Abstract
Introduction:
Human papillomavirus (HPV) vaccination protects against HPV-associated cancers and genital warts. Healthy People 2030 goal for HPV vaccine uptake is 80%, but as of 2021, only 58.5% of adolescents are up to date in Georgia. The purpose of the study is to assess the attitudes, vaccine practices, facilitators, and barriers to receiving the HPV vaccine in southwest Georgia.
Methods
We conducted 40 semi-structured interviews with three different audiences (young adults, parents, and providers and public health professionals) guided by the P3 (patient-, provider-, practice-levels) model and used deductive coding approach. Young adults and parents were interviewed to assess their perceived benefits, barriers, and susceptibility of the HPV vaccine. Providers and public health professionals were interviewed about facilitators and barriers of patients receiving the HPV vaccine in their communities.
Results
Out of the 40 interviews: 10 young adults, 20 parents, and 10 providers and public health professionals were interviewed. Emerging facilitator themes to increase the uptake of the HPV vaccine included existing knowledge (patient level), providers’ approach to the HPV vaccine recommendations (provider level) and immunization reminders (practice level). Barrier themes were lack of knowledge around HPV and the HPV vaccine (patient level), need for strong provider recommendation and discussing the vaccine with patients (provider level), and limited patient reminders and information (practice level).
Conclusions
These interviews revealed key themes around education, knowledge, importance of immunization reminders, and approaches to increasing the HPV vaccination in rural Georgia. This data can inform future interventions across all levels (patient, provider, practice, policy, etc.) to increase HPV vaccination rates in rural communities.
Keywords: adolescent, parents, young adults, providers, health systems, HPV vaccination, Cancer prevention, rural health
INTRODUCTION
Human papillomavirus (HPV) is a common sexual transmitted infection (STI) in the United States (US) with an estimated prevalence of 42.5 million people and an incidence of 13 million people.1 HPV-associated cancers can develop years or decades following persistent HPV infection. There are six HPV-associated cancers: -vulvar, vaginal, cervical, penile, anal, and oropharyngeal. Between 2015 and 2019, it was estimated HPV caused 47,199 new cancer cases each year.2 HPV vaccine was developed to prevent HPV-associated cancers and genital warts;3 currently HPV vaccine is one of two cancer prevention vaccines available globally.4
Previous research determined each HPV vaccine is safe and has at least 96% efficacy for preventing HPV-associated cancers.5 HPV vaccination was recommended in the US for adolescent females in 2006, and for adolescent males in 2011.6 The Advisory Committee on Immunization Practices (ACIP) recommends that people receive the vaccine as early as age 9 and up to age 26; the vaccine can also be received up to age 45, based on a provider-patient shared decision making process.7 The earlier a person receives the HPV vaccine before engaging in sexual activity, the better protected they will be from HPV-associated cancers and genital warts.8 If the vaccine is initiated prior to the 15th birthday, vaccine recipients need to complete a two-dose vaccine series; if the first dose is given after the 15th birthday, vaccine recipients need to complete a three-dose series.9 Healthy People 2030 offers standardized 10-year measurable health objectives for the United States. Among their target goals is to have 80% of adolescents aged 13 to 15 receive all recommended doses of the HPV vaccine. As of 2021, the current national rate is suboptimal at 58.5%.10 Low HPV vaccine uptake is due to barriers that exist at multiple levels of the socio-ecological model.
According to the National Immunization Survey-Teen (NIS-Teen) data from 2022, 76.0% of adolescents aged 13–17 have received at least one HPV vaccine dose with 62.6% having completed the series.11 Comparatively, other adolescent vaccines such as Tdap and meningococcal are closer to 90% for receiving one dose.11 Compared to the national percentage from the NIS-Teen 2022, Georgia’s HPV vaccine initiation and up-to-date rates among adolescents aged 13–17 are 70.8% and 61.5%, respectively.12 Adolescents residing in rural areas compared to urban areas have lower initiation (68% versus 77.8%) and up-to-date (49.2% versus 60.4%) HPV vaccination rates from NIS-Teen 2020.13 Similarly, in the District of Albany (rural GA), only 47.9% adolescents ages 13–17 were up-to-date on their HPV vaccinations, which is 13% lower than the rest of the state, provided by Georgia Registry of Immunization Transactions and Services (GRITS).14 Limited research has focused on rural underserved communities related to the HPV vaccine.15
Research has examined facilitators and barriers at the patient-(adolescent & parent), provider-, and practice-levels. The facilitators at both the patient- and provider-levels are patient’s trust in the provider, knowledge of the vaccine, and self-efficacy in one’s own ability to discuss the vaccine.16,17 For practice-level, the facilitators are the availability of the vaccine, scheduling future vaccine appointments, and prioritizing the vaccine.16 The barriers at the patient- and provider-levels are the lack of knowledge and self-efficacy discussing the vaccine, concerns about safety and adverse effects, and not receiving provider recommendation for HPV vaccine.16,18 The barriers for practice-level are lack of access to vaccine provider, clinic logistics, and reminder system.17 Few studies have researched the HPV vaccine in rural, underserved areas, and even fewer in rural southwest Georgia regarding the facilitators and barriers of the vaccine intersecting at multiple levels of the socio-ecological model.16,19–22
This qualitative study aimed to identify socio-ecological determinants influencing HPV vaccination uptake among parents, young adults, and public health professionals and providers. We applied the P3 (patient-, provider-, practice-levels) Model to understand parents and young adults perceived susceptibility, severity, barriers, and benefits in HPV vaccination uptake and completion.23 For providers and public health professionals, we assessed their facilitators and barriers related to HPV vaccine uptake. This unique model allows us to examine all three levels at the same time and how they impact each other, specifically around HPV vaccination. These results can inform the development of multi-level interventions to increase HPV vaccination uptake in rural communities.
METHODS
Recruitment
We conducted a cross-sectional qualitative study to assess attitudes, knowledge, perceived severity and susceptibility and reasons for HPV vaccination uptake (or lack of) among parents and young adults. Between September 2020 to March 2022, a series of 40 interviews were virtually conducted with participants from southwest Georgia. The study was deemed exempt by the Institutional Review Board at Emory University.
Interview Guide Development
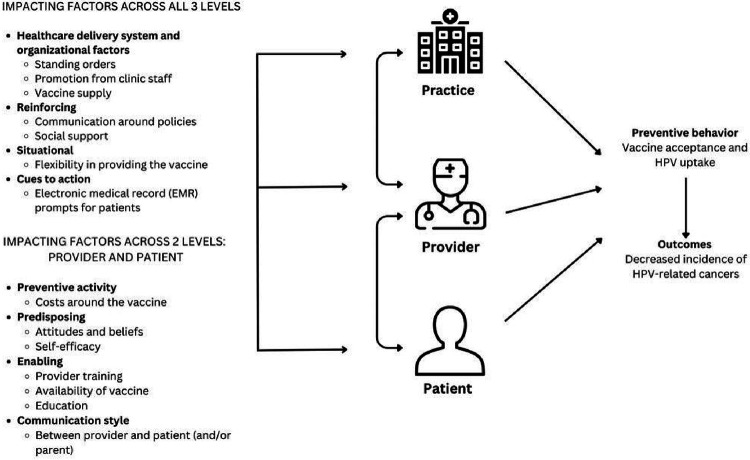
The interview guides were informed by the P3 Model and the socio-ecological model.23 The P3 Model is a unique approach since it encompasses not one but all three levels (patient, provider, and practice) of the clinic approach and integrates key components of health promotion and behavioral theoretical models (e.g., Health Belief Model, Theory of Planned Behavior and ecological models (Social Ecological Model) to impact health outcomes (Fig. 1).23 This framework addresses limitations in existing rural health literature on HPV vaccine by considering healthcare system components beyond patient-level factors influencing parents’ and young adults’ vaccination decisions.15,23 From the socio-ecological model, we included questions beyond the P3 Model including community and policy level factors.
