Abstract
Background and Objectives
Multidisciplinary clinics have been shown to improve care. Patients with patent foramen ovale (PFO)–associated stroke need evaluation by cardiology and neurology specialists. We report our experience creating a multidisciplinary Structural Heart Brain Clinic (HBC) with a focus on patients with PFO-associated stroke.
Methods
Demographic and clinical data were retrospectively collected for patients with PFO-associated ischemic stroke. Patients with PFO-associated stroke were divided into a standard care group and Heart Brain Clinic group for analysis. Outcome measures included time from stroke to PFO closure and number of clinic visits before decision regarding closure. Nonparametric analysis evaluated differences in median time to visit and clinical decision, while the chi square analysis compared differences in categorical variables between groups.
Results
From February 2017 to December 2021, 120 patients were evaluated for PFO-associated stroke. The Structural HBC began in 12/2018 with coordination between Departments of Neurology and Cardiology. For this analysis, 41 patients were considered in the standard care group and 79 patients in the HBC group. During data analysis, 107 patients had received recommendations about PFO closure. HBC patients required fewer clinic visits (p = 0.001) before decision about closure; however, among patients who underwent PFO closure, there was no significant difference in weeks from stroke to PFO closure. Clinicians were more likely to recommend against PFO closure among patients seen in HBC compared with those seen in standard care (p = 0.021).
Discussion
Our data demonstrate that a multidisciplinary, patient-centered approach to management of patients with PFO-associated ischemic stroke is feasible and may improve the quality of care in this younger patient population. The difference in recommendation to not pursue PFO closure between groups may reflect selection and referral bias. Additional work is needed to determine whether this approach improves other aspects of care and outcomes.
Introduction
Ischemic stroke is a common cause of morbidity and mortality.1 Patent foramen ovale (PFO)–associated strokes account for 5% of ischemic strokes, with the number rising to 10% in young and middle-aged adults.2 PFO closure may be recommended in appropriate patients because stroke recurrence rates in patients with PFO may be as high as 4%.3-5 While PFO is more common in patients with cryptogenic stroke (40%), it is also common in the general population (25%), and it may therefore be an incidental finding in some patients with cryptogenic stroke.6,7 To assess the etiologic relationship between PFO and stroke, other potential causes, including atrial fibrillation and hypercoagulable states, need to be excluded. Furthermore, to assess the potential benefit of PFO closure, shunt characteristics should be quantified and anatomic characteristics assessed.8 Because neurologists and cardiologists are both involved in caring for these patients, PFO-associated ischemic stroke provides an opportunity for a multidisciplinary approach, where both teams working in a single clinical setting can expedite the appropriate workup and improve shared decision-making for PFO closure. In addition, patients can be more involved in the decision because physicians can explain options available to them and support them while they deliberate which decision suits them best.
Several studies have shown the benefits of transitioning care to a multidisciplinary clinic setting. These clinics can help improve communication with the patient about their care, improve follow-up, reduce treatment cost, and improve diagnosis, patient experience, and outcomes.9-13 Because patients with ischemic stroke in the setting of PFO require both neurology and cardiology evaluation, PFO-associated ischemic stroke is a condition where a multidisciplinary clinic can be beneficial.
A significant proportion of younger patients with ischemic strokes have PFO, and appropriate treatment can decrease the risk of stroke recurrence.14 These younger patients may also accumulate increased losses due to disability, loss of income, and time away from work.15 The need for multiple outpatient visits for stroke and PFO closure evaluation in 2 different specialty clinics could lead to loss to follow-up, add social and psychological stress, and cause delays in treatment decisions. A multidisciplinary clinic that reduces the number of clinic visits and leads to more rapid treatment may lead to an enhanced experience for this younger patient population.
The primary purpose of this retrospective observational study is to present our experience with patient follow-up in our multidisciplinary Heart Brain Clinic (HBC) after PFO-associated stroke and to demonstrate whether it improves quality of care. We sought to compare the number of follow-up visits, time to intervention, and distance traveled for patients seen in the HBC compared with patients evaluated with standard care.
Methods
Stroke Clinic
Patients who are discharged from the Comprehensive Stroke Center at Memorial Hermann Hospital-Texas Medical Center are seen for follow-up in the University of Texas Health Sciences Center (UTHEALTH) stroke clinic. Patients are also referred to the stroke clinic and cardiology clinic from other neurology and cardiology practices in the metropolitan Houston area, other clinics in the UTHEALTH system, and consulting hospitals and clinics from across Southeast Texas and Louisiana.
