Abstract
Background:
Currently, there is poor evidence of the effect of hydrotherapy on patients with knee osteoarthritis (OA). The authors performed a meta-analysis from randomized controlled trials to determine the efficacy and safety of a hydrotherapy program on measures of pain and knee function in individuals living with knee OA.
Methods:
A literature review included PubMed, EMBASE, Cochrane Library, Science Citation Index, ScienceDirect, and Ovid. Studies evaluating the efficacy of hydrotherapy for knee OA up to August 2023 were included. The research was reported based on the preferred reporting items for systematic reviews and meta-analysis guidelines to ensure the reliability and verity of results. Statistical analysis was performed using Stata/SE version 15.0.
Results:
A total of six randomized controlled trials were included for data extraction and meta-analysis. The present study revealed that there were significant differences between the two groups regarding the pain intensity at 1 week (WMD=−0.429; 95% CI: −0.679 to −0.179; P=0.001), 4 week (WMD=−0.308; 95% CI: −0.587 to −0.030; P=0.030) and 8 week (WMD=−0.724; 95% CI: −1.099 to −0.348, P<0.001). Furthermore, hydrotherapy was associated with improved outcome of the Western Ontario and McMaster Universities Arthritis index at 1 week (WMD=−3.314; 95% CI: −6.484 to −0.145, P=0.040), 4 week (WMD= −3.630; 95% CI: −6.893 to −0.366, P=0.029) and 8 week (WMD=−3.775; 95% CI: −7.315 to −0.235; P=0.037). No serious adverse events were observed in all patients who received hydrotherapy.
Conclusion:
Hydrotherapy is efficacious and safe for reducing pain and improving functional status in individuals with knee OA, without increasing the risk of adverse effects.
Keywords: hydrotherapy, knee osteoarthritis, meta-analysis, pain
Introduction
Highlights
Hydrotherapy is efficacious and safe for reducing pain.
Hydrotherapy is associated with an improved knee joint function.
No significant difference in terms of adverse events was found in two groups
Osteoarthritis (OA), a leading cause of chronic joint pain and disability, has a seriously impact on the health of the individuals1. Patients with moderate to severe OA often suffer from excruciating pain with chronic inflammation and reduced range of motion, especially in the knee. It is a slowly progressive, disabling joint disorder which affects quality of life. Radiographic changes of OA occur in the majority of people by age 65 and are present in more than 80% of people over age 752,3. Conventional treatment of knee OA include nonpharmacologic therapies and pharmacologic therapies. Analgesics, low potency opioids, narcotic analgesics, and NSAIDs are commonly used in pharmacologic therapies4,5. Although they have certain curative effect on relieving joint pain, several therapies are generally accompanied by poor tolerance or adverse drug reactions, including circulatory system disorders, upper renal impairment, gastrointestinal disorders, and risk of dependence or addiction. Individuals with NSAIDs intolerance or inadequate analgesia have fewer drugs available.
Hydrotherapy is recommended as a treatment option in the elderly population because it is performed in a safer environment with a lower risk of falls than land-based exercises6. It has been reported to have positive outcomes on multiple body system functions, including cardiovascular, metabolic, and musculoskeletal functioning. Ellapen et al. 7 reported that hydrotherapy improves patients with spinal cord injury underwater gait-kinematics, cardiorespiratory and thermoregulatory responses and reduces spasticity. Hydrotherapy was a cost-effective rehabilitation compared to land-based therapy for a population with musculoskeletal disorders. However, the benefit of hydrotherapy was not observed in patients with knee OA. Recently, more and more studies have suggest that hydrotherapy was associated with an improved outcomes for patients with OA. Therefore, we performed a meta-analysis from randomized controlled trials (RCTs) to determine the efficacy and safety of a hydrotherapy program on measures of pain and knee function in individuals living with knee OA.
Materials and methods
Study selection
The systematic review and meta-analysis were done according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)8 (Supplemental Digital Content 1, http://links.lww.com/JS9/B508) (Supplemental Digital Content 2, http://links.lww.com/JS9/B509) and AMSTAR (Assessing the methodological quality of systematic reviews) guidelines9 (Supplemental Digital Content 3, http://links.lww.com/JS9/B510). PubMed, EMBASE, Cochrane Library, Science Citation Index, ScienceDirect, and Ovid were searched exhaustively from inception to August 2023. The search was restricted to articles published in the English language. The search terms included ‘hydrotherapy’, ‘knee’, ‘osteoarthritis’, and ‘randomized’. Manual search of bibliographies from reviews and selected studies was also performed for additional articles. Search strategy of PubMed was shown as supplementary (Supplemental Digital Content 4, http://links.lww.com/JS9/B511).
Selection criteria and eligibility criteria
Studies were included on the basis of the following criteria: (1) RCTs; (2) studies that compared hydrotherapy with placebo for the treatment of knee OA; (3) outcome measurements: pain intensity, The Western Ontario and McMaster Universities Arthritis (WOMAC) index, short form 12 health survey, and adverse effects. Exclusion criteria included (1) case reports, crossover studies, letters, editorials, review articles, meta-analysis, and retrospective studies; (2) studies involved in animal experiments; (3) studies with deficiency data, or data cannot be extracted.