Figure 1.
The HPV Vaccine applied to the P3 (practice, provider, and patient level) Model
The interview guide and methods were reviewed by the study team and a community advisory board working group from our Emory Prevention Research Center. This study includes diverse participant categories. The parent of a child and young adult categories were split into two groups: 1) vaccinated and 2) unvaccinated. The eligibility criteria for parents with a vaccinated child is a parent whose child received at least one dose of the HPV vaccine. The eligibility criteria of the interview sample are in Table 1. We used snowballing and convenience sampling methods for participant recruitment and recruited only from southwest Georgia. Participants (e.g., parents and young adults) were recruited from the Emory Prevention Research Center Community Advisory Board and Facebook advertisements. Some parents, young adults, and providers were recruited from elementary schools and universities. Public health professionals were recruited from non-profits and health agencies through word of mouth and fliers.
Table 1.
Interview Sample and Eligibility Criteria
| Interview Group | Sample Number | Eligibility Criteria |
|---|---|---|
| Parents with a vaccinated child | 10 | • A parent of a child ages 9–17 • Has a child who has completed at least the first dose of the HPV vaccine series, if not all doses |
| Parents with an unvaccinated child | 10 | • A parent of a child ages 9–17 • Has a child who did not receive any doses of the HPV vaccine series |
| Young adults vaccinated | 5 | • An adult age 18–35 who completed the 2 or 3 dose series |
| Young adults unvaccinated | 5 | • An adult age 18–35 who did not complete the 2 or 3 dose series |
| PCPs or providers at clinics or health department or public health staff | 10 | • Physicians, nurses, or other providers who work in a clinical setting or a person in a health department or public health organization |
At the interview, the participant was told about the study, their role and risks and benefits of the study and consented to participate and being recorded. Emory staff (coordinators and students) who were trained on the study and the interview guide conducted the interviews. The interviews lasted between 30–45 minutes and participants were compensated with a $25 electronic gift card.
The qualitative study had three interview guides for the different audiences. The questions revolved around six topical categories, including: 1) knowledge, 2) facilitators to receipt of the HPV vaccine, 3) barriers to receipt of the HPV vaccine, 4) healthcare delivery factors, 5) community and resources, and 6) demographics (Table 2). For providers, we also asked about promotional methods for the vaccine, use the Vaccine for Children’s program, staffing and supply issues, and if they have strategies or have received training on how to talk to patients and parents about the HPV vaccine. For parents and young adults, we asked about preventive care and interaction with their provider. Across all categories, we assessed participant demographics, including age, gender, race, and ethnicity (whether they are Hispanic/Spanish descent). For providers and public health professionals, we inquired about their title and discipline, the organization they work for and how long they have worked there.
Table 2.
Interview Guide Topics
| Topical Domain | Example of questions |
|---|---|
| Knowledge |
What can you tell me about the HPV vaccine?
Are you aware of cancers that are linked to HPV vaccine? |
| Attitudes |
How well do you think the HPV vaccine works?
How would you describe the HPV vaccine? |
| Facilitators to Receipt of the Vaccine |
What education does your doctor provide about the HPV vaccination? Can you tell me about each of them?
What materials have you seen or heard about the HPV vaccine in your community? |
| Barriers to Receipt of the Vaccine |
What do you think gets in the way of children or teens getting vaccinated? What are barriers related to parents or teens in general? Individual: Knowledge, costs, attitudes/thoughts about vaccine What are barriers at providers’ offices or clinics? |
| Healthcare delivery factors | What education does your doctor provide about the HPV vaccine? |
| Community and resources | What materials have you seen or heard about the HPV vaccine in your community |
| Demographics | Gender, age, insurance status, employment, education, # of children, children been vaccinated (self-report) Healthcare Provider/staff: title, type of organization, # of years at that organization |
Analysis
The interviews were recorded via Zoom or with an audio recorder and transcribed by a professional transcription service. We used standard qualitative methods for the analyses including iterative codebook development, coding of transcripts, and matrices of themes.24 A codebook with definitions was developed using a deductive coding approach from the three interview guides (parent, young adult, and health systems) and the P3 Model and inductive codes. All transcripts were uploaded to MAXQDA for analysis.25 Two trained researchers coded each transcript with the secondary coder reviewing coding from the primary coder. If there were discrepancies, then the coders would meet to discuss and come to an agreement. Thematic data analysis was applied and coding results were discussed and emerging themes were identified.26 We created matrices of the facilitators and barriers to receiving the HPV vaccine using the P3 Model and the socio-ecological model (community and policy).
RESULTS
We had 10 young adults, 20 parents, and 10 providers and public health professionals participating in the qualitative study. The young adults were 80% female and 20% male, 60% Black, and 40% White, 90% non-Hispanic and 10% Hispanic. The parents were 95% female and 5% male, 60% Black, 35% White, and 5% not specified. Adolescents were 53% female and 47% male, 42% were ages 9–12, 48% were ages 13–17 and 10% were 18 and over. Health system participants were 90% female, 10% male, 60% Black and 30% White and 10% not specified. More than half of participants identified as African American (60%), about a third identified as White (35%), and 5% of participants did not specify their race. Additional demographics of the sample are displayed in Table 3 and Table 4 and county representation in Supplemental Table 1.
Table 3.
Demographics of Participants
| Participant Demographics | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | All Participants (N=30) | Young Adults (N=10) | Parents of Non-Vaccinated Children (N=10) | Parents Of Vaccinated Children (N=10) | |||||
| N | % | N | % | N | % | N | % | ||
| Age | 18–34 | 12 | 40% | 10 | 100% | 1 | 10% | 1 | 10% |
| 35–44 | 9 | 30% | - | - | 5 | 50% | 4 | 40% | |
| 45–54 | 7 | 23% | - | - | 3 | 30% | 4 | 40% | |
| 55–64 | 2 | 7% | - | - | 1 | 10% | 1 | 10% | |
| Gender | Female | 27 | 90% | 8 | 80% | 9 | 90% | 10 | 100% |
| Male | 3 | 10% | 2 | 20% | 1 | 10% | 0 | 0% | |
| Race | Black | 18 | 60% | 6 | 60% | 5 | 50% | 7 | 70% |
| White | 11 | 37% | 4 | 40% | 4 | 40% | 3 | 30% | |
| Not Specified | 1 | 3% | 0 | 0% | 1 | 10% | 0 | 0% | |
| Ethnicity | Non-Hispanic | 28 | 93% | 9 | 90% | 10 | 100% | 9 | 90% |
| Hispanic | 2 | 7% | 1 | 10% | 0 | 0% | 1 | 10% | |
| Highest Level of Education | Associates | 4 | 13% | 3 | 30% | 1 | 10% | 0 | 0% |
| Some College | 7 | 23% | 0 | 0% | 2 | 20% | 5 | 50% | |
| Bachelors | 12 | 40% | 6 | 60% | 3 | 30% | 3 | 30% | |
| Masters | 7 | 23% | 1 | 10% | 4 | 40% | 2 | 20% | |
| Employment Status | Full-Time | 14 | 47% | 3 | 30% | 5 | 50% | 6 | 60% |
| Part-Time | 4 | 13% | 2 | 20% | 1 | 10% | 1 | 10% | |
| Unemployed | 3 | 10% | 1 | 10% | 2 | 20% | 0 | 0% | |
| Student | 4 | 13% | 3 | 30% | 0 | 0% | 1 | 10% | |
| Retired | 1 | 3% | 0 | 0% | 0 | 0% | 1 | 10% | |
| Self-Employed | 3 | 10% | 1 | 10% | 2 | 20% | 0 | 0% | |
| Unable to Work/Disabled | 1 | 3% | 0 | 0% | 0 | 0% | 1 | 10% | |
| Insurance Status | Insured | 28 | 93% | 10 | 100% | 9 | 32% | 9 | 32% |
| Uninsured | 2 | 7% | 0 | 0% | 1 | 10% | 1 | 10% | |
| Marital Status | Single | 16 | 53% | 8 | 80% | 3 | 30% | 5 | 50% |
| Married | 9 | 30% | 2 | 20% | 4 | 40% | 3 | 30% | |
| Divorced/Widowed | 5 | 17% | - | 0% | 3 | 30% | 2 | 20% | |
| HPV Vaccination Status | Started Series | 11 | 44% | 5 | 56% | 0 | 0% | 6 | 38% |
| Completed Series | 14 | 56% | 4 | 44% | 0 | 0% | 10 | 62% | |
| Number of Children per Participant | 1 child | 10 | 50% | - | - | 6 | 60% | 4 | 40% |
| 2 children | 9 | 45% | - | - | 3 | 30% | 6 | 60% | |
| 3 children | 1 | 5% | - | - | 1 | 10% | - | - | |
| Ages of Children | 9 to 12 | 13 | 42% | - | - | 8 | 53% | 5 | 31% |
| 13 to 17 | 15 | 48% | - | - | 6 | 40% | 9 | 56% | |
| 18+ | 3 | 10% | - | - | 1 | 7% | 2 | 13% | |
| Gender of Children | Male | 15 | 47% | - | - | 7 | 47% | 8 | 47% |
| Female | 17 | 53% | - | - | 8 | 53% | 9 | 53% | |
Table 4.