Standard Care
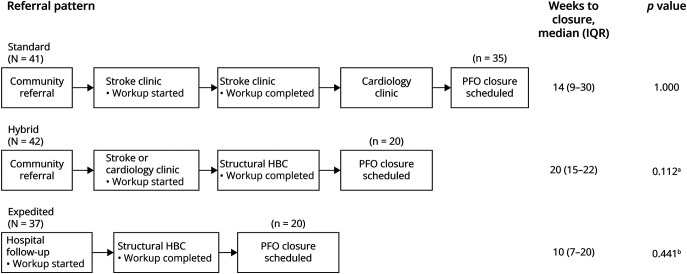
Before the initiation of HBC, patients with PFO-associated stroke were referred for PFO closure through 2 primary mechanisms: (1) direct neurology consultation: patients were referred to stroke clinic for stroke evaluation and subsequently referred to cardiology clinic for additional PFO evaluation or (2) no neurology consultation: patients directly referred to cardiology clinic for PFO closure by a community physician or were self-referred for a second opinion and were then evaluated for PFO closure by neurology (Figure 1). Stroke diagnostic evaluation began during hospitalization for stroke, with additional etiologic evaluation for cryptogenic stroke being initiated. In either setting, PFO was diagnosed mainly with transthoracic echocardiogram (TTE) and transcranial Doppler (TCD) with bubble study and rarely with transesophageal echocardiogram (TEE). If the attending neurologist felt the stroke was secondary to the presence of a PFO, the patient was referred to cardiology clinic for PFO closure assessment. Depending on the cardiologist's preference, patients were either taken directly for PFO after their TTE and TCD or if needed, a TEE was ordered if not already performed to better evaluate the anatomy of the PFO and then the patient was scheduled for PFO closure if appropriate.
Figure 1. Clinic Pathways and Number of Weeks Before Scheduling PFO Closure.
The diagram shows the different clinic pathways and number of weeks before scheduling PFO closure in the 3 different groups. aComparison of weeks before PFO closure in the standard referral and the hybrid referral systems. bComparison of weeks before PFO closure in the standard referral and the expedited referral systems. PFO = patent foramen ovale.
Heart Brain Clinic
The UTHEALTH Heart Brain Clinic consists of neurologists who specialize in the care of stroke patients and interventional cardiologists and cardiac electrophysiologists. The Structural Heart Brain Clinic (HBC) was developed in December 2018 to ensure stroke workup was complete and appropriate secondary stroke prevention was in place for 2 patient subsets: those who were potential candidates for either PFO closure or left atrial appendage closure. This clinic occurs ½ day per month and began as an in-person clinic (December 2018–February 2020) and was converted to a virtual clinic (video telehealth) in April 2020 during the COVID-19 pandemic. Between 4 and 8 patients are evaluated in each half day clinic. The second HBC (formed in April 2019) is the Embolic Stroke of Undetermined Source (ESUS) Clinic, which is focused on patients without PFO. The description and analysis in this article is limited to patients evaluated for PFO-associated stroke in the Structural HBC.
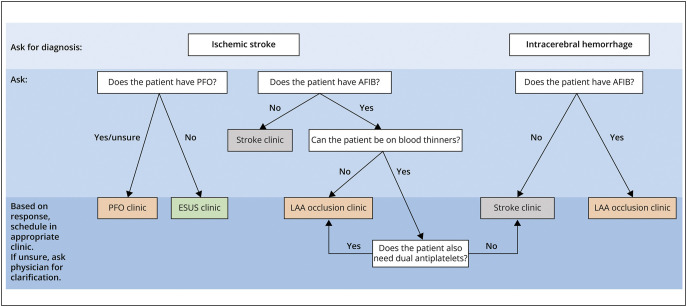
Patients could be evaluated for PFO closure in the structural HBC in several ways (Figure 2). Patients who were first hospitalized at the UTHEALTH-affiliated teaching hospital with stroke could either be referred to stroke clinic for additional workup before HBC referral (hybrid system) or directly to HBC for evaluation of their PFO-associated stroke if no other stroke etiology was found (expedited system). Even after HBC was initiated, patients referred from regional hospitals or clinics could be referred both to stroke clinic for evaluation and separately to interventional cardiology clinic for PFO evaluation. These patients could then be triaged to Structural HBC. Patients who were initially seen in stroke clinic or cardiology clinic and were subsequently referred to HBC were also categorized as a hybrid system (Figure 1).
Figure 2. Scheduling Heart Brain Clinic Referrals.
AFIB = atrial fibrillation; ESUS = embolic stroke unknown source; ICH = intracerebral hemorrhage; LAA = left atrial appendage; PFO = patent foramen ovale.
