Abstract
Background:
National trends in syphilis rates among females delivering newborns are not well characterized. We assessed 2010–2014 trends in syphilis diagnoses documented on discharge records and associated factors among females who have given birth in US hospitals.
Methods:
We calculated quarterly trends in syphilis rates (per 100,000 deliveries) by using International Classification of Diseases, Ninth Revision, Clinical Modification codes on delivery discharge records from the National Inpatient Sample. Changes in trends were determined by using Joinpoint software. We estimated relative risks (RR) to assess the association of syphilis diagnoses with race/ethnicity, age, insurance status, household income, and census region.
Results:
Overall, estimated syphilis rates decreased during 2010–2012 at 1.0% per quarter (P < 0.001) and increased afterward at 1.8% (P < 0.001). The syphilis rate increase was statistically significant across all sociodemographic groups and all US regions, with substantial increases identified among whites (35.2% per quarter; P < 0.001) and Medicaid recipients (15.1%; P < 0.001). In 2014, the risk of syphilis diagnosis was greater among blacks (RR, 13.02; 95% confidence interval [CI], 9.46–17.92) or Hispanics (RR, 4.53; 95% CI, 3.19–6.42), compared with whites; Medicaid recipients (RR, 4.63; 95% CI, 3.38–6.33) or uninsured persons (RR, 2.84; 95% CI, 1.74–4.63), compared with privately insured patients; females with the lowest household income (RR, 5.32; 95% CI, 3.55–7.97), compared with the highest income; and females in the South (RR, 2.42; 95% CI, 1.66–3.53), compared with the West.
Conclusions:
Increasing syphilis rates among pregnant females of all backgrounds reinforce the importance of prenatal screening and treatment.
Undiagnosed and untreated syphilitic infection (caused by the spirochete Treponema pallidum subspecies pallidum) during pregnancy has been linked to spontaneous abortions, stillbirth, and neonatal deaths.1,2 Among newborns who survive, congenital syphilis has been associated with deformation of bones or nasopharyngeal tissue, enlargement of internal organs (eg, liver or spleen), blood disorders (eg, leukocytosis, anemia, or thrombocytopenia), and skin conditions (eg, petechiae, mucocutaneous lesions, or jaundice).1,3 If untreated, children infected with T. pallidum can also experience ocular manifestations, auditory abnormalities, dental dystrophies, or central nervous system disorders.1,3 Although the sequelae can be severe, vertical transmission of T. pallidum from an infected female to the fetus can be effectively prevented. When diagnosed during pregnancy, syphilis can be cured with a regimen of penicillin G that is appropriate for the syphilis stage.4
Syphilis prevalence among females who delivered a newborn in the United States has not been comprehensively described in the literature. Williams et al5 analyzed data from the Centers for Disease Control and Prevention’s (CDC) National Notifiable Diseases Surveillance System and reported the annual number of syphilis cases among US females who were known to be pregnant during 2012–2014. However, that study might have underestimated the prevalence among all pregnant females, because approximately 30% of reported syphilis cases among females had an unknown pregnancy status.5 Other reports have described syphilis rates among females of reproductive age.6–8 However, those reports did not address pregnancy status. In addition, those reports were limited to reported cases of primary and secondary syphilis6–8 and did not include females with early latent or late latent infection. Because fetuses can acquire syphilis transplacentally during any stage of maternal syphilis,9 these reports are of limited value in estimating burden of disease among pregnant women. Our study uses a nationally representative sample of hospitalizations that captures syphilis diagnoses of any stage to estimate national trends in syphilis among pregnant females who delivered a live born or stillborn neonate. We also describe sociodemographic characteristics of those females who gave birth and identify characteristics of women who were more likely to have a syphilis diagnosis recorded. Understanding trends in syphilis among pregnant women and those at greater risk for infection will inform the gaps and services critical for preventing mother-to-child transmission of T. pallidum (eg, timely diagnosis and treatment of pregnant females with syphilis or presumptive treatment of their partners).1,6,10
MATERIALS AND METHODS
Data Source
We analyzed the 2010–2014 data from the National (Nationwide) Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), provided by the US Department of Health and Human Services’ Agency for Healthcare Research and Quality.11 National (Nationwide) Inpatient Sample represents more than 96% of all US hospital discharges. Each year of NIS data contains 7–8 million unweighted discharges representing 35–39 million discharges when weighted, which allows for analyses of rare conditions and special patient populations. For each hospital stay, NIS included up to 25 diagnoses during 2010–2013, up to 30 diagnoses during 2014, and patient sociodemographic characteristics for all years (eg, insurance status, income, age, race/ethnicity, and census region).
