Abstract
Introduction
Adverse childhood experiences (ACEs) are strongly correlated with many of the most common causes of preventable illness, preventable death, and health disparities. In January 2020, California launched the first statewide initiative to integrate ACE screening throughout its Medicaid system. A key element of the initiative was the California ACEs Learning and Quality Improvement Collaborative, a 48-clinic, 16-month learning collaborative. This evaluation aimed to determine whether developing a trauma-informed environment of care was associated with uptake of ACE screening.
Methods
Participants included 40 of 48 clinics that participated in the statewide learning collaborative. Clinics completed an assessment of progress in 5 essential components of trauma-informed health care at baseline and 1-year follow-up. Clinics tracked data on ACE screens completed on an ongoing basis and submitted data quarterly. A hierarchical linear model was used to examine the association between change in readiness for trauma-informed health care and change in quarterly screens.
Results
Readiness for trauma-informed health care increased for all participating clinics over the course of the learning collaborative. The average number of quarterly screens also increased, with considerable variability among clinics. Clinics with larger increases in readiness for trauma-informed health care had larger increases in quarterly screens.
Discussion
The findings align with long-standing recommendations for trauma screening to occur in the context of trauma-informed environments of care.
Conclusion
A trauma-informed clinic is the foundation for successful adoption of ACE screening. ACE screening initiatives should include education and sufficient support for clinics to embrace a trauma-informed systems change process.
Introduction
Adverse childhood experiences (ACEs) refer to 10 categories of childhood adversities clustered in 3 domains originally identified in the seminal 1998 study: child abuse (physical, emotional, or sexual); neglect (physical or emotional); and household challenges (growing up with household incarceration, mental illness, substance dependence, parental separation or divorce, or intimate partner violence).1 ACEs are common but underrecognized: 61% of US adults have had at least 1 ACE and 16% have had 4 or more.1
A large body of evidence documents a strong dose-response correlation between ACEs and many of the most common causes of preventable illness, preventable death, and disparities in health. In addition to the immediate effects of ACEs on a child’s health and well-being, the magnitude of the impact of ACEs on later health is startling.2,3 The Centers for Disease Control and Prevention estimates that 44% of adult depression, 33% of smoking, 27% of chronic lung disease, 24% of heavy drinking, and 24% of asthma are directly attributable to ACEs.4 ACEs are also correlated with many adult social and economic challenges, including high school noncompletion, unemployment, poverty, and homelessness, which can serve as additional pathways for the intergenerational transmission of adversity.
In January 2020, the Office of the California Surgeon General and the California Department of Health Care Services launched the ACEs Aware initiative.5 ACEs Aware is the first statewide effort to integrate ACE screening for children and adults throughout its 13-million-member Medicaid system. The initiative includes reimbursement for each eligible screen and substantial investments in clinician and community education, engagement, and practice transformation. Specific priorities include training primary care clinician how to screen for, prevent, and address ACEs and toxic stress; increasing awareness and utilization of evidence-informed clinical and community interventions; and building clinical capacity to screen for and respond to ACEs and toxic stress by investing in clinical quality improvement and community networks of care.
A key element of ACEs Aware was the California ACEs Learning and Quality Improvement Collaborative (CALQIC), a 48-clinic, statewide 16-month learning collaborative focused on identifying the facilitators, barriers, and impact of integrating ACE screening into frontline safety-net clinics serving children, adults, and families. Participating CALQIC health care organizations received grant funding, individualized coaching to support clinics in integrating ACE screening into their clinical workflows, statewide virtual learning sessions for skill building and information exchange, and connections to peers, experts, and resources.
Many experts in the care of patients who have experienced adversity argue that any form of trauma inquiry, including ACE screening, is best accomplished in the context of a trauma-informed clinical environment.6–9 The key principles of trauma-informed health care (TIHC) have been well described.10,11 Fundamentally, a trauma-informed clinical environment allows patients and families to feel safe and connected enough with their care team to disclose sensitive experiences of childhood adversity and/or the stigmatized situations and coping behaviors that can result from adversity. The safe, stable, and nurturing relationships formed between patients and clinician in such environments can also have positive physiologic effects and can help patients more fully engage in care and buffer the damaging impacts of ACEs and other traumas.5,12–14
For this reason, CALQIC included support for clinics to develop trauma-informed clinical environments alongside support to implement ACE screening. This support focused on 5 core components of TIHC (see Figure 1)11: 1) a foundation grounded in trauma-informed principles, an interdisciplinary team-based approach, community partnerships, buy-in from organizational leadership, and supervision and support for all staff and clinician; 2) an environment of care that is calm, safe, and empowering for patients, staff, and clinician; 3) education for all patients about the impacts of current and past trauma, the benefits of protective factors, and opportunities for healing; and 4) inquiry for and 5) response to recent and past trauma, protective factors, and adversity-associated health conditions that include on-site and/or community-based opportunities for safety, connection, and healing.