Administrative Planning for HBC
In preparation for HBC, the neurology and cardiology outpatient scheduling, billing, and clinical staff aligned processes. We developed a communication system between the neurology and cardiology schedulers. The neurology team assumed the role of primary schedulers and a neurology referral email was created. A “Heart Brain Clinic” template was created in the electronic medical record for scheduling purposes. Patients scheduled in the Heart Brain Clinic template were accessible to both neurology and cardiology clinicians for separate documentation and billing purposes. From the primary teaching hospital, the stroke nurse navigator facilitated HBC follow-up for hospitalized patients with PFO-associated stroke through the neurology referral email. The patients were placed on the designated clinic template, which was visible to all providers and clinic staff. If patients were referred directly to the neurology clinic, the designated stroke clinic schedulers looked for an indication related to “PFO” in the referral and after approval by the stroke clinic director, would place the patient on the HBC schedule. If patients were referred directly to the structural cardiology clinic, the cardiology clinic schedulers would email the designated neurology referral email to have the patient placed on the HBC schedule. Before HBC appointments, patients were notified of the clinic location (in-person or virtual) and were notified of financial obligations regarding copays for specialists. The HBC program staff and clinicians meet monthly to discuss processes and opportunities for improvements.
Approach to Patient Care
The Structural HBC team includes an attending interventional cardiologist and an attending neurologist, interventional cardiology and vascular neurology fellows, cardiology and neurology trained advanced practice providers, nursing staff, and research coordinators. Before each HBC clinic, the clinical teams review the available diagnostic and imaging data. When patients were seen in-person (December 2018–February 2020), they were seen initially by the neurology team, followed by the cardiology team. After both assessments, the team members would discuss the case and return to see the patient together. For the video telehealth encounters, both teams are present throughout the assessment. The clinical teams discuss different factors related to the PFO closure recommendation, results of the stroke workup, the likelihood that the stroke is related to the PFO (supported by the Risk Of Paradoxical Embolism score),16 and additional recommended studies. The team then engages the patient and caregiver in discussion regarding the recommendations, potential risks, and benefits and together make a decision regarding PFO closure. If the decision is for PFO closure, the cardiology team will describe the procedure using a model of the closure device and schedule a tentative date for PFO closure. The device is selected based on the cardiologist's preference. In situations where additional evaluation is recommended, including cardiac monitoring, hypercoagulability workup, or additional diagnostic imaging, the patient is scheduled for these investigations. If the results of these investigations do not demonstrate another stroke etiology, then the patients are called to schedule PFO closure. If the results do reveal an alternative stroke etiology, patients may follow-up in either stroke or cardiology clinic and workup is completed accordingly.
Data Collection
Demographic and clinical data were retrospectively collected for patients with PFO-associated stroke from February 2017 to December 2021. Patients were categorized according to referral pattern (standard, hybrid, or expedited). We abstracted age, sex, diagnostic evaluation, time from stroke to PFO closure, number of clinic visits before decision about closure, total distance traveled to clinic, referral information, and details of the neurology, cardiology, and HBC clinic visits from our electronic medical record system.
Diagnostic Evaluation
Diagnostic workup was reviewed by the neurologist and interventional cardiologist and included, but was not limited to, MRI of the brain, vascular imaging of head and neck, transcranial doppler with bubble study, TTE and TEE with bubble study, prolonged telemetry monitoring with a 30-day event monitor or implantable cardiac monitor, lipid panel, hemoglobin A1c level, and hypercoagulable workup when appropriate.
Statistical Analysis
Continuous data are presented as either mean ± SD for normal distributions or median and interquartile range for non-normal distributions. Independent sample t test or Wilcoxon rank sum test were used to compare mean or median differences for continuous variables in baseline characteristics between the groups. Categorical data were presented as frequencies and compared using the χ2 test. p < 0.05 was considered statistically significant. Further analysis was conducted to compare patients seen in Structural HBC directly (expedited Structural HBC) with patients seen in Structural HBC in the hybrid system (eTable 1, links.lww.com/CPJ/A479). Statistical analysis was conducted using SPSS for Windows version 27 statistical software (SPSS Inc, Chicago, IL).
Standard Protocol Approvals, Registrations, and Patient Consents
A waiver to conduct the study was granted by the institutional review board. Patient consent was not obtained because the study was retrospective in nature and patient data were deidentified.
Data Availability
Anonymized data not published within this article will be made available on reasonable request from any qualified investigator.
