Abstract
Introduction and importance
Highly differentiated follicular carcinoma of the ovary (HDFCO) is a rare type of thyroid carcinoma originating from struma ovarii, consisting of benign-appearing thyroid follicles spread outside the ovarian tissue.
Case presentation
We present a 22-year-old girl who underwent left salpingo-oophorectomy, omental, and peritoneal biopsies for a complex left ovarian mass. Microscopic examination and Immunohistochemical staining led to the diagnosis of HDFCO with tumor deposits affecting the omental and peritoneal biopsies. The patient was counseled about the nature of her disease and the recommended treatment. Thyroidectomy was performed later, revealing a normal thyroid gland. The patient received an ablative dose of radioactive iodine (150 mci) and a suppressive dose of levothyroxine. This is one of the youngest reported patients ever.
Clinical discussion
To our knowledge, the patient presented in this case report is one of the youngest patients ever reported in the literature. In the recent WHO Classification of Female Genital Tumors, the term highly differentiated follicular carcinoma arising from struma ovarii (HDFCO) was introduced, to emphasize its low-grade malignant behavior. Due to its rare incidence, there is no standard treatment strategy, but a plan based on surgical intervention is suggested.
Conclusion
Malignant struma ovarii should be put in the differential diagnosis in young patients with suspicious ovarian masses. Adequate patient counseling remains a cornerstone in the journey of management.
Keywords: Ovary, Thyroid, Struma ovarii, Counseling
Highlights
-
•
Highly differentiated follicular carcinoma of the ovary (HDFCO) is a rare thyroid carcinoma originating from struma ovarii.
-
•
HDFCO has a metastatic potential, so it is considered a biologically malignant tumor.
-
•
Treatment includes surgical resection followed by thyroidectomy and radioactive iodine therapy.
-
•
Adequate patient counseling remains a cornerstone in the journey of management.
1. Introduction
Struma ovarii is a rare ovarian tumor that is considered a monodermal teratoma. It literally means “ovarian goiter.” The mere presence of ectopic thyroid tissue in the dermoid cyst does not mean it can be nominated as struma ovarii except if it occupies more than 50 % of the tumor [1]. Thyroid tissue can be found in up to 20 % of ovarian teratomas, but struma ovarii make up less than 5 % of teratomas [2].
More rarely, the thyroid tissue in struma ovarii shows malignant transformation which is a diagnostic challenge due to the absence of specific imaging and laboratory criteria. The most diagnosed type is papillary thyroid carcinoma [1] which constitutes the majority of the incidence, followed by follicular thyroid carcinoma then the mixed type. Other types of thyroid cancer like anaplastic and medullary carcinoma are extremely rarely reported making the epidemiology and pathological types incidence not the same as that of thyroid cancer. The prognosis also is not the same; while differentiated thyroid cancer has an excellent prognosis and very low mortality rate, malignant struma ovarii has a good prognosis also but is relatively worse than differentiated thyroid cancer (mortality rate of 4 % vs 0.5:100,000) [3].
Highly differentiated follicular carcinoma of the ovary (HDFCO) is a rare type of thyroid carcinoma originating from struma ovarii, consisting of benign-appearing thyroid follicles spread outside the ovarian tissue. Because of this metastatic potential, it is considered a biologically malignant tumor [4].
In this case report, we present a 22-year-old girl who was diagnosed with a left ovarian highly differentiated follicular thyroid carcinoma with peritoneal and omental involvement. The patient later received radioactive iodine after surgical removal of the thyroid gland.