Two independent reviewers screened all titles and abstracts of the trials identified by the search strategy to determine whether they met the inclusion criteria. The full-text for each potentially eligible study was retrieved and assessed against the eligibility criteria. In cases of disagreement, a third reviewer was consulted.
Data extraction
Data were extracted by two independent authors. By discussion or by involving a third author, disagreements were addressed. The general data collected were first author, publication year, country, study type, sample size, patient age, sex ratio, length of the follow-up period, and relevant clinical outcomes. The primary outcomes were pain intensity, WOMAC index and short form 12 health survey. The secondary outcome were adverse effects. The corresponding author was consult to request missing data.
Quality assessment
Two authors independently evaluated the quality of the RCTs according to the Cochrane Handbook for Systematic Reviews of Interventions version. The content of evaluation involved sequence generation, allocation concealment, blinding of participants, blinding of outcome assessor, incomplete outcome data, reporting bias and other bias. Each part of the evaluation contain a low risk of bias, a high risk of bias, or an unclear risk of bias.
According to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology10, the quality of the evidence for all outcomes was assessed independently by two investigators. In this assessment, five indicators, which including risk of bias, inconsistency, indirectness, imprecision, and other considerations bias was applied to assess each outcome. Each indicator was classified as high, moderate, low, or very low. GRADE Pro, version 3.6 was applied to accomplish summary tables.
Statistical analysis
The meta-analysis of comparable data was performed using Review Manager 5.3 (The Nordic Cochrane Centre) and Stata/SE version 15.0 (StataCorp LLC) software. Dichotomous outcomes were pooled and reported as risk difference (RDs), while continuous outcomes were pooled and reported as weighted mean differences (WMDs). All outcomes were calculated at 95% CI. Inconsistency was quantified using the I 2 statistic and an I 2 of >50% indicated substantial heterogeneity. A random-effects model or the fixed-effect model was used depending on the heterogeneity of the studies included. A random-effects model was used for heterogeneous data. Otherwise, a fixed-effect model was used. For any variable presenting with high heterogeneity, sensitivity analysis or subgroup analysis was used to investigate the potential origin. Publication bias will be performed if there is sufficient included studies.
Results
Literature screening process
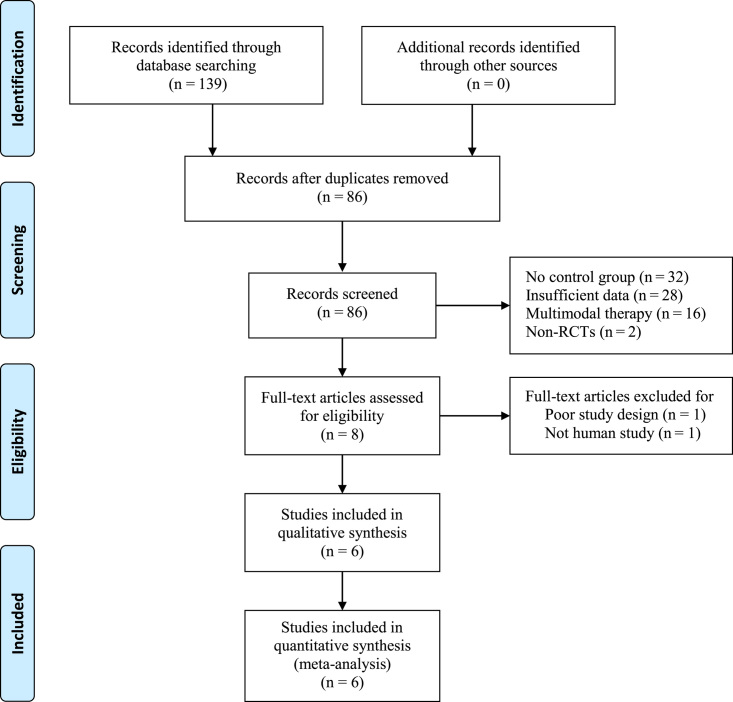
There were 139 relevant studies included according to the search strategy. After the titles and abstracts were reviewed, 53 of them were removed. A full-text review was performed for the 86 records that were maintained, and 80 of them were excluded because they did not meet the inclusion criteria. Finally, six studies representing 351 patients were included in the present meta-analysis. The process and results of literature screening were shown in Figure 1.
Figure 1.
Flow diagram of study selection.
Characteristics of included RCTs
We included six RCTs11–16 published from 2003 to 2019. In total, three studies were conducted in Australia, others were performed in Brazil, South Africa, and Germany. Experimental groups (n=183) received hydrotherapy classes and control groups (n=168) received physiotherapy. Average age ranged from 57 to 77 years old and follow-up period ranged from 4 to18 weeks. Details of the included studies were presented in Table 1.
Table 1.