Results
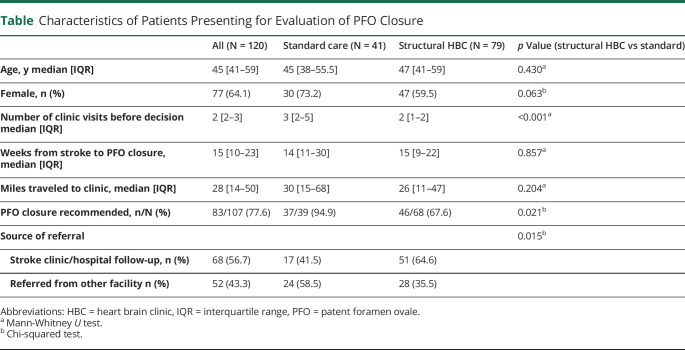
During the study period, a total of 120 patients with PFO-associated stroke were evaluated for PFO closure. The median age and interquartile range (IQR) of patients was 45 [41–59] years with the patient population being predominantly female (64.1%). Thirty-seven patients were seen over telehealth. The Table summarizes the baseline characteristics of the patients seen in clinic. Seventy-nine patients were seen in HBC while 41 patients were seen in the standard referral system. Of the 79 patients in HBC, 37 patients were directly referred to Structural HBC from the primary teaching hospital, while 42 patients were evaluated in the hybrid system (referral to HBC after initial evaluation in UTHEALTH neurology or cardiology clinic). Initially, the HBC clinic system was most efficient when patients were seen within the UTHEALTH system. However, over time, the clinic schedulers and staff became accustomed to the process and were able to move external referrals from either neurology or cardiology clinics into the HBC process.
Table.
Characteristics of Patients Presenting for Evaluation of PFO Closure
| All (N = 120) | Standard care (N = 41) | Structural HBC (N = 79) | p Value (structural HBC vs standard) | |
| Age, y median [IQR] | 45 [41–59] | 45 [38–55.5] | 47 [41–59] | 0.430a |
| Female, n (%) | 77 (64.1) | 30 (73.2) | 47 (59.5) | 0.063b |
| Number of clinic visits before decision median [IQR] | 2 [2–3] | 3 [2–5] | 2 [1–2] | <0.001a |
| Weeks from stroke to PFO closure, median [IQR] | 15 [10–23] | 14 [11–30] | 15 [9–22] | 0.857a |
| Miles traveled to clinic, median [IQR] | 28 [14–50] | 30 [15–68] | 26 [11–47] | 0.204a |
| PFO closure recommended, n/N (%) | 83/107 (77.6) | 37/39 (94.9) | 46/68 (67.6) | 0.021b |
| Source of referral | 0.015b | |||
| Stroke clinic/hospital follow-up, n (%) | 68 (56.7) | 17 (41.5) | 51 (64.6) | |
| Referred from other facility n (%) | 52 (43.3) | 24 (58.5) | 28 (35.5) |
Abbreviations: HBC = heart brain clinic, IQR = interquartile range, PFO = patent foramen ovale.
Mann-Whitney U test.
Chi-squared test.
Decision Regarding PFO Closure
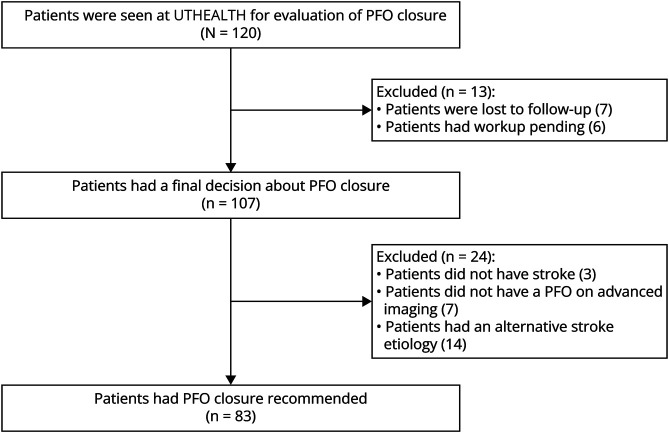
Of the 120 patients evaluated for PFO closure, 107 (89.2%) had a clear recommendation regarding PFO closure. PFO closure was recommended for 83 (77.6%) patients and not recommended for 24 (22.4%) patients. The most common reason PFO closure was not recommended was because an alternative etiology for stroke was more likely (n = 14). Additional imaging including TCD and TEE ruled out PFO in 7 patients, while 3 patients' symptoms were not related to ischemic events (Figure 3). The remaining 13 (10.8%) patients were either pending additional workup before a decision for PFO closure (n = 6) or were lost to follow-up (n = 7).
Figure 3. Screening of Patients for PFO Closure.