Figure 1:
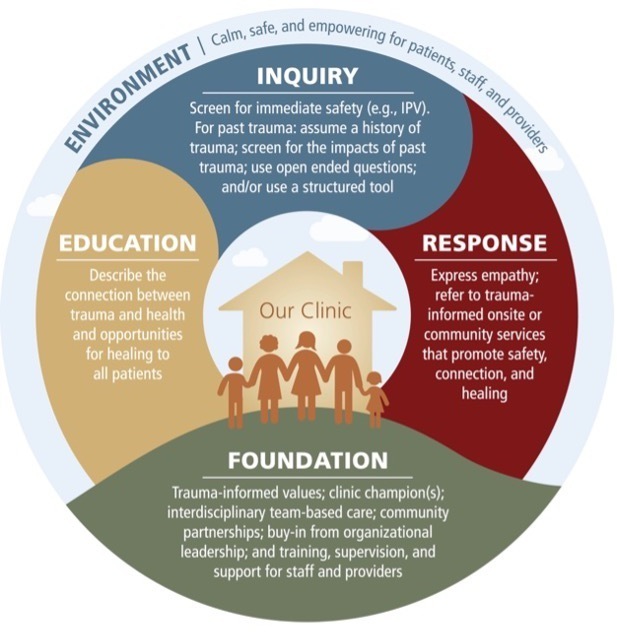
Core components of trauma-informed health care. Source: Machtinger et al. From treatment to healing: Inquiry and response to recent and past trauma in adult health care. Women’s Health Issues 2019;29(2): 97–101. IPV = intimate partner violence. Reproduced under Creative Commons CC-BY license.
As clinics and health care systems consider implementing ACE screening, there is limited empirical evidence to guide them. The current program evaluation addresses this gap by using data collected as part of the CALQIC statewide learning collaborative to examine whether developing a TIHC environment was associated with the start and increased uptake of ACE screening in participating clinics.
Methods
Participating clinics
The evaluation included 40 out of 48 clinics across 15 safety-net health care organizations that participated in the CALQIC statewide learning collaborative (the 8 excluded clinics did not provide data at both time points). Within the 15 health care organizations, 1 to 5 clinics participated (mean = 2.7, standard deviation [SD] = 1.1). The health care organizations participating in CALQIC are located throughout California and collectively serve both urban and rural populations, including large Medi-Cal (California’s Medicaid program) populations. The individual clinic sites included pediatric, family medicine, and adult primary care clinics.
Procedures
Clinics developed workflows for ACE screening as part of their participation in the statewide learning collaborative. Clinics implemented screening in the manner that made the most sense to them; the learning collaborative did not dictate specific screening workflows or patient eligibility, but coaches provided technical assistance as clinics made these decisions independently. Workflows varied across clinics, but in a typical workflow, a medical assistant gave patients or their caregivers (for patients under age 12) the ACE screener, and a clinician (physician, physician assistant, or nurse practitioner) reviewed screening results and discussed them with the patient. Clinics individually determined what populations to screen, which also varied. For instance, some adult primary care clinics focused on screening patients with certain ACE-associated health conditions (eg, diabetes, hypertension). Pediatric clinics typically screened at well-child visits and identified specific ages at which to screen. Medi-Cal requires clinician to complete the state’s ACEs Aware core training in order to be reimbursed for screening; as such, clinics commonly limited the screening to patients seen by trained clinician.
As part of learning collaborative participation, clinics completed the Clinic Readiness for Trauma-Informed Health Care Assessment tool early and late in their participation (ie, at baseline and follow-up time points roughly 1 year apart) and provided data on completed ACE screens on a quarterly basis (described further under Measures). This screening data was provided as part of standard quarterly reporting that was required as part of their learning collaboration participation. Internal review boards (IRBs) of the State of California, the Kaiser Permanente Washington Health Research Institute, and the University of California, San Francisco all determined that the project was a program evaluation not subject to IRB review.
Measures
Adverse childhood experience screening
Clinics collected data on completed ACE screens on an ongoing basis. Participating clinics reported the total number of ACE screens they conducted on a quarterly basis over a 1-year period. Pediatric ACEs were collected via the Pediatric ACEs and Related Life Events Screener (PEARLS),15,16 and adult ACEs were collected via the ACE Questionnaire (ACE-Q).17 Both the ACE-Q18–20 and the PEARLS15 questionnaire have been found to be reliable and valid, showing internal consistency, test-retest reliability, face validity, and associations with health.15,21
Clinic readiness for trauma-informed health care assessment tool
An assessment tool to measure clinic readiness to provide TIHC was developed by the CALQIC leadership team at the University of California, San Francisco and evaluation partners at the Center for Community Health and Evaluation. The content of the new Clinic Readiness Assessment for Trauma-Informed Health Care was informed by multiple existing tools, including the National Council for Behavioral Health’s Organizational Self-Assessment for Adoption of Trauma-Informed Care Approaches in a Primary Care Setting,22 the System of Care Trauma-Informed Agency Assessment,23 the Pediatric Integrated Care Collaborative framework,24 and the American Institute for Research Trauma-Informed Organizational Capacity Scale.25 The tool consists of 16 items that examine clinics’ progress in 5 essential components of a framework for TIHC26: foundation, environment, patient education, screening and assessment, and response. The items were selected to measure the capacities and practices deemed essential to successful implementation of ACE screening in a trauma-informed environment. The authors examined the reliability of the items in the tool and found that they were internally consistent (Cronbach’s alpha = 0.96).