Demographics of Provider
| Provider Demographics | |||
|---|---|---|---|
| Variable | Health Systems (N=10) | ||
| N | % | ||
| Age | 18–34 | 1 | 10% |
| 35–44 | 4 | 40% | |
| 45–54 | 2 | 20% | |
| 55–64 | 1 | 10% | |
| 65 and Above | 0 | 0% | |
| Unspecified | 1 | 10% | |
| Gender | Female | 9 | 90% |
| Male | 0 | 0% | |
| Not Specified | 1 | 10% | |
| Race | Black | 6 | 60% |
| White | 3 | 30% | |
| Not Specified | 1 | 10% | |
| Ethnicity | Non-Hispanic | 9 | 90% |
| Hispanic | 0 | 0% | |
| Not Specified | 1 | 10% | |
| Discipline/Training | Administrator/Director | 2 | 20% |
| Doctor/Physician | 1 | 10% | |
| LPN | 1 | 10% | |
| NP | 1 | 10% | |
| PA | 2 | 20% | |
| RN | 1 | 10% | |
| Not Specified | 2 | 20% | |
| Years at Organization | Less than 5 | 3 | 30% |
| 5 to 10 | 1 | 10% | |
| More than 10 | 4 | 40% | |
| Not specified | 2 | 20% | |
| Organization Type | Public Health | 2 | 20% |
| Health System | 2 | 20% | |
| Community-Based | 3 | 30% | |
| Healthcare Organization | 1 | 10% | |
| Not Specified | 2 | 20% | |
Facilitators
There were facilitators for receiving the HPV vaccine identified at each of the three levels in the P3 Model. Facilitators at the patient level were having existing knowledge of HPV and the HPV vaccine, knowing the vaccine is safe, having knowledge on who can receive the vaccine and when, and having trusted individuals provide information about the HPV vaccine to their community. Facilitators at the provider level were the efficacy of the vaccine, framing of the HPV vaccine to patients, and revisiting the HPV vaccination with hesitant parents. Facilitators at the practice level were immunization reminders, patient registries, the use of social media (e.g., educational videos), and other health clinics who support the vaccine. Immunization reminders was the most mentioned strategy mentioned across participants, both for the patients and providers to remind patients about the vaccine. See Table 5 for more facilitator quotes for each level.
Table 5.
Facilitator Quotes across levels
| FACILITATORS | |||
|---|---|---|---|
| Themes | Level | Subtheme (if applicable) | Quotes |
| Previous/existing knowledge of the HPV vaccine | Patient | Perception of the HPV vaccine | “I’m going to say it’s [HPV vaccine] some insurance for your child’s behaviors and actions later on in life, you know? Lots of insurance.” (Participant 7, parent of vaccinated child) |
| Patient | Trusted people are the source of truth in the community | “I think once they are educated, you know, by a trusted voice, you know, whether that’s their physician or, you know, pastor or somebody, whoever that trusted voice is for them, I think they’re more likely to be acceptable to that.” (Participant 39, health systems) | |
| Providers framing/approach on describing the HPV vaccine to parents | Provider | Providers framing the HPV vaccine as a preventative measure against other diseases | “Just putting it out and putting the information out and let them stress that it is an STD just like any other STD. Of course, with repercussions in the future, and if you can prevent it, why not.” (Participant 6, parent of vaccinated child) |
| Providers educating parents/patients on the HPV vaccine through various formats | Provider | N/A | “And I try to re-educate if they didn’t, just because a lot of it is that they kind of don’t know what HPV is. They’ve heard of the vaccine. They understand that it’s a vaccine, but I don’t think they really know what HPV is and why they should be concerned about it.” (Participant 40, health systems) |
| Health Systems immunization reminders to patients/young adults | Practice | N/A | “We have what’s called precall-recall, and so once a month we print out a list of our patients here that either they’re coming due for a set of immunizations they’ll be turning 11 in the next month. We’ll send out a letter that says your child will be due for immunizations on this day. We won’t specifically say what immunization, but we’ll say they’re due for immunizations, can you please either call the clinic and make an appointment or come by. And then if they’re overdue we’ll send them a card that says your immunizations are past due. Please call our office and come by so that your – we can get your immunizations up to date.” (Participant 9, health systems). |
| New ways to provide information about the HPV vaccine to parents/young adult | Provider | N/A | “Public health [health department clinics] was probably our biggest champions of it, and that’s why we didn’t have to do an awful lot, particularly because we were focusing on lower income and uninsured patients. So, we had been able to get the community health centers to do as much as public health was doing, that would have made a huge difference…” (Participant 12, health systems). |
| Implementing techniques for community engagement | Community | N/A | “I’d say insight into the community, definitely, to get the word out. Because if you don’t have somebody from the community that also buys in, then they’re not going to participate, not going to show up” (Participant 25, health systems) |
| Benefit of free vaccine programs | Policy | N/A | “I think we have a free program with HPV… We get them (adult patients) to sign something and then we can get it for free for people who are uninsured” (Participant 23, health systems). |
Patient level
At the patient level, participants (primarily parents of vaccinated children and young adults both vaccinated and unvaccinated) consistently referenced having existing knowledge of HPV as a facilitator to increase uptake in administering the HPV vaccine. In describing the vaccine, participants referenced a basic understanding of which cancers it can prevent, and ages at which adolescents can receive the vaccine. Parents and young adults understood the safety of the vaccine, which assisted in having positive attitudes towards the vaccine. One parent described: “I’m going to say it’s [HPV vaccine] some insurance for your child’s behaviors and actions later on in life, you know? Lots of insurance.” (Participant 7, parent of vaccinated child). For young adults, they learned about the vaccine on social media, and through school. Enlisting trustworthy individuals to connect community members with information within the community serves as another facilitator for increasing HPV vaccine uptake. A director of a non-profit alluded to this: “I think once they are educated, you know, by a trusted voice, you know, whether that’s their physician or, you know, pastor or somebody, whoever that trusted voice is for them, I think they’re more likely to be acceptable to that.” (Participant 39, health systems).
Provider level
At the provider level, parents of vaccinated children highlighted the approach their children’s providers took when discussion the HPV vaccine with them. The providers framed the vaccine as a preventative measure against other diseases. Providers often spoke of the efficacy the vaccine has against contracting and spreading sexually transmitted infections (STIs), and how those STIs may have more serious ramifications later in life. A parent described this perspective: “Just putting it out and putting the information out and let them stress that it is an STD just like any other STD. Of course, with repercussions in the future, and if you can prevent it, why not.” (Participant 6, parent of vaccinated child).