Patients seen in the standard referral approach had a higher rate of PFO closure compared with patients seen in Structural HBC (94.9% vs 67.6%, respectively, p = 0.021). This difference did not vary according to the referral process to HBC, whereby 70.0% of patients seen in the expedited system and 65.7% of patients seen in the hybrid system were recommended for PFO closure.
Patient-Centered Care
The median [IQR] number of clinic visits before decision on whether PFO should be closed was 2 [1–2] in the Structural HBC group and 3 [2–5] in patients seen in standard system (p < 0.001). There was no statistical difference in number of weeks from stroke to PFO closure in the Structural HBC group overall compared with that in the standard care group (p = 0.86). Median weeks to closure was higher in patients seen in standard care (14 weeks [11–30]) and hybrid system (20 weeks, [15–22]) than patients referred in the expedited system (10 weeks [7–20]). The median distance traveled to clinic was 28 [14–50] miles, with 15 (12.5%) patients driving more than 100 miles to the clinic.
SARS-CoV-2 Pandemic
During the global pandemic, elective procedures were shut down temporarily. Thirty-seven patients were seen in Structural HBC after March 2020, of which 11 were seen when elective procedures were shut down. For patients in the hybrid referral system (n = 17), it took 20 weeks (IQR 12.5–27) from stroke to PFO closure. For patients seen in expedited system (n = 20), the average time to closure was 9 weeks (IQR 5–16).
Discussion
In this single-center study evaluating a multidisciplinary HBC for patients with possible PFO-associated stroke, we demonstrated the potential to improve the efficiency of clinical care for secondary stroke prevention. Patients evaluated in HBC had fewer follow-up clinic visits, and for patients seen in the expedited system, there was a trend toward fewer weeks from stroke to PFO closure. In addition, HBC patients were less likely to have PFO closure recommended, suggesting the possibility of more careful selection of appropriate candidates for PFO closure. A multidisciplinary HBC has the potential to make clinical care more efficient by requiring fewer overall clinic visits before definitive treatment.
Multidisciplinary clinics offer a patient-centered approach, which previous studies have shown is more satisfactory for patients.17,18 While the retrospective nature of our study precluded us from assessing patient satisfaction, our results show that patients directly seen at Structural HBC have significantly fewer clinic visits before decision for PFO closure. This demonstrates that a Structural HBC can improve the quality of patient care by decreasing the total number of patient visits and thus minimize the cumulative distance traveled, time off work, the need for help with childcare, and the cost of travel. A large proportion of our patients come from outside Houston, making this decrease in travel time invaluable. Patients seen in the hybrid referral system were more likely to be referred from an outside facility and triaging them to Structural HBC increased their number of clinic visits. However, patients seen on this pathway had overall fewer visits than patients seen in standard referral system. With experience, the clinic schedulers and staff were able to triage external referrals from either neurology or cardiology clinics to the structural HBC.
With the SARS-CoV-2 pandemic, most clinics were switched effectively to a telehealth setting, which made it easier for patients to make their appointments without having to factor in time for travel.
While annual stroke recurrence with PFO-associated strokes is as low as 2%, not having a definitive recommendation for treatment/prevention may still be a source of stress to patients.19 Waiting for elective procedures can have a psychological and social impact on patients' lives.20 One aim of the Structural HBC was to efficiently evaluate patients and if they qualified for PFO closure, attempt to schedule their procedure as early as possible and alleviate some degree of stress. Our study does not show statistical difference between patients seen in the standard system and those seen in the expedited PFO and hybrid systems of referral to HBC regarding having PFO closure earlier; however, our study is limited by small sample size. Nonetheless, patients seen in the expedited Structural HBC system have a clear trend toward fewer weeks from stroke to PFO closure. While the Structural HBC was stopped for 1 month, and elective procedures held for additional months during SARS-CoV-2 global pandemic, patients seen during this time did not have longer stroke to PFO closure time.
PFO is a prevalent anatomical defect, which may be found incidentally in patients with stroke.6,7 Patients can have other stroke etiologies while also having a PFO, in which case, PFO closure may not be indicated. A neurologist's evaluation is helpful in this regard to help complete the stroke workup and provide input on the stroke etiology. In our cohort, 14 (13.1%) patients were found to have another stroke etiology. Similarly, patients might present with stroke-like symptoms but might have another explanation of their symptoms besides ischemic stroke, which was the case in 3 (2.8%) of our patients. These patients form a significant proportion of patients with PFO (15.9%) seen in our clinic and highlight the importance of stroke neurology evaluation. In the same visit, the cardiologist can also review images with the patient and counsel them in case the TEE does not demonstrate a PFO.