Table 1 shows the items associated with each of the 5 components. Each item response is on a 5-point scale (1 = no, not in place/doesn’t happen; 3 = sometimes happens/somewhat in place; 5 = yes, consistently in place/usually happens). Clinics provided responses to all 16 items at the beginning of the learning collaborative (third quarter of 2020) and at the end (third quarter of 2021). A clinic readiness for TIHC score is calculated for each component by averaging the responses to the 16 items. An overall index of each clinic’s readiness for TIHC is calculated by averaging the response of all items.
Table 1:
Clinic readiness for trauma-informed health care assessment tool
| Item | Component |
|---|---|
| Our clinic provides education or training to all staff and clinician on trauma and resilience and implications for care | Foundation |
| Data related to trauma- and resilience-informed care is tracked, analyzed, and used to address challenges and/or reinforce programs | Foundation |
| Leadership expresses commitment to implementing trauma- and resilience-informed care | Foundation |
| Clinic champions/core team engages clinic staff in trauma-informed care activities (eg, solicits and incorporates feedback; communicates about progress related to education, screening, and assessment; and response for ACEs and other traumatic experiences) | Foundation |
| People at my clinic are comfortable talking to patients and caregivers about trauma | Environment |
| Our clinic understands how working with trauma survivors can affect staff | Environment |
| Patients and families receive information about current and past trauma (ACEs) and toxic stress and how they impact health and behavior | Patient education |
| The health care team clearly explains to patients and families why screening questions are being asked | Patient education |
| Our organization has a consistent screening or assessment process to identify individuals who have been exposed to trauma (eg, using PEARLS, ACE-Q in a structured screening and referral workflow) | Screening & assessment |
| Our organization defines the roles, responsibilities, and workflows for all health care team members related to screening and assessment processes | Screening & assessment |
| Our organization has clearly established electronic health record documentation and reporting practices and processes related to ACE screening and response | Screening & assessment |
| Our organization systematically screens for traumatic experiences or ACEs (eg, uses a set protocol or tool) | Screening & assessment |
| Designated care team members discuss screening results with patients and/or families to foster shared decision making and work with the patient and/or family to develop a plan | Response |
| Care team members do warm handoff to internal supports or resources (eg, co-located mental health personnel) | Response |
| Our clinic provides a warm handoff for referrals to community-based specialists | Response |
| Health care team plans post-screening follow-up visit or phone/video call with patient to assess whether referrals were successful and appropriately adjusts plan to ensure connection to desired resources and support | Response |
ACE, adverse childhood experience; ACE-Q, ACE Questionnaire; PEARLS, Pediatric ACEs and Related Life Events Screener.
Statistical analyses
The authors used SAS Version 9.4 statistical analysis software (SAS Institute 9.4., Cary, NC, USA) to run hierarchical linear models (HLMs) in which clinics (Level 1) are nested within organizations (Level 2). HLMs are appropriate for data like these in which observations are not independent due to the clustering of data (ie, clinics within organizations).21,22 Within the HLM framework, F-tests were used to examine whether differences between means were statistically significant. First, the authors examined whether mean clinic readiness for TIHC differed significantly between baseline and follow-up, including examination of 5 components of TIHC. Next, they compared mean quarterly ACE screening volume between baseline and follow-up. Finally, they assessed the association between changes in clinic readiness for TIHC and changes in quarterly screening volume, including examination of each of the 5 components of readiness for TIHC in relation to changes in quarterly screens completed. Specifically, F-tests were used to examine whether the association with the change in quarterly screening volume was statistically significant after controlling for baseline screening volume and readiness.