In addition to framing the discussion, several education and messaging strategies were viewed as successful facilitators; these included patient visits at clinics, health departments, and utilizing community events to educate local community members. Some health system participants offered effective strategies such as revisiting the topic with hesitant parents and using information sheets to allow the parents to learn about the vaccine and its importance. One provider described their approach: “And I try to re-educate if they didn’t, just because a lot of it is that they kind of don’t know what HPV is. They’ve heard of the vaccine. They understand that it’s a vaccine, but I don’t think they really know what HPV is and why they should be concerned about it.” (Participant 40, health systems). Parents of vaccinated children emphasized the use of brochures and pamphlets offered by providers as effective learning strategies. Some reflected on how this allowed for parents to take their time learning about the vaccine, and its benefits. Others viewed the brochure as a first step towards having a deeper conversation with the provider. Ultimately, parents thought brochures may bridge the gap for parents who do not know enough about the vaccine but want to learn more about it.
Practice level
At the practice level, immunization reminders sent to parents and young adults were seen as effective strategies by parents whose children were vaccinated and vaccinated young adults for patients to receive their HPV vaccine doses. Reminders included different formats depending on the health system, including phone calls and reminder cards. Health system participants also recognized different strategies to ensure patients returned for subsequent doses. These included the use of patient registries and highlighting those due for immunizations, as well as through the standardized Georgia Registry of Immunization Transactions and Services (GRITS), the statewide immunization information system. As one provider described their practice’s strategy:
“We have what’s called precall-recall, and so once a month we print out a list of our patients here that either they’re coming due for a set of immunizations they’ll be turning 11 in the next month. We’ll send out a letter that says your child will be due for immunizations on this day. We won’t specifically say what immunization, but we’ll say they’re due for immunizations…” (Participant 9, health systems).
Community and Policy levels
At the community and policy levels, parents with vaccinated children and health system participants discussed techniques of using central and familiar locations like schools to engage in community outreach. Another one was to have champions within the community. One provider described: “I’d say insight into the community, definitely, to get the word out. Because if you don’t have somebody from the community that also buys in, then they’re not going to participate, not going to show up” (Participant 25, health systems nurse). For policy, health system participants mentioned vaccine programs, explaining: “I think we have a free program with HPV…We get them (adult patients) to sign something and then we can get it for free for people who are uninsured” (Participant 23, health systems provider).
Barriers
The barriers for receiving the HPV vaccine at each of the three levels in the P3 Model were the lack of information and dialogue around the HPV vaccine. At the patient level, the main barriers were a dearth of education on HPV and the HPV vaccine, misinformation, and stigma as is relates to STIs and sexual intercourse. At the provider level, a deficiency exists in direct provider-patient communication, including instances where providers fail to inform and recommend the HPV vaccine to their patients. At the practice level, there are a lack of systematic reminders for patient immunizations reminders, limited information, time, staff, and resources committed to the HPV vaccine (Table 6).
Table 6:
Barrier Quotes across levels
| BARRIERS | |||
|---|---|---|---|
| Themes | Level | Subtheme (if applicable) | Quotes |
| Lack of education and knowledge | Patient | N/A | “They’re (doctor) like, oh yeah, we now offer the HPV vaccine. Is it something you want to get? And my mom was like, eh, no, she doesn’t need that right now. And I was like, okay. I don’t really want a shot either, so it’s fine with me.” (Participant 17, unvaccinated young adult) |
| Patient | Misinformation surrounding the HPV vaccine | “I think all of the conspiracy theories that are out there now, and it’s even worse since COVID, nobody trusts, or a lot of people don’t trust public health messages anymore.” (Participant 12, health systems) | |
| Patient | Stigma surrounding HPV |
“Well, I think part of it is that since it is sexually transmitted, I think that a lot of parents don’t want to really delve into that thought that their kids are being sexually active or may be sexually active soon” (Participant 1, parent of vaccinated child)
“I think the – I think stigma, because it is associated with sexual – a sexual nature. So, they kind of clam up like here in southwest Georgia, Bible belt, like it’s just kind of a – you know, you don’t speak of those things. Those are kind of taboo. Like everybody knows it’s occurring, but you don’t really want to I guess see your child doing – you know, doing things like that. So, I think it’s just the culture here.” (Participant 15, health systems) |
|
| Lack of direct and consistent communication with the patient/parent | Provider | N/A | “…they presented it, and asked did I want him to receive the vaccine, but at that time, I just had not had enough information on it personally, and with that, they did not give me any more information. And so, with that being said, you know, if my – if the doctor is not willing to provide more and give me more insight into it, any side effects, you know, statistics, and things of the sort, then you know, (laughs) yeah.” (Participant 2, parent of unvaccinated child). |
| Provider | Provider not advertising the HPV vaccine to patients |
“I think maybe lack of consistent recommendations. You know, they may get tied up in, you know, other bunch of check list of things that they’ve got to do and then may – it just may not be consistent throughout the how…” (Participant 39 Health systems)
“I feel they should be more open and mention it in an exam. I do. I feel like they should. Not just have the poster up, like in the hallway. They still should mention it. The same way that they’re stressing the COVID vaccine, they should stress that vaccine in the same manner, I think.” (Participant 35, parent of unvaccinated child) |
|
| Health Systems immunization lack of reminders to patients/availability | Practice | N/A | “Yeah. I think that like, for example, in my case, if there were an actual mailing that came to our house-…I would have seen it. I would have at least began a conversation with my husband about it, and he was the one responsible for taking him to the pediatrician and getting it handled.” (Participant 1, parent of vaccinated child) |
| Limited time, information, staff, and resources | Practice | N/A | “Time would be one I would see, because with a lot of the things that we’re having to do now, you don’t’ have as much time to do the education as you would like to, and sometimes when you’re talking about sex and HPV, if it’s on a one to one basis, it’s hard to establish a rapport in five, ten minutes and get all the information that you need to get to them and then allow them to ask questions” (Participant 25, health system) |
| Differences in private practices vs public health departments | Practice | N/A |
“If you’re more familiar with the doctor you have more trust, and you’re more likely to take their advice. When you go to one of the local clinics, the convenient care clinics, it’s not a guarantee you’re going to get the same doctor. So, you may not be as comfortable having a certain conversation with one doctor as you would with a doctor that you’re used to seeing on a regular basis” (Participant 13, Parent with a vaccinated child)
“Private, is not private, and a lot of people may avoid going to the health department and would rather go to an outside pediatrician but don’t have the transportation to get there (Participant 6, Parent with a vaccinated child) |
| Lack of transportation | Community | N/A | “If I didn’t have a car, I probably wouldn’t even – I would barely go to the doctor if I had to use public transportation” (Participant 27, Parent with an unvaccinated child) |
| Lack of community discourse on the HPV vaccine | Community | N/A | “No, just that there is really not a lot of talks about it. I definitely think there needs to be more communication about it for sure” (Participant 17, unvaccinated Young adult) |
| Financial barriers | Policy | N/A | “…some insurances don’t cover vaccines, so the parents have to end up paying out of pocket…” (Participant 15, health systems) |
Patient level
At the patient level, a persistent theme among parents of both vaccinated and unvaccinated children in our study focused on a dearth of knowledge among parents and their communities about the importance of vaccinating their children against HPV. They highlighted how it is not a common topic to be discussed among parents with their children. One young adult described their experience as a child, “They’re (doctor) like, oh yeah, we now offer the HPV vaccine. Is it something you want to get? And my mom was like, eh, no, she doesn’t need that right now. And I was like, okay. I don’t really want a shot either, so it’s fine with me.” (Participant 17, unvaccinated young adult). Not only is it not being discussed, but parents described not knowing where to go to find more information about the vaccine. Health system participants also discussed how parents often did not have the necessary knowledge about the vaccine to effectively make decisions on behalf of their children. Stemming from this lack of education is the impact that misinformation has surrounding the efficacy, safety, and utility of the HPV vaccine. Two non-vaccinated young adults address misinformation, one stated, “…they’re [young adults] very hesitant about getting like even the COVID vaccine, just because, you know, they heard rumors, oh, it has this in it, it has that in it…” another stated, “They [young adults] look at social media and certain people may say this is what they do, this is what they don’t do, this is that. So I think actually with social media and peer pressure that conveys a lot of the youth.”