A high proportion of patients seen in the standard care system had PFO closure recommended. This is possibly secondary to patients only being referred to an interventional cardiologist when stroke workup was completed and the referring physician felt a procedure would be beneficial. With Structural HBC, the aim was to create a consistent organizational workflow. All patients were evaluated by both specialists in a single visit, with the opportunity for specialists to confer real time, thus decreasing selection bias.
Neurology and cardiology specialties overlap in evaluation for multiple ischemic stroke etiologies, including arrhythmias, PFO-associated strokes, patients with cardiac complications of stroke, and patients with stroke as a complication of cardiac procedures.21 However, both vascular neurology fellows and cardiology fellows have limited exposure to the other specialties. The HBC represents one setting where cardiology and neurology fellows can learn from the other specialty's diagnostic evaluation and decision-making, which will assist them, as they transition to independent practice.
Our study has several limitations. Its retrospective nature limits the number of data points that can be gathered. The small sample size limited the power of our analysis. Patients who were referred from the community might have had additional clinic visits, which could not be accounted for in the final analysis. Previous studies have shown multidisciplinary clinics reduce cost of care. However, a cost analysis was not performed for this study. Patients seen in standard care clinic might have a referral bias because all these patients were deemed to need PFO closure by the referring physician and as such might not be directly comparable with patients seen in Structural HBC.
Our study demonstrates that a dedicated, multidisciplinary approach to PFO-associated stroke is feasible and may improve the quality of patient care. Patients seen in Structural HBC required fewer clinic visits from stroke to closure decision, though this was not statistically significant. Additional research will be needed to demonstrate that this multidisciplinary approach will save cost and time and improve overall quality of care for patients with PFO-associated stroke.
Study Funding
The authors report no targeted funding.
Disclosure
A.Z. Sharrief: consultant Abbott Vascular; A. Dhoble: consultant and proctor for Abbott Vascular and Edwards Lifesciences; R.W. Smalling: consultant and proctor for Abbott Vascular; N.R. Gonzales: consultant Abbott Vascular; M.B. Tariq, S.K.S. Qadri, K. Tulod, S. Gurung, M. Lacap, M. Okpala, B. Manwani: no conflicts. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
TAKE-HOME POINTS
→ Patients with PFO and acute ischemic stroke should have evaluation by both a neurologist and cardiologist for optimal care.
→ A multidisciplinary heart brain clinic provides coordinated, patient-centered care and reduces the number of clinic visits.
→ Multidisciplinary heart brain clinic may enhance diagnostic accuracy of stroke etiology.
→ A multidisciplinary HBC provides opportunity for a unique outpatient collaborative educational experience for neurology and cardiology trainees.
→ Telemedicine is a reasonable alternative to enhance patient care by reducing long travel times.
Appendix. Authors
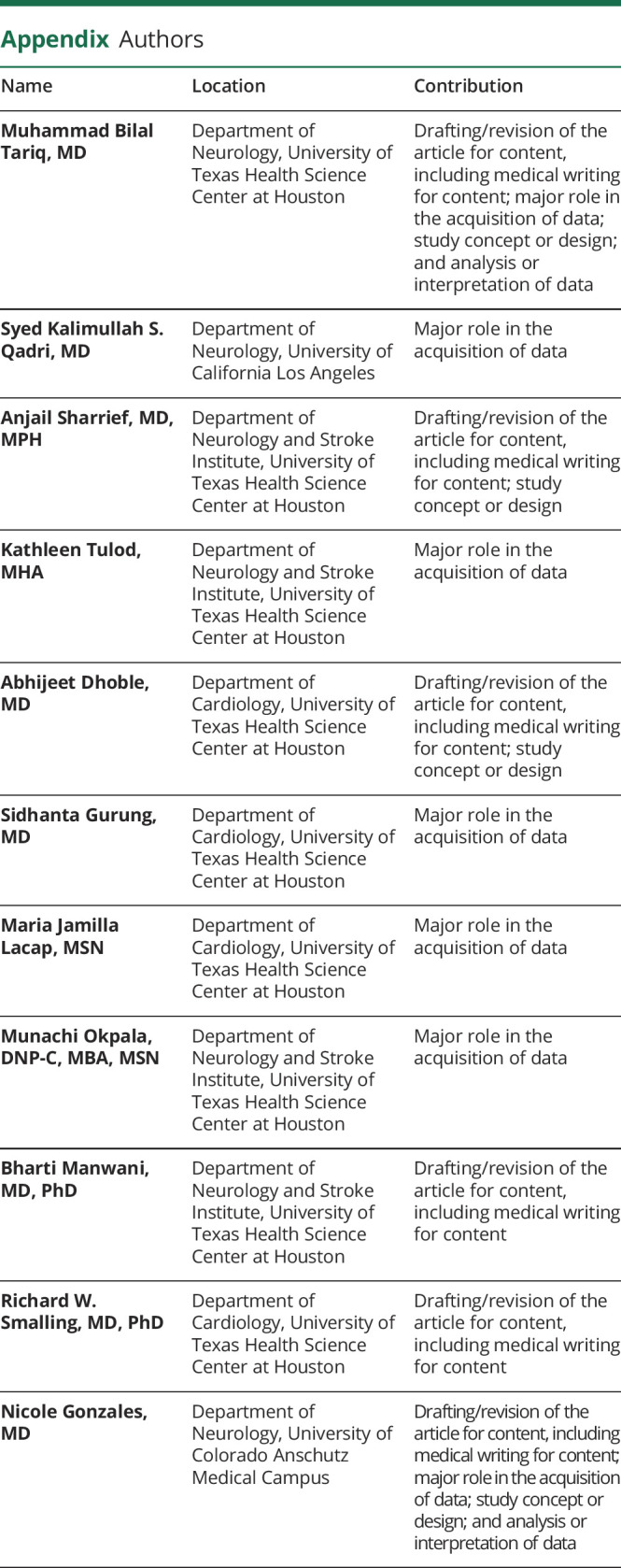
| Name | Location | Contribution |
| Muhammad Bilal Tariq, MD | Department of Neurology, University of Texas Health Science Center at Houston | Drafting/revision of the article for content, including medical writing for content; major role in the acquisition of data; study concept or design; and analysis or interpretation of data |