Results
Changes in clinic readiness for trauma-informed health care
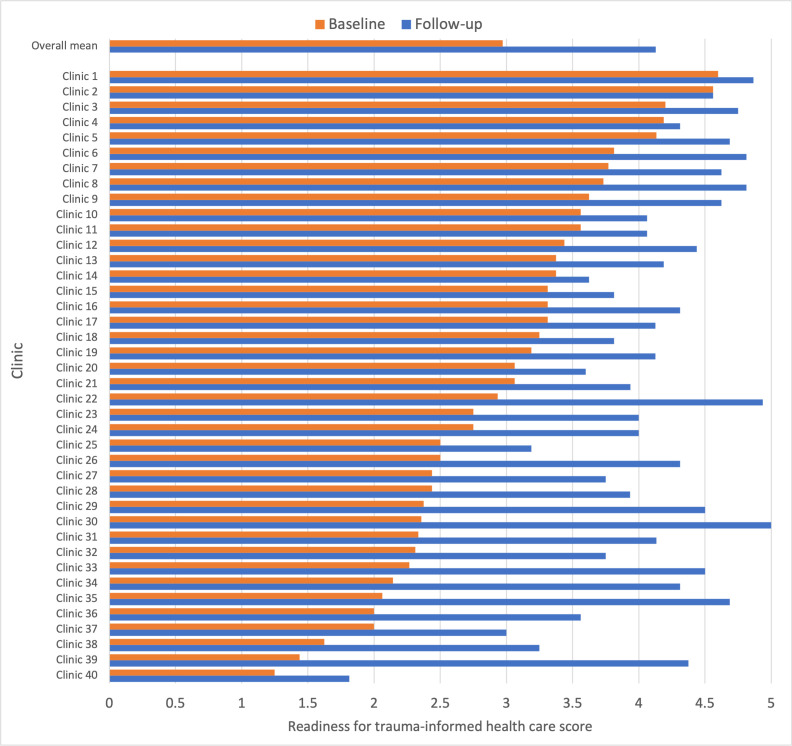
Readiness scores for TIHC increased for all 40 clinics over the 1-year period (Figure 2). On average, total readiness for TIHC scores (range: 0–5) increased from baseline (M = 3.0, SD = 0.8) to follow-up (M = 4.1, SD = 0.6), F1,80 = 50.6, p < 0.0001. There was variation across clinics, from no change (Clinic 2) to a large increase of 2.9 (Clinic 39), but clinics at both low and high starting values experienced change. Clinic 2 had a high starting value (4.6) and did not experience a change, but other clinics with high starting values did experience increases (eg, Clinic 1’s score increased from 4.6 to 4.9 and Clinic 3’s increased from 4.2 to 4.8). Clinic 39 had one of the lowest starting values (1.5), and many clinics with low starting values also experienced large increases although some experienced more modest change (eg, Clinic 40).
Figure 2:
Changes in readiness for trauma-informed health care between baseline and 1-year follow-up, by clinic. Note: scale: 1 = no—this is not in place or doesn’t happen as part of our operations; 3 = sometimes/somewhat—this is somewhat in place or sometimes happens but is not standard practice; 5 = yes—this is consistently in place/usually happens as part of our standard practice and/or our culture.
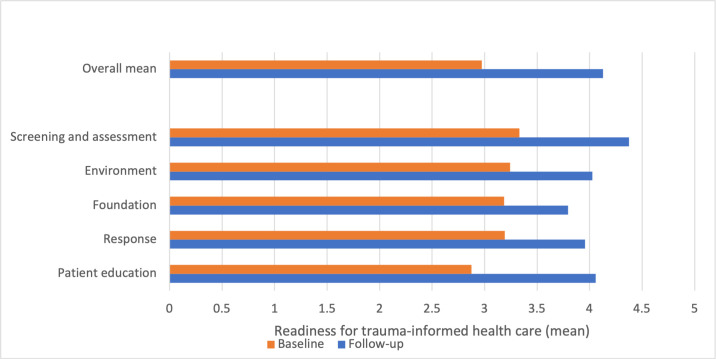
When the indices were grouped and combined according to their 5 core components, each core component also increased from baseline to follow-up (Figure 3). Patient education increased the most (from M = 2.9, SD = 0.9 to M = 4.1, SD = 0.6 across all clinics), F1,80 = 49.6, p < 0.0001, and foundation increased the least (from M = 3.2, SD = 0.7 to M = 3.8, SD = 0.6), F1,80 = 16.79, p < 0.0001.
Figure 3:
Changes in readiness for trauma-informed health care between baseline and 1-year follow-up, overall and by component. Note: scale: 1 = no—this is not in place or doesn’t happen as part of our operations; 3 = sometimes/somewhat—this is somewhat in place or sometimes happens but is not standard practice; 5 = yes—this is consistently in place/usually happens as part of our standard practice and/or our culture.