2. Case presentation
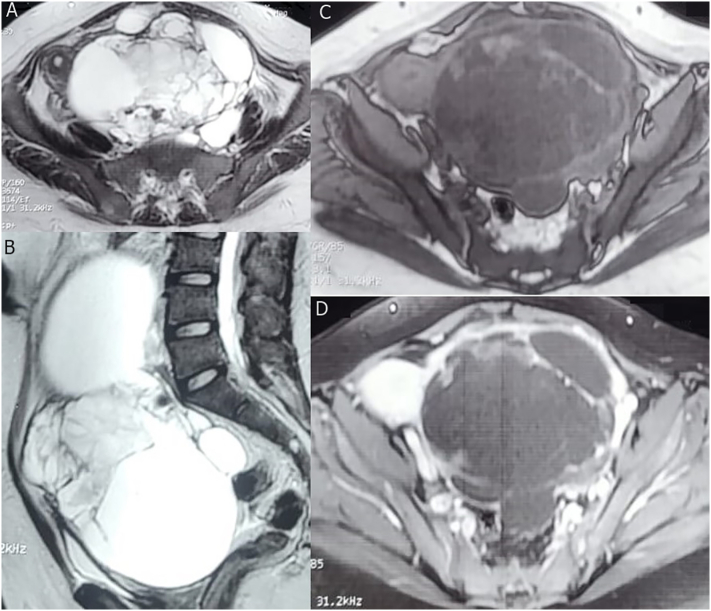
A 22-year-old girl was presented to our center outpatient clinic with a 3-week history of left iliac fossa pain radiating to the suprapubic region, and hypomenorrhea (1–2 days). She also had a history of bone aches for 2 years; for which she was previously diagnosed with osteoporosis. The patient has a positive family history of lung cancer. Physical examination revealed a palpable lower abdominal mass of about 20 cm associated with tenderness, with no palpable inguinal or supraclavicular LNs. Laboratory investigations were within normal range apart from mild elevated CA-125 60.9 U/ml and CA-19-9 61.44 U/ml. However, CEA, AFP, B-HCG, and Serum LDH were normal. Pelviabdominal ultrasound revealed a huge multicystic pelviabdominal lesion extending to the epigastrium measuring (>14 × 10 cm). Post-contrast pelvis MRI Pelvis (Fig. 1) revealed a huge midline multi-locular pelviabdominal left ovarian cystic mass that measured about 14.6 × 16.8 × 23.3 cm (AP × TR × HT). Anteriorly: it was seen abutting the inner anterior abdominal wall. Posteriorly: it was seen as related to the Psoas muscles and lumbar vertebrae. It was markedly compressing and displacing the normal-sized uterus to the right side. It was seen compressing and displacing the urinary bladder anteriorly. Its upper end was seen reaching the level of the lower pole of the right kidney. A normal right ovary was seen displaced to the right iliac region. Chest non-contrast CT was done and was free from any abnormalities.
Fig. 1.
MRI of the ovarian mass. (A & B) Axial and sagittal T2 weighted images revealed a large midline pelviabdominal complex cystic lesion with thick internal septae displacing the uterus to the right side and the urinary bladder inferiorly, with no signs of invasion. (C) Axial precontrast and (D) post-contrast T1 weighted images revealed a thick wall and septal enhancement. No pathological pelvic LNs nor ascites.
Fertility-sparing surgery was decided. The patient underwent surgical exploration through a lower midline incision, and a large left ovarian mass was noted, with free peritoneal, omental, and visceral surfaces from any suspicious deposits. Left salpingo-oophorectomy was performed in addition to omental and peritoneal biopsies. The patient tolerated the procedure well and was discharged after 48 h.