| Syed Kalimullah S. Qadri, MD | Department of Neurology, University of California Los Angeles | Major role in the acquisition of data |
| Anjail Sharrief, MD, MPH | Department of Neurology and Stroke Institute, University of Texas Health Science Center at Houston | Drafting/revision of the article for content, including medical writing for content; study concept or design |
| Kathleen Tulod, MHA | Department of Neurology and Stroke Institute, University of Texas Health Science Center at Houston | Major role in the acquisition of data |
| Abhijeet Dhoble, MD | Department of Cardiology, University of Texas Health Science Center at Houston | Drafting/revision of the article for content, including medical writing for content; study concept or design |
| Sidhanta Gurung, MD | Department of Cardiology, University of Texas Health Science Center at Houston | Major role in the acquisition of data |
| Maria Jamilla Lacap, MSN | Department of Cardiology, University of Texas Health Science Center at Houston | Major role in the acquisition of data |
| Munachi Okpala, DNP-C, MBA, MSN | Department of Neurology and Stroke Institute, University of Texas Health Science Center at Houston | Major role in the acquisition of data |
| Bharti Manwani, MD, PhD | Department of Neurology and Stroke Institute, University of Texas Health Science Center at Houston | Drafting/revision of the article for content, including medical writing for content |
| Richard W. Smalling, MD, PhD | Department of Cardiology, University of Texas Health Science Center at Houston | Drafting/revision of the article for content, including medical writing for content |
| Nicole Gonzales, MD | Department of Neurology, University of Colorado Anschutz Medical Campus | Drafting/revision of the article for content, including medical writing for content; major role in the acquisition of data; study concept or design; and analysis or interpretation of data |
References
- 1.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545-1602. doi: 10.1016/s0140-6736(16)31678-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elgendy AY, Saver JL, Amin Z, et al. Proposal for updated nomenclature and classification of potential causative mechanism in patent foramen ovale–associated stroke. JAMA Neurol. 2020;77(7):878-886. doi: 10.1001/jamaneurol.2020.0458 [DOI] [PubMed] [Google Scholar]
- 3.Messé SR, Gronseth GS, Kent DM, et al. Practice advisory update summary: patent foramen ovale and secondary stroke prevention: report of the Guideline Subcommittee of the American Academy of Neurology. Neurology. 2020;94(20):876-885. doi: 10.1212/wnl.0000000000009443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collado FMS, Poulin MF, Murphy JJ, Jneid H, Kavinsky CJ. Patent foramen ovale closure for stroke prevention and other disorders. J Am Heart Assoc. 2018;7(12):e007146. doi: 10.1161/jaha.117.007146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nasir UB, Qureshi WT, Jogu H, et al. Updated meta-analysis of closure of patent foramen ovale versus medical therapy after cryptogenic stroke. Cardiovasc Revasc Med. 2019;20(3):187-193. doi: 10.1016/j.carrev.2018.06.001 [DOI] [PubMed] [Google Scholar]
- 6.Alsheikh-Ali AA, Thaler DE, Kent DM. Patent foramen ovale in cryptogenic stroke: incidental or pathogenic? Stroke. 2009;40(7):2349-2355. doi: 10.1161/strokeaha.109.547828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lechat P, Mas JL, Lascault G, et al. Prevalence of patent foramen ovale in patients with stroke. N Engl J Med. 1988;318(18):1148-1152. doi: 10.1056/nejm198805053181802 [DOI] [PubMed] [Google Scholar]