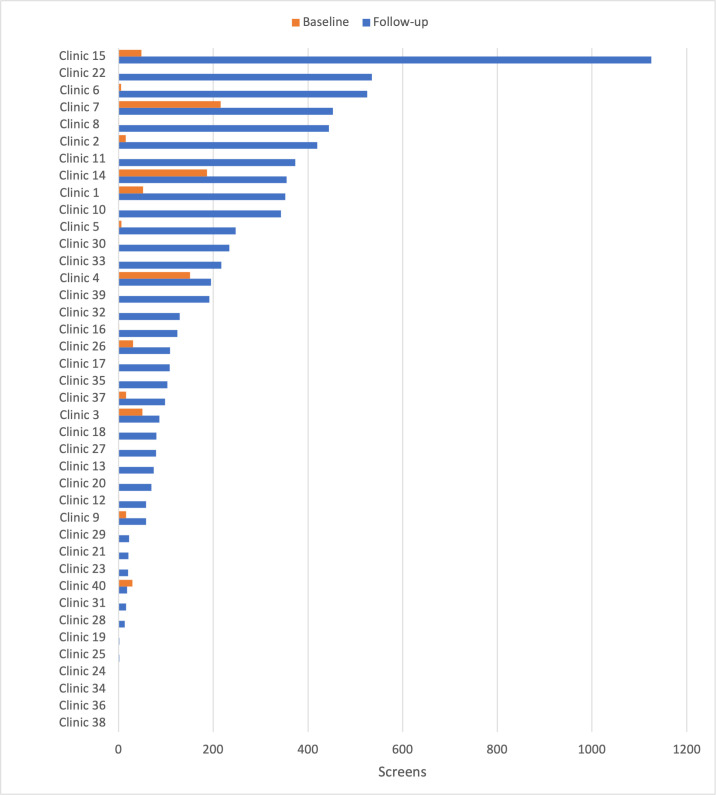
Changes in adverse childhood experiences screening
Forty clinics provided screening data for all 5 quarters. In total, they conducted 18,450 screens over the 1-year period from baseline to follow-up. The number of median quarterly screens increased over the course of the year, from 0 per quarter at baseline to 100.5 per quarter at follow-up, but there was wide variation in this change (Figure 4). Most clinics increased the number of screens they conducted per quarter, although 1 clinic conducted fewer screens at follow-up than at baseline (Clinic 40). An F-test examining the difference in mean screens between baseline and follow-up confirmed a significant increase over time, even when removing one outlier clinic that conducted an unusually large number of screens (F1,78 = 26.02 , p < 0.0001).
Figure 4:
Number of quarterly screens at baseline and 1-year follow-up, from clinic with most screens at follow-up to least. Note: clinics 19 and 25 reported conducting 2 screens at follow-up, but they are difficult to see on the Figure due to inclusion of Clinic 15, which conducted 1125 screens. Clinic ID numbers are consistent with Figure 2.
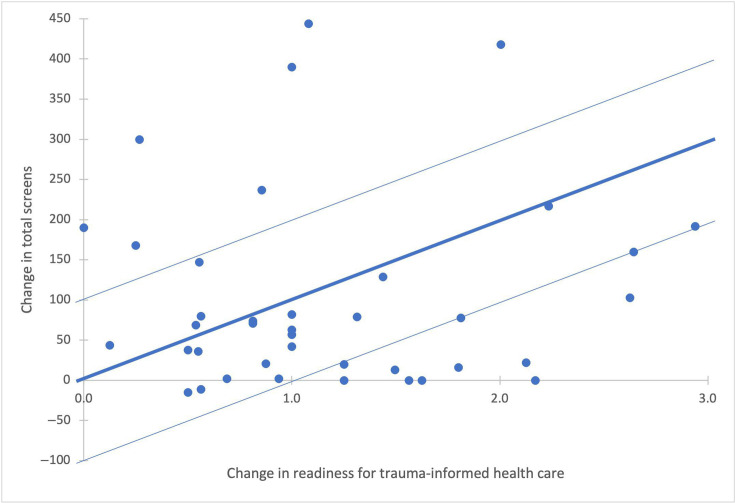
Association between change in clinic readiness for trauma-informed health care and change in ACE screens
Clinics with larger increases in readiness for TIHC had larger increases in quarterly screens (Figure 5). To quantify the association in this sample, a 1-point change in the readiness for TIHC score from baseline to follow-up was associated with 97 more screens per quarter on average (F1,21 = 4.67, p = 0.04, 95% confidence interval: 4, 190). The authors also estimated the association between the change in screens and the change in each of the 5 components of readiness for TIHC. Each component exhibited a positive association between increased readiness and ACE screen volume, though environment was the only component that had a statistically significant association between increased readiness for TIHC and increased screens. A 1-point increase in the environment component was associated with 100 more screens per quarter on average (p = 0.06, confidence interval: −2, 202, not shown).
Figure 5:
Association between change in readiness for TIHC and change in screens per quarter between baseline and follow-up (includes 95% confidence intervals for estimates). Note: dots represent observed values of change in screening and TIHC index for each site. The lines represent the estimated association between changes in TIHC index and total screens. These estimates are based on a hierarchical linear model that accounts for nesting of clinics within organizations. Dark line represents model estimate. Light lines represent the 95% confidence interval. One site with an increase of 1125 total screens (9 times the average change and 2.5 times the next-highest change) is dropped from the figure and the estimated association because this outlier made it hard to depict the main findings. TIHC = trauma-informed health care.
Discussion
This study demonstrated a positive association between the development of a trauma-informed environment of care and the start and increased uptake of ACE screening. To the best of the authors’ knowledge, this is the first published study documenting this association. The results have important implications for how ACE screening is supported and disseminated.