In 2012, NIS changed its sampling strategy from selecting a random sample of 20% of US hospitals to sampling 20% of discharges across all US hospitals.12 Additionally, NIS switched from weights based on hospital admissions to weights based on discharges. The new sampling and weighting strategies resulted in a onetime decrease in discharge counts by approximately 4%.11 To make the discharge counts comparable across all years, we used the revised 2010–2011 NIS trend weights.13 Because NIS eliminates all patient and state identifiers,11 the data do not meet the federal definition of “human subjects” as defined in 45 CFR 46.102.14 Consequently, institutional review board approval was not required.
Study Population, Case Definition, and Sociodemographic Variables
The study population included all females with discharges that indicated a delivery of a live-born or stillborn neonate with the Medicare Severity Diagnosis Related Group15 codes 765–768 or with diagnoses codes V27.x, 650, 640.0x–649.8x, (where x = 1 or 2), 651.0x–676.9x (where x = 1 or 2), 678.01, 678.11, or 679.0x–679.1x (where x = 1 or 2) from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9).16
The case definition of maternal syphilis included the following ICD-9 codes: 091.x (primary and secondary infection), 092.x (early latent infection), 093.x-095.x (cardiovascular syphilis, neurosyphilis, or other forms of latent syphilis with symptoms), 096.x (late latent infection), 097.x (unspecified syphilis), or 647.0x (syphilitic infections complicating pregnancy, childbirth, or the puerperium).17–19 Such diagnoses could have included cases of active syphilitic infection (ie, confirmed diagnoses obtained during a hospitalization or during pregnancy), presumptive diagnoses not confirmed at the time of hospital discharge, or history of syphilis during pregnancy among females who have received adequate treatment before delivery.
We assessed sociodemographic factors previously reported to be associated with syphilis among pregnant females.6,8,20 Sociodemographic variables included primary expected insurer, race/ethnicity, age, median annual household income (AHI) for patient’s zip code, and census region. Primary expected payer was represented by Medicaid, Medicare, private insurance (eg, Blue Cross, commercial carriers, private health maintenance organizations, and preferred provider organizations), and uninsured patients (ie, self-pay or no charge). Because the unweighted number of expectant females with a syphilis diagnosis enrolled in government programs (eg, Worker’s Compensation, CHAMPUS, or CHAMPVA) did not exceed 10 patients per year, we combined the uninsured and government insurance categories. Patient demographics included race/ethnicity (white, black, Hispanic, other, or missing/invalid), age at delivery (ie, 13–24, 25–34, or ≥35 years), and median AHI for patient’s zip code.21 Location was represented by 4 census regions (ie, Northeast, Midwest, South, and West).11
Statistical Analyses
To account for the sampling design of NIS data, we used the Stata version 14.0 (StataCorp LP, College Station, TX) prefix command “svy” to estimate the annual weighted number of delivery hospitalizations, the annual and quarterly syphilis rates (or the number of females who had a syphilis diagnosis on their discharge records per 100,000 newborn deliveries), and to examine the association of patients’ sociodemographic characteristics with syphilis diagnoses.
Temporal trends in syphilis rates (overall and by sociodemographic groups) were estimated by using Joinpoint software version 4.5.0.1 (National Institutes of Health/National Cancer Institute, Bethesda, MD).22 We fitted a log-linear autocorrelated errors model with a maximum of 3 joinpoints (4 line segments) allowed in each model and selected models with the smallest Bayesian information criterion. The resultant trends were described by the quarterly percentage changes (QPCs). Two-sided statistical significance (P < 0.05) for QPC was determined by using a t test. Trends based on 10 or less observations in any of the 20 quarters (2010 first quarter–2014 fourth quarter) were suppressed, as required by HCUP.23 The third and fourth AHI quartiles were combined to ensure more than 10 case subjects per quarter.
To assess the association between syphilis diagnosis on delivery discharge records and sociodemographic characteristics, we estimated relative risks (RR) and 95% confidence intervals (CIs) by using a generalized linear model with log link and binomial distribution “svy: glm …, fam(bin) link(log) eform.” In all analyses, the dependent variable indicated the presence of discharge records with syphilis-related ICD-9 codes.
RESULTS
Trends Among Females With a Syphilis Diagnosis
During 2010–2014, a total of 18.7 (95% CI, 18.2–19.2) million females gave birth in US hospitals, and 7518 (95% CI, 6781–8255) had a syphilis diagnosis on their discharge records (results not shown). The number of delivery hospitalizations remained stable: 3.7 (95% CI, 3.3–4.1) million in 2010 and 3.8 (95% CI, 3.6–4.0) million in 2014 (results not shown). By contrast, the number of delivery discharges with a syphilis diagnosis stayed stable during 2010–2011 (2010: 1523 females; 95% CI, 1050–1995; 2011: 1401 females; 95% CI, 965–1836), and increased from 1310 (95% CI, 1076–1544) during 2012 to 1830 (95% CI, 1562–2098) during 2014 (results not shown).