Characteristics of the included studies.
| First author (Year) | Design | Mean age (years) Hydrotherapy Control | Sample size (n) Hydrotherapy Control | Gender (Female, n) Hydrotherapy Control | Intervention | Drugs | Physical therapies | Follow-up |
|---|---|---|---|---|---|---|---|---|
| Foley11 | RCT | 73 70 | 30 28 | 15 20 | Hydrotherapy group: walking forwards, sideways, and backwards through the water; knee flexion and extension, and knee cycling. Control group: physiotherapy |
Celecoxib | None | 6 weeks |
| Fransen12 | RCT | 70 71 | 55 41 | 40 34 | Hydrotherapy group: walking, bar work, seated, deep water noodle; abducted leg flexed Control group: without hydrotherapy |
Nimesulide | Infrared ray | 12 weeks |
| Silva13 | RCT | 59 59 | 32 32 | 37 40 | Hydrotherapy group: gait training: forward walking with alternated movement of the upper and lower extremities; walk raising the knee; lateral walking; backward walking Control group: without hydrotherapy |
Celecoxib | Massage | 18 weeks |
| Schencking14 | RCT | 77 72 | 10 10 | 10 7 | Hydrotherapy group: isometric strengthening; isotonic strengthening; stretching Control group: joint-specific physiotherapy (30 min, components were joint-related stretching elements, muscle strengthening of weak muscles and resistance exercises) |
Diclofenac sodium | None | 10 weeks |
| Dias15 | RCT | 71 71 | 33 32 | 20 21 | Hydrotherapy group: anterior muscle exercises, posterior muscle exercises, abduction and adduction exercises, plantar flexion exercises, closed kinetic chain exercises, multidirectional walk Control group: educational protocol and weekly advice via telephone about controlling knee loading during daily activities |
Ibuprofen | Thermal therapy | 6 weeks |
| Sekome16 | RCT | 58 57 | 18 18 | 12 13 | Hydrotherapy group: double-leg squats, double-leg calf raises, single-leg squats, single-leg calf raises, step-ups and -downs Control group: without hydrotherapy |
Celecoxib | None | 4 weeks |
RCT, randomized controlled trial.
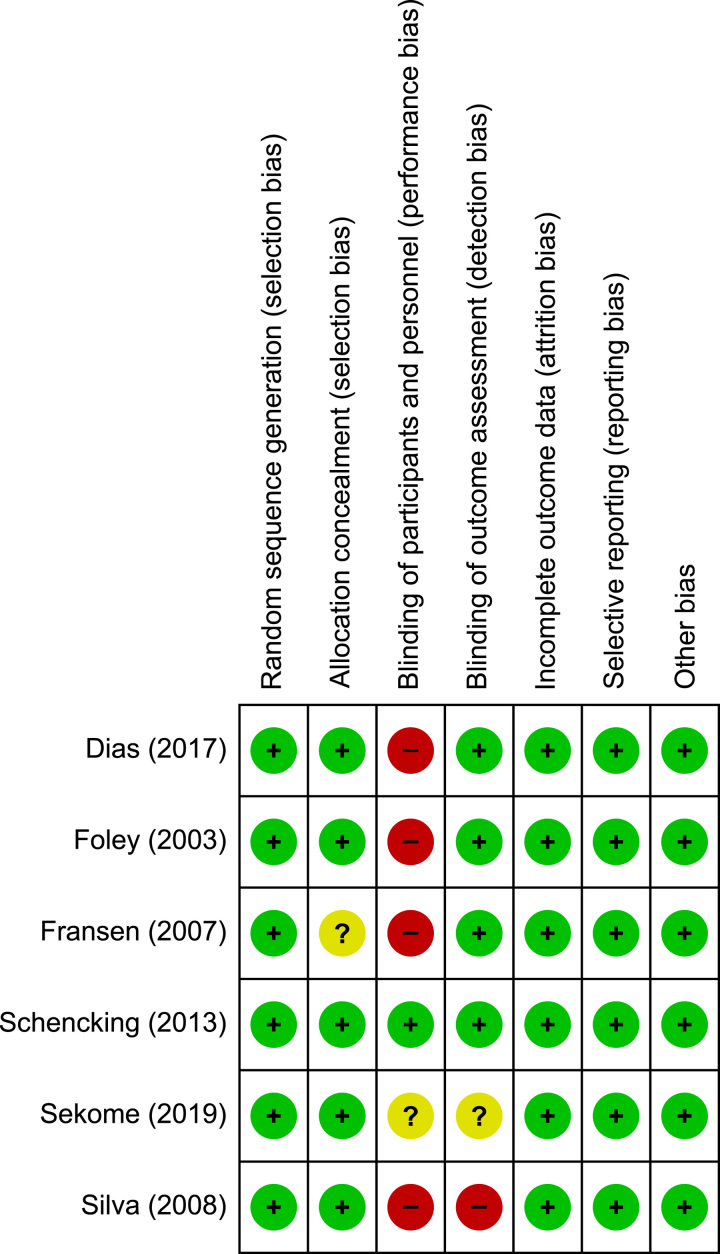
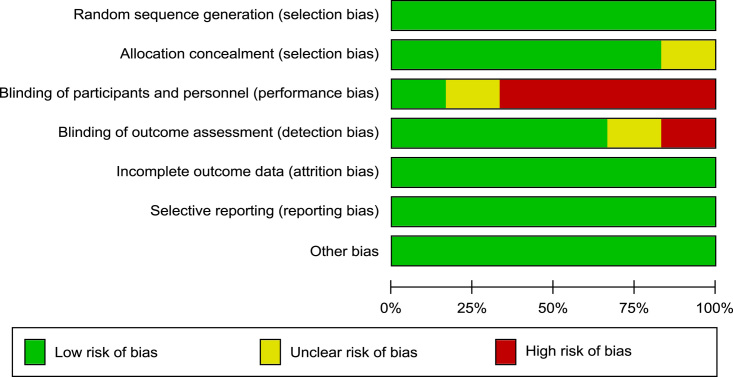
Risk of bias
The details of the risk of bias assessment can be obtained for all studies in Figure 2. All studies stated the specific way of random allocation. The allocation concealment of one article was not adequately illustrated. Only Schencking et al. 14 reported double blinding to the participants and personnel. Incomplete outcome data were low risk of bias. Each risk of the bias item was expressed in terms of the percentage across all the included articles, which indicated the proportion of risk levels for each item bias (Fig. 3).