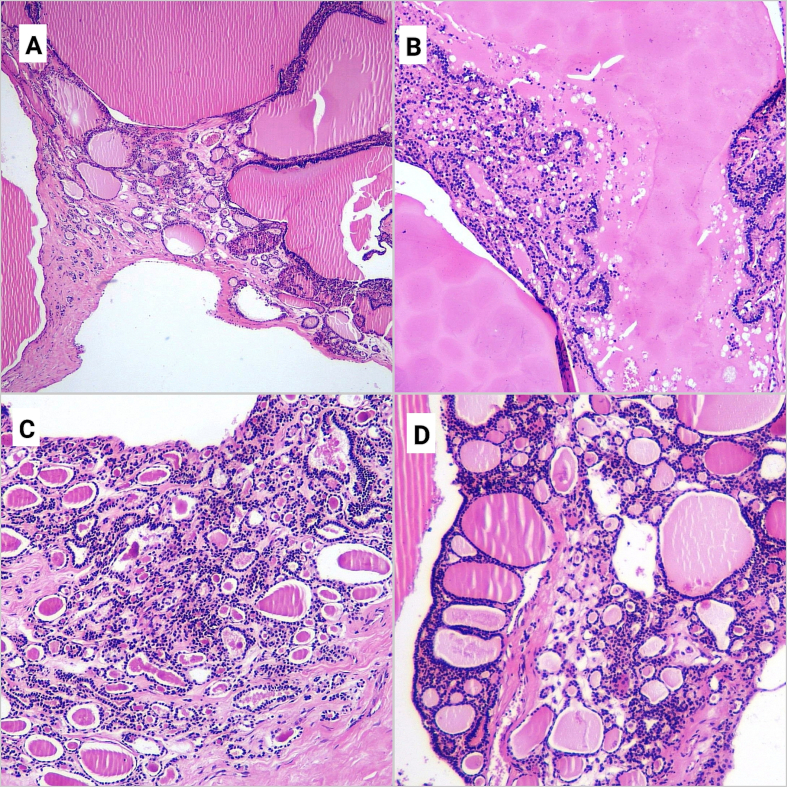
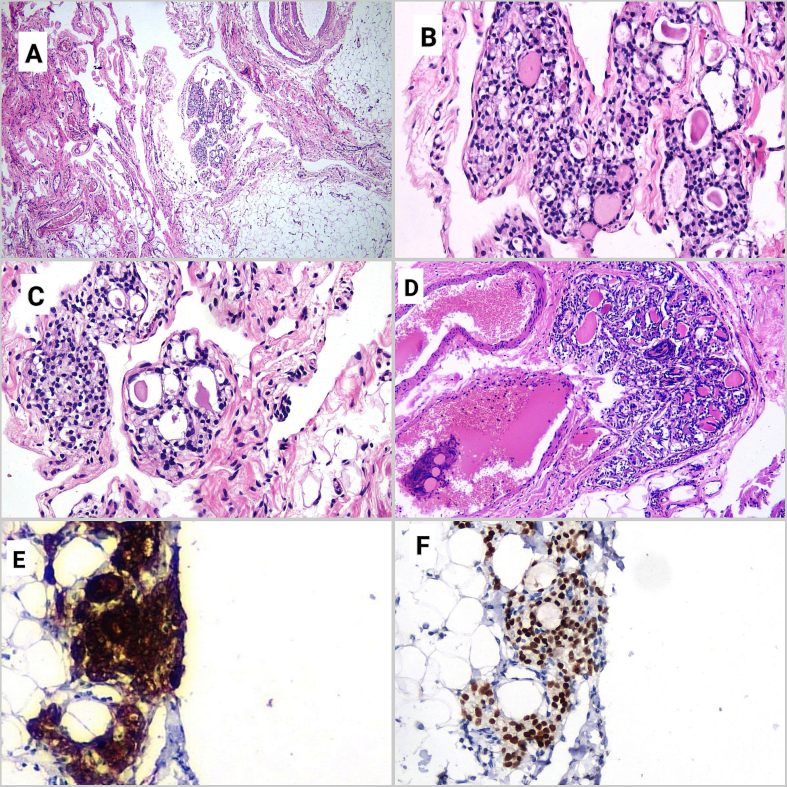
Gross examination of the excised mass revealed a 17 × 13 × 4 cm swelling which was formed of a multilocular cystic structure with a thin wall, filled with clear fluid mixed with gelatinous brown to green material. Microscopic examination (Fig. 2) revealed neoplastic proliferation composed of multiple nodules of thyroid tissue that were formed of variably sized macro and microfollicles. These were lined by cuboidal to columnar epithelial cells, filled with colloid. Secondary changes were detected in the form of fibrosis, infarction, hemorrhage, and calcification. No vascular invasion was detected. Microscopic examination (Fig. 3) of the omental and peritoneal biopsies which were grossly normal revealed microscopic deposits formed of small-sized thyroidal follicles lined by cuboidal follicular cells and contained colloid. Immunohistochemical studies (IHC) revealed a positive nuclear reaction for TTF1 and a positive cytoplasmic reaction for Thyroglobulin in tumor cells. Because of the histologically innocent appearance of the ovarian tumor, resembling colloid goiter, the diagnosis of highly differentiated follicular carcinoma (thyroid type) arising in struma ovarii with tumor deposits affecting the omental and peritoneal biopsies.
Fig. 2.
Microscopic examination of the ovarian mass: It showed multiple thyroid follicles variable in size and shape, lined by bland follicular cells, and filled with colloid (H&E, ×40, ×100, ×100, and ×100 respectively).
Fig. 3.
Microscopic examination of the omentum and peritoneal biopsy: Microscopic images from the sections taken from the omentum (A, B, C) revealed microscopic deposits of small thyroid follicles, lined by cuboidal cells, some of them containing colloid. (H&E, ×40, ×200 and ×200 respectively). Microscopic image from the peritoneal biopsy (D) showed a deposit of thyroid follicles, (H&E, ×100). Immunohistochemistry for thyroglobulin (E) showed a positive reaction in the omental deposits (Thyroglobulin, ×200). Immunohistochemistry for TTF1 (F) showed a positive reaction in the omental deposits (TTF1, ×200).
