You may be wondering, why should this special section on innovations in trauma-informed health care lead with a commentary on resilience? Or, to paraphrase an old song, “what’s resilience got to do with it?” Our hope is that, after reading this commentary, you will regard attention to resilience and its neurobiological underpinnings as an equal partner to consideration of trauma and its myriad effects on the human mind–body system. Focusing on one over the other misses the point; they are stronger together.
Recognizing that this is a critical time to set the direction of trauma-informed health care for the next decade, we framed this commentary to advocate for an intentional shift to resilience and trauma-informed care (RTIC). This framework includes attention to adversity and its sequelae, in addition to actively incorporating strengths, protective factors, and an expanded definition of resilience. The shift beyond the pathology-focused traditional biomedical model also aligns with the movement toward whole-person care and its emphasis on health promotion, well-being, and a lifelong capacity for growth and learning.
For this commentary, we will use the term “resilience” as an overarching concept that captures positive and strength-based elements inherent in other commonly used terms (eg, protective factors, positive childhood experiences, hardiness, grit, flourishing).1–5 The focus of this commentary is on individuals and families in the health care setting. However, we recognize that meaningful efforts to support resilience must occur at many levels (eg, individual, family, community, nation, ecosystem). At a societal level, these efforts face many structural impediments, will require widespread system-level changes, and deserve in-depth consideration. Though beyond the scope of this commentary, this analysis should be undertaken in future publications.
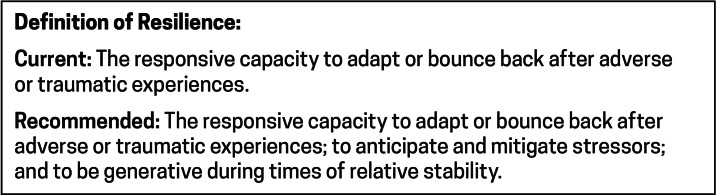
Our aim is twofold: to offer an expanded definition of resilience (Figure 1), which reflects a robust and dynamic capacity for resilience without requiring the occurrence of an adverse experience; and to recommend a new term, RTIC. This is a term that intentionally leads with resilience and aligns with current and emerging neuroscience knowledge.
Figure 1:
Leitch’s definition of resilience.
Drawing upon our combined professional experience, we have highlighted several relevant influences: the connections between adversity, health, and the development of trauma-informed care; the emerging neuroscience findings concerning neurogenesis and neuroplasticity; the role of the autonomic nervous system (ANS) in regulating responses to threat and setting conditions for resilience; and broad implications for clinical care and practice.
Our objective is to stimulate broad discussion and catalyze inclusion of resilience within clinical practice and research studies. We recognize that these recommendations may lead to debate and, in some instances, dissension, and we consider these as positive signs of a vibrant, healthy professional community whose knowledge and practice is ever-evolving.1,3–5 Working in collaboration, we welcome the opportunity to further develop and refine our understanding of RTIC.
Adversity and Health
The last 25 years have brought compelling evidence about the prevalence as well as the immediate and enduring impact of trauma and adversity across the lifespan.6 Extensive biomedical research has shown how extended exposure to overwhelming trauma (including trauma due to adverse childhood experiences and interpersonal violence as well as structural factors such as poverty, sexism, racism, community violence, and disasters) can result in a “toxic stress physiology” that increases the likelihood of multiple medical and mental health conditions.3,6,7
There is growing clinical interest in research about what mitigates the impact of trauma, facilitates recovery, and enhances resilience as well as ways to incorporate this broader perspective in patient care and institutional policies. Incorporating effective ways to identify and respond to adverse childhood experiences and other traumatic experiences as part of medical care has contributed to the development of trauma-informed care principles and implementation guidance and has accelerated its adoption.8 Although this focus on trauma has added an important lens to clinical treatment, an unintended consequence has been that less attention has been paid to the role of positive experiences and the essential role of resilience.9
The adoption of RTIC can adjust this imbalance and ensure that future workflows, patient education materials, screening forms, and data collection tools will incorporate a resilience orientation. It will promote the necessary training for health professionals across their career, and will include education on both resilience and trauma, leading to the development of guidance for implementing RTIC throughout health care. It is essential to underscore the institutional changes in clinic policies and practice that will be needed to support and sustain RTIC.
A focus that includes a resilience orientation provides a far richer and more accurate understanding of an individual and/or their family, as it includes their strengths, challenges, and needs.3,5,10 We believe it also enhances the development of a stronger therapeutic and more-trusting relationship between patient and practitioner as well as having a positive impact on the treatment plan.