Figure 2.
Risk of bias summary.
Figure 3.
Risk of bias graph.
Effects of interventions
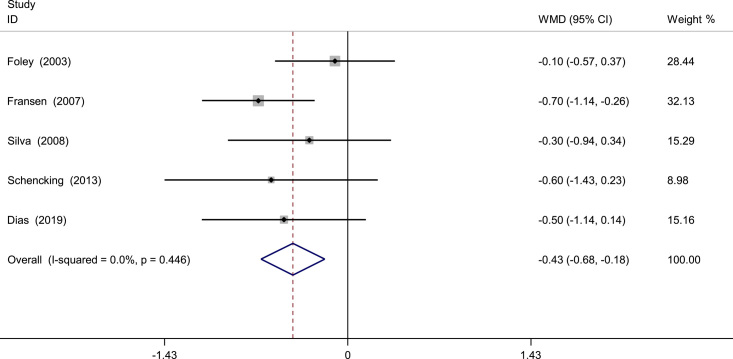
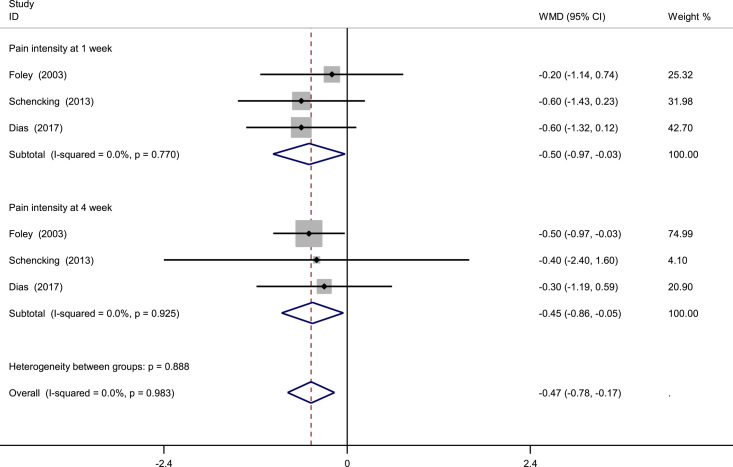
Pain intensity at 1 week
A total of five RCTs provided the data on pain intensity at 1 week. There was no significant heterogeneity and a fixed-effect model was applied (I 2= 0%, P=0.446). Our studies indicated that there was significant difference between the two groups regarding to pain intensity at 1 week (WMD=−0.429; 95% CI: −0.679 to −0.179; P=0.001; Fig. 4).
Figure 4.
Meta-analysis of pain intensity at 1 week.
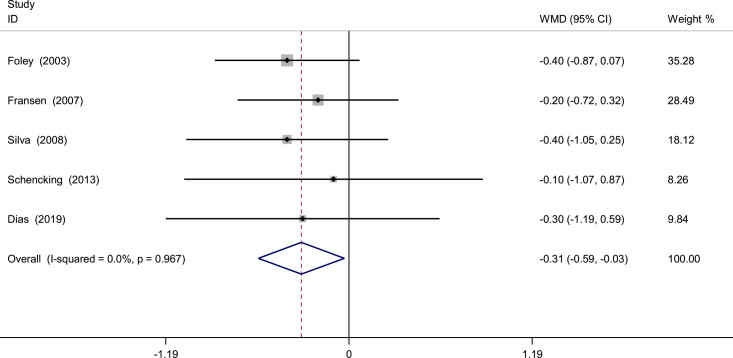
Pain intensity at 4 week
Pain intensity at 4 week was available in five studies. Based on the available data, the pooled results exhibited no significant heterogeneity (I 2=0%, P=0.967), and a fixed-effect model was utilized. The present meta-analysis indicated that hydrotherapy was associated with an improved pain relief at 4 week (WMD=−0.308; 95% CI: −0.587 to −0.030; P=0.030; Fig. 5).
Figure 5.
Meta-analysis of pain intensity at 4 week.
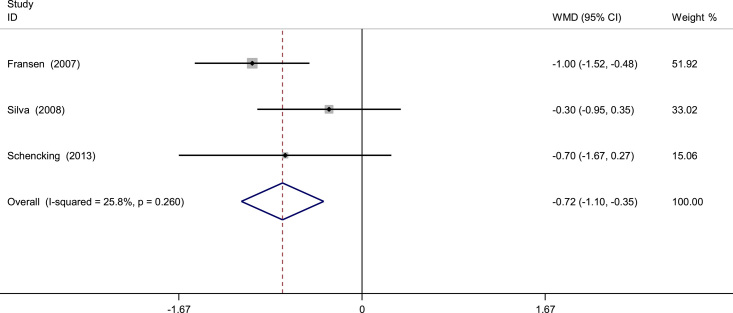
Pain intensity at 8 week
A total of three trials provided data on pain intensity at 8 week. There was no significant heterogeneity (I 2=25.8%, P=0.260), and a fixed-effect model was used. The pooled results showed significant difference between the two groups (WMD=−0.724; 95% CI: −1.099 to −0.348, P<0.001; Fig. 6).