The findings align with long-standing recommendations for trauma screening of any kind to occur in the context of trauma-informed environments of care.11,27 Trauma-informed environments of care can help patients feel safe and connected enough with clinician and/or staff to disclose experiences of trauma as well as other important potentially stigmatizing trauma-related conditions and behaviors. A trauma-informed environment of care can also improve the screening experience for both patients and clinician, providing the opportunity to deepen relationships and expand possibilities for prevention and healing. In this study, all 40 participating clinics made progress on the continuum of becoming trauma-informed regardless of where they started. This suggests that implementing ACE screening, when accompanied by a commitment and support to be trauma-informed, can have the added and synergistic benefit of catalyzing a clinic-wide trauma-informed systems change.
Although there are well-developed principles for TIHC, guidance for implementing TIHC in primary care is still in an early stage of development.10 Several recent systematic reviews identified tools for measuring TIHC in various types of care settings.28–31 However, there are few that are applicable to medical care settings and include the multiple components of a systems-based measurement. The tool used in this study fills that gap. The Clinic Readiness Assessment for Trauma-Informed Health Care was informed by and aligns with a published framework of TIHC and its essential components. It is specific to the pediatric and adult primary care settings and practical for use by clinic staff. It provided an initial assessment of clinic readiness, and the results were used to guide coaching, webinar content, and quality improvement for clinics in the learning collaborative. Although the study was not designed to validate this new instrument, the findings justify and inform efforts to do so.
The study has several limitations. It occurred in the context of a statewide learning collaborative that lacked a comparison group. As such, the data do not allow for the confirmation of a causal link between developing a trauma-informed environment of care and the start and increased uptake of ACE screening. The instrument used to measure the degree to which clinics are trauma-informed was developed for this initiative, had not been previously validated, and relied on self-report by the participating clinics. As such, the survey data is vulnerable to pressure to report better and improved performance and cannot be conclusively linked to actual changes in clinic practice. The ACE screening data were dependent on accurate reporting of completed screens, and local data collection practices for a new procedure may have varied. The design and duration of this study did not permit the use of Medicaid billing data for ACE screens because such data are not currently complete and available until up to a year after the screen occurred. Future multisite studies that quantify ACE screens should be designed to rely on state billing data because this will likely be a more consistent measure across different clinical sites. The study also lacked power to detect significant associations between each of the 5 components of TIHC and the start and increased uptake of ACE screening, which may explain why the study only detected a statistically significant association for one of the components of the assessment tool.
In addition, it is notable that the learning collaborative and data collection occurred at the height of the COVID-19 pandemic. Although clinics remained strongly engaged in the project, they experienced challenges such as loss and redeployment of staff and transition to telehealth, in many cases reducing their capacity to make system changes and conduct ACE screens. It is possible that the authors would have found a stronger association between trauma-informed environment and ACE screens if the work had been conducted at a different point in time.
Nonetheless, the study has several strengths and important implications. The study provides evidence from 40 safety-net clinics across 15 organizations serving 250,000 Medi-Cal patients in rural and urban areas across the state of California that a trauma-informed clinic is associated with, and may be the foundation for, successful implementation of ACE screening. The results suggest that ACE screening initiatives should include education and sufficient support for clinics to embrace a trauma-informed systems change process.
Future research is needed to clarify the necessary components of trauma-informed systems change and the short- and longer-term impacts of such changes on patient-clinician relationships, health outcomes, and health disparities. Similarly, controlled studies are needed to clarify if and how ACE screening in frontline health care settings serving various patient populations can lead to the prevention and mitigation of the impact of ACEs and other traumas on health outcomes and health disparities. The future of both fields—trauma-informed care and ACE screening—depends on the demonstration of clear benefits to health outcomes and health disparities among patients and on the reduction of burnout and retention of clinician. Future work in this field should also support inquiry for protective factors, strengths, and resilience alongside trauma screening as part of a whole-person approach to care. The benefit of safe, stable, and nurturing relationships and environments has been well documented to interrupt the impact of adversity on later health and well-being.13,32 There is also evidence for neuroplasticity and a lifelong capacity for learning and building resilience.33 In light of this, many experts and organizations have adopted terms such as “trauma- and resilience-informed health care” to encourage holistic assessment of individual patients that includes both experiences of adversity and sources of protective factors, strengths, and resilience.34–36
Conclusion
Growing awareness of the impact of ACEs on health and well-being has led the State of California and many clinics across the nation to integrate ACE screening into health care for children, adults, and families. The current study provides early evidence that clinics that improve their readiness to provide TIHC are better able to start and increase uptake of ACE screening. This suggests that supporting a clinic’s trauma-informed systems change is foundational for successful implementation of ACE screening.
Acknowledgments
The authors would like to express their gratitude for the trust and participation of patients and their families in this evaluation.