The patient's case was discussed at the hospital multidisciplinary team (MDT) meeting and The International Gynecologic Cancer Society - Pan-Arabian Research Society of Gynecological Oncology (IGCS-PARSGO) online tumor board which agreed on the pathological diagnosis and recommended a fertility-sparing strategy with possible thyroidectomy to facilitate the intake of radioactive iodine.
On her next follow-up in the outpatient clinic, the patient was counseled about the nature of her disease. She was in need of deep understanding that she had an ectopic thyroid tissue in her ovaries which developed a tumor with extra ovarian spread and that her tumor was not metastatic from a primary thyroid carcinoma or a primary epithelial ovarian tumor. She has also to understand the recommended plan of treatment as well as the justification of thyroidectomy in such a normal gland. Thyroidectomy was performed later, and the post-operative pathological examination revealed a normal thyroid gland with no evidence of tumor tissue.
The patient was referred to the clinical oncology department for further management. After evaluation of the patient's data, they decided to proceed with receiving an ablative dose of radioactive iodine (150 mci) and a suppressive dose of levothyroxine. The patient is well and free from any metastasis till the time of writing the case report which is eight months from the operation date. Her serum thyroglobulin was normal during her follow-up. This work has been reported in line with the SCARE criteria [5].
3. Discussion
In this case report, we presented a 22-year-old girl with a highly differentiated follicular thyroid carcinoma on top of struma ovarii with peritoneal and omental microscopic metastasis. To our knowledge, the patient presented in this case report is one of the youngest patients ever reported in the literature [6].
Struma ovarii is histologically composed of normal or benign-looking hyperplastic thyroid tissue. Roth and Karseladze were the first to describe the entity of HDFCO. Histologically, it resembles struma ovarii and is composed of ordinary thyroid tissue or adenomatous nodule but has extra ovarian dissemination. Both the ovarian and extra ovarian disease had the innocent-looking appearance of non-neoplastic thyroid tissue, so this entity cannot be diagnosed until the neoplasm spreads beyond the ovary [4].
In comparison to the typical thyroid-type carcinoma with an extra ovarian spread that is relatively easy to diagnose, those cases with an innocent look represent a challenge at the diagnostic level and regarding the terminology. All these cases were named in literature as “peritoneal strumosis” because of the absence of histological features of malignancy [4]. In the recent WHO Classification of Female Genital Tumors, the term highly differentiated follicular carcinoma arising from struma ovarii (HDFCO) was introduced, to emphasize its low-grade malignant behavior [7].
The differential diagnosis of HDFCO includes typical thyroid-type carcinomas. The absence of nuclear features of papillary thyroid carcinoma, such as nuclear clearing, grooving, and pseudo inclusions preclude this diagnosis. Regarding Follicular carcinoma arising in struma ovarii, the diagnosis requires vascular and capsular invasion. Application of this to the ovary is difficult [8]. The ovarian tumor in this case showed no definite capsule. Vascular invasion was not found. Metastasis from thyroid primary was excluded, as there were no thyroid nodules, and her thyroid function tests showed no abnormalities.
In the presented patient, omental and peritoneal microscopic infiltration was noted, and the diagnosis of the primary tumor in addition to the metastatic sites was confirmed by immunohistochemistry as well.
Due to its rare incidence, there is no standard treatment strategy, but a plan based on surgical intervention, total thyroidectomy, and radioactive iodine (especially for advanced stages) is suggested. Fertility-preserving approaches are followed in young women who are still seeking fertility [3,9]. This strategy was followed exactly in our reported patient after MDT discussion and online international tumor board evaluation. This may be considered a type of overtreatment, but for example, papillary thyroid cancer with lymph node involvement at such an age has an excellent prognosis, but it is treated in the same aggressive way, by surgery, neck dissection, and RAI. In our particular patient, in the absence of specific guidelines, we followed the guidelines of thyroid cancer management and did not follow a personal opinion but the decisions of eminent MDTs on the local and international levels. This is the best-recommended treatment approach according to the best available evidence [10].
Another point to be noted is to highlight the importance of good patient counseling in two points; the first is how to explain the disease to the patient and how to make her understand that you have a malignant thyroid tumor in your ovary, and the second one is that you need to be re-operated on to remove the thyroid gland despite it is not the site of the primary tumor.