Overall, syphilis rates per 100,000 deliveries decreased during 2010–2012 (2010 first quarter–2012 fourth quarter [2010q1–2012q4]; QPC, −1.0%; P < 0.001) and increased afterward (2012q4–2014q4; QPC, 1.8%; P < 0.001) (Fig. 1 and Table 1). Within sociodemographic subgroups, the trends in syphilis rates varied. Three groups of females had statistically significant declines during 2010–2011: women who were 35 years or older (2010q1–2011q4; QPC, −6.2%; P < 0.001), females who lived in the Northeast (2010q1–2011q4; QPC, −8.4%; P < 0.001), and those who lived in the South (2010q1–2011q4; QPC, −1.0%; P < 0.001). In the fourth quarter of 2011 or afterward, syphilis rates increased among all sociodemographic groups, with statistically significant increases identified among females who were black (2013q1–2014q4; QPC, 2.8%; P < 0.001) or Hispanic (2012q2–2014q4; QPC, 3.0%; P < 0.001); ages 25–34 years (2012q4–2014q4; QPC, 2.4%; P < 0.001) or ≥35 years (2011q4–2014q4; QPC, 1.7%; P < 0.001); privately insured patients (2012q3–2014q4; QPC, 3.0%; P < 0.001); females with the highest AHI (third and fourth income quartile, 2012q4–2014q4; QPC, 2.9%; P < 0.001); or females who lived in the Northeast (2011q1–2014q4; QPC, 2.0%; P < 0.001) or the South (2012q4–2014q4; QPC, 1.6%; P < 0.001). The greatest statistically significant increase in syphilis rates was identified among whites (2014q41–2014q4; QPC, 35.2%; P < 0.001) and Medicaid recipients (2014q1–2014q4; QPC, 15.1%; P < 0.001). Of note, a consistent increase in syphilis rates occurred throughout the study period among different sociodemographic groups, including females who were 24 years or younger (2010q1–2014q4; QPC, 0.7%; P < 0.001) and females who lived in the Midwest (2010q1–2014q4; QPC, 1.0%; P < 0.001) or the West (2010q1–2014q4; QPC, 0.9%; P < 0.001).
Figure 1.
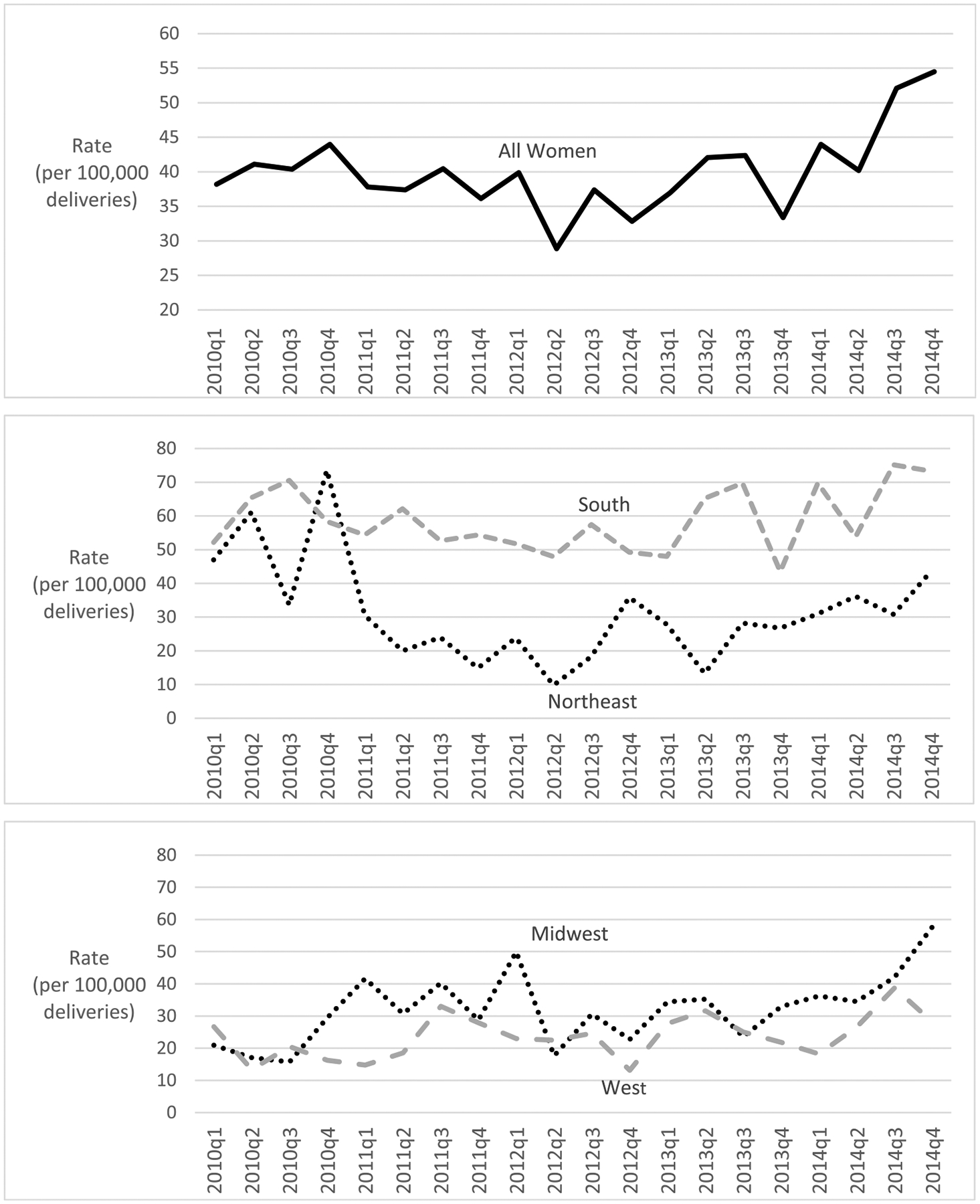
Quarterly Rates of Females With a Syphilis Diagnosis on Hospital Discharge Records at Delivery, United States, 2010–2014.
TABLE 1.
Trends in the Number of Females With a Syphilis Diagnosis per 100,000 Deliveries, United States, 2010–2014
| Annual Rate* | Inflection Years and Quarters† | Trend Segment† | QPC in Syphilis Rates* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 95% CI | P | ||||