A director of a non-profit described, “I think all of the conspiracy theories that are out there now, and it’s even worse since COVID, nobody trusts, or a lot of people don’t trust public health messages anymore.” (Participant 12, health systems). In this context, the participant emphasizes the challenge of discussing the vaccine with parents and how a lack of trust in public health complicates messaging strategies.
Coupled with this misinformation was the resulting stigma of discussing HPV due to it being a STI. Vaccinated and unvaccinated young adults, both parents of vaccinated and unvaccinated children, and health system participants described how some parents may be reluctant to vaccinate their child, because they perceive it to indicate their child could be engaging in sex, or receiving the vaccine encourages the child to be sexually active. As one parent described, “Well, I think part of it is that since it is sexually transmitted, I think that a lot of parents don’t want to really delve into that thought that their kids are being sexually active or may be sexually active soon” (Participant 1, parent of vaccinated child). Particularly in southwest Georgia, sexual intercourse is stigmatized. As one provider described,
“I think the – I think stigma, because it is associated with sexual – a sexual nature. So, they kind of clam up like here in southwest Georgia, Bible belt, like it’s just kind of a – you know, you don’t speak of those things. Those are kind of taboo. Like everybody knows it’s occurring, but you don’t really want to I guess see your child doing – you know, doing things like that. So, I think it’s just the culture here” (Participant 15, health systems nurse).
By attempting to discuss a vaccine to prevent STIs, health system participants believed this may contradict many who view teenage sexual health education as only relevant through abstinence.
Provider level
At the provider level, parents of unvaccinated children and young adults (both vaccinated and unvaccinated) alluded to the dearth of direct communication with providers about the vaccine and revisiting the topic with their patients. Specifically, some parents described how their child’s doctor did not educate them on the reasons for getting the vaccine. As one parent described their experience with a doctor as:
“…they presented it, and asked did I want him to receive the vaccine, but at that time, I just had not had enough information on it personally, and with that, they did not give me any more information. And so, with that being said, you know, if my – if the doctor is not willing to provide more and give me more insight into it, any side effects, you know, statistics, and things of the sort, then you know, (laughs) yeah.” (Participant 2, parent of unvaccinated child).
This parent highlighted how they may have been convinced had the doctor provided more details about the reason for vaccinating their child. Another parent with an unvaccinated child described providers not revisiting the HPV vaccine with them at later visits if the parent initially said “no.” Aligned with the lack of direct communication, providers were not informing and recommending the HPV vaccine to patients. As a director of a non-profit stated, “I think maybe lack of consistent recommendations. You know, they may get tied up in, you know, other bunch of check list of things that they’ve got to do and then may – it just may not be consistent throughout the flow…” (Participant 39, health systems). A parent also felt the providers need to be speaking more about the HPV vaccine in the exam room. One parent described, “I feel they should be more open and mention it in an exam. I do. I feel like they should. Not just have the poster up, like in the hallway. They still should mention it. The same way that they’re stressing the COVID vaccine, they should stress that vaccine in the same manner, I think.” (Participant 35, parent of unvaccinated child). Here, the parent wished the approach to HPV and the HPV vaccine was similar to the COVID-19 vaccine in order for them to understand its importance during their child’s visits.
Practice level
At the practice level, participants described lack of systematic reminders for patient immunizations, limited time, resources, and staff allocated per patient, and lack of education in the clinic or medical offices. A parent of each a vaccinated and unvaccinated child referenced not receiving vaccine reminders. One of the parents stated: “Yeah. I think that like, for example, in my case, if there were an actual mailing that came to our house-…I would have seen it. I would have at least begun a conversation with my husband about it, and he was the one responsible for taking him to the pediatrician and getting it handled.” (Participant 1, parent of vaccinated child). Although their child was vaccinated, the need for a mailed reminder would have facilitated discussions between the parents about vaccinating their child. Similarly, a young adult who received their first shot did not return for their second shot since they did not know when to return to the doctor’s office. Other barriers at the practice level include limited information, time, staff, and resources dedicated to the HPV vaccine. Both parents and health system participants mentioned time being a factor. One provider stated,
“Time would be one I would see, because with a lot of the things that we’re having to do now, you don’t’ have as much time to do the education as you would like to, and sometimes when you’re talking about sex and HPV, if it’s on a one to one basis, it’s hard to establish a rapport in five, ten minutes and get all the information that you need to get to them and then allow them to ask questions” (Participant 25, health system nurse).
As for the lack of resources, parents with a vaccinated child mentioned they have seen posters about measles, mumps, and rubella but not on the HPV vaccine and clinics not having enough of vaccines to distribute. A barrier widely mentioned across participants (parents, young adults unvaccinated, and health systems) were the differences between private practices and public health departments in rural communities. The differences between the two discussed were the patient-provider relationship and patient privacy differences. A parent explained:
“If you’re more familiar with the doctor you have more trust, and you’re more likely to take their advice. When you go to one of the local clinics, the convenient care clinics, it’s not a guarantee you’re going to get the same doctor. So, you may not be as comfortable having a certain conversation with one doctor as you would with a doctor that you’re used to seeing on a regular basis” (Participant 13, parent with a vaccinated child).
Another parent stated, “Private, is not private, and a lot of people may avoid going to the health department and would rather go to an outside pediatrician but don’t have the transportation to get there (Participant 6, parent with a vaccinated child). This parent explained health department layouts are openly structured and patients get called to a window to discuss their health information and people in the waiting room can hear those discussions, causing a lack of privacy for the patient, Similarly, a young adult unvaccinated also mentioned how privacy and courtesy of health professionals at certain clinics can be a barrier for patients. A lack of privacy is a concern at a patient level, while limited resources for transportation infrastructure affect the community at large.
Community and Policy levels
Several barriers at the community and policy level were mentioned by participants. At the community level the barriers include inadequate transportation, and lack of information within the community about HPV and the HPV vaccine and resources. A parent alluded to how important having a car is: “If I didn’t have a car, I probably wouldn’t even – I would barely go to the doctor if I had to use public transportation” (Participant 27, parent with an unvaccinated child). There is public transportation, but it takes more time and some unvaccinated young adults also stated how rural communities are spread out, which makes it challenging to travel to clinics that are out of their town and far away. A young adult described the lack of discussion around the vaccine in their community: “No, just that there is really not a lot of talks about it. I definitely think there needs to be more communication about it for sure” (Participant 17, unvaccinated young adult). At the policy level, the two main barriers participants mentioned were the financial barriers and lack of policies facilitating the uptake of the HPV vaccine. A provider described not being able to provide the vaccine to a minor without parental consent, “…hey, we can’t give them to you, because you’re not 18. We can give you, you know, reproductive care, but we cannot give you any vaccine without your parents’ permission” (Participant 15, health system nurse).
