, Rapp M, Jonjic S, Pavic I, Koszinowski U H. The conditions of primary infection define the load of latent viral genome in organs and the risk of recurrent cytomegalovirus disease. J Exp Med. 1994;179:185–193. doi: 10.1084/jem.179.1.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reddehase M J, Jonjic S, Weiland F, Mutter W, Koszinowski U H. Adoptive immunotherapy of murine cytomegalovirus adrenalitis in the immunocompromised host: CD4-helper-independent antiviral function of CD8-positive memory T lymphocytes derived from latently infected donors. J Virol. 1988;62:1061–1065. doi: 10.1128/jvi.62.3.1061-1065.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reddehase M J, Keil G M, Koszinowski U H. The cytolytic T lymphocyte response to the murine cytomegalovirus. II. Detection of virus replication stage-specific antigens by separate populations of in vivo active cytolytic T lymphocyte precursors. Eur J Immunol. 1984;14:56–61. doi: 10.1002/eji.1830140111. [DOI] [PubMed] [Google Scholar]
- 62.Reddehase M J, Mutter W, Munch K, Buhring H J, Koszinowski U H. CD8-positive T lymphocytes specific for murine cytomegalovirus immediate-early antigens mediate protective immunity. J Virol. 1987;61:3102–3108. doi: 10.1128/jvi.61.10.3102-3108.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Scalzo A A, Elliott S L, Cox J, Gardner J, Moss D J, Suhrbier A. Induction of protective cytotoxic T cells to murine cytomegalovirus by using a nonapeptide and a human-compatible adjuvant (montanide ISA 720) J Virol. 1995;69:1306–1309. doi: 10.1128/jvi.69.2.1306-1309.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Smiley M L, Wlodaver C G, Grossman R A, Barker C F, Perloff L J, Tustin N B, Starr S E, Plotkin S A, Friedman H M. The role of pretransplant immunity in protection from cytomegalovirus disease following renal transplantation. Transplantation. 1985;40:157–161. doi: 10.1097/00007890-198508000-00010. [DOI] [PubMed] [Google Scholar]
- 65.Smith S C, Allen P M. Myosin-induced acute myocarditis is a T cell-mediated disease. J Immunol. 1991;147:2141–2147. [PubMed] [Google Scholar]
- 66.Starr, S. E., H. M. Friedman, and S. A. Plotkin. 1991. The status of cytomegalovirus vaccine. Rev. Infect. Dis. 13(Suppl. 11):S964–S965. [DOI] [PubMed]
- 67.Tay C H, Welsh R M. Distinct organ-dependent mechanisms for the control of murine cytomegalovirus infection by natural killer cells. J Virol. 1997;71:267–275. doi: 10.1128/jvi.71.1.267-275.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Thale R, Szepan U, Hengel H, Geginat G, Lucin P, Koszinowski U H. Identification of the mouse cytomegalovirus genomic region affecting major histocompatibility complex class I molecule transport. J Virol. 1995;69:6098–6105. doi: 10.1128/jvi.69.10.6098-6105.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tonari Y, Minamishima Y. Pathogenicity and immunogenicity of temperature-sensitive mutants of murine cytomegalovirus. J Gen Virol. 1983;64:1983–1990. doi: 10.1099/0022-1317-64-9-1983. [DOI] [PubMed] [Google Scholar]
- 70.Tyler K L, Mann M A, Fields B N, Virgin H W. Protective anti-reovirus monoclonal antibodies and their effects on viral pathogenesis. J Virol. 1993;67:3446–3453. doi: 10.1128/jvi.67.6.3446-3453.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Virgin H W, Tyler K L. Role of immune cells in protection against and control of reovirus infection in neonatal mice. J Virol. 1991;65:5157–5164. doi: 10.1128/jvi.65.10.5157-5164.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Volkmer H, Bertholet C, Jonjic S, Wittek R, Koszinowski U H. Cytolytic T lymphocyte recognition of the murine cytomegalovirus nonstructural immediate-early protein pp89 expressed by recombinant vaccinia virus. J Exp Med. 1987;166:668–677. doi: 10.1084/jem.166.3.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Walter E A, Greenberg P D, Gilbert M J, Finch R J, Watanabe K S, Thomas E D, Riddell S R. Reconstitution of cellular immunity against cytomegalovirus in recipients of allogeneic bone marrow by transfer of T-cell clones from the donor. N Engl J Med. 1995;333:1038–1044. doi: 10.1056/NEJM199510193331603. [DOI] [PubMed] [Google Scholar]
- 74.Welsh R M, Brubaker J O, Vargas Cortes M, O’Donnell C L. Natural killer (NK) cell response to virus infections in mice with severe combined immunodeficiency. The stimulation of NK cells and the NK cell-dependent control of virus infections occur independently of T and B cell function. J Exp Med. 1991;173:1053–1063. doi: 10.1084/jem.173.5.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Winston D J, Ho W G, Lin C-H, Bartoni K, Budinger M D, Gale R P, Champlin R E. Intravenous immune globulin for prevention of cytomegalovirus infection and interstitial pneumonia after bone marrow transplantation. Ann Intern Med. 1987;106:12–18. doi: 10.7326/0003-4819-106-1-12. [DOI] [PubMed] [Google Scholar]
- 76.Yamashita Y, Shimokata K, Mizuno S, Yamaguchi H, Nishiyama Y. Down-regulation of the surface expression of class I MHC antigens by human cytomegalovirus. Virology. 1993;193:727–736. doi: 10.1006/viro.1993.1181. [DOI] [PubMed] [Google Scholar]