| Characteristics | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) |
| All females | 40.9 | 38.1 | 34.8 | 38.9 | 48.1 | 2012q4 | 2010q1–2012q4 | −1.0 | (−1.7 to −0.3) | <0.001 |
| 2012q4–2014q4 | 1.8 | (0.8–2.8) | <0.001 | |||||||
| Race/ethnicity | ||||||||||
| White | 14.4 | 12.9 | 13.4 | 13.1 | 13.6 | 2013q2 | 2010q1–2013q2 | −0.2 | (−1.3 to 0.9) | 0.7 |
| 2014q1 | 2013q2–2014q1 | −5.5 | (−55.4 to 100.1) | 0.9 | ||||||
| 2014q1–2014q4 | 35.2 | (0.8–81.4) | <0.001 | |||||||
| Black | 155.0 | 132.3 | 131.9 | 129.3 | 177.2 | 2013q1 | 2010q1–2013q1 | −0.7 | (−1.3 to 0) | 0.1 |
| 2013q1–2014q4 | 2.8 | (1.4–4.3) | <0.001 | |||||||
| Hispanic | 43.9 | 45.1 | 30.8 | 56.5 | 61.7 | 2012q2 | 2010q1–2012q2 | −1.4 | (−4.3 to 1.7) | 0.4 |
| 2012q2–2014q4 | 3.0 | (0.7–5.3) | <0.001 | |||||||
| Females’ age at delivery, y | ||||||||||
| 13–24 | 43.7 | 53.3 | 49.7 | 54.7 | 58.4 | — | 2010q1–2014q4 | 0.7 | (0.1–1.2) | <0.001 |
| 25–34 | 32.9 | 30.2 | 25.3 | 30.3 | 41.5 | 2012q4 | 2010q1–2012q4 | −1.2 | (−2.4 to 0.1) | 0.1 |
| 2012q4–2014q4 | 2.4 | (0.5–4.4) | <0.001 | |||||||
| ≥35 | 63.7 | 34.4 | 37.7 | 38.3 | 53.0 | 2011q4 | 2010q1–2011q4 | −6.2 | (−9.4 to −2.9) | <0.001 |
| 2011q4–2014q4 | 1.7 | (0.4–3.1) | <0.001 | |||||||
| Expected primary insurer | ||||||||||
| Medicare/Medicaid | 68.7 | 66.2 | 60.7 | 63.3 | 82.8 | 2012q2 | 2010q1–2012q2 | −0.8 | (−1.6 to 0.1) | 0.1 |
| 2014q1 | 2012q2–2014q1 | 0.5 | (−0.8 to 1.8) | 0.4 | ||||||
| 2014q1–2014q4 | 15.1 | (2.9–28.7) | <0.001 | |||||||
| Privately insured | 13.0 | 13.9 | 10.0 | 13.3 | 17.9 | 2011q1 | 2010q1–2011q1 | 1.9 | (−15.1 to 22.3) | 0.8 |
| 2012q3 | 2011q1–2012q3 | −3.4 | (−7.3 to 0.7) | 0.1 | ||||||
| 2012q3–2014q4 | 3.0 | (1.2–4.9) | <0.001 | |||||||
| Median AHI for patient’s zip code, US $ | ||||||||||
| First quartile | 86.7 | 69.2 | 64.1 | 74.8 | 98.2 | 2012q2; | 2010q1–2012q2 | −1.5 | (−3.0 to 0.0) | 0.1 |
| 2014q2 | 2012q2–2014q2 | 1.3 | (−0.6 to 3.2) | 0.2 | ||||||
| 2014q2–2014q4 | 26.4 | (−7.5 to 72.7) | 0.1 | |||||||
| Second quartile | 30.4 | 38.2 | 34.2 | 37.2 | 36.3 | — | 2010q1–2014q4 | 0.30 | (−0.3 to 1.0) | 0.3 |