DISCUSSION
Facilitators
Our study used the P3 Model framework and found common facilitators and barriers to receipt of the HPV vaccine in rural communities. Some of the facilitators we found were trusted individuals in the community, existing knowledge, and providers stating the vaccine is a cancer prevention tool. Parent participants from a study in Alabama reported that guidance from pediatricians or family physicians influenced their decision to vaccinate their children against HPV.27 Another study in Montana noted parents may be more receptive to the HPV vaccine when it is discussed as a cancer prevention tool rather than a STI prevention tool.28 A pivotal facilitator at the provider level in our study involved how providers phrase and frame the HPV vaccine to patients. Medical providers and public health stakeholders from a prior study in Montana identified a presumptive style of recommending the HPV vaccine. An announcement and conversation training HPV intervention for providers led to an increase in HPV vaccinations for adolescents ages 11–18 over those in a control group in North Carolina.29,30 This style included offering the HPV vaccine with other immunizations such as meningococcal, HPV, and Tdap together, which was successful.28,30
Additionally, our research revealed that immunization reminders were a key facilitator in improving HPV vaccination rates. A study in rural Alabama similarly reported that receiving appointment reminders via card, call, or text was helpful in ensuring all doses were received.31 Similarly, healthcare provider participants from a study in Georgia highlighted the importance of scheduling subsequent HPV vaccine appointments before patients leave their first vaccination appointment and use of reminder systems.16 In addition to immunization reminders, health education material such as educational videos, and incorporating the use of social media was mentioned as strategies to engage people on the HPV vaccine by our participants. Our participants suggest that employing simplified strategies will better attract and engage the general population more, especially those with lower health literacy. Previous research found that rural communities need increased access to education on HPV, the HPV vaccine, and sexual health.32
In addition to examining facilitators within the P3 Model, we also looked at community and policy level factors. From our study, the community facilitators were trusted community key stakeholders and how they were instrumental in the development of interventions,33 community and school education programs,34 and county-wide social marketing campaigns.35 Our participants mentioned having webinars and the use of school events and outreach is beneficial for increasing the uptake of the HPV vaccine.
Future research could investigate interventions like technological reminders and capacity-building for rural healthcare systems to boost HPV vaccination rates. Additionally, future HPV vaccine promotion efforts could focus on community education and participation in campaigns such as the American Cancer Society’s Mission HPV Cancer Free.36 At the policy level, some existing facilitators were the Vaccines for Children (VFC) program and private clinics instituting standing orders within their practice for the HPV vaccine.37 The VFC was designed so children can receive vaccines regardless if the parent or guardian can afford the vaccines. Similarly, our study participants mentioned how beneficial vaccine programs are not only children but for adults too.
Barriers
Data from the 2010–2020 National Immunization Survey-Teen identified the following barriers to receiving the HPV vaccine: lack of knowledge, abstinence, safety concerns, and viewing the vaccine as unnecessary.38 A lack of knowledge on HPV was reported as a prominent barrier among our rural participants, which has been observed across multiple rural-based studies16,17,27,31,39 Studies in rural Alabama found a lack of parental understanding about the HPV vaccine was a key barrier as reported by parents, pediatricians, and nurse participants.17,31 Provider participants from a quantitative study reported vaccinating adolescent females (13–17 years old) at higher rates compared to pre-adolescent females (9–12 years old).40 Barriers such as parental discomfort and potential adverse side effects in vaccinating their pre-adolescent child against HPV, especially if the child has underling health conditions can influence the age group disparity in vaccine uptake.40,41
Another frequently discussed barrier in our study was stigma surrounding HPV as a STI and challenges in discussing sexual health, particularly given the conservative nature of southwest Georgia, located in the “Bible Belt” region. Previous research in the south (Georgia, Alabama, Kentucky, and North and South Carolina) found that parental perception of the HPV vaccination encouraging or permitting sexual activity discourages parents from having their child vaccinated against HPV.16,27,32,39 Prior research with healthcare providers from Georgia noted providers avoid discussing sex at all when recommending the HPV vaccine due to STI stigma.16
Similarly, a lack of provider recommendations or discussion about HPV was a prominent barrier among our participants, consistent with previous literature.16,31,38 According to providers in Georgia, low provider confidence in the HPV vaccine can pose as a barrier to giving patients strong recommendations for the vaccine.16 A national survey examining the quality of physician recommendation for HPV vaccination revealed that physicians in the sample often lacked consistency, urgency, and timeliness in their recommendation of the HPV vaccine.42 Strategies such as education from other lay health professionals such as community health workers or navigators, training or mentoring of providers through technology, or partnering with other health organizations may be possible intervention strategies to explore.43 Provider training on strong recommendations and presumptive communication have been effective in approaching this discussion about the HPV vaccine with parents and/or adolescents and effective in promoting vaccination.29,44 This type of training should be delivered to rural public health and healthcare providers to address these barriers.45
Additionally, we found that a lack of patient reminders can hinder increases in HPV vaccination rates, which has been observed in prior studies. Reminder cards can easily be lost, so technology-based options, particularly email or text should be utilized based on individual patient preference.39 However, not all rural areas have the capacity to utilize text messaging based on limited cellar service.46 Future efforts to increase HPV vaccination need to include relevant reminders for patients and/or caregivers. In addition to a lack of patient reminders, there is a lack of privacy within healthcare for patients. As shown in our study, patients commented on the lack of privacy at health departments and previous research highlights healthcare does not have appropriate privacy protections for patients.47 Moreover, our participants noted that in rural areas, inadequate staffing and resources were also barriers to HPV vaccine uptake. A study in rural North and South Carolina also found that provider shortages in rural areas results in fewer opportunities for parents and adolescents to learn about the HPV vaccine.32
From previous research, barriers at the community level consist of a lack of transportation and how it negatively affects people getting to their appointments to receive medical care.48,49 Participants in our study mentioned how a lack of transportation is a challenge, especially when one does not own a car or is unable to drive. Future research can explore methods to increase vaccinations outside of clinical settings including community settings or in pharmacies, recommended by the President’s Cancer Panel report.50
Similarly, a lack of policies can impact the uptake of the HPV vaccine. For example, the HPV vaccine is not routinely mandated for school entry at the state level unlike other vaccines such as Tdap. While all states and the District of Columbia have middle school entry requirements for Tdap vaccination, only four U.S. jurisdictions (Rhode Island, Virginia, Puerto Rico, and District of Columbia) currently have HPV vaccination requirements.37,51 Georgia did propose a bill in 2019 to allow adolescents younger than 16 to consent to vaccinations without parental consent, however the bill did not pass.52,53 Due to this, minors will need parental approval in order to receive the vaccine and our participants explained the difficulty of this. Other policy barriers are financial vaccine burdens on health systems who administer the vaccines and lack of reimbursement from insurance companies.54 Future implementation and evaluation of HPV policies (e.g., school or policy requirements) could assess policy impacts on HPV vaccine uptake.
Strengthens and Limitations
The strengths of this study include interviewing three categories of community stakeholders and receiving their insights on the facilitators and barriers of the HPV vaccine in rural Georgia. In addition, for parents and young adults, we received perspectives from those who received and did not receive the HPV vaccine. Using the P3 Model in our study and the subsequent findings, allowed for consideration of multi-level interventions for increasing HPV vaccination. Research has shown numerous programs that promote HPV vaccination operate at a single level.55 Mostly focusing on either the patient or provider levels and a lack of focus of including facilitators and barriers at the practice level.56–58 Public health professionals and providers can learn from these facilitators and barriers to test strategies at different levels to increase rural HPV vaccination rates. However, our study has some limitations. There were delays in recruitment because of participants limited time due to the impact of the COVID-19 pandemic. We had to pause recruiting providers because the community asked us to due to the demands of the pandemic and we focused our efforts on recruiting parents and young adults for the study.
CONCLUSION
Identifying multi-level facilitators and barriers influencing HPV vaccination is necessary in increasing vaccine uptake, particularly in rural areas where vaccine coverage is disproportionately low. We found some key barriers at all 3 levels of the P3 model including misinformation, lack of knowledge, provider-patient communication, provider recommendation, lack of systematic reminders, and limited time and resources. These barriers showcase the need for future research to explore the effectiveness of the following strategies in rural communities: HPV vaccine education in rural communities through public health providers, provider training on strong recommendations, and technological health systems activities such as patient reminders.
Funding:
This study was supported by Centers for Disease Control and Prevention, SIP 19-005 Cancer Prevention and Control Research Network, U48 DP006377 and Winship Cancer Institute, P30CA138292. The funders had no role in the study design, data collection, analysis, and interpretation of data and in writing the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the CDC. The authors thank the members of the Emory Prevention Research Center’s Community Advisory Board for their many contributions to this project. They thank the organizations and participants that participated in this qualitative study.