Figure 6.
Meta-analysis of pain intensity at 8 week.
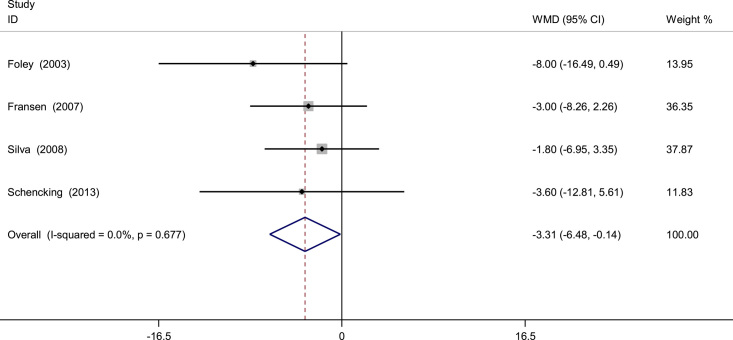
WOMAC index at 1 week
Data from four studies reported the outcome of WOMAC index at 1 week. Pooled results indicated that WOMAC index in hydrotherapy groups were significantly superior to which in control groups (WMD=−3.314; 95% CI: −6.484 to −0.145, P=0.040; Fig. 7).
Figure 7.
Meta-analysis of WOMAC index at 1 week. WOMAC, Western Ontario and McMaster Universities Arthritis.
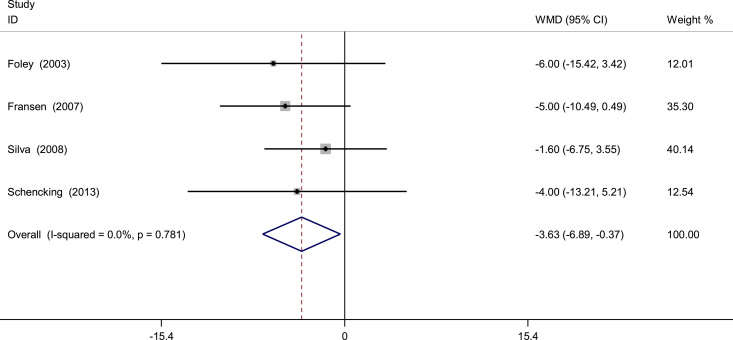
WOMAC index at 4 week
Four included studies evaluated WOMAC index at 4 week. There were significant differences between the hydrotherapy groups and the control groups (WMD=−3.630; 95% CI: −6.893 to −0.366, P=0.029; Fig. 8). A fixed-effect model was used due to no statistical heterogeneity through the meta-analysis (I 2=0%, P=0.781).
Figure 8.
Meta-analysis of WOMAC index at 4 week.
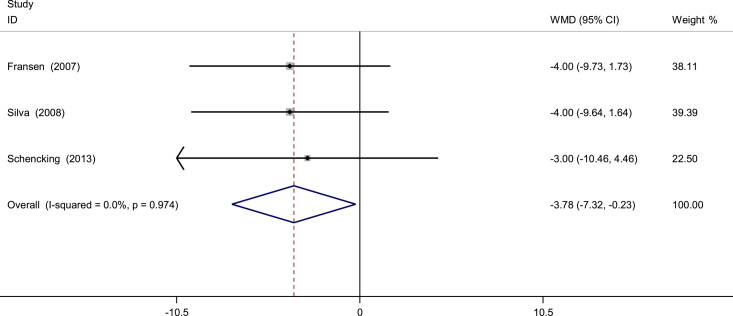
WOMAC index at 8 week
A total of three RCTs provided the data on WOMAC index at 8 week. There was no significant heterogeneity and a fixed-effect model was applied (I 2= 0%, P=0.974). Our studies indicated that there was significant difference between the two groups regarding to WOMAC index at 8 week (WMD=−3.775; 95% CI: −7.315 to −0.235; P=0.037; Fig. 9).
Figure 9.
Meta-analysis of WOMAC index at 8 week.
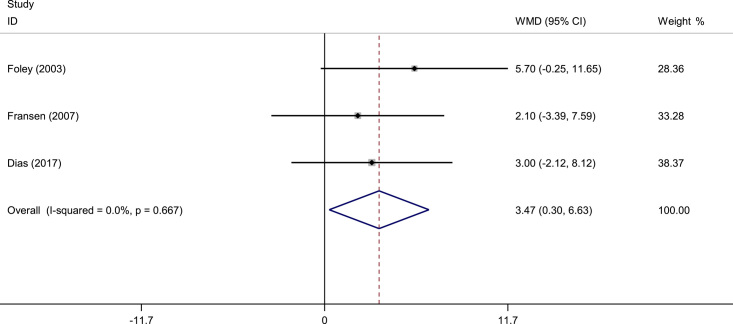
Short form 12 health survey
Short form 12 health survey was available in three studies. Based on the available data, the pooled results exhibited no significant heterogeneity (I 2=0%, P=0.667), and a fixed-effect model was utilized. The present meta-analysis indicated that hydrotherapy was associated with an improved short form 12 health survey (WMD=3.466; 95% CI: 0.298–6.635; P=0.032; Fig. 10).