Contributions to the Understanding of Resilience
Although not as familiar to medical clinicians, academic inquiry into the science of resilience has been active for many decades. It builds on research from multiple disciplines and explores aspects of individual, family, and community resilience.1–5,10–12 Masten, a developmental psychologist and leader in the field, describes 4 waves of resilience research.12 The first 3 waves focused on describing resilience and how to measure it; what factors or processes lead to resilience and how they work; and whether interventions can promote resilience. The fourth wave, now underway, is characterized by dynamic system-oriented approaches and incorporates neurobiology, the interaction of genetics and experiences, environmental factors, and cultural and intergenerational contexts.
Findings from research on resilience have already contributed to establishing the importance of safe, stable, and nurturing relationships for children and other protective factors that can inform social policy and clinical practice.3,13 The research is also influencing approaches to mental health that go beyond symptom reduction and include the promotion of well-being.2,11,14–16
Advances in neuroscience, including refinements in neuroimaging capabilities and interpretations (eg, functional magnetic resonance imaging (fMRI)), have generated a cascade of scientific detail about the intricate wiring of the human mind–body system and its lifelong capacity for resilience via growth and learning. These, in turn, are leading to practices and interventions that are resilience-informed and can be incorporated into medical practice.11,15 Below we provide a few salient examples.
Neurogenesis and Neuroplasticity
Neuroscience research shows that 2 key processes, neurogenesis (ie, growth of new neurons in response to learning) and neuroplasticity (ie, the brain’s ability to change through growth and reorganization based on individual experience), underlie the brain’s responsiveness to adaptation and change from life’s experiences in both positive and negative ways.15–17 An example of these processes in action comes from research into the health benefits of attention management programs that were conducted with individuals experiencing a wide range of health challenges. Attention management, the process of consciously focusing attention, underlies approaches such as mindfulness, meditation, and gratitude practices as well as skill-based approaches. As patients learn and practice these methods, they can better manage pain and other physical and emotional stressors.7,14,16
In the past decade, programs have emerged that do not rely on meditation or mindfulness practices, that teach practical, attention-based skills that can be used by anyone, and that are particularly useful for individuals who are not likely to use meditation.16–18 Both mindfulness and skills-based models show that the dynamic capacity for individual change, through the management of attention, can become a core competency. Routine practice strengthens nervous system function and is the basis for deepening resilience and decreasing reactivity to stressful and demanding experiences.
The ANS
The ANS is a key element in understanding how the mind–body system responds to threat and fear.7,15,17,19 The ANS controls a broad range of internal processes, including blood pressure, heart rate, body temperature, and digestion. It also plays an essential role in building the capacity for deeper resilience by an individual’s active attention to management of reactivity.
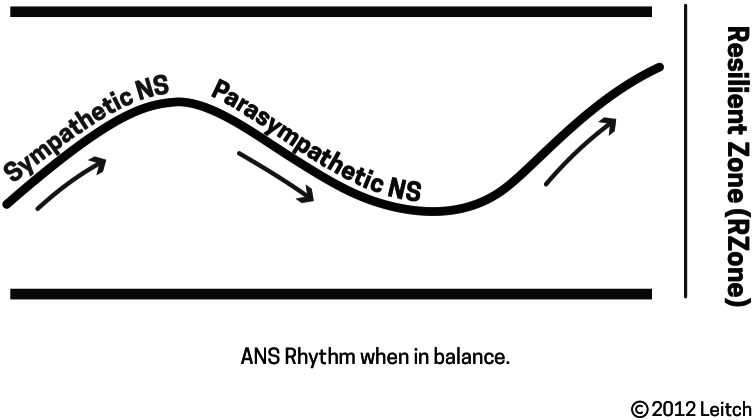
The ANS consists of 2 branches, the sympathetic branch and the parasympathetic branch. Simply put, one is primarily an activator (sympathetic) and the other is primarily a calmer (parasympathetic). Figure 2 shows the ANS rhythm when it is in balance, which can be called the resilient zone.
Figure 2:
Autonomic nervous system rhythm when in balance. ANS = autonomic nervous system; NS = nervous system.