Abbreviations
- HPV
Human papillomavirus
- P3
Model Patient-provider-practice-level Model
Footnotes
Competing interests: The authors declare that they have no relevant financial or non-financial competing interests to disclose.
Declarations
Ethics considerations: We submitted the protocol and instruments to the Emory University IRB for project approval and consent to participate. The IRB deemed this study exempt because the study meets the criteria for exemption under 45 CFR 46.104(d)(2) from Emory University.
Consent to participate: Verbal consent was obtained by all participants who enrolled in the study.
Contributor Information
Courtney N. Petagna, Emory University
Stephen Perez, Emory University.
Erica Hsu, Emory University.
Brenda M. Greene, Georgia Department of Public Health
Ionie Banner, Emory University.
Robert A. Bednarczyk, Emory University
Cam Escoffery, Emory University.
Data availability:
The data supports the findings of this study are available in tables and supplementary materials of this article. We can share general data matrices or summaries of the qualitative data if there are request. Since this is a qualitative data and there are sensitive information about the vaccine and perhaps health systems, we will not share the actual transcripts. Contact Courtney Petagna (cnpetagna@gmail.com) or Cam Escoffery (cescoff@emory.edu)
References
- 1.CDC. Sexually Transmitted Infections Prevalence, Incidence, and Cost Estimates in the United States. (https://www.cdc.gov/std/statistics/prevalence-2020-at-a-glance.htm). [Google Scholar]
- 2.CDC. Cancers Associtated with Human Papillmavirus, United States, 2015–2019. (https://www.cdc.gov/cancer/uscs/about/data-briefs/no31-hpv-assoc-cancers-UnitedStates-2015-2019.htm). [Google Scholar]
- 3.Bauer HM, Wright G, Chow J. Evidence of human papillomavirus vaccine effectiveness in reducing genital warts: an analysis of California public family planning administrative claims data, 2007–2010. Am J Public Health. 2012;102(5):833–5. 10.2105/ajph.2011.300465. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC. Vaccines (Shots). March/13/2023. (https://www.cdc.gov/cancer/dcpc/prevention/vaccination.htm). [Google Scholar]
- 5.Seyferth ER, Bratic JS, Bocchini JA Jr. Human papillomavirus epidemiology and vaccine recommendations: selected review of the recent literature. Curr Opin Pediatr. 2016;28(3):400–6. 10.1097/mop.0000000000000354. (In eng) [DOI] [PubMed] [Google Scholar]
- 6.Rosenblum HG, Lewis RM, Gargano JW, Querec TD, Unger ER, Markowitz LE. Human Papillomavirus Vaccine Impact and Effectiveness Through 12 Years After Vaccine Introduction in the United States, 2003 to 2018. Ann Intern Med. 2022;175(7):918–26. 10.7326/m21-3798. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human Papillomavirus Vaccination for Adults: Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2019;68(32):698–702. 10.15585/mmwr.mm6832a3. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. HPV Vaccine. (https://www.cdc.gov/hpv/parents/vaccine-for-hpv.html). [Google Scholar]
- 9.Petrosky E, Bocchini JA Jr., Hariri S, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2015;64(11):300–4. (In eng). [PMC free article] [PubMed] [Google Scholar]
- 10.USDHHS, Healthy People. 2030. U.S. Department of health and human services. (https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08). [DOI] [PubMed] [Google Scholar]
- 11.Pingali CYD, Elam-Evans LD, Markowitz LE, Valier MR, Benjamin Fredua B, Crowe SJ, DeSisto CL, Stokley S, Singleton JA. Vaccination Coverage Among Adolescents Aged 13–17 Years — National Immunization Survey–Teen, United States, 2022. MMWR Morb Mortal Wkly Rep 2023. 10.15585/mmwr.mm7234a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CDC, TeenVaxView Interactive!. 2021. May 13, 2021 (https://www.cdc.gov/vaccines/imz-managers/coverage/teenvaxview/data-reports/index.html). [Google Scholar]
- 13.Pingali C, Yankey D, Elam-Evans LD, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years-United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(35):1183–90. 10.15585/mmwr.mm7035a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.GDPH. Adolescent Report 2020. (https://dph.georgia.gov/immunization-study-reports). [Google Scholar]
- 15.Dennison C, King AR, Rutledge H, Bednarczyk RA. HPV Vaccine-Related Research, Promotion and Coordination in the State of Georgia: A Systematic Review. J Community Health. 2019;44(2):313–21. 10.1007/s10900-018-0589-7. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vu M, King AR, Jang HM, Bednarczyk RA. Practice-, provider- and patient-level facilitators of and barriers to HPV vaccine promotion and uptake in Georgia: a qualitative study of healthcare providers’ perspectives. Health Educ Res. 2020;35(6):512–23. 10.1093/her/cyaa026. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dilley SE, Peral S, Straughn JM Jr., Scarinci IC. The challenge of HPV vaccination uptake and opportunities for solutions: Lessons learned from Alabama. Prev Med. 2018;113:124–31. 10.1016/j.ypmed.2018.05.021. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76–82. 10.1001/jamapediatrics.2013.2752. (In eng). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paskett ED, Krok-Schoen JL, Pennell ML, et al. Results of a Multilevel Intervention Trial to Increase Human Papillomavirus (HPV) Vaccine Uptake among Adolescent Girls. Cancer Epidemiol Biomarkers Prev. 2016;25(4):593–602. 10.1158/1055-9965.Epi-15-1243. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruffin MTt Hade EM, Gorsline MR, et al. Human papillomavirus vaccine knowledge and hypothetical acceptance among women in Appalachia Ohio. Vaccine. 2012;30(36):5349–57. 10.1016/j.vaccine.2012.06.034. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryan C, Duvall KL, Weyant EC, Johnson KR, Wood D. Human Papillomavirus Vaccine Uptake, Knowledge, and Acceptance for Youth: A Systematic Review of Appalachia. J Community Health. 2018;43(3):616–24. 10.1007/s10900-018-0500-6. (In eng) [DOI] [PubMed] [Google Scholar]
- 22.Thomas TL, Strickland O, Diclemente R, Higgins M. An opportunity for cancer prevention during preadolescence and adolescence: stopping human papillomavirus (HPV)-related cancer through HPV vaccination. J Adolesc Health. 2013;52(5 Suppl):60–8. 10.1016/j.jadohealth.2012.08.011. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bednarczyk RA, Chamberlain A, Mathewson K, Salmon DA, Omer SB, Practice-. Provider-, and Patient-level interventions to improve preventive care: Development of the P3 Model. Prev Med Rep. 2018;11:131–8. 10.1016/j.pmedr.2018.06.009. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hennink M, Hutter I, Bailey A. Qualitative Research Methods. Thousand Oaks CA: Sage Publication; 2020. [Google Scholar]
- 25.VERBI. MAXQDA 2022. Software. maxqda.com; 2021. [Google Scholar]
- 26.Miles H, Huberman AM, Saldana J. Qualitative data analysis: A methods sourcebook. 4th ed. Thousand Oaks, CA: Sage Publication; 2019. [Google Scholar]