Figure 10.
Meta-analysis of short form 12 health survey.
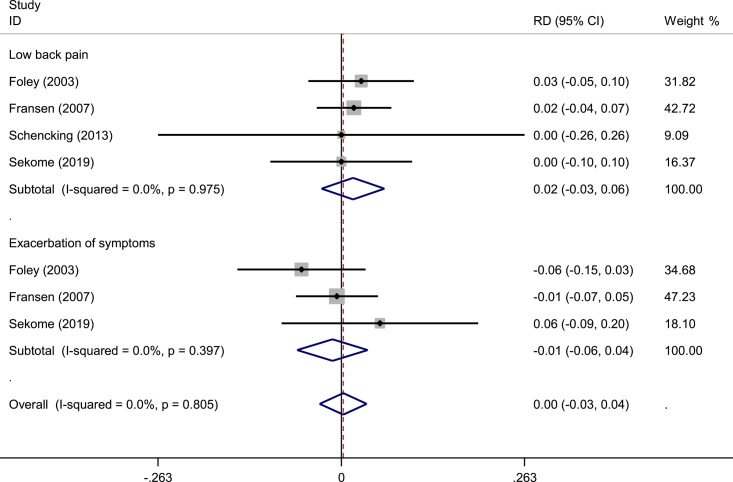
Adverse events
Four studies reported the adverse events after treatment. There was no significant heterogeneity among studies (I 2=0%, P=0.805) and a fixed-effect model was adopted. No significant difference in terms of adverse events was found in two groups (WMD=0.003; 95% CI: −0.031–0.037; P=0.870; Fig. 11).
Figure 11.
Meta-analysis of adverse effects.
Quality of the evidence and recommendation strengths
A summary of the quality of the evidence based on the GRADE approach was listed in Table 2. The evidence quality for each outcome was moderate to low. Therefore, we agree that the overall evidence quality was low, which indicates that further research is very likely to have an important impact on confidence in the estimate of effect and is likely to change the estimate.
Table 2.
Quality of the evidence and recommendation strengths.
| Quality assessment | |||||||
|---|---|---|---|---|---|---|---|
| Number of RCT | Limitations | Inconsistency | Indirectness | Imprecision | Outcome measures | Quality | Importance |
| Pain intensity at 1 week | |||||||
| 5 | Serious limitations | No serious inconsistency | No serious indirectness | No serious indirectness | WMD=−0.429; 95% CI: −0.679 to −0.179 | Moderate | Critical |
| Pain intensity at 4 week | |||||||
| 4 | Serious limitations | No serious inconsistency | No serious indirectness | No serious indirectness | WMD=−0.308; 95% CI: −0.587 to −0.030 | Moderate | Critical |
| Pain intensity at 8 week | |||||||
| 3 | Serious limitations | No serious inconsistency | No serious indirectness | No serious indirectness | WMD=−0.724; 95% CI: −1.099 to −0.348 | Moderate | Critical |
| WOMAC index at 1 week | |||||||
| 4 | Serious limitations | No serious inconsistency | No serious indirectness | No serious indirectness | WMD=−3.314; 95% CI: −6.484 to −0.145 | Moderate | Critical |
| WOMAC index at 4 week | |||||||
| 4 | Serious limitations | No serious inconsistency | No serious indirectness | No serious indirectness | WMD=−3.630; 95% CI: −6.893 to −0.366 | Moderate | Critical |
| WOMAC index at 8 week | |||||||
| 3 | Serious limitations | No serious inconsistency | No serious indirectness | No serious indirectness | WMD=−3.775; 95% CI: −7.315 to −0.235 | Moderate | Critical |
| Short form 12 health survey | |||||||
| 3 | Serious limitations | No serious inconsistency | No serious indirectness | No serious indirectness | WMD=3.466; 95% CI: 0.298–6.635 | Moderate | Critical |
| Adverse effects | |||||||
| 4 | Serious limitations | Serious inconsistency | No serious indirectness | No serious indirectness | WMD=0.003; 95% CI: −0.031 to 0.037 | Low | Critical |
WOMAC, Western Ontario and McMaster Universities Arthritis.
Subgroup analysis
Subgroup analysis was performed based on the treatment of control groups (hydrotherapy or rest). Similarly, pooled results indicated that pain intensity in hydrotherapy groups were significantly superior to which in control groups (Fig. 12).
Figure 12.
Subgroup analysis.
Discussion
This study is the first systematic review and meta-analysis of the clinical efficacy and safety of hydrotherapy for reducing pain and improving joint function in patients with knee OA. The main findings of this meta-analysis are that the hydrotherapy is associated with improved pain relief and WOMAC index. There are significant differences between groups regarding the short form 12 health survey. Furthermore, no serious adverse events are observed in all patients who received hydrotherapy.