| Third and fourth quartile | 16.2 | 19.9 | 17.0 | 18.8 | 22.8 | 2012q1; | 2010q1–2012q1 | 1.5 | (−0.9 to 3.9) | 0.2 |
| 2012q4 | 2012q1–2012q4 | −14.9 | (−61.2 to 86.6) | 0.7 | ||||||
| 2012q4–2014q4 | 2.9 | (0.8–4.9) | <0.001 | |||||||
| Census region | ||||||||||
| Northeast | 53.5 | 23.0 | 21.8 | 24.9 | 36.9 | 2011q4 | 2010q1–2011q4 | −8.4 | (−12.3 to −4.3) | <0.001 |
| 2011q4–2014q4 | 2.0 | (0.2–4.0) | <0.001 | |||||||
| Midwest | 20.7 | 35.4 | 30.0 | 31.4 | 42.6 | — | 2010q1–2014q4 | 1.0 | (0.3–1.8) | <0.001 |
| South | 61.8 | 55.8 | 51.7 | 56.7 | 68.3 | 2012q4 | 2010q1–2012q4 | −1.0 | (−1.8 to −0.1) | <0.001 |
| 2012q4–2014q4 | 1.6 | (0.3–2.9) | <0.001 | |||||||
| West | 19.2 | 23.8 | 20.9 | 26.5 | 28.2 | — | 2010q1–2014q4 | 0.9 | (0.2–1.7) | <0.001 |
All results in this table represent the weighted sample.
Number of females with a diagnosis of syphilis per 100,000 deliveries.
Inflection points and trends report years and quarters (eg, 2012q4–2012, fourth quarter).
Income quartiles, 2010: first quartile, US $1–40,999; second quartile, US $41,000–50,999; third quartile US $51,000–66,999; fourth quartile, ≥US $67,000.21
Income quartiles, 2014: First quartile, US $1–39,999; second quartile, US $40,000–50,999; third quartile, US $51,000–65,999; fourth quartile, ≥US $66,000.21
Data Source: The National (Nationwide) Inpatient Sample, HCUP, Agency for Healthcare Research and Quality for 2010–2014.11
Factors Associated With a Syphilis Diagnosis
During 2014, syphilis diagnoses were more frequent among black and Hispanic females and socially disadvantaged populations (Table 2). Approximately a half (49.5%) of females with syphilis diagnoses were black, a quarter (24.9%) were Hispanic, three fourths (75.2%) were Medicaid or Medicare recipients; and 56.0% lived in areas with the lowest AHI (first income quartile: ≤$39,999/year). By contrast, among females without a syphilis diagnosis, 13.4% were black, 19.4% were Hispanic, and 43.7% were Medicaid or Medicare recipients; and 27.4% lived in areas with the lowest AHI. The majority (54.6%) of females with syphilis lived in the South, whereas 38.5% of females without a syphilis diagnosis lived in that region.
TABLE 2.
