Key Clinical Message
Some cases of left ventricular pseudoaneurysms (LVPAs) are asymptomatic. While cardiac magnetic resonance imaging is important, a chest x‐ray can easily be performed and is also crucial for the detection of LVPA during the first outpatient visit.
Keywords: cardiac magnetic resonance imaging, chest x‐ray, left ventricular pseudoaneurysm, myocardial infarction
A 68‐year‐old man with diabetes mellitus was urgently admitted to our hospital due to dyspnea. Two weeks prior to admission, he experienced acute chest pain at rest for hours, which subsequently improved; however, shortness of breath developed. His blood pressure measured 150/80 mmHg, heart rate 120 beats per minute, and oxygen saturation level, as derived from pulse oximetry, 88% on room air. The electrocardiogram (ECG) exhibited ST elevation and abnormal Q waves in the anterior leads (Figure 1A). He was diagnosed with acute heart failure associated with a myocardial infarction (MI) that occurred 2 weeks prior, without any elevated myocardial enzymes (creatinine kinase 126 U/L, lactate dehydrogenase 259 U/L). Following the stabilization of his hemodynamic condition, cardiac catheterization was performed 7 days post‐admission. He had a severe stenosis in the proximal left anterior descending artery, and a drug‐eluting stent was implanted. He was discharged 2 weeks post‐admission with improved heart failure symptoms, as evidenced by a chest x‐ray (Figure 1B). Cardiac magnetic resonance imaging (CMRI) performed during hospitalization showed no cardiac mechanical complications and pericardial effusions after the PCI. He was asymptomatic and his blood pressure remained stable and was controlled at less than 120/80 mmHg, after discharge. However, a chest x‐ray during his first outpatient visit 1 month later revealed a projection on the left ventricle (Figure 1C). CMRI revealed a left ventricular pseudoaneurysm (LVPA) (Figure 1D). The LVPA developed between the time of discharge and the first outpatient visit. Considering the risk of a rupture, he underwent an urgent left ventriculoplasty (intraoperative pictures; Figure 1E). A pseudoaneurysm measuring 4 cm × 4 cm was identified in the anterior wall of the left ventricle, containing a rupture site measuring 3 cm × 3 cm within the same area. He was subsequently discharged from the hospital without any complications.
FIGURE 1.
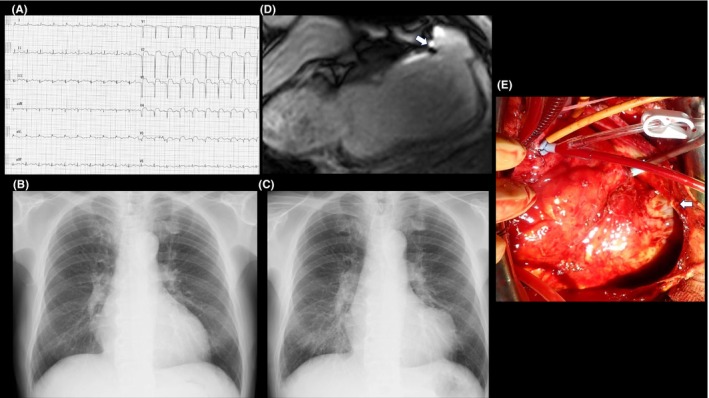
(A) ST elevation and abnormal Q waves in the anterior leads on the electrocardiogram upon admission. (B) The chest x‐ray on discharge revealed mild cardiac enlargement. (C) The chest x‐ray during the first outpatient visit 1 month after discharge revealed a projection on the left ventricle. (D) Cardiac magnetic resonance imaging (CMRI) during the first outpatient visit 1 month after discharge. CMRI revealed a left ventricular pseudoaneurysm on the anterior left ventricular wall (white arrow). (E) Intraoperative picture of the left ventricular pseudoaneurysm (white arrow).
There are two types of left ventricular aneurysms after an MI: true aneurysms and pseudoaneurysms. A left ventricular true aneurysm forms due to thinning and bulging of the infarcted myocardial wall under internal pressure. In contrast, an LVPA results from a rupture of the infarcted myocardium. In this case, the left ventricular aneurysm was enveloped by an epicardial membrane, and the intraoperative findings revealed a myocardial contusion, indicative of an LVPA. Cardiac symptoms are usually present in cases with an LVPA. However, as demonstrated in this case, patients may present to the hospital asymptomatically after discharge. Approximately 10% of patients with an LVPA are reported to be asymptomatic. 1 CMRI is a noninvasive imaging modality that is not limited by technical imaging factors. CMRI can identify normal and abnormal myocardium, thrombi, and the characteristics of the pericardium. The traditional risk factors for LVPAs include an older age, female sex, hypertension, and inferior and lateral wall MI, 2 but in this case, only an older age was present. Therefore, it is crucial to perform not only ECGs but also regular chest x‐rays, and ideally echocardiograms, and, if a detailed evaluation is needed, CMRI, despite the risk of an LVPA. Management of an acute LVPA typically is surgical, as the annual risk of a rupture is 30%–45%, which outweighs the risks associated with the surgery. 2
AUTHOR CONTRIBUTIONS
Taisuke Hanamura: Writing – review and editing. Daisuke Fukamachi: Writing – original draft. Masashi Tanaka: Supervision. Yasuo Okumura: Supervision; writing – review and editing.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors report no potential competing interests.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Hanamura T, Fukamachi D, Tanaka M, Okumura Y. Asymptomatic left ventricular pseudoaneurysm. Clin Case Rep. 2024;12:e8599. doi: 10.1002/ccr3.8599
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions.
REFERENCES
- 1. Figueras J, Alcalde O, Barrabés JA, et al. Changes in hospital mortality rates in 425 patients with acute ST‐elevation myocardial infarction and cardiac rupture over a 30‐year period. Circulation. 2008;118:2783‐2789. [DOI] [PubMed] [Google Scholar]
- 2. Alapati L, Chitwood WR, Cahill J, Mehra S, Movahed A. Left ventricular pseudoaneurysm: a case report and review of the literature. World J Clin Cases. 2014;2:90‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to privacy/ethical restrictions.