OA of the knee is a major cause of pain and locomotor disability worldwide and chronic pain that restricts function of knee joints. Age is a major risk factor for knee OA17. Given the increasing prevalence and incidence of OA, it is now considered a major public health problem not only in the United States but also worldwide. By 2030, it is predicted that 67 million people in the United States will be diagnosed with OA18. The weight-bearing joints are most frequently affected, such as knees and hips. Effective pain management plays a vital role in the treatment for OA, as well as improving the prognosis. Conservative treatment is the first choice for early-stage knee OA including physical therapy, intra-articular injections (platelet rich plasma, glucocorticoids, glucosamine, and hyaluronic acid) and oral anti-inflammatory drugs19–21.
Hydrotherapy has been shown to have positive outcomes on multiple body system functions, including cardiovascular, pulmonary, metabolic and musculoskeletal functioning22. For knee OA, hydrotherapy can provide physiological and biomechanical benefits compared to traditional exercises, which contributes to better clinical outcomes. Aquatic buoyancy potentially decreases weight-bearing stresses on knee, and muscles. Chae et al. 23 reported that stroke patients showed improvement in postural balance and paretic knee extensor strength with hydrotherapy. Hydrotherapy exhibited significant effects on improving postural balance in chronic patients than in subacute patients. Pinto et al. 24 concluded that hydrotherapy, combined or not with other therapies, may improve balance and functional mobility of patients with Parkinson disease when compared to land-based therapy alone or usual care. However, few study has determined whether hydrotherapy can relieve knee OA pain. Our meta-analysis revealed that the hydrotherapy was associated with improved pain relief within 8 week. Due to the limited number of the included studies, this evidence does not clarify the effectiveness of different types of hydrotherapy program and further research is required.
The destruction of the articular cartilage renders it less capable to distribute large loads, more susceptible to stress, and less capable to reduce friction within the joint space25. As a consequence, knee range of motion is limited. Although intra-articular injection of sodium hyaluronate has been widely used for several decades, the long-term benefit and cost-effectiveness are still under debate. Previous articles have suggest that intra-articular injection may accelerate the degeneration of articular cartilage, which leads to the surgical treatment. Water pressure and temperature could also lead to an increased sensory input and further help in blood circulation26. Therefore, hydrotherapy is usually recommended for patients with degenerative joint disorder as water provides a range of benefits, including the reduction of edema, and reduces loading on damaged arthritic joints. As outcome measures, WOMAC index was used for evaluating the functional restoration. Foley et al. 11 suggest that hydrotherapy was associated with superior outcome of WOMAC index compared to controls. However, Fransen et al. 12 reported that there was no statistically significant difference in WOMAC index. A total of four RCTs provided the data on WOMAC index and our study revealed that hydrotherapy could significantly improve WOMAC index. Although the outcome of hydrotherapy is so far satisfactory, there are potential concerns, including low back pain and exacerbation of symptoms. Therefore, hydrotherapy will hold less clinical value if there was a higher risk of adverse effects. Four RCTs reported the adverse events and no significant difference in terms of adverse events was found in both groups. All adverse effects were mild and no further treatment was required. In addition, hydrotherapy achieved significant improvements in the short form 12 health survey. Long-term of follow is still required to determine the efficacy and safety of hydrotherapy for knee OA.
Several methodological weakness of the included RCTs should be considered. The allocation concealment of study by Fransen et al. 12 was not adequately illustrated. Only Schencking et al. 14 reported double blinding to the participants and personnel, which may cause performance bias. Drug intervention were differed from each other. Foley et al. 11, Silva et al. 13, and Sekome et al. 16 used Celecoxib, the other three used Nimesulide, Diclofenac sodium, and Ibuprofen. Fransen et al. 12, Silva et al. 13, and Dias et al. 15 received physical therapies. These should be considered when analyzing the results. The overall evidence quality was low, which indicated that further research is likely to significantly alter confidence in the effect estimate and to change the estimate.
There are some limitations should be noted. First, some studies with a small sample size may lead to unreliable results during meta-analysis. Second, only published
articles in English were included in this meta-analysis, resulting in possible publication and language biases on the outcomes. Third, although subgroup analyses were used, the pooled results of some variables were still reported with high heterogeneity, which should be interpreted with caution. Last, the overall evidence quality is low. Further research into hydrotherapy should investigate the long-term effects of this form of exercise in patients with OA, and should also aim at measuring the effect of hydrotherapy on cardiovascular fitness.
Conclusion
Hydrotherapy is efficacious and safe for reducing pain and improving functional status in individuals with knee OA, without increasing the risk of adverse effects.
Ethical approval
Not needed.
Sources of funding
This work was supported by The Hubei Province Top Medical Youth Talent Program, Wuhan Knowledge Innovation Special Basic Research Project (2022020801010575), Clinical Research Project of Affiliated Hospital of Guangdong Medical University (LCYJ2021B004, LCYJ2019B010).
Author contribution
C.L., H.C., and S.Z.: original draft; Q.P.: data collections; J.X.: data analysis; Y.L. and Y.L.: review and editing.
Conflicts of interest disclosure
The authors declare that they have no financial conflict of interest with regard to the content of this report.
Research registration unique identifying number (UIN)
Reviewregistry1728.
Guarantor
Changjiang Lei.
Data availability statement
Data has been listed below each figure and table.
Supplementary Material
Footnotes
Haiting Chen and Su Zheng are co-authors.
Changjiang Lei, Haiting Chen, and Su Zheng equally contributed to the study.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website, www.lww.com/international-journal-of-surgery.