Sociodemographic Characteristics of Females With and Without a Syphilis Diagnosis on Discharge Records at Delivery, United States, 2014
| Females With a Syphilis Diagnosis (n = 1830) | Females Without a Syphilis Diagnosis (n = 3,803,405) | RR (95% CI) | |
|---|---|---|---|
| Characteristics | % | % | N = 3,805,235 |
| Race/ethnicity | |||
| White | 14.21 | 50.16 | Referent |
| Black | 49.45 | 13.41 | 13.02* (9.46–17.92) |
| Hispanic | 24.86 | 19.38 | 4.53* (3.19–6.42) |
| Other | 7.92 | 10.59 | 2.64* (1.70–4.10) |
| Missing/invalid | 3.55 | 6.46 | 1.94 (0.94–4.02) |
| Females’ age at delivery, y | |||
| 13–24 | 34.70 | 28.57 | Referent |
| 25–34 | 48.09 | 55.80 | 0.71* (0.56–0.89) |
| ≥35 | 17.21 | 15.63 | 0.91 (0.68–1.22) |
| Expected primary insurer | |||
| Medicaid/Medicare | 75.14 | 43.65 | 4.63* (3.38–6.33) |
| Private | 18.85 | 50.66 | Referent |
| Self-pay, no charge, or other | 6.01 | 5.69 | 2.84* (1.74–4.63) |
| Median AHI for patient’s zip code, US $ | |||
| First quartile | 56.01 | 27.42 | 5.32* (3.55–7.97) |
| Second quartile | 19.67 | 26.07 | 1.97* (1.27–3.04) |
| Third quartile | 13.11 | 23.56 | 1.45 (0.92–2.28) |
| Fourth quartile | 8.20 | 21.36 | Referent |
| Missing/invalid | 3.01 | 1.59 | 4.93* (2.64–9.19) |
| Census region | |||
| Northeast | 12.30 | 16.01 | 1.31 (0.83–2.06) |
| Midwest | 18.85 | 21.28 | 1.51 (0.96–2.39) |
| South | 54.64 | 38.50 | 2.42* (1.66–3.53) |
| West | 14.21 | 24.22 | Referent |
All results in this table (ie, number of hospitalizations, frequencies, and RR) represent the weighted sample.
Statistically significant at P < 0.001.
Income quartiles, 2014: First quartile, US $1–39,999; Second quartile, US $40,000–50,999; third quartile, US $51,000–65,999; fourth quartile, ≥US $66,000.21
Data Source: The National (Nationwide) Inpatient Sample, HCUP, Agency for Healthcare Research and Quality for 2014.11
The risk for having a syphilis diagnosis on discharge record at delivery was greater among blacks (RR, 13.02; 95% CI, 9.46–17.92) or Hispanics (RR, 4.53; 95% CI, 3.19–6.42), compared with whites; Medicaid recipients (RR, 4.63; 95% CI, 3.38–6.33) or uninsured (RR, 2.84; 95% CI, 1.74–4.63), compared with privately insured patients; females with the lowest household income (RR, 5.32; 95% CI, 3.55–7.97), compared with the highest income; and females in the South (RR, 2.42; 95% CI, 1.66–3.53), compared with those in the West (Table 2).
DISCUSSION
We assessed national trends in syphilis diagnosis rates and factors associated with a syphilis diagnosis among US females with a live birth or stillbirth delivery. We analyzed NIS data for 2010–2014 and estimated 1,310–1,830 (or 34.76–48.09 per 100,000) females who had given birth each year had a diagnosis of syphilis on their discharge records. Overall, we determined that syphilis rates decreased during 2010–2012 at approximately 1% per quarter and increased afterward at approximately 2%. As the number of delivery hospitalizations remained stable over the course of this study, changes in syphilis rates (per 100,000 deliveries) reflected changes in the number of females with a syphilis diagnosis on their discharge records at delivery. Since 2012, syphilis rates significantly increased among all sociodemographic groups and in all 4 US regions, whereas the risk for syphilis diagnosis at delivery during 2014 was greater among black and Hispanic females, those with the lowest AHI (≤US $39,999/year), or those living in the South.
This is the first US study that examined temporal trends among females with a syphilis diagnosis on their delivery discharge records. Importantly, our study revealed differences between populations with substantial increases in syphilis rates and populations with greater risk for syphilis diagnosis. In contrast with groups with greatest risk for syphilis diagnosis (ie, blacks or Hispanics, having the lowest AHI, uninsured, or living in the South), the largest increases in rates within each sociodemographic group were identified among whites (35.2% increase/quarter), females in the highest AHI quantiles (≥US $51,000/year, 2.9% increase), and females in the Northeast (2.0%). Medicaid recipients were the only group with a high risk for syphilis diagnosis (RR, 4.63, compared with privately insured females) and a substantial increase in syphilis rates (15.1%/quarter).