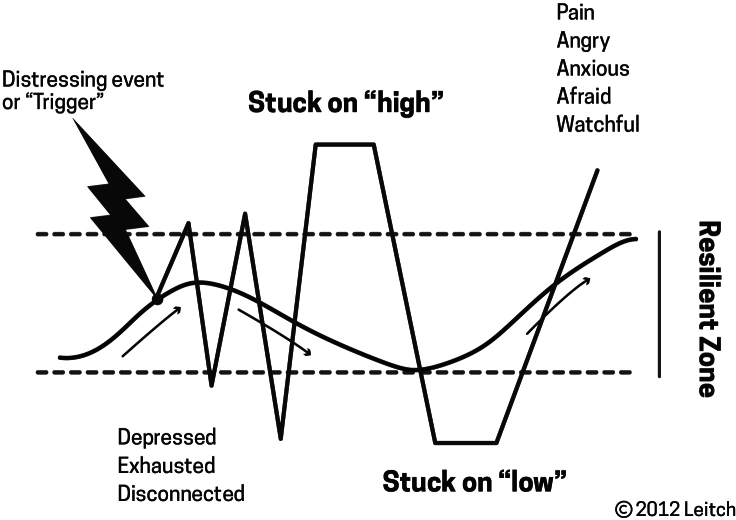
Individuals of all ages can learn how to track the sensory rhythm of the 2 ANS branches and then learn to self-regulate the rhythm by shifting their attention between activation and calming.1,2 They can identify when there is an excess of sympathetic or parasympathetic activation (Figure 3) from threat-induced body states. They can learn cognitively and experientially how to modify their responses.
Figure 3:
Disruption of the resilient zone.
Autonomic arousal states bias emotional behavior and influence memory as well as physical and psychological processes. When the balance of ANS branches is well-regulated, other key levels of functioning improve. Body functions (such as heart rate, blood flow, breathing, and digestion) are stable; thought processes are clearer and more organized; memory and decision making improve; emotions are more manageable; and social behaviors are more constructive.17,18
The Role of Attention Management
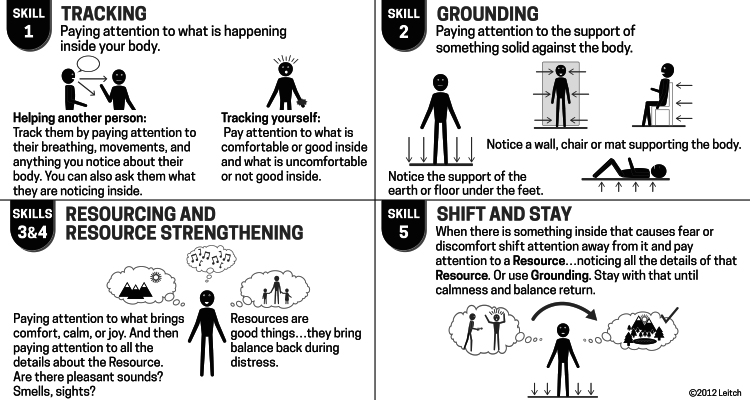
The power of learning to manage one’s attention to improve health outcomes and build resilience was initially demonstrated in mindfulness/meditation practices and, more recently, has included skills-based practices in which individuals learn ways to track and manage their level of nervous system activation, learning to stay in or return to stable nervous system functioning. Practice of attention management methods over time leads to a deepening of resilience due to neuroplasticity. This stable band of nervous system functioning has been referred to as the window of tolerance19 or as being in the resilient zone.9 Examples are easily learned practices, such as breath exercises and the self-regulation skills shown on Leitch’s self-regulation skills card (Figure 4). The skills are based in part on the work of Peter A Levine.20
Figure 4:
Self-regulation skills.
Evidence-informed tools, which support nervous system regulation and mindfulness via attention management, are resources that can be offered to any patient and family member. Presented as an opportunity to learn how their mind and body work together in support of better physical and emotional functioning, they also provide a highly relevant supportive approach for those with experiences of trauma or challenging medical conditions. Other benefits of self-regulation skills are building stronger therapeutic relationships and facilitating personal well-being and professional satisfaction among clinic staff.
Next Steps
We hope this commentary mobilizes the widespread adoption of a RTIC approach that reflects the scientific advances over the past decade and drives a commitment to the substantial system-level changes that are necessary to integrate these principles into clinical practice. RTIC is appropriate for all patients, not just those with a history of trauma, and is well aligned with the national initiative on whole-person care. Essential next steps include:
Incorporating the science of both trauma and resilience into the education and training of all health care staff
Balancing attention to trauma with a commensurate focus on a strength-based and resilience-oriented design of screening and assessment tools, workflows, interventions, educational materials, and policies11
Developing evidence-informed clinical tools, interventions, practices, and policies along with outcome measures and program evaluations that can foster resilience-oriented practices1,3,4
Including a resilience focus and multidisciplinary clinical and research partnerships.1,2,12
We want to reemphasize that a focus on individual resilience is not sufficient. Clinicians must be active partners in a broader public health approach that supports all levels of resilience (individual, family, community, state, nation, and environment).3,5,10,12,21 Medical science and clinicians have played a unique and important role in understanding, recognizing, and responding to trauma and its impact across the entire lifespan. Now, a corresponding role and vital investment are greatly needed as we shift to RTIC, a model which will build upon and amplify the existing benefits derived from the trauma-informed care model.