Footnotes
Author Contributions: Edward L Machtinger, MD, acquired funding, contributed to conceptualization, writing of draft, reviewing, and edited the manuscript. Nicole K Eberhart, PhD, contributed to the conceptualization, supervision, and writing, reviewing, editing, and submission of the final manuscript. J Scott Ashwood, PhD, designed and conducted data analyses and contributed to writing of original draft. Maggie Jones, MPH, contributed to conceptualization, data collection, and review/editing of draft manuscript. Monika Sanchez, MSc, contributed to data collection and review/editing of draft manuscript. Marguerita Lightfoot, PhD, contributed to the conceptualization, reviewing manuscript, and editing. Anda Kuo, MD, contributed to conceptualization, reviewing manuscript, and editing. Nipher Malika, PhD, MPH, contributed to the writing, reviewing, and editing. Nicole Vu Leba, PhD, contributed to conceptualization, data analyses, and writing original draft. Stephanie Williamson, BA, contributed to the data analyses and writing. Brigid McCaw, MD, contributed to the conceptualization, writing, reviewing manuscript, and editing.
Conflict of Interest: None declared
Funding: Funding for the California ACEs Learning and Quality Improvement Collaborative (CALQIC) and its evaluation was provided by the California Department of Health Care Services in partnership with the California Office of the Surgeon General.
Data-Sharing Statement: Underlying data are not available.
References
- 1.Centers for Disease Control and Prevention . Adverse Childhood Experiences [internet]. Accessed 13 March 2023. www.cdc.gov/violenceprevention/aces/index.html
- 2. Oh DL, Jerman P, Silvério Marques S, et al. . Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018;18(1):83. 10.1186/s12887-018-1037-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse Negl. 2011;35(6):408–413. 10.1016/j.chiabu.2011.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 2018;172(11):1038–1044. 10.1001/jamapediatrics.2018.2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhushan D, Kotz K, McCall J, et al. . Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health. Office of the California Surgeon General; 2020. Accessed 10 March 2023. https://osg.ca.gov/wp-content/uploads/sites/266/2020/12/Roadmap-For-Resilience_CA-Surgeon-Generals-Report-on-ACEs-Toxic-Stress-and-Health_12092020.pdf
- 6. Bassuk EL, Latta RE, Sember R, Raja S, Richard M. Universal design for underserved populations: Person-centered, recovery-oriented and trauma informed. J Health Care Poor Underserved. 2017;28(3):896–914. 10.1353/hpu.2017.0087 [DOI] [PubMed] [Google Scholar]
- 7. Raja S, Hasnain M, Hoersch M, Gove-Yin S, Rajagopalan C. Trauma informed care in medicine. Fam Community Health. 2015;38(3):216–226. 10.1097/FCH.0000000000000071 [DOI] [PubMed] [Google Scholar]
- 8. Conn A-M, Szilagyi MA, Jee SH, Manly JT, Briggs R, Szilagyi PG. Parental perspectives of screening for adverse childhood experiences in pediatric primary care. Fam Syst Health. 2018;36(1):62–72. 10.1037/fsh0000311 [DOI] [PubMed] [Google Scholar]
- 9. DiGangi MJ, Negriff S. The implementation of screening for adverse childhood experiences in pediatric primary care. J Pediatr. 2020;222:174–179. 10.1016/j.jpeds.2020.03.057 [DOI] [PubMed] [Google Scholar]
- 10.Huang LN, Flatow R, Biggs T, et al. . SAMHSA’s Concept of Truama and Guidance for a Trauma-Informed Approach. Substance Abuse and Mental Health Services Administration (SAMHSA); 2014. Accessed https://store.samhsa.gov/sites/default/files/sma14-4884.pdf
- 11. Machtinger EL, Cuca YP, Khanna N, Rose CD, Kimberg LS. From treatment to healing: The promise of trauma-informed primary care. Womens Health Issues. 2015;25(3):193–197. 10.1016/j.whi.2015.03.008 [DOI] [PubMed] [Google Scholar]
- 12. Garner A, Yogman M. Committee on; Psychosocial Aspects of Child and Family Health. Preventing childhood toxic stress: Partnering with families and communities to promote relational health. Pediatrics. 2021;148(2). 10.1542/peds.2021-052582 [DOI] [PubMed] [Google Scholar]
- 13. Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample: Associations across adverse childhood experiences levels. JAMA Pediatr. 2019;173(11):e193007. 10.1001/jamapediatrics.2019.3007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. 10.1016/j.pec.2008.11.015 [DOI] [PubMed] [Google Scholar]