Syphilis is a nationally notifiable condition and CDC monitors trends in reported cases of syphilis among pregnant women. Our estimates of the number of pregnant females with a syphilis diagnosis at delivery during 2012–2014 were 84–94% of the number of syphilis cases reported among pregnant women through CDC’s case-based surveillance system5 (our study: 1310 females in 2012 and 1830 females in 2014; case-based surveillance system: 1561 in 2012 and 1955 females in 2014). The discrepancy in the numbers is expected, because our data source is restricted to females who deliver live- or stillborn neonates and does not include spontaneous abortions. By contrast, CDC collects case data among females who are known to be pregnant and, hence, is not limited to specific birth outcomes. Overall, stillbirths and spontaneous abortions account for approximately 17% of pregnancy outcomes among all pregnant US females24 and up to 41% among untreated females with syphilitic infection.2,25 We could better assess comparability by limiting our estimates to females who delivered a live-born neonate (eg, 1800 females in 2014) and by adjusting to account for additional pregnancies that could have ended in spontaneous abortions (between 17% of pregnancies, if all females with ICD-9 syphilis diagnosis on their discharge records were cured early in pregnancy, and 41% of pregnancies, if all females with a syphilis diagnosis have not received adequate treatment by the time of delivery). We estimated 2169–3051 females in 2014 could have had a syphilitic infection during pregnancy and either delivered a live or stillborn neonate or had a spontaneous abortion. These adjusted estimates exceed the number of syphilis cases reported in the CDC’s surveillance system (1955 females in 2014). The latter may underestimate prevalence of syphilis because of missing pregnancy status in approximately 30% of reported syphilis cases among women.5 By contrast, our study could overestimate the actual burden of syphilis if some ICD-9 diagnoses were not confirmed by the time of hospital discharge.
Our findings regarding demographic factors associated with syphilis diagnoses on discharge records are consistent with previous national-level analyses of US females of reproductive age with diagnoses of primary or secondary syphilis6–8 and state analyses of females who delivered a live-born neonate.20 Similar to those studies, we identified higher rates of documented syphilis among black or Hispanic females, Medicaid recipients, and females who lived in the South. Our study is the first to include multiple socioeconomic indicators and to demonstrate higher syphilis rates among socially disadvantaged populations: females with the lowest AHI and those who were uninsured.
Our study was subject to a number of limitations. First, we were not able to estimate prevalence of syphilis in pregnant women overall, because NIS does not include information regarding pregnancies that end in spontaneous or induced abortions. Second, our estimates may be an over or underestimate of the number of syphilitic infections among females delivering live-born or stillborn neonates. Similar to data sets analyzed in previous studies,5,7,26 NIS neither reports the pregnancy stage when a female had a diagnosis of syphilis nor her treatment status. If a woman received recommended and timely treatment before delivery, then ICD-9 syphilis diagnosis on her discharge record might not have been for active syphilitic infection at time of delivery, thus resulting in an overestimate. We could also overestimate the actual burden of syphilis if some diagnoses were presumptive and not confirmed at the time of hospital discharge. Conversely, we could underestimate the actual burden of syphilitic infection among females who give birth, because NIS does not include 1% to 1.5%27,28 of females who deliver outside of a hospital. Furthermore, discharge records are more likely to include diagnoses documented during prenatal obstetrics visits or during labor and delivery admission triage, and may not include diagnoses confirmed in other locations (eg, a sexually transmitted disease clinic), thus resulting in an underestimate. Finally, similar to previous studies,5,26 we cannot assess perinatal transmission of T. pallidum among children who were born during 2010–2014 to mothers with a diagnosis of syphilis, because NIS lacks mother-to-child links.
Despite these limitations, our study makes multiple contributions to the literature. First, we use a nationally representative sample of hospitalizations to estimate the number of US females with a diagnosis of syphilis (of all stages) on their hospital delivery discharge records, report on trends in syphilis rates by sociodemographic group, and document increased rates during 2012–2014 in all sociodemographic groups, including groups at lowest risk. Second, we describe sociodemographic groups at higher risk for having a syphilis diagnosis recorded on discharge records, and we document higher risk among black and Hispanic females, Medicaid recipients, the uninsured, and females living in areas with the lowest AHI.
Public health and clinical action are needed to reduce the increasing rate of syphilis among pregnant females. Prenatal screening for syphilis remains crucial for all pregnant females. Co-ordinated efforts involving females with syphilis diagnoses, health care providers, and public health professionals can reduce the risk for mother-to-child transmission of T. pallidum among seropositive pregnant females by initiating on-the-spot treatment and promoting testing and treatment of partners to avoid reinfection.1,6,10 Syphilis among pregnant women can be further reduced by efforts to prevent the infection among all females of reproductive age. Such efforts would require sexually transmitted disease prevention programs to quickly identify syphilis cases among females of reproductive age and their partners in their jurisdictions and to prioritize such cases for case investigation and partner services.29
Footnotes
Conflict of Interest and Sources of Funding: None declared.
REFERENCES
- 1.Genç M, Ledger WJ. Syphilis in pregnancy. Sex Transm Infect 2000; 76:73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gomez GB, Kamb ML, Newman LM, et al. Untreated maternal syphilis and adverse outcomes of pregnancy: A systematic review and meta-analysis. Bull World Health Organ 2013; 91:217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lukehart S Syphilis. In: Kasper D, Fauci A, Hauser S, et al. eds. Harrison’s principles of internal medicine, 2015; 19e:1132–1140. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Morb Mortal Wkly Rep 2015; 64:1–140.25590678 [Google Scholar]
- 5.Williams C Increased cases of syphilis among pregnant women and infants—United States, 2012–2014. Paper presented at: Epidemic Intelligence Service Conference: May 2016. [Google Scholar]
- 6.Fenton KA, Breban R, Vardavas R, et al. Infectious syphilis in high-income settings in the 21st century. Lancet Infect Dis 2008; 8:244–253. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2014; 2015. Available at: https://www.cdc.gov/std/stats14/toc.htm.