- 8.Falanga G, Carerj S, Oreto G, Khandheria BK, Zito C. How to understand patent foramen ovale clinical significance: part I. J Cardiovasc Echogr. 2014;24(4):114-121. doi: 10.4103/2211-4122.147202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rabinowitz B. Interdisciplinary breast cancer care: declaring and improving the standard. Oncology (Williston Park). 2004;18(10):1263-1268. discussion 1268-70, 1275. [PubMed] [Google Scholar]
- 10.Grosse SD, Schechter MS, Kulkarni R, Lloyd-Puryear MA, Strickland B, Trevathan E. Models of comprehensive multidisciplinary care for individuals in the United States with genetic disorders. Pediatrics. 2009;123(1):407-412. doi: 10.1542/peds.2007-2875 [DOI] [PubMed] [Google Scholar]
- 11.Joret MO, Osman K, Dean A, Cao C, van der Werf B, Bhamidipaty V. Multidisciplinary clinics reduce treatment costs and improve patient outcomes in diabetic foot disease. J Vasc Surg. 2019;70(3):806-814. doi: 10.1016/j.jvs.2018.11.032 [DOI] [PubMed] [Google Scholar]
- 12.Traynor BJ, Alexander M, Corr B, Frost E, Hardiman O. Effect of a multidisciplinary amyotrophic lateral sclerosis (ALS) clinic on ALS survival: a population based study, 1996-2000. J Neurol Neurosurg Psychiatry. 2003;74(9):1258-1261. doi: 10.1136/jnnp.74.9.1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bath AP, Walsh RM, Ranalli P, et al. Experience from a multidisciplinary "dizzy" clinic. Am J Otolaryngol. 2000;21(1):92-97. doi: 10.1016/s0196-0709(00)80081-2 [DOI] [PubMed] [Google Scholar]
- 14.Gupta V, Yesilbursa D, Huang WY, et al. Research from the University of Alabama at Birmingham: patent foramen ovale in a large population of ischemic stroke patients: diagnosis, age distribution, gender, and race. Echocardiography. 2008;25(2):217-227. doi: 10.1111/j.1540-8175.2007.00583.x [DOI] [PubMed] [Google Scholar]
- 15.Tirschwell DL, Turner M, Thaler D, et al. Cost-effectiveness of percutaneous patent foramen ovale closure as secondary stroke prevention. J Med Econ. 2018;21(7):656-665. doi: 10.1080/13696998.2018.1456445 [DOI] [PubMed] [Google Scholar]
- 16.Kent DM, Ruthazer R, Weimar C, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013;81(7):619-625. doi: 10.1212/wnl.0b013e3182a08d59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berry MG, Chan SY, Engledow A, et al. An audit of patient acceptance of one-stop diagnosis for symptomatic breast disease. Eur J Surg Oncol. 1998;24(6):492-495. doi: 10.1016/s0748-7983(98)93248-6 [DOI] [PubMed] [Google Scholar]
- 18.Horvath LE, Yordan E, Malhotra D, et al. Multidisciplinary care in the oncology setting: historical perspective and data from lung and gynecology multidisciplinary clinics. J Oncology Practice. 2010;6(6):e21-e26. doi: 10.1200/jop.2010.000073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nedeltchev K, Arnold M, Wahl A, et al. Outcome of patients with cryptogenic stroke and patent foramen ovale. J Neurol Neurosurg Psychiatry. 2002;72(3):347-350. doi: 10.1136/jnnp.72.3.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oudhoff JP, Timmermans DRM, Knol DL, Bijnen AB, van der Wal G. Waiting for elective general surgery: impact on health related quality of life and psychosocial consequences. BMC Public Health. 2007;7(1):164. doi: 10.1186/1471-2458-7-164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alkhouli M, Graff-Radford J, Holmes DR. The heart-brain team—towards optimal team-based coordinated care. JAMA Cardiol. 2018;3(3):187-188. doi: 10.1001/jamacardio.2017.5072 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data not published within this article will be made available on reasonable request from any qualified investigator.