4. Conclusion
Despite being rare, malignant struma ovarii should be put in the differential diagnosis in young patients with suspicious ovarian masses. Even though papillary thyroid cancer is the commonest subtype, highly differentiated follicular thyroid carcinoma also has a place. The best-suggested treatment strategy includes optimal surgical resection followed by thyroidectomy and radioactive iodine therapy. Adequate patient counseling remains a cornerstone in the journey of management.
CRediT authorship contribution statement
All authors have read and approved the manuscript. AN: data collection and editing OH: conceptualization, writing & revision AhH: conceptualization. GS: preparation of the radiology part, AmH, RT: preparation of the pathology part.
Declaration of competing interest
All authors declare they have no conflict of interest.
Acknowledgments
Acknowledgment
N/A.
Ethics approval and consent to participate
All procedures performed in the study involving human participants followed the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publication
Available on request.
Funding
No funding was received.
Data availability
All the clinical, radiological & pathological data used in this manuscript are available on the Mansoura University medical system (Ibn Sina Hospital management system). http://srv137.mans.edu.eg/mus/newSystem/.
References
- 1.Addley S., Mihai R., Alazzam M., Dhar S., Soleymani majd H. Malignant struma ovarii: surgical, histopathological and survival outcomes for thyroid-type carcinoma of struma ovarii with recommendations for standardising multi-modal management. A retrospective case series sharing the experience of a single institution over 10 years. Arch. Gynecol. Obstet. 2021;303(4):863–870. doi: 10.1007/s00404-021-05969-0. Available from: [DOI] [PubMed] [Google Scholar]
- 2.Wolff E.F., Hughes M., Merino M.J., Reynolds J.C., Davis J.L., Cochran C.S., et al. Expression of benign and malignant thyroid tissue in ovarian teratomas and the importance of multimodal management as illustrated by a BRAF-positive follicular variant of papillary thyroid cancer. Thyroid®. 2010 Aug 18;20(9):981–987. doi: 10.1089/thy.2009.0458. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cui Y., Yao J., Wang S., Zhao J., Dong J., Liao L. The clinical and pathological characteristics of malignant struma ovarii: an analysis of 144 published patients. Front. Oncol. 2021:11. doi: 10.3389/fonc.2021.645156. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roth L.M., Karseladze A.I. Highly differentiated follicular carcinoma arising from struma ovarii: a report of 3 cases, a review of the literature, and a reassessment of so-called peritoneal strumosis. Int. J. Gynecol. Pathol. 2008;27(2):213–222. doi: 10.1097/PGP.0b013e318158e958. [DOI] [PubMed] [Google Scholar]
- 5.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsukada T., Yoshida H., Ishikawa M., Asami Y., Shiraishi K., Kato T. Malignant struma ovarii presenting with follicular carcinoma: a case report with molecular analysis. Gynecol. Oncol. Rep. 2019;30 doi: 10.1016/j.gore.2019.100498. https://www.sciencedirect.com/science/article/pii/S2352578919300876 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.W H O Classification of Tumours Editorial Board . International Agency for Research on Cancer, World Health Organization; 2020. Female Genital Tumours [Internet]https://tumourclassification.iarc.who.int/ [cited 2023 Nov 10]. Available from: [Google Scholar]
- 8.Robboy S.J., Shaco-Levy R., Peng R.Y., Snyder M.J., Donahue J., Bentley R.C., et al. Malignant struma ovarii: an analysis of 88 cases, including 27 with extraovarian spread. Int. J. Gynecol. Pathol. 2009;28(5):405–422. doi: 10.1097/PGP.0b013e3181a27777. [DOI] [PubMed] [Google Scholar]
- 9.Li S., Yang T., Xiang Y., Li X., Zhang L., Deng S. Clinical characteristics and survival outcomes of malignant struma ovarii confined to the ovary. BMC Cancer. 2021;21(1):383. doi: 10.1186/s12885-021-08118-7. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giovannopoulou E., Saliaris K., Kavoura E., Pavlakis K., Lathouras K. Highly differentiated follicular carcinoma of ovarian origin: a systematic review of the literature. Curr. Oncol. 2022;29(12):9105–9116. doi: 10.3390/curroncol29120712. https://www.mdpi.com/1718-7729/29/12/712 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the clinical, radiological & pathological data used in this manuscript are available on the Mansoura University medical system (Ibn Sina Hospital management system). http://srv137.mans.edu.eg/mus/newSystem/.