- 8.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2016; 2017. Available at: https://www.cdc.gov/std/stats16/toc.htm.
- 9.Fiumara NJ, Fleming WL, Downing JG, et al. The incidence of prenatal syphilis at the Boston City Hospital. New England Journal of Medicine 1952; 247:48–52. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Let’s work together to stem the tide of rising syphilis in the United States. 2017.
- 11.HCUP National (Nationwide) Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality: 1980–2015. https://www.hcup-us.ahrq.gov/nisoverview.jsp. [Google Scholar]
- 12.Partner organizations providing data to HCUP. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality, 2017: https://www.hcup-us.ahrq.gov/db/hcupdatapartners.jsp#liststates. [Google Scholar]
- 13.Trend weights for 1993–2011 HCUP NIS Data. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality, 2015: http://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp. [PubMed] [Google Scholar]
- 14.Protection of human subjects. Code of Federal Regulations, title 45, part 46. [PubMed]
- 15.Acute Inpatient Prospective Payment System. 2017. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html?redirect=/acuteinpatientpps/.
- 16.International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). 2015. Available at: https://www.cdc.gov/nchs/icd/icd9cm.htm. [PubMed]
- 17.Chen YC, Liu H-Y, Li CY, et al. The rising trend of sexually transmitted infections among HIV-infected persons: A population-based cohort study in Taiwan, 2000 through 2010. J Acquir Immune Defic Syndr 2015; 68:432–438. [DOI] [PubMed] [Google Scholar]
- 18.HCUP Clinical Classifications Software - Diagnoses (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality: 1980–2015. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/AppendixASingleDX.txt. [Google Scholar]
- 19.Owusu-Edusei K Jr., Hoover KW, Tao G. Estimating the direct outpatient medical cost per episode of primary and secondary syphilis in the United States: Insured population perspective, 2003–2007. Sex Transm Dis 2011; 38:175–179. [DOI] [PubMed] [Google Scholar]
- 20.Waight MT, Rahman MM, Soto P, et al. Sexually transmitted diseases during pregnancy in Louisiana, 2007–2009: High-risk populations and adverse newborn outcomes. J La State Med Soc 2013; 165:219–226. [PubMed] [Google Scholar]
- 21.NIS description of data elements. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality: 1980–2014. https://www.hcup-us.ahrq.gov/db/nation/nis/nisdde.jsp. [Google Scholar]
- 22.Jemal A, Ward EM, Johnson CJ, et al. Annual report to the nation on the status of cancer, 1975–2014, featuring survival. J Natl Cancer Inst 2017; 109:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Data use agreement for the Nationwide Databases Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality: https://www.hcup-us.ahrq.gov/team/NationwideDUA.pdf. [PubMed] [Google Scholar]
- 24.Ventura SJ, Curtin SC, Abma JC, et al. Estimated pregnancy rates and rates of pregnancy outcomes for the United States, 1990–2008. Natl Vital Stat Rep 2012; 60:1–21. [PubMed] [Google Scholar]
- 25.Qin J, Yang T, Xiao S, et al. Reported estimates of adverse pregnancy outcomes among women with and without syphilis: A systematic review and meta-analysis. PLoS One 2014; 9:e102203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kidd S, Bowen V, Torrone E, et al. Use of National Syphilis Surveillance Data to develop a congenital syphilis prevention cascade and estimate the number of potential congenital syphilis cases averted. Sex Transm Dis 2018; 45(9S Suppl 1):S23–S28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martin JA, Hamilton BE, Sutton PD, et al. Births: Final data for 2006. National vital statistics reports. Vol. 57, no 7. Hyattsville MD: Natl Cent Health Stat; 2009. [Google Scholar]
- 28.Hamilton BE, Martin JA, Osterman MJK, et al. Births: Final data for 2014. National vital statistics reports; reports; vol 64 no 12. Hyattsville, MD: National Center for Health Statistics, 2015:2015. Available at: https://www.cdc.gov/nchs/products/nvsr.htm. [PubMed] [Google Scholar]
- 29.Bowen V, Su J, Torrone E, et al. Increase in incidence of congenital syphilis—United States, 2012–2014. MMWR Morb Mortal Wkly Rep 2015; 64:1241–1245. [DOI] [PubMed] [Google Scholar]