As you read the other contributions in this special section of the Journal, we hope you will join us in imagining how, working together, we can make necessary changes to create a robust and generative system of RTIC to support health, healing, and equity and inclusion.
Footnotes
Author Contributions: Laurie Leitch, PhD, participated in the drafting, writing, and review of the manuscript. Brigid McCaw, MD, MS, MPH, participated in the drafting, writing, review, and submission of the manuscript. Each author gives final approval to the manuscript.
Conflicts of Interest: None declared
Funding: None declared
References
- 1. Chmitorz A, Kunzler A, Helmreich I, et al. Intervention studies to foster resilience - A systematic review and proposal for a resilience framework in future intervention studies. Clin Psychol Rev. 2018;59:78–100. 10.1016/j.cpr.2017.11.002 [DOI] [PubMed] [Google Scholar]
- 2. Bonanno GA, Romero SA, Klein SI. The temporal elements of psychological resilience: An integrative framework for the study of individuals, families, and communities. Psychological Inquiry. 2015;26(2):139–169. 10.1080/1047840X.2015.992677 [DOI] [Google Scholar]
- 3. Shonkoff JP, Boyce WT, Levitt P, Martinez FD, McEwen B. Leveraging the biology of adversity and resilience to transform pediatric practice. Pediatrics. 2021;147(2): e20193845. 10.1542/peds.2019-3845 [DOI] [PubMed] [Google Scholar]
- 4. Masten AS, Barnes AJ. Resilience in children: Developmental perspectives. Children (Basel). 2018;5(7):98. 10.3390/children5070098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ungar M, ed. Multisystemic Resilience: Adaptation and Transformation in Contexts of Change. New York: Oxford Academic; 2021. 10.1093/oso/9780190095888.001.0001 [DOI] [Google Scholar]
- 6. Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–e366. 10.1016/S2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- 7.Bhushan D, Kotz K, McCall J, et al. Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health. Sacramento: Office of the California Surgeon General; 2020. [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration (SAMHSA) . SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. HHS Publication No. (SMA) 14-4884. Rockville, MD: SAMHSA; 2014. [Google Scholar]
- 9. Leitch L. Action steps using ACEs and trauma-informed care: A resilience model. Health Justice. 2017;5(1):5. 10.1186/s40352-017-0050-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McEwen CA, McEwen BS. Social structure, adversity, toxic stress, and intergenerational poverty: An early childhood model. Annu Rev Sociol. 2017;43(1):445–472. 10.1146/annurev-soc-060116-053252 [DOI] [Google Scholar]
- 11. Weems CF, Russell JD, Herringa RJ, Carrion VG. Translating the neuroscience of adverse childhood experiences to inform policy and foster population-level resilience. Am Psychol. 2021;76(2):188–202. 10.1037/amp0000780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Masten AS. Resilience in developing systems: Progress and promise as the fourth wave rises. Dev Psychopathol. 2007;19(3):921–930. 10.1017/S0954579407000442 [DOI] [PubMed] [Google Scholar]
- 13. Burstein D, Yang C, Johnson K, Linkenbach J, Sege R. Transforming practice with HOPE (healthy outcomes from positive experiences). Matern Child Health J. 2021;25(7):1019–1024. 10.1007/s10995-021-03173-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goyal M, Singh S, Sibinga EMS, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–368. 10.1001/jamainternmed.2013.13018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McEwen BS. The neurobiology of stress: From serendipity to clinical relevance. Brain Res. 2000;886(1–2):172–189. 10.1016/s0006-8993(00)02950-4 [DOI] [PubMed] [Google Scholar]
- 16. Davidson RJ, McEwen BS. Social influences on neuroplasticity: Stress and interventions to promote well-being. Nat Neurosci. 2012;15(5):689–695. 10.1038/nn.3093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stanley EA. Widen the window: Training your brain and body to thrive during stress and recover from trauma. New York: Penguin Random House; 2019. [Google Scholar]
- 18.Leitch L. Brain Gain: Timely tools to tackle life’s heavy lifting. Austin, TX: Lioncrest Publishing; 2023. [Google Scholar]
- 19.Siegel DJ. The developing mind: Toward a neurobiology of interpersonal experience. New York: Guilford Press; 1999. [Google Scholar]
- 20. Payne P, Levine PA, Crane-Godreau MA. Somatic experiencing: Using interoception and proprioception as core elements of trauma therapy. Front Psychol. 2015;6:93. 10.3389/fpsyg.2015.00093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rog DJ, Reidy MC, Manian N, Daley TC, Lieberman L. Opportunities for psychologists to enact community change through adverse childhood experiences, trauma, and resilience networks. Am Psychol. 2021;76(2):379–390. 10.1037/amp0000778 [DOI] [PubMed] [Google Scholar]