- 27.Westrick SC, Hohmann LA, McFarland SJ, Teeter BS, White KK, Hastings TJ. Parental acceptance of human papillomavirus vaccinations and community pharmacies as vaccination settings: A qualitative study in Alabama. Papillomavirus Res. 2017;3:24–9. 10.1016/j.pvr.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Newcomer SR, Caringi J, Jones B, Coyle E, Schehl T, Daley MF. A Mixed-Methods Analysis of Barriers to and Facilitators of Human Papillomavirus Vaccination Among Adolescents in Montana. Public Health Rep. 2020;135(6):842–50. 10.1177/0033354920954512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements Versus Conversations to Improve HPV Vaccination Coverage: A Randomized Trial. Pediatrics. 2017;139(1). 10.1542/peds.2016-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moss JL, Reiter PL, Rimer BK, Brewer NT. Collaborative patient-provider communication and uptake of adolescent vaccines. Soc Sci Med. 2016;159:100–7. 10.1016/j.socscimed.2016.04.030. (In eng). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boyd ED, Phillips JM, Schoenberger YM, Simpson T. Barriers and facilitators to HPV vaccination among rural Alabama adolescents and their caregivers. Vaccine. 2018;36(28):4126–33. 10.1016/j.vaccine.2018.04.085. [DOI] [PubMed] [Google Scholar]
- 32.Fish LJ, Harrison SE, McDonald JA, et al. Key stakeholder perspectives on challenges and opportunities for rural HPV vaccination in North and South Carolina. Hum Vaccin Immunother. 2022;18(5):2058264. 10.1080/21645515.2022.2058264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crosby LE, Real FJ, Cunnigham J, Mitchell M. Overcoming Vaccine Hesitancy Using Community-Based Efforts. Pediatr Clin North Am. 2023;70(2):359–70. 10.1016/j.pcl.2022.11.012. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Niccolai LM, Hansen CE. Practice- and Community-Based Interventions to Increase Human Papillomavirus Vaccine Coverage: A Systematic Review. JAMA Pediatr. 2015;169(7):686–92. 10.1001/jamapediatrics.2015.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peterson CE, Silva A, Holt HK, Balanean A, Goben AH, Dykens JA. Barriers and facilitators to HPV vaccine uptake among US rural populations: a scoping review. Cancer Causes Control. 2020;31(9):801–14. 10.1007/s10552-020-01323-y. [DOI] [PubMed] [Google Scholar]
- 36.Our HPV, vaccination initiatives.. American Cancer Society. (https://www.cancer.org/health-care-professionals/hpv-vaccination-information-for-health-professionals/our-hpv-vaccination-initatives.html). [Google Scholar]
- 37.Vanderpool RC, Stradtman LR, Brandt HM. Policy opportunities to increase HPV vaccination in rural communities. Hum Vaccines Immunotherapeutics. 2019;15(7–8):1527–32. 10.1080/21645515.2018.1553475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adjei Boakye E, Nair M, Abouelella DK et al. Trends in Reasons for Human Papillomavirus Vaccine Hesitancy: 2010–2020. Pediatrics 2023;151(6). 10.1542/peds.2022-060410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Head KJ, Vanderpool RC, Mills LA. Health care providers’ perspectives on low HPV vaccine uptake and adherence in Appalachian Kentucky. Public Health Nurs. 2013;30(4):351–60. 10.1111/phn.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCave EL. Influential factors in HPV vaccination uptake among providers in four states. J Community Health. 2010;35(6):645–52. 10.1007/s10900-010-9255-4. [DOI] [PubMed] [Google Scholar]
- 41.Bairu W, King AR, Bednarczyk RA. Caregivers of Adolescents’ Motivators and Barriers to Vaccinating Children Against Human Papillomavirus. J Prev (2022) 2022;43(3):407–420. (In eng). 10.1007/s10935-022-00674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gilkey MB, Malo TL, Shah PD, Hall ME, Brewer NT. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev. 2015;24(11):1673–9. 10.1158/1055-9965.EPI-15-0326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Levit LA, Byatt L, Lyss AP, et al. Closing the Rural Cancer Care Gap: Three Institutional Approaches. JCO Oncol Pract. 2020;16(7):422–30. 10.1200/OP.20.00174. [DOI] [PubMed] [Google Scholar]
- 44.Constable C, Ferguson K, Nicholson J, Quinn GP. Clinician communication strategies associated with increased uptake of the human papillomavirus (HPV) vaccine: A systematic review. CA Cancer J Clin. 2022;72(6):561–9. 10.3322/caac.21753. [DOI] [PubMed] [Google Scholar]
- 45.Brewer NT, Mitchell CG, Alton Dailey S, et al. HPV vaccine communication training in healthcare systems: Evaluating a train-the-trainer model. Vaccine. 2021;39(28):3731–6. 10.1016/j.vaccine.2021.05.038. [DOI] [PubMed] [Google Scholar]
- 46.Cherryhomes E, Guillot-Wright S. Dissemination and Implementation of a Text Messaging Campaign to Improve Health Disparities among Im/Migrant Workers. Int J Environ Res Public Health. 2023;20(7). 10.3390/ijerph20075311. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bednarczyk RA, Nadeau JA, Davis CF et al. Privacy in the pharmacy environment: analysis of observations from inside the pharmacy. J Am Pharm Assoc (2003) 2010;50(3):362–7. (In eng). 10.1331/JAPhA.2010.09001. [DOI] [PubMed] [Google Scholar]
- 48.White AA, Neelon B, Martin RH, et al. Predicting HPV vaccination among Tdap vaccinated adolescents in Georgia at the county level. Ann Epidemiol. 2022;70:74–8. 10.1016/j.annepidem.2022.03.008. [DOI] [PubMed] [Google Scholar]
- 49.Wercholuk A, Parikh, Alexander MD, Snyder MPH, Rebecca MD. The Road Less Traveled: Transportation Barriers to Cancer Care Delivery in the Rural Patient Population. JCO Oncol Pract. 2022;18(9):652–62. 10.1200/OP.22.00122. [DOI] [PubMed] [Google Scholar]
- 50.Health NIo. Accelerating HPV vaccine uptake: Urgency for action to prevent cancer: Goal 3: Maximize access to HPV vaccination services. U S Department Health Hum Serv. (https://deainfo.nci.nih.gov/advisory/pcp/annualreports/hpv/Part3Goal3.htm).
- 51.Roundtable H. School Entry Requirements for HPV Vaccine. 2019. (http://hpvroundtable.org/wp-content/uploads/2019/09/05_School_Entry_Requirements_for_HPV_Vaccination_WEB_updated.pdf). [Google Scholar]
- 52.Zimet GD, Silverman RD, Bednarczyk RA, English A. Adolescent Consent for Human Papillomavirus Vaccine: Ethical, Legal, and Practical Considerations. J Pediatr. 2021;231:24–30. 10.1016/j.jpeds.2021.01.026. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Georgia HB. 2019–2020: Regular session. (https://legiscan.com/GA/bill/HB615/2019). [Google Scholar]
- 54.Ellingson MK, Bednarczyk RA, O’Leary ST, Schwartz JL, Shapiro ED, Niccolai LM. Understanding the Factors Influencing Health Care Provider Recommendations about Adolescent Vaccines: A Proposed Framework. J Behav Med. 2023;46(1–2):356–65. 10.1007/s10865-022-00296-4. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Escoffery C, Petagna C, Agnone C, et al. A systematic review of interventions to promote HPV vaccination globally. BMC Public Health. 2023;23(1):1262. 10.1186/s12889-023-15876-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lake PW, Kasting ML, Christy SM, Vadaparampil ST. Provider perspectives on multilevel barriers to HPV vaccination. Hum Vaccin Immunother. 2019;15(7–8):1784–93. 10.1080/21645515.2019.1581554. (In eng). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bednarczyk RA, Brewer NT, Gilkey MB, et al. Human papillomavirus vaccination at the first opportunity: An overview. Hum Vaccin Immunother. 2023;19(1):2213603. 10.1080/21645515.2023.2213603. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bednarczyk RA, Brandt HM. Descriptive epidemiology of age at HPV vaccination: Analysis using the 2020 NIS-Teen. Hum Vaccin Immunother. 2023;19(1):2204784. 10.1080/21645515.2023.2204784. (In eng) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supports the findings of this study are available in tables and supplementary materials of this article. We can share general data matrices or summaries of the qualitative data if there are request. Since this is a qualitative data and there are sensitive information about the vaccine and perhaps health systems, we will not share the actual transcripts. Contact Courtney Petagna (cnpetagna@gmail.com) or Cam Escoffery (cescoff@emory.edu)