- 15. Thakur N, Hessler D, Koita K, et al. . Pediatrics adverse childhood experiences and related life events screener (PEARLS) and health in a safety-net practice. Child Abuse Negl. 2020;108:104685. 10.1016/j.chiabu.2020.104685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Koita K, Long D, Hessler D, et al. . Development and implementation of a pediatric adverse childhood experiences (ACEs) and other determinants of health questionnaire in the pediatric medical home: A pilot study. PLoS One. 2018;13(12):e0208088. 10.1371/journal.pone.0208088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Felitti VJ, Anda RF, Nordenberg D, et al. . Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245–258. 10.1016/s0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 18. Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl. 2004;28(7):729–737. 10.1016/j.chiabu.2003.08.009 [DOI] [PubMed] [Google Scholar]
- 19. Pinto R, Correia L, Maia Â. Assessing the reliability of retrospective reports of adverse childhood experiences among adolescents with documented childhood maltreatment. J Fam Viol. 2014;29(4):431–438. 10.1007/s10896-014-9602-9 [DOI] [Google Scholar]
- 20. Zarse EM, Neff MR, Yoder R, et al. . The adverse childhood experiences questionnaire: Two decades of research on childhood trauma as a primary cause of adult mental illness, addiction, and medical diseases. Cogent Medicine. 2019;6(1):1581447. 10.1080/2331205X.2019.1581447 [DOI] [Google Scholar]
- 21. Ye M, Hessler D, Ford D, et al. . Pediatric ACEs and related life event screener (PEARLS) latent domains and child health in a safety-net primary care practice. BMC Pediatr. 2023;23(1):367. 10.1186/s12887-023-04163-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Council for Behavioral Health . Organizational Self-Assessment: Adoption of Trauma-Informed Care Approaches in a Primary Care Setting (TIPC-OSA). Accessed 5 March 2023. www.thenationalcouncil.org/wp-content/uploads/2022/04/OSA.pdf
- 23.Fallot RD, Harris M. Creating Cultures of Trauma-Informed Care (CCTIC): A Self-Assessment and Planning Protocol. 2009. Accessed https://children.wi.gov/Documents/CCTICSelf-AssessmentandPlanningProtocol0709.pdf
- 24.Center for Care Innovations . PICC Collaborative Change Framework [internet]. Accessed 13 March 2023. www.careinnovations.org/wp-content/uploads/5_PICC2ChangeFramework_3.20.17ihslw.pdf
- 25. Baker CN, Brown SM, Wilcox PD, Overstreet S, Arora P. Development and psychometric evaluation of the attitudes related to trauma-informed care (ARTIC) scale. School Mental Health. 2016;8(1):61–76. 10.1007/s12310-015-9161-0 [DOI] [Google Scholar]
- 26. Machtinger EL, Davis KB, Kimberg LS, et al. . From treatment to healing: Inquiry and response to recent and past trauma in adult health care. Womens Health Issues. 2019;29(2):97–102. 10.1016/j.whi.2018.11.003 [DOI] [PubMed] [Google Scholar]
- 27. Oral R, Ramirez M, Coohey C, et al. . Adverse childhood experiences and trauma informed care: The future of health care. Pediatr Res. 2016;79(1–2):227–233. 10.1038/pr.2015.197 [DOI] [PubMed] [Google Scholar]
- 28. Wathen CN, Schmitt B, MacGregor JCD. Measuring trauma- (and violence-) informed care: A scoping review. Trauma Violence Abuse. 2023;24(1):261–277. 10.1177/15248380211029399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Champine RB, Lang JM, Nelson AM, Hanson RF, Tebes JK. Systems measures of a trauma-informed approach: A systematic review. Am J Community Psychol. 2019;64(3–4):418–437. 10.1002/ajcp.12388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Purtle J. Systematic review of evaluations of trauma-informed organizational interventions that include staff trainings. Trauma Violence Abuse. 2020;21(4):725–740. 10.1177/1524838018791304 [DOI] [PubMed] [Google Scholar]
- 31. Bendall S, Eastwood O, Cox G, et al. . A systematic review and synthesis of trauma-informed care within outpatient and counseling health settings for young people. Child Maltreat. 2021;26(3):313–324. 10.1177/1077559520927468 [DOI] [PubMed] [Google Scholar]
- 32. Burstein D, Yang C, Johnson K, Linkenbach J, Sege R. Transforming practice with HOPE (healthy outcomes from positive experiences). Matern Child Health J. 2021;25(7):1019–1024. 10.1007/s10995-021-03173-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kandel ER, Schwartz JH, Jessell TM, Siegelbaum S, Hudspeth AJ, Mack S. Principles of Neural Science. 4th ed. McGraw-Hill; 2000. [Google Scholar]
- 34. Leitch L, Brigid M. Time to move forward: Resilience and trauma informed care. Perm J. 2023;23(76). 10.7812/TPP/23.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.California Academy of Family Physicians . Adverse childhood experiences (ACEs) and trauma-informed resilience-oriented care (TIRO). Accessed 10 March 2023. www.familydocs.org/aces/
- 36. Leitch L. Action steps using ACEs and trauma-informed care: a resilience model. Health Justice. 2017;5(1):5. 10.1186/s40352-017-0050-5 [DOI] [PMC free article] [PubMed] [Google Scholar]