Published online 4 December 2023
Contributor Information
Changjiang Lei, Email: 305069071@qq.com.
Haiting Chen, Email: haiting20077@126.com.
Su Zheng, Email: zhengsu0413@126.com.
Qingyun Pan, Email: 420679896@qq.com.
Jing Xu, Email: whdwyykjk@163.com.
Yuan Li, Email: 1036679510@qq.com.
Yang Liu, Email: ljvg53w@163.com.
References
- 1. Maly MR, Marriott KA, Chopp-Hurley JN. Osteoarthritis year in review 2019: rehabilitation and outcomes. Osteoarthritis Cartilage 2020;28:249–266. [DOI] [PubMed] [Google Scholar]
- 2. Hunt MA, Charlton JM, Esculier JF. Osteoarthritis year in review 2019: mechanics. Osteoarthritis Cartilage 2020;28:267–274. [DOI] [PubMed] [Google Scholar]
- 3. Kijowski R, Demehri S, Roemer F, et al. Osteoarthritis year in review 2019: imaging. Osteoarthritis Cartilage 2020;28:285–295. [DOI] [PubMed] [Google Scholar]
- 4. Clemett D, Goa KL. Celecoxib: a review of its use in osteoarthritis, rheumatoid arthritis and acute pain. Drugs 2000;59:957–980. [DOI] [PubMed] [Google Scholar]
- 5. Fuggle N, Curtis E, Shaw S, et al. Safety of opioids in osteoarthritis: outcomes of a systematic review and meta-analysis. . Drugs aging 2019;36(suppl 1):129–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vanderlaan J. Retrospective cohort study of hydrotherapy in labor. J Obstet Gynecol Neonatal Nurs 2017;46:403–410. [DOI] [PubMed] [Google Scholar]
- 7. Ellapen TJ, Hammill HV, Swanepoel M, et al. The benefits of hydrotherapy to patients with spinal cord injuries. Afr J Disabil 2018;7:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Page MJ, McKenzie JE, Bossuyt PM. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 9. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Foley A, Halbert J, Hewitt T, et al. Does hydrotherapy improve strength and physical function in patients with osteoarthritis–a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis 2003;62:1162–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fransen M, Nairn L, Winstanley J, et al. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum 2007;57:407–414. [DOI] [PubMed] [Google Scholar]
- 13. Silva LE, Valim V, Pessanha AP, et al. Hydrotherapy versus conventional land-based exercise for the management of patients with osteoarthritis of the knee: a randomized clinical trial. Phys Ther 2008;88:12–21. [DOI] [PubMed] [Google Scholar]
- 14. Schencking M, Wilm S, Redaelli M. A comparison of Kneipp hydrotherapy with conventional physiotherapy in the treatment of osteoarthritis: a pilot trial. J Integr Med 2013;11:17–25. [DOI] [PubMed] [Google Scholar]
- 15. Dias JM, Cisneros L, Dias R, et al. Hydrotherapy improves pain and function in older women with knee osteoarthritis: a randomized controlled trial. Braz J Phys Ther 2017;21:449–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sekome K, Maddocks S. The short-term effects of hydrotherapy on pain and self-perceived functional status in individuals living with osteoarthritis of the knee joint. S Afr J Physiother 2019;75:476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ashford S, Williard J. Osteoarthritis: a review. Nurse Pract 2014;39:1–8. [DOI] [PubMed] [Google Scholar]
- 18. Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum 2008;58:15–25. [DOI] [PubMed] [Google Scholar]
- 19. Canas CA, Osorio CJ, Coronel N, et al. Efficacy and safety of oral low-dose glucocorticoids in patients with estrogen-dependent primary osteoarthritis. Rheumatol Int 2014;34:733–735. [DOI] [PubMed] [Google Scholar]
- 20. Chen Z, Wang C, You D, et al. Platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: a meta-analysis. Medicine 2020;99:e19388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shaughnessy AF. Chondroitin/glucosamine equal to celecoxib for knee osteoarthritis. Am Fam Physician 2016;93:1032. [PubMed] [Google Scholar]
- 22. Bender T, Karagulle Z, Balint GP, et al. Hydrotherapy, balneotherapy, and spa treatment in pain management. Rheumatol Int 2005;25:220–224. [DOI] [PubMed] [Google Scholar]
- 23. Chae CS, Jun JH, Im S, et al. Effectiveness of hydrotherapy on balance and paretic knee strength in patients with stroke: a systematic review and meta-analysis of randomized controlled trials. Am J Phys Med Rehabili 2020;99:409–419. [DOI] [PubMed] [Google Scholar]
- 24. Pinto C, Salazar AP, Marchese RR, et al. The effects of hydrotherapy on balance, functional mobility, motor status, and quality of life in patients with parkinson disease: a systematic review and meta-analysis. J Injury Funct Rehab 2019;11:278–291. [DOI] [PubMed] [Google Scholar]
- 25. Stevenson KL, Neuwirth AL, Sheth N. Perioperative pain management following total joint arthroplasty: a review and update to an institutional pain protocol. J Clin Orthop Trauma 2018;9:40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Biscarini A, Cerulli G. Modeling of the knee joint load in rehabilitative knee extension exercises under water. J Biomech 2007;40:345–355. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data has been listed below each figure and table.